Abstract
Healthy life expectancy (HALE) varies substantially among countries, regions, and race/ ethnicities. Utilizing the Sullivan method, this article examines HALE for Native Hawaiian, White, Filipino, Japanese, and Chinese Americans living in Hawai’i, the United States. HALE varies by sex and race/ethnicity. The HALE at birth in 2010 for females was 78.3, 77.8, 74.2, 73.7, and 62.6 years in contrast to life expectancy of 90, 88, 88.1, 83.4, and 79.4 for Chinese, Japanese, Filipino Americans, White, and Native Hawaiians, respectively. In the same order, HALE at birth for males was 73.0, 71.6, 72.3 70.7, and 60.7 years, compared with life expectancy of 85.3, 81.2, 80.8, 78.3, and 73.9. The gaps in HALE between Native Hawaiians and the longest living Chinese Americans were 15.7 years for females and 12.3 years for males. Our results highlight sex and racial/ethnic disparities in HALE, which can inform program and policy development.
Keywords: sex, healthy life expectancy, health disparity, life table, race/ethnicity
Introduction
Healthy life expectancy (HALE) at birth is the summary measure of a population’s health developed by the World Health Organization that captures how many years a person might live in a healthy state.1 HALE provides a more complete estimate of population health than does life expectancy (LE) because it considers years spent in disability. The global HALE in 2016 was estimated at 63.3 years, 8.7 years lower than total LE at birth.1 Global HALE at birth for females was 2.8 years greater than that for males. In comparison, female’s LE at birth was 4.4 years longer than that for males.1 The 2016 LE and HALE for the United States were 78.5 and 68.5 years, respectively, similar to that in 2010 (78.7 and 68.7 years).1
Hawai’i is the most racially and ethnically diverse state in the United States. Its population is composed of Native Hawaiians—the indigenous people of Hawai’i—and others who immigrated primarily from Asia (primarily from Japan, China, and the Philippines) from 1880 to 1930 to work on sugar and pineapple plantations. In 2010, Hawai’i had a total population of 1 360 301 composed of about 21.3% Native Hawaiian, 22.7% Whites, 16.3% Japanese American, 17.2% Filipino American, 6.8% Chinese American, and 15.7% other ethnic groups including Korean, Samoan, other Pacific Islanders, African American, mixed race, and so on.2
Hawai’i has the longest LE of all 50 states in the United States; however, disparities exist among minority ethnic groups, with Chinese Americans living a decade longer than Native Hawaiians.2 In 2010, the LE for Chinese Americans was 87.8 years compared with 84.7 years for Japanese Americans, 84.3 years for Filipino Americans, 80.6 years for White residents, and 76.6 years for Native Hawaiians.2
Residents from Hawai’i are also viewed as healthy on most indicators of morbidity and mortality, including chronic conditions (eg, coronary heart disease, cancer, stroke, and diabetes) and lifestyle risk factors (eg, smoking, diet, and physical activity), when compared with other US states.3 However, there are very notable ethnic differences. Compared with Whites, Native Hawaiians have the highest prevalence of coronary heart disease, obesity, diabetes, and certain types of cancer (ie, breast, lung, colorectal, and pancreatic).3–8 Native Hawaiians had the highest mortality rates for heart disease, cancer, and other diseases of the circulatory system. Filipinos have higher mortality rates of stroke and coronary heart disease and kidney disease.3,5–7,9 Lifestyle factors, including smoking, poor nutrition, and limited physical activity, may also affect Native Hawaiians and Filipinos in Hawai’i.10–13 Acculturation has shifted lifestyles to be more sedentary and diets that include more foods with high fat, sugar, salt, and calories.3,14
As individuals live longer, greater attention needs to be placed on the extra years of life lived in a healthy condition, rather than simply attending to LE.10 The US Centers for Disease Control and Prevention (CDC) estimated state-specific HALEs for adults aged 65 years in the United States from 2007 to 2009 by sex and race (White and Black).15 In this article, we present the 2010 HALE at birth (ie, <1 year), 1 to 4 years, 5-year intervals from 5 to 84, and 85 years and above by sex for the 5 largest ethnic groups in Hawai’i—Native Hawaiians, Whites, Chinese, Japanese, and Filipino Americans. The goal was to identify notable disparities in HALE among these sub-populations and compare them with LE disparities for 2010.2
Methods
Life tables can be constructed in 2 ways according to the age intervals. A complete life table contains data for every single year of age, but an abridged life table usually contains data by 5- or 10-year age intervals.16 There have been several published guides to calculating HALE, all of which adjust LE. The Sullivan method adjusts LE using the portion of self-reported fair/poor health status.17,18 It is the most common methodology and has been recommended by the National Center for Health Statistics at the CDC. Self-reported measures of health status has been documented to be reliable and independent predictive measures of morbidity and mortality, and are included in many general population surveys.19 Because of the small death rates and population sizes by sex and race/ethnicity in Hawai’i, we utilized 5-year intervals to estimate HALE (<1 year, 1–4 years, 5-year intervals from 5 to 84, and 85 years and above) for the 5 major ethnic populations in Hawai’i—White, Native Hawaiian, Filipino, Japanese, and Chinese Americans.16–18 The 95% confidence intervals (CIs) for HALE were also estimated for each age group.
Death Record and Population Estimates
The 2010 death record data were provided by the Hawai’i Department of Health. Race/ethnicity was family reported. Numbers of death were calculated based on the mean number over a period of 3.5 years centering on April 1, 2010. Population estimates were based on the Hawai’i Census 2010 and adjusted by ethnicity estimates from the Hawai’i Health Survey (HHS). The HHS is a random-sample telephone survey modeled after the National Health Interview Survey. The HHS ethnic categorization in Hawai’i is defined by the Hawai’i Department of Health. It is based on paternal ethnicity for multi-ethnic children, with exceptions for Whites and Native Hawaiians. If only one parent is White, the child takes the ethnicity of the non-White parent. If one parent is Native Hawaiian or part-Native Hawaiian, the child is classified as part-Native Hawaiian regardless of the other parent’s ethnicity. The HHS classification system is also used for death records.
