Abstract
Objective:
This study examined the effects of optimism and gratitude on self-reported health behavior adherence, physical functioning and emotional well-being after an acute coronary syndrome (ACS).
Methods:
Among 156 patients, we examined associations between optimism and gratitude measured 2 weeks post-ACS and 6-month outcomes: adherence to medical recommendations, mental and physical health-related quality of life (HRQoL), physical functioning, depressive symptoms and anxiety. Multivariable linear regression models were used, controlling for increasing levels of adjustment.
Results:
Optimism [β=.11, standard error (S.E.)=.05, P=.038] and gratitude (β=.10, S.E.=.05, P=.027) at 2 weeks were associated with subsequent self-reported adherence to medical recommendations (diet, exercise, medication adherence, stress reduction) at 6 months in fully adjusted models. Two-week optimism and gratitude were associated with improvements in mental HRQoL (optimism: β=.44, S.E.=.13, P=.001; gratitude: β=.33, S.E.=.12, P=.005) and reductions in symptoms of depression (optimism: β=−.11, S.E.=.05, P=.039; gratitude: β=−.10, S.E.=.05, P=.028) and anxiety (optimism: β=−.15, S.E.=.05, P=.004; gratitude: β=−.10, S.E.=.05, P=.034) at 6 months.
Conclusion:
Optimism and gratitude at 2 weeks post-ACS were associated with higher self-reported adherence and improved emotional well-being 6 months later, independent of negative emotional states. Optimism and gratitude may help recovery from an ACS. Interventions promoting these positive constructs could help improve adherence and well-being.
Keywords: Optimism, Gratitude, Acute coronary syndrome, Mental health, Adherence
1. Introduction
Over one million Americans suffer from an acute coronary syndrome (ACS: myocardial infarction or unstable angina) each year [1–5], and rates of rehospitalization and death in the following year are high [6]. Psychological well-being may improve cardiac-related outcomes, independent of cardiac risk factors and negative emotional states [7]. Optimism, defined as positive expectations about the future [8], is a relatively well-studied positive psychological construct. For example, optimism has been independently associated with improved functioning and superior cardiac health [9]. While optimism has been studied in depth in the cardiac and health behavior literature, less is known about other positive constructs. We therefore chose to explore another common positive psychological construct, gratitude. Gratitude is defined as noticing and appreciating the positive [10]. Gratitude is commonly experienced following an ACS [11] and may also have effects on health outcomes, but it has been less well studied in this context [10]. Gratitude can be a powerful positive feeling following a life-threatening event. There are indications that gratitude and gratitude interventions may improve well-being and some physical markers of cardiac health [12–14]. The present study seeks to explore whether these two positive emotions, optimism and gratitude, have similar effects on a variety of cardiac outcomes.
Several pathways have been hypothesized for the beneficial effects of positive psychological constructs on cardiac health. First, positive constructs may affect cardiovascular physiology. Negative psychological syndromes (e.g., depression) are associated with abnormal levels of inflammatory cytokines and related biomarkers that have been linked to adverse cardiac outcomes [15,16]. Positive psychological constructs have been linked to improvements in cardiac biomarkers, though the findings have been mixed [17–19]. Optimism and other positive constructs have also been more consistently associated with greater adherence to health behaviors, including healthy diet, physical activity and smoking cessation [7]. Greater levels of baseline psychological well-being may also protect from subsequent development of depression and anxiety [20], which may be important given the connections of these syndromes with adverse cardiovascular events following an ACS [21].
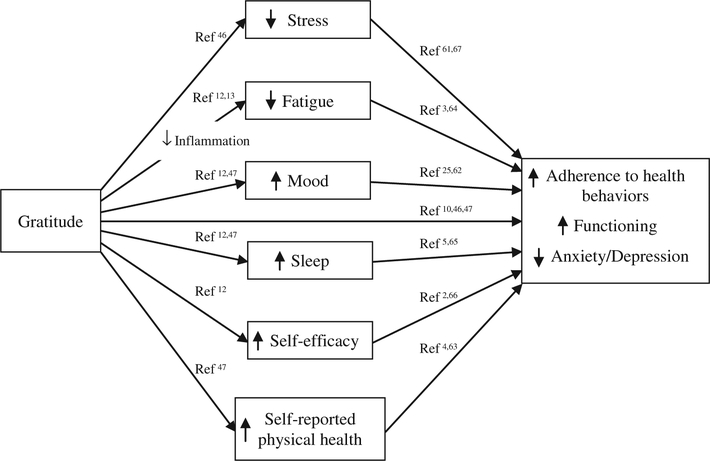
Though there is a substantial body of literature on the relationships between optimism and heart disease [7], there are less data available on gratitude in this context, despite its potential utility in understanding cardiac health. There is evidence to suggest that gratitude can influence a variety of cardiac-related outcomes, potentially mediated through emotions and behaviors such as sleep, self-efficacy, and mood. A conceptual model outlines these hypothesized relationships (Fig. 1).
