Abstract
Several studies have examined the relationship between smoking and mortality in cancer survivors. However, few have reported the relationships in several cancer sites (i.e., bladder, non-melanoma skin, uterine, melanoma, and lymphoma), and limited data exist on the dose-response relationship between number of cigarettes smoked per day or duration of smoking cessation and mortality. Cancer survivors (N = 35,093, 61% female, mean age = 47 years old) from the National Health Interview Survey with linked data retrieved from the National Death Index served as our study participants. Cox proportional-hazards models were used to assess associations between smoking status, all-cause, and disease-specific mortality. After a median follow-up of 13 years, 11,066 deaths occurred. Survivors who reported smoking at study entry had a 73%, 75%, 85% higher risk for cardiovascular disease, cancer, and all-cause mortality, respectively when compared to nonsmokers. Former smokers had a 31% and 37% higher risk of all-cause and cancer mortality, respectively when compared to nonsmokers. The observed relationships appeared to differ by the number of cigarettes smoked (i.e., ≥ 10 per day), especially for breast, cervix, lung, prostate, uterine and non-melanoma skin cancer survivors. Those who continued smoking post diagnosis were at greatest risk of all-cause and cancer mortality, but the associations varied substantially by cancer site. These data provide sufficient evidence of the health hazards associated with smoking for cancer survivors and provide further support for public health strategies designed to curb smoking in this vulnerable population.
Keywords: Post-diagnosis smoking, all-cause, cardiovascular, cancer survivors, mortality, cohort
Introduction
The number of cancer survivors is expected to reach 19 million by 2024 in the United States [1]. Cancer survivors represent a vulnerable population because they have a higher risk for cardiovascular disease (CVD), diabetes, osteoporosis, second cancers, and premature mortality when compared to age-matched controls [2-4]. Given their increased vulnerability to chronic health conditions, the American Cancer Society and the Institute of Medicine has advocated for engaging in healthy lifestyle behaviors throughout the survivorship continuum [5,6]. Smoking, in particular, may increase one’s risk for cancer because it stimulates cancer-promoting signaling cascades [7-9]. However, for those with a prior cancer diagnosis, it may escalate the risk for poor cancer-specific and all-cause mortality [10]. Thus, it is of considerable importance to clarify the association between smoking and risk of disease-specific and all-cause mortality among cancer survivors who smoke.
Previous studies have examined the association between smoking and disease-specific mortality among cancer survivors [11-18]. The studies in their entirety have confirmed associations between smoking and all-cause mortality among colon, prostate, and lung cancer survivors [13,14,19,20], and for cancer-specific mortality among colon, prostate, and breast cancer survivors [13,14,19,21,22]. However, several gaps in the literature remain unknown. For example, to our knowledge, few if any studies have examined the relationship between smoking and mortality in bladder, lymphoma, and uterine cancer survivors. In addition, limited data exist on the dose-response relationship between number of cigarettes smoked per day or duration of smoking cessation and mortality [14].
Therefore, the purpose of this study was to examine the relationship between both post-diagnosis smoking status and smoking intensity and both all-cause and disease-specific mortality among cancer survivors in the United States.
Materials and methods
Study population
The National Health Interview Survey (NHIS) is a stratified, multistage probability survey designed to examine the prevalence and incidence of disease and disability as well as the use of health care services in the United States. Black and Hispanic were oversampled to ensure equal representation in the study, but sample weights were used to ensure that estimates conform to national ethnic proportions. A detailed description of the probability sampling strategy and consenting methods were described elsewhere [23].
A total of 35,093 cancer adults from the 13 cross-sectional waves identified from 1997 to 2013 and their linked mortality data ending on December 31, 2015 were included in this analysis. For site-specific cancer, we focused on the ten most common cancer sites (i.e., bladder, breast, cervix, colon, lung, prostate, non-melanoma skin, uterine, melanoma, and lymphoma).
Mortality
Ascertainment of mortality was established using the International Classification of Diseases-10 Revision codes [24]. Study outcomes were defined as follows: 1) all-cause mortality; 2) cancer mortality (C00 to C97); and 3) CVD-mortality (I00 to I09, I11, I13, and I20 to I51, I60 to I69).
Exposure assessment
Smoking status (never, former, or current) was ascertained at the initial interview via two binary coded (i.e., yes/no) items: 1) have you smoked at least 100 cigarettes in your entire life? and 2) do you now still smoke cigarettes? Those participants responding “No” to both questions were classified as nonsmokers. Those participants responding “Yes” to the first item and “No” the second item were classified as former smokers). Those who responded “Yes” to both questions were classified as current smokers. To distinguish between current and former smokers, time since last cigarette (i.e., quit ≥ 20 years ago; quit 10 to 19 years ago; quit < 10 years ago) were used to classify former smokers, and cigarettes smoked per day (i.e. > 10 cigarettes per day; ≤ 10 cigarettes per day) were used to classify current smoker.
Covariates
Several covariates were included in the study. In particular, we included demographic variables (i.e., race, gender, education, and marital status), lifestyle variables (i.e., body mass index, physical activity, and alcohol consumption), comorbid conditions (i.e., hypertension, stroke and coronary heart disease), and self-rated health. Body mass index was calculated as weight in kilograms divided by height in meters squared.
Detailed information on the highest level of school completed was collected and the variable was categorized as “less than high school degree” (high school not completed), “high school degree” (high school diploma or general equivalency diploma), and “more than high school degree” (some college, vocational, or technical school; associate’s degree; Bachelor’s, Master’s, or professional degree) [25].
NHIS study participants answered questionnaires about their alcohol consumption and patterns of use [26]. These questions obtained information about the following: 1) consumption of ≥ 12 drinks in one’s lifetime, in any previous year, or the past year; 2) drinking frequency (days per week, month, or year) and drinking quantity (drinks per day) in the past year; and 3) binge drinking in the past year. Using these variables, we categorized survivors into four alcohol consumption groups: 1) lifetime abstainers: < 12 drinks in one’s lifetime; 2) former drinkers: ≥ 12 drinks in a previous year; 3) current drinker: current use of drinks/week.
Socioeconomic status was assessed based on the family income to poverty ratio (PIR) [27]. We separated participants into 3 groups: low-income (i.e., at or below the poverty ratio), middle-income (i.e., above the PIR to < 4), and high-income (i.e., PIR, ≥ 4) adults.
Statistical analysis
Weighted descriptive characteristics were used to describe the sample. Chi-square test of independence was used to examine categorical differences in the weighted percentages by smoking status. We also used Cox proportional hazard models with proportionality assumptions to examine all associations between smoking status and disease-specific and all-cause mortality. We adjusted for potential covariates and conducted two sensitivity analyses: (1) exclusion of individuals who died within the first 2-years and (2) participants with a history of CHD or stroke. In addition, we made comparisons between current smokers (> 10 cigarettes per day; ≤ 10 cigarettes per day) and former smokers (quit ≥ 20 years ago; quit 10 to 19 years ago; quit < 10 years ago). All analyses took into account the complex survey design (strata, clusters, and weights). All analyses were performed using STATA version 13.0 (Stata Corp, College Station, TX, USA). All P-values were two-sided and statistical significance was determined at P ≤ 0.05.
Results
The mean age of participants was 47 years at study entry. Compared with nonsmokers, former or current smokers were more likely to be men and non-Hispanic whites (p-value < 0.001). Never smokers appeared to be more educated. Current smokers were less physically active, leaner (i.e., BMI < 25 kg/m2) and consumed more alcohol. Former smokers were more likely to have a history of hypertension, diabetes, CHD and stroke. Descriptive statistics were reported in Table 1.
Table 1.
Baseline characteristics of cancer patients by smoking status
| Characteristic | Subgroups | Never smoking | Former smoking | Current smoking | P value | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| No. | % | No | % | No | % | |||
| Age | < 0.001 | |||||||
| < 45 years | 2364 | 15.99% | 861 | 7.20% | 1777 | 30.21% | ||
| 45-65 years | 5382 | 37.62% | 4159 | 35.31% | 2893 | 47.57% | ||
| > 65 years | 8116 | 46.39% | 7974 | 57.49% | 1567 | 22.22% | ||
| Sex | < 0.001 | |||||||
| Male | 4791 | 34.25% | 6831 | 56.13% | 2157 | 36.84% | ||
| Female | 11071 | 65.75% | 6163 | 43.87% | 4080 | 63.16% | ||
| Race/ethnicity | < 0.001 | |||||||
| Hispanic | 1321 | 5.78% | 582 | 3.08% | 315 | 3.23% | ||
| Non-Hispanic White | 12752 | 85.73% | 11221 | 90.67% | 5153 | 87.62% | ||
| Non-Hispanic Black | 1354 | 5.92% | 987 | 4.92% | 634 | 7.00% | ||
| Non-Hispanic Other | 435 | 2.57% | 204 | 1.34% | 135 | 2.14% | ||
| Education | < 0.001 | |||||||
| Less than high school degree | 2679 | 13.73% | 2537 | 17.50% | 1427 | 21.33% | ||
| High school degree | 4338 | 27.33% | 3691 | 28.62% | 2114 | 35.86% | ||
| More than high school degree | 8845 | 58.94% | 6766 | 53.88% | 2696 | 42.80% | ||
| Marital status | < 0.001 | |||||||
| Married/Living with partner | 7991 | 64.97% | 7080 | 69.19% | 2648 | 56.85% | ||
| Widowed/Divorced/Separated/Never married | 7871 | 35.03% | 5914 | 30.81% | 3589 | 43.15% | ||
| Income level | < 0.001 | |||||||
| Low | 1848 | 8.11% | 1137 | 6.26% | 1414 | 18.60% | ||
| Middle | 8215 | 48.49% | 7167 | 52.49% | 3381 | 55.03% | ||
| High | 5799 | 43.40% | 4690 | 41.25% | 1442 | 26.37% | ||
| Body mass index | < 0.001 | |||||||
| < 25 kg/m2 | 6087 | 38.62% | 4521 | 33.79% | 2885 | 45.61% | ||
| 25-30 kg/m2 | 5549 | 35.01% | 4992 | 39.15% | 1960 | 32.12% | ||
| > 30 kg/m2 | 4226 | 26.37% | 3481 | 27.06% | 1392 | 22.28% | ||
| Physical activity | < 0.001 | |||||||
| Low | 9927 | 59.51% | 8083 | 59.74% | 4378 | 69.52% | ||
| High | 5935 | 40.49% | 4911 | 40.26% | 1859 | 30.48% | ||
| Alcohol intake | < 0.001 | |||||||
| Lifetime abstainer | 5171 | 29.74% | 1366 | 9.93% | 681 | 10.28% | ||
| Former drinker | 2972 | 17.97% | 4001 | 28.92% | 1589 | 25.34% | ||
| Current drinker | 7648 | 51.83% | 7539 | 60.53% | 3915 | 63.71% | ||
| Self-rated health | < 0.001 | |||||||
| Excellent | 2702 | 18.84% | 1735 | 14.16% | 595 | 9.65% | ||
| Very good | 4306 | 28.46% | 3282 | 25.89% | 1337 | 22.37% | ||
| Good | 5015 | 31.04% | 4167 | 32.22% | 1955 | 31.53% | ||
| Fair | 2774 | 15.67% | 2581 | 18.84% | 1512 | 23.26% | ||
| Poor | 1065 | 5.99% | 1229 | 8.88% | 838 | 13.19% | ||
| History of hypertension | < 0.001 | |||||||
| Yes | 7835 | 46.52% | 7081 | 52.97% | 2632 | 40.77% | ||
| No | 8027 | 53.48% | 5913 | 47.03% | 3605 | 59.23% | ||
| History of diabetes | < 0.001 | |||||||
| Yes | 2317 | 13.83% | 2286 | 16.96% | 680 | 10.69% | ||
| No | 13545 | 86.17% | 10708 | 83.04% | 5557 | 89.31% | ||
| History of CHD | < 0.001 | |||||||
| Yes | 1466 | 9.04% | 2065 | 16.24% | 607 | 9.15% | ||
| No | 14396 | 90.96% | 10929 | 83.76% | 5630 | 90.85% | ||
| History of stroke | < 0.001 | |||||||
| Yes | 939 | 5.45% | 992 | 7.45% | 477 | 6.79% | ||
| No | 14923 | 94.55% | 12002 | 92.55% | 5760 | 93.21% | ||
Abbreviations: CHD = coronary heart disease.
Among 35,093 cancer survivors, 11,066 died of all-causes (including 3,979 cancer and 2,156 CVD deaths) after a median follow-up of 13 years. The most common deaths occurred among survivors of breast (752 deaths), prostate (559 deaths), lung (467 deaths), colon (435 deaths), and non-melanoma skin (384 deaths) cancer survivors. Similarly, CVD deaths occurred mostly in breast (389 deaths) , prostate (348 deaths), and non-melanoma skin (334 deaths) cancer survivors (Figure 1 Analytic sample selection).
Figure 1.
Analytic sample.
