ABSTRACT
We encountered an extremely rare case where a patient with cat eye syndrome (CES) who presented with symptoms of posterior semicircular canal dehiscence (PSCD). CES is a rare genetic disorder, resulting from duplication of chromosome 22. Patients may present with variable phenotypes, including characteristic of coloboma, heart defect, periauricular skin pit/tag, microtia, anal atresia and mildly retarded mental development in some cases. PSCD is also a disease of the inner ear, where patients present with third window signs and symptoms due to lack of bony coverage. PSCD is usually associated with a high riding jugular bulb and fibrous dysplasia. In this study, we report a new otologic finding in CES patient as an association of PSCD and high jugular pulp. We describe the work up and its findings and the management of this patient.
SIMILAR CASES PUBLISHED::
None.
INTRODUCTION
A 28-year-old male special needs teacher, a known case of CES, was referred to the otolaryngology outpatient clinic in King Fahad Specialist Hospital in Dammam for chronic dizziness. The patient complained of dizziness after head trauma, as he fell 3 months prior to presentation on the left side of his head and hit a table. Since then, he had complained of non-rotatory vertigo lasting for around 10 minutes, occurring once or twice daily. It usually occured in the early morning when he woke from sleep and he noticed that the dizziness could be evoked by a loud voice. The dizziness was associated with left ear progressive hearing loss, oscillopsia, pulsatile tinnitus and autophony. He did not complain of headache or nystagmus.
The patient had history of multiple anal fissure and accessory auricle to the right ear that was excised at the age of 2 years. In addition, he had a micopenis with bilateral undescended testis, for which an orchiopexy was performed during infancy. Also, he received growth hormone injections at the age of 10 to 12 years for short stature due to pituitary dwarfism. Before 9 years, he was operated on for carpal tunnel syndrome. Moreover, he was diagnosed with Duane syndrome in the right eye, and underwent surgery for right lateral rectus muscle resection. Finally, he was found to have thoracic scoliosis and was referred to rehabilitation therapy.
The otoscopic examination was normal with negative fistula test. There was no spontaneous nystagmus; both Romberg and Fukuda tests were negative. Tympanometry showed type A with reserved stapedial reflexes. The audiogram showed bilateral borderline to mild conductive hearing loss through 4 KHz, then gradual sloping to severe sensorineural hearing loss through 8 KHz (Figure 1).
Figure 1.
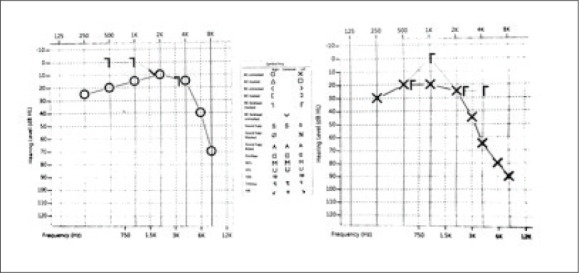
Audiogram showing bilateral low frequency conductive hearing loss and high frequency sensorineural hearing loss.
The video head impulse test showed a gain for the left anterior canal impulses within the normal range of 0.95 while the right posterior canal impulses show a reduced gain of 0.47. Vestibular evoked myogenic potential revealed a lowered threshold on the right side compared to the left side (70 dBHL versus 80 dBHL respectively), with significant inter-aural amplitude asymmetry, ratio of 44.37% to the right side (Figure 2). Temporal bone computed tomography scan with contrast showed right high riding jugular bulb with possibility of jugular diverticulum and focal dehiscence of the inferior limb of the posterior semicircular canal and vestibular aqueduct. A contrast-enhanced magnetic resonance venography showed superior out-pouch arising from the right enlarged jugular bulb, which confirms the right jugular bulb diverticulum (Figure 3). The patient was managed conservatively with vestibular rehabilitation. Three months later, symptoms were improved and patient was advised to avoid head trauma and continue follow up with vestibular clinic.
Figure 2.
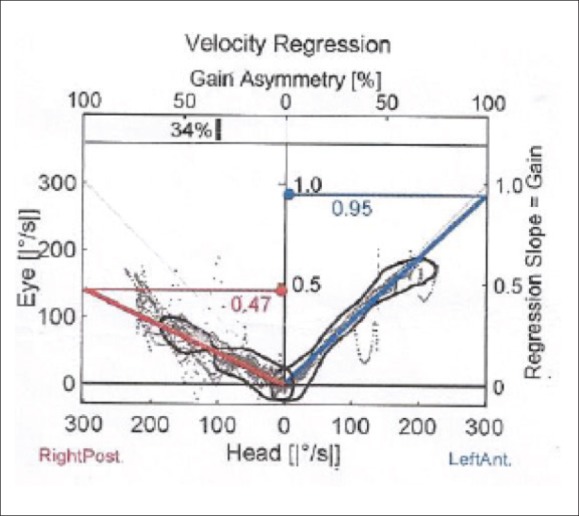
Video head impulse test showing asymmetric gain.
