Abstract
Rationale.
It has long been known that factors of the mind and of interpersonal relationships influence health, but it is only in the last 50 years that an independent scientific field of health psychology appeared, dedicated to understanding psychological and behavioral processes in health, illness, and healthcare.
Objective and method.
This article (a) reviews important research that answers the question of how human beings can have longer, happier lives; and (b) highlights trends in health psychology featuring articles in Social Science & Medicine as well as other related literature.
Results.
Since the 1970s, health psychology has embraced a biopsychosocial model such that biological factors interact and are affected by psychological and social elements. This model has illuminated all subjects of health, ranging from interventions to lower stress and/or to improve people’s ability to cope with stressors, to mental and physical health. Importantly, a health psychology perspective is behavioral: The majority of chronic diseases of today can be avoided or reduced through healthy lifestyles (e.g., sufficient exercise, proper diet, sufficient sleep). Thus, behavior change is the key target to help reduce the immense public health burden of chronic lifestyle illnesses. Health psychology also focuses on how social patterns influence health behavior and outcomes, in the form of patient-provider interactions or as social forces in communities where people live, work, and play. Health psychology is congenial to other health sciences, especially when allied with ecological perspectives that incorporate factors upstream from individual behavior, such as networks linked to individuals (e.g., peer groups, communities). Over its history, health psychology research has been responsive to societal and medical needs and has routinely focused on understanding health disparities.
Conclusion.
By relying on a strong interdisciplinary approach, research in health psychology provides a remarkably comprehensive perspective on how people can live healthier lives.
Keywords: biopsychosocial model, chronic disease, stress, coping, mental health, patient-provider interactions, health disparities
1. Introduction
What are the keys to a healthy, happy, productive life? Along with other scientific fields, this question has been richly addressed by health psychology, which is concerned with psychological and behavioral processes in health, illness, and healthcare. Health psychology emerged in recent decades as an important contributor to a broader effort aimed to ameliorate the most pressing health-related issues in the world today: health, medical care, stress and coping, and how best to prevent, treat, and/or manage chronic disease. Health psychology offers a diverse, interdisciplinary perspective featuring a biopsychosocial model that takes into account psychological, physiological, and environmental influences on health. Health psychology also brings other key factors to bear on health, including culture, socioeconomic factors, stigma, patient-provider interactions, among others. Health psychology is concerned both with morbidity and mortality.
Our main goal in this article is to review health psychology’s prominent findings and theoretical perspectives, while giving some sense of the field’s history. Of course, it is impossible to do this subject justice in a single article; moreover, it is important to honor all of the history of health psychology as well as influences from related fields, even while we highlight research published in Social Science & Medicine. Many of the trends we observe in health psychology are in fact part of trends in science and health; at key junctures, we elucidate intersections of this field with other disciplines. It is also important to acknowledge that whereas the field of health psychology addresses global health, this review focuses mainly on issues related to Western society and its health. In Section 2, we describe the dominant theoretical perspective in health psychology, the biopsychosocial model, which reveals the often dynamic interrelationships between biological, psychological, and social factors. This model emerged from research on health psychology’s most central subject matter, stress. This section highlights the central role that habitual behavior plays in setting the stage for chronic illnesses such as hypertension and coronary heart disease. In Section 3, we consider how social interactions and networks (e.g., patient-provider interactions; community stress) affect health and review interventions to lower stress, to improve people’s ability to cope with stressors, and to address other health issues. In Section 4, we offer reflections on trends in health psychology, and Section 5 sums up the field’s answers to the question of how best to maximize lives lived.
2. The Necessity of an Integrative Conceptualization of Health
2.1. From Communicable to Non-Communicable Diseases and the Centrality of Health Behaviors
Medical science has witnessed many revolutions in its history, and these continue to unfold at a quickening pace. As medical science improved, so did public health: Until this era, human lives might in fact be well typified as nasty, brutish, and short, to paraphrase the 17th century political philosopher, Thomas Hobbes. Between 1800 and 2000, lifespans doubled from an average of about 35 years to 70; developed countries led the trend in expanding lifespan, but in recent decades, lagging nations have been closing the gap. Medical science steadily developed better maternal care—saving the lives not only of more women giving birth but also the lives of their newborn infants. Until at least the first half of the 20th century, viral influenza strains regularly killed millions of people in brief epidemics—medical science developed antibiotics and vaccines that transformed fatal or debilitating diseases into nuisance conditions that can be stopped before they threaten life or, at best, prevent them altogether. It is important to recognize that it was not just improvements in medical care that drove progress but also improved nutrition, shelter, transportation, and perhaps most of all, improved public sanitation services.
Even as medical solutions and technological advances improved public health, they also created unanticipated problems. In developed countries, the decreasing incidence of acute infections appears to be contributing to the increase in autoimmune and allergic diseases, according to the hygiene hypothesis (Okada et al., 2010). Moreover, assistive technology has also led to a sedentary lifestyle coupled with the easy availability of fast (and processed) food that has created a rise in avoidable chronic diseases. While there are still over 800 million people in the world suffering from chronic hunger, worldwide obesity rates have more than doubled since 1980, and youth obesity rates have tripled in the past 30 years (Chan, 2016; Ogden et al., 2015). America is in the midst of a healthcare crisis; approximately 84 million U.S. adults have prediabetes, and more than one-third of American adults have obesity, contributing to some of the leading causes of preventable death (Ogden et al., 2015).
The financial burden of chronic lifestyle illness is rising, placing a large toll on the healthcare system that may not be sustainable. In 2014, 16 million people died prematurely – before the age of 70 – due to chronic disease, according to the World Health Organization (WHO) (2015). Chronic disease conditions are noncommunicable diseases as they are not passed from person to person, and include four main types: 1) cardiovascular diseases (e.g., heart attacks and stroke); 2) cancers; 3) chronic respiratory diseases (e.g., chronic obstructive pulmonary disease, asthma); and 4) diabetes. In 2015, the WHO stated that “Premature noncommunicable disease deaths can be significantly reduced through government policies reducing tobacco use, harmful use of alcohol, unhealthy diets and physical inactivity, and delivering universal health care.” Notably, the success of this perspective hinges on individuals adopting and maintaining healthy lifestyles and receiving network support such as care from providers who understand and address the causes of these conditions. Accordingly, policy officials increasingly view behavior change on the population level as a key target to help reduce the immense burden of chronic disease.
2.2. A Biopsychosocial Approach Emerges
For the past two centuries, the biomedical model dominated medical science and practice, defining health as freedom from disease, pain, and defects; thus, the normal human condition is “healthy.” Yet, health is a continuum, and the absence of disease does not necessarily mean one is in a state of good health. Modern medical systems are expected to excel at treating diseases of biological etiology, but in the past, the biomedical model was built on a narrow, reductionist strategy that focused on biological aspects of disease and illness. Is illness always caused by biological factors? Will targeting detrimental biological factors guarantee a return to health? Health psychologists increasingly have argued that these are false assumptions, and stress is known to interact with and exasperate diseases of biological etiology (e.g., Wade & Halligan, 2004). Although the biomedical model certainly drove and still drives many innovations in medicine and medical care (e.g., including increasing understanding of the biological mechanisms of mental disorders), a biomedical perspective alone does not guarantee a positive outcome, nor explain a number of phenomena such as placebo effects and health disparities; psychological and social elements must also be included, as well as community-level factors and environment.