Smoking status
All-cause mortality
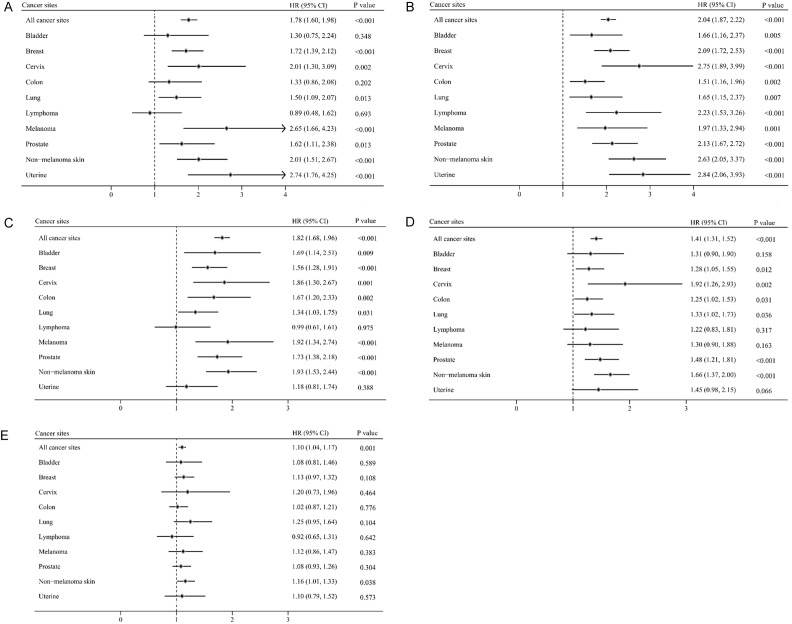
Among all survivors, current smokers had an 85%, 75% and 73% higher risk for all-cause, cancer, and CVD-related mortality when compared to never smokers. However, former smokers had a higher risk for all-cause (31%) and cancer mortality (37%), but not CVD mortality (see Figures 2, 3 and Table 2). For specific cancer sites, there was a 60% increase in all-cause mortality among current smokers who were survivors of bladder, breast, lung, colon, lymphoma and prostate cancer, and 130% increase in all-cause mortality among survivors of cervical, uterine, melanoma and non-melanoma cancer when compared to never smokers. Similarly, former smokers had a 27% higher risk for all-cause mortality when compared to select cancer survivors (i.e., breast, colon, lung, melanoma, prostate, uterine and non-melanoma skin cancer survivors) who never smoked. These relationships were stronger for cervical cancer survivors (Hazard Ratio [HR] = 1.58, 95% CI = 1.16 to 2.15) who never smoked, but no associations were observed in bladder and lymphoma cancer survivors (Figure 2-Current smoking and risk of all-cause mortality).
Figure 2.
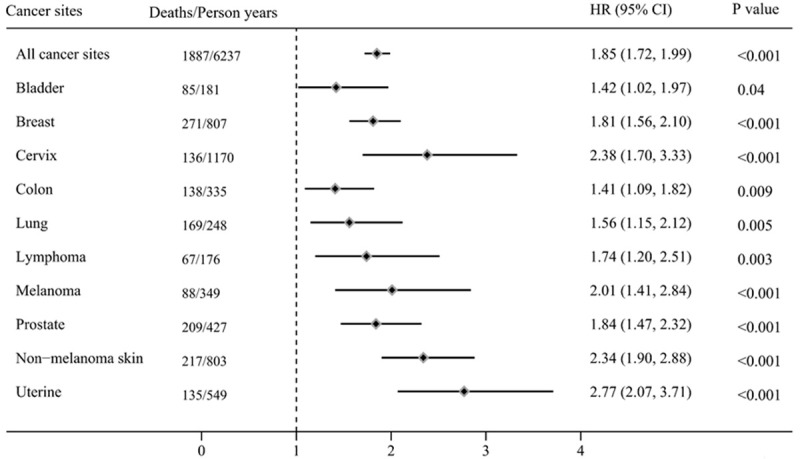
Current smoking and risk of all-cause mortality.
Figure 3.
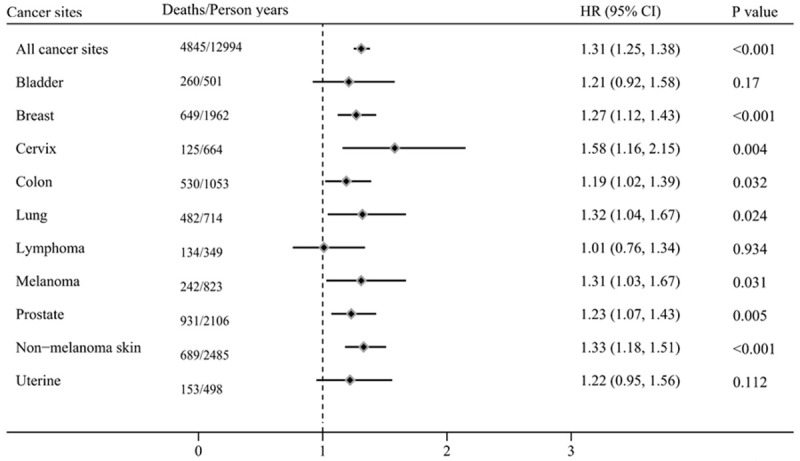
Former smoking and risk of all-cause mortality.
Table 2.
Cancer, CVD and other cause mortality among cancer survivors according to smoking status
| Cancer sites | Smoking status | Subgroups | Cancer mortality | CVD mortality | Other mortality | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||
| Deaths | Person years | HR (95% CI) | P valuea | Deaths | Person years | HR (95% CI) | P valuea | Deaths | Person years | HR (95% CI) | P valuea | |||
| All sites | ||||||||||||||
| Never smoking | 1386 | 15862 | 1 (Reference) | 941 | 15862 | 1 (Reference) | 2007 | 15862 | 1 (Reference) | |||||
| Current smoking | 825 | 6237 | 1.75 (1.57 to 1.95) | < 0.001 | 292 | 6237 | 1.73 (1.47 to 2.05) | < 0.001 | 770 | 6237 | 2.06 (1.83 to 2.33) | < 0.001 | ||
| < 10 cigarette per day | 1.74 (1.50 to 2.03) | < 0.001 | 1.83 (1.42 to 2.37) | < 0.001 | 1.80 (1.50 to 2.16) | < 0.001 | ||||||||
| ≥ 10 cigarette per day | 1.89 (1.67 to 2.14) | < 0.001 | 1.79 (1.47 to 2.18) | < 0.001 | 2.39 (2.09 to 2.75) | < 0.001 | ||||||||
| Former smoking | 1768 | 12994 | 1.37 (1.25 to 1.49) | < 0.001 | 923 | 12994 | 1.08 (0.96 to 1.22) | 0.194 | 2154 | 12994 | 1.38 (1.27 to 1.49) | < 0.001 | ||
| Quit smoking < 10 years | 1.87 (1.66 to 2.10) | < 0.001 | 1.50 (1.23 to 1.83) | < 0.001 | 1.88 (1.65 to 2.14) | < 0.001 | ||||||||
| Quit smoking 10-19 years | 1.49 (1.31 to 1.68) | < 0.001 | 1.26 (1.07 to 1.48) | 0.006 | 1.42 (1.27 to 1.60) | < 0.001 | ||||||||
| Quit smoking ≥ 20 years | 1.09 (0.98 to 1.21) | 0.122 | 0.91 (0.79 to 1.05) | 0.204 | 1.21 (1.11 to 1.33) | < 0.001 | ||||||||
| P for trend | < 0.001 | < 0.001 | < 0.001 | |||||||||||
| Bladder | ||||||||||||||
| Never smoking | 23 | 210 | 1 (Reference) | 17 | 210 | 1 (Reference) | 47 | 210 | 1 (Reference) | |||||
| Current smoking | 34 | 181 | 1.62 (0.92 to 2.86) | 0.092 | 13 | 181 | 1.11 (0.45 to 2.70) | 0.824 | 38 | 181 | 1.37 (0.81 to 2.32) | 0.242 | ||
| < 10 cigarette per day | 2.40 (1.07 to 5.38) | 0.033 | 0.33 (0.07 to 1.57) | 0.163 | 0.93 (0.39 to 2.25) | 0.877 | ||||||||
| ≥ 10 cigarette per day | 1.73 (0.91 to 3.26) | 0.092 | 1.41 (0.54 to 3.64) | 0.48 | 0.68 (0.96 to 2.97) | 0.071 | ||||||||
| Former smoking | 86 | 501 | 1.11 (0.66 to 1.87) | 0.682 | 50 | 501 | 1.29 (0.70 to 2.38) | 0.419 | 124 | 501 | 1.18 (0.82 to 1.71) | 0.366 | ||
| Quit smoking < 10 years | 2.11 (1.06 to 4.19) | 0.033 | 0.98 (0.31 to 3.10) | 0.978 | 1.59 (0.86 to 2.93) | 0.135 | ||||||||
| Quit smoking 10-19 years | 1.16 (0.60 to 2.22) | 0.657 | 1.72 (0.83 to 3.59) | 0.147 | 1.19 (0.73 to 1.96) | 0.487 | ||||||||
| Quit smoking ≥ 20 years | 0.86 (0.47 to 1.57) | 0.612 | 1.20 (0.60 to 2.40) | 0.615 | 1.15 (0.76 to 1.73) | 0.507 | ||||||||
| P for trend | 0.075 | 0.504 | 0.293 | |||||||||||
| Breast | ||||||||||||||
| Never smoking | 392 | 3608 | 1 (Reference) | 240 | 3608 | 1 (Reference) | 473 | 3608 | 1 (Reference) | |||||
| Current smoking | 120 | 807 | 1.47 (1.16 to 1.85) | 0.001 | 39 | 807 | 1.79 (1.17 to 2.72) | 0.007 | 112 | 807 | 2.46 (1.90 to 3.18) | < 0.001 | ||
| < 10 cigarette per day | 1.53 (1.12 to 2.11) | 0.008 | 2.16 (1.29 to 3.63) | 0.004 | 1.83 (1.26 to 2.65) | 0.002 | ||||||||
| ≥ 10 cigarette per day | 1.55 (1.15 to 2.10) | 0.005 | 1.97 (1.08 to 3.58) | 0.028 | 3.32 (2.43 to 4.54) | < 0.001 | ||||||||
| Former smoking | 240 | 1962 | 1.20 (1.00 to 1.45) | 0.053 | 110 | 1962 | 0.95 (0.71 to 1.26) | 0.702 | 299 | 1962 | 1.50 (1.25 to 1.81) | < 0.001 | ||
| Quit smoking < 10 years | 1.31 (0.96 to 1.78) | 0.086 | 1.89 (1.17 to 3.06) | 0.01 | 1.90 (1.39 to 2.61) | < 0.001 | ||||||||
| Quit smoking 10-19 years | 1.51 (1.12 to 2.04) | 0.007 | 0.87 (0.58 to 1.31) | 0.516 | 1.20 (0.88 to 1.63) | 0.241 | ||||||||
| Quit smoking ≥ 20 years | 0.95 (0.72 to 1.24) | 0.682 | 0.67 (0.44 to 1.02) | 0.062 | 1.54 (1.23 to 1.94) | < 0.001 | ||||||||
| P for trend | 0.011 | 0.253 | < 0.001 | |||||||||||
| Cervix | ||||||||||||||
| Never smoking | 41 | 1023 | 1 (Reference) | 34 | 1023 | 1 (Reference) | 56 | 1023 | 1 (Reference) | |||||
| Current smoking | 40 | 1170 | 1.67 (0.91 to 3.06) | 0.098 | 16 | 1170 | 1.50 (0.68 to 3.34) | 0.315 | 80 | 1170 | 3.66 (2.28 to 5.89) | < 0.001 | ||
| < 10 cigarette per day | 1.43 (0.61 to 3.36) | 0.407 | 2.36 (0.80 to 6.95) | 0.119 | 2.54 (1.40 to 4.60) | 0.002 | ||||||||
| ≥ 10 cigarette per day | 1.94 (1.03 to 3.63) | 0.039 | 1.16 (0.49 to 2.80) | 0.732 | 4.46 (2.67 to 7.43) | < 0.001 | ||||||||
| Former smoking | 32 | 664 | 1.44 (0.85 to 2.45) | 0.172 | 22 | 664 | 0.96 (0.50 to 1.83) | 0.895 | 71 | 664 | 2.08 (1.33 to 3.25) | 0.001 | ||
| Quit smoking < 10 years | 1.73 (0.93 to 3.21) | 0.085 | 1.39 (0.58 to 3.32) | 0.463 | 2.39 (1.42 to 4.02) | 0.001 | ||||||||
| Quit smoking 10-19 years | 1.52 (0.62 to 3.68) | 0.356 | 1.24 (0.40 to 3.85) | 0.706 | 2.60 (1.50 to 4.51) | 0.001 | ||||||||
| Quit smoking ≥ 20 years | 1.15 (0.46 to 2.84) | 0.765 | 0.54 (0.22 to 1.33) | 0.179 | 1.65 (0.83 to 3.29) | 0.156 | ||||||||
| P for trend | 0.09 | 0.321 | < 0.001 | |||||||||||
| Colon | ||||||||||||||
| Never smoking | 165 | 1133 | 1 (Reference) | 107 | 1133 | 1 (Reference) | 234 | 1133 | 1 (Reference) | |||||
| Current smoking | 63 | 335 | 1.33 (0.95 to 1.88) | 0.098 | 22 | 335 | 1.81 (0.98 to 3.34) | 0.06 | 53 | 335 | 1.46 (0.98 to 2.17) | 0.062 | ||
| < 10 cigarette per day | 1.24 (0.74 to 2.08) | 0.416 | 2.22 (0.93 to 5.29) | 0.072 | 1.11 (0.50 to 2.46) | 0.8 | ||||||||
| ≥ 10 cigarette per day | 1.38 (0.92 to 2.07) | 0.114 | 1.62 (0.75 to 3.53) | 0.22 | 1.79 (1.15 to 2.81) | 0.011 | ||||||||
| Former smoking | 207 | 1053 | 1.26 (0.99 to 1.61) | 0.061 | 109 | 1053 | 1.17 (0.84 to 1.62) | 0.342 | 214 | 1053 | 1.18 (0.89 to 1.55) | 0.242 | ||
| Quit smoking < 10 years | 1.32 (0.88 to 2.00) | 0.181 | 1.84 (1.02 to 3.32) | 0.043 | 1.93 (1.16 to 3.21) | 0.011 | ||||||||
| Quit smoking 10-19 years | 1.18 (0.83 to 1.69) | 0.349 | 1.15 (0.69 to 1.92) | 0.578 | 1.40 (1.01 to 1.93) | 0.042 | ||||||||
| Quit smoking ≥ 20 years | 1.27 (0.98 to 1.66) | 0.076 | 1.00 (0.68 to 1.47) | 0.985 | 0.90 (0.68 to 1.20) | 0.477 | ||||||||
| P for trend | 0.13 | 0.059 | 0.004 | |||||||||||
| Lung | ||||||||||||||
| Never smoking | 58 | 172 | 1 (Reference) | 8 | 172 | 1 (Reference) | 23 | 172 | 1 (Reference) | |||||