Fig. 1.
Conceptual model of the relationships between gratitude and the outcomes used in this study.
No prior studies had simultaneously examined the prospective effects of multiple positive psychological constructs on a broad range of psychological, functional and adherence-based outcomes after an ACS. Accordingly, we examined associations between optimism and gratitude, measured 2 weeks post-ACS, and self-reported adherence to health behaviors, physical functioning, health-related quality of life (HRQoL) and psychiatric outcomes (depression/anxiety) 6 months later. We hypothesized that both positive psychological constructs would be prospectively associated with these outcomes, independent of baseline levels of these outcome measures and multiple relevant covariates.
2. Methods
2.1. Study design and sample
The parent study (the Gratitude Research in Acute Coronary Events [GRACE] study) was a prospective observational study of the impact of gratitude and optimism on health-related outcomes among patients admitted for an ACS between September 2012 and January 2014 to one of three cardiac units at an urban academic medical center. Approval from our healthcare system’s institutional review board was obtained prior to commencement of study procedures, and all participants underwent full written informed consent. Full study methods have been described elsewhere [22]. In a previous analysis from this trial, optimism (but not gratitude) measured 2 weeks post-ACS was associated with increased physical activity measured by accelerometer and reduced cardiac readmissions 6 months post-ACS [18]. The previous analysis did not examine the effects of optimism and gratitude on a broad range of self-reported clinical outcomes, which is the focus of the current analysis.
2.1.1. Measures
Baseline self-report measures were completed 2 weeks after hospital discharge. Follow-up measures were collected 6 months thereafter.
2.1.1.1. Positive psychological constructs.
Optimism was measured using the well-validated six-item Life Orientation Test–Revised (LOT-R) [23]. Gratitude was measured using the validated six-item Gratitude Questionnaire-6 (GQ-6) [10].
2.1.1.2. Adherence.
Four items from the Medical Outcomes Study Specific Adherence Scale (MOS SAS) [24] were used to measure self-reported frequency of adherence to diet, physical activity, stress reduction and medication over the past 2 weeks. The items were asked with the stem: “How often have you done each of the following in the past two weeks? 1) Cut down on stress in your life, 2) Exercised regularly, 3) Followed a low-fat, low-salt, or diabetic diet, 4) Took prescribed medication.” For each item, ratings were made on a 1–6 Likert/qualitative scale ranging from 1 (none of the time) to 6 (all of the time). This scale has been used to examine adherence in prior studies of cardiac patients [25].
2.1.1.3. Medical and functional status.
The 12-item well-validated Medical Outcomes Study Short Form-12 (SF-12) [26] was used to measure mental (mental component score [MCS]) and physical (physical component score [PCS]) components of HRQoL. The Duke Activity Symptom Index (DASI) [27] was used to measure health-related limitations and physical function with 12 yes/no items. These scales have been used to assess these constructs in prior studies of patients with cardiac illness [28].
2.1.1.4. Depressive symptoms and anxiety.
We assessed depressive symptoms with the well-validated Patient Health Questionnaire-9 (PHQ-9) [29]. The PHQ-9 inquires about the frequency of the nine symptoms of major depression in the prior 2 weeks and has good sensitivity and specificity [30]. Anxiety was measured via the seven-item Hospital Anxiety and Depression Scale anxiety subscale (HADS-A) [31]. The HADS-A is designed for use with medically ill patients. It has few somatic symptom items and has been used in studies of patients with heart disease [32].
