Abstract
Despite advances in diagnostic tools and therapeutic options, treatment resistance remains a challenge for many cancer patients. Recent studies have found evidence that autophagy, a cellular pathway that delivers cytoplasmic components to lysosomes for degradation and recycling, contributes to treatment resistance in different cancer types. A role for autophagy in resistance to chemotherapies and targeted therapies has been described based largely on associations with various signaling pathways, including MAPK and PI3K/AKT signaling. However, our current understanding of the molecular mechanisms underlying the role of autophagy in facilitating treatment resistance remains limited. Here we provide a comprehensive summary of the evidence linking autophagy to major signaling pathways in the context of treatment resistance and tumor progression, and then highlight recently emerged molecular mechanisms underlying autophagy and the p62/KEAP1/NRF2 and FOXO3A/PUMA axes in chemoresistance.
Keywords: autophagy, cancer, treatment resistance, targeted agents, chemotherapy, molecular mechanisms, chemoresistance
1. Introduction
Autophagy is an intracellular degradative pathway that delivers cytoplasmic components to lysosomes for degradation and recycling. The term “autophagy” is derived from the Greek words “auto” meaning oneself and “phagy” meaning to eat and was first coined by Christian de Duve at the 1963 Ciba Foundation Symposium on Lysosomes. In mammalian systems, there are at least three co-existing forms of autophagy that are morphologically distinct, as follows: Microautophagy, chaperone-mediated autophagy (CMA), and macroautophagy [1,2]. Microautophagy is characterized by the uptake of small cytoplasmic fragments into lysosomes through the formation of inward lysosomal membrane invaginations. This is unlike CMA, where chaperone proteins facilitate the direct uptake and translocation of cytosolic components into lysosomes for degradation and recycling [1,2]. Macroautophagy is characterized by the formation of double-membrane structures, known as autophagosomes, that fuse with lysosomes to form autolysosomes that degrade and recycle engulfed cellular components [3,4]. Macroautophagy is the most extensively studied form of autophagy and is the main mechanism used by eukaryotes for the maintenance of cellular homeostasis and quality control [3,4].
Significant progress has been made over the past decade in regards to our understanding of the roles of macroautophagy (hereafter referred to as autophagy) in health and disease [5,6]. In particular, autophagy has been shown to play both pro- and anti-tumorigenic roles during the onset and progression of cancers, and in response to anti-cancer treatment [7,8]. Autophagy functions in tumor suppression during early stages of tumorigenesis by maintaining cellular homeostasis and genome stability through the clearance of cytotoxic proteins and damaged organelles, and by the regulation of cell death and senescence [9,10,11,12,13]. During later stages of cancer progression, autophagy favors tumorigenesis by contributing to tumor survival under conditions of oxidative stress and nutrient deprivation, by initiating cellular survival responses and catabolizing redundant organelles and proteins for energy [14,15,16,17,18,19,20]. Recent excellent reviews cover the tumor-promoting and -suppressive roles of autophagy in cancer in greater detail [7,21,22]. The pro-tumorigenic roles of autophagy have primed it as an attractive therapeutic target for cancer treatments [23,24,25]. Autophagy can be modulated through genetic approaches, like small interfering RNAs (siRNAs) and small hairpin RNAs (shRNAs) that target key autophagy-related (ATG) genes. Many pharmacological compounds that inhibit different stages of autophagy have also been developed and have been used to inhibit autophagy (Table 1). Despite many ongoing preclinical and clinical studies investigating the therapeutic benefit of autophagy inhibition alone or in combination treatment strategies in cancers [26,27,28], our current understanding of the actual molecular mechanisms underlying the pro-tumorigenic contributions of autophagy to treatment resistance remains largely unknown.
2. Autophagy Contributes to Treatment Resistance in Cancer
Tumor initiation is largely stochastic by nature and involves a coordinated destabilization of major cellular processes. The dynamic and evolutionary manner by which this occurs creates molecularly heterogenous tumors [29,30]. The ability of cancers to adapt to and survive the effects of cancer therapies remains one of the greatest impediments in medical and clinical oncology. Treatment resistance directly translates to the ineffectiveness and eventual failures of cancer therapies [31,32,33,34,35,36]. Innate treatment resistance predates therapeutic intervention, whereas acquired treatment resistance is a refractory outcome of cancer therapy that occurs when subpopulations of cancer cells within tumors acquire mutations and adaptations that desensitize them to ongoing treatment [37,38,39,40,41]. To date, treatment resistance remains a major challenge to successful cancer treatment and control, but the mechanisms involved remain poorly understood [42,43].
2.1. Autophagy and Resistance Against Chemotherapy
Chemotherapy, with or without surgery and/or radiation, is commonly administered as part of routine first-line treatment of most cancers [44,45]. Chemotherapy involves the use of toxic chemical compounds that target and kill rapidly growing and dividing cells. Most chemotherapeutic agents interfere with the ability of the cells to divide, and often work at the DNA level. Examples include anti-mitotic agents like paclitaxel and docetaxel, topoisomerase II inhibitors (anthracyclines), like doxorubicin and epirubicin, and DNA alkylating agents, such as cisplatin and carboplatin [44,45]. Although such chemotherapeutic agents are systemic and affect normal cells as well, most cancers are characterized by rapid growth and this makes them most amenable to the cytotoxic effects of chemotherapy. However, the therapeutic success of chemotherapy is limited by a large variety of cellular adaptations that provide tumor cells with the ability to tolerate the cytotoxic effects of chemotherapy [45]. Of note, the activation of autophagy in response to standard chemotherapy has been shown to aid in chemoresistance in certain cancer contexts. In such cases, autophagy inhibition in combination with chemotherapy can significantly augment tumor cell killing, supporting a pro-survival role of autophagy in contributing to tumor resistance against chemotherapies (Table 2).
Table 1.
Examples of pharmacological autophagy inhibitors.
| Name | Mechanism of Action | Targeted Stage in Autophagy | Ref. |
|---|---|---|---|
| Inhibitors that target late stages of autophagy | |||
| Lys05 | Lysosomotropic agent |
|
[46,47] |
| Chloroquine (CQ) | Lysosomotropic agent |
|
[48,49] |
| Hydroxychloroquine (HCQ) | |||
| Quinacrine (QNX) | |||
| IITZ-01 | Lysosomotropic agent |
|
[50] |
| ROC-325 | unknown |
|
[51,52,53] |
| Bafilomycin A1 (Baf A1) | Vacuolar ATPase inhibitor |
|
[54] |
| ECDD-S27 | Vacuolar ATPase inhibitor |
|
[55] |
| Ca-5f | Unknown |
|
[56] |
| EACC | Syntaxin 17 (STX17) translocation inhibitor |
|
[57] |
| MHY1485 | Mammalian target of rapamycin (mTOR) activator |
|
[58] |
| Pepstatin A | Acid protease inhibitor |
|
[59,60] |
| E64-d | Acid protease inhibitor |
|
[59,60] |
| Alpha-hederin | Unknown |
|
[61] |
| Inhibitors that target early stages of autophagy | |||
| SB02024 | Vacuolar protein sorting protein 34 (Vps34) inhibitor |
|
[62] |
| SAR405 | Vacuolar protein sorting protein 18 and 34 (Vps18 and Vps34) inhibitor |
|
[63] |
| PIK-III | Vacuolar protein sorting protein 34 (Vps34) inhibitor |
|
[64] |
| Autophinib | Vacuolar protein sorting protein 34 (Vps34) inhibitor |
|
[65] |
| SBI-0206965 | Unc-51-like kinase 1 (ULK1) inhibitor |
|
[66] |
| ULK-100, ULK-101 | Unc-51-like kinase 1 (ULK1) inhibitor |
|
[67] |
| LY294002 | Phosphoinositide 3-kinase (PI3) inhibitor |
|
[68,69] |
| 3-Methyladenine (3-MA) | Phosphoinositide 3-kinase (PI3) inhibitor |
|
[70] |
| Wortmannin | Phosphoinositide 3-kinase (PI3) inhibitor |
|
[68,71,72] |
| Spautin-1 | Ubiquitin Specific Peptidase 10 and 13 (USP10 and USP13) inhibitor |
|
[73,74] |
| NSC185058 | Autophagy-related (ATG) protein 4A and 4B (ATG4A and ATG4B) inhibitor |
|
[75] |
| UAMC-2526 | Autophagy-related (ATG) protein 4B (ATG4B) inhibitor |
|
[76] |
| DMP-1 | unknown |
|
[77] |
| Inhibitors that target both early and late stages of autophagy | |||
| Tioconazole | Autophagy-related (ATG) protein 4A and 4B (ATG4A and ATG4B) inhibitor |
|
[78] |
| LV-320 | Autophagy-related (ATG) protein 4A and 4B (ATG4A and ATG4B) inhibitor |
|
[79] |
| S130 | Autophagy-related (ATG) protein 4A and 4B (ATG4A and ATG4B) inhibitor |
|
[80] |
| Xanthium strumarium Fruit Extract | Autophagy-related (ATG) protein 4B (ATG4B) inhibitor |
|
[81] |
| Verteporfin | unknown |
|
[82] |
Table 2.
Examples of pre-clinical studies demonstrating that autophagy and autophagy-related (ATG) genes contribute to chemotherapy resistance in different types of cancers.
| Cancer Type | Chemotherapeutic Agent | Mode of Autophagy Inhibition | Ref. | |
|---|---|---|---|---|
| Pharmacological | Genetic | |||
| Bladder cancers | Cisplatin, Gemcitabine, Mitomycin, Pirarubicin |
CQ, HCQ, Baf A1, Wortmannin, 3-MA | ATG7 shRNA, ATG12 shRNA, BECN1 shRNA, BECN1 siRNA, ATG3 siRNA |
[83,84,85,86,87] |
| Bone cancers | Doxorubicin, Cisplatin, Methotrexate, Paclitaxel |
Spautin-1, 3-MA, CQ | BECN1 shRNA, BECN1-targeting deoxyribozyme, miR-410 (ATG16L knockdown), ATG14 siRNA, ATG7 siRNA |
[88,89,90,91,92,93,94,95,96,97,98] |
| Breast cancers | 5-Fluorouracil, Doxorubicin, Docetaxel, Adriamycin, Cyclophosphamide, Epirubicin, Paclitaxel, Cisplatin, Gemcitabine |
Baf A1, CQ, HCQ, 3-MA, Verteporfin | ATG5 shRNA, ATG5 siRNA, ATG7 siRNA, FIP200 shRNA, ATG13 shRNA, BECN1 shRNA, BECN1 siRNA, BECN1 CRISPR/Cas9 KO, BNIP3L CRISPR/Cas9 KO, AMBRA1 shRNA |
[99,100,101,102,103,104,105,106,107] |
| Cervical cancers | Cisplatin, Oncothermia, Paclitaxel |
3-MA, CQ, Baf A1 | BECN1 siRNA, ATG5 siRNA, ATG7 siRNA |
[108,109,110,111,112] |
| Colorectal cancers | 5-FU, Oxaliplatin |
CQ, 3-MA, Baf A1 | ATG7 siRNA, BECN1 siRNA, ATG5 siRNA |
[113,114,115,116] |
| Endometrial cancers | Paclitaxel, Cisplatin, Resveratrol, Oncothermia |
CQ, 3-MA | BECN1 shRNA, ATG5 siRNA, ATG7 siRNA |
[117,118,119,120,121] |
| Gastric cancers | Vincristine, 5-fluorouracil, Cisplatin, Bufalin, Matrine, Oxaliplatin, Cinobufagin |
CQ, 3-MA, Baf A1 | miR-23b (ATG12 knockdown), ATG5 siRNA |
[122,123,124,125,126,127,128,129,130,131,132] |
| Gliomas | Temozolomide, Vorinostat |
HCQ, CQ, 3-MA, QNX, Baf A1, ATG4B inhibitor (NSC185058) |
LC3A siRNA, LC3B siRNA, TFEB siRNA, ATG4C shRNA, ATG4B shRNA |
[133,134,135,136,137,138,139,140] |
| Head and neck cancers | Paclitaxel, Cisplatin, Nedaplatin |
3-MA, CQ, Baf A1 | LC3B siRNA, ATG3 siRNA, ATG5 siRNA, ATG6 siRNA, ATG7 siRNA |
[141,142,143,144,145,146] |
| Liver cancers | Epirubicin, Oxaliplatin, Mitomycin, Cisplatin, Doxorubicin |
3-MA, CQ, Baf A1 | ATG4B shRNA, ATG5 siRNA, ATG5 shRNA, ATG7 shRNA, LC3 shRNA, miR-101 (RAB5A, STMN1, ATG4B knockdown) |
[147,148,149,150,151,152,153,154,155] |
| Lung cancers | Paclitaxel, Camptothecin, Cisplatin, 5-fluorouracil, Gemcitabine, Pterostilbene |
3-MA, CQ, Alpha-hederin, Baf A1, ATG4B inhibitors (Compound 1, 17) |
ATG7 siRNA, BECN1 siRNA, ATG5 siRNA |
[61,141,156,157,158,159,160,161,162,163] |
| Neuroblastomas | Vincristine, Doxorubicin, Cisplatin, Paclitaxel |
HCQ, 3-MA | ATG5 shRNA, ATG5 siRNA, BECN1 siRNA, TRP14 siRNA |
[164,165,166] |
| Ovarian cancers | Cisplatin, Carboplatin, Vincristine, Gemcitabine, Ifosfamide, Docetaxel, Paclitaxel |
3-MA, CQ, Quinacrine | ATG5 siRNA, BECN1 siRNA, AMBRA1 shRNA, ATG5 CRISPR/Cas9 KO, miR-204 (LC3B and ATG7 knockdown) |
[167,168,169,170,171,172,173,174,175,176] |
| Pancreatic cancers | Doxorubicin, Gemcitabine, Docetaxel |
CQ, Verteporfin | ATG7 siRNA, ATG12 siRNA, USP22 siRNA, miR-23b (ATG12 knockdown), miR-29a (ATG9A and TFEB knockdown), miR-29c (USP22 knockdown), miR-137 (ATG5 knockdown) |
[177,178,179,180,181,182,183,184,185] |
| Skin cancers | Temozolomide, Cisplatin |
CQ, HCQ, LY294002 | ATG5 shRNA | [186,187,188] |
Lung cancer is one of the leading causes of cancer-related deaths worldwide, and approximately 80% are defined as non-small cell lung carcinomas (NSCLC) [156]. Treatment regimes administered to NSCLC patients typically include paclitaxel. However, the issue of acquired resistance to paclitaxel in NSCLC remains an obstacle in chemotherapy success [156]. Recent studies have demonstrated that the pharmacological inhibition of autophagy using CQ, prior to paclitaxel treatment, significantly reduces in vitro tumorigenic potential and induces apoptosis of NSCLC cells [156]. Of note, autophagy inhibition also increased intracellular reactive oxidative species (ROS), and this was associated with a reduction in AKT activity [156]. Recent efforts have also been focused on the development of novel small molecule inhibitors of the autophagy related 4B cysteine peptidase 4B (ATG4B), a core cysteine protease in the autophagy process [157]. Pharmacological inhibition of ATG4B was associated with a reduction in autophagic flux, and significantly augmented tumor cell killing effects of tamoxifen or cisplatin in NSCLC cells [157].
Similarly, inhibition of autophagy was shown to improve the responses of osteosarcomas to chemotherapies. Osteosarcoma is a common primary bone cancer that occurs in young adults and, like lung cancer, acquired resistance to chemotherapies remains a clinical challenge [88]. Recent studies have demonstrated that cisplatin-resistant osteosarcoma cells exhibit elevated levels of autophagy, and the pharmacological inhibition of autophagy, using 3-MA, significantly improved sensitivity to cisplatin [88]. Autophagy inhibition was found to increase levels of the FOXO3A transcription factor, which consequently increased levels of the pro-apoptotic protein, PUMA, thereby increasing apoptosis [88]. Interestingly, a similar mechanism of autophagy in treatment resistance was also recently reported and investigated in greater depth in colorectal cancers [189]. We refer our readers to Section 3 of this review for a greater discussion of the findings of this recent paper by Fitzwalter et al. [189]. Taken together, these studies strongly support the role of autophagy in treatment resistance against various chemotherapies in different cancers. Table 2 below provides a more comprehensive summary of examples from pre-clinical studies that support a role for autophagy or autophagy-related (ATG) genes in chemotherapy resistance in a variety of cancer types.
2.2. Autophagy and Resistance Against Targeted Agents
Advances in cellular and molecular biology and technology have paved the way for significant improvements in our knowledge of tumor biology, molecular profiling of tumors, and discovery of predictive biomarkers and molecular therapeutic targets [44,45]. These efforts have driven the evolution of cancer treatments and the rise of targeted agents that act selectively on proteins and/or genes that have been altered as part of the pathogenesis of cancer [44,45]. Two main classes of targeted agents are as follows: (i) Small molecules (usually with an “-ib” suffix), that act on cellular targets and interfere with oncogenic signaling pathways, and (ii) monoclonal antibodies (usually with a “-mab” suffix), that bind and inhibit tumor-specific and/or -associated antigens [44,45]. Although targeted therapy has succeeded in prolonging the survival of cancer patients, long-term therapeutic success, again, is limited by the development of molecular and cellular adaptations that confer treatment resistance [190,191]. Both the upregulation of autophagy in response to targeted agents and elevation of autophagy levels in cancers resistant to targeted agents have been observed in many cancer types (Table 3). There is strong pre-clinical support demonstrating that the inhibition of the autophagy process, through either pharmacological and/or genetic means, potentiates the anti-tumorigenic effects of many targeted therapies (Table 3).
Table 3.
Examples of pre-clinical studies demonstrating that autophagy and autophagy-related (ATG) genes contribute to cancer resistance to different targeted therapies.
| Targeted Agent | Cancer Types | Mode of Autophagy Inhibition | Ref. | |
|---|---|---|---|---|
| Pharmacological | Genetic | |||
| Monoclonal antibodies | ||||
| Bevacizumab (VEGF (vascular endothelial growth factor) inhibitor) |
Gliomas, Colorectal cancers, Liver cancers |
CQ, HCQ | BECN1 siRNA (small interfering Ribonucleic Acid), ATG7 shRNA (short hairpin Ribonucleic Acid) |
[113,192,193,194,195,196] |
| Trastuzumab (HER2 (human epidermal growth factor receptor 2) inhibitor) |
Breast cancers | 3-MA, Baf A1 | LC3B siRNA, ATG4B siRNA, ATG12 shRNA, ATG4B siRNA |
[197,198,199,200] |
| Cetuximab (EGFR (epidermal growth factor receptor) inhibitor) |
Vulvar cancers, Lung cancers, Head and neck cancers |
CQ, 3-MA | BECN1 siRNA, ATG7 siRNA |
[201,202,203] |
| Small molecule inhibitors | ||||
| Sorafenib (multi-kinase inhibitor—VEGFRs, PDGFRs (platelet-derived growth factor receptor), RAF (Rapidly Accelerated Fibrosarcoma) kinases) |
Endometrial cancers, Liver cancers, Kidney cancers, Gliomas, Desmoid tumors |
CQ, 3-MA, Baf A1 | BECN1 siRNA, BECN1 shRNA, ATG5 siRNA, ATG5 shRNA, miR (microRNA)-375 (ATG7 knockdown) |
[204,205,206,207,208,209,210] |
| Linifanib (multi-kinase inhibitor—VEGFRs and PDFRs) |
Liver cancers | CQ, 3-MA | ATG7 siRNA, ATG5 siRNA |
[211] |
| Sunitinib (Multi-kinase inhibitor—PDGFRs, VEGFRs, KIRs (Killer cell immunoglobulin like receptors), FLT-3 (fms like tyrosine kinase-3), CSF-1R (Colony stimulating factor 1 receptor), RET (rearranged during transfection) kinases) |
Ovarian cancers, Kidney cancers, Prostate cancers, Pancreatic cancers |
Lys05, CQ, 3-MA, Baf A1 | ATG7 siRNA, ATG5 siRNA, ATG5 shRNA, LAMP2 shRNA |
[212,213,214,215,216] |
| Gefitinib (EGFR inhibitor) |
Breast cancers, Bladder cancers, Skin cancers, Lung cancers, Liver cancers, Pancreatic cancers |
3-MA, Baf A1, CQ, HCQ | ATG12 siRNA, BECN1 siRNA, ATG7 siRNA, ATG5 siRNA, VPS34 siRNA, miR-153-3p (ATG5 knockdown) |
[217,218,219,220,221,222,223,224,225,226,227,228] |
| Osimertinib (EGFR inhibitor) |
Lung cancers, Breast cancers, Colorectal cancers |
Spautin-1, CQ, 3-MA | BECN1 siRNA, ATG5 siRNA |
[229,230,231,232,233] |
| Erlotinib (EGFR inhibitor) |
Lung cancers, Glioblastomas, Head and neck cancers |
l CQ, 3-MA, Quinacrine |
ATG5 siRNA, ATG7 siRNA, BECN1 siRNA, LC3 siRNA |
[228,234,235,236,237,238,239] |
| Everolimus (mTORC1 (mammalian target of rapamycin complex 1) inhibitor) |
Blood cancers, Kidney cancers, Bladder cancers, Breast cancer, Neuroendocrine tumors |
HCQ, CQ, Baf A1, 3-MA | - | [240,241,242,243,244,245,246,247] |
| Temsirolimus (mTORC1 inhibitor) |
Colorectal cancers, Skin cancers, Kidney cancers |
CQ, HCQ | ATG7 shRNA | [248,249,250] |
| Dactolisib/NVP-BEZ235 (Dual mTOR/Class I PI3K (phosphoinositide 3-kinase) inhibitor) |
Kidney cancers, Liver cancers, Blood cancers, Colorectal cancers, Head and neck cancers, Gliomas, Mesotheliomas, Gastric cancers, Rhabdomyosarcomas, Neuroblastomas, Lung cancers |
3-MA, CQ, Baf A1, VPS34 inhibitor (VPS34-IN1) |
ATG5 siRNA, BECN1 siRNA |
[251,252,253,254,255,256,257,258,259,260] |
| Buparlisib/BKM120 (Pan-Class I PI3K inhibitor) |
Lung cancers | CQ | - | [261] |
| Pictilisib/GDC-0941 (Pan-Class I PI3K inhibitor) |
Breast cancers | CQ | ATG5 siRNA, ATG7 siRNA |
[262] |
| Lapatinib (Dual EGFR/HER2 inhibitor) |
Breast cancers, Esophageal cancers |
CQ, 3-MA | ATG12 shRNA, ATG5 siRNA, BECN1 siRNA |
[200,263,264,265] |
| Afatinib (EGFR/HER2/HER4 inhibitor) |
Lung cancers | HCQ, 3-MA | - | [266] |
| Bortezomib (Proteasome inhibitor) |
Breast cancers, Blood cancers, Pancreatic cancers, Cervical cancers, Prostate cancers, Neuroblastomas |
3-MA, HCQ, CQ, Baf A1 | LC3B siRNA, ATG5 siRNA, P62 shRNA, GABARAPL1 shRNA, BECN1 siRNA |
[267,268,269,270,271,272,273,274,275,276] |
| Carfilzomib (Proteasome inhibitor) |
Blood cancers, Neuroblastomas |
CQ, HCQ | - | [277,278,279] |
| Vemurafenib (B-RAF inhibitor) |
Brain cancers, Skin cancers, Thyroid cancers, Colorectal cancers |
CQ, HCQ, Baf A1, Lys05 | ATG5 siRNA, ATG5 shRNA, ATG7 siRNA, ATG13 siRNA |
[280,281,282,283,284,285,286] |
| Trametinib (MEK1/2 (mitogen-activated protein kinase kinase 1/ 2) inhibitor) |
Skin cancers, Pancreatic cancers |
CQ, HCQ, PIK-III | Inactive dominant-negative ATG4BC74A | [287,288] |
| AKTi-1/2 (Dual AKT 1/2 (Protein kinase B 1/ 2) inhibitor) |
Ovarian cancers, Liver cancers, Prostate cancers |
CQ, Spautin-1, 3-MA, Baf A1 | ATG7 siRNA, ATG5 siRNA, BECN1 siRNA, BECN1 shRNA |
[289,290,291] |
| AZD5363 (AKT 1/2/3 inhibitor) |
Prostate cancers | CQ, 3-MA, Baf A1 | ATG3 siRNA, ATG7 siRNA |
[292] |
| Tamoxifen (ER (estrogen receptor) inhibitor; anti-estrogenic analog) |
Breast cancers | HCQ, Baf A1, 3-MA | ATG7 siRNA, BECN1 siRNA, LAMP3 shRNA, LC3B siRNA, ATG5 siRNA, BECN1 siRNA |
[293,294,295,296,297,298,299] |
| Imatinib (BCR-ABL (breakpoint cluster region-abelson murine leukemia viral oncogene homolog 1) inhibitor) |
Blood cancers, Gastrointestinal cancers, Colorectal cancers |
Spautin-1, CQ, HCQ, Quinacrine, Vincristine |
ATG7 siRNA, ATG12 siRNA, ATG4B shRNA, BECN1 shRNA, ATG5 shRNA, miR-30a (BECN1 and ATG5 knockdown) |
[73,300,301,302,303,304,305,306] |
| HDIL-2 (high-dose interleukin-2 immunotherapy) |
Liver cancers | CQ | - | [307,308] |
Bevacizumab is a monoclonal antibody that binds to and inhibits the cellular activity of the vascular endothelial growth factor (VEGF), a potent angiogenic factor that stimulates the formation of blood vessels. The role of autophagy in resistance to bevacizumab has been demonstrated in several cancers, including gliomas, colorectal cancers, and liver cancers [113,192,193,194,195,196]. Most recently, it has been demonstrated that treatment of glioblastomas with bevacizumab induces autophagy, and the pharmacological inhibition of autophagy, using HCQ, in combination with bevacizumab resulted in a greater mitigation of cancer cell growth compared to either treatment alone [194]. Similarly, bevacizumab treatment was also associated with an upregulation of autophagy in colorectal cancer cells, and the pharmacological or genetic inhibition of autophagy both improved the growth inhibitory and pro-apoptotic effects of bevacizumab in vitro and in vivo [192].