Self-Reported Health Status Measures (HBRFSS/NSCH)
Proportions of self-reported fair/poor health status were computed using data from the Hawai’i Behavioral Risk Factor Surveillance System (HBRFSS) and National Survey of Children’s Health (NSCH), the most population representative surveys in Hawai’i.20,21 The health status was measured using the following question: “In general, how is your (or your child’s) health? Is your health excellent, very good, good, fair, or poor?” To estimate the numerator for fair/poor health for the age group 15–19 years from the HSCH (with data for children age 15–17 years) and HBRFSS (with data for adults age 18–19 years), we took the pooled proportions weighted by survey sample size.
The HBRFSS started in 1986 with results reported annually. Participants are non-institutionalized adults, aged 18 years or older, who reside in Hawai’i. The HBRFSS collects detailed ethnic data, including a breakdown of Asian and Pacific Islander populations. Since 2011, participants are randomly selected from houses with listed and unlisted landline and cellular phone numbers. A new-weighted analysis was applied in 2011 to account for the type of telephones respondents used (eg, cell phone or landline), as well as demographic characteristics (eg, education level, marital status, and home renter/owner) besides age, ethnicity, and sex.22
The NSCH started in 2003 and is a cross-sectional telephone survey that examines the physical and emotional health of children aged 0 to 17 years, along with factors that may affect a child’s well-being. The NSCH utilizes a large-scale random-digit-dial sampling frame to contact US households with at least one resident child at the time of the interview. The NSCH collects detailed ethnic data for residents in Hawai’i who identified as Native Hawaiian; however, there were no ethnic breakdowns for Asians. The NSCH is a complex survey design, with stratification by state and phone type (landline or cell phone).
We used 2 waves of the HBRFSS (2011 and 2012) and the 2011–2012 wave of NSCH for the analyses of self-reported fair/poor health. The HBRFSS response rates were 53% for the landline sample and 27.9% for the cell phone sample in 2011, and 49.1% and 35.3%, respectively, in 2012. The NSCH 2011–2012 sample’s response rates were 38.2% for the landline sample and 15.5% for the cell phone sample. The ethnic categorization schema for both the surveys were the same and based on which ethnicity the participant (HBRFSS) or family member (NSCH) most identified with.
Results
HALE Estimates Differ Across Ethnicity
Presented in Table 1 are HALE estimates and 95% CIs by ethnicity from birth (<1 years) to age 85 years and older (male and female combined). The LE estimates are also listed as comparison.2 The pattern of HALE disparities is similar to that of the LE disparities: Native Hawaiians had the shortest HALE among all ethnic groups and thus spend the greatest number of years living with fair/poor health. The greatest gap in HALE was between Native Hawaiians and Chinese American: 13.7 years, compared with the LE gap of 11.1 years.
Table 1.
Estimates of Healthy Life Expectancy (HALE) and 95% Confidence Intervals (CIs) by Ethnicity (Male and Female Combined) for Hawai’i State, USA. Life Expectancies (LE)a Are Listed for Comparison.
| Overall | Native Hawaiian | White | Filipino | Japanese | Chinese | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (Years) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) |
| <1 | 82.4 | 67.6 (67.1–68.0) | 76.6 | 62.2 (61.0–63.4) | 80.6 | 72.1 (71.5–72.7) | 84.3 | 73.3 (72.0–74.6) | 84.7 | 74.8 (73.9–75.6) | 87.8 | 75.9 (74.1–77.7) |