2.2. Statistical analyses
Multivariable linear regressions were used to examine the prospective associations between optimism and gratitude (in separate models) on each 6-month outcome. Four models, with increasing covariate adjustment, were used to assess associations. Model 1 included only the corresponding baseline value of the 6-month outcome variable (e.g., controlling for baseline adherence when looking at 6-month adherence as the outcome). Model 2 included each baseline value from model 1 plus sociodemographic factors: age, gender and race. Model 3 included all variables in the previous models plus medical severity indicators [Charlson comorbidity index [30], peak troponin T (a protein that indicates cardiac muscle damage used as a marker of ACS severity), prior ACS] and social (living alone) risk factors. Model 4 (full model) included all previous covariates (baseline demographic, medical and social risk factors as above), plus anxiety and depressive symptoms. Two supplemental analyses were run building on the full model (model 4): one including cardiac rehospitalizations and the other including spirituality as measured by the sum of four items from the Daily Spiritual Experiences Scale (DSES) [33], with results shown in Supplemental Table 1a and b.
All analyses were completed using Stata 11.2 (StataCorp, College Station, TX, USA). Statistical significance was set a priori at two-tailed P<.05. However, since two different positive psychology constructs (optimism and gratitude) were examined as independent variables in our analyses, findings with P≥.025 (threshold for significance after Bonferroni correction [34]) should be interpreted with caution.
3. Results
Overall, 164 participants enrolled and completed baseline assessments at 2 weeks post-ACS; 156 (95%) completed all relevant self-report assessments and were included in analyses. Baseline demographic, medical and self-reported characteristics are listed in Table 1. Unadjusted (model 1) and fully adjusted regression results (model 4) are described in the text, with all model results presented in Table 2. For each regression result, the β coefficient represents the amount of change in the outcome variable (e.g., anxiety score) given a one-point increase on the optimism or gratitude scale.
Table 1.
Baseline sociodemographic, functional, medical and emotional characteristics (n=156)
| Variable | Mean (S.D.) or n (%)a |
|---|---|
| Demographic characteristics | |
| Age(y) | 61.5 (10.6) |
| Male | 137 (84)a |
| White | 137 (84)a |
| Living alone | 38 (23)a |
| Medical history | |
| First ACS | 95 (58)a |
| Charlson Index (age-adjusted) | 3.3 (1.6) |
| Peak troponin T (ng/ml) | 1.5 (3.5) |
| Diagnosis: MI | 85 (54.5) |
| BMI (kg/m2) | 28.7 (5.2) |
| Hypertension | 98 (62.8) |
| Hyperlipidemia | 126 (80.8) |
| Diabetes | 29 (18.6) |
| Left ventricular ejection fraction | .58 (.1) |
| Self-report measures at baseline (range) | |
| Optimism (LOT-R) (1–24) | 17.7 (5.6) |
| Gratitude (GQ.-6) (6–42) | 36.5 (5.8) |
| Adherence (MOS SAS) (4–24) | 17.0 (3.1) |
| Physical Function (DASI) (0–58.2) | 38.7 (15.8) |
| Physical HRQpL (SF-12 PCS) (0–100) | 40.8 (10.4) |
| Mental HRQoL (SF-12 MCS) (0–100) | 50.8 (9.2) |
| Depressive symptoms (PHQ-9) (0–27) | 4.3 (4.4) |
| Anxiety (HADS-A) (0–21) | 4.3 (4.0) |
All figures are reported as mean (S.D.) unless otherwise specified.
Table 2.
