Abstract
Background
Patients who undergo ventricular assist device (VAD) implantation and their caregivers must rapidly learn a significant amount of self-care skills and knowledge.
Objective
To explore patient, caregiver, VAD coordinator, and physician perspectives and perceptions of existing VAD self-care training to inform development of a simulation-based mastery learning (SBML) curriculum to teach patients and caregivers VAD self-care skills and knowledge.
Methods
We conducted semi-structured, in-person interviews with patients with a VAD, their caregivers, VAD coordinators, and physicians (cardiac surgeons, an infectious disease physician, and advanced heart failure cardiologists). We used a two-cycle team-based iterative inductive approach to coding and analysis.
Results
We interviewed 16 patients, 12 caregivers, 7 VAD coordinators and 11 physicians. Seven major themes were derived from the interviews including: identification of critical curricular content, need for standardization and assessment, training modalities (“everybody learns differently”), benefits of repetition (“it’s like tying your shoes”), piecing it all together (knowing the how, but not the why or when), need for refresher training (“could I do it today?”), and provision of training prior to implant (“we know they’re coming”).
Conclusions
This study explored perspectives related to VAD self-care among a multidisciplinary group of stakeholders, which included patients with a VAD, their caregivers, VAD coordinators, and physicians. Themes derived from our analysis allowed us to incorporate these critical participant perspectives in the design and development of a VAD SBML self- care curriculum.
Ventricular assist device (VAD) implantation is a surgical treatment for patients with advanced heart failure, which improves survival and health-related quality of life for these patients.1 A VAD is a mechanical pump implanted into the heart to help circulate blood. A percutaneous lead (i.e., driveline) exits from the pump through the patient’s abdomen and is attached to a small controller (computer that controls actions of the pump), which is connected to either batteries or AC power. After implantation and hospital discharge, patients and caregivers become the primary individuals responsible for “VAD self-care.”2,3
VAD self-care is particularly daunting because errors can result in serious adverse events and possibly death. Patients and their caregivers must be able to monitor pump function, troubleshoot alarms, change the controller if it malfunctions, manipulate power sources, and maintain sterility while changing the driveline exit site dressing. They must also learn about new medications, monitor symptoms that may be related to the VAD, and adjust to a new lifestyle. Adverse events including driveline site infections, stroke, and pump failure are more likely to occur if patients and their caregivers are unable to perform self-care tasks properly.4–6
Patients and their caregivers typically learn VAD self-care during the patient’s admission for VAD implant surgery. This training can be rushed and erratic due to time and availability constraints of patients and caregivers as well as qualified trainers. Patient and caregiver VAD self-care knowledge and skills likely vary at the time of discharge because no standardized methods for training exist.7–9 Rigorous methods are needed to ensure a high level of proficiency in VAD self-care to facilitate a safe patient discharge.
There is a paucity of research on VAD self-care educational content and evaluation of competency. Casida and colleagues developed and tested usability of a VAD self-management mobile phone application.10 Their interactive application taught a) maintenance of the battery, driveline and controller, b) evaluating and reporting abnormal signs and symptoms, c) prevention and recognition of complications and, d) heart failure health maintenance. Educational and clinical outcomes have not yet been reported from this education strategy. Other researchers described needed content for VAD self-care education as including rigorous medication teaching,11 driveline exit site infection identification, and the importance of sterile technique during dressing changes.12 Another study evaluated self-care educational strategies and identified the need for VAD skills competency assessments and reassessments after discharge.13 None of the above articles described how content and/or strategies were incorporated into a VAD self-care teaching curriculum for patients and their caregivers. Yet, Laughran and colleagues described a VAD self-care curriculum that used nursing judgment as a surrogate for evaluation of competency wherein knowledge and skills were checked off once they were completed.14 However, to our knowledge, there are no published VAD self-care curricula that use advanced educational methods and rigorously evaluate VAD self-care competency. Recognizing the deficit in VAD self-care educational research, Kato and colleagues concluded, “For patients to perform optimal self-care once they are discharged, they need optimal education that focuses on knowledge and skills through a collaborative, adult learning approach.”3
In order to address the gaps in the literature and improve care of patients who undergo VAD implantation and their caregivers, we aimed to develop a VAD self-care curriculum informed by Riegel and colleagues’2 heart failure self-care theory and mastery learning theory, using simulation-based mastery learning (SBML).15,16 Riegel and colleagues2 defined heart failure self-care as decision making (in real world situations) that influences actions to maintain physiological stability and facilitate and manage symptoms. This theory and its three components has been applied to VAD self-care.3 These components are critical to safe and successful VAD self-care, as follows: a) self-care maintenance (e.g., driveline care including proper immobilization and exit site care), b) symptom perception (e.g., identifying exit site infections and worsening heart failure) and c) self-care management (e.g., interpreting VAD alarms and knowing what to do when they occur).2 To address these components of self-care theory, we used an SBML education strategy. SBML is a rigorous form of adult learning wherein all learners must meet or exceed a minimum passing standard (MPS) or competency standard on a knowledge and/or simulated skills assessment before completing training.15 The MPS is the level of skill that is safe and effective for patient care as determined by a team of clinical experts.7 Those unable to meet the MPS complete additional practice until they can be retested and meet the standard. Additionally, SBML provides a provision for follow-up competency testing months after initial training.17,18
SBML has been used extensively to train healthcare professionals; its use leads to improved education and clinical outcomes.19–22 Yet, little is known about using simulation as an educational modality to train patients and/or caregivers on self-care tasks.23,24 Further, no studies have described use of semi-structured qualitative interviews to develop a simulation-based curriculum for VAD patient self-care.25,26 Our objective was to explore patient, caregiver, VAD coordinator and physician perspectives and perceptions of existing VAD self-care training, which included an exploration of what knowledge and skills were identified as critical, perceived barriers and facilitators to existing VAD self-care training, and strategies to improve existing training. This information informed the creation of an SBML intervention for patients with VADs and their caregivers to improve self-care knowledge and skills.