Autophagy inhibition has also been associated with improved responses to small molecule inhibitors, like sorafenib. Sorafenib is a multi-protein kinase inhibitor that inhibits the activity of serine/threonine and receptor tyrosine kinases, including RAF (Rapidly Accelerated Fibrosarcoma) kinases, the VEGF receptor (VEGFR), and platelet-derived growth factor receptors 2/3 (PDGFR 2/3). Recent studies in hepatocellular carcinoma (HCC) demonstrated that pharmacological or genetic inhibition of autophagy in combination with sorafenib resulted in a significant increase in apoptosis and greater reduction in tumor viability [204]. Interestingly, findings from this study were also the first to show an association between the cell surface adhesion protein CD24, sorafenib resistance, and autophagy. Elevated levels of CD24 were associated with poor HCC patient prognosis and sorafenib resistance, and the knockdown of CD24 both improved sorafenib sensitivity and reduced autophagy level [204]. More recently, pharmacological or genetic inhibition of autophagy also improved responses of desmoid tumors to sorafenib [205]. Taken together, these studies provide strong support for the role of autophagy in tumor tolerance against various targeted therapies in diverse cancers. We refer our readers to Table 3 for a more comprehensive list of examples.
2.3. Clinical Trials
To date, the only autophagy inhibitors that have been approved by the FDA and used as part of clinical trials in combination with chemotherapy and targeted therapies are the lysosomotropic agent chloroquine (CQ) and its derivative hydroxychloroquine (HCQ). The use of CQ or HCQ as a single agent in the treatment of cancers has been associated with minimal or lack of therapeutic benefit, and this is likely due, in part, to the absence of a secondary agent or stress stimulus that would otherwise induce or create a dependency on the autophagy pathway. To this end, Phase I/II clinical trials that examine the safety and efficacy of CQ or HCQ in combination with various chemotherapies and targeted therapies are underway (http://clinicaltrials.gov/) [27,309,310]. However, dose-limiting toxicities of CQ and HCQ remain a clinical challenge in some patients, with side effects that include neutropenias, retinopathies, and sepsis [27,311,312].
3. Crosstalk between Autophagy and Diverse Signaling Pathways Contributes to Treatment Resistance in Cancer
Although previous studies have provided strong evidence supporting a role of autophagy in tumor tolerance against anti-cancer therapies, the molecular mechanisms underlying this relationship remain poorly understood. Existing evidence in the literature thus far has been primarily correlative and suggests crosstalk between autophagy and various signaling pathways that aids and/or supports tumor treatment resistance [313]. Despite our limited understanding of the molecular mechanisms underlying these interplays, knowledge of autophagy-signaling pathway crosstalk has been successfully leveraged at the preclinical stage and targeted to mitigate cancer growth and progression [313].
3.1. The Contributions of Autophagy and Major Signaling Pathways to Pro-Survival Responses that Resist Anti-Cancer Therapies—Guilt by Association?
In this section, we first review the mitogen-activated protein kinase (MAPK) and phosphoinositide 3-kinase/ protein kinase B (PI3K/AKT) signaling pathways and their known links to cancer progression and therapy resistance. We then describe the associations between these common cancer-related signaling pathways and the autophagy process, along with corresponding implications for treatment resistance.
3.1.1. Mitogen-Activated Protein Kinase (MAPK) Signaling
The Role of MAPK Signaling in Cancer Progression
The MAPK signaling pathway is a convergent signaling axis that is critical for the regulation of homeostatic cell growth, proliferation, and cell fate [314]. There are 3 primary arms of MAPK signaling, as follows: (i) Extracellular signal regulated kinases (ERK) signaling, (ii) c-jun N-terminal kinases (JNK) signaling, and (iii) p38 MAPK signaling [314,315]. Each arm is activated by a host of different extracellular stimuli and regulates various downstream transcriptional targets [314,315]. Mutations in genes and aberrations in protein functions involved in MAPK signaling have been known to promote tumor cell survival, metastasis, and resistance to anticancer therapies [316]. MAPK signaling may be initiated by a variety of different growth factor receptors on the cell surface that respond to extracellular stimuli [316]. Some of these growth factor receptors are proteins that belong to the human epidermal growth factor receptor (HER) family, which include HER1, also known as epidermal growth factor receptor (EGFR), and HER2 [317]. Overexpression of or mutations in EGFR and HER2 have been widely observed in certain cancers, like lung [318] and breast [319], and have been associated with tumorigenic activation of MAPK signaling.
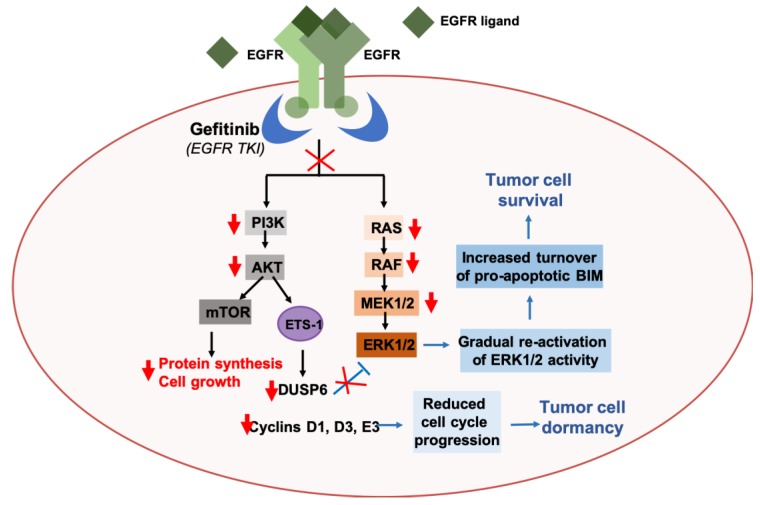
Approximately 14% of non-small cell lung cancer (NSCLC) patients harbor activating mutations in EGFR, yet do not achieve significant tumor reduction in response to EGFR tyrosine kinase inhibitors (TKIs) [320]. It was previously demonstrated that treatment with EGFR TKIs is associated with gradual re-activation of MAPK signaling in cell line models of NSCLC harboring EGFR mutations, following an initial inhibition of both ERK and protein kinase B (PKB/AKT) signaling [321]. The re-activation of MAPK signaling occurs as a result of a reduction in AKT activity, which blocks the activation of the transcription factor ETS-1. Inhibition of ETS-1 activity reduces levels of the dual specificity phosphatase 6 (DUSP6), a negative regulator of ERK1/2, and this consequently allows for the gradual reactivation of ERK1/2. Overall, this leads to tumor cell dormancy, as a result of reduced expression of ETS-1 target genes that are involved in cell cycle regulation, and survival of NSCLC cells, through sustained ERK1/2 activity and increased turnover of the pro-apoptotic protein, B-cell lymphoma-2-like protein 11 (BIM) (Figure 1) [321]. Results from this study demonstrate that MAPK/ERK signaling plays an important role in cancer cell survival and growth and suggest a novel crosstalk between MAPK and AKT signaling that contributes to innate resistance of NSCLCs to EGFR TKIs. We refer our readers to recent reviews that cover the various other mechanisms of resistance to EGFR TKIs in cancers in greater detail [322,323,324,325]. Clinical trials investigating the potential of targeting MAPK/ERK signaling in NSCLC patients are currently underway, with the recent clinical approval of the combined use of the Raf inhibitor dafarenib, and the MEK inhibitor trametinib, in patients with metastatic NSCLC [326,327].
Figure 1.
Reactivation of ERK signaling via AKT-ETS-1-mediated positive feedback loop contributes to resistance to the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI), Gefitinib, in non-small cell lung cancers (NSCLCs). Gefitinib treatment inhibits EGFR-mediated activation of AKT and ERK1/2 signaling in NSCLCs. Reduced AKT signaling inhibits the activation of the E26 transformation-specific (ETS) transcription factor, Ets-1. Ets-1 is responsible for the transcriptional upregulation of dual specificity phosphatase 6 (DUSP6), a negative regulator of ERK1/2 activity. Reduced DUSP6 levels therefore result in a gradual reactivation of ERK1/2 activity, which promotes the turnover of the pro-apoptotic protein, BIM, and consequently supports tumor cell survival. Reduced Ets-1 activity also leads to a decrease in the transcriptional upregulation of cell cycle regulatory proteins, like cyclins D1, D3, and E3, and this consequently leads to tumor cell dormancy [321].
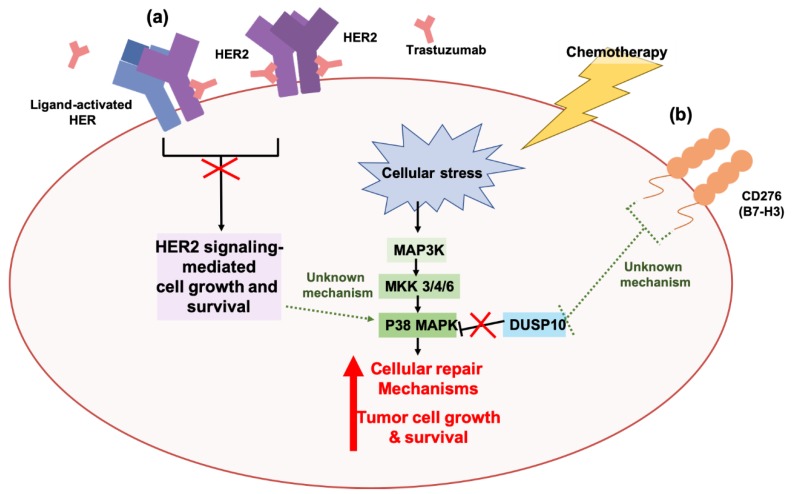
Similarly, the HER2 protein is overexpressed in approximately 25% of breast cancer patients [328]. Although patient survival outcomes have significantly improved since the development and approval of the anti-HER2 targeted agent trastuzumab, the issue of treatment resistance still remains a challenge in advanced/metastatic cases of HER2+ breast cancer patients [329,330]. Previous studies have demonstrated that the p38 MAPK facilitates resistance to trastuzumab in breast cancers that overexpress the HER2 protein [331]. Both pharmacological and genetic inhibition of p38 MAPK sensitized trastuzumab-refractory HER2+ breast cancers that exhibit elevated activation of p38 MAPK to trastuzumab [331]. Genetic induction of p38 MAPK activation was also shown to increase cellular invasiveness and confer tolerance to trastuzumab in cells previously sensitive to trastuzumab [331], supporting the role of p38 MAPK signaling in promoting the tumorigenic potential of HER2+ breast cancers and their tolerance to trastuzumab (Figure 2). We refer our readers to recent reviews that cover the various other mechanisms of resistance to trastuzumab in cancers in greater detail [329,332,333,334]. More recently, p38 MAPK was also implicated in treatment resistance against the chemotherapeutic agents cisplatin and dacarbazine, through the immune checkpoint molecule, CD276 (B7-H3), in melanoma cells [335]. High expression of CD276 has been associated with poor patient survival in cancers, like pancreatic cancer [336] and renal cell carcinoma [337]. Genetic inhibition of CD276 increased the sensitivity of melanoma cells to cisplatin and dacarbazine. Increased levels of dual specificity protein phosphatase 10 (DUSP10), a negative regulator of p38 MAPK activity, was also observed, and genetic inhibition of DUSP10 in CD276-knockdown melanoma cells was associated with an increase in p38 MAPK activation and drug resistance. These studies suggest that a novel CD276-DUSP10-p38 MAPK axis functions in the regulation of chemoresistance in melanomas, and supports the role of p38 MAPK in chemoresistance [335] (Figure 2).
Figure 2.
The stress-activated p38 MAPK pathway contributes to tumor resistance against targeted therapies and chemotherapies in cancers. (a) Overexpression of the human epidermal growth factor receptor 2 (HER2) protein has been observed in cancers, like breast, and has been associated with the aberrant activation of growth and survival pathways, like AKT signaling and ERK signaling. The HER2-targeted antibody trastuzumab binds to the extracellular domain of HER2 and inhibits HER2 dimerization and HER2-mediated signaling events, consequently mitigating tumorigenesis. Ectopic activation of the p38 MAPK pathway in HER2-overexpressing (HER2+) breast cancers can confer resistance to trastuzumab by promoting cell growth and survival independent of HER2 activity [331]. To date, the mechanisms underlying the relationship between HER2 signaling and p38 MAPK remain unknown. (b) Resistance to chemotherapies, like cisplatin and dacarbazine, have also been associated with p38 MAPK activity in melanoma cells. Chemotherapy-induced cellular stress activates the p38 MAPK pathway, and this results in the activation of cellular repair mechanisms that promote tumor cell growth and survival. Activation of p38 MAPK is further sustained by the immune checkpoint molecule, CD276/B7-H3, which inhibits the p38 MAPK-negative regulator dual specificity protein phosphatase 10 (DUSP10) [335]. To date, the mechanistic relationship between CD276/B7-H3 activity and DUSP10 inhibition remains unknown.
Dysregulation of p38 MAPK signaling has also been reported in other cancer types and associated with poor clinical outcomes [338,339]. However, despite their clinical potential, the therapeutic value of current p38 MAPK inhibitors is limited by their high toxicities and off-target effects [340,341]. Clinical trials examining the potential of targeting the p38 MAPK pathway using novel small molecule compounds in advanced cancers are currently underway [342,343] (http://clinicaltrials.gov/).
MAPK Signaling and Autophagy: Connections to Treatment Resistance in Cancers
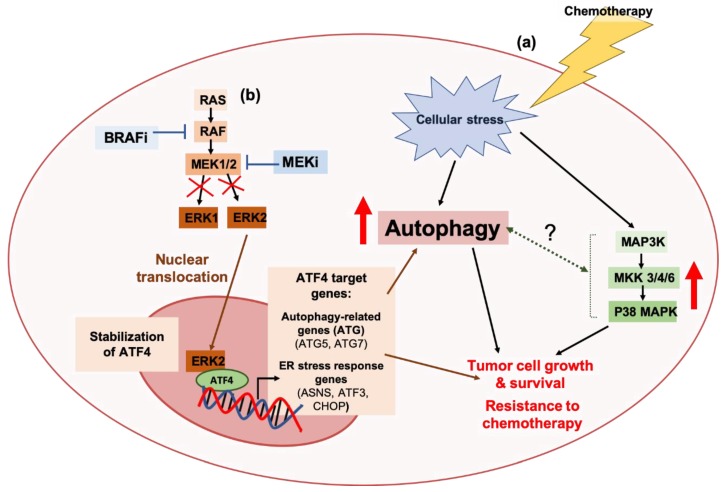
Both MAPK signaling and the autophagy pathway have been shown to promote tumor tolerance to anti-cancer therapies. Resistance to the anti-metabolite 5-fluorouracil (5-FU), which is a commonly used chemotherapy in cancers like colorectal cancers, has been linked to increased activation of p38 MAPK [344]. In such cases of chemoresistance, inhibition of p38 MAPK has been associated with elevated autophagy levels, suggesting that autophagy is upregulated under conditions of 5-FU-induced chemotherapeutic stress to compensate for loss of p38 MAPK signaling [344]. It was also demonstrated that subsequent inhibition of autophagy in p38 MAPK-deficient cancer cells was synergistic in increasing sensitivity to 5-FU, suggesting a crosstalk between the autophagy pathway and p38 MAPK signaling that confers resistance to chemotherapy [344] (Figure 3). Associations between the autophagy pathway and MAPK/ERK signaling have also been drawn and implicated in resistance to BRAF inhibitors (BRAFi) and MEK inhibitors (MEKi) in melanoma. Studies have demonstrated that, in response to BRAFi or MEKi, major signaling components of the MAPK/ERK pathway translocate initially to the endoplasmic reticulum (ER) and then to the nucleus to activate autophagy and ER stress responses [345]. Of note, it was shown that translocation of ERK2 to the nucleus aids in the stabilization of the transcription factor Activating Transcription Factor 4 (ATF4), which acts to transcriptionally activate proteins involved in ER stress response and autophagy [345]. It was further shown that patient-derived melanoma xenografts (PDX) that were resistant to combined HCQ, dabrafenib, and trametinib treatments presented with an upregulation of MAPK components in the ER, an increase in nuclear levels of activated ATF4, and an upregulation of autophagy levels when exposed to MEKi or BRAFi [345]. These observations suggest a model whereby crosstalk occurs between the autophagy pathway and MAPK/ERK signaling function to promote resistance to BRAFi and MEKi in melanomas, mediating tumor growth and survival [345] (Figure 3). Most recently, the concurrent inhibition of autophagy and ERK activity in pancreatic ductal adenocarcinomas (PDAC) was also found to be additive in suppressing tumor growth and survival both in vitro and in vivo [287,346], further suggesting a crosstalk between MAPK signaling and autophagy in promoting resistance to anti-cancer treatments [347].
Figure 3.
Associations between the autophagy pathway and MAPK signaling in to tumor tolerance against targeted therapies and chemotherapies. (a) Chemotherapeutic agents, like 5-fluorouracil, activate the p38 MAPK pathway in response to cellular stress, and thus promote cell survival in colorectal cancers. Pharmacological or genetic inhibition of p38 MAPK induces the autophagy pathway, and autophagy inhibition in p38 MAPK-deficient colorectal cancer cells potentiates the cytotoxic effects of chemotherapy [344]. To date, the relationship between autophagy regulation and the p38 MAPK remains poorly understood. (b) Crosstalk between the autophagy pathway and the ERK signaling arm of the MAPK pathway has been associated with resistance to B-RAF inhibitors (BRAFi) or MEK inhibitors (MEKi) in melanomas. BRAFi or MEKi-mediated inhibition of ERK1/2 signaling has been associated with the nuclear translocation of ERK2, and stabilization of the transcription factor, Activating Transcription Factor 4 (ATF4). This promotes the transcriptional upregulation of ATF4 target genes, like autophagy-related genes (ATGs) ATG5 and ATG7, and ER stress response genes, Asparagine synthetase 3 (ASN3), Cyclic AMP-dependent transcription factor (ATF3), and C/EBP-Homologous Protein (CHOP) [345].
To date, the actual molecular mechanisms underlying how MAPK signaling interacts with the autophagy pathway to promote tumor tolerance against anti-cancer therapies remains unclear. Regardless, at least 3 clinical trials investigating the therapeutic potential of concomitant targeting of MAPK signaling, through trametinib, and the autophagy pathway, through HCQ, in cancers are in progress (http://clinicaltrials.gov/).
3.1.2. Protein Kinase B/AKT (PKB/AKT) Pathway
The Role of PKB/AKT Signaling in Cancer Progression
The PKB pathway, hereafter referred to as the AKT pathway, is a major signaling node that also plays important roles in the regulation of various cellular processes [348]. Of the three classes of Phosphoinositide-3-Kinases (PI3Ks), AKT signaling is regulated by the class I. Class II PI3Ks primarily regulate membrane trafficking, whereas class III PI3Ks have been implicated in the regulation of both membrane trafficking and nutrient sensing [348]. Unlike class II and III, class I PI3Ks have demonstrated roles in the regulation of cellular growth, survival, and protein synthesis [348]. Class I PI3Ks (hereafter referred to as PI3Ks) are activated via signals received from activated cell surface receptors, like the G-protein coupled receptors (GPCRs), activated Ras, and the receptor tyrosine kinases EGFR and HER2. Activated PI3Ks mediate the phosphorylation of the phospholipid PtdIns (4,5) P2 to PtdIns(4,5)P3, which functions as a secondary messenger that facilitates the recruitment and activation of kinases that belong to the protein kinase A, G, and C family, like serum/glucocorticoid-regulated kinases (SGKs) and AKT. AKT is a major downstream target of PI3K activation, and is responsible for the subsequent activation of the mammalian target of rapamycin complex 1 (mTORC1), which plays a vital role in the regulation of cellular protein synthesis and survival [348].
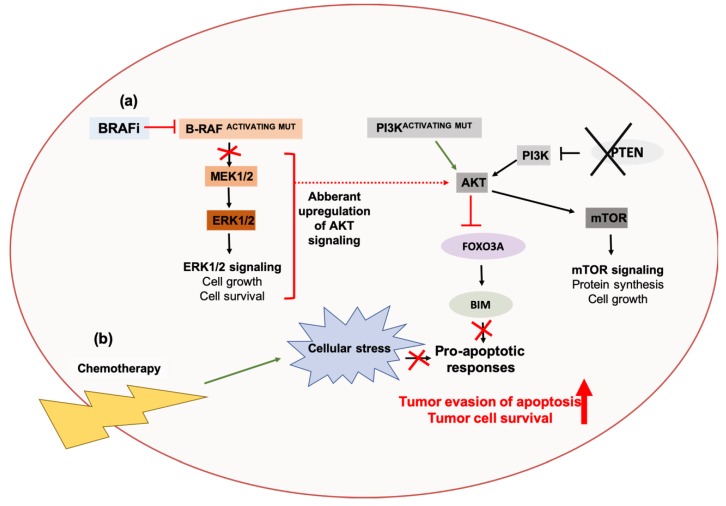
Like MAPK signaling, the AKT pathway can also be initiated by various growth factor receptors, including the HER proteins [348]. Aberrations in the regulation of AKT signaling and its pathway components have been implicated in tumorigenesis and the development of resistance to anti-cancer therapies in many cancers [349]. The phosphatase and tensin homolog (PTEN) protein is a key negative regulator of PI3K/AKT signaling, and functions as a phosphatase that inhibits AKT activity via dephosphorylation of PtdIns (4,5) P3. Loss of PTEN function is a frequent observation in many cases of melanoma and has been associated with poor clinical outcomes [350,351]. Concurrently, most patients also present with activating BRAF mutations, but a subset of such patients possess tumors that are insensitive to BRAF inhibitors [350,351]. It was previously demonstrated that PTEN is required for the upregulation of the pro-apoptotic protein, BIM, following inhibition of BRAF. In melanomas that present with concurrent PTEN loss and activating BRAFV600E mutations, BRAF inhibition results in aberrant upregulation of AKT signaling, causing constitutive AKT-mediated inhibition of the transcription factor FOXO3A, and this consequently results in a downregulation of BIM and impairment of apoptotic responses [352]. Pharmacological inhibition of both PI3K and BRAF increases BIM levels and potentiates apoptosis [352], suggesting that AKT signaling contributes to resistance of melanomas with activating BRAFv600E mutations to BRAFi (Figure 4). Mutations in the alpha catalytic subunit (PIK3CA) of PI3Ks have also been associated with first-line chemoresistance to folinic acid, fluorouracil, and oxaliplatin (FOLFOX) treatment regimens in cases of colorectal cancers [353]. Treatment of a patient-derived chemoresistant colorectal cancer cell line model with the PI3K inhibitors perifosine or LY294002, reduced tumorigenesis and sensitized resistant cells to FOLFOX both in vitro and in vivo (Figure 4) [353].
Figure 4.
The AKT signaling pathway contributes to treatment resistance against targeted therapies and chemotherapies in cancers. (a) BRAF inhibition (BRAFi) upregulates AKT activity in melanomas with concurrent PTEN loss and activating BRAFv600E mutations. This result in AKT-mediated inhibition of the transcription factor Forkhead Box O3A (FOXO3A), and reduces the transcriptional upregulation of its pro-apoptotic target gene, BIM. Combined pharmacological inhibition of BRAF activity and AKT activity, by PI3K inhibition, increases BIM expression and potentiates apoptosis, suggesting that AKT activity contributes to the resistance of BRAFV600E mutation-bearing melanomas to BRAFi [352]. (b) Activating mutations in the catalytic subunit of PI3K (PI3KCA) also contribute to resistance against chemotherapies in colorectal cancers through suppression of pro-apoptotic responses, and inhibition of PI3K can potentiate the cytotoxic effects of chemotherapy [353].
Clinical trials investigating the therapeutic benefit of various small molecule inhibitors targeting pathway components of PI3K/AKT signaling are currently underway, and show great promise [349,354,355,356]. Everolimus is a mTORC1 inhibitor that has been FDA approved for use in combination treatment of advanced and/or metastatic cases of breast cancer [357], renal cancer [358], and neuroendocrine tumors [359]. It should also be noted that, through its inhibitory effects on mTORC1, everolimus also induces the autophagy pathway [360]. This suggests that, in certain cancer contexts, autophagy can function as an anti-tumorigenic process. Clinical trials investigating the clinical benefit of everolimus in combination treatment of other cancers are also underway (http://clinicaltrials.gov/).