| 1–4 | 81.8 | 67.0 (66.6–67.4) | 76.2 | 61.7 (60.4–62.9) | 79.9 | 71.4 (70.7–72.0) | 83.8 | 72.7 (71.4–74.0) | 84.2 | 74.3 (73.4–75.1) | 87.0 | 75.1 (73.3–76.9) |
| 5–9 | 77.9 | 63.1 (62.6–63.5) | 72.3 | 57.7 (56.5–58.9) | 75.9 | 67.4 (66.8–68.0) | 79.8 | 68.9 (67.6–70.2) | 80.3 | 70.4 (69.6–71.3) | 83.0 | 71.3 (69.4–73.1) |
| 10–14 | 72.9 | 58.2 (57.7–58.6) | 67.3 | 52.7 (51.5–53.9) | 71.0 | 62.5 (61.9–63.2) | 74.8 | 63.9 (62.6–65.2) | 75.4 | 65.5 (64.7–66.4) | 78.0 | 66.3 (64.5–68.1) |
| 15–19 | 68.0 | 53.4 (53.0–53.8) | 62.3 | 48.2 (47.0–49.3) | 66.0 | 57.8 (57.2–58.3) | 69.8 | 59.2 (57.9–60.4) | 70.4 | 60.8 (60.0–61.7) | 73.0 | 61.6 (59.7–63.4) |
| 20–24 | 63.1 | 48.7 (48.2–49.1) | 57.5 | 43.5 (42.3–44.7) | 61.2 | 52.9 (52.3–53.5) | 65.0 | 54.4 (53.2–55.7) | 65.5 | 56.1 (55.2–56.9) | 68.1 | 56.7 (54.9–58.5) |
| 25–29 | 58.3 | 48.4 (48.0–48.8) | 52.8 | 38.8 (37.6–39.9) | 56.4 | 48.6 (48.0–49.1) | 60.1 | 50.1 (48.8–51.3) | 60.7 | 51.6 (50.8–52.3) | 63.1 | 52.2 (50.4–53.9) |
| 30–34 | 53.5 | 44.1 (43.7–44.5) | 48.0 | 34.6 (33.5–35.8) | 51.6 | 44.2 (43.7–44.7) | 55.3 | 45.5 (44.3–46.8) | 55.7 | 46.9 (46.1–47.6) | 58.2 | 47.8 (46.1–49.4) |
| 35–39 | 48.7 | 39.9 (39.5–40.2) | 43.3 | 30.9 (29.8–32.0) | 46.9 | 39.9 (39.4–40.4) | 50.5 | 41.5 (40.3–42.7) | 50.8 | 42.2 (41.4–42.9) | 53.3 | 43.6 (42.0–45.1) |
| 40–44 | 44.0 | 35.6 (35.3–36.0) | 38.7 | 27.2 (26.1–28.3) | 42.2 | 35.5 (35.0–36.0) | 45.7 | 37.1 (35.9–38.3) | 46.0 | 37.7 (37.0–38.4) | 48.4 | 39.1 (37.6–40.7) |
| 45–49 | 39.4 | 31.6 (31.2–31.9) | 34.2 | 23.8 (22.8–24.9) | 37.6 | 31.3 (30.9–31.8) | 41.0 | 32.9 (31.8–34.1) | 41.3 | 33.4 (32.7–34.0) | 43.5 | 34.6 (33.1–36.0) |
| 50–54 | 34.9 | 27.5 (27.2–27.8) | 29.8 | 20.6 (19.6–21.6) | 33.2 | 27.2 (26.8–27.6) | 36.4 | 28.4 (27.3–29.6) | 36.7 | 29.3 (28.6–29.9) | 38.8 | 30.4 (29.0–31.8) |
| 55–59 | 30.6 | 23.9 (23.6–24.2) | 25.8 | 17.6 (16.7–18.6) | 28.9 | 23.5 (23.1–23.9) | 31.9 | 24.4 (23.3–25.6) | 32.2 | 25.5 (24.9–26.0) | 34.1 | 26.2 (24.8–27.6) |
| 60–64 | 26.4 | 20.5 (20.2–20.8) | 21.9 | 15.5 (14.6–16.5) | 24.8 | 20.0 (19.6–20.4) | 27.6 | 21.4 (20.3–22.5) | 27.8 | 21.8 (21.3–22.4) | 29.5 | 22.3 (21.0–23.6) |
| 65–69 | 22.3 | 17.2 (16.8–17.5) | 18.3 | 12.9 (12.0–13.9) | 20.7 | 16.4 (16.0–16.9) | 23.3 | 18.2 (17.1–19.3) | 23.6 | 18.3 (17.7–18.8) | 25.0 | 18.6 (17.3–19.9) |
| 70–74 | 18.5 | 14.0 (13.7–14.3) | 15.1 | 10.9 (9.9–11.8) | 16.9 | 13.2 (12.8–13.6) | 19.3 | 15.0 (13.9–16.1) | 19.6 | 14.7(14.2–15.3) | 20.7 | 15.4 (14.2–16.7) |
| 75–79 | 15.0 | 11.2 (10.9–11.5) | 12.1 | 8.8 (7.8–9.8) | 13.4 | 10.1 (9.6–10.5) | 15.7 | 12.1 (11.0–13.2) | 15.8 | 12.1 (11.6–12.6) | 16.9 | 11.4 (10.1–12.7) |
| 80–84 | 11.9 | 8.8 (8.4–9.1) | 9.5 | 6.9 (5.8–8.0) | 10.4 | 7.4 (6.9–7.9) | 12.5 | 10.0 (8.8–11.2) | 12.4 | 9.4 (8.9–9.9) | 13.3 | 9.3 (8.1–10.6) |
| 85+ | 9.3 | 6.9 (6.6–7.3) | 7.5 | 5.2 (3.9–6.6) | 7.8 | 5.7 (5.1–6.2) | 10.1 | 8.5 (7.2–9.8) | 9.5 | 7.4 (6.9–8.0) | 10.2 | 7.2 (5.9–8.5) |
LE estimates from 2010 life tables study2.
HALE Estimates Differ by Sex
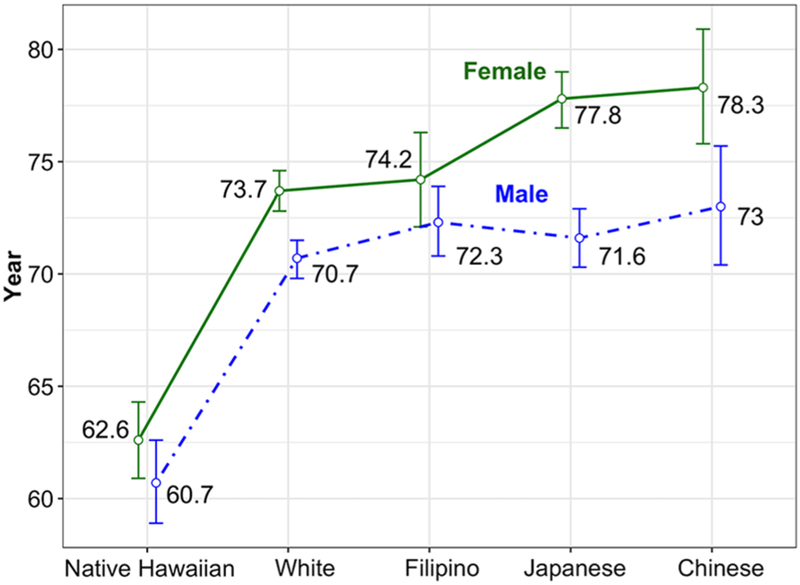
Table 2 shows the 2010 HALE and 95% CIs by sex and ethnicity from birth (<1 years) to age 85 years and older. The overall sex gap at birth in HALE was 4.1 years (female: 73.7 years; male: 69.6 years) compared with 6.4 years in LE (female: 85.6 years; male: 79.2 years). Figure 1 shows the HALE estimates and 95% CIs at birth by sex and race/ethnicity. The sex differences for White, Japanese Americans, and Chinese Americans are larger and stronger (non-overlapping 95% CIs) than that for Native Hawaiians and Filipinos.
