Abstract
Background:
Prompted by the ongoing debate regarding whether cannabis serves as a complement to or substitute for alcohol, this study uses prospective data to examine daily associations between medicinal versus recreational cannabis and alcohol use in veterans.
Methods:
Three semi-annual waves of Timeline Followback Interview data were collected from a sample of veterans who reported co-using alcohol and cannabis on at least one day (N = 115; 56% medicinal users; 93% male; 62,100 observations). Linear mixed effects models were used to examine the association between daily cannabis use and number of drinks consumed across time for both medicinal and recreational users and to examine the frequency medicinal cannabis used to substitute for alcohol.
Results:
Compared to medicinal users, recreational users were more likely to drink more on cannabis use days relative to non-use days. Among medicinal users, those endorsing more frequent use of cannabis as a substitute for alcohol reported fewer number of drinks consumed on days when cannabis was used relative to non-use days.
Conclusions:
Among veterans, recreational users are at greater risk for increased drinking when co-using cannabis at the daily level, an association that is stable over time. Medicinal users may be at lower risk for increased drinking on days when cannabis is also used, especially those who endorse using cannabis to substitute for alcohol. Findings help clarify the debate on cannabis-alcohol substitution or complementary associations in a sample of veterans and suggests that alcohol interventions should address cannabis use as a risk factor, especially for recreational users.
Keywords: Cannabis, Alcohol, Medicinal, Recreational, Veterans, Co-use
1. Introduction
In the wake of increased legislation sanctioning the recreational and medicinal use of cannabis in the United States, there is growing interest on the impact of cannabis on other substance use, including alcohol (Staiger et al., 2012; Yurasek et al., 2017). Alcohol consumption and related consequences are of significant public health concern, as alcohol is the 3rd leading cause of preventable death in the United States (Centers for Disease Control and Prevention (CDC), 2013). Cannabis is frequently used with alcohol, and this co-use has been associated with increased alcohol consumption, consequences, and alcohol use disorder (AUD) (Brière et al., 2011; Haas et al., 2015; Patrick et al., 2017; Shillington and Clapp, 2006; Subbaraman and Kerr, 2015). Individuals with cannabis dependence have nearly double the long-term risk for experiencing alcohol related problems (Copeland et al., 2012) and are more likely to develop AUD (Lopez-Quintero et al., 2010) compared to drinkers who do not use cannabis. Further, cannabis use during alcohol treatment is associated with negative alcohol-related treatment outcomes (Aharonovich et al., 2005; Mojarrad et al., 2014; Subbaraman et al., 2019, 2018; Subbaraman et al., 2017). Despite the clinical and public health risks associated with co-use, questions remain whether cannabis use acts as a substitute (cannabis is used to replace the effects of alcohol) or complement (cannabis is used to enhance alcohol intoxication) for alcohol use (Subbaraman, 2016), and whether these patterns change over time.
Conflicting evidence exists suggesting cannabis acts as both a substitute and complement of cannabis use (see review, Subbaraman, 2016). Regarding substitution, individuals abstinent from cannabis reported greater alcohol consumption and craving during an experimental abstinence period (Peters and Hughes, 2010). State-level policy studies also find that cannabis can function as a substitute for alcohol consumption (Chaloupka and Laixuthai, 1997; Clements and Daryal, 2005; Subbaraman, 2016). There is equally compelling evidence that cannabis acts as a complement to alcohol use: the majority of epidemiological studies, as well as studies examining individual-level outcomes, indicate cannabis use is related to increased consumption of alcohol (Subbaraman, 2016). Thus, it is critical to use nuanced measurement of alcohol and cannabis use, including daily and event-level studies, in order to clarify these patterns.
Rather than examine the effects of cannabis on alcohol consumption, to date most event-level studies of co-use have examined outcomes and consequences related to simultaneous use of alcohol and cannabis among adolescents and college students (Lipperman-Kreda et al., 2017; Mallett et al., 2017) or effects of co-use on cannabis intoxication (Hughes et al., 2014) or use (O’Hara et al., 2016). However, recent work found that daily cannabis use among veterans was associated with increased likelihood of same-day moderate drinking compared to no drinking, and same-day heavy drinking compared to moderate drinking (Metrik et al., 2018b). Similarly, the first longitudinal study examining the effect of cannabis use on alcohol use (Gunn et al., 2018) found that cannabis use days were associated with more drinks and higher estimated blood alcohol concentration (eBAC) compared to non-cannabis use days. This study also found that these associations strengthened over the course the study (the first two years of college), suggesting the link between cannabis use at the daily level and more drinking increases over these formative years. Although compelling, data collection for this study included a sample of college students, limiting generalizability.
In addition to person-level factors such as age (Wen et al., 2015), several moderators of the association between cannabis and alcohol use have been identified. Metrik et al. (2018b) revealed that individuals with an AUD were significantly more likely to drink heavily on cannabis use days compared to drinkers without an AUD; however, individuals with cannabis use disorder (CUD) were significantly less likely to drink heavily on cannabis use days. In Gunn et al (2018), pre-college levels of alcohol use and problems predicted increased alcohol consumption on cannabis use days. Together with clinical and epidemiological studies, this research suggests that those with problematic alcohol use or AUD are at increased risk for heavier consumption when also using cannabis. However, a potential substitution effect may be present for individuals who are using cannabis at heavy or dependent levels—specifically for those without any evidence of AUD—as their demand for alcohol may be diminished in the presence of cannabis (Metrik et al., 2018b). To further elucidate the nature of the cannabis-alcohol association, it would be informative to closely examine medicinal cannabis users, who report using cannabis at a daily or nearly daily level (Lin et al., 2016).