| Current smoking | 115 | 248 | 1.24 (0.87 to 1.76) | 0.242 | 15 | 248 | 1.13 (0.34 to 3.79) | 0.837 | 39 | 248 | 3.78 (1.99 to 7.18) | < 0.001 | ||
| < 10 cigarette per day | 1.09 (0.73 to 1.63) | 0.683 | 1.87 (0.54 to 6.47) | 0.32 | 3.62 (1.76 to 7.44) | 0.001 | ||||||||
| ≥ 10 cigarette per day | 1.43 (0.95 to 2.15) | 0.085 | 0.51 (0.10 to 2.62) | 0.419 | 4.10 (1.94 to 8.67) | < 0.001 | ||||||||
| Former smoking | 294 | 714 | 1.09 (0.82 to 1.45) | 0.538 | 47 | 714 | 1.15 (0.44 to 3.00) | 0.771 | 141 | 714 | 2.27 (1.36 to 3.79) | 0.002 | ||
| Quit smoking < 10 years | 1.11 (0.81 to 0.92) | 0.522 | 1.15 (0.41 to 3.23) | 0.79 | 2.50 (1.42 to 4.40) | 0.002 | ||||||||
| Quit smoking 10-19 years | 1.12 (0.78 to 1.59) | 0.541 | 1.31 (0.46 to 3.75) | 0.612 | 2.12 (1.20 to 3.75) | 0.01 | ||||||||
| Quit smoking ≥ 20 years | 1.05 (0.76 to 1.46) | 0.751 | 0.91 (0.27 to 3.08) | 0.877 | 2.15 (1.20 to 3.86) | 0.01 | ||||||||
| P for trend | 0.433 | 0.545 | 0.004 | |||||||||||
| Lymphoma | ||||||||||||||
| Never smoking | 72 | 475 | 1 (Reference) | 23 | 475 | 1 (Reference) | 54 | 475 | 1 (Reference) | |||||
| Current smoking | 39 | 176 | 1.69 (1.04 to 2.74) | 0.035 | 4 | 176 | 0.81 (0.22 to 3.02) | 0.751 | 24 | 176 | 1.92 (0.96 to 3.82) | 0.065 | ||
| < 10 cigarette per day | 0.91 (0.43 to 1.93) | 0.813 | 0.26 (0.02 to 2.94) | 0.273 | 0.96 (0.27 to 3.34) | 0.945 | ||||||||
| ≥ 10 cigarette per day | 2.21 (1.33 to 3.65) | 0.002 | 0.91 (0.18 to 4.56) | 0.904 | 2.35 (1.09 to 5.09) | 0.03 | ||||||||
| Former smoking | 70 | 349 | 1.01 (0.68 to 1.49) | 0.976 | 20 | 349 | 1.09 (0.49 to 2.42) | 0.838 | 44 | 349 | 0.97 (0.59 to 1.57) | 0.886 | ||
| Quit smoking < 10 years | 1.15 (0.63 to 2.09) | 0.651 | 0.73 (0.16 to 3.24) | 0.677 | 0.89 (0.36 to 2.21) | 0.799 | ||||||||
| Quit smoking 10-19 years | 0.94 (0.51 to 1.73) | 0.853 | 1.46 (0.53 to 4.06) | 0.464 | 1.44 (0.74 to 2.80) | 0.287 | ||||||||
| Quit smoking ≥ 20 years | 0.93 (0.57 to 1.52) | 0.782 | 0.98 (0.35 to 2.79) | 0.973 | 0.79 (0.44 to 1.43) | 0.432 | ||||||||
| P for trend | 0.77 | 0.95 | 0.525 | |||||||||||
| Melanoma | ||||||||||||||
| Never smoking | 64 | 1036 | 1 (Reference) | 53 | 1036 | 1 (Reference) | 99 | 1036 | 1 (Reference) | |||||
| Current smoking | 40 | 349 | 2.31 (1.35 to 3.93) | 0.002 | 9 | 349 | 1.34 (0.48 to 3.75) | 0.572 | 39 | 349 | 2.15 (1.26 to 3.66) | 0.005 | ||
| < 10 cigarette per day | 2.12 (1.02 to 4.44) | 0.046 | 3.32 (0.84 to 13.17) | 0.087 | 3.12 (1.39 to 7.02) | 0.006 | ||||||||
| ≥ 10 cigarette per day | 2.34 (1.30 to 4.22) | 0.005 | 0.86 (0.28 to 2.63) | 0.789 | 2.29 (1.26 to 4.15) | 0.006 | ||||||||
| Former smoking | 80 | 823 | 1.18 (0.75 to 1.88) | 0.473 | 50 | 823 | 1.05 (0.63 to 1.74) | 0.85 | 112 | 823 | 1.50 (1.04 to 2.17) | 0.031 | ||
| Quit smoking < 10 years | 1.04 (0.56 to 1.94) | 0.897 | 1.39 (0.65 to 2.96) | 0.396 | 2.94 (1.82 to 4.77) | < 0.001 | ||||||||
| Quit smoking 10-19 years | 1.71 (0.89 to 3.27) | 0.107 | 0.83 (0.38 to 1.82) | 0.647 | 1.20 (0.69 to 2.11) | 0.515 | ||||||||
| Quit smoking ≥ 20 years | 1.09 (0.64 to 1.86) | 0.755 | 0.99 (0.55 to 1.79) | 0.967 | 1.19 (0.81 to 1.75) | 0.378 | ||||||||
| P for trend | 0.389 | 0.74 | 0.003 | |||||||||||
| Prostate | ||||||||||||||
| Never smoking | 161 | 1411 | 1 (Reference) | 112 | 1411 | 1 (Reference) | 225 | 1411 | 1 (Reference) | |||||
| Current smoking | 86 | 427 | 1.95 (1.45 to 2.64) | < 0.001 | 43 | 427 | 1.39 (0.89 to 2.16) | 0.15 | 80 | 427 | 2.00 (1.39 to 2.88) | < 0.001 | ||
| < 10 cigarette per day | 2.19 (1.52 to 3.16) | < 0.001 | 0.91 (0.39 to 2.14) | 0.832 | 1.50 (0.75 to 2.98) | 0.251 | ||||||||
| ≥ 10 cigarette per day | 1.97 (1.32 to 2.95) | 0.001 | 1.97 (1.24 to 3.13) | 0.004 | 2.40 (1.63 to 3.54) | < 0.001 | ||||||||
| Former smoking | 312 | 2106 | 1.26 (1.00 to 1.59) | 0.052 | 193 | 2106 | 0.96 (0.73 to 1.27) | 0.77 | 426 | 2106 | 1.37 (1.11 to 1.70) | 0.004 | ||
| Quit smoking < 10 years | 1.56 (1.07 to 2.27) | 0.02 | 1.85 (1.12 to 3.05) | 0.016 | 1.82 (1.29 to 2.56) | 0.001 | ||||||||
| Quit smoking 10-19 years | 1.65 (1.20 to 2.25) | 0.002 | 0.89 (0.58 to 1.37) | 0.587 | 1.72 (1.32 to 2.26) | < 0.001 | ||||||||
| Quit smoking ≥ 20 years | 1.07 (0.82 to 1.39) | 0.619 | 0.85 (0.65 to 1.12) | 0.257 | 1.22 (0.96 to 1.55) | 0.101 | ||||||||
| P for trend | 0.001 | 0.144 | 0.042 | |||||||||||
| Non-melanoma skin | ||||||||||||||
| Never smoking | 123 | 2998 | 1 (Reference) | 145 | 2998 | 1 (Reference) | 324 | 2998 | 1 (Reference) | |||||
| Current smoking | 81 | 803 | 3.01 (2.15 to 4.21) | < 0.001 | 33 | 803 | 1.73 (1.07 to 2.81) | 0.026 | 103 | 803 | 2.27 (1.69 to 3.05) | < 0.001 | ||
| < 10 cigarette per day | 2.58 (1.49 to 4.46) | 0.001 | 1.77 (0.89 to 3.53) | 0.104 | 1.86 (1.21 to 2.86) | 0.005 | ||||||||
| ≥ 10 cigarette per day | 3.44 (2.36 to 5.00) | < 0.001 | 1.66 (0.93 to 2.98) | 0.089 | 2.62 (1.84 to 3.72) | < 0.001 | ||||||||
| Former smoking | 180 | 2485 | 1.47 (1.12 to 1.94) | 0.005 | 156 | 2485 | 1.12 (0.84 to 1.50) | 0.429 | 353 | 2485 | 1.38 (1.15 to 1.66) | 0.001 | ||
| Quit smoking < 10 years | 2.71 (1.84 to 3.99) | < 0.001 | 1.14 (0.61 to 2.15) | 0.677 | 1.93 (1.38 to 2.70) | < 0.001 | ||||||||
| Quit smoking 10-19 years | 1.65 (1.05 to 2.59) | 0.031 | 1.75 (1.17 to 2.61) | 0.006 | 1.63 (1.23 to 2.17) | 0.001 | ||||||||
| Quit smoking ≥ 20 years | 1.17 (0.85 to 1.59) | 0.337 | 0.98 (0.71 to 1.36) | 0.926 | 1.24 (1.01 to 1.53) | 0.039 | ||||||||
| P for trend | < 0.001 | 0.097 | 0.001 | |||||||||||
| Uterine | ||||||||||||||
| Never smoking | 65 | 935 | 1 (Reference) | 64 | 935 | 1 (Reference) | 145 | 935 | 1 (Reference) | |||||
| Current smoking | 41 | 549 | 2.57 (1.51 to 4.37) | 0.001 | 48 | 549 | 2.78 (1.54 to 5.04) | 0.001 | 66 | 549 | 2.96 (2.00 to 4.38) | < 0.001 | ||
| < 10 cigarette per day | 2.26 (1.05 to 4.89) | 0.038 | 1.65 (0.72 to 3.79) | 0.237 | 3.55 (1.98 to 6.39) | < 0.001 | ||||||||
| ≥ 10 cigarette per day | 3.14 (1.71 to 5.77) | < 0.001 | 3.62 (1.85 to 7.09) | < 0.001 | 2.58 (1.65 to 4.05) | < 0.001 | ||||||||
| Former smoking | 35 | 498 | 1.18 (0.76 to 1.85) | 0.461 | 32 | 498 | 0.92 (0.54 to 1.56) | 0.761 | 86 | 498 | 1.40 (1.01 to 1.96) | 0.046 | ||
| Quit smoking < 10 years | 1.61 (0.76 to 3.43) | 0.213 | 0.42 (0.15 to 1.14) | 0.089 | 1.42 (0.79 to 2.57) | 0.239 | ||||||||
| Quit smoking 10-19 years | 2.15 (1.18 to 3.92) | 0.012 | 0.97 (0.39 to 2.45) | 0.952 | 1.39 (0.80 to 2.40) | 0.245 | ||||||||
| Quit smoking ≥ 20 years | 0.56 (0.27 to 1.17) | 0.125 | 1.12 (0.59 to 2.15) | 0.726 | 1.35 (0.88 to 2.07) | 0.173 | ||||||||
| P for trend | 0.073 | 0.366 | 0.342 | |||||||||||
Abbreviations: CVD = cardiovascular disease; CI = confidence interval; HR = hazard ratio, CHD = coronary heart disease.
Adjusted for age, sex, race, education level, marital status, body mass index, physical activity, alcohol intake, income level, self-rated health, history of hypertension, diabetes, CHD, stroke and duration of cancer.
Cancer mortality
The HRs for cancer mortality ranged from 1.47 to 3.01 among current smokers who were survivors of non-melanoma skin (HR = 3.01, 95% CI = 2.15 to 4.21) and uterine cancer (HR = 2.57, 95% CI = 1.51 to 4.37), followed by survivors of melanoma (HR = 2.31, 95% CI = 1.35 to 3.93), prostate (HR = 1.95, 95% CI = 1.45 to 2.64), lymphoma (HR = 1.69, 95% CI = 1.04 to 2.74), and breast (HR = 1.47, 95% CI = 1.16 to 1.85) cancer. In contrast, former smokers who were survivors of on-melanoma skin cancer (HR = 1.47, 95% CI = 1.12 to 1.94) had a higher risk for cancer mortality than survivors who never smoked.