Table 2.
Estimates of Healthy Life Expectancy (HALE) and 95% Confidence Intervals (CIs) by Sex and Ethnicity for Hawai’i State, USA. Life Expectancies (LE)a Are Listed for Comparison.
| Overall | Native Hawaiian | White | Filipino | Japanese | Chinese | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (Years) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) | LE | HALE (95% Cl) |
| Male | ||||||||||||
| <1 | 79.2 | 69.6 (69.0–70.2) | 73.9 | 60.7 (58.9–62.6) | 78.3 | 70.7 (69.8–71.5) | 80.8 | 72.3 (70.8–73.9) | 81.2 | 71.6 (70.3–72.9) | 85.3 | <1 |
| 1–4 | 78.7 | 69.1 (68.5–69.7) | 73.4 | 60.2 (58.3–62.1) | 77.6 | 70.0 (69.1–70.8) | 80.3 | 71.8 (70.2–73.4) | 80.7 | 71.0 (69.8–72.3) | 84.5 | 1–4 |
| 5–9 | 74.7 | 65.2 (64.6–65.8) | 69.5 | 56.3 (54.4–58.1) | 73.7 | 66.0 (65.2–66.8) | 76.3 | 67.9 (66.3–69.5) | 76.8 | 67.2 (66.0–68.5) | 80.5 | 5–9 |
| 10–14 | 69.8 | 60.3 (59.7–60.9) | 64.6 | 51.3 (49.4–53.2) | 68.7 | 61.1 (60.3–62.0) | 71.3 | 62.9 (61.3–64.5) | 71.9 | 62.3 (61.0–63.5) | 75.6 | 10–14 |
| 15–19 | 64.8 | 55.5 (54.9–56.1) | 59.6 | 47.1 (45.3–48.9) | 63.7 | 56.4 (55.6–57.1) | 66.4 | 58.0 (56.4–59.6) | 66.9 | 57.4 (56.1–58.6) | 70.6 | 15–19 |
| 20–24 | 60.0 | 50.8 (50.2–51.4) | 54.9 | 42.4 (40.6–44.3) | 59.0 | 51.6 (50.8–52.4) | 61.5 | 53.4 (51.9–54.9) | 62 | 52.7 (51.5–54.0) | 65.6 | 20–24 |
| 25–29 | 55.3 | 46.3 (45.8–46.9) | 50.2 | 37.9 (36.1–39.7) | 54.2 | 46.9 (46.1–47.7) | 56.8 | 49.5 (48.0–50.9) | 57.2 | 48.3 (47.2–49.5) | 60.7 | 25–29 |
| 30–34 | 50.5 | 42.1 (41.6–42.7) | 45.6 | 34.0 (32.2–35.8) | 49.5 | 42.6 (41.9–43.3) | 52.0 | 45.0 (43.6–46.5) | 52.3 | 43.5 (42.4–44.7) | 55.7 | 30–34 |
| 35–39 | 45.8 | 38.1 (37.6–38.6) | 40.9 | 30.3 (28.6–32.0) | 44.8 | 38.5 (37.8–39.2) | 47.3 | 41.3 (40.0–42.7) | 47.5 | 38.9 (37.8–40.0) | 50.9 | 35–39 |
| 40–44 | 41.2 | 33.9 (33.4–34.4) | 36.4 | 26.6 (24.9–28.3) | 40.1 | 34.3 (33.7–34.9) | 42.6 | 36.9 (35.6–38.2) | 42.7 | 34.5 (33.5–35.6) | 46 | 40–44 |
| 45–49 | 36.6 | 30.0 (29.6–30.5) | 32.1 | 23.5 (21.9–25.1) | 35.6 | 30.3 (29.7–30.9) | 38.0 | 32.9 (31.6–34.2) | 38 | 30.6 (29.6–31.6) | 41.1 | 45–49 |
| 50–54 | 32.3 | 26.0 (25.6–26.5) | 27.9 | 20.0 (18.4–21.6) | 31.4 | 26.2 (25.6–26.8) | 33.5 | 28.5 (27.2–29.8) | 33.6 | 26.5 (25.6–27.4) | 36.5 | 50–54 |
| 55–59 | 28.1 | 22.4 (22.0–22.8) | 24.0 | 16.9 (15.3–18.5) | 27.2 | 22.5 (21.9–23.0) | 29.0 | 24.3 (23.0–25.6) | 29.2 | 23.1 (22.3–24.0) | 31.9 | 55–59 |
| 60–64 | 24.1 | 19.1 (18.7–19.6) | 20.3 | 14.8 (13.3–16.4) | 23.3 | 19.1 (18.5–19.7) | 24.8 | 21.4 (20.2–22.6) | 24.9 | 19.5 (18.7–20.3) | 27.4 | 60–64 |
| 65–69 | 20.2 | 15.9 (15.4–16.3) | 16.8 | 11.9 (10.3–13.5) | 19.4 | 15.7 (15.1–16.2) | 20.7 | 17.8 (16.7–19.0) | 20.9 | 16.2 (15.4–17.0) | 23 | 65–69 |
| 70–74 | 16.6 | 12.9 (12.5–13.4) | 13.9 | 9.6 (7.9–11.4) | 15.7 | 12.6 (12.0–13.2) | 16.9 | 15.0 (13.9–16.1) | 17.1 | 12.9 (12.0–13.7) | 18.9 | 70–74 |
| 75–79 | 13.2 | 10.2 (9.7–10.6) | 11.1 | 7.6 (5.6–9.5) | 12.4 | 9.6 (9.0–10.2) | 13.5 | 12.2 (11.2–13.3) | 13.5 | 10.3 (9.5–11.1) | 15.2 | 75–79 |
| 80–84 | 10.3 | 7.7 (7.2–8.2) | 8.6 | 6.1 (3.9–8.3) | 9.6 | 7.1 (6.4–7.7) | 10.5 | 9.7 (8.7–10.8) | 10.2 | 7.6 (6.8–8.4) | 11.8 | 80–84 |
| 85+ | 7.9 | 6.0 (5.5–6.5) | 6.9 | 4.1 (1.1–7.0) | 7.2 | 5.6 (4.9–6.3) | 8.2 | 7.7 (6.5–8.9) | 7.6 | 5.6 (4.8–6.5) | 9.1 | 85+ |