Health care professionals bear witness to the importance of other factors besides disease in the etiology of illness, and health psychology has provided updated models to take these factors into account. It was in the 1970s that the field of health psychology more formally emerged, allied with behavioral medicine, which posited that positive behavior change creates better health (Schwartz & Weiss, 1978). Physician George L. Engel (1977) was one of the first to propose and label a broad biopsychosocial model that emphasized the importance of an ecological relationship between an individual and his/her environment, and how an individual perceives his/her environment. Health psychologists quickly embraced and promoted this perspective, and today, biopsychosocial models are nearly universally embraced—at least in theory, if not in practice (Adler, 2009; Ogden, 1995). Moreover, as Section 3.2 expands, a biopsychosocial perspective is congenial not only to health psychology but also to other disciplines. It provides a foundation for “lifestyle medicine”, which is an emerging effort to broaden the scope of mainstream medicine to include the use of evidence-based lifestyle therapeutic approaches, such as a predominantly whole food, plant-based diet, exercise, sleep, stress management, alcohol moderation and tobacco cessation, and other non-drug modalities, to prevent, treat, and, potentially even reverse lifestyle-related, chronic diseases (Antonovsky, 1993; Egger et al., 2009). Similarly, education programs for medical professionals are incorporating lifestyle medicine into their curriculum to help healthcare providers better assist patients in developing self-care strategies to improve one’s own health (Vinje et al., 2017; Egger et al., 2009). In short, a more holistic view of health is necessary.
2.3. Mechanisms Underlying Stress and Chronic Disease
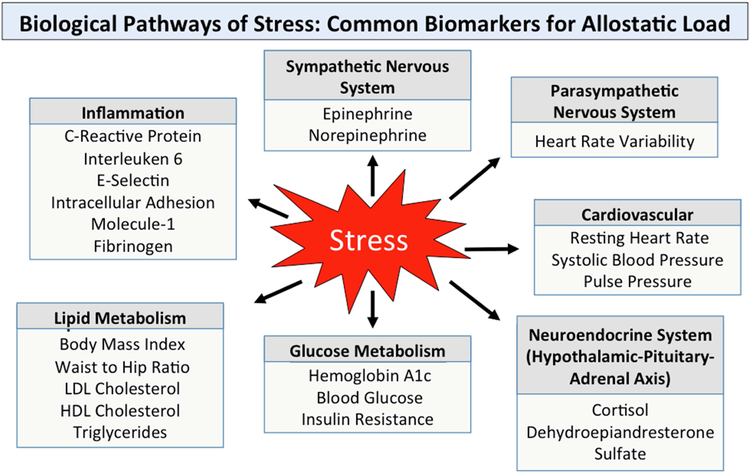
Stress is a central concept in health psychology because it impacts nearly any bodily system, either directly or indirectly. Traditionally, health psychologists measured stress based on self-reports of daily stressors, stressful life events, adverse childhood experiences (ACEs) such as emotional, physical, and sexual abuse, or food insecurity. More recently, biological measures of chronic stress have become more commonplace with cortisol as a predominant biomarker. Studies linking stressful life conditions to later morbidity and mortality show that stress can have direct and measureable effects on the body through allostatic load, which is overall stress-induced physiological wear-and-tear. Studies often divide common measurements of allostatic load into categories representing the underlying physiological systems, such as (a) neuroendocrine system, (b) immune and inflammatory system, (c) metabolic system, (d) cardiovascular and respiratory systems, and (e) nervous system (Solís et al., 2016). New biomarkers are emerging at a rapid pace to measure the impact of stress upon each of these biological pathways. A recent study used 23 different biomarkers to quantify allostatic load (see Fig. 1; Schwartz, 2017); multivariate approaches that employ a broad range of biomarkers are preferred due to the high complexity of the underlying biological systems, whereas studies that focus on only one or two biomarkers may yield inconsistent findings (Morrisette-Thomas et al., 2014).
Fig. 1.
Stress can have a negative long-term impact on health through multiple physiological pathways and biological systems (Schwartz, 2017). Biological measures appear below each system; researchers commonly combine measurements such as these to quantify overall allostatic load.
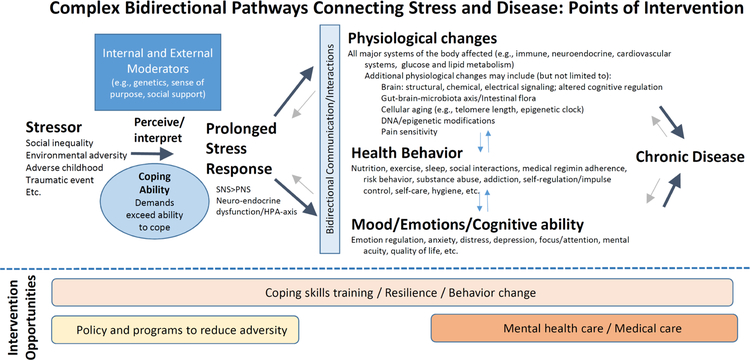
In more detail, Fig. 2 illustrates pathways through which chronic stress can contribute to chronic disease, including physiological responses that interact with changes in mood, behavior, and environment, and may also be influenced by genetics and epigenetic modifications. Pathways are complex, bidirectional, and can be self-reinforcing. Studies have shown that social and environmental stressors such as low parental education, maternal distress, and child abuse lead to increased cardiovascular disease-related risks in children, which may be due in part to desensitization of the children’s neuroendocrine-immune response (Riis et al., 2016). Among other results, Schwartz (2017) found that allostatic load was higher in people who perceived more inequality, emphasizing the importance of perceptions in determining how stimuli convey their effects. Similarly, social adversity (e.g., poverty, unemployment, low education, lack of social support) increases the risk of chronic disease through changes in immune cell distribution, contributing to the dualistic response of immune function in the face of chronic stress (i.e., reduced immune function and increased chronic inflammation) (Acabchuk et al., 2017; Simons et al., 2017). Disparities in education offer a further example of a stress-related impact, with inflammation accounting for the largest portion of the link between low education and increased risk of mortality (Todd, Shkolnikov, & Goldman, 2016). Thus, inflammation is emerging as an important biological pathway underlying health disparities.
Fig. 2.
Pathways and points of intervention between stress and chronic disease. The relationship between stress and chronic disease is highly complex, bidirectional, and often self-reinforcing (blue and light gray arrows). Intervention opportunities to reduce the negative health burden of stress along the pathway appear below the dashed line. See Fig. 1 for additional physiological changes. PNS=parasympathetic nervous system; SNS=sympathetic nervous system.
Much research has shown that stress leaves a biological mark, getting “under the skin” through various pathways to contribute to long-term health or disease (Acabchuk et al., 2017; Das, 2016). Given that stress has such powerful effects, it is crucial not only to understand what causes stress but also to identify plausible opportunities of intervention (Fig. 2). Programs that enhance coping skills, especially those that build resilience, can offer a protective buffer against the negative health burden of stress. Resilience is defined as the ability to survive and thrive despite exposure to difficulties (e.g., trauma, adversity). Factors that improve resilience include positive appraisal coping, effective cognitive and emotion regulation, self-efficacy, strong social support and family bonds (e.g., Bonanno, 2004; Li et al., 2017). A large part of current research focuses on investigating mechanisms of action, or “active ingredients” of interventions aimed to improve self-regulation and build resilience to stress in order to maximize outcomes when such interventions are translated into community-based programs. The points of intervention opportunities visualized in Fig. 2 emphasize the broad reach of behavior change and resilience building strategies to reduce the burden of mental health and medical care.