AKT Signaling and Autophagy: Connections to Treatment Resistance in Cancers
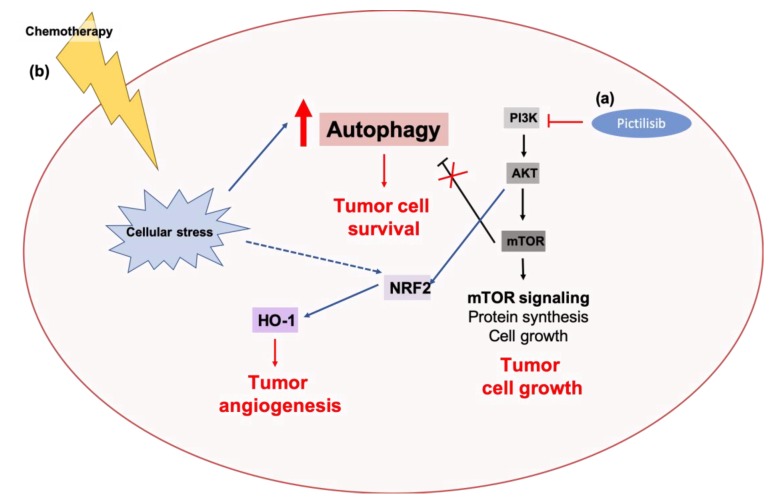
Associations between the autophagy pathway and AKT signaling have been implicated in the progression and acquisition of treatment resistance in various cancers. Studies in prostate cancer have demonstrated that the essential autophagy gene, Atg7, cooperates with PTEN loss of function aberrations to promote in vivo tumorigenesis [361]. The genetic deletion of Atg7 in mouse models of PTEN-deficient prostate cancer was associated with reduced tumor growth and elevated ER stress, suggesting a crosstalk between the autophagy pathway and hyperactivated AKT signaling in tumorigenesis [361]. It was recently demonstrated that treatment of estrogen receptor-overexpressing (ER+) breast cancer cell lines with the pan-class I PI3K inhibitor pictilisib, induces autophagy as a cytoprotective mechanism [262]. Both pharmacological inhibition of autophagy using the lysosomotropic agent, CQ, or genetic inhibition of autophagy through RNAi-mediated knockdown of ATG5 or ATG7 potentiated the pro-apoptotic and growth inhibitory effects of pictilisib in vitro and in vivo (Figure 5) [262]. Studies in triple-negative breast cancers (TNBC) also demonstrated that both the autophagy pathway and PI3K/AKT signaling contribute to resistance to anthracyclines. Treatment of TNBC cell lines with the anthracycline pharmorubicin, was associated with an increase in levels of autophagy and heme oxygenase-1 (HO-1), a cytoprotective enzyme that catalyzes the oxidation of heme to produce biological molecules, like carbon monoxide (CO), ferrous ions (Fe2+, Fe3+), and biliverdin [362]. Elevated levels of HO-1 have been associated with the growth and angiogenesis of prostate [363,364] and lung cancers [365,366]. It was also demonstrated that PI3K/AKT signaling regulates the expression levels of HO-1 in TNBC at both the mRNA- and protein-level [362]. Pharmacological inhibition of PI3K/AKT signaling with the PI3K inhibitor, LY294002, in combination with pharmorubicin was associated with an additive reduction in cell survival, autophagy, and HO-1 mRNA and protein levels [362]. These studies suggest a correlation between PI3K/AKT signaling and autophagy in the regulation of cytoprotective mechanisms and chemotherapy response (Figure 5). Previous studies have also demonstrated that the inhibition of autophagy, pharmacologically using CQ or genetically by ATG5 or ATG7 knockdown, potentiates the cytotoxic effects of the anthracycline, epirubicin, in TNBC [99]. These studies further suggest a crosstalk between the PI3K/AKT and the autophagy pathway in treatment response in cancers.
Figure 5.
Associations between AKT signaling and autophagy in tumor tolerance against targeted therapies and chemotherapies. (a) The pan-PI3K inhibitor, pictilisib, inhibits PI3K-mediated AKT activation, and results in cytoprotective autophagy. Pharmacological and genetic inhibition of autophagy potentiates the pro-apoptotic and growth inhibitory effects of pictilisib in breast cancers [262]. (b) Chemotherapy-induced cellular stress results in the activation of autophagy and the cytoprotective enzyme, heme oxygenase-1 (HO-1). HO-1 is transcriptionally upregulated by NRF2, a downstream target of AKT. Pharmacological inhibition of AKT signaling, by PI3K inhibition, potentiates the cytotoxic effects of anthracyclines, like pharmorubicin, and is associated with a reduction of autophagy and HO-1 levels [362].
To date, the molecular mechanisms underlying how AKT signaling interacts with the autophagy pathway to promote treatment resistance also remains unclear. Clinical trials examining the potential of combined targeting of the autophagy-PI3K/AKT axis in cancer are currently underway. For example, the therapeutic potential of combination treatment with everolimus and HCQ in advanced cases of renal cell carcinoma are currently undergoing mid-phase clinical trials [240]. Similarly, early clinical trials investigating the therapeutic benefit of combination treatment with the AKT inhibitor MK2206, and HCQ in various solid tumors, like melanoma, prostate, and kidney, are currently in progress [347,367]. It is important to note that treatment with everolimus [240,360] or AKT inhibition [367] both inhibit mTORC1 and induce autophagy. The ability of either in augmenting the therapeutic effects of HCQ-mediated autophagy inhibition highlights a complex relationship between AKT signaling and the regulation of autophagy, which remains to be clarified.
3.2. The Cellular Recycling and Self-Degradative Functions of Autophagy Contribute to Chemoresistance in Cancers
Despite many pre-clinical and clinical studies supporting the pro-tumorigenic roles of autophagy in various cancers, the molecular mechanisms underlying how autophagy acts to alleviate cytotoxic stresses that stem from anti-cancer treatments remain poorly understood. However, as highlighted in this section, a few studies establishing molecular contributions of autophagy in chemoresistance have recently emerged.
3.2.1. The p62-KEAP1-NRF2 Axis
p62-KEAP1-NRF2 Signaling in Cancers
The process of autophagy occurs under both basal conditions and conditions of stress. Stress-induced autophagy is usually equated with selective autophagy, which involves the removal of specific substrates recognized by autophagy cargo receptors [368,369,370]. One such autophagy cargo receptor is the ubiquitin binding protein Sequestosome 1(SQSTM1), also known as p62. p62 is a pleiotropic scaffolding protein that has been implicated in various cellular processes, and dysregulation of p62 function has been implicated in pathological diseases, like cancer [371].
NF-E2-related factor 2 (NRF2) is a major transcription factor that plays important roles in regulating cellular oxidative stress responses. The Kelch-like ECH-associated protein 1 (KEAP1) is an adaptor protein that functions as part of an ubiquitin ligase complex that is involved in cellular proteosomal degradation [371]. Under basal conditions, KEAP1 interacts with NRF2 and targets it for proteosomal degradation, thereby downregulating levels of NRF2 in the cell. The oxidation of KEAP1 under conditions of oxidative stress inhibits the interaction between KEAP1 and NRF2, and this increases the overall cellular levels of active NRF2 in the cell [372]. One major function of NRF2 in oxidative stress response is its transcriptional upregulation of genes containing the antioxidant response element (ARE) in their regulatory regions. Some of these genes encode for metabolic enzymes, stress response proteins, autophagy-related (ATG) proteins, and adaptor proteins like p62 [372].
The p62-NRF2-KEAP1 signaling axis has been implicated in promoting cancer progression through metabolic reprogramming. Studies in hepatocellular carcinoma (HCC) have previously demonstrated that the phosphoactivation of p62 is associated with elevated levels of nuclear NRF2 and an increase in the expression of various NRF2 target genes that are involved in the regulation of metabolic processes [373]. Examples include genes involved in the pentose-phosphate pathway, glutathione biosynthesis, and glutaminolysis [373]. The phosphoactivation of p62 in HCC cell lines was also associated with increased growth rates and resistance to anti-cancer agents, like sorafenib and cisplatin [373]. Similar observations regarding the pro-tumorigenic functions of the p62-NRF2-KEAP1 signaling network have been made in other cancers, like pancreatic [374], ovarian [375], and breast [376].
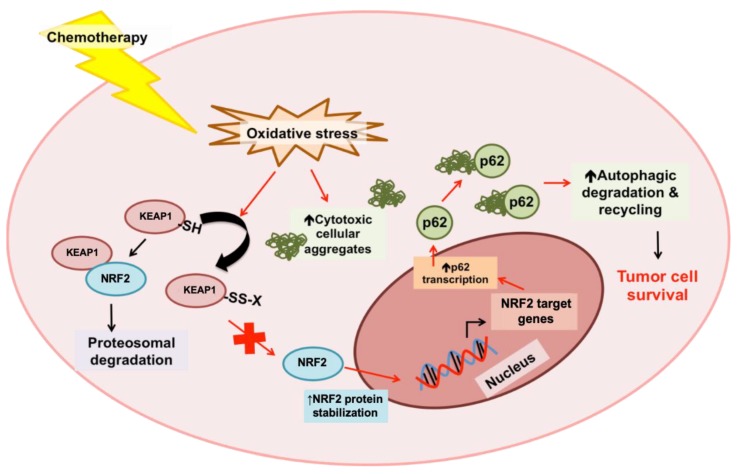
Crosstalk between Autophagy Pathway and the p62-KEAP1-NRF2 Axis in Cancer Progression and Chemoresistance
Recent studies have demonstrated that crosstalk between the autophagy process and the p62-NRF2-KEAP1 signaling axis are involved in mediating tumor tolerance to chemotherapy [377]. An increase in basal oxidative stress and elevated expression levels of NRF2 target genes, including p62, and various ATG genes were observed in epithelial cancer cell lines resistant to cisplatin, docetaxel, and 5-FU [377]. Treatment of resistant lines with chemotherapy was associated with an increase in NRF2 activity, and p62 protein levels and stability [377]. An increase in autophagy-mediated clearance of p62-bound cellular aggregates was observed in chemo-resistant cells, and both the genetic and pharmacological inhibition of autophagy sensitized resistant epithelial cancer cells to chemotherapy [377]. The genetic silencing of p62 in combination with autophagy inhibition was not associated with a further increase in chemosensitivity [377]. p62 silencing alone was associated with a reduction in chemosensitivity, whereas the expression of a truncated p62 mutant lacking ubiquitin- and LC3-binding domains, and the NRF2-activating domain significantly increased chemosensitivity [377], suggesting that the anti-cancer effect of p62 inhibition was autophagy-dependent. These studies support a model whereby KEAP1 is oxidized by chemotherapy-induced oxidative stress, which inhibits interactions between KEAP1 and NRF2 thereby stabilizing levels of the latter in the cell. This consequently results in an upregulation of the NRF2 target gene p62. The p62 adaptor protein binds to cellular aggregates that are generated as a result of chemotherapy-induced oxidative stress, and these aggregates are then degraded and recycled by autophagy. Taken together, this model proposes a functional role of autophagy in mediating the clearance of potentially cytotoxic cellular aggregates generated by chemotherapy, promoting tumor survival and chemoresistance [377] (Figure 6). Most recently, it was also demonstrated that genetic inhibition of autophagy, through ATG7 knockout, is associated with defects in proteolysis and an increase in NRF2 signaling through a p62-KEAP1 mechanism [378]. The genetic inhibition of NRF2 in autophagy-deficient cancers was associated with a greater increase in apoptosis in response to proteasome inhibition by bortezomib, compared to NRF2 inhibition or autophagy inhibition alone [378]. These studies suggest that NRF2 signaling compensates for autophagy defects in cancers, and further supports a crosstalk between the autophagy pathway and NRF2 signaling in contributing to tumor survival and treatment resistance.
Figure 6.
Autophagy mediates the clearance of p62-bound cytotoxic cellular aggregates generated by chemotherapy-induced oxidative stresses. Chemotherapy-induced oxidative stress results in the oxidation of the ubiquitin ligase complex adaptor protein, KEAP1. This inhibits the interaction between KEAP1 and the oxidative stress response transcription factor NRF2, and stabilizes cellular levels of NRF2. NRF2 transcriptionally upregulates various target genes involved in cellular anti-oxidation and stress response, like p62. The autophagy cargo receptor, p62, binds to cellular aggregates generated by chemotherapy-induced oxidative stress, and targets these cytotoxic aggregates for degradation and recycling through the process of autophagy [377].
3.2.2. The FOXO3A-PUMA Axis
FOXO3A-PUMA Signaling in Cancer
Apoptosis is a form of cell death mediated by a distinct intracellular proteolytic cascade, and its dysregulation is often associated with cancer progression and treatment resistance [379,380]. There are two main apoptotic pathways that may be induced depending on the apoptotic signal, as follows: (i) The extrinsic apoptotic pathway, which is induced by the activation of death receptors and (ii) the intrinsic apoptotic pathway, which is induced by intracellular signals in response to cellular stresses, like radiation and chemotherapy [379,380].
Death receptors involved in the extrinsic apoptotic pathway include tumor necrosis factor receptors (TNFRs), TNF receptor superfamily member 6 (TNFRSF6/FAS), and TNF-related apoptosis-inducing ligand receptors (TRAILRs) [379,380]. Death receptor activation results in the recruitment of adaptor proteins, like Fas-associated protein with death domain (FADD) and Tumor necrosis factor receptor type 1-associated DEATH domain (TRADD), that initiate the formation of a death-inducing signaling complex (DISC) by recruiting capase-8 and -10, which are protease enzymes that function as initiators of the apoptotic response. Activation of these initiator caspases is followed by the activation of the downstream effector caspases, caspase-3, -6, and -7, that cleave essential cellular substrates and potentiate cell death [379,380].
The intrinsic apoptotic cascade is induced by intracellular stress signals, like DNA damage, hypoxia, and oxidative stress, that activate members of the B-cell lymphoma 2 (Bcl-2) homology domain 3 (BH3)-only family of Bcl-2 proteins, like BH3 interacting-domain (BID) death agonist and p53 unregulated modulator of apoptosis (PUMA) [379,380]. Pro-apoptotic BH3-only Bcl-2 proteins inhibit the activity of anti-apoptotic proteins, like Bcl-2, B-cell lymphoma-extra large (Bcl-xL), and induced myeloid leukemia cell differentiation protein-1 (Mcl-1). BH3-only Bcl-2 proteins also induce the oligomerization of pro-apoptotic Bcl-2-associated X protein (BAX) and Bcl-2 antagonist or killer (BAK) in the outer mitochondrial membrane, and this results in the formation of supramolecular channels on the mitochondria, also known as mitochondrial outer membrane permeabilization (MOMP). MOMP facilitates the leakage of proteins from the mitochondrial intermembrane space that promotes cell death [379,380]. The regulation of BH-3 only Bcl-2 proteins can occur at the transcriptional level by transcription factors, like forkhead box O3A (FOXO3A) and transformation-related protein 53 (p53) [381,382,383,384].
Crosstalk between Autophagy Pathway and the FOXO3A-PUMA Axis in Cancer Progression and Chemoresistance
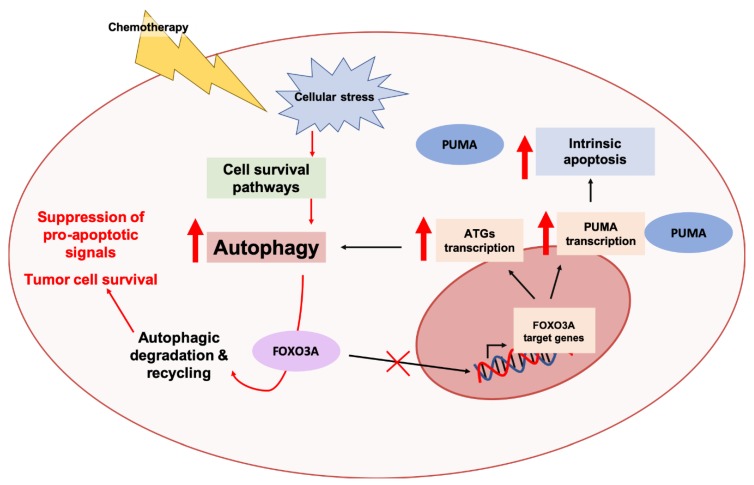
Like autophagy, the apoptotic machinery is a key catabolic process in cells and various nodes of crosstalk between these two processes have been extensively reported in the literature [385,386]. Previous studies in various cancer cell lines have demonstrated that the autophagic program is involved in regulation of the intrinsic apoptotic pathway [385,386]. Autophagy is able to temporally regulate MOMP and cellular responses post-MOMP [385,386]. Induction of autophagy was associated with delays in MOMP, and inhibition of autophagy caused a selective increase in levels of the pro-apoptotic protein PUMA [387]. Similar to autophagy induction, reduction of PUMA levels was associated with a delay in MOMP [387]. Autophagy inhibition sensitized cells to apoptosis, whereas knockdown of PUMA delayed the initiation of apoptosis and rescued cell death associated with autophagy inhibition following apoptotic stimuli [387]. These studies suggest that autophagy may regulate the kinetics and degree of intrinsic apoptosis through regulation of cellular PUMA levels [387]. The underlying mechanisms in regard to how this regulation occurs were recently uncovered using a model of colorectal cancer [189]. Genetic and pharmacological inhibition of autophagy was associated with an increase in PUMA levels at the transcriptional level independent of p53 [189]. However, this increase was not observed when FOXO3A, a transcription factor previously shown to regulate the expression of PUMA [383] and various ATG genes [388,389], was inhibited. An increase in binding of FOXO3A to an intronic response element of the PUMA gene was observed following autophagy inhibition, supporting its role in the regulation of PUMA transcription. It was also demonstrated that protein, and not mRNA, levels of FOXO3A increased following autophagy inhibition. FOXO3A localized to autolysosomes under basal conditions, and accumulated in the nucleus following autophagy inhibition [189]. Autophagy inhibition, in combination with the chemotherapeutic cytotoxic agents etoposide and doxorubicin, was associated with an increase in apoptosis only in colorectal cancer cells that expressed PUMA [189]. Collectively, these studies present a mechanistic model whereby autophagy regulates protein levels of FOXO3A, and, consequently PUMA and apoptosis. Under conditions of chemotherapy-induced stress, autophagy is upregulated and this reduces FOXO3A and PUMA levels, thereby presenting an outlet by which cancer cells evade apoptosis [189] (Figure 7).
Figure 7.
Autophagic degradation of the transcription factor FOXO3A confers tumor tolerance to pro-apoptotic signals. FOXO3A is a transcription factor involved in the transcriptional upregulation of pro-apoptotic genes, like PUMA, and genes involved in cellular stress responses, like autophagy-related genes (ATG). Autophagy is upregulated in response to chemotherapy-induced cellular stresses as a pro-survival response. Stress-induced autophagy mediates the degradation and turnover of FOXO3A, thereby greatly mitigating the transcription of genes encoding pro-apoptotic proteins, like PUMA, and reducing sensitivity to apoptosis [189].
4. Conclusions and Perspectives
Autophagy has long been considered Janus-faced in the onset and progression of cancers. It is recognized that various nodes of crosstalk between autophagy and many signaling pathways exist, and these nodes can contribute to tumor tolerance against anti-cancer treatments. As such, there has been a longstanding interest in identifying cancer contexts that may benefit from autophagy inhibition in treatment. Previous studies have established key associations between autophagy and major pathways, like MAPK and AKT signaling, that contribute to resistance to both chemo- and targeted therapies in various cancers (Figure 3 and Figure 5). Clinical trials investigating the therapeutic benefit of autophagy inhibition in combination with chemotherapy and/or targeted therapies are currently underway.
Despite these efforts, there still exists a large gap in our knowledge regarding the actual molecular mechanisms underlying how the autophagy process contributes to treatment resistance in cancers. Better understanding of the molecular contributions of autophagy to tumor tolerance against anti-cancer therapies is important for developing rational and more effective combination strategies to improve patient responses to current treatments. To date, two mechanistic models have been proposed that describe how autophagy may act to relieve apoptotic signals and cytotoxic stresses that stem from chemotherapy, thereby promoting tumor survival in treatment settings. Oxidative stress that occurs as a result of chemotherapeutic treatment generates toxic cellular aggregates that promote apoptosis [390,391]. One recent model proposed that how cancers may overcome chemotherapy-induced cell death is through stabilization of the oxidative stress response transcription factor NRF2. NRF2 upregulates the autophagy cargo receptor p62, which binds to cytotoxic cellular aggregates, and consequently delivers them to the autophagy machinery for removal [377] (Figure 6). To overcome pro-apoptotic signals activated in response to cancer treatments, autophagy may also be upregulated to promote the turnover of the pro-apoptotic transcription factor, FOXO3A [189]. This consequently reduces cellular levels of pro-apoptotic proteins, like PUMA, and promotes tumor survival and allows for tumor evasion of apoptosis [189] (Figure 7). Taken together, both these models provide strong rationale for autophagy inhibition as a potential therapeutic strategy in enhancing the cytotoxic effects of chemotherapy.
However, given the dual, context-dependent roles of autophagy in tumor onset and progression, several questions remain, as follows: What cancers are most prone to developing adaptations to circumvent autophagy inhibition strategies [378]? Is there a therapeutic window during which autophagy inhibition will be most beneficial [392,393]? What are the cellular and cancer contexts in which autophagy inhibition will be therapeutically beneficial [22,394,395,396]? Are there indirect or direct caveats to autophagy inhibition in certain cancer contexts, and how can we minimize them [395,397,398]? Are there clinical and/or molecular tumor features that will allow us to better stratify patients that may benefit from autophagy inhibition in treatment [399,400,401,402]? Furthermore, our understanding of how the crosstalk between autophagy and signaling pathways, like MAPK and PI3K/AKT, contributes to treatment resistance remains largely unknown. Understanding these signaling interplays at the molecular level is a prerequisite for identifying combination strategies in which autophagy inhibition will be beneficial in mitigating cancer progression and treatment resistance.
Acknowledgments
The authors thank Gayathri Samarasekera, Morgana J. Xu, Kevin C. Yang, Robert Camfield, and Paalini Sathiyaseelan for helpful comments on this manuscript.
Author Contributions
Literature research, C.J.H. and S.M.G.; Writing—Original Draft Preparation, C.J.H.; Writing—Review & Editing, C.J.H. and S.M.G.
