Abstract
Background and Aims
Intraoperative perforation is a major adverse event of endoscopic submucosal dissection (ESD). To avoid perforation, it is important for the endoscope to approach the portion to be resected carefully and to ensure that the knife can approach the submucosa at an angle parallel to the muscle layer. The multibending endoscope has 2 bends at its tip and may facilitate the ESD procedure. To the best of our knowledge, very few studies have reported the use of the multibending endoscope during gastric ESD. The aim of this study was, therefore, to introduce the usefulness of the multibending endoscope for gastric ESD.
Methods
We report 2 cases of early gastric cancer in which ESD was performed using a multibending endoscope.
Results
Unlike conventional single-bending endoscopes that have only 1 moveable part, the multibending endoscope allowed difficult areas to be approached more easily. Small adjustments could be made to the upward or downward angle of both the first and the second bending sections of the endoscope. This ensured that the knife would approach the submucosa at an angle parallel to the muscle layer. In patient 1, initially the conventional endoscope was used, but it became more difficult to approach the site, and paradoxic movement occurred. When the conventional endoscope was changed to the multibending endoscope, the ESD procedure became safer and more efficient. Another ESD using the multibending endoscope was performed successfully without any adverse events.
Conclusions
The use of a multibending endoscope for ESD will enable safer and faster treatment of patients.
Abbreviation: ESD, endoscopic submucosal dissection
The occurrence of intraoperative perforation due to endoscopic submucosal dissection (ESD) for early gastric cancer has been reported to be 3.02%.1 In particular, reports have indicated that the risk of perforation is higher if ESD is performed in the body or the lesser/greater curvature of the stomach.1, 2 ESD is also challenging to perform in the lesser curvature because of the risk of arterial bleeding.3 To avoid bleeding or perforation and to treat patients effectively and without adverse events, it is important that the surgeon is able to secure a good visual field during dissection. A good visual field is one that allows the endoscope to carefully approach the area to be resected and ensures that the knife can approach the submucosa at an angle parallel to the muscle layer.
When dissection is performed from a distance, the blood vessels and the boundaries of the submucosal and muscle layers cannot be visually distinguished; this increases the risk of bleeding or perforation. Previous studies have reported a 1-sided expandable balloon4 for use in gastric ESD and a multibending endoscope5 for use in gastric EMR. It is particularly difficult to approach the lesser curvature of the stomach, the anterior wall of the gastric body, the fundus, and the angulus of the stomach. When ESD is performed at the body or angulus of stomach, the endoscope must be oriented in either a forward direction or an inverted orientation. If dissection is performed in the forward direction, it is relatively easy to bring the endoscope toward the portion to be dissected, but respiratory fluctuations in the location of the site can be quite substantial and difficult to manage. Inverting the orientation of the endoscope often reduces the magnitude of these respiratory fluctuations. However, if a conventional single-bending endoscope is used in the inverted orientation, the knife ends up at an angle adversarial to the muscle layer (especially at the lesser curvature of the stomach and the angulus), even if it is approaching the site to be operated. This increases the risk of perforation. Additionally, it is common for attempts to push the endoscope farther toward the lesser curvature of the lower body or angulus to cause movements away from the lesion site instead (paradoxic movements), which increases the difficulty of the operation.
The multibending endoscope (GIF-2TQ260M; Olympus Medical Corp, Tokyo, Japan) has 2 bends at its tip (Fig. 1), making it easier to approach areas that would be challenging to approach with a conventional single-bending endoscope. Furthermore, after the area is approached, small adjustments can be made to the upward or downward angle of either bending section of the endoscope; this ensures that the knife will approach the submucosa at an angle parallel to the muscle layer (Video 1, available online at www.VideoGIE.org).