| Female | ||||||||||||
| <1 | 85.6 | 73.7 (73.1–74.3) | 79.4 | 62.6 (60.9–64.3) | 83.4 | 73.7 (72.8–74.6) | 88.1 | 74.2 (72.1–76.3) | 88.0 | 77.8 (76.5–79.0) | 90.0 | 78.3 (75.8–80.9) |
| 1–4 | 85.1 | 73.1 (72.5–73.7) | 79.0 | 62.0 (60.3–63.7) | 82.6 | 72.9 (72.0–73.8) | 87.5 | 73.6 (71.5–75.6) | 87.6 | 77.3 (76.1–78.5) | 89.3 | 77.6 (75.1–80.1) |
| 5–9 | 81.1 | 69.2 (68.6–69.8) | 75.0 | 58.0 (56.4–59.7) | 78.6 | 68.9 (68.0–69.8) | 83.6 | 69.8 (67.7–71.9) | 83.6 | 73.5 (72.3–74.7) | 85.3 | 73.8 (71.2–76.3) |
| 10–14 | 76.2 | 64.3 (63.7–64.9) | 70.1 | 53.1 (51.4–54.8) | 73.8 | 64.1 (63.2–65.0) | 78.6 | 64.8 (62.7–66.9) | 78.7 | 68.6 (67.4–69.7) | 80.3 | 68.8 (66.2–71.3) |
| 15–19 | 71.2 | 59.5 (58.9–60.1) | 65.1 | 48.2 (46.5–49.9) | 68.8 | 59.3 (58.4–60.2) | 73.6 | 60.3 (58.3–62.3) | 73.7 | 64.1 (62.9–65.2) | 75.3 | 64.3 (61.8–66.8) |
| 20–24 | 66.3 | 54.7 (54.1–55.3) | 60.2 | 43.5 (41.8–45.2) | 63.9 | 54.4 (53.5–55.3) | 68.7 | 55.4 (53.4–57.5) | 68.8 | 59.2 (58.1–60.3) | 70.3 | 59.4 (56.9–61.9) |
| 25–29 | 61.4 | 50.4 (49.9–5 1.0) | 55.4 | 39.7 (38.1–41.4) | 59.1 | 50.4 (49.6–5 1.2) | 63.8 | 50.7 (48.6–52.7) | 63.9 | 54.6 (53.5–55.6) | 65.4 | 55.1 (52.8–57.5) |
| 30–34 | 56.5 | 46.1 (45.5–46.6) | 50.4 | 35.3 (33.7–36.9) | 54.2 | 46.0 (45.2–46.8) | 58.8 | 46.1 (44.1–48.1) | 58.9 | 50.0 (49.0–51.0) | 60.4 | 50.2 (47.8–52.5) |
| 35–39 | 51.6 | 41.6 (41.1–42.2) | 45.6 | 31.6 (30.1–33.2) | 49.4 | 41.3 (40.6–42.1) | 54.0 | 41.7 (39.7–43.7) | 54.0 | 45.3 (44.3–46.2) | 55.5 | 45.7 (43.4–47.9) |
| 40–44 | 46.8 | 37.3 (36.8–37.9) | 40.9 | 27.9 (26.4–29.4) | 44.5 | 36.8 (36.1–37.5) | 49.2 | 37.4 (35.4–39.3) | 49.2 | 40.7 (39.8–41.6) | 50.6 | 41.6 (39.6–43.6) |
| 45–49 | 42.1 | 33.1 (32.6–33.6) | 36.2 | 24.2 (22.8–25.6) | 39.8 | 32.4 (31.7–33.1) | 44.3 | 33.1 (31.2–35.0) | 44.3 | 36.1 (35.2–37.0) | 45.7 | 37.3 (35.4–39.2) |
| 50–54 | 37.5 | 29.0 (28.5–29.4) | 31.8 | 21.3 (19.9–22.6) | 35.3 | 28.2 (27.5–28.9) | 39.7 | 28.5 (26.5–30.4) | 39.6 | 31.8 (31.0–32.7) | 40.9 | 32.8 (31.0–34.7) |
| 55–59 | 33.0 | 25.3 (24.8–25.8) | 27.6 | 18.4 (17.1–19.7) | 30.8 | 24.6 (23.9–25.2) | 35.0 | 24.7 (22.8–26.6) | 34.9 | 27.6 (26.8–28.5) | 36.1 | 28.6 (26.7–30.4) |
| 60–64 | 28.6 | 21.8 (21.4–22.3) | 23.4 | 16.2 (15.0–17.5) | 26.4 | 20.8 (20.2–21.5) | 30.6 | 21.5 (19.6–23.4) | 30.4 | 24.0 (23.2–24.8) | 31.4 | 24.3 (22.5–26.1) |
| 65–69 | 24.3 | 18.3 (17.9–18.8) | 19.6 | 13.8 (12.5–15.0) | 22.1 | 17.1 (16.4–17.7) | 26.2 | 18.8 (16.9–20.6) | 25.9 | 20.1 (19.4–20.9) | 26.8 | 20.4 (18.7–22.1) |
| 70–74 | 20.3 | 15.0 (14.5–15.4) | 16.0 | 11.7 (10.5–13.0) | 18.1 | 13.7 (13.0–14.3) | 22.0 | 15.4 (13.5–17.3) | 21.6 | 16.3 (15.5–17.0) | 22.3 | 17.1 (15.5–18.7) |
| 75–79 | 16.5 | 12.1 (11.6–12.5) | 12.9 | 9.7 (8.5–10.9) | 14.3 | 10.3 (9.7–11.0) | 18.1 | 12.4 (10.5–14.3) | 17.7 | 13.5 (12.8–14.2) | 18.3 | 12.9 (11.2–14.6) |
| 80–84 | 13.2 | 9.6 (9.2–10.1) | 10.1 | 7.4 (6.1–8.8) | 11.0 | 7.5 (6.8–8.2) | 14.9 | 10.5 (8.5–12.6) | 14.1 | 10.9 (10.3–11.6) | 14.5 | 10.4 (8.8–12.0) |
| 85+ | 10.3 | 7.7 (7.2–8.2) | 7.9 | 5.8 (4.3–7.4) | 8.3 | 5.5 (4.7–6.2) | 12.4 | 9.4 (7.2–11.7) | 11.0 | 8.8 (8.1–9.5) | 11.1 | 8.0 (6.3–9.6) |
LE estimates from 2010 life tables2.