3. Social Interactions, Networks, and Interventions
3.1. Social Networks for—or Against—Health
Section 2 documented the powerful role that stressors play in health and listed some social pressures that are connected to stress (e.g., trauma, stigma). In fact, stresses humans face often result from other people: family obligations, relationships, work stress, financial issues, legal problems, and even minor disruptions like traffic or waiting in line. Furthermore, struggling to maintain healthy behavior (trying a new diet, too much or too little exercise, quitting smoking) can also be a major source of stress. Regardless of whether stresses are caused by other people or not (e.g., food insecurity, lack of electricity, extreme weather), social support is a key element of the solution; allied networks can be a force for health.
3.1.1. Networks can be positive or negative for health
There are two sides to social networks, negative and positive. On the negative side, it is no surprise that other people cause stress, ranging from the death of a close friend or family member to the stress caused by a demanding boss, abusive spouse, or sick child. The influence of the social environment is especially critical during development: Youth from a family environment marked by socioeconomic disadvantage, a lack of support and structure, hostility, and conflict (and other ACEs) are at higher risk for developing poor mental and physical health outcomes such as depression, substance use, cardiovascular disease, hypertension, and obesity (Repetti et al., 2002). Parental smoking is one of the best predictors for smoking in their children (Palmer, 1970). More family illnesses occur when a parent is deeply depressed (Lewis et al., 1989). Stressed or burnt-out teachers also stress their pupils (Oberle & Schonert-Reichl, 2016). Of course, having a particular disease or illness potentially links into negative social pressures, as has been amply demonstrated in the stigma associated with HIV/AIDS (e.g., Parker & Aggleton, 2003), mental illness (Livingston & Boyd, 2010), and addiction (McGinty et al., 2015). The same is true for people with stigmatized identities in terms of gender (Hankivsky, 2012), sexual orientation (Hatzenbuehler et al., 2014), or race (Reid, Dovidio, Ballester, & Johnson, 2014). Workplace inequality creates stress-related illness (e.g., de Jonge, Bosma, Peter, & Siegrist, 2000; Marmot et al., 1991; Schnorpfeil et al., 2003; Siegrist et al., 2004). People commonly fret economic debts or time commitments to others. Such robust effects offer stark testimony to the stress that negative social networks often create. It may even often be, as the French existential philosopher Jean-Paul Sartre put it, that “hell is other people.”
On the positive side, other people are essential to human development itself and good social relationships help individuals thrive (Folkman, 1997). Of course, secure child development is associated with longer, happier, more productive lives (Berkman, Glass, Brissette, & Seeman, 2000). But the health benefits of strong relationships are not limited to development; they are essential throughout the lifespan. Marital satisfaction was found to be a better buffer of day-to-day fluctuations in perceived health and happiness in older adults compared to time spent with others, emphasizing the importance of strong relationship bonds in maintaining happiness in the lives of older adults (Waldinger et al., 2010). Quality of close relationships appear crucial; for example, in a Harvard study, relationship satisfaction at age 50 predicted health at age 80 better than any biomarker (Waldinger & Schulz, 2016). People with larger social networks suffer fewer colds despite direct exposure to a rhinovirus (Cohen et al., 1997). Positive networks can promote having a greater sense of purpose, which is a critical determinant of longevity (Boyle et al., 2010). People who volunteer for community causes improve their mental health (Borgonovi, 2008). Social support, whether in the form of friends or family, was found to assist minority women in initiating an exercise regimen (Eyler et al., 1999). Marriage is consistently linked to health (Lewis et al., 2006); Umberson (1992) found that married men engage in healthier behavior because their spouses monitor and attempt to control their health behavior. As Mineo (2017) aptly summarized, “Good genes are nice, but joy is better.” Open communication between father and child positively affects the family’s psychosocial functioning (Christensen, 2004). Social networks also have a role in illness recovery: Breast cancer patients who felt satisfied with the level of support they received from family members were significantly less anxious and depressed (Neuling & Winefield, 1988). Many people with serious disabilities nonetheless report having a high quality of life, in part due to good relationships (Albrecht & Devlieger, 1999). Some people and communities are more resilient than others due to the positive social interactions at critical junctures (Bonanno, 2004; Berkman & Syme, 1979). In summary, positive social networks improve productivity, healthy behavior, immune function, disease recovery, purpose, resilience and overall quality of life. Clearly, social networks, at their best, improve physical health and are probably the biggest contributor to positive mental health.
3.1.2. Interventions to improve behavior are positive networks in action
Interventions to improve health behavior by altering appraisal strategies are common. Stressful life events may be inevitable, but how one perceives and interprets these events can greatly influence the magnitude of harm imparted upon one’s health (Hagger et al., 2017; Leventhal, Leventhal, & Contrada, 1998). Cognitive distortions, such as rumination, magnification and catastrophizing can cause additional stress beyond the initial stressor, contributing to prolonged, chronic stress (Zola, 1973), which can contribute to chronic disease (Fig. 2). Thus, coping interventions (e.g., cognitive behavioral therapy, mindfulness-based interventions, goal setting) emphasize strategies such as emotion regulation, impulse control and cognitive restructuring to improve mental health and health behavior (e.g., Giles-Corti & Donovan, 2002; Barker, 2014; Britton et al., 2012; Loucks et al., 2015; Ferguson, Bender, & Thompson, 2015; Folkman & Lazarus, 1988). New research is beginning to determine the components of behavior change interventions in order to identify critical regulatory mechanisms that underlie improved coping skills for stress reduction. For example, a recent dismantling trial identified acceptance as a critical component of mindfulness training, in which acceptance is an attitude of receptivity and equanimity toward all momentary experiences that allows even stressful stimuli to pass without reactivity (Lindsay et al., 2017).
Most health psychology interventions focus closely on self-regulation of emotions, cognitions, and behaviors (e.g., Barker, 2014; Felton, Revenson, & Hinrichsen, 1984; Folkman & Lazarus, 1988). In so doing, interventionists network with target individuals to promote health in person, or more recently, through technology and social media (Head, Noar, Iannarino, & Harrington, 2013; Johnson et al., 2010). This strategy attempts to educate, provide needed skills, or to enhance motivation to act in a healthy fashion. Behavior change theories provide frameworks for evaluating interventions and identifying target mechanisms that produce desired outcomes (e.g., Fisher & Fisher, 1992; Gardner et al., 2010). A behavior change technique taxonomy provides researchers with a reliable method for identifying the key “active ingredients” of a behavior change intervention (e.g., prompts/cues, social support, and feedback) (Michie et al., 2013). Certain behavior change techniques, such as goal setting and self-monitoring, appear particularly useful in promoting the development of healthy behaviors, while factors related to internal motivation and autonomy appear more critical for maintaining those efforts (Kwasnicka et al., 2016; Samdal et al., 2017). Nonetheless, health behavior change and maintenance do not happen in a vacuum; social networks are critical. Interventions that accommodate social contagion will spread behavior change more effectively (Aral & Nicolaides, 2017). Loneliness and high conflict relationships undermine health, and strong positive close relationships offer protective factors to both the mind and body. Close relationships help keep us happy and healthy, but they are not a quick fix: relationships take time and effort to establish and maintain. Although much research has highlighted the importance of close personal relationships to improve physical and mental health, the challenge remains to translate such knowledge into interventions to improve social relationships (Dunkel Schetter, 2017).