Funding
The authors gratefully acknowledge support from CIHR MOP-78882 and PJT-159536 grants to S.M.G. C.J.H. was supported in part by a CIHR Canada Graduate Scholarship (CGS-M) and a SFU Molecular Biology and Biochemistry (MBB) Graduate Fellowship.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Yu L., Chen Y., Tooze S.A. Autophagy pathway: Cellular and molecular mechanisms. Autophagy. 2018;14:207–215. doi: 10.1080/15548627.2017.1378838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parzych K.R., Klionsky D.J. An Overview of Autophagy: Morphology, Mechanism, and Regulation. Antioxid. Redox Signal. 2014;20:460–473. doi: 10.1089/ars.2013.5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryter S.W., Cloonan S.M., Choi A.M.K. Autophagy: A critical regulator of cellular metabolism and homeostasis. Mol. Cells. 2013;36:7–16. doi: 10.1007/s10059-013-0140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chun Y., Kim J. Autophagy: An Essential Degradation Program for Cellular Homeostasis and Life. Cells. 2018;7:278. doi: 10.3390/cells7120278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saha S., Panigrahi D.P., Patil S., Bhutia S.K. Autophagy in health and disease: A comprehensive review. Biomed. Pharmacother. 2018;104:485–495. doi: 10.1016/j.biopha.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Levine B., Kroemer G. Biological Functions of Autophagy Genes: A Disease Perspective. Cell. 2019;176:11–42. doi: 10.1016/j.cell.2018.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amaravadi R., Kimmelman A.C., White E. Recent insights into the function of autophagy in cancer. Genes Dev. 2016;30:1913–1930. doi: 10.1101/gad.287524.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Santana-Codina N., Mancias J.D., Kimmelman A.C. The Role of Autophagy in Cancer. Annu. Rev. Cancer Biol. 2017;1:19–39. doi: 10.1146/annurev-cancerbio-041816-122338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vessoni A.T., Filippi-Chiela E.C., Menck C.F., Lenz G. Autophagy and genomic integrity. Cell Death Differ. 2013;20:1444–1454. doi: 10.1038/cdd.2013.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eliopoulos A.G., Havaki S., Gorgoulis V.G. DNA Damage Response and Autophagy: A Meaningful Partnership. Front. Genet. 2016;7:59. doi: 10.3389/fgene.2016.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galluzzi L., Pedro J.M.B.-S., Kroemer G. Autophagy Mediates Tumor Suppression via Cellular Senescence. Trends Cell Biol. 2016;26:1–3. doi: 10.1016/j.tcb.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Zhao G.S., Gao Z.R., Zhang Q., Tang X.F., Lv Y.F., Zhang Z.S., Zhang Y., Tan Q.L., Peng D.B., Jiang D.M., et al. TSSC3 promotes autophagy via inactivating the Src-mediated PI3K/AKT/mTOR pathway to suppress tumorigenesis and metastasis in osteosarcoma, and predicts a favorable prognosis. J. Exp. Clin. Cancer Res. 2018;37:188. doi: 10.1186/s13046-018-0856-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Slobodnyuk K., Radic N., Ivanova S., Llado A., Trempolec N., Zorzano A., Nebreda A.R. Autophagy-induced senescence is regulated by p38α signaling. Cell Death Dis. 2019;10:1–18. doi: 10.1038/s41419-019-1607-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vera-Ramirez L., Vodnala S.K., Nini R., Hunter K.W., Green J.E. Autophagy promotes the survival of dormant breast cancer cells and metastatic tumour recurrence. Nat. Commun. 2018;9:1–12. doi: 10.1038/s41467-018-04070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu Y., Xia X., Pan H. Active autophagy in the tumor microenvironment: A novel mechanism for cancer metastasis (Review) Oncol. Lett. 2013;5:411–416. doi: 10.3892/ol.2012.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimmelman A.C., White E. Autophagy and Tumor Metabolism. Cell Metab. 2017;25:1037–1043. doi: 10.1016/j.cmet.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giuliani C.M., Dass C.R. Metabolic stress and cancer: Is autophagy the common denominator and a feasible target? J. Pharm. Pharmacol. 2014;66:597–614. doi: 10.1111/jphp.12191. [DOI] [PubMed] [Google Scholar]
- 18.Yu Z., Yu Z., Chen Z., Yang L., Ma M., Lu S., Wang C., Teng C., Nie Y. Zinc chelator TPEN induces pancreatic cancer cell death through causing oxidative stress and inhibiting cell autophagy. J. Cell. Physiol. 2019;234:20648–20661. doi: 10.1002/jcp.28670. [DOI] [PubMed] [Google Scholar]
- 19.Zhou W., Xu G., Wang Y., Xu Z., Liu X., Xu X., Ren G., Tian K. Oxidative stress induced autophagy in cancer associated fibroblast enhances proliferation and metabolism of colorectal cancer cells. Cell Cycle. 2017;16:73–81. doi: 10.1080/15384101.2016.1252882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo J.Y., Teng X., Laddha S.V., Ma S., Van Nostrand S.C., Yang Y., Khor S., Chan C.S., Rabinowitz J.D., White E. Autophagy provides metabolic substrates to maintain energy charge and nucleotide pools in Ras-driven lung cancer cells. Genes Dev. 2016;30:1704–1717. doi: 10.1101/gad.283416.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amaravadi R.K., Kimmelman A.C., Debnath J. Targeting Autophagy in Cancer: Recent Advances and Future Directions. Cancer Discov. 2019 doi: 10.1158/2159-8290.CD-19-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Folkerts H., Hilgendorf S., Vellenga E., Bremer E., Wiersma V.R. The multifaceted role of autophagy in cancer and the microenvironment. Med. Res. Rev. 2019;39:517–560. doi: 10.1002/med.21531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhat P., Kriel J., Shubha Priya B., Basappa, Shivananju N.S., Loos B. Modulating autophagy in cancer therapy: Advancements and challenges for cancer cell death sensitization. Biochem. Pharmacol. 2018;147:170–182. doi: 10.1016/j.bcp.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 24.Onorati A.V., Dyczynski M., Ojha R., Amaravadi R.K. Targeting autophagy in cancer. Cancer. 2018;124:3307–3318. doi: 10.1002/cncr.31335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levy J.M.M., Towers C.G., Thorburn A. Targeting autophagy in cancer. Nat. Rev. Cancer. 2017;17:528–542. doi: 10.1038/nrc.2017.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khandia R., Dadar M., Munjal A., Dhama K., Karthik K., Tiwari R., Yatoo M.I., Iqbal H.M.N., Singh K.P., Joshi S.K., et al. A Comprehensive Review of Autophagy and Its Various Roles in Infectious, Non-Infectious, and Lifestyle Diseases: Current Knowledge and Prospects for Disease Prevention, Novel Drug Design, and Therapy. Cells. 2019;8:674. doi: 10.3390/cells8070674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu R., Ji Z., Xu C., Zhu J. The clinical value of using chloroquine or hydroxychloroquine as autophagy inhibitors in the treatment of cancers: A systematic review and meta-analysis. Medicine. 2018;97:e12912. doi: 10.1097/MD.0000000000012912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maiuri M.C., Kroemer G. Therapeutic modulation of autophagy: Which disease comes first? Cell Death Differ. 2019;26:680–689. doi: 10.1038/s41418-019-0290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dagogo-Jack I., Shaw A.T. Tumour heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 2018;15:81–94. doi: 10.1038/nrclinonc.2017.166. [DOI] [PubMed] [Google Scholar]
- 30.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Wang J., Seebacher N., Shi H., Kan Q., Duan Z. Novel strategies to prevent the development of multidrug resistance (MDR) in cancer. Oncotarget. 2017;8:84559–84571. doi: 10.18632/oncotarget.19187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hansen E., Woods R.J., Read A.F. How to Use a Chemotherapeutic Agent When Resistance to It Threatens the Patient. PLoS Biol. 2017;15:e2001110. doi: 10.1371/journal.pbio.2001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hawkes N. Drug resistance: The next target for cancer treatment. BMJ. 2019;365:l2228. doi: 10.1136/bmj.l2228. [DOI] [PubMed] [Google Scholar]
- 34.Greene J.M., Gevertz J.L., Sontag E.D. A mathematical approach to differentiate spontaneous and induced evolution to drug resistance during cancer treatment. bioRxiv. 2018 doi: 10.1200/CCI.18.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hasan S., Taha R., Omri H.E. Current Opinions on Chemoresistance: An Overview. Bioinformation. 2018;14:80–85. doi: 10.6026/97320630014080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Panda M., Biswal B.K. Cell signaling and cancer: A mechanistic insight into drug resistance. Mol. Biol. Rep. 2019 doi: 10.1007/s11033-019-04958-6. [DOI] [PubMed] [Google Scholar]
- 37.Zheng H.C. The molecular mechanisms of chemoresistance in cancers. Oncotarget. 2017;8:59950–59964. doi: 10.18632/oncotarget.19048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zahreddine H., Borden K. Mechanisms and insights into drug resistance in cancer. Front. Pharmacol. 2013 doi: 10.3389/fphar.2013.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parseghian C.M., Napolitano S., Loree J.M., Kopetz S. Mechanisms of Innate and Acquired Resistance to anti-EGFR therapy: A Review of Current Knowledge with a Focus on Rechallenge Therapies. Clin. Cancer Res. 2019 doi: 10.1158/1078-0432.CCR-19-0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salgia R., Kulkarni P. The Genetic/Non-genetic Duality of Drug ‘Resistance’ in Cancer. Trends Cancer. 2018;4:110–118. doi: 10.1016/j.trecan.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hammerlindl H., Schaider H. Tumor cell-intrinsic phenotypic plasticity facilitates adaptive cellular reprogramming driving acquired drug resistance. J. Cell Commun. Signal. 2018;12:133–141. doi: 10.1007/s12079-017-0435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nikolaou M., Pavlopoulou A., Georgakilas A.G., Kyrodimos E. The challenge of drug resistance in cancer treatment: A current overview. Clin. Exp. Metastasis. 2018;35:309–318. doi: 10.1007/s10585-018-9903-0. [DOI] [PubMed] [Google Scholar]
- 43.Chatterjee N., Bivona T.G. Polytherapy and Targeted Cancer Drug Resistance. Trends Cancer. 2019;5:170–182. doi: 10.1016/j.trecan.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Falzone L., Salomone S., Libra M. Evolution of Cancer Pharmacological Treatments at the Turn of the Third Millennium. Front. Pharmacol. 2018:9. doi: 10.3389/fphar.2018.01300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Masui K., Gini B., Wykosky J., Zanca C., Mischel P.S., Furnari F.B., Cavenee W.K. A tale of two approaches: Complementary mechanisms of cytotoxic and targeted therapy resistance may inform next-generation cancer treatments. Carcinogenesis. 2013;34:725–738. doi: 10.1093/carcin/bgt086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McAfee Q., Zhang Z., Samanta A., Levi S.M., Ma X.-H., Piao S., Lynch J.P., Uehara T., Sepulveda A.R., Davis L.E., et al. Autophagy inhibitor Lys05 has single-agent antitumor activity and reproduces the phenotype of a genetic autophagy deficiency. Proc. Natl. Acad. Sci. USA. 2012;109:8253–8258. doi: 10.1073/pnas.1118193109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Amaravadi R.K., Winkler J.D. Lys05: A new lysosomal autophagy inhibitor. Autophagy. 2012;8:1383–1384. doi: 10.4161/auto.20958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mauthe M., Orhon I., Rocchi C., Zhou X., Luhr M., Hijlkema K.-J., Coppes R.P., Engedal N., Mari M., Reggiori F. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14:1435–1455. doi: 10.1080/15548627.2018.1474314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Golden E.B., Cho H.-Y., Hofman F.M., Louie S.G., Schönthal A.H., Chen T.C. Quinoline-based antimalarial drugs: A novel class of autophagy inhibitors. Neurosurg Focus. 2015;38:E12. doi: 10.3171/2014.12.FOCUS14748. [DOI] [PubMed] [Google Scholar]
- 50.Guntuku L., Gangasani J.K., Thummuri D., Borkar R.M., Manavathi B., Ragampeta S., Vaidya J.R., Sistla R., Vegi N.G.M. IITZ-01, a novel potent lysosomotropic autophagy inhibitor, has single-agent antitumor efficacy in triple-negative breast cancer in vitro and in vivo. Oncogene. 2019;38:581–595. doi: 10.1038/s41388-018-0446-2. [DOI] [PubMed] [Google Scholar]
- 51.Nawrocki S.T., Han Y., Visconte V., Przychodzen B., Espitia C.M., Phillips J., Anwer F., Advani A., Carraway H.E., Kelly K.R., et al. The novel autophagy inhibitor ROC-325 augments the antileukemic activity of azacitidine. Leukemia. 2019:1–4. doi: 10.1038/s41375-019-0529-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carew J.S., Espitia C.M., Zhao W., Han Y., Visconte V., Phillips J., Nawrocki S.T. Disruption of Autophagic Degradation with ROC-325 Antagonizes Renal Cell Carcinoma Pathogenesis. Clin. Cancer Res. 2017;23:2869–2879. doi: 10.1158/1078-0432.CCR-16-1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carew J.S., Nawrocki S.T. Drain the lysosome: Development of the novel orally available autophagy inhibitor ROC-325. Autophagy. 2017;13:765–766. doi: 10.1080/15548627.2017.1280222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mauvezin C., Neufeld T.P. Bafilomycin A1 disrupts autophagic flux by inhibiting both V-ATPase-dependent acidification and Ca-P60A/SERCA-dependent autophagosome-lysosome fusion. Autophagy. 2015;11:1437–1438. doi: 10.1080/15548627.2015.1066957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paha J., Kanjanasirirat P., Munyoo B., Tuchinda P., Suvannang N., Nantasenamat C., Boonyarattanakalin K., Kittakoop P., Srikor S., Kongklad G., et al. A novel potent autophagy inhibitor ECDD-S27 targets vacuolar ATPase and inhibits cancer cell survival. Sci. Rep. 2019;9:1–16. doi: 10.1038/s41598-019-45641-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang L., Qiang P., Yu J., Miao Y., Chen Z., Qu J., Zhao Q., Chen Z., Liu Y., Yao X., et al. Identification of compound CA-5f as a novel late-stage autophagy inhibitor with potent anti-tumor effect against non-small cell lung cancer. Autophagy. 2019;15:391–406. doi: 10.1080/15548627.2018.1511503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vats S., Manjithaya R. A reversible autophagy inhibitor blocks autophagosome-lysosome fusion by preventing Stx17 loading onto autophagosomes. MBoC. 2019;30:2283–2295. doi: 10.1091/mbc.E18-08-0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Choi Y.J., Park Y.J., Park J.Y., Jeong H.O., Kim D.H., Ha Y.M., Kim J.M., Song Y.M., Heo H.S., Yu B.P., et al. Inhibitory effect of mTOR activator MHY1485 on autophagy: Suppression of lysosomal fusion. PLoS ONE. 2012;7:e43418. doi: 10.1371/journal.pone.0043418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sato K., Tsuchihara K., Fujii S., Sugiyama M., Goya T., Atomi Y., Ueno T., Ochiai A., Esumi H. Autophagy is activated in colorectal cancer cells and contributes to the tolerance to nutrient deprivation. Cancer Res. 2007;67:9677–9684. doi: 10.1158/0008-5472.CAN-07-1462. [DOI] [PubMed] [Google Scholar]
- 60.Hwang K.E., Kim Y.S., Jung J.W., Kwon S.J., Park D.S., Cha B.K., Oh S.H., Yoon K.H., Jeong E.T., Kim H.R. Inhibition of autophagy potentiates pemetrexed and simvastatin-induced apoptotic cell death in malignant mesothelioma and non-small cell lung cancer cells. Oncotarget. 2015;6:29482–29496. doi: 10.18632/oncotarget.5022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhan Y., Wang K., Li Q., Zou Y., Chen B., Gong Q., Ho H.I., Yin T., Zhang F., Lu Y., et al. The Novel Autophagy Inhibitor Alpha-Hederin Promoted Paclitaxel Cytotoxicity by Increasing Reactive Oxygen Species Accumulation in Non-Small Cell Lung Cancer Cells. Int. J. Mol. Sci. 2018;19:3221. doi: 10.3390/ijms19103221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dyczynski M., Yu Y., Otrocka M., Parpal S., Braga T., Henley A.B., Zazzi H., Lerner M., Wennerberg K., Viklund J., et al. Targeting autophagy by small molecule inhibitors of vacuolar protein sorting 34 (Vps34) improves the sensitivity of breast cancer cells to Sunitinib. Cancer Lett. 2018;435:32–43. doi: 10.1016/j.canlet.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 63.Ronan B., Flamand O., Vescovi L., Dureuil C., Durand L., Fassy F., Bachelot M.-F., Lamberton A., Mathieu M., Bertrand T., et al. A highly potent and selective Vps34 inhibitor alters vesicle trafficking and autophagy. Nat. Chem. Biol. 2014;10:1013–1019. doi: 10.1038/nchembio.1681. [DOI] [PubMed] [Google Scholar]
- 64.Dowdle W.E., Nyfeler B., Nagel J., Elling R.A., Liu S., Triantafellow E., Menon S., Wang Z., Honda A., Pardee G., et al. Selective VPS34 inhibitor blocks autophagy and uncovers a role for NCOA4 in ferritin degradation and iron homeostasis in vivo. Nat. Cell Biol. 2014;16:1069–1079. doi: 10.1038/ncb3053. [DOI] [PubMed] [Google Scholar]
- 65.Robke L., Laraia L., Carnero Corrales M.A., Konstantinidis G., Muroi M., Richters A., Winzker M., Engbring T., Tomassi S., Watanabe N., et al. Phenotypic Identification of a Novel Autophagy Inhibitor Chemotype Targeting Lipid Kinase VPS34. Angew. Chem. Int. Ed. Engl. 2017;56:8153–8157. doi: 10.1002/anie.201703738. [DOI] [PubMed] [Google Scholar]
- 66.Egan D.F., Chun M.G.H., Vamos M., Zou H., Rong J., Miller C.J., Lou H.J., Raveendra-Panickar D., Yang C.C., Sheffler D.J., et al. Small Molecule Inhibition of the Autophagy Kinase ULK1 and Identification of ULK1 Substrates. Mol. Cell. 2015;59:285–297. doi: 10.1016/j.molcel.2015.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martin K.R., Celano S.L., Solitro A.R., Gunaydin H., Scott M., O’Hagan R.C., Shumway S.D., Fuller P., MacKeigan J.P. A Potent and Selective ULK1 Inhibitor Suppresses Autophagy and Sensitizes Cancer Cells to Nutrient Stress. iScience. 2018;8:74–84. doi: 10.1016/j.isci.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Blommaart E.F., Krause U., Schellens J.P., Meijer A.J. The phosphatidylinositol 3-kinase inhibitors wortmannin and LY294002 inhibit autophagy in isolated rat hepatocytes. Eur. J. Biochem. 1997;243:240–246. doi: 10.1111/j.1432-1033.1997.0240a.x. [DOI] [PubMed] [Google Scholar]
- 69.Feng Y., Gao Y., Wang D., Xu Z., Sun W., Ren P. Autophagy Inhibitor (LY294002) and 5-fluorouracil (5-FU) Combination-Based Nanoliposome for Enhanced Efficacy Against Esophageal Squamous Cell Carcinoma. Nanoscale Res. Lett. 2018:13. doi: 10.1186/s11671-018-2716-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu YT., Tan H.L., Shui G., Bauvy C., Huang Q., Wenk M.R., Ong C.N., Codogno P., Shen H.M. Dual role of 3-methyladenine in modulation of autophagy via different temporal patterns of inhibition on class I and III phosphoinositide 3-kinase. J. Biol. Chem. 2010;285:10850–10861. doi: 10.1074/jbc.M109.080796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Arcaro A., Wymann M.P. Wortmannin is a potent phosphatidylinositol 3-kinase inhibitor: The role of phosphatidylinositol 3,4,5-trisphosphate in neutrophil responses. Biochem. J. 1993;296:297–301. doi: 10.1042/bj2960297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang Y., Hu L., Zheng H., Mao C., Hu W., Xiong K., Wang F., Liu C. Application and interpretation of current autophagy inhibitors and activators. Acta Pharmacol. Sin. 2013;34:625–635. doi: 10.1038/aps.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shao S., Li S., Qin Y., Wang X., Yang Y., Bai H., Zhou L., Zhao C., Wang C. Spautin-1, a novel autophagy inhibitor, enhances imatinib-induced apoptosis in chronic myeloid leukemia. Int. J. Oncol. 2014;44:1661–1668. doi: 10.3892/ijo.2014.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu J., Xia H., Kim M., Xu L., Li Y., Zhang L., Cai Y., Norberg H.V., Zhang T., Furuya T., et al. Beclin1 controls the levels of p53 by regulating the deubiquitination activity of USP10 and USP13. Cell. 2011;147:223–234. doi: 10.1016/j.cell.2011.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Akin D., Wang S.K., Habibzadegah-Tari P., Law B., Ostrov D., Li M., Yin X.-M., Kim J.-S., Horenstein N., Dunn W.A. A novel ATG4B antagonist inhibits autophagy and has a negative impact on osteosarcoma tumors. Autophagy. 2014;10:2021–2035. doi: 10.4161/auto.32229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kurdi A., Cleenewerck M., Vangestel C., Lyssens S., Declercq W., Timmermans J.-P., Stroobants S., Augustyns K., De Meyer G.R.Y., Van Der Veken P., et al. ATG4B inhibitors with a benzotropolone core structure block autophagy and augment efficiency of chemotherapy in mice. Biochem. Pharmacol. 2017;138:150–162. doi: 10.1016/j.bcp.2017.06.119. [DOI] [PubMed] [Google Scholar]
- 77.Robke L., Rodrigues T., Schröder P., Foley D.J., Bernardes G.J.L., Laraia L., Waldmann H. Discovery of 2,4-dimethoxypyridines as novel autophagy inhibitors. Tetrahedron. 2018;74:4531–4537. doi: 10.1016/j.tet.2018.07.021. [DOI] [Google Scholar]
- 78.Liu P.F., Tsai K.L., Hsu C.J., Tsai W.L., Cheng J.S., Chang H.W., Shiau C.W., Goan Y.G., Tseng H.H., Wu C.H., et al. Drug Repurposing Screening Identifies Tioconazole as an ATG4 Inhibitor that Suppresses Autophagy and Sensitizes Cancer Cells to Chemotherapy. Theranostics. 2018;8:830–845. doi: 10.7150/thno.22012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bosc D., Vezenkov L., Bortnik S., An J., Xu J., Choutka C., Hannigan A.M., Kovacic S., Loo S., Clark P.G.K., et al. A new quinoline-based chemical probe inhibits the autophagy-related cysteine protease ATG4B. Sci. Rep. 2018;8:11653. doi: 10.1038/s41598-018-29900-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fu Y., Hong L., Xu J., Zhong G., Gu Q., Gu Q., Guan Y., Zheng X., Dai Q., Luo X., et al. Discovery of a small molecule targeting autophagy via ATG4B inhibition and cell death of colorectal cancer cells in vitro and in vivo. Autophagy. 2019;15:295–311. doi: 10.1080/15548627.2018.1517073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chang H.W., Liu P.F., Tsai W.L., Hu W.H., Hu Y.C., Yang H.C., Lin W.Y., Weng J.R., Shu C.W. Xanthium strumarium Fruit Extract Inhibits ATG4B and Diminishes the Proliferation and Metastatic Characteristics of Colorectal Cancer Cells. Toxins. 2019;11:313. doi: 10.3390/toxins11060313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Donohue E., Tovey A., Vogl A.W., Arns S., Sternberg E., Young R.N., Roberge M. Inhibition of autophagosome formation by the benzoporphyrin derivative verteporfin. J. Biol. Chem. 2011;286:7290–7300. doi: 10.1074/jbc.M110.139915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lin J.F., Lin Y.C., Tsai T.F., Chen H.E., Chou K.Y., Hwang T.I.S. Cisplatin induces protective autophagy through activation of BECN1 in human bladder cancer cells. Drug Des. Dev. Ther. 2017;11:1517–1533. doi: 10.2147/DDDT.S126464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ojha R., Jha V., Singh S.K., Bhattacharyya S. Autophagy inhibition suppresses the tumorigenic potential of cancer stem cell enriched side population in bladder cancer. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2014;1842:2073–2086. doi: 10.1016/j.bbadis.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 85.Yin H., Yang X., Gu W., Liu Y., Li X., Huang X., Zhu X., Tao Y., Gou X., He W. HMGB1-mediated autophagy attenuates gemcitabine-induced apoptosis in bladder cancer cells involving JNK and ERK activation. Oncotarget. 2017;8:71642–71656. doi: 10.18632/oncotarget.17796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mani J., Vallo S., Rakel S., Antonietti P., Gessler F., Blaheta R., Bartsch G., Michaelis M., Cinatl J., Haferkamp A., et al. Chemoresistance is associated with increased cytoprotective autophagy and diminished apoptosis in bladder cancer cells treated with the BH3 mimetic (-)-Gossypol (AT-101) BMC Cancer. 2015;15:224. doi: 10.1186/s12885-015-1239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li K., Chen X., Liu C., Gu P., Li Z., Wu S., Xu K., Lin T., Huang J. Pirarubicin induces an autophagic cytoprotective response through suppression of the mammalian target of rapamycin signaling pathway in human bladder cancer cells. Biochem. Biophys. Res. Commun. 2015;460:380–385. doi: 10.1016/j.bbrc.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 88.Jiang K., Zhang C., Yu B., Chen B., Liu Z., Hou C., Wang F., Shen H., Chen Z. Autophagic degradation of FOXO3a represses the expression of PUMA to block cell apoptosis in cisplatin-resistant osteosarcoma cells. Am. J. Cancer Res. 2017;7:1407–1422. [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang W., Li Q., Song C., Lao L. Knockdown of autophagy-related protein 6, Beclin-1, decreases cell growth, invasion, and metastasis and has a positive effect on chemotherapy-induced cytotoxicity in osteosarcoma cells. Tumour Biol. 2015;36:2531–2539. doi: 10.1007/s13277-014-2868-y. [DOI] [PubMed] [Google Scholar]