CVD mortality
For CVD mortality, current smokers had a higher risk of CVD mortality in uterine (HR = 2.78, 95% CI = 1.54 to 5.04), breast (HR = 1.79, 95% CI = 1.17 to 2.72), and non-melanoma skin cancer survivors (HR = 1.73, 95% CI = 1.07 to 2.81) when compared to those who never smoked. Former smokers, regardless of cancer diagnosis did not have a higher risk for CVD mortality when compared to never smokers (Figure 3 Former smoking and risk of all-cause mortality).
Smoking intensity
All-cause mortality
As summarized in Figure 4A, 4B and Table 2, when compared to those who never smoked, current smokers who smoked ≥ 10 cigarettes per day had a higher risk of all-cause (HR = 2.04, 95% CI = 1.87 to 2.22) and cancer (HR = 1.89, 95% CI = 1.67 to 2.14) mortality when compared to those who smoked < 10 cigarettes per day. For site-specific cancers, current smokers who smoked ≥ 10 cigarettes per day had a higher risk for all-cause mortality than those who smoked < 10 cigarettes per day for breast, cervix, lung, prostate, uterine and non-melanoma skin cancer survivors.
Figure 4.
Cigarettes per day and risk of all-cause mortality among current smokers (A. Current smokers smoked < 10 cigarettes per day and risk of all-cause mortality; B. Current smokers smoked ≥ 10 cigarettes per day and risk of all-cause mortality). Time since smoking cesstions and risk of all-cause mortality among former smokers (C. Former smokers quit smoking < 10 years and risk of all-cause mortality; D. Former smokers quit smoking 10-19 years and risk of all-cause mortality; E. Former smokers quit smoking ≥ 20 years and risk of all-cause mortality).
Cancer mortality
When compared to those who never smoked, the risk for cancer mortality was higher for current smokers who smoked ≥ 10 cigarettes per day than those who smoked < 10 cigarettes per day for breast, melanoma, uterine and non-melanoma skin cancer survivors.
CVD mortality
There were no statistically significant differences between CVD mortality and cigarettes per day for current smokers in other select cancer sites survivors excepted in breast cancer survivors [Figure 4A, 4B Cigarettes per day and risk of all-cause mortality among current smokers. (A) Current smokers smoked < 10 cigarettes per day and risk of all-cause mortality; (B) Current smokers smoked ≥ 10 cigarettes per day and risk of all-cause mortality].
Time since smoking cessations
Figure 4C-E and Table 2 showed that the risk for all-cause mortality was higher for former smokers who had quit more recently than for those who had quit earlier (Ptrend < 0.001). For all-cause mortality, there were obvious dose-response relationships among former smokers as the quit time increased in those diagnosed with non-melanoma skin cancer (Ptrend < 0.001). For cancer mortality, there were no apparent dose-response relationships among former smokers as the quit time increased in any survivor groups. In addition, there was no apparent significant dose-response relationship between former smoking and the risk of CVD mortality [Figure 4C-E Time since smoking cessation and risk of all-cause mortality among former smokers. (C) Former smokers quit smoking < 10 years and risk of all-cause mortality; (D) Former smokers quit smoking 10-19 years and risk of all-cause mortality; (E) Former smokers quit smoking ≥ 20 years and risk of all-cause mortality].
Sensitivity analysis
When deaths within the first 2-years of follow-up were excluded for models examining associations between risk factors and all-cause mortality, the dose-response relationship was apparent for former smokers as the smoking quit time increased in lung cancer survivors (Ptrend < 0.001). Former smoking was associated with a higher risk for cancer mortality among breast (HR = 1.26, 95% CI = 1.04 to 1.54) cancer survivors when compared to those who never smoked. Current smoking was associated with a higher risk for cancer mortality among lung (HR = 1.58, 95% CI = 1.05 to 2.37) and colon (HR = 1.50, 95% CI = 1.06 to 2.13) cancer survivors when compared to those who never smoked. There were no statistically significant differences between former smoking and never smokers for the risk of all-cause mortality in lung cancer survivors. (Detailed in Table 3).
Table 3.
All-cause, cancer, CVD and other cause mortality among cancer survivors by cigarettes per day and time since quitting smoking after excluding individuals who died within the 2 years
| Cancer sites | Smoking status | Subgroups | All cause mortality | Cancer mortality | CVD mortality | Other mortality | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| HR (95% CI) | P valuea | HR (95% CI) | P valuea | HR (95% CI) | P valuea | HR (95% CI) | P valuea | |||
| All sites | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.96 (1.82 to 2.11) | < 0.001 | 1.92 (1.72 to 2.15) | < 0.001 | 1.83 (1.54 to 2.18) | < 0.001 | 2.11 (1.87 to 2.38) | < 0.001 | ||
| < 10 cigarette per day | 1.87 (1.68 to 2.07) | < 0.001 | 1.89 (1.61 to 2.21) | < 0.001 | 1.94 (1.49 to 2.52) | < 0.001 | 1.82 (1.51 to 2.19) | < 0.001 | ||
| ≥ 10 cigarette per day | 2.18 (2.01 to 2.38) | < 0.001 | 2.09 (1.85 to 2.37) | < 0.001 | 1.92 (1.56 to 2.36) | < 0.001 | 2.47 (2.15 to 2.84) | < 0.001 | ||
| Former smoking | 1.31 (1.25 to 1.38) | < 0.001 | 1.36 (1.25 to 1.49) | < 0.001 | 1.09 (0.97 to 8.18) | 0.162 | 1.38 (1.27 to 1.49) | < 0.001 | ||
| Quit smoking < 10 years | 1.84 (1.70 to 1.99) | < 0.001 | 1.89 (1.67 to 2.14) | < 0.001 | 1.57 (1.28 to 1.92) | < 0.001 | 1.91 (1.67 to 2.18) | < 0.001 | ||
| Quit smoking 10-19 years | 1.42 (1.32 to 1.53) | < 0.001 | 1.47 (1.29 to 1.68) | < 0.001 | 1.30 (1.10 to 1.54) | 0.002 | 1.44 (1.28 to 1.62) | < 0.001 | ||
| Quit smoking ≥ 20 years | 1.10 (1.04 to 1.16) | 0.001 | 1.09 (0.98 to 1.21) | 0.133 | 0.89 (0.77 to 1.04) | 0.139 | 1.21 (1.10 to 1.32) | < 0.001 | ||
| P for trend | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||
| Bladder | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.52 (1.09 to 2.11) | 0.013 | 1.72 (0.97 to 3.05) | 0.062 | 1.41 (0.54 to 1.18) | 0.479 | 1.39 (0.82 to 2.36) | 0.216 | ||
| < 10 cigarette per day | 1.47 (0.85 to 2.55) | 0.167 | 2.87 (1.28 to 6.41) | 0.01 | 0.42 (0.09 to 2.05) | 0.282 | 1.05 (0.43 to 2.56) | 0.919 | ||
| ≥ 10 cigarette per day | 1.74 (1.22 to 2.49) | 0.003 | 1.78 (0.93 to 3.40) | 0.079 | 1.76 (0.63 to 2.91) | 0.281 | 1.66 (0.94 to 2.95) | 0.082 | ||
| Former smoking | 1.18 (0.89 to 1.55) | 0.246 | 0.95 (0.57 to 1.57) | 0.828 | 1.59 (0.82 to 4.18) | 0.168 | 1.16 (0.79 to 1.71) | 0.442 | ||
| Quit smoking < 10 years | 1.58 (1.07 to 2.36) | 0.023 | 1.73 (0.90 to 3.34) | 0.102 | 1.26 (0.37 to 2.27) | 0.71 | 1.46 (0.77 to 2.80) | 0.247 | ||
| Quit smoking 10-19 years | 1.30 (0.89 to 1.90) | 0.181 | 0.99 (0.50 to 1.94) | 0.971 | 2.18 (1.01 to 1.71) | 0.048 | 1.19 (0.71 to 1.98) | 0.507 | ||
| Quit smoking ≥ 20 years | 1.06 (0.79 to 1.43) | 0.69 | 0.73 (0.39 to 1.34) | 0.309 | 1.39 (0.66 to 2.93 | 0.388 | 1.16 (0.76 to 1.77) | 0.479 | ||
| P for trend | 0.058 | 0.192 | 0.215 | 0.402 | ||||||
| Breast | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.90 (1.64 to 2.22) | < 0.001 | 1.56 (1.22 to 1.98) | < 0.001 | 1.84 (1.19 to 3.18) | 0.007 | 2.57 (1.99 to 3.32) | < 0.001 | ||
| < 10 cigarette per day | 1.78 (1.43 to 2.21) | < 0.001 | 1.61 (1.15 to 2.26) | 0.005 | 2.01 (1.14 to 2.53) | 0.015 | 1.92 (1.33 to 2.78) | 0.001 | ||
| ≥ 10 cigarette per day | 2.22 (1.83 to 2.69) | < 0.001 | 1.65 (1.22 to 2.24) | 0.001 | 1.91 (1.02 to 2.56) | 0.043 | 3.47 (2.54 to 4.74) | < 0.001 | ||
| Former smoking | 1.30 (1.15 to 1.47) | < 0.001 | 1.26 (1.04 to 1.54) | 0.018 | 0.90 (0.66 to 1.18) | 0.498 | 1.54 (1.27 to 1.85) | < 0.001 | ||
| Quit smoking < 10 years | 1.58 (1.29 to 1.94) | < 0.001 | 1.39 (1.02 to 1.91) | 0.04 | 1.59 (0.98 to 1.60) | 0.062 | 1.92 (1.39 to 2.65) | < 0.001 | ||
| Quit smoking 10-19 years | 1.31 (1.08 to 1.59) | 0.006 | 1.60 (1.18 to 2.18) | 0.003 | 0.88 (0.57 to 1.34) | 0.539 | 1.23 (0.91 to 1.67) | 0.185 | ||
| Quit smoking ≥ 20 years | 1.16 (1.00 to 1.36) | 0.057 | 0.97 (0.74 to 1.29) | 0.847 | 0.69 (0.44 to 1.09) | 0.115 | 1.58 (1.26 to 1.98) | < 0.001 | ||
| P for trend | < 0.001 | 0.003 | 0.554 | 0.129 | ||||||
| Cervix | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.50 (1.80 to 3.48) | < 0.001 | 1.84 (0.99 to 3.42) | 0.055 | 1.53 (0.67 to 1.18) | 0.309 | 3.87 (2.44 to 6.14) | < 0.001 | ||
| < 10 cigarette per day | 2.12 (1.35 to 3.32) | 0.001 | 1.58 (0.67 to 3.72) | 0.299 | 2.38 (0.79 to 3.17) | 0.124 | 2.62 (1.39 to 4.92) | 0.003 | ||
| ≥ 10 cigarette per day | 2.86 (1.98 to 4.13) | < 0.001 | 2.10 (1.10 to 4.00) | 0.024 | 1.19 (0.49 to 4.88) | 0.699 | 4.73 (2.88 to 7.76) | < 0.001 | ||
| Former smoking | 1.61 (1.18 to 2.18) | 0.003 | 1.29 (0.74 to 2.24) | 0.363 | 0.98 (0.50 to 2.18) | 0.95 | 2.30 (1.49 to 3.54) | < 0.001 | ||
| Quit smoking < 10 years | 1.86 (1.29 to 2.66) | 0.001 | 1.43 (0.73 to 2.82) | 0.296 | 1.41 (0.59 to 2.37) | 0.442 | 2.70 (1.62 to 4.49) | < 0.001 | ||
| Quit smoking 10-19 years | 1.94 (1.26 to 3.00) | 0.003 | 1.40 (0.55 to 3.56) | 0.482 | 1.31 (0.40 to 3.22) | 0.655 | 2.72 (1.54 to 4.80) | 0.001 | ||