METHODS
Study Design
For this study, we used an interpretivist research paradigm,27 which recognizes that there is no one ultimate truth; rather that participants’ perceptions of their reality are both subjective and fluctuating. Engaging a variety of relevant stakeholders, specifically patients, caregivers, VAD coordinators, and physicians who are involved with either training or learning VAD self-care, allowed us to capture multiple, and potentially diverging perspectives to inform development of a VAD SBML self-care curriculum.
A multidisciplinary team of clinicians and researchers with expertise in advanced heart failure and cardiac surgery, VAD self-care and self-care theory, mastery learning theory and SBML, curriculum development, medical education, qualitative methods, and patient-provider communication developed interview guides informed by Riegel’s heart failure self-care theory.2 Separate guides were developed for patients, caregivers, VAD coordinators, and physicians, but all sought to elicit participant perceptions of VAD self-care training. Topics addressed included: knowledge and skill components perceived to be critical to incorporate into VAD self-care training; aspects perceived to be difficult and easy for patients and caregivers; perceived barriers and facilitators to both learning and training; VAD coordinators’ experience with training processes; and participants’ perceptions on improving training.
We then conducted semi-structured, in-person interviews with patients with a VAD, caregivers, VAD coordinators (i.e., nurses and advance practice providers) who teach patients VAD self-care skills, and physicians (i.e., board certified in cardiac surgery, infectious diseases and advanced heart failure cardiology) who care for patients with a VAD. These interviews informed creation of the VAD SBML curriculum, which addressed self-care maintenance, symptom perception, and self-care management.2 This study was approved by the Northwestern University Institutional Review Board.
Participants and Setting
We conducted individual participant interviews during February and March 2017. We recruited VAD coordinators, and physicians at a large urban academic Midwestern medical center where over 50 VAD implant surgeries are performed annually. We further recruited patients with a VAD and their caregivers who were engaged in VAD self-care at the same medical center. Patients and caregivers were excluded if they were non-English speaking, less than 18 years of age, or unable to provide written informed consent.
Data Collection
VAD coordinators and physicians were recruited via email and asked to participate in a face-to-face interview. Patients and caregivers were recruited either in person during a clinic visit or while hospitalized, or via telephone. All interviews were conducted on-site at the medical center (i.e., in private offices/private conference rooms, or, for hospitalized patients, in the patient’s hospital room).
Experienced interviewers (JHB, KLG, KAC) explained the study to participants, who completed written informed consent prior to the interviews. All interviewers reviewed the interview guide and practiced the questions together before conducting interviews. All three interviewers attended each of the first three interviews conducted, with each individual leading one interview and receiving post interview feedback from the others. Subsequently, the vast majority of interviews were performed by 2 of the 3 interviewers. All interviews were conducted independently of others (e.g., patients and caregivers were interviewed separately). Patients and caregivers received parking validation and a $25 gift card as compensation; VAD coordinator and physician participants were not compensated. We collected demographic information from all participants including age, sex, race, and ethnicity. Education level, date and type of VAD implant (HeartWare™ or HeartMate™), VAD implant strategy (e.g., destination therapy vs. bridge to transplant), and time since implant were collected from patients and caregivers, as appropriate. Clinical experience and level of training were collected from VAD coordinators and physicians.
Data Analysis
Digital audio recordings of interviews were transcribed verbatim by an independent organization (GMR Transcription, Tustin, CA), de-identified, and analyzed. We used a team-based iterative inductive approach to coding.28 A detailed audit trail was created and maintained throughout the analytic process, which included memos to record team discussions and decisions.29,30 The team consisted of coders with expertise in advanced heart failure and cardiac surgery, VAD self-care, SBML, curriculum development, medical education, qualitative methods, and patient-provider communication.
In our first cycle coding,28,29 all coders (KAC, RSH, ERC, JEW, KLG, KBS) independently reviewed and coded two transcripts using line-by-line descriptive coding and subcoding to generate a preliminary codebook with code definitions.28,29 The team met repeatedly to compare independent coding and to compile the codebook, clarifying and revising code definitions as necessary. Each coder then independently recoded the two transcripts with the developed codebook. The coders met again to triangulate perspectives and reach consensus on the final codebook. Using multiple coders is a common collaborative process to control for subjective bias that one coder could bring to the coding process; multiple coders allowed for the creation of a shared interpretation of the data.29,31 The coders then split into three teams of two (KAC, RSH; ERC, JEW; KLG, KBS) to code the remaining transcripts. Each team included an advanced heart failure or VAD clinician paired with a partner with qualitative experience. Team members independently coded assigned transcripts and then reconciled coding with their counterpart; resolving discrepancies through discussion. Every transcript therefore was coded independently by at least two team members to establish both trustworthiness and credidibility.
All coded transcripts were then entered into Dedoose version 8.0.35 (Los Angeles, CA) for subsequent analysis. Three coders (KAC, RSH, ERC) engaged in second cycle coding, utilizing pattern coding to summarize emerging categories and themes, identifying consistency within and between transcripts and discerning associations between codes.28,29,32 Coders identified any participant responses that were relevant to creating a VAD self-care curriculum, and reviewed those responses to derive themes. Constant comparison was used to compare responses across all participants, as well as between patients, caregivers, VAD coordinators, and physicians.33 Following second cycle coding and reconciling, the analyses were presented to the larger research team for feedback and critique. VAD coordinator and physician recruitment ended upon completion of interviews with all identified relevant providers. Patient and caregiver recruitment and interviews continued until saturation occurred (i.e., consensus of the research team that no new information was emerging from the interviews).33
RESULTS
All individuals approached for interviews agreed to participate. We interviewed 16 patients, 12 caregivers, 7 VAD coordinators (5 nurses and 2 physician assistants) and 11 physicians (4 cardiac surgeons, 1 infectious disease physician, and 6 advanced heart failure cardiologists). Patients were primarily male with either HeartWare™ or HeartMate™ VAD devices and varying time since implant (Table 1). Caregivers were primarily female, and the majority were the patient’s spouse or partner (Table 1). Most VAD coordinators were female, white, and all had more than 3 years of experience caring for VAD patients (Table 2). Physician interviewees were most typically male, white, and also had more than 3 years’ experience caring for VAD patients (Table 2).
Table 1.