Associations between optimism and gratitude and self-report outcomes based on multivariable regressions (n=156)
| 6-month outcome variable | 2-week optimism (LOT-R), β (S.E.) | 2-week gratitude (GQ-6), β (S.E.) | ||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 | |
| Adherence (MOS SAS) | .11* (.04) | .08* (.04) | .07 (.04) | .11* (.05) R2=0.29 | .09* (.04) | .07† (.04) | .07† (.04) | .10* (.05) R2=0.29 |
| Physical Function (DASI) | .23 (.16) | .33* (.16) | .21 (.15) | .12 (.17) R2=0.55 | .12 (.15) | .18 (.15) | .19 (.14) | .09 (.16) R2=0.55 |
| Physical HRQoL (SF-12 PCS) | .09 (.13) | .13 (.14) | .05 (.13) | −.02 (.15) R2=0.41 | .04 (.13) | .07 (.13) | .08 (.12) | .01 (.14) R2=0.41 |
| Mental HRQoL (SF-12 MCS) | .53*** (.12) | .50*** (.12) | .52*** (.12) | .44** (.13) R2=0.38 | .42*** (.11) | .41*** (.11) | .43*** (.11) | .33** (.12) R2=0.37 |
| Depressive symptoms (PHQ-9) | −.14** (.05) | −.14** (.05) | −.13* (.05) | −.11* (.05) R2=0.51 | −.10* (.05) | −.10* (.05) | −.11* (.05) | −.10* (.05) R2=0.51 |
| Anxiety (HADS-A) | −.16** (.05) | −.15** (.05) | −.14** (.05) | −.15** (.05) R2=0.47 | −.09* (.04) | −.08† (.04) | −.09* (.04) | −.10* (.05) R2=0.46 |
Model 1: adjusted only for corresponding baseline value of the 6-month outcome variable. Model 2: as above plus age, gender, and race. Model 3: as above plus medical and social risk factors (Charlson comorbidity index, peak troponin T, prior ACS, living alone). Model 4: as above plus anxiety and depressive symptoms.
P<.10
P<.05.
P<.01.
P<.001.
In unadjusted analyses (model 1), 2-week optimism and gratitude were positively associated with 6-month health behavior adherence (MOS SAS) [optimism β=.11, standard error (S.E.)=.04, P=.011; gratitude β=.09, S.E.=.04, P=.033] and mental HRQoL (SF-12 MCS) (optimism β=.53, S.E.=.12, P<.001; gratitude β=.42, S.E.=.11, P<.001], and negatively associated with depressive symptoms (PHQ-9) (optimism β=−.14, S.E.=.05, P=.004; gratitude β=−.10, S.E.=.05, P=.043) and anxiety (HADS-A) (optimism β=−.16, S.E.=.05, P= .001; gratitude β=−.09, S.E.=.04, P=.035).
After adjusting for social, medical and psychiatric covariates (model 4), optimism (β=.11, S.E.=.05, P=.038) and gratitude (β=.10, S.E.= .05, P=.027) at 2 weeks post-ACS were associated with 6-month health behavior adherence (MOS SAS). Optimism (β=.44, S.E.=.13, P=.001) and gratitude (β=.33, S.E.=.12, P=.005) were also associated with 6-month mental HRQoL (SF-12 MCS). In contrast, neither optimism nor gratitude was significantly associated with physical HRQoL (SF-12 PCS) or functional status (DASI).
After adjusting for social and medical covariates, optimism at 2 weeks was associated with lower 6-month depressive symptoms (PHQ-9) (β=−.11, S.E.=.05, P=.039) and anxiety (HADS-A) (β=−.15, S.E.=.05, P=.004) scores. Gratitude at 2 weeks was also associated with lower depressive symptoms (β=−.10, S.E.=.05, P=.028) and anxiety (β=−.10, S.E.=.05, P=.034) scores.
Supplemental Table 1a shows the fully adjusted models with the addition of cardiac rehospitalizations. Most of the significant results did not change with this addition, with the exception that the depression outcome was slightly attenuated (P<.05 to P<.10). In Supplemental Table 1b, when adding spirituality (DSES items) to the full model, the effects of gratitude on adherence and mental HRQoL persisted, and the anxiety and depression results became marginally significant (P<.10).
4. Discussion
The present study found that optimism and gratitude following an ACS were associated with greater subsequent self-reported adherence to key cardiac health behaviors and mental HRQoL, as well as lower anxiety and depressive symptom scores. All significant associations remained after controlling for social and medical covariates. Notably, the associations with adherence and mental HRQoL were independent of concurrent negative psychological states (depressive symptoms and anxiety).