3.1.3. Patient-provider interactions as social networks
Medical and other health providers must interact with patients for routine care and in the case of illness and other maladies. Since the 1970s, medical practice has moved toward a patient-centered approach such that patients are no longer passive recipients of health instructions but in fact “have expectations of the doctor, evaluate the doctor’s actions, and are able to make their own treatment decisions” (Stimson 1974, p. 97; see also Mead & Bower, 2000). Indeed, part of the placebo response to medical treatments may stem from the patient’s beliefs and expectations about the provider (Bishop et al., 2012; Noble, Douglas, & Newman, 2001). Interestingly, Hall and Dornam’s (1988) meta-analysis on patient satisfaction surveys found that patients considered the overall quality, humaneness, and competence of the provider to be of higher importance than actual health outcomes. How and when doctors choose to impart critical medical information can influence a patient’s ability to comprehend and recall such information (e.g., providing instructions while under the duress of impending test results may not be ideal; Portnoy, 2010). Effective communication strategies may be even more important when the patients are members of vulnerable populations (e.g., low SES patients, children). In their systematic review, Kodjebacheva, Sabo, and Xiong (2016) found that medical communications with children improved when providers undertook role-playing and seminars, when parents read booklets or attended discussions, and when children watched videos showing how to communicate with physicians. Together, these studies illustrate just some of the reasons why patient-provider interactions are an important component of the healthcare network.
Another issue related to patient-provider interactions is the need to adhere to medical regimens that the provider prescribes, because adherence is a primary determinant of treatment success. The WHO found that only 50% of patients who suffer from chronic diseases adhere to treatment recommendations (Sabate, 2003). Consequences of poor adherence include both health and economic implications; thus, the issue of compliance is a major focus of health change research. Since the 1980s, medical regimen adherence has been viewed more as an issue of self-regulation, albeit triggered by a visit with a provider, rather than of compliance based on the doctor-patient relationship (Conrad, 1985); that is, even if patients have a strong positive relationship with their doctor (and finances are not the issue), they may still have trouble adhering. Not surprisingly, interventions to improve medical regimen adherence succeed better when they incorporate more social support (de Bruin et al., 2010). Thus, some part of medical compliance stems from others’ influence, the network regulation of health behavior.
3.2. Connections of Health Psychological Processes Mediate Upstream and Downstream Forces
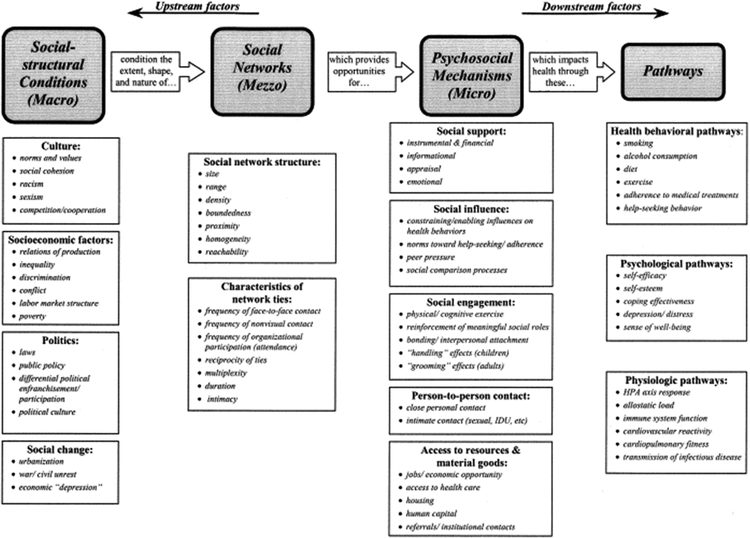
Our discourse highlights the fact that networks are crucial for individual health. Berkman and colleagues (2000) posited that factors at a broader, upstream level cascade into lower levels downstream using processes and structures such as Fig. 3 lists. Thus, cultural, socioeconomic, political, and social change factors influence social networks, which in turn affect individual outcomes. This and other ecological models emphasize that, without congenial upstream factors, it is difficult to reduce health burdens at the individual level. Accordingly, for example, neighborhood factors such as perceived safety, sidewalks, and proximity to recreational facilities have some influence on physical activity levels (Carver et al., 2010); similarly, a supportive physical environment is necessary to enhance recreational physical activity, but not sufficient to induce behavior (Giles-Corti & Donovan, 2002). In the U.S. and many developed nations, income inequality has increased in recent decades, which marks an environment that selectively disadvantages some over others and worsens health (Pickett & Wilkinson, 2015). Thus, reducing income inequality is increasingly a good way to improve public health, because it improves the ecology for all concerned. Note that the material we have covered in this article is congenial to both upstream and downstream factors that Bergman and colleagues identified: Health psychology mechanisms would seem to be central to public health.
Fig. 3.
A conceptual model of how social networks impact health (from Berkman et al., 2000).
4. Trends in Health Psychology Research
Although health psychologists have published their work in a wide variety of outlets, many have appeared in the journal in which this article appears, Social Science & Medicine (SSM), which Pergamon Press established in 1967 (in 1991, Elsevier Limited acquired Pergamon Press). Thus, this article and others celebrate SSM’s golden jubilee; in this article, we cited classic sources, many of which appeared in SSM (for methods, see Appendix A in the online supplement). From its onset, SSM featured articles from the then-fashionable term medical psychology and it has maintained a health psychology office for decades. In the past 50 years, SSM has published over 18,000 articles, with a substantial subset focusing on health psychology.
4.1. Trends in topics.
As Figure 4 shows, prominent articles published in the 1970s tended to focus more on doctor-patient relationships/satisfaction, stress, coping, and cardiovascular health, whereas articles since 2010 have focused more on health or mortality, obesity, mental illness/health, and socioeconomic factors impacting health, illustrating a shift towards a more proactive approach by looking at behavior change and programs that attempt to improve practices for better health. Yet, such illustrations cannot capture all recent advances, such as the crucial importance of sufficient sleep for health (e.g., Exelmans & Van den Bulck, 2016). Trends in health psychology often reflect current disease epidemics, especially when funding is allocated to address the issue. For example, the HIV/AIDS epidemic that began in the 1980s led to a flow of funding that allowed researchers to work across national boundaries, focusing efforts on behavior change research evaluating prevention programs and strategies to improve care for those living with or affected by HIV/AIDS (e.g., Parker & Aggleton, 2003). Knowledge gained from HIV/AIDS interventions is now being translated to additional health domains. Similarly, research follows the impact of world events, such as the mental health of refugees arriving from war-torn countries (e.g., Miller & Rasmussen, 2010). Topics in health psychology also address policy ramifications, which can be powerful motivators of behavior change. For example, Noar et al.’s (2016) meta-analysis documented that strengthened cigarette pack warnings increased knowledge, quit line calls, and quit attempts, and ultimately were associated with decreased smoking consumption and prevalence.
Fig. 4.
Primary subjects of prominent articles published in Social Science & Medicine during the 1970s (left) and between 2010 and 2016 (right), sized according to frequency of appearance. Appendix C in the online supplement offers additional such word cloud figures.