Patient and Caregiver Characteristics.
| Patients (n=16) | Caregivers (n=12) | |
|---|---|---|
| Age, years: mean ± standard deviation | 53.1 ± 14.2 | 51.3 ± 14.3 |
| Sex, n | ||
| Female | 6 | 10 |
| Race, n | ||
| Caucasian | 9 | 6 |
| African American | 6 | 5 |
| Asian | 0 | 0 |
| Other | 1 | 1 |
| Ethnicity, n | ||
| Hispanic or Latino/a | 1 | 1 |
| Non-Hispanic or Latino/a | 15 | 10 |
| Missing | 0 | 1 |
| Marital status, n | ||
| Single | 5 | 3 |
| Married/Partner | 10 | 9 |
| Separated/Divorced | 1 | 0 |
| Widowed | 0 | 0 |
| Education level, n | ||
| < High School | 1 | 1 |
| High School graduate | 6 | 2 |
| Technical school, some college, or associate degree | 6 | 5 |
| Bachelors | 1 | 2 |
| Graduate/Professional | 2 | 1 |
| Unknown | 0 | 1 |
| Home life, n | ||
| Living alone | 2 | 0 |
| Work, n | ||
| Not working | 13 | 4 |
| Insurance, na | ||
| Private | 4 | |
| Medicaid | 11 | |
| Medicare | 3 | |
| Other | 2 | |
| Ventricular Assist Device type, n | ||
| HeartWare™ | 11 | |
| HeartMate II™ | 5 | |
| Implant strategy at time of implant, n | ||
| Destination Therapy | 7 | |
| Bridge to Transplant | 9 | |
| Implant strategy at time of interview | ||
| Destination Therapy | 9 | |
| Bridge to Transplant | 7 | |
| Time since implant, n | ||
| < 6 months | 5 | |
| ≥ 6 months < 24 months | 5 | |
| ≥ 24 months | 6 | |
Patients could select more than one response
Table 2.
Ventricular Assist Device (VAD) Coordinator and Physician Characteristics.
| VAD Coordinators (n=7) | Physicians (n=11) | |
|---|---|---|
| Age, years: mean ± standard deviation | 35.4 ± 7.1 | 46.1 ± 10.0 |
| Sex, n | ||
| Male | 1 | 8 |
| Female | 6 | 3 |
| Race, n | ||
| African American | 0 | 1 |
| Asian | 1 | 2 |
| Caucasian | 6 | 7 |
| Native Hawaiian or Pacific Islander | 0 | 1 |
| Ethnicity, n | ||
| Hispanic or Latino/a | 0 | 0 |
| Non-Hispanic or Latino/a | 7 | 11 |
| Education level (highest degree), n | ||
| Bachelor of Science in Nursing | 3 | |
| Master of Science in Nursinga | 2 | |
| Master of Science in Physician Assistant Studies | 2 | |
| Medical Doctor, Board Certified | 11 | |
| Years in practice, median (Interquartile Range)b | 5.0 (4.0–11.0) | 7.0 (2.0–16.3) |
| Years of VAD experience, median (Interquartile Range)b | 3.0 (3.5–4.0) | 7.5 (3.4–14.0) |
Advanced Practice Nurses
Non-parametric data
Interview Themes
Seven overall themes emerged from our analysis. Table 3 provides an overview and summary of the themes and representative quotes.
Table 3.
Themes and Representative Quotes from Interview Participants.
| Identified themes | Representative quotes |
|---|---|
| Critical curricular content | They have to know the batteries; the power source… and the driveline dressing. The big three major complications of all our VAD patients are infection, stroke, and GI bleeding. (#302 - VAD Coordinator) I think it’s pretty complicated to basically master the whole aspect of taking care of [an] LVAD… when they leave the hospital we should make sure that they are able to change the batteries, deal with the emergency alarms, and change the controller. (#109 - Physician) Well, I think, as far as the alarms, if they would give you some examples of what some of them might be, so if you do see it and -you know, to alert you as to okay, this is what this means….A card or like the booklet that they gave us. (#508 - Patient) There’s a long laundry list of pills that she has to take and some are at different times: Coumadin at night and the other pills during the day and so I took it upon myself to create a spreadsheet that lists both the pharmaceutical name and then the consumer name, which are different sometimes. (#604 - Caregiver) |
| Standardization & assessment | I would say if you wanted to improve it … I don’t know if this might already be [happening], if they have an absolute systematic checklist that they go through. because there’s been turnover and so to make sure that there’s always a smooth transition as new folks come on the team and other folks leave the team. (#107 - Physician) What we have right now are a series of ad hoc pieces of equipment that we have put together. It varies from institution to institution. I think having a standardized simulator that we can train not only people in our center but other centers across the board and show that this definitely makes a difference, which can only help the field, as a whole. (#105 - Physician) That’s a big thing; is try to have consistency wherever they go; to have the same kind of care. So it’s a lot of education and reeducation of the nurses over there and at the facilities we send them to. (#302 - VAD Coordinator) “…it’s just like any teaching. There’s got to be curriculum. There’s got to be assessment, and maybe even self-assessment. (#102 - Physician) |
| Training modalities: “Everybody learns differently” | “…everybody learns differently. Not everyone can just watch people do it and go I’ve got it. Like there’s people that like to have visuals that are like on a screen…The other people that want to do it in person with the LVAD team; they should do that if they’re more comfortable with that… Me personally, it’s more just I like having somebody in front of me teaching me hand on hand how to do it. I don’t like the visual thing. It’s not for me. (#505 - Patient) I think that would be good…having a video of someone doing it [controller change]… that would be great. Because I think what I felt is everything was going too fast and I could not catch up and.I could not comprehend. It was too much. (#611 - Caregiver) … it’s all individual…And it all probably depends on time spent. If someone spends more time with the …patient, and the caregiver was here only for like one or two sessions, or three - then the patient is likely to know better. But if a caregiver, let’s say, [is] more intelligent or more skilled. then maybe a couple sessions with [the] caregiver will be enough to be able to better handle that than the patient. (#102 - Physician) You have to vary training to each patient and family, right? It can’t be the same rote training for everything. (#304 - VAD Coordinator) |
| “It’s like tying your shoes”: The benefits of repetition | .I notice through doing it, making them talk through the steps, it makes them feel a little bit more comfortable and not so, “I’m on my own.” Then, we keep doing it like that until they’ve got it … and do it perfect. (#301 - VAD Coordinator) I mean she’s probably changed it over…I don’t know how many times - hundreds and hundreds of times in the last three years. I’m the one that watches the clock to make sure that things set for this amount of time before we do this and before we do that and we’ve just kind of got it down to a science. (#511 - Patient) I ended up doing two times dressing changes in front of a nurse as opposed to like they were going to have a one-time repeat demonstration. It was kind of nice to have that second one. It was a whole week later. A nurse was there watching and confirmed, yeah; you’re doing it right or maybe do this. (#610 - Caregiver) 'Well, some of this is repetitive motion. So the only way you get good at it is do it over and over and over again. (#104 - Physician) |