Medicinal cannabis users have cited use of cannabis as a substitute for alcohol and as a way to better manage alcohol withdrawal symptoms (Reiman, 2007, 2009). Among medicinal cannabis users, cannabis may be less strongly associated with increased alcohol consumption. For instance, national data suggest that medicinal users are less likely to have an AUD compared to recreational users (Lin et al., 2016). In a large study (N =1971) of veterans, those who reported cannabis use for medicinal purposes also reported using alcohol less frequently, compared to those who reported only recreational cannabis use (Loflin et al., 2017a,b). Finally, veterans who use cannabis recreationally (compared to those who use medicinally) report higher frequency of alcohol use and are more likely to report alcohol intoxication as a motive for cannabis use (e.g., using cannabis “because you were under the influence of alcohol”) (Metrik et al., 2018a). Together, these studies suggest that medicinal users may use cannabis to reduce alcohol consumption (i.e. substitution) (Lin et al., 2016; Loflin et al., 2017b; Metrik et al., 2018a). However, to date, there are no event or daily-level examinations of the association between cannabis and alcohol use among medicinal versus recreational cannabis users.
1.1. The current study
The current study sought to extend this body of literature by examining daily associations between cannabis and alcohol use across one and a half years in medicinal and recreational cannabis users. The sample was recruited from a Veterans Health Administration (VHA) facility to examine a specific population with disproportionately higher rates of substance use disorders, relative to the general population (Seal et al., 2011). In order to elucidate competing substitution versus complementation hypotheses, follow-up exploratory analyses were conducted to specifically examine self-reported alcohol use as a substitute for cannabis by medicinal cannabis users. We hypothesized: (a) associations between cannabis and alcohol consumption (number of standard drinks per day) would be stable over time among both types of users; (b) recreational cannabis users would be more likely to drink more on cannabis use days compared to non-cannabis use days, whereas medicinal users would not; and (c) alcohol consumption on cannabis use days would be lower for medicinal users who reported more frequent use of cannabis to substitute for alcohol
2. Methods
2.1. Sample and procedure
Data were drawn from a larger prospective study (3 semi-annual waves) examining cannabis use and related problems in 361 veterans returning from Iraq and Afghanistan from post 9/11/2001 deployments (Metrik et al., 2016). Veterans were recruited from a VHA facility in the Northeast of the US based on use of cannabis at least once in their lifetime (see Metrik et al., 2016 for details on recruitment procedures). Veterans were screened for eligibility by telephone and subsequently invited for a baseline visit, at which point they completed informed consent and a battery of interview and self-report assessments. Follow-up visits were conducted in-person at 6-months (N = 312; 86.4%) and 12-months (N =310, 85.9%) with parallel assessments. All study procedures were approved by the university and local VHA Institutional Review Boards. Analyses for the present study were completed on the subsample of participants who reported co-using both alcohol and cannabis on at least one day on the Time-Line Follow-Back (see section 2.2.3) across all three time points (n = 115).
2.2. Measures
2.2.1. Demographic information
Demographic and background information, such as sex, race, age, and marital status was collected at baseline and verified through the VHA Computerized Patient Record System (CPRS).
2.2.2. Alcohol (AUD) and Cannabis Use Disorder (CUD)
The Structured Clinical Interview for DSM nonpatient edition (SCIDNP (First et al., 2002)) was used to assess lifetime and current (past year) DSM-5 AUD and CUD at baseline and 12-months.
2.2.3. Daily cannabis and alcohol use
The Timeline Followback (TLFB) is a psychometrically-sound, calendar-assisted structured interview, shown to give valid assessment (including agreement with biological measures) of alcohol, cannabis, and other substance use (Dennis et al., 2004; Hjorthøj et al., 2012; Sobell and Sobell, 1992) and high test–retest reliability and stability over 180 days (Carey, 1997) and up to 1 year (Sobell and Sobell, 1992). TLFB uses a calendar to cue participants to events (e.g. personal anniversaries, holidays, personal calendar events) to enhance accurate recall. TLFB assessments covered the 180 days prior to each visit (baseline, 6-months, and 12-months; 540 consecutive days) and was used to measure daily cannabis (any use), alcohol (number of standard drinks), tobacco (any use), and other drug use (any use).
2.2.4. Type of cannabis user
Participants were classified as a medicinal cannabis user if they endorsed ever using cannabis for medicinal purposes on the Medical Marijuana Patient Questionnaire (MMPQ (Cohen et al., 2016) at baseline or at the 12-month follow-up visit. The item used stated: “How often have you used marijuana for medicinal purposes?” Participants were classified as recreational users if they reported never using cannabis for medicinal purposes at either time point.
2.2.5. Substitution reason
Participants completed the Reasons for Medical Marijuana Questionnaire (RFUMM (Reinarman et al., 2011) to assess how often they used medical cannabis for 25 reasons. Medicinal users rated frequency of cannabis use on a likert scale of 1 = “almost never/never” to 5 = “almost always/always” in response to the prompt, “Thinking of all the times you have used medical marijuana, how often would you say that you use for each of the following reasons.” The present study focused on the reason “using cannabis as substitute for alcohol” only. Participants classified as recreational users did not complete the RFUMM.
2.3. Data analysis
Multilevel modeling (Raudenbush and Bryk, 2002; Snijders and Bosker, 1999) was used to conduct all analyses as data are nested within individuals, using the lmer4 package (Bates et al., 2015) within R (R Core Team, 2013). A series of linear mixed effects models (LMEM) tested the prediction of number of drinks by cannabis use across all days and moderation of these effects by subject-level variables (type of user and substitution reason). Dependent variables in all three models were daily number of drinks as self-reported on the TLFB. All models included fixed effects of percent of cannabis use days (person-level), calculated from all TLFB days as a percentage of those days in which any cannabis was used (grand-mean centered in all models). All models also included fixed effects of any daily cannabis use (binary), time (days 1 through 540), baseline age, any daily cigarette use (binary), any other daily drug use (binary), day of the week (binary: weekend or weekday), and random effects for individual. The initial model examining the longitudinal effect of daily cannabis use on alcohol consumption also included the interaction of time and daily cannabis use. For the model examining moderation by type of user (medicinal versus recreational), time and two- and three-way interactions between time, type of user (binary, with recreational as the reference), and daily cannabis use (binary) were included. For the final exploratory analysis examining moderation by alcohol substitution reason among medicinal users only, time and two- and three-way interactions between time, substitution reason (grand-mean centered), and daily cannabis use were included. Due to the small number of females in the sample (n = 7) and the effect of sex being non-significant in all models, sex was removed from final analyses. Initial models also included marital status, race, and ethnicity, which were also non-significant and removed from final analyses.