Health disparities have always been an important research agenda for social science, and health psychology in particular; health disparities are known to persist even after controlling for access-related factors (Bastos et al., 2010). Racial disparities exist in terms of how physicians perceive and act with patients, and vice versa (Sussman et al., 1987; Van Ryn & Burke, 2000). Such discrimination can directly impact treatments or treatment-seeking behavior. For example, Burgess et al. (2008) showed experimentally that doctors use racial stereotyping when prescribing opioids to manage pain, employing different decision-making strategies for Whites and Blacks. Rising awareness of extremes of wealth and prevalence of poverty ought to pressure society’s leaders to address health inequalities. As noted, in the U.S. and many developed nations, income inequality has increased in recent decades, which marks an environment that selectively disadvantages some over others and worsens health (Pickett & Wilkinson, 2015). Thus, reducing income inequality is logically a way to improve public health.
4.2. Societal and Technological Trends.
Culture and social networks shape habits and behavior in almost an unconscious level, having a strong impact on how we cope with stress and handle anxiety (Bourdieau, 1984; Zola, 1973). Fewer people are involved in organized religion, which traditionally helped facilitate a sense of community and connection with a meaningful set of values. A contemporary rise in spirituality may be an attempt to fill this void, as people seek to find meaning in their lives (e.g., WHOQoL SRPB Group, 2006). Importantly, educational systems are working to bring healthy meals and mind-body programs into the classroom to improve student attention and behavior; corporations are investing in lifestyle programs for employees to increase productivity and reduce healthcare costs; law enforcement personnel are receiving training to reduce implicit bias and discrimination to improve relationships between police officers and community members.
Technology continues to change society rapidly, altering many facets of daily life and as an extension, people’s health. With these changes come both new opportunities and new problems, and new problems require novel solutions. Health-related benefits of an ever-more-wired era include online support groups, easily accessible apps to help people deal with problems like addiction, and an array of fitness trackers, app monitors, and feedback tools that empower people to take control over their own personal health. Technology is also transforming the doctor-patient relationship in positive ways, through improved communication, increased monitoring capabilities, and more personalized care. Of course there are also many concerns associated with the rise in use of technology, such as reduced face-to-face interactions with physicians due to the push towards telemedicine, which could potentially impair quality of interaction and subsequent compliance. Examples of other concerns include increased screen time in youth contributing to childhood obesity, diminished social skills, depression, or issues with attention and impulse control in a society surrounded by instant gratification (e.g., Liu et al., 2015; Exelmans & Van den Bulck, 2016; Head et al., 2013). It is not yet known whether social media addiction (e.g., obsessive monitoring of ‘likes’ on Instagram) will translate into increased health issues and risk behaviors, but research does suggest that repetitive stimulation of dopaminergic reward systems can prime addiction pathways, especially during development (Kim et al., 2017). Recent studies investigate new internet-related issues that arise, such as the prevalence of biased online reviews of medical treatment outcomes (de Barra, 2017), which can lead to consumers/patients basing treatment decisions on evidence-based hearsay rather than principles of evidence-based medicine (Ioannidis, 2017).
4.3. Research Trends and Scientific Advancements.
Similar to trends found in related fields, health psychology increasingly investigates causal pathways. While earlier work focused on identifying and exploring what mental, behavioral, environmental, and cultural factors influence health and illness, as we documented in section 2.3, more recent investigations work to identify how these factors influence health. Exemplifying this trend in depression, early studies focused on identifying groups vulnerable to depression, and investigated ethnic differences in care seeking behavior (Sussman et al., 1987). More recent studies address how environmental factors contribute to depression. For example, studies ask: Does neighborhood crime influence depressive symptoms via epigenetic alterations (Lei et al., 2015)? And, what is the directional link between inflammation and depression (Das, 2016)? These studies illustrate a larger biodemographic trend that relies on interdisciplinary strategies, often combining “big data” (e.g., spatially linking large public datasets) with advanced biomarker technology to address challenging health-related issues.
As collaborations across fields seek to provide novel insight into complex health issues that are often beyond any single scientist’s area of expertise, it becomes essential to proceed with care; social scientists must appreciate the rigor required and honor the limitations of biological measurements, and basic scientists must appreciate the challenges involved in working with uncontrolled samples outside of the laboratory setting (Johnson & Michie, 2015; Kaufman et al., 2014). Choosing appropriate study designs is critical, especially when using biomarkers such as cortisol or alpha-amylase that have naturally occurring diurnal variations (Skoluda et al., 2017). As we noted, new biomarkers for stress and inflammation are emerging and more commonly used, especially as less invasive methods of collection become available. Rather than having to obtain blood or urine samples, several markers can now be analyzed via saliva, and hair samples may even be used to examine temporal change in chronic stress gauged through cortisol levels (Pacella et al., 2017).
In the future, emerging scientific advances including those derived from animal studies will likely spur the field of health psychology to address novel questions related to health, stress, and disease. As an illustration, animal studies on the microbiota-gut-brain axis have shown that stress changes the internal environment of the intestinal tract to make it less habitable for the ‘good’ bacteria, increasing levels of the ‘bad’ bacteria. Changes in the microbiome can affect signaling in the brain, alter mood regulation, increase pain sensitivity and may even be related to increased risk of disease (e.g., vascular issues that can lead to stroke or cognitive decline) (Tang et al., 2017). Scientific advances in understanding the influence of gut microbiota on emotion, cognition and behavior may propel social scientists to ask new questions about the associations between nutrition and stress, mental health and disease. This interdisciplinary research is essential to tackling maternal depression and developmental consequences of child malnutrition worldwide.
Advances in neuroscience demonstrate that while environmental stressors can create lasting impairments in behavior and brain functioning through neuroplasticity, these effects can also be reversible through persistent re-patterning (Liston et al, 2009). Such findings lend important implications for stress reduction strategies and learned coping skills to mitigate the sequelae of chronic stress (e.g., improve cognitive function and behavior). New forms of cognitive behavioral therapy based on mindfulness, compassion, gratitude, and acceptance (Kahl et al., 2012; Otto et al., 2016) are examples of mind-body interventions geared towards empowering individuals to take greater control over their own thoughts, emotions, behaviors and habits. Fortunately, neuroplasticity exists even late in life (Ellwardt, Van Tilburg, & Aartsen, 2015; Boyke et al., 2008), potentiating positive health behavior change and maintenance. Similarly, rejecting negative stereotypes about aging is associated with more successful aging (Levy, Pilver, & Pietrzak, 2014).
5. Conclusion: The Secret to Successful Living
To reduce the immense burden of chronic disease, health behavior change is necessary at the population level. Positive social networks along with efforts to improve self-regulation are critical to establishing and maintaining healthy attitudes and behavior. Public policy to address income inequality will help alleviate health disparities, but similar to the underlying biological mechanisms of stress, issues surrounding inequality are highly complex and often bidirectional. A wide opportunity for intervention lies in improving coping strategies and stress reactions, such as resilience training to reduce additional suffering that often goes beyond the initial stressor.
Although not commonly stated as such, the lessons of health psychology research offer an answer to the secret to successful living: Maintain a sense of purpose, positive social relationships and healthy habits, including a healthy diet, sufficient exercise and sleep; moderation and optimism are best. Not only is this a recipe for successful living, but successful aging, as well. The caveat is that many factors can interfere with these lessons, and unless social networks are supportive, health will be compromised. Although many factors may remain out of an individual’s control (Figs. 2 and 3), behavior change strategies can empower individuals and populations to improve health, longevity, and quality of life. In the end, the ultimate lesson of health psychology is that good health hinges on taking a comprehensive approach that optimizes biological, psychological, social, and environmental (natural and built) forces. Future research that uses increasingly rigorous and interdisciplinary perspectives will elaborate the mechanisms involved and ensure that, in years to come, health psychology will continue to play an essential role in understanding the keys to a long, happy, productive life.