| Piecing it all together: Knowing how but not why (or when) (providers only) | One woman was getting nervous - the caregiver - because I was waiting so long for it to dry because she didn’t think the driveline should be exposed to the air for that long. And so I said, “You’re not supposed to wipe it off. You’re supposed to let it dry” [otherwise] you’re wiping the antiseptic off. (#103 - Physician) So, often, they are so focused on learning how to work the stuff, that I think they forget a lot of the theory stuff, about how the VAD works.I always try to remind them, as we do the pieces, that if you are changing controller, the VAD stops. That means that the pump in the heart is no longer pushing blood and the patient’s reliant on just their own heart during that period of time. That’s why we need to do it quickly. (#304 - VAD Coordinator) |
| “Could I do it today?” The need for refresher training | They had me do it when I was in the hospital [controller change]. But if I had to do it right now, I wouldn’t be able to do it on my own. (#512 - Patient) Follow up make sure you [are] on point…I mean once yon feel kind of secure or you [are] so secure that you really [are] not on point but you think you are. That’s why I think that a follow-up actually one-on-one or-a team or whatever…where you can actually show it or they’ll demonstrate it again, I think that would be beneficial. (#607 - Caregiver) I had done some research in the past about driveline infection and dressing and stuff. And, kind of what they came up with was that the whole technique starts to break down after six months of going home. And that, I’ve kind of kept in mind, seeing patients in the hospital, or in clinic. (#306 - VAD Coordinator) So it would entail two dimensions. One would be the actual scheduled activity, where you come and then do it again. So you have the training experience, whether it’s sim-training, or an interactive sessions talking about the LVAD. And in six weeks, you come back and you do it again. My sense is that there’s a certain amount of retention that is enhanced every time you repeat the information…if you go to adult learning theory, the arguments are made now that the teach-back method is really important. (#108 - Physician) |
| “We know they’re coming”: Provision of training prior to implant | I think more materials in one place, rather than having to call in to get questions answered. Providing people exposure before… And my case might have been special because I think my discharge sort of happened suddenly. But, with everything else that was going on, on the day of discharge, it was a little much to get the six to eight hours of data dumping from everybody, on the way out the door. (#504 - Patient) It would be most helpful…probably like a little bit before they actually put it in, but we didn’t know either that they were going to. He just got sick all of a sudden and they had to get him in there, but I mean it would be helpful too to have [teaching]… beforehand just to see what it does, looks like. (#605 - Caregiver) First of all, the person who’s thinking about VAD can come in and play around with this. See, this is what i’ts going to be like. Now you can give them the tools and equipment and stuff like that, but this gives them real world experience. I’ts like, “Ooh, can I do this?” And more important, for the person who says, “I can’t do that. I’m never going to be able -” I mean there are people that say, “I ain’t going to have a VAD because I can’t do all of this.” (#104 - Physician) I think maybe the better thing that we could - only source of improvement would be training more beforehand. Before the actual implant. I think that.our challenges with education are the things that I highlighted with our patient acuity and illness when they come to us. How do you accommodate to somebody that’s on a balloon pump, multiple inotropes, and plus or minus borderline being intubated? (#305 - VAD Coordinator) |
Critical Curricular Content
Aspects regarding both knowledge and skills emerged among all participants as critical for inclusion in a VAD self-care curriculum. When reflecting on the training either provided (from the perspective of VAD coordinators and physicians) or received (patients and caregivers), participants noted the need for training to include necessary VAD self-care skills: battery changes, changing power sources (e.g., from battery to AC power and vice versa), controller changes, dressing changes, general driveline care, and how to shower with a VAD. Dressing changes and controller changes often were identified as the most critical skills. Dressing changes were highlighted due to the potential for infection, as infection is one of the major post implant complications. The need for patients and caregivers to be able to complete a controller change was emphasized, while simultaneously recognized as an uncommon event, and one that cannot be practiced on the VAD patient. Additionally, participants noted the need to understand controller alarms (e.g., what an alarm means and what to do when an alarm occurs), and patient medication needs, dosages, and timing.
Standardization and Assessment
Ensuring that both standardization and assessment were built into the training curriculum was identified as a key feature, primarily by VAD coordinators and physicians. This need for standardization was recommended both within an individual institution (e.g., for training in the event of staff turnover) as well as across institutions (e.g., VAD centers nationwide and skilled nursing facilities caring for patients post discharge). Of note, physician participants often qualified their responses, with the recognition that they did not train patients and caregivers and thus were not fully aware of all existing processes. Coupled with standardization of training, were statements of the need for assessment following training to ensure patients and caregivers were prepared to engage in necessary VAD self-care following hospital discharge.
Training modalities: “Everybody learns differently”
Participants stated that people benefit when they can learn both “in their own way” (e.g., having a variety of training modalities available for adult learners), and “in their own time” (e.g., some participants may need more time than others to feel as though they understand). Discussions of potential training modalities included printed information, content provided didactically, videos (both to watch as an initial learning opportunity and to have on hand as a refresher when needed), and repeated opportunities for hands-on practice, with some participants noting how having a “dummy doll,” (i.e., a simulator), on which to practice needed VAD self-care skills would be beneficial.