3. Results
3.1. Descriptive statistics
For the present study, participants were those who endorsed co-use of both alcohol and cannabis on at least one day in the full 18-month TLFB period (comprised of reports at baseline, 6-month, and 1-year follow-up), resulting in 62,100 daily observations across all three time points (540 calendar days). Table 1 presents demographics and substance use descriptive statistics for the full sample (N =115) and the subsamples of medicinal (n = 64) and recreational (n = 51) users. Overall, compared to the medicinal users, recreational users reported more drinking days and heavy drinking days and were more likely to meet criteria for past-year AUD at baseline and 1-year follow-up. However, the only statistically significant group difference in alcohol use characteristics was in the frequency of drinking days. Conversely, medicinal users reported significantly more cannabis use days, co-use days, and were more likely to be diagnosed with current CUD at baseline and 1-year follow up.
Table 1:
Demographic and substance use characteristics by type of cannabis user.
| Full Sample (n =115) |
Medicinal Users (n = 64) |
Recreational Users (n = 51) |
Group Comparison | |
|---|---|---|---|---|
| Demographics | ||||
| Age (M, SD) | 31.34 (8.30) | 31.69 (8.42) | 30.90 (8.20) | F(1,113) = .35, p =.62 |
| Employment (% full or part time) | 71 | 64 | 80 | χ2(1, 115) = 2.94, p =.09 |
| Sex (% Male) | 93 | 92 | 94 | χ2(1, 115) = .001, p =1.0 |
| Race (% Caucasian) | 77 | 81 | 71 | χ2(1, 115) = 1.67, p =.20 |
| Substance Use Characteristics M (SD) % cannabis use days |
37.58 (38.70) | 56.92 (37.00) | 13.32 (24.69) | F(1,113) = 52.25, p < .001 |
| % Drinking days | 27.97 (27.62) | 23.23 (25.78) | 33.93 (28.93) | F(1,113) = 4.39, p =.04 |
| % Heavy drinking days | 15.26 (22.46) | 13.32 (20.50) | 17.70 (24.69) | F(1,113) = 1.08, p =.30 |
| No. of drinks per drinking day | 5.73 (4.02) | 5.83 (4.37) | 5.65 (3.68) | F(1,94b) =.01, p =.92 |
| % Co-use day | 8.23 (17.23) | 12.17 (21.73) | 3.29 (6.05) | F(1,113) = 8.01, p =.01 |
| % Cigarette use daysa | 60.96 (34.61) | 63.85 (31.95) | 55.31 (39.43) | F(1,66) = .93, p =.34 |
| % Other drug use days | 3.25 (10.60) | 2.39 (8.79) | 4.33 (12.52) | F(1,113) = .95, p =.33 |
| Diagnostic Characteristics (%) Current AUD (Baseline) |
45 | 39 | 53 | F(1,113) = 2.21, p =.14 |
| Current CUD (Baseline) | 35 | 44 | 24 | F(1,113) = 5.26, p =.02 |
| Current AUD (1-Year) | 46 | 42 | 51 | F(1,113) = .88, p =.35 |
| Current CUD (1-Year) | 38 | 53 | 20 | F(1,113) = 15.03, p < .001 |
Note. Data calculated from TLFB
Calculated for subsamples of tobacco smokers (full sample: n= 68; medicinal users: n = 45; recreational users: n = 23)
19 observations removed due to missingness.
3.2. Longitudinal association between cannabis and alcohol use
The mixed effect multilevel model predicting number of drinks from any cannabis use, time (days), and the interaction of cannabis use and time (day) revealed that cannabis use on a given day positively predicted number of drinks on the same day (OR =1.45; 95% CI =1.31, 1.61; p < .001) (see Table 2 for model estimates). In other words, on days when cannabis was used, individuals also consumed more drinks relative to days when cannabis was not used, even controlling for person-level cannabis use (percent cannabis use days), which itself was negatively associated with number of drinks (OR =.99; 95% CI = .98, 1.00; p =. 01). There was also a significant effect of time and a time by cannabis use interaction (OR = .9991; 95% CI = .9988, .9994; p < .001). Specifically, individuals increased their likelihood of drinking more on a given day over time but were less likely to drink more drinks on cannabis use days over the 540 calendar days. Overall, results suggest that with time, individuals reported marginally fewer drinks on cannabis use days. This small-magnitude effect was observed while controlling for significant covariates of subject-level cannabis use, age, day of the week, cigarette use, and other drug use.
Table 2:
Mixed Effects model of association between cannabis and time on alcohol use.
| Estimate | SE | p-value | Lower CI | OR | Upper CI | |
|---|---|---|---|---|---|---|
| Intercept | −.82 | .73 | – | – | – | – |
| Any cannabis usea | 0.37 | 0.05 | < .001 | 1.31 | 1.45 | 1.61 |
| Timea | 0.001 | 8.51E-05 | < .001 | 1.0004 | 1.0005 | 1.0007 |
| % cannabis use days | −0.012 | 0.01 | .01 | .98 | .99 | 1.00 |
| Any ciga | 0.23 | 0.04 | < .001 | 1.16 | 1.25 | 1.36 |
| Any other druga | 1.31 | 0.07 | < .001 | 3.22 | 3.72 | 4.30 |
| Day (ref: weekday) a | 0.98 | 0.02 | < .001 | 2.66 | 2.56 | 2.77 |
| Baseline age | 0.06 | 0.02 | .006 | 1.02 | 1.06 | 1.11 |
| Any cannabis usea × timea | −0.001 | 0.0001 | < .001 | .9988 | .9991 | .9994 |
Note. Coefficients are unstandardized.