The connections between positive psychological constructs and HRQoL may be relevant to clinical care and outcomes in ACS patients. HRQoL is an important component of physical, social and psychological health that can impact functioning among cardiac patients [35,36]. HRQoL is sensitive to changes and linked with health behaviors and cardiac prognosis [37–39]. As the longevity of cardiac patients has increased over time, HRQoL is seen as an important outcome in its own right. The NHLBI emphasized this in a position paper indicating that they are “committed to supporting efforts to measure HQL [health-related quality of life] as an important end point in trials of cardiovascular interventions […]” [40]. Further demonstrating its importance in research, HRQoL is now included in two major US epidemiological surveys, the National Health and Nutrition Examination and the Behavioral Risk Factor Surveillance System [36]. In the present study, the significant positive relationships between optimism and mental HRQoL were found across all models. These findings are consistent with previous studies, including a meta-analysis of optimism’s associations with HRQoL among cardiac patients [7]. The present study extends work in this area by demonstrating these relationships in high-risk patients following an ACS. This is also the first study to demonstrate a relationship between gratitude and mental HRQoL in a medically ill population, an area with much potential for further study.
The association of optimism with adherence to health behaviors is consistent with prior studies. Several studies have linked higher optimism with improved health behaviors like physical activity, medication adherence and adopting a heart-healthy diet [7,41–44]. In addition, the present findings are consistent with a prior analysis from this cohort, finding that optimism was associated with physical activity measured by accelerometer [18]. Adherence to health behaviors like physical activity reduces morbidity and mortality after ACS [45]. Thus, the optimism–physical activity association is promising when considering ways to improve health outcomes among cardiac patients.
A recent review indicated that although there are few gratitude intervention studies, most indicate promising results with respect to social and psychological outcomes [46]. In particular, gratitude interventions (e.g., recording daily gratitudes, behavioral expressions of gratitude) have been associated with improved well-being [47], reduced worry [48] and positive affect [49]. One intervention also led to greater physical activity and fewer self-reported physical symptoms [47]. In the gratitude intervention and physical health literature, one recent randomized controlled pilot trial examined a daily gratitude journaling intervention among cardiac patients and found preliminary indications that the intervention improved some markers of heart failure/cardiac prognosis (e.g., inflammation, parasympathetic heart rate variability) [13]. With these promising early findings and given the need for improved adherence post-ACS, more research on the effects of gratitude on health behaviors is needed, particularly in the context of cardiac patients. The present study is the first to demonstrate the association of gratitude with health behavior adherence in a medical or cardiac population.
Finally, this study found that baseline optimism and gratitude were associated with lower 6-month anxiety and depressive symptoms, independent of their baseline values. This finding has important implications for recovery because depression and anxiety are associated with poorer cardiac prognosis and mortality [50,51]. Depression following an ACS has been associated with recurrent cardiac events, rehospitalizations and morbidity [52–54]. Further, lower levels of depression and anxiety are linked to reduced rates of cardiac events and mortality [55]. The present finding that optimism and gratitude were associated with improved mental health states is important when considering ways to improve well-being and prognosis for high risk post-ACS patients.
In examining the magnitude of the regression effects found, there are several important considerations. First, there are no established clinical cutoffs for the measures of optimism (LOT-R) and gratitude (GQ-6) used in this study. Second, for several of the outcomes used (e.g., MOS SAS), there are very limited data on minimally clinically important differences (MCIDs). Third, for the outcomes used that do have MCID data (SF-12 for HRQoL, HADS-A for anxiety and PHQ-9 for depressive symptoms), relatively large differences in optimism and gratitude were required to see clinically important differences. For the SF-12, published data indicate that a 4- to 5-point score change is considered clinically significant [56]. In the present study, we found that an 8.5-point increase [1.5 standard deviation (S.D.)] in optimism (LOT-R) or 10.2-point increase (1.75 S.D.) in gratitude (GQ-6) would be required to meet this clinical significance threshold. Likewise, changes of >1 S.D. in optimism and gratitude were required to see the 5-point change MCID for the PHQ-9 [57] and the 1.4-point change MCID for the HADS-A [58].
This observational study had several limitations, including a moderate sample size, potentially limiting power to identify associations and a largely white male sample from a single academic center, which could limit generalizability. Furthermore, all outcomes in this analysis were self-reported, and future studies could benefit from using objective measures of health behavior adherence and functioning. Other related and potentially relevant constructs were not included, such as prosocial behavior or perceived social support. Future studies would benefit from examining adherence to each specific health behavior and exploring the role of self-regulation or conscientiousness on these health behaviors.