“It’s like tying your shoes”: The benefits of repetition
Repetition was noted as contributing to muscle memory and enhancing confidence among those who have to perform VAD self-care skills. VAD coordinators and physicians often reflected on benefits of reinforcement, noting that repeated practice allows patients and caregivers to feel comfortable with the self-care skills they will be required to perform upon hospital discharge. Simulation again was mentioned as a method through which patients and caregivers could have the opportunity to engage in repetition. Patients and caregivers echoed the idea that repetition begets comfort and that the more opportunities they had to practice, the more comfortable and confident they felt in their abilities to perform VAD self-care.
Piecing it all together: Knowing how but not why (or when)
A theme that emerged among clinicians was that patients and caregivers were not always aware of why they had to perform self-care, as taught. An example was maintaining sterile technique while changing a driveline exit site dressing, which is second nature to clinicians, but not a common experience for most patients and caregivers. Clinicians noted the necessity of reminding patients and caregivers about how a sterile field can be broken (e.g., even though their gloved hands may be sterile, as soon as they touch an object including their face or hair, the sterile field is broken). Another example related to the fact that, while patients and caregivers were taught to wait after performing a particular task (e.g., following application of chlorhexidine during a driveline dressing change), it appeared to not always be clear to patients and caregivers why they should wait (e.g., so the antiseptic could be effective at killing bacteria). Not surprisingly, this theme was absent from patient and caregiver interviews.
“Could I do it today?” The need for refresher training
Currently, any refresher training given to patients and caregivers is provided ad hoc, (e.g., if a patient requests a refresher on how to change a controller, the VAD coordinator provides a demonstration and has the patient practice on a training controller, to the extent that time allows). Also, if a patient is hospitalized due to a driveline infection, the VAD team will review the dressing change protocol and sterile technique with both patient and caregiver. However, there is no existing protocol for refresher training for patients and caregivers. Participants from each group commented on the potential benefits of regular retraining and appeared to be open to its implementation. All agreed that the primary barrier to formal retraining was personnel (i.e., VAD coordinator) time.
“We know they’re coming”: Provision of training prior to VAD implant
A final theme identified, again primarily by clinicians, was related to when VAD self-care skills training should be offered to patients and caregivers. Participants commented that the opportunity for patients and caregivers to be able to see and hold a VAD in their hand prior to implant could be helpful. Additionally, participants suggested being able to meet a patient with a VAD may allow them to obtain a sense of what it would be like to “live with” a VAD, and that having earlier exposure to training (i.e., pre-implant) may be beneficial as patients and caregivers may be better able to see themselves as capable of performing the required tasks. However, it was noted that VAD implants are often performed emergently, which presents a significant barrier to “pre-training.”
Creation of the Final Curriculum
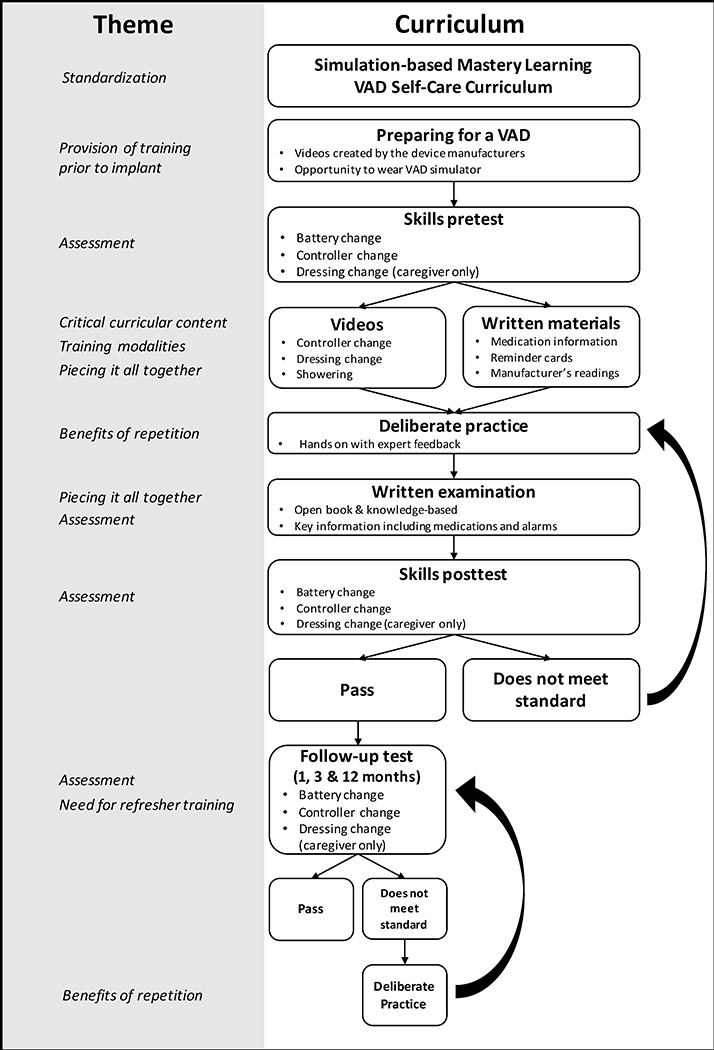
The derived themes guided creation of the final SBML curriculum. The Figure presents an overview of how these themes mapped to the final SBML curriculum.
Figure.
Derived Themes Mapped to the Simulation-based Mastery Learning Ventricular Assist Device Self-Care Curriculum.
We created videos to address key content including controller and dressing changes (with pictures and descriptions of infected driveline sites), and showering with a VAD. A video on power source changes was not created as interviewees deemed it to be a simple task, and it is partially demonstrated in the controller change video. Patients and caregivers view the showering video once the VAD team authorizes the patient to shower (usually six weeks after implant). The training curriculum also was created to emphasize information on medications and VAD controller alarms, which is reinforced during an open-book written examination we developed.7 Reminder cards with detailed information on how to respond to controller alarms, and reminders about supplies/equipment needed when travelling, were created and attached to the patients’ VAD peripheral equipment carry bag. We also provided patients with a weekly pill organizer coupled with specific instructions on organizing medications.