| Quit smoking ≥ 20 years | 1.27 (0.79 to 2.04) | 0.316 | 1.12 (0.46 to 2.74) | 0.803 | 0.54 (0.21 to 1.35) | 0.187 | 1.88 (0.97 to 3.65) | 0.063 | ||
| P for trend | < 0.001 | 0.264 | 0.295 | 0.006 | ||||||
| Colon | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.51 (1.16 to 1.97) | 0.002 | 1.50 (1.06 to 2.13) | 0.023 | 1.99 (1.04 to 2.18) | 0.038 | 1.44 (0.94 to 2.21) | 0.09 | ||
| < 10 cigarette per day | 1.48 (0.93 to 2.34) | 0.098 | 1.41 (0.83 to 2.40) | 0.203 | 2.51 (1.07 to 2.90) | 0.034 | 1.14 (0.49 to 2.66) | 0.764 | ||
| ≥ 10 cigarette per day | 1.63 (1.23 to 2.15) | 0.001 | 1.56 (1.03 to 2.36) | 0.036 | 1.76 (0.71 to 2.32) | 0.219 | 1.80 (1.12 to 2.91) | 0.016 | ||
| Former smoking | 1.18 (1.01 to 1.39) | 0.039 | 1.26 (0.97 to 1.63) | 0.087 | 1.14 (0.83 to 9.18) | 0.423 | 1.18 (0.89 to 1.56) | 0.249 | ||
| Quit smoking < 10 years | 1.80 (1.29 to 2.52) | 0.001 | 1.43 (0.92 to 2.21) | 0.111 | 1.98 (1.11 to 2.54) | 0.022 | 2.02 (1.22 to 3.36) | 0.007 | ||
| Quit smoking 10-19 years | 1.22 (1.00 to 1.49) | 0.05 | 1.10 (0.75 to 1.61) | 0.627 | 1.22 (0.72 to 1.05) | 0.458 | 1.39 (0.99 to 1.94) | 0.057 | ||
| Quit smoking ≥ 20 years | 1.00 (0.84 to 1.18) | 0.966 | 1.26 (0.95 to 1.66) | 0.108 | 0.91 (0.61 to 1.35) | 0.637 | 0.90 (0.67 to 1.20) | 0.475 | ||
| P for trend | < 0.001 | 0.123 | 0.03 | 0.092 | ||||||
| Lung | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.94 (1.38 to 2.73) | < 0.001 | 1.58 (1.05 to 2.37) | 0.028 | 1.36 (0.34 to 1.18) | 0.667 | 3.91 (2.02 to 7.60) | < 0.001 | ||
| < 10 cigarette per day | 1.79 (1.24 to 2.58) | 0.002 | 1.28 (0.79 to 2.05) | 0.314 | 2.25 (0.56 to 2.96) | 0.249 | 3.80 (1.75 to 8.27) | 0.001 | ||
| ≥ 10 cigarette per day | 2.14 (1.44 to 3.18) | < 0.001 | 1.94 (1.24 to 3.03) | 0.004 | 0.57 (0.08 to 3.02) | 0.573 | 4.22 (1.94 to 9.19) | < 0.001 | ||
| Former smoking | 1.46 (1.11 to 1.92) | 0.006 | 1.17 (0.83 to 1.63) | 0.371 | 1.43 (0.47 to 4.18) | 0.529 | 2.50 (1.45 to 4.32) | 0.001 | ||
| Quit smoking < 10 years | 1.53 (1.13 to 2.06) | 0.006 | 1.20 (0.83 to 1.73) | 0.335 | 1.57 (0.48 to 2.09) | 0.452 | 2.78 (1.50 to 5.14) | 0.001 | ||
| Quit smoking 10-19 years | 1.47 (1.09 to 1.98) | 0.011 | 1.18 (0.78 to 1.78) | 0.439 | 1.62 (0.49 to 1.36) | 0.427 | 2.28 (1.25 to 4.17) | 0.008 | ||
| Quit smoking ≥ 20 years | 1.35 (1.00 to 1.81) | 0.049 | 1.11 (0.76 to 1.61) | 0.6 | 0.80 (0.21 to 3.02) | 0.74 | 2.41 (1.31 to 4.46) | 0.005 | ||
| P for trend | 0.002 | 0.198 | 0.241 | 0.193 | ||||||
| Lymphoma | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.01 (1.39 to 2.91) | < 0.001 | 1.83 (1.08 to 3.10) | 0.026 | 1.00 (0.27 to 4.18) | 0.995 | 2.55 (1.35 to 4.80) | 0.004 | ||
| < 10 cigarette per day | 1.08 (0.59 to 1.98) | 0.8 | 1.04 (0.47 to 2.28) | 0.924 | 0.31 (0.02 to 1.15) | 0.372 | 1.36 (0.41 to 4.52) | 0.619 | ||
| ≥ 10 cigarette per day | 2.59 (1.77 to 3.79) | < 0.001 | 2.38 (1.37 to 4.13) | 0.002 | 1.18 (0.24 to 3.75) | 0.833 | 3.25 (1.60 to 6.62) | 0.001 | ||
| Former smoking | 1.10 (0.82 to 1.47) | 0.537 | 1.06 (0.70 to 1.60) | 0.789 | 1.06 (0.45 to 1.18) | 0.891 | 1.12 (0.69 to 1.82) | 0.632 | ||
| Quit smoking < 10 years | 1.14 (0.70 to 1.83) | 0.603 | 1.19 (0.64 to 2.23) | 0.576 | 0.96 (0.22 to 1.09) | 0.953 | 1.15 (0.47 to 2.81) | 0.766 | ||
| Quit smoking 10-19 years | 1.31 (0.86 to 1.99) | 0.207 | 0.90 (0.45 to 1.79) | 0.755 | 1.56 (0.51 to 1.71) | 0.433 | 1.71 (0.86 to 3.37) | 0.123 | ||
| Quit smoking ≥ 20 years | 1.00 (0.69 to 1.45) | 0.998 | 1.02 (0.62 to 1.69) | 0.934 | 0.82 (0.25 to 2.74) | 0.748 | 0.96 (0.53 to 1.73) | 0.889 | ||
| P for trend | 0.425 | 0.678 | 0.806 | 0.855 | ||||||
| Melanoma | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.08 (1.44 to 3.01) | < 0.001 | 2.39 (1.38 to 4.12) | 0.002 | 1.46 (0.52 to 9.18) | 0.468 | 2.20 (1.25 to 3.86) | 0.006 | ||
| < 10 cigarette per day | 2.87 (1.77 to 4.66) | < 0.001 | 2.25 (1.07 to 4.73) | 0.032 | 3.60 (0.92 to 4.15) | 0.067 | 3.41 (1.47 to 7.88) | 0.004 | ||
| ≥ 10 cigarette per day | 2.02 (1.33 to 3.09) | 0.001 | 2.40 (1.30 to 4.43) | 0.005 | 0.93 (0.30 to 3.87) | 0.904 | 2.36 (1.27 to 4.40) | 0.007 | ||
| Former smoking | 1.29 (1.01 to 1.65) | 0.04 | 1.10 (0.71 to 1.71) | 0.677 | 1.14 (0.69 to 4.18) | 0.603 | 1.48 (1.01 to 2.16) | 0.045 | ||
| Quit smoking < 10 years | 1.98 (1.39 to 2.83) | < 0.001 | 1.07 (0.57 to 2.02) | 0.825 | 1.39 (0.64 to 2.01) | 0.403 | 3.07 (1.88 to 5.01) | < 0.001 | ||
| Quit smoking 10-19 years | 1.24 (0.85 to 1.80) | 0.259 | 1.60 (0.82 to 3.09) | 0.164 | 0.92 (0.42 to 1.03) | 0.841 | 1.10 (0.61 to 1.99) | 0.74 | ||
| Quit smoking ≥ 20 years | 1.09 (0.84 to 1.42) | 0.509 | 0.97 (0.57 to 1.64) | 0.904 | 1.10 (0.61 to 1.99) | 0.761 | 1.15 (0.77 to 1.71) | 0.504 | ||
| P for trend | 0.002 | 0.379 | 0.617 | 0.002 | ||||||
| Prostate | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.91 (1.51 to 2.41) | < 0.001 | 2.14 (1.58 to 2.89) | < 0.001 | 1.43 (0.91 to 4.18) | 0.125 | 1.97 (1.35 to 2.86) | < 0.001 | ||
| < 10 cigarette per day | 1.65 (1.13 to 2.42) | 0.01 | 2.31 (1.60 to 3.33) | < 0.001 | 0.99 (0.42 to 2.34) | 0.979 | 1.41 (0.68 to 2.90) | 0.356 | ||
| ≥ 10 cigarette per day | 2.23 (1.74 to 2.86) | < 0.001 | 2.19 (1.46 to 3.28) | < 0.001 | 2.02 (1.26 to 2.24) | 0.004 | 2.41 (1.63 to 3.56) | < 0.001 | ||
| Former smoking | 1.24 (1.07 to 1.43) | 0.005 | 1.27 (1.00 to 1.61) | 0.05 | 0.98 (0.73 to 1.18) | 0.885 | 1.35 (1.09 to 1.68) | 0.006 | ||
| Quit smoking < 10 years | 1.76 (1.40 to 2.23) | < 0.001 | 1.51 (1.03 to 2.21) | 0.036 | 2.03 (1.22 to 2.38) | 0.007 | 1.85 (1.30 to 2.62) | 0.001 | ||
| Quit smoking 10-19 years | 1.50 (1.22 to 1.83) | < 0.001 | 1.62 (1.18 to 2.24) | 0.003 | 0.96 (0.62 to 1.47) | 0.838 | 1.73 (1.32 to 2.28) | < 0.001 | ||
| Quit smoking ≥ 20 years | 1.08 (0.93 to 1.26) | 0.302 | 1.10 (0.84 to 1.44) | 0.478 | 0.84 (0.63 to 1.12) | 0.224 | 1.20 (0.95 to 1.53) | 0.129 | ||
| P for trend | < 0.001 | 0.002 | 0.068 | 0.036 | ||||||
| Non-melanoma skin | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.39 (1.94 to 2.95) | < 0.001 | 3.09 (2.20 to 4.33) | < 0.001 | 1.89 (1.17 to 3.18) | 0.01 | 2.25 (1.67 to 3.02) | < 0.001 | ||
| < 10 cigarette per day | 2.04 (1.52 to 2.74) | < 0.001 | 2.64 (1.52 to 4.57) | 0.001 | 1.94 (0.98 to 2.87) | 0.059 | 1.81 (1.17 to 2.82) | 0.009 | ||
| ≥ 10 cigarette per day | 2.69 (2.10 to 3.45) | < 0.001 | 3.52 (2.41 to 5.13) | < 0.001 | 1.82 (1.02 to 3.24) | 0.043 | 2.60 (1.83 to 3.70) | < 0.001 | ||
| Former smoking | 1.32 (1.17 to 1.50) | < 0.001 | 1.47 (1.12 to 1.94) | 0.006 | 1.13 (0.84 to 1.18) | 0.417 | 1.35 (1.12 to 1.63) | 0.002 | ||
| Quit smoking < 10 years | 1.92 (1.52 to 2.44) | < 0.001 | 2.63 (1.78 to 3.89) | < 0.001 | 1.22 (0.64 to 2.30) | 0.543 | 1.91 (1.36 to 2.68) | < 0.001 | ||
| Quit smoking 10-19 years | 1.68 (1.39 to 2.04) | < 0.001 | 1.66 (1.05 to 2.63) | 0.029 | 1.84 (1.23 to 2.76) | 0.003 | 1.63 (1.23 to 2.17) | 0.001 | ||
| Quit smoking ≥ 20 years | 1.14 (0.99 to 1.31) | 0.072 | 1.17 (0.85 to 1.61) | 0.322 | 0.96 (0.69 to 1.35) | 0.826 | 1.21 (0.98 to 1.49) | 0.08 | ||
| P for trend | < 0.001 | < 0.001 | 0.061 | 0.001 | ||||||
| Uterine | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.93 (2.19 to 3.92) | < 0.001 | 2.91 (1.69 to 5.00) | < 0.001 | 2.84 (1.56 to 2.18) | 0.001 | 3.08 (2.08 to 4.57) | < 0.001 | ||
| < 10 cigarette per day | 2.93 (1.89 to 4.54) | < 0.001 | 2.78 (1.29 to 5.96) | 0.009 | 1.71 (0.76 to 4.88) | 0.195 | 3.64 (2.00 to 6.62) | < 0.001 | ||
| ≥ 10 cigarette per day | 3.00 (2.15 to 4.16) | < 0.001 | 3.36 (1.79 to 6.31) | < 0.001 | 3.66 (1.82 to 4.35) | < 0.001 | 2.75 (1.75 to 4.31) | < 0.001 | ||
| Former smoking | 1.26 (0.98 to 1.61) | 0.068 | 1.28 (0.80 to 2.06) | 0.308 | 0.92 (0.53 to 3.18) | 0.747 | 1.44 (1.03 to 2.02) | 0.032 | ||
| Quit smoking < 10 years | 1.26 (0.85 to 1.87) | 0.246 | 1.86 (0.88 to 3.93) | 0.105 | 0.43 (0.16 to 1.17) | 0.098 | 1.50 (0.83 to 2.71) | 0.18 | ||
| Quit smoking 10-19 years | 1.44 (0.96 to 2.15) | 0.079 | 2.19 (1.16 to 4.13) | 0.015 | 0.90 (0.34 to 2.39) | 0.83 | 1.41 (0.81 to 2.45) | 0.221 | ||
| Quit smoking ≥ 20 years | 1.14 (0.83 to 1.58) | 0.422 | 0.61 (0.29 to 1.32) | 0.209 | 1.14 (0.60 to 2.18) | 0.695 | 1.38 (0.90 to 2.14) | 0.143 | ||
| P for trend | 0.042 | 0.032 | 0.352 | 0.293 | ||||||
Abbreviations: CVD = cardiovascular disease; CI = confidence interval; HR = hazard ratio, CHD = coronary heart disease.
Adjusted for age, sex, race, education level, marital status, body mass index, physical activity, alcohol intake, income level, self-rated health, history of hypertension, diabetes, CHD, stroke and duration of cancer.
Excluding patients with a CVD history, there was a 57% increase in all-cause mortality among former smokers who were diagnosed with bladder cancer and a 91% increase in CVD mortality among all cancer survivors when compared to never smokers. Current smoking was associated with a higher risk for cancer mortality in bladder (HR = 2.12, 95% CI = 1.05 to 4.30) and colon (HR = 1.49, 95% CI = 1.03 to 2.15) cancer survivors when compared to those who never smoked. (Detailed in Table 4).
Table 4.