Despite these limitations, this prospective study is the first to simultaneously examine the independent effects of two positive psychological constructs on a wide range of medical, functional and emotional outcomes in a high-risk post-ACS cohort. The analysis revealed independent contributions of optimism and gratitude to adherence, mental HRQoL, anxiety and depressive symptoms. This work also adds to the literature by describing the effects of gratitude on mental HRQoL and self-reported health behavior adherence in a medical population. If optimism, gratitude and related positive psychological constructs are associated with superior prognosis, research should examine whether interventions designed to cultivate positive psychological experiences can result in improved clinical outcomes. There has been limited work to-date in this area. In one randomized trial, a gratitude intervention led to greater physical activity in a nonmedical population [47]. In two randomized trials among hypertension and heart disease patients, a positive affect-based program was associated with improvements in physical activity and medication adherence [59,60]. The relationships between positive psychological constructs and HRQoL, health behavior adherence and reduced depressive symptoms and anxiety may begin to explain the associations of optimism and gratitude with superior cardiac prognosis. Future studies are warranted to determine whether intervention programs are effective and can modify prognosis among ACS patients.
Supplementary Material
Funding
This work was supported by UC Berkeley’s Greater Good Science Center with funding from the John Templeton Foundation (grant number 15627). Additional funding for analysis and interpretation time was funded by NIH grant to the senior author (grant number R01HL113272) and by NIH grant to the second author (grant number K23HL123607). The authors declare no conflicts of interest regarding the publication of this paper [61–67].
Footnotes
ClinicalTrials.gov identifier .
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.genhosppsych.2016.08.006.
References
- [1].Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- [2].Marks R, Allegrante JP. A review and synthesis of research evidence for self-efficacy enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract 2005;6(2):148–56. [DOI] [PubMed] [Google Scholar]
- [3].Dimeo FC, Thomas F, Raabe-Menssen C, Pröpper F, Mathias M. Effect of aerobic exercise and relaxation training on fatigue and physical performance of cancer patients after surgery. A randomised controlled trial. Support Care Cancer 2004;12(11): 774–9. [DOI] [PubMed] [Google Scholar]
- [4].Sullivan MD, LaCroix AZ, Russo JE, Walker EA. Depression and self-reported physical health in patients with coronary disease: mediating and moderating factors. Psychosom Med 2001;63(2):248–56. [DOI] [PubMed] [Google Scholar]
- [5].Redeker NS, Ruggiero JS, Hedges C. Sleep is related to physical function and emotional well-being after cardiac surgery. Nurs Res 2004;53(3):154–62. [DOI] [PubMed] [Google Scholar]
- [6].Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care 2009;15(2 Suppl.):S36–41. [PubMed] [Google Scholar]
- [7].DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol 2015;195:265–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev 2010;30:879–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med 2009;37:239–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].McCullough ME, Emmons RA, Tsang JA. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol 2002;82(1):112–27. [DOI] [PubMed] [Google Scholar]
- [11].Laerum E, Johnsen N, Smith P, Larsen S. Myocardial infarction may induce positive changes in life-style and in the quality of life. Scand J Prim Health Care 1988;6(2): 67–71. [DOI] [PubMed] [Google Scholar]
- [12].Mills PJ, Redwine L, Wilson K, Pung MA, Chinh K, Greenberg BH, et al. The role of gratitude in spiritual well-being in asymptomatic heart failure patients. Spiritual Clin Pract 2015;2(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Redwine LS, Henry BL, Pung MA, Wilson K, Chinh K, Knight B, et al. Pilot randomized study of a gratitude journaling intervention on heart rate variability and inflammatory biomarkers in patients with stage B heart failure. Psychosom Med 2016;78(6): 667–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].McCraty R, Atkinson M, Tiller WA, Rein G, Watkins AD. The effects of emotions on short-term power spectrum analysis of heart rate variability. Am J Cardiol 1995; 76(14):1089–93. [DOI] [PubMed] [Google Scholar]