Supplementary Material
Highlights.
Health psychology’s biopsychosocial model of illness improves on the biomedical model.
Without positive coping strategies, stress can result in harmful biological cascades.
Behavior change is a key target to help improve lifestyles and reduce chronic illnesses.
Understanding and controlling factors upstream from individuals can improve health.
Heathy habits along with supportive environments enable successful living and aging.
Acknowledgments
We thank Frances Aboud, Chris Dunkel Schetter, Emily Alden Hennessy, Benjamin X. White, and Richard Wolferz, Jr. for their very helpful comments on a prior draft of this article; and, we thank Emma Atkinson for her assistance in organizing citations relevant to this article.
The preparation of this article was supported in part by a subcontract from U.S. Public Health Service grant 5U24AG052175.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acabchuk RL, Kamath J, Salamone JD, & Johnson BT (2017). Stress and chronic illness: The inflammatory pathway. Social Science & Medicine, 185, 158–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler RH (2009). Engel’s biopsychosocial model is still relevant today. Journal of Psychosomatic Research, 67(6), 607–611. [DOI] [PubMed] [Google Scholar]
- Albrecht GL, & Devlieger PJ (1999). The disability paradox: High quality of life against all odds. Social Science & Medicine, 48(8), 977–988. [DOI] [PubMed] [Google Scholar]
- Antonovsky A (1993). The structure and properties of the sense of coherence scale. Social Science & Medicine, 36(6), 725–733. [DOI] [PubMed] [Google Scholar]
- Aral S, & Nicolaides C (2017). Exercise contagion in a global social network. Nature Communications, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker KK (2014). Mindfulness meditation: Do-it-yourself medicalization of every moment. Social Science & Medicine, 106, 168–176. [DOI] [PubMed] [Google Scholar]
- Bastos JL, Celeste RK, Faerstein E, & Barros AJ (2010). Racial discrimination and health: A systematic review of scales with a focus on their psychometric properties. Social Science & Medicine, 70(7), 1091–1099. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. [DOI] [PubMed] [Google Scholar]
- Berkman LF, & Syme SL (1979). Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology, 109(2), 186–204. [DOI] [PubMed] [Google Scholar]
- Bishop FL, Jacobson EE, Shaw JR, & Kaptchuk TJ (2012). Scientific tools, fake treatments, or triggers for psychological healing: How clinical trial participants conceptualise placebos. Social Science & Medicine, 74(5), 767–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair IV, & Brondolo E (2017). Moving beyond the individual: Community-level prejudice and health. Social Science & Medicine, 183, 169–172. [DOI] [PubMed] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20–28. [DOI] [PubMed] [Google Scholar]
- Borgonovi F (2008). Doing well by doing good: The relationship between formal volunteering and self-reported health and happiness. Social Science & Medicine, 66(11), 2321–2334. [DOI] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, & Bennett DA (2010). Purpose in life is associated with a reduced risk of incident disability among community-dwelling older persons. The American Journal of Geriatric Psychiatry, 18(12), 1093–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdieu P (1984). Distinction: A social critique of the judgement of taste. Harvard University Press. [Google Scholar]
- Boyke J, Driemeyer J, Gaser C, Büchel C, & May A (2008). Training-induced brain structure changes in the elderly. Journal of Neuroscience, 28, 7031–7035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Crowley-Matoka M, Phelan S, Dovidio JF, Kerns R, Roth C, … & van Ryn M (2008). Patient race and physicians’ decisions to prescribe opioids for chronic low back pain. Social Science & Medicine, 67(11), 1852–1860. [DOI] [PubMed] [Google Scholar]
- Carver A, Timperio A, Hesketh K, & Crawford D (2010). Are children and adolescents less active if parents restrict their physical activity and active transport due to perceived risk? Social Science & Medicine, 70(11), 1799–1805. [DOI] [PubMed] [Google Scholar]
- Chan M (2016) Obesity and diabetes: The slow-motion disaster Keynote address at the 47th meeting of the National Academy of Medicine, World Health Organization. Accessed on 3 Oct 2017 http://www.who.int/dg/speeches/2016/obesity-diabetes-disaster/en/ [Google Scholar]
- Christensen P (2004). The health-promoting family: a conceptual framework for future research. Social Science & Medicine, 59(2), 377–387. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM (1997). Social ties and susceptibility to the common cold. JAMA, 277(24), 1940–1944. [PubMed] [Google Scholar]
- Conrad P (1985). The meaning of medications: Another look at compliance. Social Science & Medicine, 20(1), 29–37. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM (1997). Social ties and susceptibility to the common cold. JAMA, 277(24), 1940–1944. [PubMed] [Google Scholar]
- Das A (2016). Psychosocial distress and inflammation: Which way does causality flow? Social Science & Medicine, 170, 1–8. [DOI] [PubMed] [Google Scholar]
- de Barra M (2017). Reporting bias inflates the reputation of medical treatments: A comparison of outcomes in clinical trials and online product reviews. Social Science & Medicine, 177, 248–255. [DOI] [PubMed] [Google Scholar]
- de Bruin M, Viechtbauer W, Schaalma HP, Kok G, Abraham C, & Hospers HJ (2010). Standard care impact on effects of highly active antiretroviral therapy adherence interventions: A meta-analysis of randomized controlled trials. Archives of Internal Medicine, 170(3), 240–250. [DOI] [PubMed] [Google Scholar]
- de Jonge J, Bosma H, Peter R, & Siegrist J (2000). Job strain, effort-reward imbalance and employee well-being: A large-scale cross-sectional study. Social Science & Medicine, 50(9), 1317–1327. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C (2017). Moving research on health and close relationships forward—a challenge and an obligation: Introduction to the special issue. American Psychologist, 72(6), 511–516. doi: 10.1037/amp0000158 [DOI] [PubMed] [Google Scholar]
- Egger GJ, Binns AF, & Rossner SR (2009). The emergence of “lifestyle medicine” as a structured approach for management of chronic disease. Medical Journal of Australia, 190(3), 143–145. [DOI] [PubMed] [Google Scholar]
- Ellwardt L, Van Tilburg TG, & Aartsen MJ (2015). The mix matters: Complex personal networks relate to higher cognitive functioning in old age. Social Science & Medicine, 125, 107–115. [DOI] [PubMed] [Google Scholar]
- Engel GL (1977). The need of a new medical model: A challenge for biomedicine. Science, 196, 129–136. [DOI] [PubMed] [Google Scholar]
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, & Sallis JF (1999). Physical activity social support and middle-and older-aged minority women: results from a US survey. Social Science & Medicine, 49(6), 781–789. [DOI] [PubMed] [Google Scholar]
- Exelmans L, & Van den Bulck J (2016). Bedtime mobile phone use and sleep in adults. Social Science & Medicine, 148, 93–101. [DOI] [PubMed] [Google Scholar]
- Felton BJ, Revenson TA, & Hinrichsen GA (1984). Stress and coping in the explanation of psychological adjustment among chronically ill adults. Social Science & Medicine, 18(10), 889–898. [DOI] [PubMed] [Google Scholar]
- Ferguson KM, Bender K, & Thompson SJ (2015). Gender, coping strategies, homelessness stressors, and income generation among homeless young adults in three cities. Social Science & Medicine, 135, 47–55. [DOI] [PubMed] [Google Scholar]