The curriculum was standardized by requiring patients and caregivers to participate in an SBML intervention. First, patients and caregivers participate in a skills pretest on a wearable simulator, specifically created for this study.7 We created three assessments consisting of a dichotomous skills checklist for key tasks including controller, power source, and dressing change (caregiver only due to the difficulty of patients maintaining sterile technique during their own dressing changes).7 We created learning materials to address varying training modalities, utilizing diverse learning strategies including videos, hands-on experiences, reminder cards, face-to-face teaching, manufacturers’ reading materials, and provision of copies of all training videos and materials. Patients and caregivers receive the benefits of repetition (deliberate practice) on the simulator, with an expert instructor who provides feedback. Each participant is required to complete each of the skills accurately a minimum of three times during the deliberate practice sessions. Alarm reminder cards, patient medications, written materials, and VAD and peripheral equipment function are reviewed with patients and caregivers. After deliberate practice, participants again perform the simulated skills examinations consisting of the same skills (posttest) and complete the written knowledge exam.7 We also measure self-efficacy before and after the curriculum education to assess change in patients’ and caregivers’ confidence in skill acquisition.
All participants are required to meet or exceed an MPS on each of the skills and knowledge exams before completing training.7 Standard setting techniques used to create the MPS are described elsewhere.7 Participants unable to meet the MPS complete more deliberate practice and/or study until they can be retested and meet the standard. Patients and caregivers are trained in a time independent fashion as required by SBML. This mastery learning approach acknowledges variation in learning speed, while ensuring that all participants achieve a high level of competency.
Key information and skills are emphasized with explanation as to the importance of performance so patients and caregivers understand the why and when of required self-care skills. For example, during training we explain that patients or caregivers should slowly sing the song “Happy Birthday” twice during hand washing because it takes 30 seconds–the recommended duration of hand washing. We also explain why it is important to use chlorhexidine scrubbing of the driveline site using a vigorous back and forth motion for thirty seconds, followed by thirty seconds of drying.9 We explain that bacteria can grow up to five skin cell layers deep, and this motion and timing allow for optimal effectiveness in deeper skin layers. Finally, we show patients and caregivers a simulator with a closed circuit VAD pump to demonstrate how the mechanics of the VAD work to circulate blood.
Refresher training is addressed routinely in SBML interventions.17,18 Specifically, in the VAD SBML curriculum, we require patients and caregivers to meet or exceed the MPS on simulated skills [controller, power source, and dressing change tasks] at one, three, and 12 months after their original posttest. Those unable to meet or exceed the MPS participate in further training until they can be retested and meet this standard. Fortunately, patients with a VAD and their caregivers come to clinic frequently so these follow-up assessments and retrainings are not overly burdensome and can occur regularly.
Finally, some interviewees requested provision of training prior to implant. As soon as patients are identified as potential VAD candidates, patients and their caregivers are provided access to videos created by the device manufacturers that describe life with a VAD.34,35 However, creation of specific standardized pre-implant curriculum months before VAD implantation is not realistic due to the often lengthy process for evaluation and shared decision making about this advanced surgical treatment option, which may not necessarily result in the decision to proceed with a VAD, as well as the sometimes emergent nature of VAD implantation. Nevertheless, the new wearable simulator created for this curriculum responds to this theme by allowing patients and caregivers to experience what it is like to wear and carry peripheral VAD equipment prior to implant.
DISCUSSION
Our analysis of patient, caregiver, VAD coordinator, and physician perspectives and perceptions of existing VAD self-care training led us to derive seven unique training-related themes that informed creation of a VAD SBML self-care curriculum: identification of critical curricular content; need for standardization and assessment; recognition of the importance of providing varied training modalities for the learners; the benefits of repetition; piecing it all together to connect the how, why and when; a need for refresher training; and the provision of training prior to implant. Some of these themes have already been described in the VAD self-care education literature, while others provide new information. For instance, other studies have identified similar key curricular content to include in a VAD self-care curriculum that was also identified through our interviews (e.g., dressing changes and medication teaching).10–12 Additionally, other authors have called for standardization and competency assessment as well as a need for refresher training.13,14 In a mixed methods study, Casida and colleagues noted that patients and caregivers identified a need for competency assessment and reassessment of VAD self-care after discharge.13
Our study identified new areas that patients, caregivers, VAD coordinators, and physicians discussed as being critical for a VAD self-care education curriculum: a) use of multiple training modalities (e.g., videos, reminder cards, simulation), b) benefits of repetition (e.g., deliberate practice on the simulator), c) piecing it all together (e.g., provision of a clear explanation as to why particular self-care tasks are performed), d) and provision of training prior to implant (e.g., videos and wearable simulator). These areas are aligned with adult learning theory in many ways. Adults learn best through experiential (e.g., simulation) and self-directed learning (e.g., videos, open-book assessments) on topics of immediate value.36,37 Repetition (via deliberate practice) is a proven method for gaining expertise in complex skills.38 Additionally, adults need to know why they need to learn something because if there is no specific reason for why a particular task needs to be performed the way it is taught, the task is more easily forgotten.36,37 Finally, early (limited) training allows the potential for pre-implant decision making and sets expectations for life with a VAD (i.e., topic of immediate value).36,37
The theme of critical curricular content was heavily informed by Riegel’s self-care theory.2 Interviewees identified key content within the three components of Riegel’s theory: a) self-care maintenance (e.g., dressing changes, controller changes, medications, showering with a VAD), b) symptom perception (e.g., identifying exit site infections) and c) self-care management (e.g., interpreting VAD alarms and knowing what to do when they occur).2 Riegel’s self-care theory did not aid in identifying the best methods for education or the “how, why, or when” of a VAD self-care curriculum, which emerged from our interviews. For instance, patient and caregiver interviewees suggested creation of emergency and reminder cards (“how”). Providers emphasized that patients and caregivers needed to learn why they were doing the tasks they were asked to perform (“why”). Providers also stated that “pre-training” has benefits for patients considering VAD implant as a treatment option (“when”).