All-cause, cancer, CVD and other cause mortality among cancer survivors by cigarettes per day and time since quitting smoking after excluding participants with CVD history
| Cancer sites | Smoking status | Subgroups | All cause mortality | Cancer mortality | CVD mortality | Other mortality | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| HR (95% CI) | P valuea | HR (95% CI) | P valuea | HR (95% CI) | P valuea | HR (95% CI) | P valuea | |||
| All cancer sites | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.87 (1.72 to 2.02) | < 0.001 | 1.72 (1.51 to 1.94) | < 0.001 | 1.91 (1.57 to 2.33) | < 0.001 | 2.09 (1.82 to 2.38) | < 0.001 | ||
| < 10 cigarette per day | 1.77 (1.56 to 2.00) | < 0.001 | 1.69 (1.42 to 2.02) | < 0.001 | 1.97 (1.45 to 2.67) | < 0.001 | 1.77 (1.43 to 2.20) | < 0.001 | ||
| ≥ 10 cigarette per day | 2.06 (1.87 to 2.26) | < 0.001 | 1.85 (1.61 to 2.14) | < 0.001 | 1.99 (1.57 to 2.52) | < 0.001 | 2.40 (2.06 to 2.80) | < 0.001 | ||
| Former smoking | 1.34 (1.26 to 1.42) | < 0.001 | 1.39 (1.26 to 1.53) | < 0.001 | 1.18 (1.57 to 1.37) | 0.025 | 1.35 (1.23 to 1.48) | < 0.001 | ||
| Quit smoking < 10 years | 1.86 (1.72 to 2.01) | < 0.001 | 1.88 (1.65 to 2.15) | < 0.001 | 1.74 (1.39 to 2.18) | < 0.001 | 1.80 (1.59 to 2.04) | < 0.001 | ||
| Quit smoking 10-19 years | 1.42 (1.30 to 1.55) | < 0.001 | 1.46 (1.27 to 1.67) | < 0.001 | 1.32 (1.08 to 1.63) | 0.008 | 1.44 (1.25 to 1.67) | < 0.001 | ||
| Quit smoking ≥ 20 years | 1.11 (1.04 to 1.19) | 0.003 | 1.10 (0.98 to 1.23) | 0.106 | 0.98 (0.81 to 1.18) | 0.814 | 1.18 (1.05 to 1.32) | 0.004 | ||
| P for trend | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||
| Bladder | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.58 (1.06 to 2.37) | 0.026 | 2.12 (1.05 to 4.30) | 0.036 | 1.64 (0.44 to 6.22) | 0.462 | 1.23 (1.65 to 2.31) | 0.52 | ||
| < 10 cigarette per day | 1.37 (0.62 to 3.00) | 0.433 | 2.32 (0.64 to 8.41) | 0.2 | 0.88 (0.11 to 7.08) | 0.903 | 0.90 (0.27 to 3.02) | 0.864 | ||
| ≥ 10 cigarette per day | 1.89 (1.24 to 2.88) | 0.003 | 2.32 (1.14 to 4.73) | 0.021 | 2.09 (0.56 to 7.83) | 0.273 | 1.51 (0.77 to 2.93) | 0.226 | ||
| Former smoking | 1.57 (1.13 to 2.18) | 0.007 | 1.65 (0.90 to 3.03) | 0.107 | 1.96 (0.72 to 5.37) | 0.19 | 1.39 (0.89 to 2.17) | 0.151 | ||
| Quit smoking < 10 years | 2.21 (1.37 to 3.56) | 0.001 | 2.87 (1.32 to 6.20) | 0.008 | 1.64 (0.39 to 6.88) | 0.499 | 1.71 (0.78 to 3.73) | 0.176 | ||
| Quit smoking 10-19 years | 1.47 (0.92 to 2.34) | 0.104 | 1.40 (0.66 to 2.97) | 0.372 | 1.52 (0.43 to 5.33) | 0.51 | 1.33 (0.73 to 2.41) | 0.347 | ||
| Quit smoking ≥ 20 years | 1.62 (1.13 to 2.32) | 0.009 | 1.23 (0.60 to 2.50) | 0.568 | 2.51 (0.91 to 6.91) | 0.075 | 1.55 (0.92 to 2.62) | 0.099 | ||
| P for trend | 0.009 | 0.002 | 0.636 | 0.983 | ||||||
| Breast | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.78 (1.50 to 2.11) | < 0.001 | 1.36 (1.05 to 1.75) | 0.02 | 1.69 (1.01 to 2.80) | 0.044 | 2.87 (2.09 to 3.94) | < 0.001 | ||
| < 10 cigarette per day | 1.62 (1.26 to 2.07) | < 0.001 | 1.36 (0.95 to 1.94) | 0.095 | 2.06 (1.06 to 3.99) | 0.034 | 1.98 (1.28 to 3.07) | 0.002 | ||
| ≥ 10 cigarette per day | 2.11 (1.69 to 2.62) | < 0.001 | 1.45 (1.05 to 2.00) | 0.025 | 1.71 (0.85 to 3.46) | 0.131 | 4.06 (2.77 to 5.95) | < 0.001 | ||
| Former smoking | 1.27 (1.11 to 1.45) | 0.001 | 1.21 (0.99 to 1.47) | 0.06 | 0.88 (0.62 to 1.27) | 0.507 | 1.53 (1.23 to 1.92) | < 0.001 | ||
| Quit smoking < 10 years | 1.46 (1.16 to 1.84) | 0.002 | 1.21 (0.87 to 1.69) | 0.249 | 2.04 (1.17 to 3.58) | 0.012 | 1.69 (1.10 to 2.59) | 0.016 | ||
| Quit smoking 10-19 years | 1.23 (0.99 to 1.53) | 0.059 | 1.50 (1.10 to 2.04) | 0.011 | 0.83 (0.48 to 1.44) | 0.509 | 1.13 (0.77 to 1.64) | 0.534 | ||
| Quit smoking ≥ 20 years | 1.19 (1.00 to 1.42) | 0.049 | 1.01 (0.76 to 1.35) | 0.93 | 0.58 (0.32 to 1.05) | 0.074 | 1.70 (1.32 to 2.19) | < 0.001 | ||
| P for trend | 0.001 | 0.04 | 0.303 | 0.449 | ||||||
| Cervix | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.72 (1.87 to 3.97) | < 0.001 | 1.89 (0.96 to 3.71) | 0.067 | 3.01 (1.32 to 6.88) | 0.009 | 3.73 (2.18 to 6.38) | < 0.001 | ||
| < 10 cigarette per day | 2.17 (1.27 to 3.71) | 0.005 | 1.65 (0.64 to 4.22) | 0.296 | 4.26 (1.49 to 12.18) | 0.007 | 2.18 (0.99 to 4.81) | 0.054 | ||
| ≥ 10 cigarette per day | 3.17 (2.13 to 4.72) | < 0.001 | 2.15 (1.05 to 4.38) | 0.035 | 2.63 (1.04 to 6.65) | 0.041 | 4.55 (2.61 to 7.96) | < 0.001 | ||
| Former smoking | 2.08 (1.48 to 2.92) | < 0.001 | 1.70 (0.99 to 2.94) | 0.056 | 1.91 (0.91 to 4.02) | 0.087 | 2.72 (1.65 to 4.49) | < 0.001 | ||
| Quit smoking < 10 years | 2.17 (1.44 to 3.27) | < 0.001 | 1.82 (0.92 to 3.59) | 0.085 | 1.89 (0.63 to 5.69) | 0.256 | 2.83 (1.58 to 5.07) | < 0.001 | ||
| Quit smoking 10-19 years | 2.39 (1.46 to 3.92) | 0.001 | 1.95 (0.79 to 4.80) | 0.146 | 5.17 (1.64 to 16.29) | 0.005 | 2.21 (1.06 to 4.63) | 0.036 | ||
| Quit smoking ≥ 20 years | 1.93 (1.15 to 3.24) | 0.013 | 1.49 (0.59 to 3.74) | 0.399 | 0.74 (0.23 to 2.41) | 0.617 | 3.08 (1.49 to 6.35) | 0.002 | ||
| P for trend | < 0.001 | 0.091 | 0.003 | 0.01 | ||||||
| Colon | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.57 (1.19 to 2.06) | 0.001 | 1.49 (1.03 to 2.15) | 0.032 | 2.60 (1.32 to 5.10) | 0.006 | 1.41 (0.88 to 2.24) | 0.151 | ||
| < 10 cigarette per day | 1.45 (0.88 to 2.40) | 0.148 | 1.56 (0.91 to 2.69) | 0.106 | 3.20 (1.20 to 8.55) | 0.021 | 0.78 (0.23 to 2.59) | 0.683 | ||
| ≥ 10 cigarette per day | 1.64 (1.25 to 2.16) | < 0.001 | 1.43 (0.92 to 2.22) | 0.108 | 2.33 (1.05 to 5.19) | 0.038 | 1.84 (1.13 to 3.02) | 0.015 | ||
| Former smoking | 1.13 (0.96 to 1.32) | 0.137 | 1.22 (0.94 to 1.60) | 0.139 | 1.48 (0.98 to 2.24) | 0.066 | 0.95 (0.72 to 1.25) | 0.709 | ||
| Quit smoking < 10 years | 1.33 (1.03 to 1.73) | 0.03 | 1.24 (0.78 to 1.97) | 0.358 | 2.27 (1.12 to 4.56) | 0.022 | 1.09 (0.69 to 1.72) | 0.708 | ||
| Quit smoking 10-19 years | 1.25 (1.01 to 1.54) | 0.042 | 1.13 (0.76 to 1.66) | 0.545 | 1.43 (0.77 to 2.64) | 0.255 | 1.31 (0.92 to 1.87) | 0.128 | ||
| Quit smoking ≥ 20 years | 1.02 (0.84 to 1.24) | 0.873 | 1.26 (0.94 to 1.68) | 0.116 | 1.28 (0.78 to 2.10) | 0.319 | 0.78 (0.55 to 1.10) | 0.158 | ||
| P for trend | 0.004 | 0.263 | 0.011 | 0.919 | ||||||
| Lung | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.82 (1.31 to 2.52) | < 0.001 | 1.36 (0.92 to 2.01) | 0.124 | 1.56 (0.32 to 7.71) | 0.582 | 4.82 (2.38 to 9.77) | < 0.001 | ||
| < 10 cigarette per day | 1.67 (1.16 to 2.40) | 0.006 | 1.14 (0.73 to 1.78) | 0.576 | 2.16 (0.35 to 13.39) | 0.407 | 5.00 (2.22 to 11.25) | < 0.001 | ||
| ≥ 10 cigarette per day | 2.06 (1.40 to 3.01) | < 0.001 | 1.70 (1.09 to 2.67) | 0.02 | 1.00 (0.14 to 6.94) | 0.996 | 4.96 (2.12 to 11.60) | < 0.001 | ||
| Former smoking | 1.42 (1.09 to 1.86) | 0.01 | 1.15 (0.83 to 1.59) | 0.405 | 1.87 (0.59 to 5.91) | 0.287 | 2.50 (1.37 to 4.54) | 0.003 | ||
| Quit smoking < 10 years | 1.49 (1.11 to 2.01) | 0.008 | 1.18 (0.82 to 1.68) | 0.368 | 2.37 (0.74 to 7.54) | 0.145 | 2.92 (1.50 to 5.68) | 0.002 | ||
| Quit smoking 10-19 years | 1.44 (1.06 to 1.95) | 0.019 | 1.27 (0.86 to 1.89) | 0.232 | 1.72 (0.44 to 6.65) | 0.432 | 2.12 (1.05 to 4.27) | 0.035 | ||
| Quit smoking ≥ 20 years | 1.27 (0.92 to 1.77) | 0.145 | 1.02 (0.68 to 1.52) | 0.933 | 1.23 (0.29 to 5.24) | 0.777 | 2.39 (1.18 to 4.82) | 0.015 | ||
| P for trend | 0.008 | 0.201 | 0.083 | 0.225 | ||||||
| Lymphoma | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.66 (1.09 to 2.51) | 0.017 | 1.40 (0.83 to 2.37) | 0.211 | 1.99 (0.52 to 7.54) | 0.313 | 2.61 (1.21 to 5.67) | 0.015 | ||
| < 10 cigarette per day | 0.61 (0.29 to 1.27) | 0.185 | 0.61 (0.26 to 1.44) | 0.258 | 0.79 (0.09 to 6.98) | 0.829 | 0.60 (0.10 to 3.65) | 0.577 | ||
| ≥ 10 cigarette per day | 2.23 (1.45 to 3.41) | < 0.001 | 1.91 (1.11 to 3.28) | 0.02 | 1.81 (0.35 to 9.25) | 0.477 | 3.41 (1.47 to 7.88) | 0.004 | ||
| Former smoking | 1.07 (0.77 to 1.49) | 0.701 | 1.05 (0.67 to 1.64) | 0.837 | 1.39 (0.49 to 3.93) | 0.529 | 1.14 (0.65 to 2.02) | 0.644 | ||
| Quit smoking < 10 years | 1.02 (0.59 to 1.76) | 0.949 | 1.12 (0.59 to 2.10) | 0.73 | 0.96 (0.12 to 7.45) | 0.971 | 0.95 (0.34 to 2.70) | 0.929 | ||
| Quit smoking 10-19 years | 1.29 (0.83 to 2.01) | 0.257 | 1.02 (0.51 to 2.04) | 0.955 | 1.96 (0.51 to 7.61) | 0.327 | 1.79 (0.78 to 4.15) | 0.171 | ||
| Quit smoking ≥ 20 years | 0.99 (0.65 to 1.49) | 0.945 | 0.98 (0.57 to 1.70) | 0.955 | 1.33 (0.34 to 5.17) | 0.675 | 0.89 (0.43 to 1.83) | 0.742 | ||
| P for trend | 0.744 | 0.868 | 0.636 | 0.86 | ||||||
| Melanoma | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.23 (1.48 to 3.36) | < 0.001 | 2.08 (1.12 to 3.83) | 0.02 | 1.90 (0.52 to 6.98) | 0.33 | 2.49 (1.32 to 4.70) | 0.005 | ||
| < 10 cigarette per day | 3.09 (1.70 to 5.60) | < 0.001 | 1.78 (0.69 to 4.58) | 0.229 | 6.93 (1.40 to 34.28) | 0.018 | 3.90 (1.53 to 9.95) | 0.005 | ||
| ≥ 10 cigarette per day | 2.20 (1.42 to 3.40) | < 0.001 | 2.13 (1.08 to 4.21) | 0.029 | 0.89 (0.17 to 4.60) | 0.894 | 2.65 (1.37 to 5.13) | 0.004 | ||
| Former smoking | 1.33 (1.01 to 1.76) | 0.046 | 1.34 (0.81 to 2.21) | 0.249 | 1.50 (0.84 to 2.67) | 0.172 | 1.26 (0.80 to 2.01) | 0.32 | ||
| Quit smoking < 10 years | 1.52 (0.98 to 2.36) | 0.061 | 1.30 (0.65 to 2.60) | 0.453 | 1.21 (0.40 to 3.71) | 0.736 | 1.76 (0.86 to 3.60) | 0.118 | ||
| Quit smoking 10-19 years | 1.41 (0.93 to 2.14) | 0.108 | 1.80 (0.87 to 3.73) | 0.111 | 0.88 (0.28 to 2.81) | 0.83 | 1.30 (0.69 to 2.42) | 0.417 | ||
| Quit smoking ≥ 20 years | 1.27 (0.93 to 1.73) | 0.127 | 1.23 (0.69 to 2.18) | 0.487 | 1.76 (0.93 to 3.34) | 0.084 | 1.15 (0.68 to 1.93) | 0.6 | ||
| P for trend | 0.059 | 0.25 | 0.741 | 0.748 | ||||||
| Prostate | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 1.86 (1.45 to 2.39) | < 0.001 | 1.82 (1.28 to 2.57) | 0.001 | 1.51 (0.87 to 2.60) | 0.14 | 2.02 (1.34 to 3.03) | 0.001 | ||
| < 10 cigarette per day | 1.84 (1.30 to 2.60) | 0.001 | 2.11 (1.31 to 3.38) | 0.002 | 0.95 (0.32 to 2.81) | 0.927 | 1.81 (0.90 to 3.60) | 0.094 | ||
| ≥ 10 cigarette per day | 2.02 (1.49 to 2.74) | < 0.001 | 1.81 (1.16 to 2.82) | 0.009 | 2.05 (1.13 to 3.73) | 0.019 | 2.14 (1.29 to 3.55) | 0.003 | ||
| Former smoking | 1.21 (1.04 to 1.41) | 0.014 | 1.24 (0.96 to 1.61) | 0.104 | 1.07 (0.76 to 1.51) | 0.701 | 1.24 (0.98 to 1.57) | 0.071 | ||
| Quit smoking < 10 years | 1.75 (1.39 to 2.20) | < 0.001 | 1.58 (1.06 to 2.36) | 0.024 | 2.37 (1.36 to 4.13) | 0.002 | 1.61 (1.13 to 2.31) | 0.009 | ||