- 90.Schott C.R., Ludwig L., Mutsaers A.J., Foster R.A., Wood G.A. The autophagy inhibitor spautin-1, either alone or combined with doxorubicin, decreases cell survival and colony formation in canine appendicular osteosarcoma cells. PLoS ONE. 2018;13:e0206427. doi: 10.1371/journal.pone.0206427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wu W., Li W., Zhou Y., Zhang C. Inhibition of beclin1 affects the chemotherapeutic sensitivity of osteosarcoma. Int. J. Clin. Exp. Pathol. 2014;7:7114–7122. [PMC free article] [PubMed] [Google Scholar]
- 92.Chen R., Li X., He B., Hu W. MicroRNA-410 regulates autophagy-related gene ATG16L1 expression and enhances chemosensitivity via autophagy inhibition in osteosarcoma. Mol. Med. Rep. 2017;15:1326–1334. doi: 10.3892/mmr.2017.6149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhao Z., Tao L., Shen C., Liu B., Yang Z., Tao H. Silencing of Barkor/ATG14 sensitizes osteosarcoma cells to cisplatin-induced apoptosis. Int. J. Mol. Med. 2014;33:271–276. doi: 10.3892/ijmm.2013.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shen C., Wang W., Tao L., Liu B., Yang Z., Tao H. Chloroquine blocks the autophagic process in cisplatin-resistant osteosarcoma cells by regulating the expression of p62/SQSTM1. Int. J. Mol. Med. 2013;32:448–456. doi: 10.3892/ijmm.2013.1399. [DOI] [PubMed] [Google Scholar]
- 95.Kim M., Jung J.Y., Choi S., Lee H., Morales L.D., Koh J.T., Kim S.H., Choi Y.D., Choi C., Slaga T.J., et al. GFRA1 promotes cisplatin-induced chemoresistance in osteosarcoma by inducing autophagy. Autophagy. 2017;13:149–168. doi: 10.1080/15548627.2016.1239676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhao D., Yuan H., Yi F., Meng C., Zhu Q. Autophagy prevents doxorubicin-induced apoptosis in osteosarcoma. Mol. Med. Rep. 2014;9:1975–1981. doi: 10.3892/mmr.2014.2055. [DOI] [PubMed] [Google Scholar]
- 97.Kim H.J., Lee S.G., Kim Y.J., Park J.E., Lee K.Y., Yoo Y.H., Kim J.M. Cytoprotective role of autophagy during paclitaxel-induced apoptosis in Saos-2 osteosarcoma cells. Int. J. Oncol. 2013;42:1985–1992. doi: 10.3892/ijo.2013.1884. [DOI] [PubMed] [Google Scholar]
- 98.Guo Y., Huang C., Li G., Chen T., Li J., Huang Z. Paxilitaxel induces apoptosis accompanied by protective autophagy in osteosarcoma cells through hypoxia-inducible factor-1α pathway. Mol. Med. Rep. 2015;12:3681–3687. doi: 10.3892/mmr.2015.3860. [DOI] [PubMed] [Google Scholar]
- 99.Chittaranjan S., Bortnik S., Dragowska W.H., Xu J., Abeysundara N., Leung A., Go N.E., DeVorkin L., Weppler S.A., Gelmon K., et al. Autophagy inhibition augments the anticancer effects of epirubicin treatment in anthracycline-sensitive and -resistant triple-negative breast cancer. Clin. Cancer Res. 2014;20:3159–3173. doi: 10.1158/1078-0432.CCR-13-2060. [DOI] [PubMed] [Google Scholar]
- 100.Das C.K., Linder B., Bonn F., Rothweiler F., Dikic I., Michaelis M., Cinatl J., Mandal M., Kögel D. BAG3 Overexpression and Cytoprotective Autophagy Mediate Apoptosis Resistance in Chemoresistant Breast Cancer Cells. Neoplasia. 2018;20:263–279. doi: 10.1016/j.neo.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lefort S., Joffre C., Kieffer Y., Givel A.-M., Bourachot B., Zago G., Bieche I., Dubois T., Meseure D., Vincent-Salomon A., et al. Inhibition of autophagy as a new means of improving chemotherapy efficiency in high-LC3B triple-negative breast cancers. Autophagy. 2014;10:2122–2142. doi: 10.4161/15548627.2014.981788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Aydinlik S., Erkisa M., Cevatemre B., Sarimahmut M., Dere E., Ari F., Ulukaya E. Enhanced cytotoxic activity of doxorubicin through the inhibition of autophagy in triple negative breast cancer cell line. Biochim. Biophys. Acta Gen. Subj. 2017;1861:49–57. doi: 10.1016/j.bbagen.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 103.Wen J., Yeo S., Wang C., Chen S., Sun S., Haas M.A., Tu W., Jin F., Guan J.-L. Autophagy inhibition re-sensitizes pulse stimulation-selected paclitaxel-resistant triple negative breast cancer cells to chemotherapy-induced apoptosis. Breast Cancer Res. Treat. 2015;149:619–629. doi: 10.1007/s10549-015-3283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang L., Yang A., Wang M., Liu W., Wang C., Xie X., Chen X., Dong J., Li M. Enhanced Autophagy reveals vulnerability of P-gp mediated Epirubicin Resistance in Triple Negative Breast Cancer Cells. Apoptosis. 2016;21:473–488. doi: 10.1007/s10495-016-1214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bousquet G., El Bouchtaoui M., Sophie T., Leboeuf C., de Bazelaire C., Ratajczak P., Giacchetti S., de Roquancourt A., Bertheau P., Verneuil L., et al. Targeting autophagic cancer stem-cells to reverse chemoresistance in human triple negative breast cancer. Oncotarget. 2017;8:35205–35221. doi: 10.18632/oncotarget.16925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sun W.L., Wang L., Luo J., Zhu H.W., Cai Z.W. Ambra1 modulates the sensitivity of breast cancer cells to epirubicin by regulating autophagy via ATG12. Cancer Sci. 2018;109:3129–3138. doi: 10.1111/cas.13743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chen M., He M., Song Y., Chen L., Xiao P., Wan X., Dai F., Shen P. The cytoprotective role of gemcitabine-induced autophagy associated with apoptosis inhibition in triple-negative MDA-MB-231 breast cancer cells. Int. J. Mol. Med. 2014;34:276–282. doi: 10.3892/ijmm.2014.1772. [DOI] [PubMed] [Google Scholar]
- 108.Peng X., Gong F., Chen Y., Jiang Y., Liu J., Yu M., Zhang S., Wang M., Xiao G., Liao H. Autophagy promotes paclitaxel resistance of cervical cancer cells: Involvement of Warburg effect activated hypoxia-induced factor 1-α-mediated signaling. Cell Death Dis. 2014;5:e1367. doi: 10.1038/cddis.2014.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu L., Liu J.H., Zhang J., Zhang N., Wang Z.H. Blockade of Autophagy Aggravates Endoplasmic Reticulum Stress and Improves Paclitaxel Cytotoxicity in Human Cervical Cancer Cells. Cancer Res. Treat. 2014;47:313–321. doi: 10.4143/crt.2013.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yang W., Han G.H., Shin H.-Y., Lee E.-J., Cho H., Chay D.B., Kim J.-H. Combined treatment with modulated electro-hyperthermia and an autophagy inhibitor effectively inhibit ovarian and cervical cancer growth. Int. J. Hyperthermia. 2019;36:9–20. doi: 10.1080/02656736.2018.1528390. [DOI] [PubMed] [Google Scholar]
- 111.Leisching G., Loos B., Botha M., Engelbrecht A.M. A Nontoxic Concentration of Cisplatin Induces Autophagy in Cervical Cancer: Selective Cancer Cell Death with Autophagy Inhibition as an Adjuvant Treatment. Int. J. Gynecol. Cancer. 2015;25:380–388. doi: 10.1097/IGC.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 112.Lin W.M., Li Z.G. Blockage of cisplatin-induced autophagy sensitizes cervical cancer cells to cisplatin. Genet. Mol. Res. 2015;14:16905–16912. doi: 10.4238/2015.December.14.18. [DOI] [PubMed] [Google Scholar]
- 113.Selvakumaran M., Amaravadi R.K., Vasilevskaya I.A., O’Dwyer P.J. Autophagy Inhibition Sensitizes Colon Cancer Cells to Antiangiogenic and Cytotoxic Therapy. Clin. Cancer Res. 2013;19:2995–3007. doi: 10.1158/1078-0432.CCR-12-1542. [DOI] [PubMed] [Google Scholar]
- 114.Sasaki K., Tsuno N.H., Sunami E., Tsurita G., Kawai K., Okaji Y., Nishikawa T., Shuno Y., Hongo K., Hiyoshi M., et al. Chloroquine potentiates the anti-cancer effect of 5-fluorouracil on colon cancer cells. BMC Cancer. 2010;10:370. doi: 10.1186/1471-2407-10-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Li J., Hou N., Faried A., Tsutsumi S., Kuwano H. Inhibition of autophagy augments 5-fluorouracil chemotherapy in human colon cancer in vitro and in vivo model. Eur. J. Cancer. 2010;46:1900–1909. doi: 10.1016/j.ejca.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 116.Chen J., Fan G., Xiao C., Wang X., Wang Y., Song G., Liu X., Chen J., Lu H., Guo W., et al. Loss of SHMT2 mediates 5-FU chemoresistance by inducing autophagy in colorectal cancer. bioRxiv. 2019:680892. [Google Scholar]
- 117.Liu S., Li X. Autophagy inhibition enhances sensitivity of endometrial carcinoma cells to paclitaxel. Int. J. Oncol. 2015;46:2399–2408. doi: 10.3892/ijo.2015.2937. [DOI] [PubMed] [Google Scholar]
- 118.Fukuda T., Oda K., Wada-Hiraike O., Sone K., Inaba K., Ikeda Y., Miyasaka A., Kashiyama T., Tanikawa M., Arimoto T., et al. The anti-malarial chloroquine suppresses proliferation and overcomes cisplatin resistance of endometrial cancer cells via autophagy inhibition. Gynecol. Oncol. 2015;137:538–545. doi: 10.1016/j.ygyno.2015.03.053. [DOI] [PubMed] [Google Scholar]
- 119.Fukuda T., Oda K., Wada-Hiraike O., Sone K., Inaba K., Ikeda Y., Makii C., Miyasaka A., Kashiyama T., Tanikawa M., et al. Autophagy inhibition augments resveratrol-induced apoptosis in Ishikawa endometrial cancer cells. Oncol. Lett. 2016;12:2560–2566. doi: 10.3892/ol.2016.4978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Xi G., Hu X., Wu B., Jiang H., Young C.Y.F., Pang Y., Yuan H. Autophagy inhibition promotes paclitaxel-induced apoptosis in cancer cells. Cancer Lett. 2011;307:141–148. doi: 10.1016/j.canlet.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 121.Yang S., Wang H., Li D., Li M. Role of Endometrial Autophagy in Physiological and Pathophysiological Processes. J. Cancer. 2019;10:3459–3471. doi: 10.7150/jca.31742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhao H., Li Q., Pang J., Jin H., Li H., Yang X. Blocking autophagy enhances the pro-apoptotic effect of bufalin on human gastric cancer cells through endoplasmic reticulum stress. Biol. Open. 2017;6:1416–1422. doi: 10.1242/bio.026344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.An Y., Zhang Z., Shang Y., Jiang X., Dong J., Yu P., Nie Y., Zhao Q. miR-23b-3p regulates the chemoresistance of gastric cancer cells by targeting ATG12 and HMGB2. Cell Death Dis. 2015;6:e1766. doi: 10.1038/cddis.2015.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang H.Q., Fang N., Liu X.M., Xiong S.P., Liao Y.Q., Jin W.J., Song R.F., Wan Y.Y. Antitumor activity of chloroquine in combination with Cisplatin in human gastric cancer xenografts. Asian Pac. J. Cancer Prev. 2015;16:3907–3912. doi: 10.7314/APJCP.2015.16.9.3907. [DOI] [PubMed] [Google Scholar]
- 125.Zhang H.Q., He B., Fang N., Lu S., Liao Y.Q., Wan Y.-Y. Autophagy inhibition sensitizes cisplatin cytotoxicity in human gastric cancer cell line SGC7901. Asian Pac. J. Cancer Prev. 2013;14:4685–4688. doi: 10.7314/APJCP.2013.14.8.4685. [DOI] [PubMed] [Google Scholar]
- 126.Li Y., Zhang J., Ma H., Chen X., Liu T., Jiao Z., He W., Wang F., Liu X., Zeng X. Protective role of autophagy in matrine-induced gastric cancer cell death. Int. J. Oncol. 2013;42:1417–1426. doi: 10.3892/ijo.2013.1817. [DOI] [PubMed] [Google Scholar]
- 127.Li L.Q., Pan D., Zhang S.W., Xie D.Y., Zheng X.L., Chen H. Autophagy regulates chemoresistance of gastric cancer stem cells via the Notch signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 2018;22:3402–3407. doi: 10.26355/eurrev_201806_15162. [DOI] [PubMed] [Google Scholar]
- 128.Dong X., Wang Y., Zhou Y., Wen J., Wang S., Shen L. Aquaporin 3 facilitates chemoresistance in gastric cancer cells to cisplatin via autophagy. Cell Death Discov. 2016;2:1–6. doi: 10.1038/cddiscovery.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Xu L., Qu X.J., Liu Y.P., Xu Y.Y., Liu J., Hou K.Z., Zhang Y. Protective autophagy antagonizes oxaliplatin-induced apoptosis in gastric cancer cells. Chin. J. Cancer. 2011;30:490–496. doi: 10.5732/cjc.010.10518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Li L.Q., Xie W.J., Pan D., Chen H., Zhang L. Inhibition of autophagy by bafilomycin A1 promotes chemosensitivity of gastric cancer cells. Tumor Biol. 2015;37:653–659. doi: 10.1007/s13277-015-3842-z. [DOI] [PubMed] [Google Scholar]
- 131.Pei G., Luo M., Ni X., Wu J., Wang S., Ma Y., Yu J. Autophagy Facilitates Metadherin-Induced Chemotherapy Resistance Through the AMPK/ATG5 Pathway in Gastric Cancer. Cell. Physiol. Biochem. 2018;46:847–859. doi: 10.1159/000488742. [DOI] [PubMed] [Google Scholar]
- 132.Xiong X., Lu B., Tian Q., Zhang H., Wu M., Guo H., Zhang Q., Li X., Zhou T., Wang Y. Inhibition of autophagy enhances cinobufagin-induced apoptosis in gastric cancer. Oncol. Rep. 2019;41:492–500. doi: 10.3892/or.2018.6837. [DOI] [PubMed] [Google Scholar]
- 133.Buccarelli M., Marconi M., Pacioni S., Pascalis I.D., D’Alessandris Q.G., Martini M., Ascione B., Malorni W., Larocca L.M., Pallini R., et al. Inhibition of autophagy increases susceptibility of glioblastoma stem cells to temozolomide by igniting ferroptosis. Cell Death Dis. 2018;9:1–17. doi: 10.1038/s41419-018-0864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lohitesh K., Saini H., Srivastava A., Mukherjee S., Roy A., Chowdhury R. Autophagy inhibition potentiates SAHA-mediated apoptosis in glioblastoma cells by accumulation of damaged mitochondria. Oncol. Rep. 2018;39:2787–2796. doi: 10.3892/or.2018.6373. [DOI] [PubMed] [Google Scholar]
- 135.Golden E.B., Cho H.-Y., Jahanian A., Hofman F.M., Louie S.G., Schönthal A.H., Chen T.C. Chloroquine enhances temozolomide cytotoxicity in malignant gliomas by blocking autophagy. Neurosurg Focus. 2014;37:E12. doi: 10.3171/2014.9.FOCUS14504. [DOI] [PubMed] [Google Scholar]
- 136.Hori Y.S., Hosoda R., Akiyama Y., Sebori R., Wanibuchi M., Mikami T., Sugino T., Suzuki K., Maruyama M., Tsukamoto M., et al. Chloroquine potentiates temozolomide cytotoxicity by inhibiting mitochondrial autophagy in glioma cells. J. Neurooncol. 2015;122:11–20. doi: 10.1007/s11060-014-1686-9. [DOI] [PubMed] [Google Scholar]
- 137.Lee S.W., Kim H.K., Lee N.H., Yi H.Y., Kim H.S., Hong S.H., Hong Y.K., Joe Y.A. The synergistic effect of combination temozolomide and chloroquine treatment is dependent on autophagy formation and p53 status in glioma cells. Cancer Lett. 2015;360:195–204. doi: 10.1016/j.canlet.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 138.Kanzawa T., Germano I.M., Komata T., Ito H., Kondo Y., Kondo S. Role of autophagy in temozolomide-induced cytotoxicity for malignant glioma cells. Cell Death Differ. 2004;11:448–457. doi: 10.1038/sj.cdd.4401359. [DOI] [PubMed] [Google Scholar]
- 139.Huang T., Kim C.K., Alvarez A.A., Pangeni R.P., Wan X., Song X., Shi T., Yang Y., Sastry N., Horbinski C.M., et al. MST4 Phosphorylation of ATG4B Regulates Autophagic Activity, Tumorigenicity, and Radioresistance in Glioblastoma. Cancer Cell. 2017;32:840–855.e8. doi: 10.1016/j.ccell.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wen Z., Zeng W., Chen Y., Li H., Wang J., Cheng Q., Yu J., Zhou H., Liu Z., Xiao J., et al. Knockdown ATG4C inhibits gliomas progression and promotes temozolomide chemosensitivity by suppressing autophagic flux. J. Exp. Clin. Cancer Res. 2019;38:298. doi: 10.1186/s13046-019-1287-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hsieh M.J., Lin C.W., Yang S.F., Sheu G.T., Yu Y.Y., Chen M.K., Chiou H.L. A combination of pterostilbene with autophagy inhibitors exerts efficient apoptotic characteristics in both chemosensitive and chemoresistant lung cancer cells. Toxicol. Sci. 2014;137:65–75. doi: 10.1093/toxsci/kft238. [DOI] [PubMed] [Google Scholar]
- 142.Song Y., Li W., Peng X., Xie J., Li H., Tan G. Inhibition of autophagy results in a reversal of taxol resistance in nasopharyngeal carcinoma by enhancing taxol-induced caspase-dependent apoptosis. Am. J. Transl. Res. 2017;9:1934–1942. [PMC free article] [PubMed] [Google Scholar]
- 143.Aga T., Endo K., Tsuji A., Aga M., Moriyama-Kita M., Ueno T., Nakanishi Y., Hatano M., Kondo S., Sugimoto H., et al. Inhibition of autophagy by chloroquine makes chemotherapy in nasopharyngeal carcinoma more efficient. Auris Nasus Larynx. 2019;46:443–450. doi: 10.1016/j.anl.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 144.Su Z., Li G., Liu C., Ren S., Deng T., Zhang S., Tian Y., Liu Y., Qiu Y. Autophagy inhibition impairs the epithelial-mesenchymal transition and enhances cisplatin sensitivity in nasopharyngeal carcinoma. Oncol. Lett. 2017;13:4147–4154. doi: 10.3892/ol.2017.5963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Liu Z., Liu J., Li L., Nie D., Tao Q., Wu J., Fan J., Lin C., Zhao S., Ju D. Inhibition of Autophagy Potentiated the Antitumor Effect of Nedaplatin in Cisplatin-Resistant Nasopharyngeal Carcinoma Cells. PLoS ONE. 2015;10:e0135236. doi: 10.1371/journal.pone.0135236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhang X., Zhao W. Effect of autophagy inhibitor 3-methyladenine combined with TP chemotherapy on nasopharyngeal carcinoma and EGFR and VEGF levels in tissues. Int. J. Clin. Exp. Med. 2019;12:6403–6410. [Google Scholar]
- 147.Zhang N., Wu Y., Lyu X., Li B., Yan X., Xiong H., Li X., Huang G., Zeng Y., Zhang Y., et al. HSF1 upregulates ATG4B expression and enhances epirubicin-induced protective autophagy in hepatocellular carcinoma cells. Cancer Lett. 2017;409:81–90. doi: 10.1016/j.canlet.2017.08.039. [DOI] [PubMed] [Google Scholar]
- 148.Ding Z.B., Hui B., Shi Y.H., Zhou J., Peng Y.F., Gu C.-Y., Yang H., Shi G.-M., Ke A.-W., Wang X.-Y., et al. Autophagy activation in hepatocellular carcinoma contributes to the tolerance of oxaliplatin via reactive oxygen species modulation. Clin. Cancer Res. 2011;17:6229–6238. doi: 10.1158/1078-0432.CCR-11-0816. [DOI] [PubMed] [Google Scholar]
- 149.Zhou Y., Sun K., Ma Y., Yang H., Zhang Y., Kong X., Wei L. Autophagy inhibits chemotherapy-induced apoptosis through downregulating Bad and Bim in hepatocellular carcinoma cells. Sci. Rep. 2014:4. doi: 10.1038/srep05382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Li L., Liu X., Zhou L., Wang W., Liu Z., Cheng Y., Li J., Wei H. Autophagy Plays a Critical Role in Insulin Resistance- Mediated Chemoresistance in Hepatocellular Carcinoma Cells by Regulating the ER Stress. J. Cancer. 2018;9:4314–4324. doi: 10.7150/jca.27943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Peng W.X., Xiong E.M., Ge L., Wan Y.Y., Zhang C.L., Du F.Y., Xu M., Bhat R.A., Jin J., Gong A.H. Egr-1 promotes hypoxia-induced autophagy to enhance chemo-resistance of hepatocellular carcinoma cells. Exp. Cell Res. 2016;340:62–70. doi: 10.1016/j.yexcr.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 152.Liu G., Fan X., Tang M., Chen R., Wang H., Jia R., Zhou X., Jing W., Wang H., Yang Y., et al. Osteopontin induces autophagy to promote chemo-resistance in human hepatocellular carcinoma cells. Cancer Lett. 2016;383:171–182. doi: 10.1016/j.canlet.2016.09.033. [DOI] [PubMed] [Google Scholar]
- 153.Fu X.T., Song K., Zhou J., Shi Y.H., Liu W.R., Shi G.M., Gao Q., Wang X.Y., Ding Z.B., Fan J. Tumor-associated macrophages modulate resistance to oxaliplatin via inducing autophagy in hepatocellular carcinoma. Cancer Cell Int. 2019;19:71. doi: 10.1186/s12935-019-0771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Xu Y., An Y., Wang Y., Zhang C., Zhang H., Huang C., Jiang H., Wang X., Li X. miR-101 inhibits autophagy and enhances cisplatin-induced apoptosis in hepatocellular carcinoma cells. Oncol. Rep. 2013;29:2019–2024. doi: 10.3892/or.2013.2338. [DOI] [PubMed] [Google Scholar]
- 155.Peng W., Du T., Zhang Z., Du F., Jin J., Gong A. Knockdown of autophagy-related gene LC3 enhances the sensitivity of HepG2 cells to epirubicin. Exp. Ther. Med. 2015;9:1271–1276. doi: 10.3892/etm.2015.2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Datta S., Choudhury D., Das A., Mukherjee D.D., Dasgupta M., Bandopadhyay S., Chakrabarti G. Autophagy inhibition with chloroquine reverts paclitaxel resistance and attenuates metastatic potential in human nonsmall lung adenocarcinoma A549 cells via ROS mediated modulation of β-catenin pathway. Apoptosis. 2019;24:414–433. doi: 10.1007/s10495-019-01526-y. [DOI] [PubMed] [Google Scholar]
- 157.Endo S., Uchibori M., Suyama M., Fujita M., Arai Y., Hu D., Xia S., Ma B., Kabir A., Kamatari Y.O., et al. Novel Atg4B inhibitors potentiate cisplatin therapy in lung cancer cells through blockade of autophagy. Computational Toxicology. 2019;12:100095. doi: 10.1016/j.comtox.2019.100095. [DOI] [Google Scholar]
- 158.Chen K., Shi W. Autophagy regulates resistance of non-small cell lung cancer cells to paclitaxel. Tumour Biol. 2016;37:10539–10544. doi: 10.1007/s13277-016-4929-x. [DOI] [PubMed] [Google Scholar]
- 159.Chiu Y.H., Hsu S.H., Hsu H.W., Huang K.C., Liu W., Wu C.Y., Huang W.P., Chen J.Y.F., Chen B.H., Chiu C.C. Human non-small cell lung cancer cells can be sensitized to camptothecin by modulating autophagy. Int. J. Oncol. 2018;53:1967–1979. doi: 10.3892/ijo.2018.4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hao C., Liu G., Tian G. Autophagy inhibition of cancer stem cells promotes the efficacy of cisplatin against non-small cell lung carcinoma. Ther. Adv. Respir. Dis. 2019;13:1753466619866097. doi: 10.1177/1753466619866097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Pan X., Zhang X., Sun H., Zhang J., Yan M., Zhang H. Autophagy inhibition promotes 5-fluorouraci-induced apoptosis by stimulating ROS formation in human non-small cell lung cancer A549 cells. PLoS ONE. 2013;8:e56679. doi: 10.1371/journal.pone.0056679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Liu W., Lo Y.L., Hsu C., Wu Y.T., Liao Z.X., Wu W.J., Chen Y.J., Kao C., Chiu C.C., Wang L.F. CS-PEI/Beclin-siRNA Downregulate Multidrug Resistance Proteins and Increase Paclitaxel Therapeutic Efficacy against NSCLC. Mol. Ther. Nucleic Acids. 2019;17:477–490. doi: 10.1016/j.omtn.2019.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chen J., Zhang L., Zhou H., Wang W., Luo Y., Yang H., Yi H. Inhibition of autophagy promotes cisplatin-induced apoptotic cell death through Atg5 and Beclin 1 in A549 human lung cancer cells. Mol. Med. Rep. 2018;17:6859–6865. doi: 10.3892/mmr.2018.8686. [DOI] [PubMed] [Google Scholar]