- [15].Celano CM, Huffman JC. Depression and cardiac disease: a review. Cardiol Rev 2011; 19(3):130–42. [DOI] [PubMed] [Google Scholar]
- [16].Young JJ, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord 2014;169:15–20. [DOI] [PubMed] [Google Scholar]
- [17].Friedman EM, Ryff CD. Living well with medical comorbidities: a biopsychosocial perspective. J Gerontol B Psychol Sci Soc Sci 2012;67(5):535–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Huffman JC, Beale EE, Celano CM, Beach SR, Belcher AM, Moore SV, et al. Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: the Gratitude Research in Acute Coronary Events study. Circ Cardiovasc Qual Outcomes 2016;9(1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ikeda A, Schwartz J, Peters JL, Fang S, Spiro III A, Sparrow D, et al. Optimism in relation to inflammation and endothelial dysfunction in older men: the VA Normative Aging Study. Psychosom Med 2011;73(8):664–71. [DOI] [PubMed] [Google Scholar]
- [20].Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol 2009;65(5):467–87. [DOI] [PubMed] [Google Scholar]
- [21].Bradley SM, Rumsfeld JS. Depression and cardiovascular disease. Trends Cardiovasc Med 2015;25(7):614–22. [DOI] [PubMed] [Google Scholar]
- [22].Huffman JC, Beale EE, Beach SR, Celano CM, Belcher AM, Moore SV, et al. Design and baseline data from the Gratitude Research in Acute Coronary Events (GRACE) study. Contemp Clin Trials 2015;44:11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67(6):1063–78. [DOI] [PubMed] [Google Scholar]
- [24].DiMatteo MR, Hays RD, Sherbourne CD. Adherence to cancer regimens: implications for treating the older patient. Oncology 1992;6(2 Suppl):50–7. [PubMed] [Google Scholar]
- [25].Bauer LK, Caro MA, Beach SR, Mastromauro CA, Lenihan E, Januzzi JL, et al. Effects of depression and anxiety improvement on adherence to medication and health behaviors in recently hospitalized cardiac patients. Am J Cardiol 2012;109(9):1266–71. [DOI] [PubMed] [Google Scholar]
- [26].Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- [27].Parissis JT, Nikolaou M, Birmpa D, Farmakis D, Paraskevaidis I, Bistola V, et al. Clinical and prognostic value of Duke’s Activity Status Index along with plasma B-type natriuretic peptide levels in chronic heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 2009;103(1):73–5. [DOI] [PubMed] [Google Scholar]
- [28].Rollman BL, Belnap BH, LeMenager MS, Mazumdar S, Houck PR, Counihan PJ, et al. Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial. JAMA 2009;302(19):2095–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32(9):1–7. [Google Scholar]
- [30].Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47(11):1245–51. [DOI] [PubMed] [Google Scholar]
- [31].Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52(2):69–77. [DOI] [PubMed] [Google Scholar]
- [32].Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 2008; 65(1):62–71. [DOI] [PubMed] [Google Scholar]
- [33].Underwood LG, Teresi JA. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann Behav Med 2002;24(1):22–33. [DOI] [PubMed] [Google Scholar]
- [34].Dunn OJ. Multiple comparisons among means. J Am Stat Assoc 1961;56(293):52–64. [Google Scholar]
- [35].O’Loughlin C, Murphy NF, Conlon C, O’Donovan A, Ledwidge M, McDonald K. Quality of life predicts outcome in a heart failure disease management program. Int J Cardiol 2010;139(1):60–7. [DOI] [PubMed] [Google Scholar]
- [36].Young DR, Coughlin J, Jerome GJ, Myers V, Chae SE, Brantley PJ. Effects of the PREMIER interventions on health-related quality of life. Ann Behav Med 2010;40(3):302–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Haas DC. Depression and disability in coronary patients: time to focus on quality of life as an end point. Heart 2006;92(1):8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995;273(1):59–65. [PubMed] [Google Scholar]
- [39].Zuluaga MC, Guallar-Castillon P, Lopez-Garcia E, Banegas JR, Conde-Herrera M, Olcoz-Chiva M, et al. Generic and disease-specific quality of life as a predictor of long-term mortality in heart failure. Eur J Heart Fail 2010;12(12):1372–8. [DOI] [PubMed] [Google Scholar]
- [40].Czajkowski SM. Health-related quality of life outcomes in clinical research: NHLBI policy and perspectives. Ann Thorac Surg 1998;66(4):1486–7. [DOI] [PubMed] [Google Scholar]