Denotes time-varying.
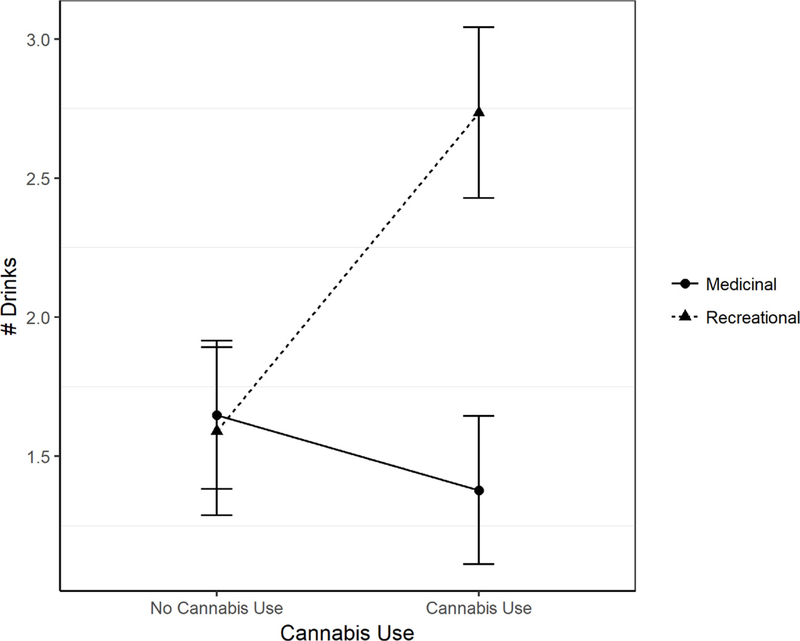
3.3. Longitudinal association between cannabis and alcohol use by type of user
Table 3 shows model estimates for the mixed effect multilevel model examining type of cannabis user (medicinal v. recreational users). Findings revealed a significant interaction of cannabis use and type of user (OR =4.10; 95% CI = 3.52, 4.78; p < .001), with greater odds of drinking more on cannabis use days vs. non-use days for recreational users compared to medicinal users (Fig. 1). The interaction of time by cannabis use remained significant, as did the interaction of recreational user and time. The non-significant three-way interaction between time, cannabis use, and type of user was removed from the final models. Overall, results suggest that recreational users were more likely to consume more alcohol on cannabis use days. Of note, the main effect of time was no longer significant. Cigarette use, other drug use, weekend days, and age remained positive predictors of number of drinks.
Table 3:
Mixed Effects model of association between cannabis and time on alcohol use: moderation by type of cannabis user.
| Estimate | SE | p-value | Lower CI | OR | Upper CI | |
|---|---|---|---|---|---|---|
| Intercept | −0.77 | 0.80 | – | – | – | – |
| Any cannabis usea | −0.13 | 0.06 | 0.04 | 0.78 | 0.88 | 0.99 |
| Recreational | −0.21 | 0.43 | 0.63 | 0.35 | 0.81 | 1.87 |
| Timea | 0.0002 | 0.0001 | 0.11 | 0.99 | 1.00 | 1.00 |
| % cannabis use days | −0.01 | 0.01 | .07 | 0.98 | 0.99 | 1.00 |
| Any ciga | 0.22 | 0.04 | < .001 | 1.15 | 1.25 | 1.35 |
| Any other druga | 1.28 | 0.07 | < .001 | 3.12 | 3.60 | 4.15 |
| Weekenda | 0.97 | 0.02 | < .001 | 2.53 | 2.63 | 2.74 |
| Baseline age | 0.06 | 0.02 | < .01 | 1.02 | 1.01 | 1.11 |
| Any cannabis usea × Recreational | 1.41 | 0.08 | < .001 | 3.52 | 4.10 | 4.78 |
| Any cannabis usea × timea | −0.001 | 0.0002 | < .001 | 0.99 | 0.99 | 0.99 |
| Recreational × timea | 0.001 | 0.0002 | < .001 | 1.0002 | 1.001 | 1.001 |
Note. Coefficients are unstandardized.
Denotes time-varying.
Fig. 1.
Interaction of cannabis use by type of user on alcohol use.