- 164.Belounis A., Nyalendo C., Le Gall R., Imbriglio T.V., Mahma M., Teira P., Beaunoyer M., Cournoyer S., Haddad E., Vassal G., et al. Autophagy is associated with chemoresistance in neuroblastoma. BMC Cancer. 2016;16:891. doi: 10.1186/s12885-016-2906-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang L., Zhang H., Sun M., Yin Z., Qian J. High mobility group box 1-mediated autophagy promotes neuroblastoma cell chemoresistance. Oncol. Rep. 2015;34:2969–2976. doi: 10.3892/or.2015.4278. [DOI] [PubMed] [Google Scholar]
- 166.Zhen Z., Yang K., Ye L., You Z., Chen R., Liu Y., He Y. Suberoylanilide hydroxamic acid sensitizes neuroblastoma to paclitaxel by inhibiting thioredoxin-related protein 14-mediated autophagy. Cancer Sci. 2017;108:1485–1492. doi: 10.1111/cas.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang J., Wu G.S. Role of autophagy in cisplatin resistance in ovarian cancer cells. J. Biol. Chem. 2014;289:17163–17173. doi: 10.1074/jbc.M114.558288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bao L., Jaramillo M.C., Zhang Z., Zheng Y., Yao M., Zhang D.D., Yi X. Induction of autophagy contributes to cisplatin resistance in human ovarian cancer cells. Mol. Med. Rep. 2015;11:91–98. doi: 10.3892/mmr.2014.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Li X., Zhang L., Yu L., Wei W., Lin X., Hou X., Tian Y. shRNA-mediated AMBRA1 knockdown reduces the cisplatin-induced autophagy and sensitizes ovarian cancer cells to cisplatin. J. Toxicol. Sci. 2016;41:45–53. doi: 10.2131/jts.41.45. [DOI] [PubMed] [Google Scholar]
- 170.Pagotto A., Pilotto G., Mazzoldi E.L., Nicoletto M.O., Frezzini S., Pastò A., Amadori A. Autophagy inhibition reduces chemoresistance and tumorigenic potential of human ovarian cancer stem cells. Cell Death Dis. 2017;8:e2943. doi: 10.1038/cddis.2017.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liang B., Liu X., Liu Y., Kong D., Liu X., Zhong R., Ma S. Inhibition of autophagy sensitizes MDR-phenotype ovarian cancer SKVCR cells to chemotherapy. Biomed. Pharmacother. 2016;82:98–105. doi: 10.1016/j.biopha.2016.04.054. [DOI] [PubMed] [Google Scholar]
- 172.Khurana A., Roy D., Kalogera E., Mondal S., Wen X., He X., Dowdy S., Shridhar V. Quinacrine promotes autophagic cell death and chemosensitivity in ovarian cancer and attenuates tumor growth. Oncotarget. 2015;6:36354–36369. doi: 10.18632/oncotarget.5632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bao L.J., Jaramillo M.C., Zhang Z.B., Zheng Y.X., Yao M., Zhang D.D., Yi X.F. Nrf2 induces cisplatin resistance through activation of autophagy in ovarian carcinoma. Int. J. Clin. Exp. Pathol. 2014;7:1502–1513. [PMC free article] [PubMed] [Google Scholar]
- 174.Tang J., Zhu J., Ye Y., Liu Y., He Y., Zhang L., Tang D., Qiao C., Feng X., Li J., et al. Inhibition LC3B can increase chemosensitivity of ovarian cancer cells. Cancer Cell Int. 2019;19:199. doi: 10.1186/s12935-019-0921-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Sun Y., Liu J.H., Jin L., Sui Y.X., Han L.L., Huang Y. Effect of autophagy-related beclin1 on sensitivity of cisplatin-resistant ovarian cancer cells to chemotherapeutic agents. Asian Pac. J. Cancer Prev. 2015;16:2785–2791. doi: 10.7314/APJCP.2015.16.7.2785. [DOI] [PubMed] [Google Scholar]
- 176.Zhang S.-F., Wang X.-Y., Fu Z.-Q., Peng Q.-H., Zhang J.-Y., Ye F., Fu Y.-F., Zhou C.-Y., Lu W.-G., Cheng X.-D., et al. TXNDC17 promotes paclitaxel resistance via inducing autophagy in ovarian cancer. Autophagy. 2015;11:225–238. doi: 10.1080/15548627.2014.998931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chen H., Zhao C., He R., Zhou M., Liu Y., Guo X., Wang M., Zhu F., Qin R., Li X. Danthron suppresses autophagy and sensitizes pancreatic cancer cells to doxorubicin. Toxicol In Vitro. 2019;54:345–353. doi: 10.1016/j.tiv.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 178.Xu X.D., Zhao Y., Zhang M., He R.Z., Shi X.H., Guo X.J., Shi C.J., Peng F., Wang M., Shen M., et al. Inhibition of Autophagy by Deguelin Sensitizes Pancreatic Cancer Cells to Doxorubicin. Int. J. Mol. Sci. 2017;18:370. doi: 10.3390/ijms18020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Fu Z., Cheng X., Kuang J., Feng H., Chen L., Liang J., Shen X., Yuen S., Peng C., Shen B., et al. CQ sensitizes human pancreatic cancer cells to gemcitabine through the lysosomal apoptotic pathway via reactive oxygen species. Mol. Oncol. 2018;12:529–544. doi: 10.1002/1878-0261.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Huang L., Hu C., Cao H., Wu X., Wang R., Lu H., Li H., Chen H. MicroRNA-29c Increases the Chemosensitivity of Pancreatic Cancer Cells by Inhibiting USP22 Mediated Autophagy. Cell. Physiol. Biochem. 2018;47:747–758. doi: 10.1159/000490027. [DOI] [PubMed] [Google Scholar]
- 181.Wang Z.C., Huang F.Z., Xu H.B., Sun J.C., Wang C.F. MicroRNA-137 inhibits autophagy and chemosensitizes pancreatic cancer cells by targeting ATG5. Int. J. Biochem. Cell Biol. 2019;111:63–71. doi: 10.1016/j.biocel.2019.01.020. [DOI] [PubMed] [Google Scholar]
- 182.Ma T., Chen W., Zhi X., Liu H., Zhou Y., Chen B.W., Hu L., Shen J., Zheng X., Zhang S., et al. USP9X inhibition improves gemcitabine sensitivity in pancreatic cancer by inhibiting autophagy. Cancer Lett. 2018;436:129–138. doi: 10.1016/j.canlet.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 183.Zhang M., Zhang W., Tang G., Wang H., Wu M., Yu W., Zhou Z., Mou Y., Liu X. Targeted Codelivery of Docetaxel and Atg7 siRNA for Autophagy Inhibition and Pancreatic Cancer Treatment. ACS Appl. Bio Mater. 2019;2:1168–1176. doi: 10.1021/acsabm.8b00764. [DOI] [PubMed] [Google Scholar]
- 184.Donohue E., Thomas A., Maurer N., Manisali I., Zeisser-Labouebe M., Zisman N., Anderson H.J., Ng S.S.W., Webb M., Bally M., et al. The autophagy inhibitor verteporfin moderately enhances the antitumor activity of gemcitabine in a pancreatic ductal adenocarcinoma model. J. Cancer. 2013;4:585–596. doi: 10.7150/jca.7030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kwon J.J., Willy J.A., Quirin K.A., Wek R.C., Korc M., Yin X.-M., Kota J. Novel role of miR-29a in pancreatic cancer autophagy and its therapeutic potential. Oncotarget. 2016;7:71635–71650. doi: 10.18632/oncotarget.11928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ryabaya O.O., Inshakov A.N., Egorova A.V., Emelyanova M.A., Nasedkina T.V., Zasedatelev A.S., Khochenkov D.A., Stepanova E.V. Autophagy inhibitors chloroquine and LY294002 enhance temozolomide cytotoxicity on cutaneous melanoma cell lines in vitro. Anticancer Drugs. 2017;28:307–315. doi: 10.1097/CAD.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 187.Ma X.-H., Piao S., Wang D., McAfee Q.W., Nathanson K.L., Lum J.J., Li L.Z., Amaravadi R.K. Measurements of tumor cell autophagy predict invasiveness, resistance to chemotherapy, and survival in melanoma. Clin. Cancer Res. 2011;17:3478–3489. doi: 10.1158/1078-0432.CCR-10-2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Cervia D., Assi E., De Palma C., Giovarelli M., Bizzozero L., Pambianco S., Di Renzo I., Zecchini S., Moscheni C., Vantaggiato C., et al. Essential role for acid sphingomyelinase-inhibited autophagy in melanoma response to cisplatin. Oncotarget. 2016;7:24995–25009. doi: 10.18632/oncotarget.8735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Fitzwalter B.E., Towers C.G., Sullivan K.D., Andrysik Z., Hoh M., Ludwig M., O’Prey J., Ryan K.M., Espinosa J.M., Morgan M.J., et al. Autophagy Inhibition Mediates Apoptosis Sensitization in Cancer Therapy by Relieving FOXO3a Turnover. Dev. Cell. 2018;44:555–565.e3. doi: 10.1016/j.devcel.2018.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Joo W.D., Visintin I., Mor G. Targeted cancer therapy - Are the days of systemic chemotherapy numbered? Maturitas. 2013;76:308–314. doi: 10.1016/j.maturitas.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ke X., Shen L. Molecular targeted therapy of cancer: The progress and future prospect. Front. Lab. Med. 2017;1:69–75. doi: 10.1016/j.flm.2017.06.001. [DOI] [Google Scholar]
- 192.Zhao Z., Xia G., Li N., Su R., Chen X., Zhong L. Autophagy Inhibition Promotes Bevacizumab-induced Apoptosis and Proliferation Inhibition in Colorectal Cancer Cells. J. Cancer. 2018;9:3407–3416. doi: 10.7150/jca.24201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Huang H., Song J., Liu Z., Pan L., Xu G. Autophagy activation promotes bevacizumab resistance in glioblastoma by suppressing AKT/mTOR signaling pathway. Oncol. Lett. 2018;15:1487–1494. doi: 10.3892/ol.2017.7446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Liu L., Wang S., Shao Y., Shi J., Wang W., Chen W., Ye Z., Jiang J., Fang Q., Zhang G., et al. Hydroxychloroquine potentiates the anti-cancer effect of bevacizumab on glioblastoma via the inhibition of autophagy. Biomed. Pharmacother. 2019;118:109339. doi: 10.1016/j.biopha.2019.109339. [DOI] [PubMed] [Google Scholar]
- 195.Guo X., Li D., Sun K., Wang J., Liu Y., Song J., Zhao Q., Zhang S., Deng W., Zhao X., et al. Inhibition of autophagy enhances anticancer effects of bevacizumab in hepatocarcinoma. J. Mol. Med. (Berl) 2013;91:473–483. doi: 10.1007/s00109-012-0966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Hu Y.L., DeLay M., Jahangiri A., Molinaro A.M., Rose S.D., Carbonell W.S., Aghi M.K. Hypoxia-induced autophagy promotes tumor cell survival and adaptation to antiangiogenic treatment in glioblastoma. Cancer Res. 2012;72:1773–1783. doi: 10.1158/0008-5472.CAN-11-3831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Vazquez-Martin A., Oliveras-Ferraros C., Menendez J.A. Autophagy Facilitates the Development of Breast Cancer Resistance to the Anti-HER2 Monoclonal Antibody Trastuzumab. PLoS ONE. 2009;4:e6251. doi: 10.1371/journal.pone.0006251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Rodríguez C.E., Reidel S.I., Bal de Kier J.E.D., Jasnis M.A., Fiszman G.L. Autophagy Protects from Trastuzumab-Induced Cytotoxicity in HER2 Overexpressing Breast Tumor Spheroids. PLoS ONE. 2015;10:e0137920. doi: 10.1371/journal.pone.0137920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Bortnik S., Choutka C., Horlings H.M., Leung S., Baker J.H., Lebovitz C., Dragowska W.H., Go N.E., Bally M.B., Minchinton A.I., et al. Identification of breast cancer cell subtypes sensitive to ATG4B inhibition. Oncotarget. 2016;7:66970–66988. doi: 10.18632/oncotarget.11408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Cufí S., Vazquez-Martin A., Oliveras-Ferraros C., Corominas-Faja B., Urruticoechea A., Martin-Castillo B., Menendez J.A. Autophagy-related gene 12 (ATG12) is a novel determinant of primary resistance to HER2-targeted therapies: Utility of transcriptome analysis of the autophagy interactome to guide breast cancer treatment. Oncotarget. 2012;3:1600–1614. doi: 10.18632/oncotarget.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Eckers J., Skiba J., Senthilkumar G., Nickel K.P., Swick A.D., Kimple R.J. Abstract 1344: Autophagy contributes to therapeutic resistance in head and neck cancer. Cancer Res. 2018;78:1344. [Google Scholar]
- 202.Li X., Fan Z. The EGFR antibody cetuximab induces autophagy in cancer cells by downregulating HIF-1α and Bcl-2 and activating the beclin-1/hVps34 complex. Cancer Res. 2010;70:5942–5952. doi: 10.1158/0008-5472.CAN-10-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Li X., Lu Y., Pan T., Fan Z. Roles of autophagy in cetuximab-mediated cancer therapy against EGFR. Autophagy. 2010;6:1066–1077. doi: 10.4161/auto.6.8.13366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Lu S., Yao Y., Xu G., Zhou C., Zhang Y., Sun J., Jiang R., Shao Q., Chen Y. CD24 regulates sorafenib resistance via activating autophagy in hepatocellular carcinoma. Cell Death Dis. 2018;9:1–13. doi: 10.1038/s41419-018-0681-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Braggio D., Koller D., Jin F., Siva N., Zewdu A., Lopez G., Batte K., Casadei L., Welliver M., Strohecker A., et al. Autophagy inhibition overcomes sorafenib resistance in S45F-mutated desmoid tumors. Cancer. 2019:125. doi: 10.1002/cncr.32120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Eritja N., Chen B.-J., Rodríguez-Barrueco R., Santacana M., Gatius S., Vidal A., Martí M.D., Ponce J., Bergadà L., Yeramian A., et al. Autophagy orchestrates adaptive responses to targeted therapy in endometrial cancer. Autophagy. 2017;13:608–624. doi: 10.1080/15548627.2016.1271512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Shi Y.-H., Ding Z.-B., Zhou J., Hui B., Shi G.-M., Ke A.-W., Wang X.-Y., Dai Z., Peng Y.-F., Gu C.-Y., et al. Targeting autophagy enhances sorafenib lethality for hepatocellular carcinoma via ER stress-related apoptosis. Autophagy. 2011;7:1159–1172. doi: 10.4161/auto.7.10.16818. [DOI] [PubMed] [Google Scholar]
- 208.Zhao P., Li M., Wang Y., Chen Y., He C., Zhang X., Yang T., Lu Y., You J., Lee R.J., et al. Enhancing anti-tumor efficiency in hepatocellular carcinoma through the autophagy inhibition by miR-375/sorafenib in lipid-coated calcium carbonate nanoparticles. Acta Biomater. 2018;72:248–255. doi: 10.1016/j.actbio.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 209.Zheng B., Zhu H., Gu D., Pan X., Qian L., Xue B., Yang D., Zhou J., Shan Y. MiRNA-30a-mediated autophagy inhibition sensitizes renal cell carcinoma cells to sorafenib. Biochem. Biophys. Res. Commun. 2015;459:234–239. doi: 10.1016/j.bbrc.2015.02.084. [DOI] [PubMed] [Google Scholar]
- 210.Liu X., Sun K., Wang H., Dai Y. Inhibition of Autophagy by Chloroquine Enhances the Antitumor Efficacy of Sorafenib in Glioblastoma. Cell Mol. Neurobiol. 2016;36:1197–1208. doi: 10.1007/s10571-015-0318-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Pan H., Wang Z., Jiang L., Sui X., You L., Shou J., Jing Z., Xie J., Ge W., Cai X., et al. Autophagy inhibition sensitizes hepatocellular carcinoma to the multikinase inhibitor linifanib. Sci. Rep. 2014;4:6683. doi: 10.1038/srep06683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.DeVorkin L., Hattersley M., Kim P., Ries J., Spowart J., Anglesio M.S., Levi S.M., Huntsman D.G., Amaravadi R.K., Winkler J.D., et al. Autophagy Inhibition Enhances Sunitinib Efficacy in Clear Cell Ovarian Carcinoma. Mol. Cancer Res. 2017;15:250–258. doi: 10.1158/1541-7786.MCR-16-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li M.L., Xu Y.-Z., Lu W.-J., Li Y.-H., Tan S.-S., Lin H.-J., Wu T.-M., Li Y., Wang S.-Y., Zhao Y.-L. Chloroquine potentiates the anticancer effect of sunitinib on renal cell carcinoma by inhibiting autophagy and inducing apoptosis. Oncol. Lett. 2018;15:2839–2846. doi: 10.3892/ol.2017.7635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Wang B., Lu D., Xuan M.J., Hu W. Antitumor effect of sunitinib in human prostate cancer cells functions via autophagy. Exp. Ther. Med. 2017 doi: 10.3892/etm.2017.4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Wiedmer T., Blank A., Pantasis S., Normand L., Bill R., Krebs P., Tschan M.P., Marinoni I., Perren A. Autophagy Inhibition Improves Sunitinib Efficacy in Pancreatic Neuroendocrine Tumors via a Lysosome-dependent Mechanism. Mol. Cancer Ther. 2017;16:2502–2515. doi: 10.1158/1535-7163.MCT-17-0136. [DOI] [PubMed] [Google Scholar]
- 216.Abdel-Aziz A.K., Shouman S., El-Demerdash E., Elgendy M., Abdel-Naim A.B. Chloroquine synergizes sunitinib cytotoxicity via modulating autophagic, apoptotic and angiogenic machineries. Chem. Biol. Interact. 2014;217:28–40. doi: 10.1016/j.cbi.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 217.Liu Z., He K., Ma Q., Yu Q., Liu C., Ndege I., Wang X., Yu Z. Autophagy inhibitor facilitates gefitinib sensitivity in vitro and in vivo by activating mitochondrial apoptosis in triple negative breast cancer. PLoS ONE. 2017;12:e0177694. doi: 10.1371/journal.pone.0177694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Kang M., Lee K.-H., Lee H.S., Jeong C.W., Kwak C., Kim H.H., Ku J.H. Concurrent Autophagy Inhibition Overcomes the Resistance of Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Human Bladder Cancer Cells. Int. J. Mol. Sci. 2017;18:321. doi: 10.3390/ijms18020321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wang J., Wang C., Hu X., Yu C., Zhou L., Ding Z., Zhou M. Gefitinib-mediated apoptosis is enhanced via inhibition of autophagy by chloroquine diphosphate in cutaneous squamous cell carcinoma cells. Oncol. Lett. 2019;18:368–374. doi: 10.3892/ol.2019.10308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Tang M.C., Wu M.-Y., Hwang M.-H., Chang Y.-T., Huang H.-J., Lin A.M.-Y., Yang J.C.-H. Chloroquine Enhances Gefitinib Cytotoxicity in Gefitinib-Resistant Nonsmall Cell Lung Cancer Cells. PLoS ONE. 2015;10:e0119135. doi: 10.1371/journal.pone.0119135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Liu J.-T., Li W.-C., Gao S., Wang F., Li X.-Q., Yu H.-Q., Fan L.-L., Wei W., Wang H., Sun G.-P. Autophagy Inhibition Overcomes the Antagonistic Effect Between Gefitinib and Cisplatin in Epidermal Growth Factor Receptor Mutant Non--Small-Cell Lung Cancer Cells. Clin. Lung Cancer. 2015;16:e55–e66. doi: 10.1016/j.cllc.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 222.Zhang W., Dong Y.Z., Du X., Peng X.N., Shen Q.M. MiRNA-153-3p promotes gefitinib-sensitivity in non-small cell lung cancer by inhibiting ATG5 expression and autophagy. Eur. Rev. Med. Pharmacol. Sci. 2019;23:2444–2452. doi: 10.26355/eurrev_201903_17391. [DOI] [PubMed] [Google Scholar]
- 223.Meng J., Chang C., Chen Y., Bi F., Ji C., Liu W. EGCG overcomes gefitinib resistance by inhibiting autophagy and augmenting cell death through targeting ERK phosphorylation in NSCLC. Onco Targets Ther. 2019;12:6033–6043. doi: 10.2147/OTT.S209441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Qi M., Tian Y., Li W., Li D., Zhao T., Yang Y., Li Q., Chen S., Yang Y., Zhang Z., et al. ERK inhibition represses gefitinib resistance in non-small cell lung cancer cells. Oncotarget. 2018;9:12020–12034. doi: 10.18632/oncotarget.24147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Zhao L., Yang G., Shi Y., Su C., Chang J. Co-delivery of Gefitinib and chloroquine by chitosan nanoparticles for overcoming the drug acquired resistance. J. Nanobiotechnol. 2015;13:57. doi: 10.1186/s12951-015-0121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Chen C.-H., Lin Y.C., Yen Y. Inhibition of autophagy by MPT0L145, a novel PIK3C3 inhibitor, to overcome drug resistance in cancer cells. JCO. 2018;36:e14583. doi: 10.1200/JCO.2018.36.15_suppl.e14583. [DOI] [Google Scholar]
- 227.Dragowska W.H., Weppler S.A., Wang J.C., Wong L.Y., Kapanen A.I., Rawji J.S., Warburton C., Qadir M.A., Donohue E., Roberge M., et al. Induction of autophagy is an early response to gefitinib and a potential therapeutic target in breast cancer. PLoS ONE. 2013;8:e76503. doi: 10.1371/journal.pone.0076503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Han W., Pan H., Chen Y., Sun J., Wang Y., Li J., Ge W., Feng L., Lin X., Wang X., et al. EGFR Tyrosine Kinase Inhibitors Activate Autophagy as a Cytoprotective Response in Human Lung Cancer Cells. PLoS ONE. 2011;6:e18691. doi: 10.1371/journal.pone.0018691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Li L., Wang Y., Jiao L., Lin C., Lu C., Zhang K., Hu C., Ye J., Zhang D., Wu H., et al. Protective autophagy decreases osimertinib cytotoxicity through regulation of stem cell-like properties in lung cancer. Cancer Lett. 2019;452:191–202. doi: 10.1016/j.canlet.2019.03.027. [DOI] [PubMed] [Google Scholar]
- 230.Li L., Wang Y., Jiao L., Lin C., Lu C., Zhang K., Hu C., Ye J., Zhang D., Feng M., et al. Autophagy determines osimertinib resistance through regulation of stem cell-like properties in EGFR-mutant lung cancer. bioRxiv. 2018:330092. [Google Scholar]
- 231.Fleisher B., Mody H., Werkman C., Bihorel S. Chloroquine and Osimertinib Induce Synergic Reduction in Cell Viability through Autophagy/Apoptosis Crosstalk. FASEB J. 2019;33:675. [Google Scholar]
- 232.Zhang Z., Zhang M., Liu H., Yin W. AZD9291 promotes autophagy and inhibits PI3K/AKT pathway in NSCLC cancer cells. J. Cell. Biochem. 2019;120:756–767. doi: 10.1002/jcb.27434. [DOI] [PubMed] [Google Scholar]
- 233.Jin P., Jiang J., Xie N., Zhou L., Huang Z., Zhang L., Qin S., Fu S., Peng L., Gao W., et al. MCT1 relieves osimertinib-induced CRC suppression by promoting autophagy through the LKB1/AMPK signaling. Cell Death Dis. 2019;10:1–15. doi: 10.1038/s41419-019-1844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Li Y.Y., Lam S.K., Mak J.C.W., Zheng C.Y., Ho J.C.-M. Erlotinib-induced autophagy in epidermal growth factor receptor mutated non-small cell lung cancer. Lung Cancer. 2013;81:354–361. doi: 10.1016/j.lungcan.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 235.Wang Z., Du T., Dong X., Li Z., Wu G., Zhang R. Autophagy inhibition facilitates erlotinib cytotoxicity in lung cancer cells through modulation of endoplasmic reticulum stress. Int. J. Oncol. 2016;48:2558–2566. doi: 10.3892/ijo.2016.3468. [DOI] [PubMed] [Google Scholar]
- 236.Zou Y., Ling Y.-H., Sironi J., Schwartz E.L., Perez-Soler R., Piperdi B. The autophagy inhibitor chloroquine overcomes the innate resistance of wild-type EGFR non-small-cell lung cancer cells to erlotinib. J. Thorac. Oncol. 2013;8:693–702. doi: 10.1097/JTO.0b013e31828c7210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Eimer S., Belaud-Rotureau M.-A., Airiau K., Jeanneteau M., Laharanne E., Véron N., Vital A., Loiseau H., Merlio J.-P., Belloc F. Autophagy inhibition cooperates with erlotinib to induce glioblastoma cell death. Cancer Biol. Ther. 2011;11:1017–1027. doi: 10.4161/cbt.11.12.15693. [DOI] [PubMed] [Google Scholar]
- 238.Sobhakumari A., Schickling B.M., Love-Homan L., Raeburn A., Fletcher E.V.M., Case A.J., Domann F.E., Miller F.J., Simons A.L. NOX4 mediates cytoprotective autophagy induced by the EGFR inhibitor erlotinib in head and neck cancer cells. Toxicol. Appl. Pharmacol. 2013;272:736–745. doi: 10.1016/j.taap.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Dermawan J.K.T., Gurova K., Pink J., Dowlati A., De S., Narla G., Sharma N., Stark G.R. Quinacrine overcomes resistance to erlotinib by inhibiting FACT, NF-κB, and cell-cycle progression in non-small cell lung cancer. Mol. Cancer Ther. 2014;13:2203–2214. doi: 10.1158/1535-7163.MCT-14-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Haas N.B., Appleman L.J., Stein M., Redlinger M., Wilks M., Xu X., Onorati A., Kalavacharla A., Kim T., Zhen C.J., et al. Autophagy Inhibition to Augment mTOR Inhibition: A Phase I/II Trial of Everolimus and Hydroxychloroquine in Patients with Previously Treated Renal Cell Carcinoma. Clin. Cancer Res. 2019;25:2080–2087. doi: 10.1158/1078-0432.CCR-18-2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Lui A., New J., Ogony J., Thomas S., Lewis-Wambi J. Everolimus downregulates estrogen receptor and induces autophagy in aromatase inhibitor-resistant breast cancer cells. BMC Cancer. 2016;16:487. doi: 10.1186/s12885-016-2490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Rosich L., Xargay-Torrent S., López-Guerra M., Campo E., Colomer D., Roué G. Counteracting autophagy overcomes resistance to everolimus in mantle cell lymphoma. Clin. Cancer Res. 2012;18:5278–5289. doi: 10.1158/1078-0432.CCR-12-0351. [DOI] [PubMed] [Google Scholar]