Figure 1.
Estimates of healthy life expectancy (HALE) and the 95% confidence intervals for HALE at birth by sex and ethnicity for Hawai’i State, USA.
HALE Estimates Differ by Ethnicity for Males
As shown in Figure 1, the HALEs at birth for Chinese, Japanese, and Filipino Americans, and White males were similar to each other (73.0, 71.6, 72.3, and 70.7 years, respectively). However, the HALE at birth for Native Hawaiian males was 60.7 years, which is 12.3 years shorter than for Chinese American males, similar to the 11.4 years of difference in LE at birth (73.9 and 85.3 years, respectively).
HALE Estimates Differ by Ethnicity for Females
Similar patterns were seen among females. The HALE at birth in 2010 for females were 78.3, 77.8, 74.2, 73.7, and 62.6 years in contrast to LE of 90, 88, 88.1, 83.4, and 79.4 for Chinese, Japanese, Filipino Americans, White, and Native Hawaiians, respectively. The gaps of HALE and LE at birth between Native Hawaiian and Chinese American females were 15.7 and 10.6 years, respectively.
Supplementary Figure 1 (available online) visualizes the differences of HALE and LE in Table 2 for all age groups by sex and race/ethnicity. This series of graphs shows that all differences diminish gradually with age.
Discussion
There are significant disparities among ethnic and sex subpopulations among Hawai’i residents. Native Hawaiians not only experience premature mortality but also less years spent in excellent or good health compared with all other ethnic populations in Hawai’i. Similar to research on LE estimates, we found that females live longer than males; females not only live on average 6.4 years longer but also spend 4.1 more years in excellent and good health compared with males in Hawai’i.1
According to the CDC, the US average HALE for age 65 to 69 years in 2007 to 2009 was 14.8 years for females and 12.9 years for males, with the state of Hawai’i having the highest HALE at 17.3 years for females and 15.0 years for males.15 Our 2010 HALE estimates for ages 65 to 69 years were 18.3 years for females and 15.9 years for males, which were consistent with the 2007–2009 CDC estimates.
There was a trend for sex and ethnic differences in LE and HALE to get smaller toward the end of life, which can be attributed to mortality disparities and self-rated fair/poor health throughout all age groups. For all age groups, males had higher mortality rates than females, and Native Hawaiians had higher mortality rates than the other race/ethnicities. Native Hawaiians also reported the highest rates of self-reported fair/poor health. The differences are manifested stronger before 65 years of age.6
Differences in HALE estimates across sex and ethnicity might be attributed to numerous factors, including socioeconomic status, health care system (eg, access to health care services, culturally competent medical providers), individual behaviors (eg, diet, physical activity, obesity, diabetes, etc), biological factors (eg, genetics), and the built physical environment (eg, transportation infrastructure, access to fast food outlets, etc).10–13 For example, individuals with higher educational attainment are more likely to have a longer LE and a higher HALE.10 In Hawai’i, Native Hawaiians have the lowest levels of educational attainment, lowest mean household income, and highest rates of poverty.2,3,5,8 Native Hawaiians are disproportionately affected by various factors that could directly affect both their quality and length of life. However, Filipino had lower levels of socioeconomic status and higher prevalence of chronic decreases but much higher LE and HALE than Native Hawaiians.2 It might due to the fact that Filipino Americans in Hawai’i may return to their home country for end-of-life care. According to practitioners in Hawai’i’s community health centers, which serve many of the state’s new immigrant groups, it is very likely that older Filipinos return to the Philippines when they are sick and near death, taking advantage of strong family support systems and low medical costs in their natal homes. The phenomenon is also seen in Hispanics.23 This may confound the true life expectancy of this population, which may in fact be artifactually lower than that calculated.2
The challenge for Hawai’i is to work at eliminating the disparities observed in HALE estimates among Native Hawaiians in Hawai’i. Therefore, our findings can be used in addition to other health indicators that highlight the ethnic disparities in Hawai’i. Our findings can also supplement discussions on the need for policies that seek to improve the health of Hawai’i’s indigenous population. As others have noted, our government and private sector need to work together to develop, evaluate, and implement public health policies that focus on early childhood, education, income support, employment, housing, and income redistribution.11 Furthermore, there is an extensive amount of national and international literature on the need for a fundamental paradigm shift to improve the health status of indigenous peoples.24,25 Health care and health services research need to not only take a culturally competent approach, but an indigenous-centered approach. It is essential that public health professionals and researchers have an understanding of indigenous peoples’ concepts of health, knowledge, science, and research.24 Building capacity of indigenous peoples to raise household income and family security, and collaborating together in the development and dissemination of public health programs and interventions, will ultimately improve health status.24,26
Advancing LE and HALE should lead to increasing numbers of older adults, which suggests the need for a reworking of policies and programs around the globe. Eligibility criteria that use age as a qualifying criterion may need to be altered to reflect longer lives. At the same time, the findings of this study highlight the importance of data disaggregation. For example, in the United States, increasing the age eligibility for national policies and programs such as Social Security or Medicare based on a higher LE may be discriminatory to those with shorter LE, even with accounting for earlier disability. Moreover, increases in LE do not always equate with increases in HALE. Adding years of poor health and disability often result in increased human, family, community, and economic costs. Subsequently, the need for long-term services and supports— those services that provide help to those unable to perform activities of daily living—rely heavily on the availability of aid level personnel; there are international and national shortages in this type of needed help.