- Fisher JD, & Fisher WA (1992). Changing AIDS risk behavior. Psychological Bulletin, 111, 455–474. [DOI] [PubMed] [Google Scholar]
- Folkman S (1997). Positive psychological states and coping with severe stress. Social Science & Medicine, 45(8), 1207–1221. [DOI] [PubMed] [Google Scholar]
- Folkman S, & Lazarus RS (1988). The relationship between coping and emotion: Implications for theory and research. Social Science & Medicine, 26(3), 309–317. [DOI] [PubMed] [Google Scholar]
- Gardner B, Whittington C, McAteer J, Eccles MP, & Michie S (2010). Using theory to synthesise evidence from behaviour change interventions: The example of audit and feedback. Social Science & Medicine, 70(10), 1618–1625. [DOI] [PubMed] [Google Scholar]
- Giles-Corti B, & Donovan RJ (2002). The relative influence of individual, social and physical environment determinants of physical activity. Social Science & Medicine, 54(12), 1793–1812. [DOI] [PubMed] [Google Scholar]
- Glass TA, & McAtee MJ (2006). Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine, 62(7), 1650–1671. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Koch S, Chatzisarantis NL, & Orbell S (2017). The Common Sense Model of Self-Regulation: Meta-analysis and test of a process model. Psychological Bulletin, 143(11), 1117–1154. [DOI] [PubMed] [Google Scholar]
- Hall JA, & Dornan MC (1988). What patients like about their medical care and how often they are asked: A meta-analysis of the satisfaction literature. Social Science & Medicine, 27(9), 935–939. [DOI] [PubMed] [Google Scholar]
- Hankivsky O (2012). Women’s health, men’s health, and gender and health: Implications of intersectionality. Social Science & Medicine, 74(11), 1712–1720. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, & Fiscella K (2014). Structural stigma and all-cause mortality in sexual minority populations. Social Science & Medicine, 103, 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head KJ, Noar SM, Iannarino NT, & Harrington NG (2013). Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Social Science & Medicine, 97, 41–48. [DOI] [PubMed] [Google Scholar]
- Ioannidis JPA (2017). Does evidence-based hearsay determine the use of medical treatments? Social Science & Medicine, 177, 256–258. [DOI] [PubMed] [Google Scholar]
- Johnson BT, & Michie S (2015). Towards healthy theorising about health behaviouACrs in the maze of messy reality: A reaction to Peters, de Bruin, and Crutzen. Health Psychology Review, 9(1), 21–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge B, Sheeran P, …& Carey MP (2010). A network-individual-resource model for HIV prevention. AIDS and Behavior, 14(2), 204–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahl KG, Winter L, & Schweiger U (2012). The third wave of cognitive behavioural therapies: What is new and what is effective? Current Opinion in Psychiatry, 25(6), 522–528. [DOI] [PubMed] [Google Scholar]
- Kaufman MR, Cornish F, Zimmerman RS, & Johnson BT (2014). Health behavior change models for HIV prevention and AIDS care: Practical recommendations for a multi-level approach. JAIDS Journal of Acquired Immune Deficiency Syndromes, 66, S250–S258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, & Subramanian SV (2017). Social epidemiology for the 21st century. Social Science & Medicine. [DOI] [PubMed] [Google Scholar]
- Kendall E, Catalano T, Kuipers P, Posner N, Buys N, & Charker J (2007). Recovery following stroke: The role of self-management education. Social Science & Medicine, 64(3), 735–746. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Lee JH, Yun K, & Kim JH (2017). Alterations in Striatal Circuits Underlying Addiction-Like Behaviors. Molecules and cells, 40(6), 379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodjebacheva GD, Sabo T, & Xiong J (2016). Interventions to improve child-parent-medical provider communication: A systematic review. Social Science & Medicine, 166, 120–127. [DOI] [PubMed] [Google Scholar]
- Kwasnicka D, Dombrowski SU, White M, & Sniehotta F (2016). Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychology Review, 10(3), 277–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei MK, Beach SR, Simons RL, & Philibert RA (2015). Neighborhood crime and depressive symptoms among African American women: Genetic moderation and epigenetic mediation of effects. Social Science & Medicine, 146, 120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy BR, Pilver CE, & Pietrzak RH (2014). Lower prevalence of psychiatric conditions when negative age stereotypes are resisted. Social Science & Medicine, 119, 170–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitner JB, Hehman E, Ayduk O, & Mendoza-Denton R (2016). Racial bias is associated with ingroup death rate for Blacks and Whites: Insights from Project Implicit. Social Science & Medicine, 170, 220–227. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Leventhal EA, & Contrada RJ (1998). Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychology and Health, 13(4), 717–733. [Google Scholar]
- Lewis FM, Woods NF, Hough EE, & Bensley LS (1989). The family’s functioning with chronic illness in the mother: The spouse’s perspective. Social Science & Medicine, 29, 1261–1269. [DOI] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: An interdependence and communal coping approach. Social Science & Medicine, 62(6), 1369–1380. [DOI] [PubMed] [Google Scholar]
- Li X, Harrison SE, Fairchild AJ, Chi P, Zhao J, & Zhao G (2017). A randomized controlled trial of a resilience-based intervention on psychosocial well-being of children affected by HIV/AIDS: Effects at 6-and 12-month follow-up. Social Science & Medicine, 190, 256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Smyth JM, Brown KW, & Creswell JD (2017). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlledtrial. Psychoneuroendocrinology. [DOI] [PubMed] [Google Scholar]
- Livingston JD, & Boyd JE (2010). Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine, 71(12), 2150–2161. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, & Fulwiler C (2015). Mindfulness and cardiovascular disease risk: State of the evidence, plausible mechanisms, and theoretical framework. Current Cardiology Reports, 17(12), 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot MG, Stansfeld S, Patel C, North F, Head J, White I, …& Smith GD (1991). Health inequalities among British civil servants: The Whitehall II study. The Lancet, 337(8754), 1387–1393. [DOI] [PubMed] [Google Scholar]
- Marrouch N, & Johnson BT (in press). Geocoding: Using space to enhance social psychological research In Blanton H & Webster GD (Eds.), Social psychological assessment. New York: Psychology Press. [Google Scholar]
- McGinty EE, Goldman HH, Pescosolido B, & Barry CL (2015). Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Social Science & Medicine, 126, 73–85. [DOI] [PubMed] [Google Scholar]
- Mead N, & Bower P (2000). Patient-centredness: A conceptual framework and review of the empirical literature. Social Science & Medicine, 51(7), 1087–1110. [DOI] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, …& Wood CE (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. [DOI] [PubMed] [Google Scholar]
- Miller KE, & Rasmussen A (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine, 70(1), 7–16. [DOI] [PubMed] [Google Scholar]
- Mineo L (2017). Good genes are nice, but joy is better. Harvard Gazette https://news.harvard.edu/gazette/story/2017/04/over-nearly-80-years-harvard-study-has-been-showing-how-to-live-a-healthy-and-happy-life accessed 27 October 2017.