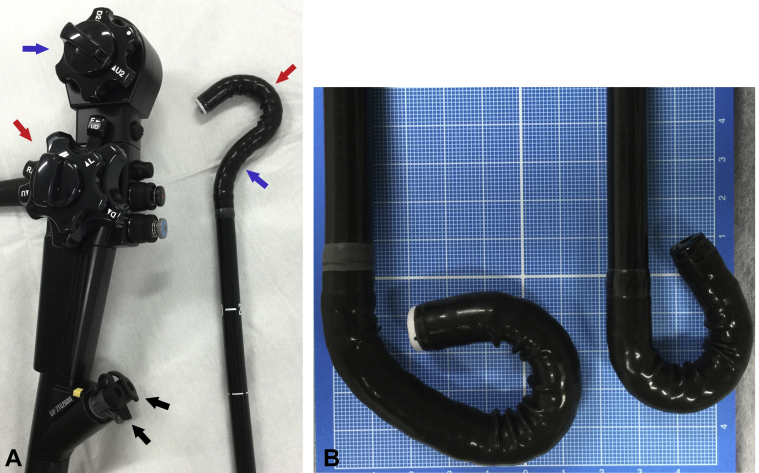
Figure 1.
Multibending endoscope (GIF-2TQ260M). A, This multibending endoscope has 2 bending sections and 2 channels (black arrows). The first bending section angulates up (red arrow), whereas the second angulates down (blue arrow). B, Comparison of the multibending endoscope (left) and the conventional endoscope (right). In the multibending endoscope, both bending sections angulate up.
We believe that the use of this endoscope will enable safer ESD procedures.
Despite these benefits, very few studies have reported the use of the multibending endoscope during gastric ESD. Therefore, the purpose of this case series was to present 2 cases of gastric ESD performed with the use of this endoscope (Table 1).
Table 1.
Specifications of the 2 cases of endoscopic submucosal dissection with use of a multibending endoscope
| Patient | Location | Tumor dimensions (mm) | Resected specimen dimensions (mm) | Procedure time∗ (min) | Submucosal dissection speed† (mm2/min) | Histologic type | Depth of invasion | Ulceration | Perforation | Curability |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M, less | 25 × 12 | 44 × 28 | 65 | 15 | Well | M | Negative | None | Cured |
| 2 | U, less, ante, post | 44 × 34 | 65 × 53 | 84 | 32 | Well | M | Negative | None | Cured |
Ante, anterior wall of the stomach; less, lesser curvature of the stomach; M, middle body of the stomach; m, mucosa; post, posterior wall of the stomach; U, upper body of the stomach; Well, well-differentiated tubular adenocarcinoma.
Procedure time: time from beginning of the submucosal injection to complete removal.
The average dissection speed was calculated by dividing the time of the procedure by the area of the resected specimen, which was calculated as 3.14 × 0.25 × long axis × minor axis.
This study was approved by the Ethics Committee of the Southern-Tohoku General Hospital. Informed consent was obtained from all patients for being included in the study.
A Dual Knife (KD-655L; Olympus Medical Corp) was used for all procedures. The VIO300D (ERBE Elektromedizin Gmbh, Tübingen, Germany) was used as the electrosurgery unit.
Case reports
Patient 1
A 71-year-old man presented with a type 0-IIc lesion at the lesser curvature of the lower body of the stomach (Fig. 2A). Initially, we used a conventional endoscope (GIF-Q260J; Olympus Medical Corp) and, from an inverted position, made an approximate semicircular cut on the distal side. We attempted dissection; however, the knife was at an adversarial angle to the muscle layer, even after the site was deaerated and approached (Fig. 2B and C). This presented a high risk for muscle layer damage; therefore, we modified our approach, added an incision on the proximal side, and proceeded with dissection in the forward direction. However, as dissection progressed it became more and more difficult to approach the site, and paradoxic movement occurred; consequently, pushing the endoscope forward caused it to move farther away from the site (Fig. 2D). For this reason, we changed endoscopes and began using the multibending endoscope. By using the second bending section in addition to the first, we were easily able to approach the dissected portion and to orient the knife so that it was nearly parallel with the muscle layer (Fig. 2E and F).