There are several limitations in this study. First, NSCH and HBRFSS data are self-reported, and participants’ perception of one’s health may vary by culture. Research has shown ethnic minorities in the United States typically report poorer self-reported health status than Whites.27,28 Among Asian American subpopulations, Chinese reported worse self-reported health status when nativity and English proficiency were not taken into account, which might cause underestimated HALE.28 Second, the low response rate of the HBRFSS and the small sample sizes of NSCH and HBRFSS by age group may have given bias to underestimates of health status.28,29 Third, the NSCH did not disaggregate the Asian race into specific ethnicities (eg, Japanese, Chinese, and Filipino). The assignment of the same self-reported health status for these children may have impacted our HALE estimates, resulting in an inaccurate reflection of the Japanese, Chinese, and Filipino ethnicities in this study. Fourth, we had relatively small populations, number of deaths, and multiple data sources with self-reported ethnicity that could have increased the variability in the HALE estimates among ethnic groups. Fifth, we had to use the pooled proportions weighted by survey sample size to estimate the proportion of fair/poor health for the age group 15–19 years. Therefore, the accuracy of the HALE estimates may be reduced. Last, the abridged life tables were based on 2010 death record and population estimates; however, the self-reported health status data were from 2011 to 2012. When compared with HALE estimates calculated by the CDC, similar patterns were seen; however, our results for Hawai’i were approximately 1 year higher. This could be a result of their HALE estimates being age-specific (ie, aged 65 years) and analyzing 2007 to 2009 BRFSS data.
A major strength of this study is that it is among the first to examine ethnic differences in HALE estimates among the 5 major ethnic groups in Hawai’i, US. The state’s multi-ethnic population allowed for comparisons in LE and HALE estimates by sex and by age among Native Hawaiians and Asian American subpopulations (eg, Chinese, Japanese, and Filipino). Therefore, another important strength is that our findings provide some insight into the average number of years lived and the average number of years spent in excellent or good health among other ethnic groups in the United States besides Black and Hispanic populations. The HALE and LE estimates for Chinese, Japanese, and Filipino Americans in this article might provide some insight of differences between these Asian Americans living in the United States versus their home countries.
Conclusion
HALE is a simple measure that public health officials, health care providers, researchers, and policy makers can utilize to not only identify health disparities but also monitor changes in the health of populations. Our results serve as a baseline for Hawai’i to monitor trends in the HALE of residents by age. It also highlights the disparities in LE and HALE experienced by Hawai’i’s indigenous population compared with Japanese, Chinese, Filipino, and White residents of Hawai’i. The findings from our study further support the need for our government and private sector to develop and evaluate public health policies that attempt to not only increase the number of years lived, but the proportion of life spent in excellent or good health for Native Hawaiians in Hawai’i.
Supplementary Material
What We Already Know
HALE (healthy life expectancy) combines mortality and morbidity or health status data into a single population health measure. The World Health Organization and the US Centers for Disease Control and Prevention utilize HALE at birth to summarize country-level and state-level population health. HALE varies substantially by sex, race/ethnicity, and country. There is an 11-year gap in life expectancy between Native Hawaiians and Chinese Americans residing in Hawai’i, but HALE has not been estimated.
What This Study Adds
Located in the center of Pacific Ocean between Asia and America, Hawai’i is the most racially and ethnically diverse state in the United States. This article examines HALE disparities by sex among the state’s 5 largest ethnic groups: Native Hawaiians, Whites, and Filipino, Japanese, and Chinese Americans. Our findings show noteworthy gaps in LE and HALE estimates by age between Native Hawaiians and all other major racial/ethnic groups. Native Hawaiians not only experience premature mortality but also spend less years in excellent or good health compared with all other racial/ethnic populations in Hawai’i.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research project was supported in part by the Mountain West IDeA CTR-IN Program under the National Institute of General Medical Sciences of the National Institutes of Health (U54GM104944), the National Institute on Minority Health and Health Disparities of National Institutes of Health, Ola HAWAI’I (Health And Wellness Achieved by Impacting Inequalities) grant #2U54MD007601-31, the Hā Kūpuna National Resource Center for Native Hawaiian Elders funded by the US Administration for Community Living (#90OI0006/01), and Hawai’i Chamber of Commerce.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants participated in the original survey study.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.World Health Organization. Global Health Observatory (GHO) data: world health statistics. https://www.who.int/gho/publications/world_health_statistics/en/. Accessed June 16, 2019.