To our knowledge, this is the first study to describe a VAD self-care SBML curriculum that was created based on stakeholder interviews and informed by self-care theory.3 SBML has never been used to teach patients and caregivers the skills and knowledge they need to perform high risk tasks such as VAD self-care. SBML is an ideal method for training providers on high risk healthcare tasks. It has been successfully used to improve the skills of nurses,20 medical students39 residents,40 fellows,41 and attending physicians42 and provides superior educational outcomes compared to other forms of educational training.43,44 Additionally, SBML has been shown to improve patient outcomes after training clinicians in multiple clinical skill sets including central venous catheter insertion,45,46 paracentesis,47 thoracentesis,48 and laparoscopic surgery.22,49 Therefore, we are now comparing performance and retention of VAD self-care skills between SBML-trained and a usual care-trained groups immediately following training as part of a randomized controlled trial. Our next step will be to examine differences in clinical and health-related quality of life outcomes in patients who undergo VAD implantation and their caregivers in a larger, multisite trial.
Our study has limitations. First, as it was conducted with participants affiliated with a single academic medical center; responses may not represent perspectives across all academic centers. However, we have no reason to believe that responses from our diverse patient and caregiver population as well as our VAD coordinators and physicians with varied clinical experience would not accurately reflect VAD self-care training needs. Second, self-selection bias among individuals who agreed to participate in interviews is a potential concern. However, as all of those approached consented to be interviewed, we believe such bias did not affect our results. Third, while interviewer and/or coder bias may have occurred, we sought to minimize this occurrence by using both non-clinicians and clinicians as interviewers, engaging multidisciplinary team members as coders, and having two or more individuals code each interview. Finally, we recognize that we were unable to completely address the final theme, provision of training prior to implant, in the SBML curriculum. In our center, and probably most other VAD centers, VADs are sometimes implanted in acutely ill patients in emergent situations. Somewhat similarly, it is not always possible to make final decisions about device type, implant strategy, and timing of surgery to allow training to begin before VAD implantation for advanced heart failure patients who are relatively stable.
CONCLUSIONS
We derived key themes via interviews of patients, caregivers, and clinicians to inform the creation of a patient-centered VAD SBML self-care curriculum. This curriculum is unique because it incorporated advanced educational techniques (multimodal adult learning), and combined self-care and mastery learning theories, as well as identified important curricular content not previously described in the literature. Based on our interviews, SBML was a natural fit for the high risk tasks needed for safe VAD self-care. Further study is needed to determine if our VAD SBML self-care curriculum improves patient and caregiver skills as well as patient outcomes such as reduced driveline exit site infections and stroke and enhanced health-related quality of life.
Acknowledgments
We would like to acknowledge Drs. Douglas Vaughan, Kevin O’Leary, Duc Pham, and Clyde Yancy for their support and encouragement of this work. We thank the patients, caregivers, VAD coordinators and physicians at Northwestern Memorial Hospital for their dedication to education and patient safety.
Funding: This work was supported by the National Institutes of Health, National Institute of Nursing Research [grant number 1R21NR016745-01].
Footnotes
Conflict of Interest Disclosures: The authors have no relevant financial disclosures to report.
REFERENCES
- 1.Kormos RL, Cowger J, Pagani FD, et al. The Society of Thoracic Surgeons Intermacs database annual report: Evolving indications, outcomes, and scientific partnerships. J Heart Lung Transplant. 2019;38:114–26. [DOI] [PubMed] [Google Scholar]
- 2.Riegel B, Dickson VV, Faulkner KM. The Situation-Specific Theory of Heart Failure Self-Care: Revised and Updated. J Cardiovasc Nurs. 2016;31:226–35. [DOI] [PubMed] [Google Scholar]
- 3.Kato N, Jaarsma T, Ben Gal T. Learning self-care after left ventricular assist device implantation. Curr Heart Fail Rep. 2014;11:290–8. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein DJ, Naftel D, Holman W, et al. Continuous-flow devices and percutaneous site infections: clinical outcomes. J Heart Lung Transplant. 2012;31(11):1151–1157. [DOI] [PubMed] [Google Scholar]
- 5.Kirklin JK, Pagani FD, Kormos RL, et al. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36(10):1080–1086. [DOI] [PubMed] [Google Scholar]
- 6.Yarboro LT, Bergin JD, Kennedy JL, et al. Technique for minimizing and treating driveline infections. Ann Cardiothorac Surg. 2014;3(6):557–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barsuk JH, Harap RS, Cohen ER, Cameron KA, Grady KL, Wilcox JE et al. The effect of judge selection on standard setting using the mastery angoff method during development of a ventricular assist device self-care curriculum. Clin Simul Nurs. 2019;27:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Widmar SB, Dietrich MS, Minnick AF. How self-care education in ventricular assist device programs is organized and provided: a national study. Heart Lung. 2014;43:25–31. [DOI] [PubMed] [Google Scholar]
- 9.Wilcox JE, Cameron KA, Harap RS, et al. Ventricular Assist Device Driveline Dressing Change Protocols: A Need for Standardization. A report from the SimVAD investigators. J Card Fail. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casida JM, Aikens JE, Craddock H, Aldrich MW, Pagani FD. Development and Feasibility of Self-Management Application in Left-Ventricular Assist Devices. ASAIO J. 2018;64:159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hermsen JL, Smith JW, Mokadam NA. Self-administration education and polypharmacy in mechanical circulatory support patients. J Heart Lung Transplant. 2013;32:1141–2. [DOI] [PubMed] [Google Scholar]