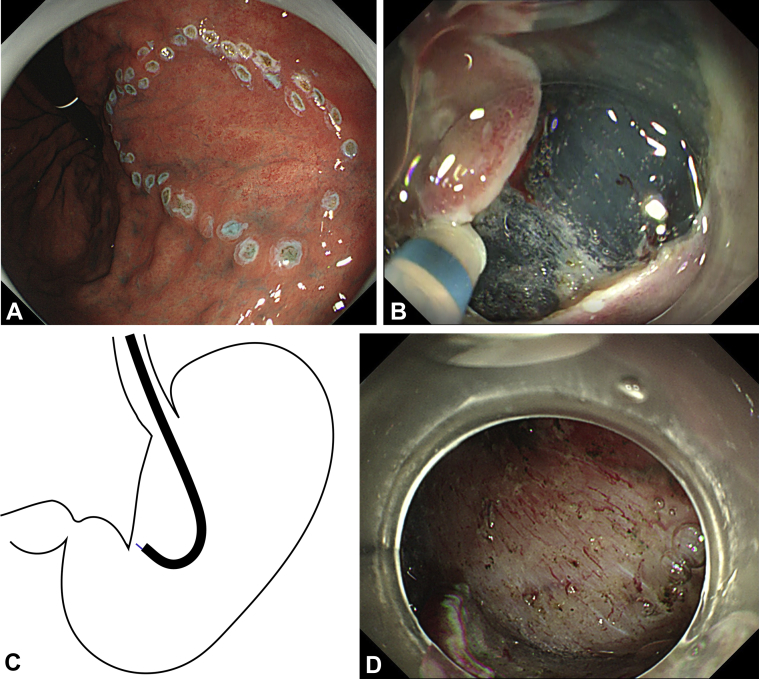
Figure 2.
Patient 1. A, Type 0-IIc lesion at the lesser curvature of the lower body of the stomach. B, During use of a conventional endoscope, the knife-edge points toward the muscle layer. C, Approach to the lesser curvature of the lower body of the stomach by use of a conventional endoscope. The knife is angled toward the muscle layer. D, Pushing a conventional endoscope in the forward direction causes it to move away from the lesion (paradoxical movement). E, Using a multibending endoscope, we approached the resection site and adjusted the knife-edge angle to be parallel with the muscle layer. F, Approach to the lesser curvature of the lower body of the stomach by use of the multibending endoscope. The knife-edge approaches the dissection site and is angled so that it is parallel with the muscle layer. G, Performing dissection while maintaining a parallel angle between the knife-edge and muscle layer. H, Ulcer after endoscopic submucosal dissection. We used a hemostatic clip on large blood vessels to prevent secondary bleeding.
Thereafter, we were able to insert the endoscope between the mucosa and the muscle layer, enabling traction through the use of a hood. Dissection proceeded with the knife parallel to the muscle layer throughout the entire procedure (Fig. 2G). We were able to complete en bloc resection without perforation (Fig. 2H). The change from the conventional endoscope to the multibending endoscope made the ESD procedure safer and more efficient. For this lesion, we should have considered using the multibending endoscope from the start.
Patient 2
An 83-year-old man presented with a type 0-IIc lesion at the anterior-to-posterior wall of the upper body of the stomach (Fig. 3A). ESD was performed by use of a multibending endoscope. The incision on the fundus, which was the most difficult to access, was made possible by the multibend functionality of the endoscope, which enabled us to efficiently approach and treat the site (Fig. 3B-E). We extended the knife out of the right channel of the endoscope when performing incisions toward the left (Fig. 3B). By contrast, when performing incisions toward the right, we found that extending the knife out of the left channel of the endoscope expanded our visual field considerably and increased the operability of the endoscope (Fig. 3F). Similarly, extending the knife out of the left channel of the endoscope during dissection toward the right improved our ability to visually distinguish blood vessels in the movement path of the endoscope and the boundaries of the submucosal and muscle layers (Fig. 3G). Despite many large blood vessels at the lesion site, our close approach to the site enabled us to visually confirm their presence and use hemostatic forceps (Coagrasper, FD-411QR; Olympus Medical Corp) to carry out preventive coagulation (Fig. 3H). However, the use of hemostatic forceps blindly from a distance can cause the muscle layer to coagulate as well. Nonetheless, the multibending endoscope enabled us to approach the blood vessel or bleeding site, view it directly, and avoid coagulation of the muscle layer with the hemostatic forceps. We were able to complete en bloc resection. (Fig. 3I).