| Quit smoking 10-19 years | 1.58 (1.25 to 1.99) | < 0.001 | 1.54 (1.05 to 2.27) | 0.029 | 0.92 (0.49 to 1.74) | 0.805 | 1.93 (1.41 to 2.63) | < 0.001 | ||
| Quit smoking ≥ 20 years | 1.03 (0.87 to 1.21) | 0.748 | 1.06 (0.80 to 1.42) | 0.673 | 0.90 (0.61 to 1.31) | 0.574 | 1.04 (0.80 to 1.36) | 0.766 | ||
| P for trend | < 0.001 | 0.004 | 0.026 | 0.168 | ||||||
| Non-melanoma skin | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 2.34 (1.84 to 2.96) | < 0.001 | 3.68 (2.49 to 5.44) | < 0.001 | 1.89 (1.09 to 3.28) | 0.024 | 1.92 (1.37 to 2.69) | < 0.001 | ||
| < 10 cigarette per day | 1.85 (1.30 to 2.63) | 0.001 | 3.09 (1.72 to 5.54) | < 0.001 | 1.60 (0.74 to 3.46) | 0.235 | 1.39 (0.80 to 2.42) | 0.242 | ||
| ≥ 10 cigarette per day | 2.75 (2.07 to 3.65) | < 0.001 | 4.30 (2.77 to 6.69) | < 0.001 | 2.02 (1.01 to 4.04) | 0.047 | 2.35 (1.59 to 3.47) | < 0.001 | ||
| Former smoking | 1.39 (1.19 to 1.63) | < 0.001 | 1.87 (1.35 to 2.57) | < 0.001 | 1.10 (0.77 to 1.58) | 0.588 | 1.31 (1.04 to 1.65) | 0.022 | ||
| Quit smoking < 10 years | 2.27 (1.75 to 2.94) | < 0.001 | 3.47 (2.23 to 5.40) | < 0.001 | 1.66 (0.85 to 3.26) | 0.138 | 1.99 (1.36 to 2.93) | < 0.001 | ||
| Quit smoking 10-19 years | 1.77 (1.38 to 2.26) | < 0.001 | 2.18 (1.30 to 3.66) | 0.003 | 1.69 (0.99 to 2.87) | 0.054 | 1.60 (1.12 to 2.30) | 0.01 | ||
| Quit smoking ≥ 20 years | 1.13 (0.95 to 1.35) | 0.171 | 1.40 (0.96 to 2.04) | 0.077 | 0.88 (0.58 to 1.35) | 0.564 | 1.12 (0.86 to 1.46) | 0.394 | ||
| P for trend | < 0.001 | < 0.001 | 0.05 | 0.003 | ||||||
| Uterine | ||||||||||
| Never smoking | 1 (Reference) | 1 (Reference) | 1 (Reference) | 1 (Reference) | ||||||
| Current smoking | 3.44 (2.48 to 4.78) | < 0.001 | 3.17 (1.84 to 5.46) | < 0.001 | 3.49 (1.52 to 8.04) | 0.003 | 3.62 (2.27 to 5.79) | < 0.001 | ||
| < 10 cigarette per day | 3.39 (2.04 to 5.64) | < 0.001 | 2.36 (1.01 to 5.54) | 0.048 | 2.58 (0.86 to 7.75) | 0.09 | 4.36 (2.22 to 8.58) | < 0.001 | ||
| ≥ 10 cigarette per day | 3.55 (2.50 to 5.06) | < 0.001 | 4.17 (2.16 to 8.05) | < 0.001 | 4.17 (1.63 to 10.70) | 0.003 | 3.16 (1.90 to 5.24) | < 0.001 | ||
| Former smoking | 1.33 (1.00 to 1.78) | 0.053 | 1.33 (0.81 to 2.19) | 0.26 | 1.16 (0.64 to 2.11) | 0.615 | 1.40 (0.93 to 2.11) | 0.104 | ||
| Quit smoking < 10 years | 1.17 (0.69 to 2.00) | 0.556 | 1.67 (0.71 to 3.91) | 0.235 | 0.30 (0.06 to 1.45) | 0.134 | 1.36 (0.66 to 2.80) | 0.41 | ||
| Quit smoking 10-19 years | 1.65 (1.07 to 2.52) | 0.022 | 2.25 (1.11 to 4.56) | 0.025 | 1.92 (0.73 to 5.01) | 0.184 | 1.34 (0.70 to 2.54) | 0.379 | ||
| Quit smoking ≥ 20 years | 1.22 (0.81 to 1.81) | 0.338 | 0.72 (0.30 to 1.70) | 0.455 | 1.31 (0.62 to 2.78) | 0.479 | 1.40 (0.82 to 2.37) | 0.215 | ||
| P for trend | 0.097 | 0.058 | 0.868 | 0.301 | ||||||
Abbreviations: CVD = cardiovascular disease; CI = confidence interval; HR = hazard ratio, CHD = coronary heart disease.
Adjusted for age, sex, race, education level, marital status, body mass index, physical activity, alcohol intake, income level, self-rated health, history of hypertension, diabetes, CHD, stroke and duration of cancer.
Discussion
This large prospective study showed that cancer survivors who reported being current or former smokers had a higher risk for all-cause and cancer mortality when compared with those who never smoked, but effects varied substantially by cancer site, especially for breast, prostate, and non-melanoma skin cancer survivors. Compared to nonsmokers, risk of CVD mortality increased among current smokers diagnosed with breast, non-melanoma skin and uterine cancer. However, there were no differences between former and never smokers for CVD mortality. Also, smoking cessation appears to benefit those with longer quit times as observed by the decreasing risk of mortality, especially for non-melanoma skin cancer survivors.
In the present study, we observed that current or former smokers had a higher risk of all-cause mortality when compared to nonsmokers among cancer survivors, similar to what was observed in a recent study [28]. The associations observed here between smoking status and all-cause mortality among colon and prostate cancer survivors was lower than what was observed elsewhere [13,19]. The difference might be explained by the statistical methods such as adjusting for lag time, family history of colon cancer, tumor stage and first course of cancer treatment in our models. Our study sheds new insight on the relationships between smoking status and all-cause mortality for bladder, lymphoma, melanoma, uterine and non-melanoma skin cancer survivors. In effort to advance our understanding of these relationships, future studies should consider examining the relationship smoking and mortality among various cancer survivor populations.
Previous studies have indicated that breast cancer survivors who report varying smoking histories have the same risk for cancer mortality [29]. However, here, we observed a different pattern of relationships. In particular, current smokers had higher risk for cancer mortality than never smokers. Similar associations were observed for prostate cancer survivors, with our study showing higher hazard ratios than what was observed in another prospective cohort study [14]. Conversely, we did not observe significant associations in cervical survivors, a finding which differs from what others have reported [21].
In our study, there was no dose-response relationships between duration of smoking cessation and risk of cancer mortality in prostate cancer survivors, consistent with a previous study [14], but a greater number of cigarettes per day was associated with a significantly increased risk of all-cause mortality. Significant dose-response association for breast cancer mortality was observed for number of cigarettes smoked per day (≤ 5, 6-10, 11-15 and ≥ 16) [30]. In particular, our study found the risk of all-cause and cancer mortality increased as the cigarettes per day increased (< 10 and ≥ 10). Besides, current smoking had the highest risk of all-cause mortality with daily cigarette consumption among cervical cancer survivors for cancer mortality, but another study found that both moderate and high daily cigarette consumption resulted in the highest risk for cervical cancer mortality [21]. We did not found any significant association between number of cigarettes per day and cancer mortality among colon cancer survivors, which differs from a previous study [13]. The dose-response relationship between duration of smoking cessation or cigarettes per day and risk of all-cause mortality was significant among non-melanoma skin cancer survivors, which was not reported previously.
Several potential mechanisms could contribute to the associations we observed between smoking and increased risk of all-cause mortality. In particular, smoking decreases the effectiveness of cancer treatments [31-33]. Studies have also shown that smoking increases the probability of recurrence and distant metastases [34,35] and increases the risk for second primary tumors [36], and premature mortality in cancer survivors [37,38].
Among survivors, we also observed a higher risk for CVD mortality. Several pathways might explain these associations. For example, smoking activates several CVD-relevant inflammatory markers, which lead to a significant shift toward a prothrombotic, procoagulative state, and release of pro-oxidant enzymes in the vascular wall by activating the nuclear factor-kB cascade [39]. The increase in reactive oxygen species and oxidant-generating systems induced by smoking leads to both systemic and local immune system activation [40,41]. Systemic inflammation is supported by upregulating the expression of various matrix metalloproteinases and proinflammatory cytokines among smokers. Tumor necrosis factor-α and interleukin-1β maintain sustained activation of nuclear factor-kB, perpetuating the inflammatory response in smokers [42]. Besides, nicotine also stimulates growth of advanced atherosclerotic lesions by increasing lesion vascularization [43] and smoking and/or nicotine might also accelerate atherosclerosis in other ways [44].
Limitations
Our study’s strengths include a prospective design, a large number of cancer cases and examining the associations between active smoking and risk of all-cause and disease-specific mortality. Information on smoking and other essential covariates was prospectively collected and updated periodically. However, there were several limitations. Firstly, smoking status was self-reported and assessed post-diagnosis, which may limit the risk difference comparison between pre-diagnosis and post-diagnosis smoking as well as be subject to recall and reporting biases. In addition, because of the nature of an observational study, causality cannot be established. Given that we have no information on passive smoking among non-smokers, the present risk estimate for the association between smoking and mortality may have been underestimated.
Implications for clinicians
The prevalence of smoking among cancer patients is still higher than expected since [45] smoking is detrimental to cancer therapy and survival [31,32,34-37]. Our data provides compelling evidence that smoking increases the risk of all-cause and cause-specific mortality among cancer survivors. Thus clinicians should provide survivors with care guidelines that promote smoking cessation as a crucial strategy for improving survival outcomes, especially since quit time was associated with mortality. The association between smoking and CVD mortality risk in select groups deserve further attention and has clinical implications for many as a reasonable proportion of survivors die of CVD. Thus, there is a need for strategies to manage CVD risk factors throughout the cancer continuum.
Conclusions
Post-diagnosis smoking was associated with increased all-cause, cancer and CVD mortality among cancer survivors, with varying associations depending on the survivor population. Dose-response associations of quit time for former smokers were obvious among all cancer survivors, especially in non-melanoma skin cancer survivors. Further research is needed to understand mechanisms whereby smoking may increase colorectal cancer-specific mortality and determine whether quit time after diagnosis lowers the risk of colorectal cancer-specific mortality.