- 2.Wu YY, Braun K, Horiuchi BY, Tottori C, Onaka AT, Wilkins L. Life expectancies in Hawaii: a multi-ethnic analysis of 2010 life tables. Hawai J Med Public Health. 2017;76:9–14. [PMC free article] [PubMed] [Google Scholar]
- 3.Pobutsky A, Cuaresma C, Kishaba G, et al. The social, cultural and behavioral determinants of health among Hawaii Filipinos: the Filipino Healthy Communities Project. Calif J Health. 2015;13:1–12. [Google Scholar]
- 4.Uchima O, Wu YY, Browne C, Braun KL. Disparities in diabetes prevalence among native Hawaiians/ other Pacific Islanders and Asians in Hawai’i. Prev Chronic Dis. 2019;16:E22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson DB, Oyama N, LeMarchand L, Wilkens L. Native Hawaiians mortality, morbidity, and lifestyle: comparing data from 1982, 1990, and 2000. Pac Health Dialog. 2004;11:120–130. [PubMed] [Google Scholar]
- 6.Hawaii Health Data Warehouse. Health reports & data. Demographic characteristics: resident deaths by race-ethnicity. http://hhdw.org/health-reports-data/data-source/vital-statistics/death-data/demographic-characteristics/. Accessed June 28, 2019.
- 7.Hawaii Health Data Warehouse. Leading causes of death by DOH race-ethnicity 2001–2015. http://hhdw.org/wp-content/uploads/Vital-Statistics_Leading-Causes-of-Deaths_IND_000341.pdf. Published February 13, 2017. Accessed June 10, 2019.
- 8.Ka’opua LS, Braun KL, Browne CV, Mokuau N, Park CB. Why are Native Hawaiians underrepresented in Hawaii’s older adult population? Exploring social and behavioral factors of longevity. J Aging Res. 2011;2011:701232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hastings KG, Jose PO, Kapphahn KI, et al. Leading causes of death among Asian American subgroups (2003–2011). PLoS One. 2015;10:e0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang CF, Nocetti D, Rubin RM. Healthy life expectancy for selected race and gender subgroups: the case of Tennessee. South Med J. 2005;98:977–985. [DOI] [PubMed] [Google Scholar]
- 11.Avendano M, Kawachi I. Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Ann Rev Public Health. 2014;35:307–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pamuk ER, Wagener DK, Molla MT. Achieving national health objectives: the impact on life expectancy and on healthy life expectancy. Am J Public Health. 2004;94:378–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reus-Pons M, Kibele EUB, Janssen F. Differences in healthy life expectancy between older migrants and non-migrants in three European countries over time. Int J Public Health. 2017;62:531–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aitaoto N, Tsark J, Braun KL. Sustainability of the Pacific diabetes today coalitions. Prev Chronic Dis. 2009;6:A130. [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. State-specific healthy life expectancy at age 65 years—United States, 2007–2009. MMWR Morb Mortal Wkly Rep. 2013;62:561–566. [PMC free article] [PubMed] [Google Scholar]
- 16.Chiang CL. The life table and its applications. https://www.popline.org/node/401451. Published 1984. Accessed August 27, 2019. [Google Scholar]
- 17.Robine JM, Jagger C, Oyen HV, et al. Health expectancy calculation by the Sullivan method: a practical guide. Third edition https://webgate.ec.europa.eu/chafea_pdb/assets/files/pdb/2006109/2006109_d5sullivan_guide_final_jun2007.pdf. Published June 2007. Accessed August 27, 2019. [Google Scholar]
- 18.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86:347–354. [PMC free article] [PubMed] [Google Scholar]
- 19.Stiefel MC, Perla RJ, Zell BL. A healthy bottom line: healthy life expectancy as an outcome measure for health improvement efforts. Milbank Q. 2010;88:30–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.State of Hawaii, Department of Health. Hawaii behavioral risk factor surveillance system. http://health.hawaii.gov/brfss/.Accessed August 27, 2019.
- 21.Bramlett MD, Blumberg SJ, Zablotsky B, et al. Design and operation of the National Survey of Children’s Health, 2011–2012. https://www.cdc.gov/nchs/data/series/sr_01/sr01_059.pdf. Published July 2017. Accessed August 27, 2019. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss. Accessed June 23, 2019.
- 23.Hayward MD, Hummer RA, Chiu CT, González-González C, Wong R. Does the Hispanic paradox in US adult mortality extend to disability? Popul Res Policy Rev. 2014;33:81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palafox NA, Buenconsejo-Lum L, Riklon S, Waitzfelder B. Improving health outcomes in diverse populations: competency in cross-cultural research with indigenous Pacific Islander populations. Ethn Health. 2002;7:279–285. [DOI] [PubMed] [Google Scholar]
- 25.Clifford A, McCalman J, Bainbridge R, Tsey K. Interventions to improve cultural competency in health care for Indigenous peoples of Australia, New Zealand, Canada and the USA: a systematic review. Int J Qual Health Care. 2015;27:89–98. [DOI] [PubMed] [Google Scholar]
- 26.Donato R, Segal L. Does Australia have the appropriate health reform agenda to close the gap in Indigenous health? Aust Health Rev. 2013;37:232–238. [DOI] [PubMed] [Google Scholar]
- 27.Su D, Wen M, Markides KS. Is self-rated health comparable between non-Hispanic whites and Hispanics? Evidence from the health and retirement study. J Gerontol B Psychol Sci Soc Sci. 2013;68:622–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lommel LL, Chen JL. The relationship between self-rated health and acculturation in Hispanic and Asian adult immigrants: a systematic review. J Immigr Minor Health. 2016;18:468–478. [DOI] [PubMed] [Google Scholar]
- 29.Dowd JB, Todd M. Does self-reported health bias the measurement of health inequalities in US adults? Evidence using anchoring vignettes from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2011;66:478–489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.