Figure 3.
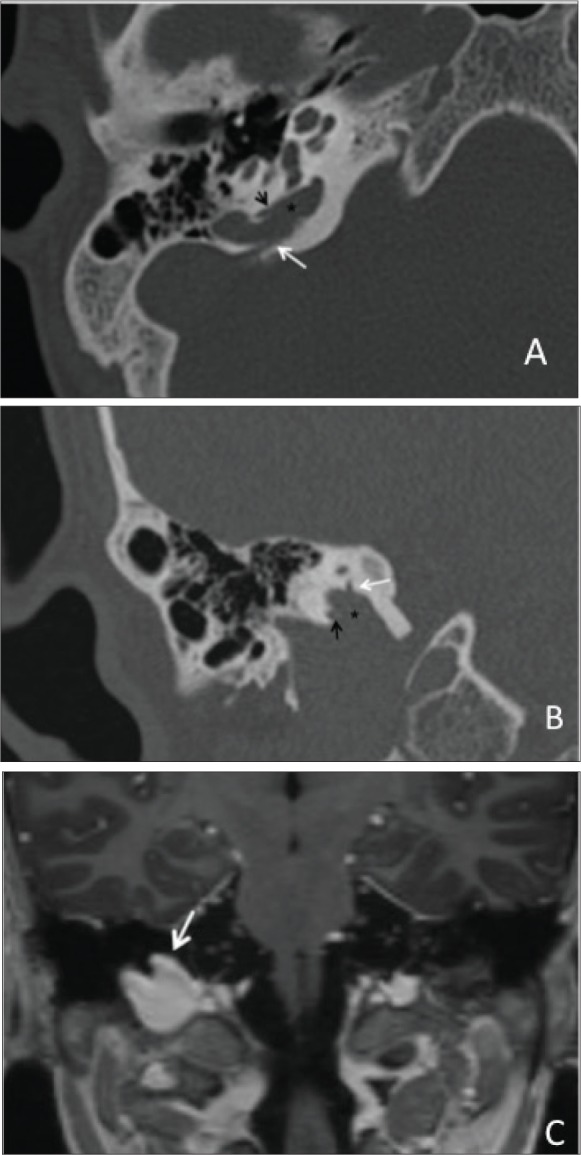
Axial (A) and coronal (B) temporal bone CT in bone window demonstrates a superior lobulation (asterisk) emanating from the high ridIng jugular bulb. There are two focal bony dehiscences along the inferior limb of posterior SSC (black arrow) and vestibular aqueduct (white arrow). C: Coronal 3D T1 post contrast demonstrates a focal out-pouch of the right jugular bulb extending superiorly (arrow) consistent with a jugular bulb diverticulum.
DISCUSSION
PSCD has not been described in association with CES before this case report. It seems to be an incidental association but adds to the varying otologic presentations of this syndrome. It is important to differentiate this association from otologic manifestations of CES because it might be managed differently. Intractable 3rd window symptoms seen with PSCD can be managed with obliteration of dehiscence.