Acknowledgements
We greatly appreciate the support from other members of the study team who provided their generous contribution of time and efforts help during the research and the help from Chengye Li for commenting on the manuscript. This study was not funded by any funding agencies in the public, commercial, or not-for-profit sectors. The study was funded by the National Natural Science Foundation of China (Grant No. 81773552) and the National Key Research and Development Program of China (No. 2018YFC1315302, 2017YFC1200502).
Disclosure of conflict of interest
None.
References
- 1.de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, Forsythe L, Scoppa S, Hachey M, Rowland JH. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwangbo Y, Kang D, Kang M, Kim S, Lee EK, Kim YA, Chang YJ, Choi KS, Jung SY, Woo SM, Ahn JS, Sim SH, Hong YS, Pastor-Barriuso R, Guallar E, Lee ES, Kong SY, Cho J. Incidence of diabetes after cancer development: a Korean national cohort study. JAMA Oncol. 2018;4:1099–1105. doi: 10.1001/jamaoncol.2018.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coviello JS. Cardiovascular and cancer risk: the role of cardio-oncology. J Adv Pract Oncol. 2018;9:160–176. [PMC free article] [PubMed] [Google Scholar]
- 4.Armenian SH, Xu L, Ky B, Sun C, Farol LT, Pal SK, Douglas PS, Bhatia S, Chao C. Cardiovascular disease among survivors of adult-onset cancer: a community-based retrospective cohort study. J. Clin. Oncol. 2016;34:1122–1130. doi: 10.1200/JCO.2015.64.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warren GW, Dibaj S, Hutson A, Cummings KM, Dresler C, Marshall JR. Identifying targeted strategies to improve smoking cessation support for cancer patients. J Thorac Oncol. 2015;10:1532–1537. doi: 10.1097/JTO.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 6.Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243–274. doi: 10.3322/caac.21142. [DOI] [PubMed] [Google Scholar]
- 7.Schuller HM. Is cancer triggered by altered signalling of nicotinic acetylcholine receptors? Nat Rev Cancer. 2009;9:195–205. doi: 10.1038/nrc2590. [DOI] [PubMed] [Google Scholar]
- 8.Singh S, Pillai S, Chellappan S. Nicotinic acetylcholine receptor signaling in tumor growth and metastasis. J Oncol. 2011;2011:456743. doi: 10.1155/2011/456743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schaal C, Chellappan SP. Nicotine-mediated cell proliferation and tumor progression in smoking-related cancers. Mol Cancer Res. 2014;12:14–23. doi: 10.1158/1541-7786.MCR-13-0541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Price SN, Studts JL, Hamann HA. Tobacco use assessment and treatment in cancer patients: a scoping review of oncology care clinician adherence to clinical practice guidelines in the U.S. Oncologist. 2019;24:229–238. doi: 10.1634/theoncologist.2018-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the national institutes of health-AARP diet and health study. JAMA Intern Med. 2017;177:87–95. doi: 10.1001/jamainternmed.2016.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taghizadeh N, Vonk JM, Boezen HM. Lifetime smoking history and cause-specific mortality in a cohort study with 43 years of follow-up. PLoS One. 2016;11:e0153310. doi: 10.1371/journal.pone.0153310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang B, Jacobs EJ, Gapstur SM, Stevens V, Campbell PT. Active smoking and mortality among colorectal cancer survivors: the Cancer Prevention Study II nutrition cohort. J. Clin. Oncol. 2015;33:885–893. doi: 10.1200/JCO.2014.58.3831. [DOI] [PubMed] [Google Scholar]
- 14.Kenfield SA, Stampfer MJ, Chan JM, Giovannucci E. Smoking and prostate cancer survival and recurrence. JAMA. 2011;305:2548–2555. doi: 10.1001/jama.2011.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parajuli R, Bjerkaas E, Tverdal A, Le Marchand L, Weiderpass E, Gram IT. Cigarette smoking and colorectal cancer mortality among 602,242 Norwegian males and females. Clin Epidemiol. 2014;6:137–145. doi: 10.2147/CLEP.S58722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharp L, McDevitt J, Brown C, Comber H. Smoking at diagnosis significantly decreases 5-year cancer-specific survival in a population-based cohort of 18 166 colon cancer patients. Aliment Pharmacol Ther. 2017;45:788–800. doi: 10.1111/apt.13944. [DOI] [PubMed] [Google Scholar]
- 17.Sharp L, McDevitt J, Brown C, Carsin AE, Comber H. Association between smoking at diagnosis and cause-specific survival in patients with rectal cancer: results from a population-based analysis of 10,794 cases. Cancer. 2017;123:2543–2550. doi: 10.1002/cncr.30583. [DOI] [PubMed] [Google Scholar]
- 18.Praestegaard C, Jensen A, Jensen SM, Nielsen TS, Webb PM, Nagle CM, DeFazio A Australian Ovarian Cancer Study Group; Hogdall E, Rossing MA, Doherty JA, Wicklund KG, Goodman MT, Modugno F, Moysich K, Ness RB, Edwards R, Matsuo K, Hosono S, Goode EL, Winham SJ, Fridley BL, Cramer DW, Terry KL, Schildkraut JM, Berchuck A, Bandera EV, Paddock LE, Massuger LF, Wentzensen N, Pharoah P, Song H, Whittemore A, McGuire V, Sieh W, Rothstein J, Anton-Culver H, Ziogas A, Menon U, Gayther SA, Ramus SJ, Gentry-Maharaj A, Wu AH, Pearce CL, Pike M, Lee AW, Sutphen R, Chang-Claude J, Risch HA, Kjaer SK Ovarian Cancer Association Consortium. Cigarette smoking is associated with adverse survival among women with ovarian cancer: results from a pooled analysis of 19 studies. Int J Cancer. 2017;140:2422–2435. doi: 10.1002/ijc.30600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pelser C, Arem H, Pfeiffer RM, Elena JW, Alfano CM, Hollenbeck AR, Park Y. Prediagnostic lifestyle factors and survival after colon and rectal cancer diagnosis in the national institutes of health (NIH)-AARP diet and health study. Cancer. 2014;120:1540–1547. doi: 10.1002/cncr.28573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee SJ, Lee J, Park YS, Lee CH, Lee SM, Yim JJ, Yoo CG, Han SK, Kim YW. Impact of smoking on mortality of patients with non-small cell lung cancer. Thorac Cancer. 2014;5:43–49. doi: 10.1111/1759-7714.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang J, Pang H, Liu B, Nasca PC, Zhang B, Wu Y, Han W, Gates M, Lu T, Zou X, Xue F, Hou L, Wang Z, Wang Y, Chen Y, Li J. Effects of active, passive, and combined smoking on cervical cancer mortality: a nationwide proportional mortality study in Chinese urban women. Cancer Causes Control. 2015;26:983–991. doi: 10.1007/s10552-015-0580-x. [DOI] [PubMed] [Google Scholar]
- 22.Parada H Jr, Bradshaw PT, Steck SE, Engel LS, Conway K, Teitelbaum SL, Neugut AI, Santella RM, Gammon MD. Postdiagnosis changes in cigarette smoking and survival following breast cancer. JNCI Cancer Spectr. 2017;1 doi: 10.1093/jncics/pkx001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the national health interview survey, 2006-2015. Vital Health Stat 2. 2014:1–53. [PubMed] [Google Scholar]
- 24.Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, Williams DE, Geiss L. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014;370:1514–1523. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 25.Dray-Spira R, Gary-Webb TL, Brancati FL. Educational disparities in mortality among adults with diabetes in the U.S. Diabetes Care. 2010;33:1200–1205. doi: 10.2337/dc09-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in U.S. adults. J Am Coll Cardiol. 2017;70:913–922. doi: 10.1016/j.jacc.2017.06.054. [DOI] [PubMed] [Google Scholar]
- 27.Odutayo A, Gill P, Shepherd S, Akingbade A, Hopewell S, Tennankore K, Hunn BH, Emdin CA. Income disparities in absolute cardiovascular risk and cardiovascular risk factors in the United States, 1999-2014. JAMA Cardiology. 2017;2:782. doi: 10.1001/jamacardio.2017.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin YH, Ku PW, Chou P. Smoking behavioral changes and subsequent mortality during a 18-year follow-up in Kinmen, Taiwan. J Chin Med Assoc. 2017;80:283–287. doi: 10.1016/j.jcma.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Izano M, Satariano WA, Hiatt RA, Braithwaite D. Smoking and mortality after breast cancer diagnosis: the health and functioning in women study. Cancer Med. 2015;4:315–324. doi: 10.1002/cam4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bjerkaas E, Parajuli R, Engeland A, Maskarinec G, Weiderpass E, Gram IT. The association between lifetime smoking exposure and breast cancer mortality--results from a Norwegian cohort. Cancer Med. 2014;3:1448–1457. doi: 10.1002/cam4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Browman GP, Wong G, Hodson I, Sathya J, Russell R, McAlpine L, Skingley P, Levine MN. Influence of cigarette smoking on the efficacy of radiation therapy in head and neck cancer. N Engl J Med. 1993;328:159–163. doi: 10.1056/NEJM199301213280302. [DOI] [PubMed] [Google Scholar]
- 32.Gritz ER, Dresler C, Sarna L. Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Cancer Epidemiol Biomarkers Prev. 2005;14:2287–2293. doi: 10.1158/1055-9965.EPI-05-0224. [DOI] [PubMed] [Google Scholar]
- 33.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 34.Ramamoorthy S, Luo L, Luo E, Carethers JM. Tobacco smoking and risk of recurrence for squamous cell cancer of the anus. Cancer Detect Prev. 2008;32:116–120. doi: 10.1016/j.cdp.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maxwell JH, Kumar B, Feng FY, Worden FP, Lee JS, Eisbruch A, Wolf GT, Prince ME, Moyer JS, Teknos TN, Chepeha DB, McHugh JB, Urba SG, Stoerker J, Walline HM, Kurnit DM, Cordell KG, Davis SJ, Ward PD, Bradford CR, Carey TE. Tobacco use in human papillomavirus-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res. 2010;16:1226–1235. doi: 10.1158/1078-0432.CCR-09-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Do KA, Johnson MM, Doherty DA, Lee JJ, Wu XF, Dong Q, Hong WK, Khuri FR, Fu KK, Spitz MR. Second primary tumors in patients with upper aerodigestive tract cancers: joint effects of smoking and alcohol (United States) Cancer Causes Control. 2003;14:131–138. doi: 10.1023/a:1023060315781. [DOI] [PubMed] [Google Scholar]
- 37.Browman GP, Mohide EA, Willan A, Hodson I, Wong G, Grimard L, MacKenzie RG, El-Sayed S, Dunn E, Farrell S. Association between smoking during radiotherapy and prognosis in head and neck cancer: a follow-up study. Head Neck. 2002;24:1031–1037. doi: 10.1002/hed.10168. [DOI] [PubMed] [Google Scholar]
- 38.Warren GW, Kasza KA, Reid ME, Cummings KM, Marshall JR. Smoking at diagnosis and survival in cancer patients. Int J Cancer. 2013;132:401–410. doi: 10.1002/ijc.27617. [DOI] [PubMed] [Google Scholar]
- 39.Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–515. doi: 10.1161/ATVBAHA.113.300156. [DOI] [PubMed] [Google Scholar]
- 40.Kunitomo M, Yamaguchi Y, Kagota S, Yoshikawa N, Nakamura K, Shinozuka K. Biochemical evidence of atherosclerosis progression mediated by increased oxidative stress in apolipoprotein E-deficient spontaneously hyperlipidemic mice exposed to chronic cigarette smoke. J Pharmacol Sci. 2009;110:354–61. doi: 10.1254/jphs.09100fp. [DOI] [PubMed] [Google Scholar]
- 41.Orosz Z, Csiszar A, Labinskyy N, Smith K, Kaminski PM, Ferdinandy P, Wolin MS, Rivera A, Ungvari Z. Cigarette smoke-induced proinflammatory alterations in the endothelial phenotype: role of NAD(P)H oxidase activation. Am J Physiol Heart Circ Physiol. 2007;292:H130–139. doi: 10.1152/ajpheart.00599.2006. [DOI] [PubMed] [Google Scholar]
- 42.Morris PB, Ference BA, Jahangir E, Feldman DN, Ryan JJ, Bahrami H, El-Chami MF, Bhakta S, Winchester DE, Al-Mallah MH, Sanchez Shields M, Deedwania P, Mehta LS, Phan BA, Benowitz NL. Cardiovascular effects of exposure to cigarette smoke and electronic cigarettes: clinical perspectives from the prevention of cardiovascular disease section leadership council and early career councils of the American college of cardiology. J Am Coll Cardiol. 2015;66:1378–1391. doi: 10.1016/j.jacc.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 43.Heeschen C, Jang JJ, Weis M, Pathak A, Kaji S, Hu RS, Tsao PS, Johnson FL, Cooke JP. Nicotine stimulates angiogenesis and promotes tumor growth and atherosclerosis. Nat Med. 2001;7:833–9. doi: 10.1038/89961. [DOI] [PubMed] [Google Scholar]
- 44.Powell JT. Vascular damage from smoking: disease mechanisms at the arterial wall. Vascular Medicine. Vasc Med. 1998;3:21–8. doi: 10.1177/1358836X9800300105. [DOI] [PubMed] [Google Scholar]
- 45.Burcu M, Steinberger EK, Sorkin JD. Health care access and smoking cessation among cancer survivors: implications for the affordable care act and survivorship care. J Cancer Surviv. 2016;10:1–10. doi: 10.1007/s11764-015-0446-y. [DOI] [PMC free article] [PubMed] [Google Scholar]