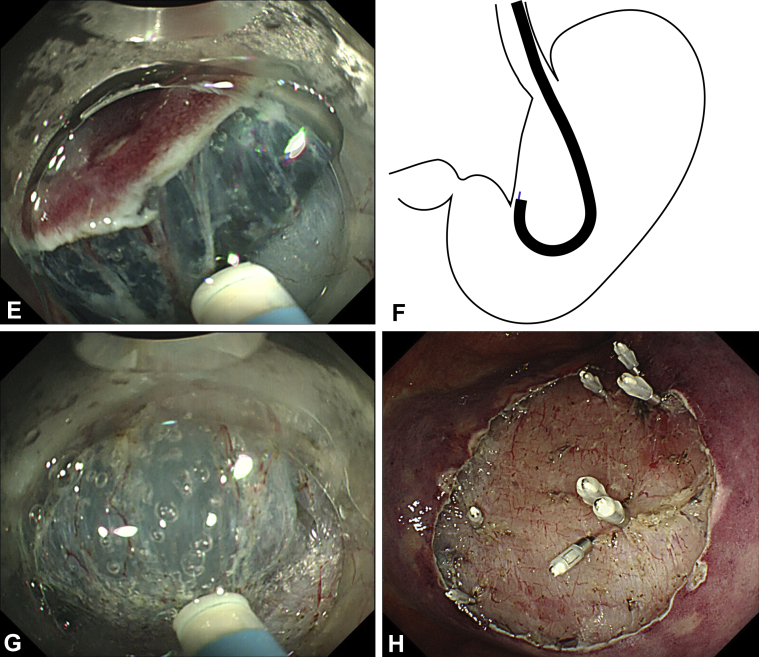
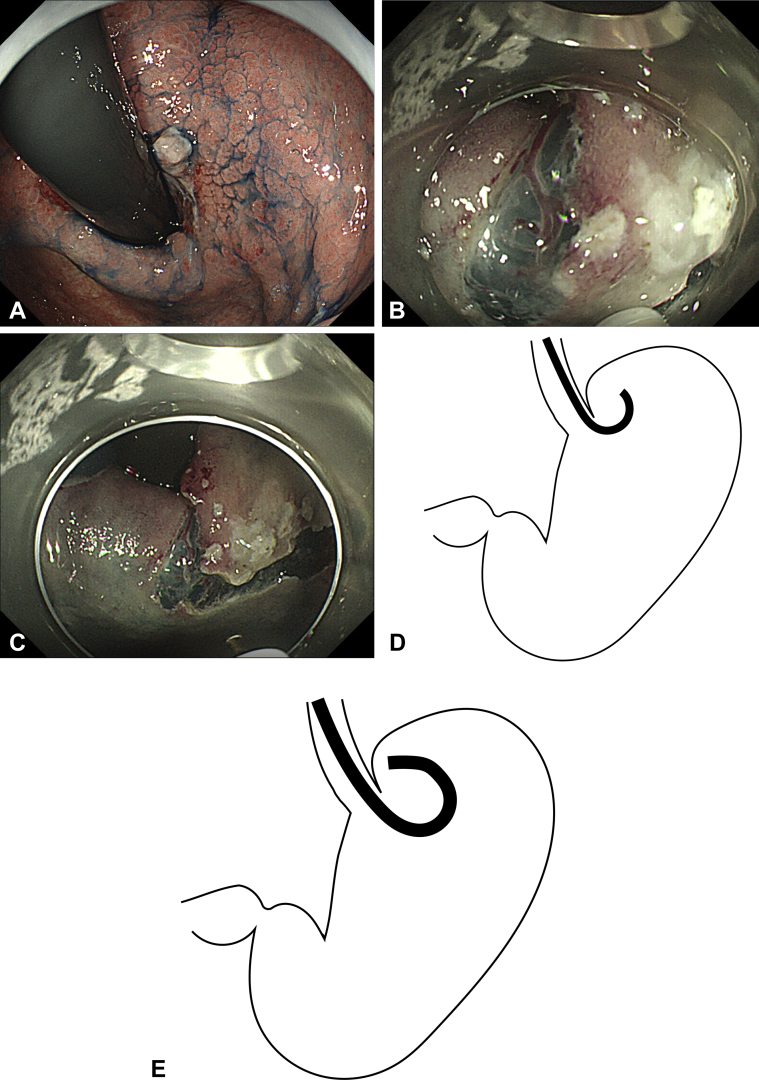
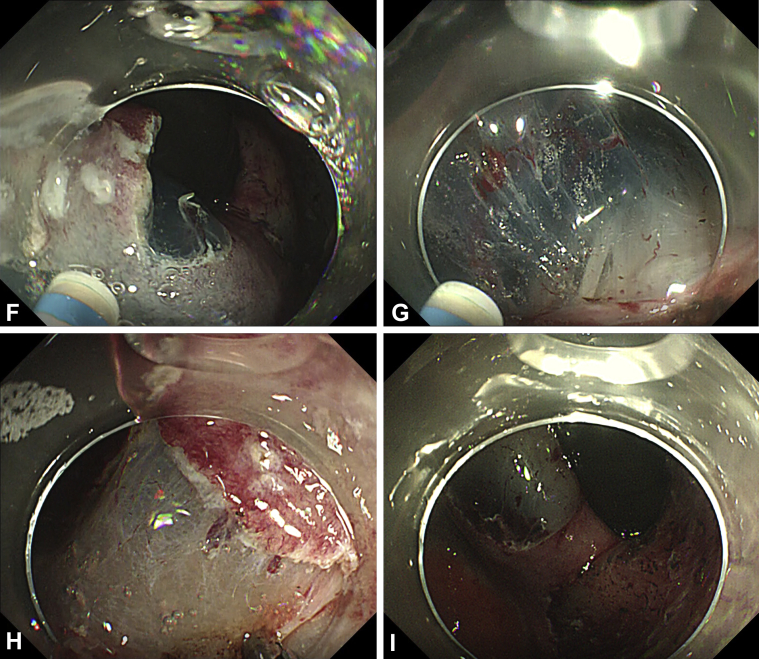
Figure 3.
Patient 2. A, Type 0-IIc lesion at the anterior wall to posterior wall of the upper body of the stomach. B, Incision on the fornix side, the most difficult area to reach with the endoscope. C, Incision on the fornix side. D, Approach to the fornix by use of a conventional endoscope. The endoscope cannot reach the dissection site. E, Approach to the fornix by use of the multibending endoscope. The multibend functionality of the endoscope enables us to efficiently approach and treat the site. F, Extension of the knife from the left channel while incision was made on the posterior wall expanded the right visual field. G, In dissection, when performing a cut toward the right, extending the knife from the left channel secured the visual field in the direction of the cut. H, Close approach to the site enabled us to visually confirm location of the blood vessels, and these vessels can be precisely targeted and grasped with hemostatic forceps. I, Ulcer after endoscopic submucosal dissection.
Discussion
We believe there are 2 reasons why the multibending endoscope is advantageous during ESD. First, when using a conventional endoscope, if the surgeon cannot reach the dissection site, the knife is simply extended far out of the endoscope, and dissection is performed from a distance. When the knife has been extended far out of the endoscope, the movements of the knife-edge become larger and more unstable. By using the second bending section of the multibending endoscope, the surgeon can access sites, including the lesser curvature of the stomach, anterior wall of the gastric body, fundus, and angulus of the stomach that are unreachable by a conventional endoscope, preventing extension of the knife out of the endoscope and thereby stabilizing its movements. Approaching the dissection site allows the vasculature and layers to be easily distinguished, which minimizes the risk of bleeding and muscle layer damage.
Second, it is difficult to achieve an angle parallel to the muscle layer during use of a conventional endoscope. In situations where dissection must be performed with the knife angled toward the muscle layer, the risk of muscle layer damage increases. With a multibending endoscope, the angles at the first and second bending sections of the instrument can be adjusted, enabling a more favorable parallel angle with the muscle layer and, thereby, decreasing the risk of muscle layer damage and increasing the safety of the operation.