- 12.Barber J, Leslie G. A simple education tool for ventricular assist device patients and their caregivers. J Cardiovasc Nurs. 2015;30(3):E1–E10. [DOI] [PubMed] [Google Scholar]
- 13.Casida JM, Combs P, Schroeder SE, Hickey KT. Ventricular Assist Device Self- Management Issues: The Patient and Caregiver Perspectives. ASAIO J. 2018;64:e148–e50. [DOI] [PubMed] [Google Scholar]
- 14.Loughran S, Kealy J, Shook A, Kaan A. The development and evaluation of a competency-based program for patients with a ventricular assist device. Can J Cardiovasc Nurs. 2012;22(3):18–23. [PubMed] [Google Scholar]
- 15.McGaghie WC, Barsuk JH, Wayne DB. AM last page: mastery learning with deliberate practice in medical education. Acad Med. 2015;90(11):1575. [DOI] [PubMed] [Google Scholar]
- 16.McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation- based mastery learning with translational outcomes. Med Educ. 2014;48(4):375–385. [DOI] [PubMed] [Google Scholar]
- 17.Didwania A, McGaghie WC, Cohen ER, et al. Progress toward improving the quality of cardiac arrest medical team responses at an academic teaching hospital. J Grad Med Educ.. 2011;3(2):211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barsuk JH, Cohen ER, McGaghie WC, Wayne DB. Long-term retention of central venous catheter insertion skills after simulation-based mastery learning. Acad Med. 2010;85(10 Suppl):S9–12. [DOI] [PubMed] [Google Scholar]
- 19.Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37(10):2697–2701. [PubMed] [Google Scholar]
- 20.Barsuk JH, Cohen ER, Mikolajczak A, Seburn S, Slade M, Wayne DB. Simulation-based mastery learning improves central line maintenance skills of ICU nurses. J Nurs Adm. 2015;45(10):511–517. [DOI] [PubMed] [Google Scholar]
- 21.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern. 2009;169(15):1420–1423. [DOI] [PubMed] [Google Scholar]
- 22.Schwab B, Teitelbaum EN, Barsuk JH, Soper NJ, Hungness ES. Single-stage laparoscopic management of choledocholithiasis: An analysis after implementation of a mastery learning resident curriculum. Surgery. 2018;163(3):503–508. [DOI] [PubMed] [Google Scholar]
- 23.Haupt BA, Beauvais A. Veterans receive high-fidelity simulation educaiton preoperatively. Clin Simul Nurs. 2014;10(11):538–545. [Google Scholar]
- 24.Tofil NM, Rutledge C, Zinkan JL, et al. Ventilator caregiver education through the use of high-fidelity pediatric simulators: a pilot study. Clin Pediatr (Phila). 2013;52(11):1038–1043. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed K, Khan R, Mottrie A, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015;116(1):93–101. [DOI] [PubMed] [Google Scholar]
- 26.McKee R, Sussman AL, Nelson MT, Russell JC. Using qualitative and quantitative assessment to develop a patient safety curriculum for surgical residents. J Surg Educ. 2016;73(3):529–535. [DOI] [PubMed] [Google Scholar]
- 27.Bunniss S, Kelly DR. Research paradigms in medical education research. Med Educ. 2010;44(4):358–366. [DOI] [PubMed] [Google Scholar]
- 28.Miles MB, Huberman M, Saldana J. Qualitative Data Analysis. 3rd ed. Thousand Oaks, CA: SAGE Publications; 2014. [Google Scholar]
- 29.Saldana J The Coding Manual for Qualitative Researchers. Thousand Oaks, CA: SAGE publications; 2013. [Google Scholar]
- 30.Birks M, Chapman Y, Francis K. Memoing in qualitative research: probing data and processes. J Res Nurs. 2008;13:68–75. [Google Scholar]
- 31.Lincoln YS, Guba EG. Naturalistic Inquiry. 1st ed. Beverly Hills, CA: SAGE Publications; 1985. [Google Scholar]
- 32.Kolb SM. Grounded theory and the constant comparative method: valid research strategies for educators. JETERAPS. 2012;3(1):83–86. [Google Scholar]
- 33.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Taylor and Francis Group; 1967. [Google Scholar]
- 34.Abbott. HeartMate 3 Ventricular Assist System: Patient Education Program. Version 1.5. Copyright 2017.
- 35.Medtronic Inc. Patient Stories [Educational Video]. Copyright 2016.
- 36.Merriam SB, Caffarella RS, Baumgartner L. Learning in adulthood : a comprehensive guide. 3rd ed. San Francisco: Jossey-Bass; 2007. [Google Scholar]
- 37.Merriam SB, Bierema LL. Adult Learning: Linking Theory and Practice. First ed: John Wiley & Sons, Inc; 2014. [Google Scholar]
- 38.Ericsson KA. Peak : Secrets from the New Science of Expertise. Boston: Houghton Mifflin Harcourt; 2016. [Google Scholar]
- 39.Butter J, McGaghie WC, Cohen ER, Kaye M, Wayne DB. Simulation-based mastery learning improves cardiac auscultation skills in medical students. J Gen Intern Med. 2010;25(8):780–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barsuk JH, Cohen ER, Vozenilek JA, O’Connor LM, McGaghie WC, Wayne DB. Simulation-based education with mastery learning improves paracentesis skills. J Grad Med Educ. 2012;4(1):23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barsuk JH, Ahya SN, Cohen ER, McGaghie WC, Wayne DB. Mastery learning of temporary hemodialysis catheter insertion by nephrology fellows using simulation technology and deliberate practice. Am J Kidney Dis. 2009;54(1):70–76. [DOI] [PubMed] [Google Scholar]
- 42.Barsuk JH, Cohen ER, Nguyen D, et al. Attending physician adherence to a 29-component central venous catheter bundle checklist during simulated procedures. Crit Care Med. 2016;44(10):1871–1881. [DOI] [PubMed] [Google Scholar]
- 43.Cook DA, Brydges R, Zendejas B, Hamstra SJ, Hatala R. Mastery learning for health professionals using technology-enhanced simulation: a systematic review and meta-analysis. Acad Med. 2013;88(8):1178–1186. [DOI] [PubMed] [Google Scholar]
- 44.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Medical education featuring mastery learning with deliberate practice can lead to better health for individuals and populations. Acad Med. 2011;86(11):e8–9. [DOI] [PubMed] [Google Scholar]
- 45.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–1423. [DOI] [PubMed] [Google Scholar]
- 46.Barsuk JH, Cohen ER, Potts S, et al. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23(9):749–756. [DOI] [PubMed] [Google Scholar]
- 47.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126(4):349–356. [DOI] [PubMed] [Google Scholar]
- 48.Barsuk JH, Cohen ER, Williams MV, et al. Simulation-based mastery learning for thoracentesis skills improves patient outcomes: a randomized trial. Acad Med.. 2018;93(5):729–735. [DOI] [PubMed] [Google Scholar]
- 49.Zendejas B, Cook DA, Bingener J, et al. Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg. 2011;254(3):502–509; discussion 509–511. [DOI] [PubMed] [Google Scholar]