CES is a rare genetic disorder, resulting from the duplication of chromosome 22, as the short arm (p) and small region of the long arm (q) of are present 3 (trisomy) to 4 (tetrasomy) times instead of twice.1 The name of CES is derived from the eye abnormality that is usually associated with the syndrome. But it is also known as Schmid Fraccaro syndrome, chromosome 22 partial tetrasomy, chromosome 22 partial trisomy and chromo-some 22-inverted duplication. Until recently, there was no accurate estimation of the likelihood of CES occur-rence possibly because patients who have some or a few of the associated symptoms and signs are rarely diagnosed with CES or are undiagnosed all together. Schinzel et al estimated an incidence of approximately 1:50,000 to 1:150,000 individuals in Northeastern Switzerland, with no gender preference.2
CES patients may present with variable phenotypes, which vary from near normal to fatal malformations, rendering diagnostic clinical criteria difficult to establish.3 Classically, patient present with a triad of iris coloboma, anal atresia and preauricular skin tag/pit. However, Berends et al reported in his study that only 41% of CES patients had the triad, which means that it might be difficult to diagnose almost 60% of the patients.1 Cat eye is known as coloboma, i.e. failure to close a fissure in the lower part of the eye during early development, which gives the eye a keyhole appearance. It may involve the iris, choroid and the retina. If only the iris is affected, vision is not affected but if the choroid and retina are affected as well, vision will be affected and the patient may develop blindness. They may present with other eye abnormalities including strabismus, cataract, aniridia or microphthalmia. They may develop also Duane syndrome, an abduction/adduction limitation due to failure of innervation of the lateral rectus by the abducens nerve.4
Otologic manifestations in the majority of the patients involve mainly preauricular skin tag and pits. They may present with low set ears and microtia, conductive or sensorineural hearing loss.5 However, to our knowledge there are no reports of PSCD and the jugular diverticulum in this syndrome before this paper. PSCD is a rare disease of the inner ear, where a 3rd window is created due to defects in the bony structures of the inner ear. A CT scans analysis of 700 temporal bone showed 9.6% semicircular canal dehiscence; 8% in the superior canal, 1.2% in the posterior canal and 0.4% in the lateral canal.6 Clinically, PSCD patients present with nonspecific auditory and vestibular complaints including hearing loss, autophony, aural fullness, vertigo, disequilibrium, pulsatile tinnitus, Tullio phenomenon and Hennebert sign.7 Developing the 3rd window symptoms after sustaining a head trauma is a common scenario in canal dehiscence patients.8 Studies showed an association between PSCD and high riding jugular bulb with fibrous dysplasia.7 Reaching the diagnosis requires CT scan and VEMP which is very sensitive to detect third window, as it shows lowered threshold at increased amplitude.9 For such variable phenotypes, a multidisciplinary management team is needed according to the individual symptoms and signs. With appropriate care, the majority of the CES patients will have a normal life expectancy unless they have severe symptoms, such as heart or kidney defects. In conclusion, highly variable phenotype in CES makes it difficult to diagnose the patient. A thorough examination is mandatory to diagnose all variable presentations in this syndrome. Although there are no reported cases of CES patients presenting with PSCD, this case proves that it is a possible finding and should be ruled out by radiologic and available audiological tests.
Funding Statement
None.
REFERENCES
- 1.Berends MJ, Tan-Sindhunata G, Leegte B, van Essen AJ.. Phenotypic variability of Cat-Eye syndrome. Genet Couns Geneva Switz. 2001;12(1):23-34. [PubMed] [Google Scholar]
- 2.Ko JM, Kim JB, Pai KS, Yun J-N, Park S-J.. Partial tetrasomy of chromosome 22q11.1 resulting from a supernumerary isodicentric marker chromosome in a boy with cat-eye syndrome. J Korean Med Sci. 2010;25(12):1798-1801. doi: 10.3346/jkms.2010.25.12.1798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosias PR, Sijstermans JM, Theunissen PM, Pulles-Heintzberger CF, De Die-Smulders CE, Engelen JJ, et al. Phenotypic variability of the cat eye syndrome. Case report and review of the literature. Genet Couns Geneva Switz. 2001;12(3):273-282. [PubMed] [Google Scholar]
- 4.Andrews CV, Hunter DG, Engle EC.. Duane Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993. http://www.ncbi.nlm.nih.gov/books/NBK1190/. Accessed May 12, 2018. [Google Scholar]
- 5.Cullen P, Rodgers CS, Callen DF, Connolly VM, Eyre H, Fells P, et al. Association of familial Duane anomaly and urogenital abnormalities with a bisatellited marker derived from chromosome 22. Am J Med Genet. 1993;47(6):925-930. doi: 10.1002/ajmg.1320470623 [DOI] [PubMed] [Google Scholar]
- 6.Stimmer H, Hamann KF, Zeiter S, Nau-mann A, Rummeny EJ.. Semicircular canal dehiscence in HR multislice computed tomography: distribution, frequency, and clinical relevance. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. 2012;269(2):475-480. doi: 10.1007/s00405-011-1688-6 [DOI] [PubMed] [Google Scholar]
- 7.Chien WW, Carey JP, Minor LB.. Canal dehiscence. Curr Opin Neurol. 2011;24(1):25-31. doi: 10.1097/WCO.0b013e328341ef88 [DOI] [PubMed] [Google Scholar]
- 8.Gubbels SP, Zhang Q, Lenkowski PW, Hansen MR.. Repair of posterior semicircular canal dehiscence from a high jugular bulb. Ann Otol Rhinol Laryngol. 2013;122(4):269-272. doi: 10.1177/000348941312200409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spasic M, Trang A, Chung LK, Ung N, Thill K, Zarinkhou G, et al. Clinical Characteristics of Posterior and Lateral Semi-circular Canal Dehiscence. J Neurol Surg Part B Skull Base. 2015;76(6):421-425. doi: 10.1055/s-0035-1551667 [DOI] [PMC free article] [PubMed] [Google Scholar]