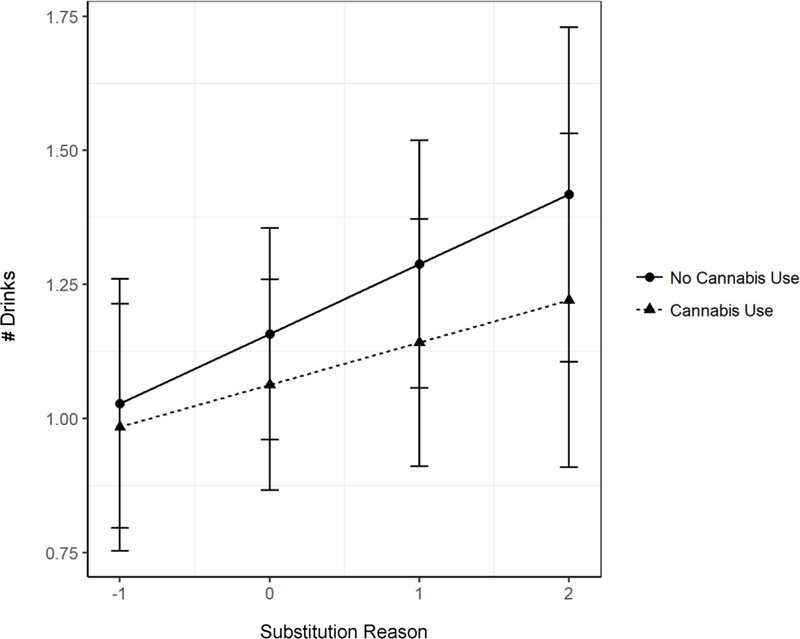
3.4. Longitudinal association between cannabis and alcohol use by alcohol substitution reason
Next, we examined frequency of self-reported medical cannabis substitution for alcohol as a moderator of the association between day-level cannabis use and number of drinks among medicinal users. Results revealed a significant interaction of any cannabis use and substitution reason (OR =.79; 95% CI =.73, .86; p < .001) (see Table 4 for model estimates). This suggests that among medicinal users, those who reported using cannabis to substitute for alcohol more frequently drank less on cannabis use days (Fig. 2). Finally, there was a small in magnitude three-way interaction between cannabis use, time, and substitution reason, suggesting medicinal users who reported more frequent use of cannabis as a substitute for alcohol drank less on cannabis use days over time, compared to those who reported less frequent use for substitution, who drank more on cannabis use days over time (OR =1.0007; 95% CI =1.0004, 1.001; p < .001).
Table 4:
Mixed Effects model of association between cannabis and time on alcohol use: moderation by alcohol substitution reason among medicinal users.
| Estimate | SE | p-value | Lower CI | OR | Upper CI | |
|---|---|---|---|---|---|---|
| Intercept | −1.22 | 0.83 | – | – | – | – |
| Any cannabis usea | −0.21 | 0.07 | <.01 | 0.71 | 0.81 | 0.93 |
| Substitution reason | 0.21 | 0.12 | 0.10 | 0.97 | 1.23 | 1.56 |
| Timea | 0.0002 | 0.0001 | 0.26 | 1.00 | 1.0001 | 1.0004 |
| % cannabis use days | 0.0004 | 0.005 | 0.94 | 0.99 | 1.0004 | 1.01 |
| Any ciga | 0.57 | 0.05 | <.001 | 1.59 | 1.76 | 1.95 |
| Any other druga | 2.09 | 0.16 | <.001 | 5.94 | 8.10 | 11.06 |
| Weekenda | 0.59 | 0.029 | <.001 | 1.70 | 1.80 | 1.91 |
| Baseline age | 0.06 | 0.02 | 0.03 | 1.01 | 1.06 | 1.11 |
| Any cannabis usea × substitution reason | −0.23 | 0.04 | <.001 | 0.73 | 0.79 | 0.86 |
| Any cannabis usea × timea | 0.0004 | 0.0002 | 0.04 | 1.00002 | 1.0004 | 1.001 |
| Substitution reason × timea | −0.0003 | 0.0001 | <.01 | 0.9995 | 0.9997 | 0.9999 |
| Any cannabis usea × substitution reason × timea | 0.001 | 0.0001 | <.001 | 1.0004 | 1.0007 | 1.001 |
Note. This analysis was conducted in the subsample of medicinal users only (n =64; 34,560 observations); Coefficients are unstandardized.
Denotes time-varying.
Fig. 2.
Interaction of substitution reason and cannabis use among medicinal users on alcohol use.
4. Discussion
This is the first study to examine day-level associations between daily cannabis use and alcohol consumption among medicinal and recreational cannabis users. We examined: (a) whether daily cannabis use predicted increased daily alcohol consumption across 18 months; (b) whether recreational cannabis users would drink more on cannabis use days compared to medicinal users; and (c) the role of cannabis as a self-reported substitution for alcohol among medicinal users. Results indicated that cannabis use was associated with higher levels of alcohol consumption at the daily level, and that this effect was consistent over time. There was also a significant moderation by type of user, in that recreational users drank more on cannabis use days compared to medicinal users. Follow-up analyses showed that among these medicinal users, those who reported more frequent use of cannabis to substitute alcohol were more likely to drink less on cannabis use days.
Our findings are consistent with other studies suggesting complementary use of alcohol and cannabis among recreational users (Gunn et al., 2018; Metrik et al., 2018b; Subbaraman, 2016). Further, significant negative effect of time and cannabis use on alcohol consumption was detected in our initial model, and in our second which considers type of user. However, in both models, these effects are of small magnitude, suggesting that the positive association between alcohol and cannabis use is relatively stable, but may reduce, over time. Although this is inconsistent with a recent study of college students in their first two years of school, which found a strong positive association between time and cannabis use on daily number of drinks (Gunn et al., 2018), this discrepancy may be a function of the unique samples. Compared to the present study sample of veterans, of which 45% and 35% had an AUD and CUD respectively at baseline, college students in their first two years of school in Gunn et al. (2018) were following a population-based trend of increased alcohol consumption during this developmental period (Stone et al., 2012; White et al., 2006). Our results supporting complementary use are also consistent with prospective studies that suggest cannabis use during treatment for alcohol use may result in poorer alcohol-related treatment outcomes (Aharonovich et al., 2005; Mojarrad et al., 2014; Subbaraman et al., 2018, 2017). Taken together, although results were of relatively modest effect sizes, this daily-level study suggests that cannabis use consistently complements alcohol consumption over time among recreational users.