- [41].Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. J Psychosom Res 2007;63(5):483–90. [DOI] [PubMed] [Google Scholar]
- [42].Boehm JK, Kubzansky LD. The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol Bull 2012;138(4):655–91. [DOI] [PubMed] [Google Scholar]
- [43].Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers 2009;77(6):1747–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol 2006;11(Pt 1):71–84. [DOI] [PubMed] [Google Scholar]
- [45].Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation 2010;121(6):750–8. [DOI] [PubMed] [Google Scholar]
- [46].Wood AM, Froh JJ, Geraghty AWA. Gratitude and well-being: a review and theoretical integration. Clin Psychol Rev 2010;30(7):890–905. [DOI] [PubMed] [Google Scholar]
- [47].Emmons RA, McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol 2003;84(2):377–89. [DOI] [PubMed] [Google Scholar]
- [48].Geraghty AW, Wood AM, Hyland ME. Dissociating the facets of hope: agency and pathways predict dropout from unguided self-help therapy in opposite directions. J Res Pers 2010;44(1):155–8. [Google Scholar]
- [49].Froh JJ, Kashdan TB, Ozimkowski KM, Miller N. Who benefits the most from a gratitude intervention in children and adolescents? Examining positive affect as a moderator. J Posit Psychol 2009;4(5):408–22. [Google Scholar]
- [50].Roest AM, Zuidersma M, de Jonge P. Myocardial infarction and generalised anxiety disorder: 10-year follow-up. Br J Psychiatry 2012;200(4):324–9. [DOI] [PubMed] [Google Scholar]
- [51].Watkins LL, Koch GG, Sherwood A, Blumenthal JA, Davidson JR, O’Connor C, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc 2013;2(2):e000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kronish IM, Rieckmann N, Schwartz JE, Schwartz DR, Davidson KW. Is depression after an acute coronary syndrome simply a marker of known prognostic factors for mortality? Psychosom Med 2009;71(7):697–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Frasure-Smith N, Lesperance F, Irwin MR, Sauve C, Lesperance J, Theroux P. Depression, C-reactive protein and two-year major adverse cardiac events in men after acute coronary syndromes. Biol Psychiatry 2007;62(4):302–8. [DOI] [PubMed] [Google Scholar]
- [54].Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations a scientific statement from the American Heart Association. Circulation 2014;129(12):1350–69. [DOI] [PubMed] [Google Scholar]
- [55].Huffman JC, Celano CM, Januzzi JL. The relationship between depression, anxiety, and cardiovascular outcomes in patients with acute coronary syndromes. Neuropsychiatr Dis Treat 2010;6:123–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Parker SL, Mendenhall SK, Shau D, Adogwa O, Cheng JS, Anderson WN, et al. Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. J Neurosurg Spine 2012;16(1):61–7. [DOI] [PubMed] [Google Scholar]
- [57].Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care 2004;42(12): 1194–201. [DOI] [PubMed] [Google Scholar]
- [58].Puhan MA, Frey M, Büchi S, Schünemann HJ. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes 2008;6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med 2012;172(4):322–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong SC, Hollenberg JP, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med 2012;172(4): 329–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Schnohr P, Kristensen TS, Prescott E, Scharling H. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time–The Copenhagen City Heart Study. Scand J Med Sci Sports 2005;15(2):107–12. [DOI] [PubMed] [Google Scholar]
- [62].Callahan CM, Kroenke K, Counsell SR, Hendrie HC, Perkins AJ, Katon W, et al. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc 2005;53(3):367–73. [DOI] [PubMed] [Google Scholar]
- [63].DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: a meta-analysis. Med Care 2007;45(6):521–8. [DOI] [PubMed] [Google Scholar]
- [64].Lesperance F, Frasure-Smith N. Depression in patients with cardiac disease: a practical review. J Psychosom Res 2000;48(4–5):379–91. [DOI] [PubMed] [Google Scholar]
- [65].Bei B, Ong JC, Rajaratnam SM, Manber R. Chronotype and improved sleep efficiency independently predict depressive symptom reduction after group cognitive behavioral therapy for insomnia. J Clin Sleep Med 2015;11(9):1021–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 2002;34(12): 1996–2001. [DOI] [PubMed] [Google Scholar]
- [67].Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry 2001;23(4):183–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.