- 243.Zeng Y., Tian X., Wang Q., He W., Fan J., Gou X. Attenuation of everolimus-induced cytotoxicity by a protective autophagic pathway involving ERK activation in renal cell carcinoma cells. Drug Des. Dev. Ther. 2018;12:911–920. doi: 10.2147/DDDT.S160557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Lin J.-F., Lin Y.-C., Yang S.-C., Tsai T.-F., Chen H.-E., Chou K.-Y., Hwang T.I.-S. Autophagy inhibition enhances RAD001-induced cytotoxicity in human bladder cancer cells. Drug Des. Dev. Ther. 2016;10:1501–1513. doi: 10.2147/DDDT.S95900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Grimaldi A., Santini D., Zappavigna S., Lombardi A., Misso G., Boccellino M., Desiderio V., Vitiello P.P., Di Lorenzo G., Zoccoli A., et al. Antagonistic effects of chloroquine on autophagy occurrence potentiate the anticancer effects of everolimus on renal cancer cells. Cancer Biol. Ther. 2015;16:567–579. doi: 10.1080/15384047.2015.1018494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Rosich L., Colomer D., Roué G. Autophagy controls everolimus (RAD001) activity in mantle cell lymphoma. Autophagy. 2013;9:115–117. doi: 10.4161/auto.22483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Singla M., Bhattacharyya S. Autophagy as a potential therapeutic target during epithelial to mesenchymal transition in renal cell carcinoma: An in vitro study. Biomed. Pharmacother. 2017;94:332–340. doi: 10.1016/j.biopha.2017.07.070. [DOI] [PubMed] [Google Scholar]
- 248.Kaneko M., Nozawa H., Hiyoshi M., Tada N., Murono K., Nirei T., Emoto S., Kishikawa J., Iida Y., Sunami E., et al. Temsirolimus and chloroquine cooperatively exhibit a potent antitumor effect against colorectal cancer cells. J. Cancer Res. Clin. Oncol. 2014;140:769–781. doi: 10.1007/s00432-014-1628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Xie X., White E.P., Mehnert J.M. Coordinate Autophagy and mTOR Pathway Inhibition Enhances Cell Death in Melanoma. PLoS ONE. 2013;8:e55096. doi: 10.1371/journal.pone.0055096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Bray K., Mathew R., Lau A., Kamphorst J.J., Fan J., Chen J., Chen H.-Y., Ghavami A., Stein M., DiPaola R.S., et al. Autophagy suppresses RIP kinase-dependent necrosis enabling survival to mTOR inhibition. PLoS ONE. 2012;7:e41831. doi: 10.1371/journal.pone.0041831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Li H., Jin X., Zhang Z., Xing Y., Kong X. Inhibition of autophagy enhances apoptosis induced by the PI3K/AKT/mTor inhibitor NVP-BEZ235 in renal cell carcinoma cells. Cell Biochem. Funct. 2013;31:427–433. doi: 10.1002/cbf.2917. [DOI] [PubMed] [Google Scholar]
- 252.Chang Z., Shi G., Jin J., Guo H., Guo X., Luo F., Song Y., Jia X. Dual PI3K/mTOR inhibitor NVP-BEZ235-induced apoptosis of hepatocellular carcinoma cell lines is enhanced by inhibitors of autophagy. Int. J. Mol. Med. 2013;31:1449–1456. doi: 10.3892/ijmm.2013.1351. [DOI] [PubMed] [Google Scholar]
- 253.Ma Y., Jin Z., Yu K., Liu Q. NVP-BEZ235-induced autophagy as a potential therapeutic approach for multiple myeloma. Am. J. Transl. Res. 2019;11:87–105. [PMC free article] [PubMed] [Google Scholar]
- 254.Yang X., Niu B., Wang L., Chen M., Kang X., Wang L., Ji Y., Zhong J. Autophagy inhibition enhances colorectal cancer apoptosis induced by dual phosphatidylinositol 3-kinase/mammalian target of rapamycin inhibitor NVP-BEZ235. Oncol. Lett. 2016;12:102–106. doi: 10.3892/ol.2016.4590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Echeverry N., Ziltener G., Barbone D., Weder W., Stahel R.A., Broaddus V.C., Felley-Bosco E. Inhibition of autophagy sensitizes malignant pleural mesothelioma cells to dual PI3K/mTOR inhibitors. Cell Death Dis. 2015;6:e1757. doi: 10.1038/cddis.2015.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kim M.-Y., Kruger A.J., Jeong J.-Y., Kim J., Shin P.K., Kim S.Y., Cho J.Y., Hahm K.B., Hong S.P. Combination Therapy with a PI3K/mTOR Dual Inhibitor and Chloroquine Enhances Synergistic Apoptotic Cell Death in Epstein-Barr Virus-Infected Gastric Cancer Cells. Mol. Cells. 2019;42:448–459. doi: 10.14348/molcells.2019.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Xu C.-X., Zhao L., Yue P., Fang G., Tao H., Owonikoko T.K., Ramalingam S.S., Khuri F.R., Sun S.-Y. Augmentation of NVP-BEZ235’s anticancer activity against human lung cancer cells by blockage of autophagy. Cancer Biol. Ther. 2011;12:549–555. doi: 10.4161/cbt.12.6.16397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Hugle M., Fulda S. Dual phosphatidylinositol 3-kinase/mammalian target of rapamycin inhibitor NVP-BEZ235 synergizes with chloroquine to induce apoptosis in embryonal rhabdomyosarcoma. Cancer Lett. 2015;360:1–9. doi: 10.1016/j.canlet.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 259.Seitz C., Hugle M., Cristofanon S., Tchoghandjian A., Fulda S. The dual PI3K/mTOR inhibitor NVP-BEZ235 and chloroquine synergize to trigger apoptosis via mitochondrial-lysosomal cross-talk. Int. J. Cancer. 2013;132:2682–2693. doi: 10.1002/ijc.27935. [DOI] [PubMed] [Google Scholar]
- 260.Wu Y.-Y., Wu H.-C., Wu J.-E., Huang K.-Y., Yang S.-C., Chen S.-X., Tsao C.-J., Hsu K.-F., Chen Y.-L., Hong T.-M. The dual PI3K/mTOR inhibitor BEZ235 restricts the growth of lung cancer tumors regardless of EGFR status, as a potent accompanist in combined therapeutic regimens. J. Exp. Clin. Cancer Res. 2019;38:282. doi: 10.1186/s13046-019-1282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Ren H., Guo H., Thakur A., Zhang S., Wang T., Liang Y., Shi P., Gao L., Liu F., Feng J., et al. Blockade efficacy of MEK/ERK-dependent autophagy enhances PI3K/AKT inhibitor NVP-BKM120’s therapeutic effectiveness in lung cancer cells. Oncotarget. 2016;7:67277–67287. doi: 10.18632/oncotarget.11645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Yang W., Hosford S.R., Traphagen N.A., Shee K., Demidenko E., Liu S., Miller T.W. Autophagy promotes escape from phosphatidylinositol 3-kinase inhibition in estrogen receptor-positive breast cancer. FASEB J. 2018;32:1222–1235. doi: 10.1096/fj.201700477R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Chen S., Zhu X., Qiao H., Ye M., Lai X., Yu S., Ding L., Wen A., Zhang J. Protective autophagy promotes the resistance of HER2-positive breast cancer cells to lapatinib. Tumour Biol. 2016;37:2321–2331. doi: 10.1007/s13277-015-3800-9. [DOI] [PubMed] [Google Scholar]
- 264.Janser F.A., Adams O., Bütler V., Schläfli A.M., Dislich B., Seiler C.A., Kröll D., Langer R., Tschan M.P. Her2-Targeted Therapy Induces Autophagy in Esophageal Adenocarcinoma Cells. Int. J. Mol. Sci. 2018;19:3069. doi: 10.3390/ijms19103069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Martin A.P., Mitchell C., Rahmani M., Nephew K.P., Grant S., Dent P. Inhibition of MCL-1 enhances lapatinib toxicity and overcomes lapatinib resistance via BAK-dependent autophagy. Cancer Biol. Ther. 2009;8:2084–2096. doi: 10.4161/cbt.8.21.9895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Hu X., Shi S., Wang H., Yu X., Wang Q., Jiang S., Ju D., Ye L., Feng M. Blocking autophagy improves the anti-tumor activity of afatinib in lung adenocarcinoma with activating EGFR mutations in vitro and in vivo. Sci. Rep. 2017;7:4559. doi: 10.1038/s41598-017-04258-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Milani M., Rzymski T., Mellor H.R., Pike L., Bottini A., Generali D., Harris A.L. The role of ATF4 stabilization and autophagy in resistance of breast cancer cells treated with Bortezomib. Cancer Res. 2009;69:4415–4423. doi: 10.1158/0008-5472.CAN-08-2839. [DOI] [PubMed] [Google Scholar]
- 268.Heine S., Kleih M., Giménez N., Böpple K., Ott G., Colomer D., Aulitzky W.E., van der Kuip H., Silkenstedt E. Cyclin D1-CDK4 activity drives sensitivity to bortezomib in mantle cell lymphoma by blocking autophagy-mediated proteolysis of NOXA. J. Hematol. Oncol. 2018;11:112. doi: 10.1186/s13045-018-0657-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Jia L., Gopinathan G., Sukumar J.T., Gribben J.G. Blocking autophagy prevents bortezomib-induced NF-κB activation by reducing I-κBα degradation in lymphoma cells. PLoS ONE. 2012;7:e32584. doi: 10.1371/journal.pone.0032584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Fang J., Rhyasen G., Bolanos L., Rasch C., Varney M., Wunderlich M., Goyama S., Jansen G., Cloos J., Rigolino C., et al. Cytotoxic effects of bortezomib in myelodysplastic syndrome/acute myeloid leukemia depend on autophagy-mediated lysosomal degradation of TRAF6 and repression of PSMA1. Blood. 2012;120:858–867. doi: 10.1182/blood-2012-02-407999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Li X., Liang M., Jiang J., He R., Wang M., Guo X., Shen M., Qin R. Combined inhibition of autophagy and Nrf2 signaling augments bortezomib-induced apoptosis by increasing ROS production and ER stress in pancreatic cancer cells. Int. J. Biol. Sci. 2018;14:1291–1305. doi: 10.7150/ijbs.26776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Li X., Zhu F., Jiang J., Sun C., Zhong Q., Shen M., Wang X., Tian R., Shi C., Xu M., et al. Simultaneous inhibition of the ubiquitin-proteasome system and autophagy enhances apoptosis induced by ER stress aggravators in human pancreatic cancer cells. Autophagy. 2016;12:1521–1537. doi: 10.1080/15548627.2016.1191722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Zhang Y., Bai C., Lu D., Wu X., Gao L., Zhang W. Endoplasmic reticulum stress and autophagy participate in apoptosis induced by bortezomib in cervical cancer cells. Biotechnol. Lett. 2016;38:357–365. doi: 10.1007/s10529-015-1968-0. [DOI] [PubMed] [Google Scholar]
- 274.Modernelli A., Naponelli V., Giovanna Troglio M., Bonacini M., Ramazzina I., Bettuzzi S., Rizzi F. EGCG antagonizes Bortezomib cytotoxicity in prostate cancer cells by an autophagic mechanism. Sci. Rep. 2015;5:15270. doi: 10.1038/srep15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Sha Z., Schnell H.M., Ruoff K., Goldberg A. Rapid induction of p62 and GABARAPL1 upon proteasome inhibition promotes survival before autophagy activation. J. Cell Biol. 2018;217:1757–1776. doi: 10.1083/jcb.201708168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Lu Y., Wang Y., Xu H., Shi C., Jin F., Li W. Profilin 1 induces drug resistance through Beclin1 complex-mediated autophagy in multiple myeloma. Cancer Sci. 2018;109:2706–2716. doi: 10.1111/cas.13711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Riz I., SHawley T., GHawley R. KLF4-SQSTM1/p62-associated prosurvival autophagy contributes to carfilzomib resistance in multiple myeloma models. Oncotarget. 2015;6:14814–14831. doi: 10.18632/oncotarget.4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Jarauta V., Jaime P., Gonzalo O., de Miguel D., Ramírez-Labrada A., Martínez-Lostao L., Anel A., Pardo J., Marzo I., Naval J. Inhibition of autophagy with chloroquine potentiates carfilzomib-induced apoptosis in myeloma cells in vitro and in vivo. Cancer Lett. 2016;382:1–10. doi: 10.1016/j.canlet.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 279.Baranowska K., Misund K., Starheim K.K., Holien T., Johansson I., Darvekar S., Buene G., Waage A., Bjørkøy G., Sundan A. Hydroxychloroquine potentiates carfilzomib toxicity towards myeloma cells. Oncotarget. 2016;7:70845–70856. doi: 10.18632/oncotarget.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Mulcahy Levy J.M., Zahedi S., Griesinger A.M., Morin A., Davies K.D., Aisner D.L., Kleinschmidt-DeMasters B., Fitzwalter B.E., Goodall M.L., Thorburn J., et al. Autophagy inhibition overcomes multiple mechanisms of resistance to BRAF inhibition in brain tumors. eLife. 2017;6:e19671. doi: 10.7554/eLife.19671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Martin S., Dudek-Perić A.M., Maes H., Garg A.D., Gabrysiak M., Demirsoy S., Swinnen J.V., Agostinis P. Concurrent MEK and autophagy inhibition is required to restore cell death associated danger-signalling in Vemurafenib-resistant melanoma cells. Biochem. Pharmacol. 2015;93:290–304. doi: 10.1016/j.bcp.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 282.Levy J.M.M., Thompson J.C., Griesinger A.M., Amani V., Donson A.M., Birks D.K., Morgan M.J., Mirsky D.M., Handler M.H., Foreman N.K., et al. Autophagy inhibition improves chemosensitivity in BRAF(V600E) brain tumors. Cancer Discov. 2014;4:773–780. doi: 10.1158/2159-8290.CD-14-0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Ma X.-H., Piao S.-F., Dey S., McAfee Q., Karakousis G., Villanueva J., Hart L.S., Levi S., Hu J., Zhang G., et al. Targeting ER stress-induced autophagy overcomes BRAF inhibitor resistance in melanoma. J. Clin. Investig. 2014;124:1406–1417. doi: 10.1172/JCI70454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Wang W., Kang H., Zhao Y., Min I., Wyrwas B., Moore M., Teng L., Zarnegar R., Jiang X., Fahey T.J. Targeting Autophagy Sensitizes BRAF-Mutant Thyroid Cancer to Vemurafenib. J. Clin. Endocrinol. Metab. 2016;102:634–643. doi: 10.1210/jc.2016-1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Sueda T., Sakai D., Kawamoto K., Konno M., Nishida N., Koseki J., Colvin H., Takahashi H., Haraguchi N., Nishimura J., et al. BRAF V600E inhibition stimulates AMP-activated protein kinase-mediated autophagy in colorectal cancer cells. Sci. Rep. 2016;6:18949. doi: 10.1038/srep18949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Goulielmaki M., Koustas E., Moysidou E., Vlassi M., Sasazuki T., Shirasawa S., Zografos G., Oikonomou E., Pintzas A. BRAF associated autophagy exploitation: BRAF and autophagy inhibitors synergise to efficiently overcome resistance of BRAF mutant colorectal cancer cells. Oncotarget. 2016;7:9188–9221. doi: 10.18632/oncotarget.6942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Kinsey C.G., Camolotto S.A., Boespflug A.M., Guillen K.P., Foth M., Truong A., Schuman S.S., Shea J.E., Seipp M.T., Yap J.T., et al. Protective autophagy elicited by RAF→MEK→ERK inhibition suggests a treatment strategy for RAS-driven cancers. Nat. Med. 2019;25:620–627. doi: 10.1038/s41591-019-0367-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Verykiou S., Alexander M., Edwards N., Plummer R., Chaudhry B., Lovat P.E., Hill D.S. Harnessing autophagy to overcome mitogen-activated protein kinase kinase inhibitor-induced resistance in metastatic melanoma. Br. J. Dermatol. 2019;180:346–356. doi: 10.1111/bjd.17333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Correa R.J.M., Valdes Y.R., Peart T.M., Fazio E.N., Bertrand M., McGee J., Préfontaine M., Sugimoto A., DiMattia G.E., Shepherd T.G. Combination of AKT inhibition with autophagy blockade effectively reduces ascites-derived ovarian cancer cell viability. Carcinogenesis. 2014;35:1951–1961. doi: 10.1093/carcin/bgu049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Zhang Q., Yang M., Qu Z., Zhou J., Jiang Q. Autophagy prevention sensitizes AKTi-1/2-induced anti-hepatocellular carcinoma cell activity in vitro and in vivo. Biochem. Biophys. Res. Commun. 2016;480:334–340. doi: 10.1016/j.bbrc.2016.10.043. [DOI] [PubMed] [Google Scholar]
- 291.Degtyarev M., De Mazière A., Orr C., Lin J., Lee B.B., Tien J.Y., Prior W.W., van Dijk S., Wu H., Gray D.C., et al. AKT inhibition promotes autophagy and sensitizes PTEN-null tumors to lysosomotropic agents. J. Cell Biol. 2008;183:101–116. doi: 10.1083/jcb.200801099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Lamoureux F., Thomas C., Crafter C., Kumano M., Zhang F., Davies B.R., Gleave M.E., Zoubeidi A. Blocked autophagy using lysosomotropic agents sensitizes resistant prostate tumor cells to the novel AKT inhibitor AZD5363. Clin. Cancer Res. 2013;19:833–844. doi: 10.1158/1078-0432.CCR-12-3114. [DOI] [PubMed] [Google Scholar]
- 293.Lee M.H., Koh D., Na H., Ka N.L., Kim S., Kim H.J., Hong S., Shin Y.K., Seong J.K., Lee M.-O. MTA1 is a novel regulator of autophagy that induces tamoxifen resistance in breast cancer cells. Autophagy. 2018;14:812–824. doi: 10.1080/15548627.2017.1388476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Das C.K., Parekh A., Parida P.K., Bhutia S.K., Mandal M. Lactate dehydrogenase A regulates autophagy and tamoxifen resistance in breast cancer. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2019;1866:1004–1018. doi: 10.1016/j.bbamcr.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 295.Nagelkerke A., Sieuwerts A.M., Bussink J., Sweep F.C.G.J., Look M.P., Foekens J.A., Martens J.W.M., Span P.N. LAMP3 is involved in tamoxifen resistance in breast cancer cells through the modulation of autophagy. Endocr. Relat. Cancer. 2014;21:101–112. doi: 10.1530/ERC-13-0183. [DOI] [PubMed] [Google Scholar]
- 296.Qadir M.A., Kwok B., Dragowska W.H., To K.H., Le D., Bally M.B., Gorski S.M. Macroautophagy inhibition sensitizes tamoxifen-resistant breast cancer cells and enhances mitochondrial depolarization. Breast Cancer Res. Treat. 2008;112:389–403. doi: 10.1007/s10549-007-9873-4. [DOI] [PubMed] [Google Scholar]
- 297.Gu Y., Chen T., Li G., Xu C., Xu Z., Zhang J., He K., Zheng L., Guan Z., Su X., et al. Lower Beclin 1 downregulates HER2 expression to enhance tamoxifen sensitivity and predicts a favorable outcome for ER positive breast cancer. Oncotarget. 2017;8:52156–52177. doi: 10.18632/oncotarget.11044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Samaddar J.S., Gaddy V.T., Duplantier J., Thandavan S.P., Shah M., Smith M.J., Browning D., Rawson J., Smith S.B., Barrett J.T., et al. A role for macroautophagy in protection against 4-hydroxytamoxifen-induced cell death and the development of antiestrogen resistance. Mol. Cancer Ther. 2008;7:2977–2987. doi: 10.1158/1535-7163.MCT-08-0447. [DOI] [PubMed] [Google Scholar]
- 299.Kim H.S., Tian L., Jung M., Choi S.K., Sun Y., Kim H., Moon W.K. Downregulation of Choline Kinase-Alpha Enhances Autophagy in Tamoxifen-Resistant Breast Cancer Cells. PLoS ONE. 2015;10:e0141110. doi: 10.1371/journal.pone.0141110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Gupta A., Roy S., Lazar A.J.F., Wang W.-L., McAuliffe J.C., Reynoso D., McMahon J., Taguchi T., Floris G., Debiec-Rychter M., et al. Autophagy inhibition and antimalarials promote cell death in gastrointestinal stromal tumor (GIST) Proc. Natl. Acad. Sci. USA. 2010;107:14333–14338. doi: 10.1073/pnas.1000248107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Mishima Y., Mishima Y., Terui Y., Kimura S., Hatake K. An Autophagy Inhibitor, Chloroquine, Overcomes an Imatinib-Resistant T315I Mutant of Bcr/Abl, Whose Latent May Exist Before Imatinib Treatment. Blood. 2009;114:2183. doi: 10.1182/blood.V114.22.2183.2183. [DOI] [Google Scholar]
- 302.Crowley L.C., O’Donovan T.R., Nyhan M.J., McKenna S.L. Pharmacological agents with inherent anti-autophagic activity improve the cytotoxicity of imatinib. Oncol. Rep. 2013;29:2261–2268. doi: 10.3892/or.2013.2377. [DOI] [PubMed] [Google Scholar]
- 303.Rothe K., Lin H., Lin K.B.L., Leung A., Wang H.M., Malekesmaeili M., Brinkman R.R., Forrest D.L., Gorski S.M., Jiang X. The core autophagy protein ATG4B is a potential biomarker and therapeutic target in CML stem/progenitor cells. Blood. 2014;123:3622–3634. doi: 10.1182/blood-2013-07-516807. [DOI] [PubMed] [Google Scholar]
- 304.Lee J., Park D., Lee Y. Metformin Synergistically Potentiates the Antitumor Effects of Imatinib in Colorectal Cancer Cells. Dev. Reprod. 2017 doi: 10.12717/DR.2017.21.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Yu Y., Cao L., Yang L., Kang R., Lotze M., Tang D. microRNA 30A promotes autophagy in response to cancer therapy. Autophagy. 2012;8:853–855. doi: 10.4161/auto.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Yu Y., Yang L., Zhao M., Zhu S., Kang R., Vernon P., Tang D., Cao L. Targeting microRNA-30a-mediated autophagy enhances imatinib activity against human chronic myeloid leukemia cells. Leukemia. 2012;26:1752–1760. doi: 10.1038/leu.2012.65. [DOI] [PubMed] [Google Scholar]
- 307.Liang X., De Vera M.E., Buchser W.J., Romo de Vivar Chavez A., Loughran P., Beer Stolz D., Basse P., Wang T., Van Houten B., Zeh H.J., et al. Inhibiting systemic autophagy during interleukin 2 immunotherapy promotes long-term tumor regression. Cancer Res. 2012;72:2791–2801. doi: 10.1158/0008-5472.CAN-12-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Lotze M.T., Buchser W.J., Liang X. Blocking the interleukin 2 (IL2)-induced systemic autophagic syndrome promotes profound antitumor effects and limits toxicity. Autophagy. 2012;8:1264–1266. doi: 10.4161/auto.20752. [DOI] [PubMed] [Google Scholar]
- 309.Chude C.I., Amaravadi R.K. Targeting Autophagy in Cancer: Update on Clinical Trials and Novel Inhibitors. Int. J. Mol. Sci. 2017;18:1279. doi: 10.3390/ijms18061279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Verbaanderd C., Maes H., Schaaf M.B., Sukhatme V.P., Pantziarka P., Sukhatme V., Agostinis P., Bouche G. Repurposing Drugs in Oncology (ReDO)-chloroquine and hydroxychloroquine as anti-cancer agents. Ecancermedicalscience. 2017;11:781. doi: 10.3332/ecancer.2017.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Poklepovic A., Gewirtz D.A. Outcome of early clinical trials of the combination of hydroxychloroquine with chemotherapy in cancer. Autophagy. 2014;10:1478–1480. doi: 10.4161/auto.29428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Solitro A.R., MacKeigan J.P. Leaving the lysosome behind: Novel developments in autophagy inhibition. Future Med. Chem. 2015;8:73–86. doi: 10.4155/fmc.15.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Das C.K., Mandal M. Pro-survival autophagy and cancer cell resistance to therapy. Cancer Metastasis Rev. 2018;37:749–766. doi: 10.1007/s10555-018-9727-z. [DOI] [PubMed] [Google Scholar]
- 314.Cargnello M., Roux P.P. Activation and Function of the MAPKs and Their Substrates, the MAPK-Activated Protein Kinases. Microbiol. Mol. Biol. Rev. 2011;75:50–83. doi: 10.1128/MMBR.00031-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Sun Y., Liu W.Z., Liu T., Feng X., Yang N., Zhou H.-F. Signaling pathway of MAPK/ERK in cell proliferation, differentiation, migration, senescence and apoptosis. J. Recept. Signal Transduct. Res. 2015;35:600–604. doi: 10.3109/10799893.2015.1030412. [DOI] [PubMed] [Google Scholar]
- 316.Burotto M., Chiou V.L., Lee J.-M., Kohn E.C. The MAPK pathway across different malignancies: A new perspective. Cancer. 2014;120:3446–3456. doi: 10.1002/cncr.28864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Katz M., Amit I., Yarden Y. Regulation of MAPKs by growth factors and receptor tyrosine kinases. Biochim. Biophys. Acta. 2007;1773:1161–1176. doi: 10.1016/j.bbamcr.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Fujimoto N., Wislez M., Zhang J., Iwanaga K., Dackor J., Hanna A.E., Kalyankrishna S., Cody D.D., Price R.E., Sato M., et al. High expression of ErbB family members and their ligands in lung adenocarcinomas that are sensitive to inhibition of epidermal growth factor receptor. Cancer Res. 2005;65:11478–11485. doi: 10.1158/0008-5472.CAN-05-1977. [DOI] [PubMed] [Google Scholar]