- Morrisette-Thomas V, Cohen AA, Fülöp T, Riesco É, Legault V, Li Q, … & Ferrucci L (2014). Inflamm-aging does not simply reflect increases in pro-inflammatory markers. Mechanisms of Ageing and Development, 139, 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, & Brewer NT (2016). The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. Social Science & Medicine, 164, 118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble LM, Douglas BC, & Newman SP (2001). What do patients expect of psychiatric services? A systematic and critical review of empirical studies. Social Science & Medicine, 52(7), 985–998. [DOI] [PubMed] [Google Scholar]
- Neuling SJ, & Winefield HR (1988). Social support and recovery after surgery for breast cancer: frequency and correlates of supportive behaviours by family, friends and surgeon. Social Science & Medicine, 27(4), 385–392. [DOI] [PubMed] [Google Scholar]
- Oberle E, & Schonert-Reichl KA (2016). Stress contagion in the classroom? The link between classroom teacher burnout and morning cortisol in elementary school students. Social Science & Medicine, 159, 30–37. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Fryar CD, & Flegal KM (2015). Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS data brief, no 219. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- Ogden J (1995). Psychosocial theory and the creation of the risky self. Social Science & Medicine, 40(3), 409–415. [DOI] [PubMed] [Google Scholar]
- Okada H, Kuhn C, Feillet H, & Bach JF (2010). The ‘hygiene hypothesis’ for autoimmune and allergic diseases: An update. Clinical & Experimental Immunology, 160(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orchard J, & Price J (2017). County-level racial prejudice and the black-white gap in infant health outcomes. Social Science & Medicine, 181, 191–198. [DOI] [PubMed] [Google Scholar]
- Otto AK, Szczesny EC, Soriano EC, Laurenceau JP, & Siegel SD (2016). Effects of a randomized gratitude intervention on death-related fear of recurrence in breast cancer survivors. Health Psychology, 35(12), 1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, Steudte-Schmiedgen S, George RL, & Delahanty DL (2017). The utility of hair cortisol concentrations in the prediction of PTSD symptoms following traumatic physical injury. Social Science & Medicine, 175, 228–234. [DOI] [PubMed] [Google Scholar]
- Palmer AB (1970). Some variables contributing to the onset of cigarette smoking among junior high school students. Social Science & Medicine, 4, 359–366. [DOI] [PubMed] [Google Scholar]
- Parker R, & Aggleton P (2003). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57(1), 13–24. [DOI] [PubMed] [Google Scholar]
- Pickett KE, & Wilkinson RG (2015). Income inequality and health: a causal review. Social Science & Medicine, 128, 316–326. [DOI] [PubMed] [Google Scholar]
- Portnoy DB (2010). Waiting is the hardest part: Anticipating medical test results affects processing and recall of important information. Social Science & Medicine, 71(2), 421–428. [DOI] [PubMed] [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, & Johnson BT (2014). HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine, 103, 118–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: family social environments and the mental and physical health of offspring. Psychological bulletin, 128(2), 330. [PubMed] [Google Scholar]
- Riis JL, Granger DA, Minkovitz CS, Bandeen-Roche K, DiPietro JA, & Johnson SB (2016). Maternal distress and child neuroendocrine and immune regulation. Social Science & Medicine, 151, 206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabate E (2003). Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization. [Google Scholar]
- Samdal GB, Eide GE, Barth T, Williams G, & Meland E (2017). Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults: Systematic review and meta-regression analyses. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnorpfeil P, Noll A, Schulze R, Ehlert U, Frey K, & Fischer JE (2003). Allostatic load and work conditions. Social Science & Medicine, 57(4), 647–656. [DOI] [PubMed] [Google Scholar]
- Schwartz GE& Weiss SM (1978). Behavioral medicine revisited: An amended definition. Journal of Behavioral Medicine, 1, 249–251. [DOI] [PubMed] [Google Scholar]
- Schwartz JA (2017). Long-term physical health consequences of perceived inequality: Results from a twin comparison design. Social Science & Medicine, 187, 184–192. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, & Peter R (2004). The measurement of effort–reward imbalance at work: European comparisons. Social Science & Medicine, 58(8), 1483–1499. [DOI] [PubMed] [Google Scholar]
- Simons RL, Lei MK, Beach SR, Barr AB, Cutrona CE, Gibbons FX, & Philibert RA (2017). An index of the ratio of inflammatory to antiviral cell types mediates the effects of social adversity and age on chronic illness. Social Science & Medicine, 185, 166–170. [DOI] [PubMed] [Google Scholar]
- Skoluda N, La Marca R, Gollwitzer M, Müller A, Limm H, Marten-Mittag B, …& Nater UM (2017). Long-term stability of diurnal salivary cortisol and alpha-amylase secretion patterns. Physiology & Behavior, 175, 1–8. [DOI] [PubMed] [Google Scholar]
- Solís CB, Fantin R, Castagné R, Lang T, Delpierre C, & Kelly-Irving M (2016). Mediating pathways between parental socio-economic position and allostatic load in mid-life: Findings from the 1958 British birth cohort. Social Science & Medicine, 165, 19–27. [DOI] [PubMed] [Google Scholar]
- Stimson GV (1974). Obeying doctor’s orders: A view from the other side. Social Science & Medicine, 8, 97–104. [DOI] [PubMed] [Google Scholar]
- Sussman LK, Robins LN, & Earls F (1987). Treatment-seeking for depression by black and white Americans. Social Science & Medicine, 24(3), 187–196. [DOI] [PubMed] [Google Scholar]
- Tang AT, Choi JP, Kotzin JJ, Yang Y, Hong CC, Hobson N, …& Cao Y (2017). Endothelial TLR4 and the microbiome drive cerebral cavernous malformations. Nature, 545(7654), 305–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd MA, Shkolnikov VM, & Goldman N (2016). Why are well-educated Muscovites more likely to survive? Understanding the biological pathways. Social Science & Medicine, 157, 138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine, 34(8), 907–917. [DOI] [PubMed] [Google Scholar]
- Van Ryn M, & Burke J (2000). The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine, 50(6), 813–828. [DOI] [PubMed] [Google Scholar]
- Vinje HF, Ausland LH, & Langeland E (2017). The application of salutogenesis in the training of health professionals In The Handbook of Salutogenesis (pp.307–318). Springer International Publishing. [PubMed] [Google Scholar]
- Wade DT, & Halligan PW (2004). Do biomedical models of illness make for good healthcare systems? BMJ: British Medical Journal, 329(7479), 1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldinger RJ, & Schulz MS (2016). The long reach of nurturing family environments: links with midlife emotion-regulatory styles and late-life security in intimate relationships. Psychological Science, 27(11), 1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2015, 19 January). WHO news release: Noncommunicable diseases prematurely take 16million lives annually, WHO urges more action.http://www.who.Int/mediacentre/news/releases/2015/noncommunicable-diseases/en/
- WHO (1946). Preamble to the Constitution of WHO as adopted by the International Health Conference, New York, 19 June - 22 July 1946. [Google Scholar]
- WHOQoL SRPB Group. (2006). A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Social Science & Medicine, 62(6), 1486–1497 [DOI] [PubMed] [Google Scholar]
- Williams B (1994). Patient satisfaction: A valid concept? Social Science & Medicine, 38(4), 509–516. [DOI] [PubMed] [Google Scholar]
- Zola IK (1973). Pathways to the doctor—from person to patient. Social Science & Medicine, 7(9), 677–689. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.