Further, our finding that type of user moderated the effect of cannabis use on alcohol consumption helps to elucidate conflicting evidence in the field as to whether cannabis acts as a substitute or a complement to alcohol consumption (O’Hara et al., 2016; Subbaraman, 2014, 2016; Williams et al., 2004). Results suggest that cannabis is more likely to act as a substitute among medicinal users, but not recreational users. These results are consistent with other survey studies suggesting that medicinal users report using cannabis as a substitute for alcohol (Reiman, 2007, 2009). Overall, it may be that those who use cannabis for medicinal reasons may be less likely to experience the additional risks associated with co-use, compared to recreational users. Consistent with other studies (Lin et al., 2016; Loflin et al., 2017b; Subbaraman and Kerr, 2018), our sample of medicinal users were less likely to have an AUD and drank on fewer days compared to recreational users. However, our sample was also more likely to have a CUD and reported more frequent cannabis use days and co-use days across the assessment period. Therefore, although medicinal users may be less likely to experience clinically significant symptoms related to alcohol use, they were more likely to meet criteria for a CUD. However, this finding should be tempered by an important consideration in the literature regarding whether assessment methods for DSM-5 CUD symptoms translate for medicinal users. For instance, Loflin et al. (2017a,b) suggest that symptoms that assess frequency and density (average number of uses per day) of cannabis use may not be as indicative of problems in medicinal users compared to recreational users. Our preliminary follow-up analyses examining the role substitution among medicinal users confirmed that those who reported using cannabis to substitute for alcohol’s effects more frequently were less likely to drink more on cannabis use days, compared to medicinal users who reported less frequent substitution.
The present study has important implications for treatment and prevention. First, our results are consistent with several other recent studies of treatment samples suggesting that recreational use of cannabis is associated with increased alcohol consumption and should be avoided for those in treatment for AUD or alcohol related problems. These findings suggest caution should be taken in the wake of changes in recreational cannabis policy, as increased cannabis use could lead to increased problematic drinking among recreational users (Wen et al., 2015). In addition, there is a clear documented negative impact of cannabis use on AUD recovery for individuals with AUD in alcohol treatment (Subbaraman et al., 2018, 2017). Medicinal cannabis users in our sample consumed alcohol less frequently than recreational cannabis users, which could be interpreted as an additional indication that medicinal cannabis may serve as a replacement for alcohol use. However, these data were drawn from an observational longitudinal study not limited to an alcohol treatment-seeking sample and should not be applied to those in treatment for alcohol misuse. Furthermore, veterans in this sample endorsed a number of conditions for medical cannabis use including anxiety, stress, PTSD, pain, depression, and insomnia (Metrik et al., 2018a). Therefore, besides using cannabis as a substitute for alcohol, there may be important additional moderators among reasons for medical cannabis use that could clarify the cannabis-alcohol co-use association.
4.1. Limitations
This study should be understood in the context of several limitations. First, although the TLFB has established reliability and validity, it does require retrospective recounting of substance use. As with all self-report measures, this may be subject to recall biases. Although prior research suggests that this potential bias may be more pronounced in day-level analyses covering periods longer than 60 days (Hoeppner et al., 2010) and that the TLFB may underestimate frequency and quantity of alcohol use (Searles et al., 2002), there is also evidence to suggest that the TLFB is not subject to reduced reliability with increased time intervals (Carey, 1997; Searles et al., 2002). In other words, reports are shown to be consistent with increased intervals from 30 or 60 days to 366 days (Searles et al., 2002) or from 30 to 180 days (Carey, 1997). Second, we were also unable to establish temporal ordering of cannabis and alcohol use at the daily level. More detailed event-level ecological momentary assessment data would more directly address the question of whether or not cannabis use directly impacts alcohol consumption. Third, we relied on self-report data to determine user status (medicinal versus recreational). There is significant variability in the reported diagnoses for using cannabis, and often veterans reported more than one condition for using cannabis medicinally (Metrik et al., 2018a). It is also likely that some individuals use cannabis for both medicinal and recreational reasons. More nuanced measurement at the event-level regarding whether cannabis is being used recreationally or medicinally, and if medicinally, what condition it is used for (e.g., pain, anxiety) would provide important context for understanding the function of medicinal versus recreational cannabis use and its association with alcohol consumption. Ecological momentary assessment studies could examine these more nuanced associations in the moment to reduce recall bias and to more precisely examine related complex questions regarding the relative impact of medicinal versus recreational use on alcohol consumption. Fourth, we were unable to examine the effect of different cannabis products on these associations. For instance, there is evidence that cannabis products with higher concentrations of cannabidiol (CBD), a non-psychoactive cannabinoid, compared to products higher in Δ9–tetrahydrocannabinol (THC), may have unique medicinal and therapeutic benefits without the abuse potential (Freeman et al., 2019; Spindle et al., 2019) and CBD may even have promise as a candidate AUD pharmacotherapy (Turna et al., 2019). Therefore, medicinal users may be more likely to use cannabis products with CBD, which may pose a reduced risk of alcohol misuse. Fifth, we were unable to examine the order of onset for those with CUD and AUD during the assessment period. As our previous work shows, AUD and CUD status does has an impact on daily co-use behaviors (Metrik et al., 2018b), therefore future research should examine how onset of these diagnoses would further explicate the nature of the association between daily cannabis and alcohol use for medicinal and recreational users. Sixth, we were also unable to assess substitution reasons among recreational users given this measure was specific to medicinal users. Future research should examine whether using cannabis for substitution reasons is also associated with reduced alcohol consumption among recreational cannabis users. Finally, confidence in the accuracy of the current pattern of findings, particularly the observed interactions, will be strengthened by replication in larger and more representative populations (e.g. samples with a larger proportion of females with sufficiently powered sample sizes).
5. Conclusions
This is the first prospective study to examine the association between cannabis and alcohol consumption at the daily level and the first study to examine whether these daily use patterns differ as a function of medicinal versus recreational users. Results provide additional clarification to conflicting literature on whether cannabis and alcohol are substitutes or complements and suggest that medicinal cannabis users are more likely to substitute cannabis for alcohol, whereas recreational users are more likely to complement the two. Future studies should examine temporal ordering and event-level associations between cannabis and alcohol consumption and whether these effects are moderated by the conditions for which individuals use cannabis.