- 319.Carlsson J., Nordgren H., Sjöström J., Wester K., Villman K., Bengtsson N.O., Ostenstad B., Lundqvist H., Blomqvist C. HER2 expression in breast cancer primary tumours and corresponding metastases. Original data and literature review. Br. J. Cancer. 2004;90:2344–2348. doi: 10.1038/sj.bjc.6601881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Rosell R., Carcereny E., Gervais R., Vergnenegre A., Massuti B., Felip E., Palmero R., Garcia-Gomez R., Pallares C., Sanchez J.M., et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–246. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 321.Phuchareon J., McCormick F., Eisele D.W., Tetsu O. EGFR inhibition evokes innate drug resistance in lung cancer cells by preventing AKT activity and thus inactivating Ets-1 function. Proc. Natl. Acad. Sci. USA. 2015;112:E3855––E3863. doi: 10.1073/pnas.1510733112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Liu Q., Yu S., Zhao W., Qin S., Chu Q., Wu K. EGFR-TKIs resistance via EGFR-independent signaling pathways. Mol. Cancer. 2018;17:53. doi: 10.1186/s12943-018-0793-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Wu S.G., Shih J.Y. Management of acquired resistance to EGFR TKI–targeted therapy in advanced non-small cell lung cancer. Mol. Cancer. 2018;17:38. doi: 10.1186/s12943-018-0777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Westover D., Zugazagoitia J., Cho B.C., Lovly C.M., Paz-Ares L. Mechanisms of acquired resistance to first- and second-generation EGFR tyrosine kinase inhibitors. Ann. Oncol. 2018;29:10–19. doi: 10.1093/annonc/mdx703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Ricordel C., Friboulet L., Facchinetti F., Soria J.-C. Molecular mechanisms of acquired resistance to third-generation EGFR-TKIs in EGFR T790M-mutant lung cancer. Ann. Oncol. 2018;29:28–37. doi: 10.1093/annonc/mdx705. [DOI] [PubMed] [Google Scholar]
- 326.Nagaria T.S., Shi C., Leduc C., Hoskin V., Sikdar S., Sangrar W., Greer P.A. Combined targeting of Raf and Mek synergistically inhibits tumorigenesis in triple negative breast cancer model systems. Oncotarget. 2017;8:80804–80819. doi: 10.18632/oncotarget.20534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Khunger A., Khunger M., Velcheti V. Dabrafenib in combination with trametinib in the treatment of patients with BRAF V600-positive advanced or metastatic non-small cell lung cancer: Clinical evidence and experience. Ther. Adv. Respir. Dis. 2018;12:1753466618767611. doi: 10.1177/1753466618767611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Wolff A.C., Hammond M.E.H., Allison K.H., Harvey B.E., Mangu P.B., Bartlett J.M.S., Bilous M., Ellis I.O., Fitzgibbons P., Hanna W., et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J. Clin. Oncol. 2018;36:2105–2122. doi: 10.1200/JCO.2018.77.8738. [DOI] [PubMed] [Google Scholar]
- 329.Luque-Cabal M., García-Teijido P., Fernández-Pérez Y., Sánchez-Lorenzo L., Palacio-Vázquez I. Mechanisms Behind the Resistance to Trastuzumab in HER2-Amplified Breast Cancer and Strategies to Overcome It. Clin. Med. Insights Oncol. 2016;10:21–30. doi: 10.4137/CMO.S34537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Kabraji S., Ni J., Lin N.U., Xie S., Winer E.P., Zhao J.J. Drug Resistance in HER2-Positive Breast Cancer Brain Metastases: Blame the Barrier or the Brain? Clin. Cancer Res. 2018;24:1795–1804. doi: 10.1158/1078-0432.CCR-17-3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Donnelly S.M., Paplomata E., Peake B.M., Sanabria E., Chen Z., Nahta R. P38 MAPK contributes to resistance and invasiveness of HER2- overexpressing breast cancer. Curr. Med. Chem. 2014;21:501–510. doi: 10.2174/0929867320666131119155023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Jin M.H., Nam A.-R., Park J.E., Bang J.-H., Bang Y.-J., Oh D.-Y. Resistance Mechanism against Trastuzumab in HER2-Positive Cancer Cells and Its Negation by Src Inhibition. Mol. Cancer Ther. 2017;16:1145–1154. doi: 10.1158/1535-7163.MCT-16-0669. [DOI] [PubMed] [Google Scholar]
- 333.Iwatsuki M., Kojiro E., Baba H. Molecular mechanism of secondary-resistant for trastuzumab in gastric cancer. JCO. 2016;34:58. doi: 10.1200/jco.2016.34.4_suppl.58. [DOI] [Google Scholar]
- 334.De Gagliato D.M., Jardim D.L.F., Marchesi M.S.P., Hortobagyi G.N. Mechanisms of resistance and sensitivity to anti-HER2 therapies in HER2+ breast cancer. Oncotarget. 2016;7:64431–64446. doi: 10.18632/oncotarget.7043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Flem-Karlsen K., Tekle C., Øyjord T., Flørenes V.A., Mælandsmo G.M., Fodstad Ø., Nunes-Xavier C.E. p38 MAPK activation through B7-H3-mediated DUSP10 repression promotes chemoresistance. Sci. Rep. 2019;9:5839. doi: 10.1038/s41598-019-42303-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Inamura K., Takazawa Y., Inoue Y., Yokouchi Y., Kobayashi M., Saiura A., Shibutani T., Ishikawa Y. Tumor B7-H3 (CD276) Expression and Survival in Pancreatic Cancer. J. Clin. Med. 2018;7:172. doi: 10.3390/jcm7070172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Inamura K., Amori G., Yuasa T., Yamamoto S., Yonese J., Ishikawa Y. Relationship of B7-H3 expression in tumor cells and tumor vasculature with FOXP3+ regulatory T cells in renal cell carcinoma. Cancer Manag. Res. 2019;11:7021–7030. doi: 10.2147/CMAR.S209205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Koul H.K., Pal M., Koul S. Role of p38 MAP Kinase Signal Transduction in Solid Tumors. Genes Cancer. 2013;4:342–359. doi: 10.1177/1947601913507951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.García-Cano J., Roche O., Cimas F.J., Pascual-Serra R., Ortega-Muelas M., Fernández-Aroca D.M., Sánchez-Prieto R. p38MAPK and Chemotherapy: We Always Need to Hear Both Sides of the Story. Front. Cell Dev. Biol. 2016:4. doi: 10.3389/fcell.2016.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Hammaker D., Firestein G.S. ‘Go upstream, young man’: Lessons learned from the p38 saga. Ann. Rheum. Dis. 2010;69(Suppl. 1):i77–i82. doi: 10.1136/ard.2009.119479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Dambach D.M. Potential adverse effects associated with inhibition of p38alpha/beta MAP kinases. Curr. Top. Med. Chem. 2005;5:929–939. doi: 10.2174/1568026054985911. [DOI] [PubMed] [Google Scholar]
- 342.Patnaik A., Haluska P., Tolcher A.W., Erlichman C., Papadopoulos K.P., Lensing J.L., Beeram M., Molina J.R., Rasco D.W., Arcos R.R., et al. A First-in-Human Phase I Study of the Oral p38 MAPK Inhibitor, Ralimetinib (LY2228820 Dimesylate), in Patients with Advanced Cancer. Clin. Cancer Res. 2016;22:1095–1102. doi: 10.1158/1078-0432.CCR-15-1718. [DOI] [PubMed] [Google Scholar]
- 343.Goldman J.W., Rosen L.S., Tolcher A.W., Papadopoulos K., Beeram M., Shi P., Pitou C., Bell R., Kulanthaivel P., Zhang X., et al. Phase 1 and pharmacokinetic study of LY3007113, a p38 MAPK inhibitor, in patients with advanced cancer. Investig. New Drugs. 2018;36:629–637. doi: 10.1007/s10637-017-0532-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.De la Cruz-Morcillo M.A., Valero M.L.L., Callejas-Valera J.L., Arias-González L., Melgar-Rojas P., Galán-Moya E.M., García-Gil E., García-Cano J., Sánchez-Prieto R. P38MAPK is a major determinant of the balance between apoptosis and autophagy triggered by 5-fluorouracil: Implication in resistance. Oncogene. 2012;31:1073–1085. doi: 10.1038/onc.2011.321. [DOI] [PubMed] [Google Scholar]
- 345.Ojha R., Leli N.M., Onorati A., Piao S., Verginadis I.I., Tameire F., Rebecca V.W., Chude C.I., Murugan S., Fennelly C., et al. ER Translocation of the MAPK Pathway Drives Therapy Resistance in BRAF-Mutant Melanoma. Cancer Discov. 2019;9:396–415. doi: 10.1158/2159-8290.CD-18-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Bryant K.L., Stalnecker C.A., Zeitouni D., Klomp J.E., Peng S., Tikunov A.P., Gunda V., Pierobon M., Waters A.M., George S.D., et al. Combination of ERK and autophagy inhibition as a treatment approach for pancreatic cancer. Nat. Med. 2019;25:628–640. doi: 10.1038/s41591-019-0368-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Dolgin E. Anticancer autophagy inhibitors attract ’resurgent’ interest. Nat. Rev. Drug Discov. 2019;18:408. doi: 10.1038/d41573-019-00072-1. [DOI] [PubMed] [Google Scholar]
- 348.Martini M., Santis M.C.D., Braccini L., Gulluni F., Hirsch E. PI3K/AKT signaling pathway and cancer: An updated review. Ann. Med. 2014;46:372–383. doi: 10.3109/07853890.2014.912836. [DOI] [PubMed] [Google Scholar]
- 349.Yang J., Nie J., Ma X., Wei Y., Peng Y., Wei X. Targeting PI3K in cancer: Mechanisms and advances in clinical trials. Mol. Cancer. 2019;18:26. doi: 10.1186/s12943-019-0954-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Giles K.M., Rosenbaum B.E., Berger M., Izsak A., Li Y., Illa Bochaca I., Vega-Saenz de Miera E., Wang J., Darvishian F., Zhong H., et al. Revisiting the Clinical and Biologic Relevance of Partial PTEN Loss in Melanoma. J. Invest. Dermatol. 2019;139:430–438. doi: 10.1016/j.jid.2018.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Catalanotti F., Cheng D.T., Shoushtari A.N., Johnson D.B., Panageas K.S., Momtaz P., Higham C., Won H.H., Harding J.J., Merghoub T., et al. PTEN Loss-of-Function Alterations Are Associated With Intrinsic Resistance to BRAF Inhibitors in Metastatic Melanoma. JCO Precision Oncology. 2017:1–15. doi: 10.1200/PO.16.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Paraiso K.H.T., Xiang Y., Rebecca V.W., Abel E.V., Chen Y.A., Munko A.C., Wood E., Fedorenko I.V., Sondak V.K., Anderson A.R.A., et al. PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res. 2011;71:2750–2760. doi: 10.1158/0008-5472.CAN-10-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Wang Q., Shi Y., Zhou K., Wang L., Yan Z., Liu Y., Xu L., Zhao S., Chu H., Shi T., et al. PIK3CA mutations confer resistance to first-line chemotherapy in colorectal cancer. Cell Death Dis. 2018;9:1–11. doi: 10.1038/s41419-018-0776-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Dillon L.M., Miller T.W. Therapeutic targeting of cancers with loss of PTEN function. Curr. Drug Targets. 2014;15:65–79. doi: 10.2174/1389450114666140106100909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Li X., Dai D., Chen B., Tang H., Xie X., Wei W. Efficacy of PI3K/AKT/mTOR pathway inhibitors for the treatment of advanced solid cancers: A literature-based meta-analysis of 46 randomised control trials. PLoS ONE. 2018;13:e0192464. doi: 10.1371/journal.pone.0192464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Jansen V.M., Mayer I.A., Arteaga C.L. Is There a Future for AKT Inhibitors in the Treatment of Cancer? Clin. Cancer Res. 2016;22:2599–2601. doi: 10.1158/1078-0432.CCR-16-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Yoshida-Ichikawa Y., Tanabe M., Tokuda E., Shimizu H., Horimoto Y., Miura K., Saito M. Overcoming the Adverse Effects of Everolimus to Achieve Maximum Efficacy in the Treatment of Inoperable Breast Cancer: A Review of 11 Cases at Our Hospital. Case Rep. Oncol. 2018;11:511–520. doi: 10.1159/000490787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Motzer R.J., Escudier B., Oudard S., Hutson T.E., Porta C., Bracarda S., Grünwald V., Thompson J.A., Figlin R.A., Hollaender N., et al. Efficacy of everolimus in advanced renal cell carcinoma: A double-blind, randomised, placebo-controlled phase III trial. Lancet. 2008;372:449–456. doi: 10.1016/S0140-6736(08)61039-9. [DOI] [PubMed] [Google Scholar]
- 359.Chan D.L., Segelov E., Singh S. Everolimus in the management of metastatic neuroendocrine tumours. Therap. Adv. Gastroenterol. 2017;10:132–141. doi: 10.1177/1756283X16674660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Crazzolara R., Bradstock K.F., Bendall L.J. RAD001 (Everolimus) induces autophagy in acute lymphoblastic leukemia. Autophagy. 2009;5:727–728. doi: 10.4161/auto.5.5.8507. [DOI] [PubMed] [Google Scholar]
- 361.Santanam U., Banach-Petrosky W., Abate-Shen C., Shen M.M., White E., DiPaola R.S. Atg7 cooperates with Pten loss to drive prostate cancer tumor growth. Genes Dev. 2016;30:399–407. doi: 10.1101/gad.274134.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Pei L., Kong Y., Shao C., Yue X., Wang Z., Zhang N. Heme oxygenase-1 induction mediates chemoresistance of breast cancer cells to pharmorubicin by promoting autophagy via PI3K/AKT pathway. J. Cell. Mol. Med. 2018;22:5311–5321. doi: 10.1111/jcmm.13800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Ferrando M., Gueron G., Elguero B., Giudice J., Salles A., Leskow F.C., Jares-Erijman E.A., Colombo L., Meiss R., Navone N., et al. Heme oxygenase 1 (HO-1) challenges the angiogenic switch in prostate cancer. Angiogenesis. 2011;14:467–479. doi: 10.1007/s10456-011-9230-4. [DOI] [PubMed] [Google Scholar]
- 364.Halin Bergström S., Nilsson M., Adamo H., Thysell E., Jernberg E., Stattin P., Widmark A., Wikström P., Bergh A. Extratumoral Heme Oxygenase-1 (HO-1) Expressing Macrophages Likely Promote Primary and Metastatic Prostate Tumor Growth. PLoS ONE. 2016;11:e0157280. doi: 10.1371/journal.pone.0157280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Degese M.S., Mendizabal J.E., Gandini N.A., Gutkind J.S., Molinolo A., Hewitt S.M., Curino A.C., Coso O.A., Facchinetti M.M. Expression of heme oxygenase-1 in non-small cell lung cancer (NSCLC) and its correlation with clinical data. Lung Cancer. 2012;77:168–175. doi: 10.1016/j.lungcan.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Tsai J.R., Wang H.M., Liu P.L., Chen Y.H., Yang M.C., Chou S.H., Cheng Y.J., Yin W.H., Hwang J.J., Chong I.W. High expression of heme oxygenase-1 is associated with tumor invasiveness and poor clinical outcome in non-small cell lung cancer patients. Cell Oncol. (Dordr) 2012;35:461–471. doi: 10.1007/s13402-012-0105-5. [DOI] [PubMed] [Google Scholar]
- 367.Kaveney A.D., Mehnert J.M., Tan A.R., Aisner J., Moss R.A., Gibbon D., Adams S., Fischer J., Scott P., Gable C., et al. A phase I trial of MK-2206 and hydroxychloroquine(HCQ) in solid tumors, melanoma, renal, and prostate cancer to examine the role of autophagy in tumorigenesis. JCO. 2014;32:TPS2640. doi: 10.1200/jco.2014.32.15_suppl.tps2640. [DOI] [Google Scholar]
- 368.Mancias J.D., Kimmelman A.C. Mechanisms of selective autophagy in normal physiology and cancer. J. Mol. Biol. 2016;428:1659–1680. doi: 10.1016/j.jmb.2016.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Galluzzi L., Baehrecke E.H., Ballabio A., Boya P., Bravo-San Pedro J.M., Cecconi F., Choi A.M., Chu C.T., Codogno P., Colombo M.I., et al. Molecular definitions of autophagy and related processes. EMBO J. 2017;36:1811–1836. doi: 10.15252/embj.201796697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Cohen-Kaplan V., Livneh I., Avni N., Fabre B., Ziv T., Kwon Y.T., Ciechanover A. p62- and ubiquitin-dependent stress-induced autophagy of the mammalian 26S proteasome. Proc. Natl. Acad. Sci. USA. 2016;113:E7490–E7499. doi: 10.1073/pnas.1615455113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Sánchez-Martín P., Komatsu M. p62/SQSTM1—Steering the cell through health and disease. J. Cell. Sci. 2018;131:jcs222836. doi: 10.1242/jcs.222836. [DOI] [PubMed] [Google Scholar]
- 372.Ichimura Y., Komatsu M. Activation of p62/SQSTM1-KEAP1-Nuclear Factor Erythroid 2-Related Factor 2 Pathway in Cancer. Front. Oncol. 2018;8:210. doi: 10.3389/fonc.2018.00210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Saito T., Ichimura Y., Taguchi K., Suzuki T., Mizushima T., Takagi K., Hirose Y., Nagahashi M., Iso T., Fukutomi T., et al. p62/Sqstm1 promotes malignancy of HCV-positive hepatocellular carcinoma through Nrf2-dependent metabolic reprogramming. Nat. Commun. 2016;7:12030. doi: 10.1038/ncomms12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Todoric J., Antonucci L., Di Caro G., Li N., Wu X., Lytle N.K., Dhar D., Banerjee S., Fagman J.B., Browne C.D., et al. Stress-Activated NRF2-MDM2 Cascade Controls Neoplastic Progression in Pancreas. Cancer Cell. 2017;32:824–839.e8. doi: 10.1016/j.ccell.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Xia M., Yu H., Gu S., Xu Y., Su J., Li H., Kang J., Cui M. p62/SQSTM1 is involved in cisplatin resistance in human ovarian cancer cells via the Keap1-Nrf2-ARE system. Int. J. Oncol. 2014;45:2341–2348. doi: 10.3892/ijo.2014.2669. [DOI] [PubMed] [Google Scholar]
- 376.Ryoo I.G., Choi B.H., Ku S.K., Kwak M.K. High CD44 expression mediates p62-associated NFE2L2/NRF2 activation in breast cancer stem cell-like cells: Implications for cancer stem cell resistance. Redox Biol. 2018;17:246–258. doi: 10.1016/j.redox.2018.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Battista R.A., Resnati M., Facchi C., Ruggieri E., Cremasco F., Paradiso F., Orfanelli U., Giordano L., Bussi M., Cenci S., et al. Autophagy mediates epithelial cancer chemoresistance by reducing p62/SQSTM1 accumulation. PLoS ONE. 2018;13:e0201621. doi: 10.1371/journal.pone.0201621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Towers C.G., Fitzwalter B.E., Regan D., Goodspeed A., Morgan M.J., Liu C.-W., Gustafson D.L., Thorburn A. Cancer Cells Upregulate NRF2 Signaling to Adapt to Autophagy Inhibition. Dev. Cell. 2019;50:690–703.e6. doi: 10.1016/j.devcel.2019.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Fernald K., Kurokawa M. Evading apoptosis in cancer. Trends Cell Biol. 2013;23:620–633. doi: 10.1016/j.tcb.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Chen L., Zeng Y., Zhou S.F. Current Understanding of Apoptosis—Programmed Cell Death. IntechOpen Limited; London, UK: 2018. Role of Apoptosis in Cancer Resistance to Chemotherapy. [DOI] [Google Scholar]
- 381.Pistritto G., Trisciuoglio D., Ceci C., Garufi A., D’Orazi G. Apoptosis as anticancer mechanism: Function and dysfunction of its modulators and targeted therapeutic strategies. Aging. 2016;8:603–619. doi: 10.18632/aging.100934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Hata A.N., Engelman J.A., Faber A.C. The BCL2 Family: Key Mediators of the Apoptotic Response to Targeted Anticancer Therapeutics. Cancer Discov. 2015;5:475–487. doi: 10.1158/2159-8290.CD-15-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.You H., Pellegrini M., Tsuchihara K., Yamamoto K., Hacker G., Erlacher M., Villunger A., Mak T.W. FOXO3a-dependent regulation of Puma in response to cytokine/growth factor withdrawal. J. Exp. Med. 2006;203:1657–1663. doi: 10.1084/jem.20060353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Akhter R., Sanphui P., Biswas S.C. The essential role of p53 Upregulated Modulator of Apoptosis and its regulation by FOXO3A transcription factor in β-amyloid induced neuron death. J. Biol. Chem. 2014 doi: 10.1074/jbc.M113.519355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.DeVorkin L., Choutka C., Gorski S.M. The interplay between autophagy and apoptosis. In: Hayat E., editor. Autophagy: Cancer, Other Pathologies, Inflammation, Immunity, and Infection. Volume 3 Elsevier; Amsterdam, The Netherlands: 2014. Chapter XXIV. [Google Scholar]
- 386.Su M., Mei Y., Sinha S. Role of the Crosstalk between Autophagy and Apoptosis in Cancer. J. Oncol. 2013 doi: 10.1155/2013/102735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Thorburn J., Andrysik Z., Staskiewicz L., Gump J., Maycotte P., Oberst A., Green D.R., Espinosa J.M., Thorburn A. Autophagy controls the kinetics and extent of mitochondrial apoptosis by regulating PUMA levels. Cell Rep. 2014;7:45–52. doi: 10.1016/j.celrep.2014.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Eijkelenboom A., Mokry M., de Wit E., Smits L.M., Polderman P.E., van Triest M.H., van Boxtel R., Schulze A., de Laat W., Cuppen E., et al. Genome-wide analysis of FOXO3 mediated transcription regulation through RNA polymerase II profiling. Mol. Syst. Biol. 2013;9:638. doi: 10.1038/msb.2012.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Warr M.R., Binnewies M., Flach J., Reynaud D., Garg T., Malhotra R., Debnath J., Passegué E. FOXO3A directs a protective autophagy program in haematopoietic stem cells. Nature. 2013;494:323–327. doi: 10.1038/nature11895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Zhang J., Lei W., Chen X., Wang S., Qian W. Oxidative stress response induced by chemotherapy in leukemia treatment. Mol. Clin. Oncol. 2018;8:391–399. doi: 10.3892/mco.2018.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Vasconcellos L.R.C., Dutra F.F., Siqueira M.S., Paula-Neto H.A., Dahan J., Kiarely E., Carneiro L.A.M., Bozza M.T., Travassos L.H. Protein aggregation as a cellular response to oxidative stress induced by heme and iron. Proc. Natl. Acad. Sci. USA. 2016;113:E7474–E7482. doi: 10.1073/pnas.1608928113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Towers C.G., Thorburn A. Therapeutic Targeting of Autophagy. EBioMedicine. 2016;14:15–23. doi: 10.1016/j.ebiom.2016.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Barnard R.A., Regan D.P., Hansen R.J., Maycotte P., Thorburn A., Gustafson D.L. Autophagy Inhibition Delays Early but Not Late-Stage Metastatic Disease. J. Pharmacol. Exp. Ther. 2016;358:282–293. doi: 10.1124/jpet.116.233908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Wang Y., Xiong H., Liu D., Hill C., Ertay A., Li J., Zou Y., Miller P., White E., Downward J., et al. Autophagy inhibition specifically promotes epithelial-mesenchymal transition and invasion in RAS-mutated cancer cells. Autophagy. 2019;15:886–899. doi: 10.1080/15548627.2019.1569912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Thorburn A. Autophagy and Its Effects: Making Sense of Double-Edged Swords. PLoS Biol. 2014;12:e1001967. doi: 10.1371/journal.pbio.1001967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Lauzier A., Normandeau-Guimond J., Vaillancourt-Lavigueur V., Boivin V., Charbonneau M., Rivard N., Scott M.S., Dubois C.M., Jean S. Colorectal cancer cells respond differentially to autophagy inhibition in vivo. Sci. Rep. 2019;9:1–16. doi: 10.1038/s41598-019-47659-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Thorburn J., Staskiewicz L., Goodall M.L., Dimberg L., Frankel A.E., Ford H.L., Thorburn A. Non-cell-autonomous Effects of Autophagy Inhibition in Tumor Cells Promote Growth of Drug-resistant Cells. Mol. Pharmacol. 2017;91:58–64. doi: 10.1124/mol.116.106070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Lindqvist L.M., Simon A.K., Baehrecke E.H. Current questions and possible controversies in autophagy. Cell Death Discov. 2015;1:1–7. doi: 10.1038/cddiscovery.2015.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Gewirtz D.A. The challenge of developing autophagy inhibition as a therapeutic strategy. Cancer Res. 2016;76:5610–5614. doi: 10.1158/0008-5472.CAN-16-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Görgülü K., Diakopoulos K.N., Ai J., Schoeps B., Kabacaoglu D., Karpathaki A.F., Ciecielski K.J., Kaya-Aksoy E., Ruess D.A., Berninger A., et al. Levels of the Autophagy-Related 5 Protein Affect Progression and Metastasis of Pancreatic Tumors in Mice. Gastroenterology. 2019;156:203–217.e20. doi: 10.1053/j.gastro.2018.09.053. [DOI] [PubMed] [Google Scholar]
- 401.An Y., Bi F., You Y., Liu X., Yang Q. Development of a Novel Autophagy-related Prognostic Signature for Serous Ovarian Cancer. J. Cancer. 2018;9:4058–4071. doi: 10.7150/jca.25587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Bortnik S., Gorski S.M. Clinical Applications of Autophagy Proteins in Cancer: From Potential Targets to Biomarkers. Int. J. Mol. Sci. 2017;18:1496. doi: 10.3390/ijms18071496. [DOI] [PMC free article] [PubMed] [Google Scholar]