Furthermore, the GIF-2TQ260M is a 2-channel endoscope, and previous reports have described a technique whereby the knife is extended through 1 channel and an injection needle is extended through the other channel. After submucosal injection, immediate cutting can be performed before the collapse of the submucosal cushion.6 In treating patient 2, we considered this 2-channel functionality when determining the best method for developing a good visual field. In the ESD procedures in our case series, we extended the knife through the left channel when moving toward the right, and vice versa. Using this method expands our visual field in the direction of the cut, which further facilitates our ability to visualize the vasculature and the muscle layer.
When hemostatic forceps are used on large vessels for precoagulation or to perform hemostasis, blind operation from a distance can inadvertently cause the surgeon to grasp the muscle layer, increasing the risk of perforation. Previous reports have also described an association between hypercoagulation of the muscle layer and delayed perforation.7 Using the multibending endoscope, the surgeon can approach the site, determine the location of the bleeding, and perform coagulation while grasping only the vessel. Doing this prevents the passage of an unnecessary current through the muscle layer. Furthermore, when a conventional endoscope is used, the insertion of devices such as a knife or hemostatic forceps narrows the channel of the endoscope and reduces suction power. However, with a 2-channel endoscope, suction is performed with the left channel, meaning that the insertion of devices into the right channel of the endoscope will not reduce suction; this enables rapid deaeration and aspiration of blood. The disadvantages of the GIF-2TQ260M endoscope are the heavy weight of the operative end and the large endoscope diameter, which limits its operability in narrow spaces, such as the pyloric ring and the esophagogastric junction.
Through this case series, we have demonstrated the utility of the multibending endoscope for gastric ESD. We believe that its benefits outweigh the risks and will enable safer and faster treatment of patients with early gastric cancer.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Acknowledgment
The authors thank Editage [http://www.editage.com] for editing and reviewing this manuscript for English language.
Supplementary data
Endoscopic submucosal dissection using the multibending endoscope for early gastric cancers.
References
- 1.Yamamoto Y., Kikuchi D., Nagami Y. Management of adverse events related to endoscopic resection of upper gastrointestinal neoplasms: review of the literature and recommendations from experts. Dig Endosc. 2019;31:4–20. doi: 10.1111/den.13388. [DOI] [PubMed] [Google Scholar]
- 2.Daegu-Kyungpook Gastrointestinal Study Group (DGSG) Kim M., Jeon S.W., Cho K.B. Predictive risk factors of perforation in gastric endoscopic submucosal dissection for early gastric cancer: a large, multicenter study. Surg Endosc. 2013;27:1372–1378. doi: 10.1007/s00464-012-2618-4. [DOI] [PubMed] [Google Scholar]
- 3.Imagawa A., Okada H., Kawahara Y. Endoscopic submucosal dissection for early gastric cancer: results and degrees of technical difficulty as well as success. Endoscopy. 2006;38:987–990. doi: 10.1055/s-2006-944716. [DOI] [PubMed] [Google Scholar]
- 4.Kawamura M., Sekine H., Kikuchi T. Endoscopic submucosal dissection for gastric neoplasms by using a novel attachment device-a one-sided, expandable balloon. Gastrointest Endosc. 2011;74:415–418. doi: 10.1016/j.gie.2011.03.1247. [DOI] [PubMed] [Google Scholar]
- 5.Isshi K., Tajiri H., Fujisaki J. The effectiveness of a new multibending scope for endoscopic mucosal resection. Endoscopy. 2004;36:294–297. doi: 10.1055/s-2004-814203. [DOI] [PubMed] [Google Scholar]
- 6.Nishizawa T., Uraoka T., Ochiai Y. The "two-sword fencing technique" in endoscopic submucosal dissection. Clin Endosc. 2015;48:85–86. doi: 10.5946/ce.2015.48.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamamoto Y., Nishisaki H., Sakai H. Clinical factors of delayed perforation after endoscopic submucosal dissection for gastric neoplasms. Gastroenterol Res Pract. 2017;2017:7404613. doi: 10.1155/2017/7404613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic submucosal dissection using the multibending endoscope for early gastric cancers.