Acknowledgements
The authors gratefully acknowledge Cassandra Tardiff, Suzanne Sales, and Timothy Souza for their contribution to the project T32 AA007459 from National Institute on Alcohol Abuse and Alcoholism (Gunn).”The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.”
Role of funding sources
This study was supported by a grant R01 DA033425 (PIs Metrik, Borsari), from the National Institute on Drug Abuse (NIDA). The views expressed in this article do not necessarily reflect the position or policy of the Department of Veteran Affairs.
Footnotes
Declaration of Competing Interest
All of the listed authors declare that they have no conflicts of interests.
References
- Aharonovich E, Liu X, Samet S, Nunes E, Waxman R, Hasin D, 2005. Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: a prospective study. Am. J. Psychiatry 162 (8), 1507–1514. 10.1176/appi.ajp.162.8.1507. [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker BM, Walker SC, 2015. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67 (1), 1–48. 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Brière FN, Fallu JS, Descheneaux A, Janosz M, 2011. Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addict. Behav. 36, 785–788. 10.1016/j.addbeh.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Carey KB, 1997. Reliability and validity of the time-line follow-back interview among psychiatric outpatients: a preliminary report. Psychol. Addict. Behav. 11 (1), 26–33. 10.1037/0893-164x.11.1.26. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2013. Alcohol and Public Health: Alcohol-Related Disease Impact (ARDI). [Google Scholar]
- Chaloupka FJ, Laixuthai A, 1997. Do youths substitute alcohol and marijuana? Some econometric evidence. East. Econ. J. 23 (3), 253–276. [Google Scholar]
- Clements KW, Daryal M, 2005. Exogenous shocks and related goods: drinking and the legalisation of marijuana B. Econ. Lett. 89, 101–106. 10.1016/j.econlet.2005.05.017. [DOI] [Google Scholar]
- Cohen NL, Heinz AJ, Ilgen M, Bonn-Miller MO, 2016. Pain, Cannabis species, and cannabis use disorders. J. Stud. Alcohol Drugs 77, 515–520. 10.15288/jsad.2016.77.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W, Angold A, Shanahan L, Dreyfuss J, Dlamini I, Jane Costello E, 2012. Predicting persistent alcohol problems: a prospective analysis from the Great Smoky Mountain Study. Psychol. Med. 42 (9), 1925–1935. 10.1017/S0033291711002790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Funk R, Harrington Godley S, Godley MD, Waldron H, 2004. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction 99 (2), 125–133. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, First Spitzer, Gibbon W, 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) for DSMIV Biometrics Research, New York State Psychiatric Institute, New York. [Google Scholar]
- Freeman TP, Hindocha C, Green SF, Bloomfield MA, 2019. Medicinal use of cannabis based products and cannabinoids. BMJ 365 (l1141). 10.1136/bmj.l1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, Norris AL, Sokolovsky A, Micalizzi L, Jennifer E, Barnett NP, 2018. Marijuana use is associated with alcohol use and consequences across the first 2 years of college. Psychol. Addict. Behav. 32 (8), 885–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas AL, Wickham R, Macia K, Shields M, Macher R, Schulte T, 2015. Identifying classes of conjoint alcohol and marijuana use in entering freshmen. Psychol. Addict. Behav. 29 (3), 620–626. 10.1037/adb0000089. [DOI] [PubMed] [Google Scholar]
- Hjorthøj CR, Hjorthøj AR, Nordentoft M, 2012. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances — systematic review and meta-analysis. Addict. Behav. 37, 225–233. 10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Stout RL, Jackson KM, Barnett NP, 2010. How good is fine-grained Timeline Follow-back data? Comparing 30-day TLFB and repeated 7-day TLFB alcohol consumption reports on the person and daily level. Addict. Behav. 35 (12), 1138–1143. 10.1016/j.addbeh.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Fingar JR, Budney AJ, Naud S, Helzer JE, Callas PW, 2014. Marijuana use and intoxication among daily users: an intensive longitudinal study. Addict. Behav. 39, 1464–1470. 10.1016/j.addbeh.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LA, Ilgen MA, Jannausch M, Bohnert KM, 2016. Comparing adults who use cannabis medically with those who use recreationally: results from a national sample. Addict. Behav. 61, 99–103. 10.1016/j.addbeh.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Gruenewald PJ, Grube JW, Bersamin M, 2017. Adolescents, alcohol, and marijuana: context characteristics and problems associated with simultaneous use. Drug Alcohol Depend. 179, 55–60. 10.1016/j.drugalcdep.2017.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loflin M, Babson K, Browne K, Bonn-Miller M, 2017a. Assessment of the validity of the CUDIT-R in a subpopulation of cannabis users Assessment of the validity of the CUDIT-R in a subpopulation of cannabis users. J. Drug Alcohol Abuse 44 (1), 19–23. 10.1080/00952990.2017.1376677. [DOI] [PubMed] [Google Scholar]
- Loflin M, Earleywine M, Bonn-Miller M, 2017b. Medicinal versus recreational cannabis use: Patterns of cannabis use, alcohol use, and cued-arousal among veterans who screen positive for PTSD. Addict. Behav. 68, 18–23. 10.1016/j.addbeh.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Pérez De Los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C, 2010. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend. 115, 120–130. 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett KA, Turrisi R, Hultgren BA, Sell N, Reavy R, Cleveland M, 2017. When alcohol is only part of the problem: an event-level analysis of negative consequences related to alcohol and other substance use. Psychol. Addict. Behav. 31 (3), 307–314. 10.1037/adb0000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Bassett S, Aston ER, Jackson K, Borsari B, 2018a. Medicinal versus recreational cannabis use among returning veterans. Transl. Issues Psychol. Sci. 4 (1), 6–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Gunn RL, Jackson KM, Sokolovsky AW, Borsari B, 2018b. Daily patterns of marijuana and alcohol co-use among individuals with alcohol and cannabis use disorders. Alcohol. Clin. Exp. Res. 42 (6). 10.1111/acer.13639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, Borsari B, 2016. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychol. Addict. Behav. 30 (7), 743–754. 10.1037/adb0000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojarrad M, Samet JH, Cheng DM, Winter MR, Saitz R, 2014. Marijuana use and achievement of abstinence from alcohol and other drugs among people with substance dependence: a prospective cohort study. Drug Alcohol Depend. 142, 91–97. 10.1016/j.drugalcdep.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara RE, Armeli S, Tennen H, 2016. Alcohol and cannabis use among college students: substitutes or complements? Addict. Behav. 58, 1–6. 10.1016/j.addbeh.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Kloska DD, Terry-McElrath YM, Lee CM, O’Malley PM, Johnston LD, 2017. Patterns of simultaneous and concurrent alcohol and marijuana use among adolescents. Am. J. Drug Alcohol Abuse 44 (4), 441–451. 10.1080/00952990.2017.1402335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Hughes JR, 2010. Daily marijuana users with past alcohol problems increase alcohol consumption during marijuana abstinence. Drug Alcohol Depend. 106, 111–118. 10.1016/j.drugalcdep.2009.07.027. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2013. R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Raudenbush SW, Bryk AS, 2002. Hierarchical linear models: applications and data analysis methods, 2nd ed. Advanced Quantitative Techniques in the Social Sciences Vol. 2nd Sage, Thousand Oaks, CA. [Google Scholar]
- Reiman A, 2007. Medical Cannabis patients: patient profiles and health care utilization patterns. Complement. Health Pract. Rev. 12 (1), 31–50. 10.1177/1533210107301834. [DOI] [Google Scholar]
- Reiman A, 2009. Cannabis as a substitute for alcohol and other drugs. Harm Reduct. J 10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinarman C, Nunberg H, Lanthier F, Heddleston T, 2011. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J. Psychoactive Drugs 43, 128–135. 10.1080/02791072.2011.587700. [DOI] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L, 2011. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: implications for screening, diagnosis and treatment. Drug Alcohol Depend. 116, 93–101. 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Searles JS, Helzer JE, Rose GL, Badger GJ, 2002. Concurrent and retrospective reports of alcohol consumption across 30, 90 and 366 days: interactive voice response compared with the timeline follow back. J. Stud. Alcohol 63 (3), 352–362. 10.15288/jsa.2002.63.352. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD, 2006. Heavy alcohol use compared to alcohol and marijuana use: do college students experience a difference in substance use problems? J. Drug Educ. 36 (1), 91–103. [DOI] [PubMed] [Google Scholar]
- Snijders T, Bosker R, 1999. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Sage, Thousand Oaks, CA. [Google Scholar]
- Sobell L, Sobell M, 1992. Timeline Follow-Back: a technique for assessing self-reported alcohol consumption Psychosocial and Biological Methods. Humana Press, Totowa, NJ, pp. 41–72. [Google Scholar]
- Spindle TR, Bonn-Miller MO, Vandrey R, 2019. Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr. Opin. Psychol. 10.1016/j.copsyc.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staiger PK, Richardson B, Long CM, Carr V, Marlatt GA, 2012. Overlooked and underestimated? Problematic alcohol use in clients recovering from drug dependence. Addiction 108, 1188–1193. 10.1111/j.1360-0443.2012.04075.x. [DOI] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, Catalano RF, 2012. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict. Behav. 37 (7), 747–775. 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, 2014. Can cannabis be considered a substitute medication for alcohol? Alcohol Alcohol. 49 (3), 292–298. 10.1093/alcalc/agt182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, 2016. Substitution and complementarity of alcohol and Cannabis: a review of the literature. Subst. Use Misuse 51 (11), 1399–1414. 10.3109/10826084.2016.1170145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Barnett SB, Karriker-Jaffe KJ, 2019. Risks associated with mid level cannabis use among people treated for alcohol use disorder. Alcohol. Clin. Exp. Res. 43 (4), 690–694. 10.1111/acer.13973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Kerr WC, 2015. Simultaneous vs. Concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcohol. Clin. Exp. Res. 39 (5), 872–879. 10.1111/nyas.12666.Saccadic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Kerr WC, 2018. Alcohol use and risk of related problems among cannabis users is lower among those with medical cannabis recommendations, though not due to health. J. Stud. Alcohol Drugs 79 (6), 935–942. 10.15288/jsad.2018.79.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, Stout R, 2018. Cannabis use during alcohol treatment is associated with alcohol-related problems one-year post-treatment. Drug Alcohol Depend. 193, 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, Swift R, 2017. Cannabis use during treatment for alcohol use disorders predicts alcohol treatment outcomes. Addiction 112 (4), 685–694. 10.1111/add.13693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turna J, Syan SK, Frey BN, Rush B, Costello MJ, Weiss M, Mackillop J, 2019. Cannabidiol as a novel candidate alcohol use disorder pharmacotherapy: a systematic review. Alcohol. Clin. Exp. Res. 43 (4), 550–563. 10.1111/acer.13964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR, 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ. 42, 64–80. 10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- White HR, McMorris BJ, Catalano RF, Fleming CB, Haggerty KP, Abbott RD, 2006. Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood: the effects of leaving home, going to college, and high school protective factors. J. Stud. Alcohol 67 (6), 810–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Liccardo Pacula R, Chaloupka FJ, Wechsler H, 2004. Alcohol and marijuana use among college students: economic complements or substitutes? Health Econ. 13 (9), 825–843. 10.1002/hec.859. [DOI] [PubMed] [Google Scholar]
- Yurasek A, Aston ER, Metrik J, 2017. Co-use of alcohol and cannabis: a review. Curr. Addict. Rep. 4 (2), 184–193. 10.1007/s40429-017-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]