Abstract
The current review presents a meta-analysis of the existing empirical literature on the prevalence of non-suicidal self-injury (NSSI) among lesbian, gay, bisexual, and transgender (LGBT) individuals, as well as on correlates of NSSI within sexual and gender minority populations. Eligible publications (n = 51) were identified through a systematic search of PsycINFO, MEDLINE, and Embase, supplemented by a search of references of prior reviews on this topic. NSSI prevalence rates were quite elevated among sexual (29.68% lifetime) and gender (46.65% lifetime) minority individuals compared to heterosexual and/or cisgender peers (14.57% lifetime), with transgender (46.65% lifetime) and bisexual (41.47% lifetime) individuals being at greatest risk. Even among these group findings, sexual minority youth emerged as an especially vulnerable population. Moreover, current evidence suggests these rates and differences between LGBT and heterosexual and/or cisgender peers have not declined over time. These findings may in some measure be due to the existence of LGBT-specific risk correlates combined with general risk correlates being more severe among sexual and gender minority populations. Additional research, particularly employing a longitudinal design, is needed in this area to advance efforts to reduce risk for NSSI among sexual and gender minority individuals.
Keywords: LGBT, meta-analysis, non-suicidal self-injury, self-harm, sexual minority
1. Introduction
Non-suicidal self-injury, defined as the direct and deliberate destruction of one’s own body tissue without any suicidal intent, has received growing attention over the past several decades. as phenomenologically distinct from suicidal behavior (Brent, 2011; Mars et al., 2014; Wichstrøm, 2009), its clinical importance has been the subject of increasing recognition (American Psychiatric Association, 2013). Indeed, substantial evidence has emerged to indicate that NSSI is a stronger predictor of suicide attempts than is a history of attempts (Asarnow et al., 2011; Ribeiro et al., 2016; Wilkinson, Kelvin, Roberts, Dubicka, & Goodyer, 2011). Despite these important developments, the current evidence base for psychological interventions targeting NSSI appears to be quite modest (for two recent meta-analyses on this issue, see Calati & Courtet, 2016; Ougrin, Tranah, Stahl, Moran, & Asarnow, 2015).
Characterizing populations at risk for engaging in NSSI is imperative for furthering the development of intervention strategies to reduce the prevalence of this behavior and associated negative outcomes. Sexual and gender minority populations have been identified as especially at risk for a variety of negative health conditions, including poorer mental health functioning (Conron, Mimiaga, & Landers, 2010; Garofalo, Wolf, Wissow, Woods, & Goodman, 1999; Pakula, Shoveller, Ratner, & Carpiano, 2016). Indeed, disparities in health outcomes among lesbian, gay, bisexual, and transgender (LGBT) individuals have received increasing attention in recent years (Institute of Medicine, 2011; Obedin-Maliver et al., 2011). Self-injurious thoughts and behaviors, including NSSI, are no exception in this regard (Batejan, Jarvi, & Swenson, 2015; Jackman, Honig, & Bockting, 2016; O’Brien, Liu, Putney, Burke, & Aguinaldo, 2017).
Nonetheless, several fundamental aspects of NSSI in sexual and gender minority populations remain relatively undefined. In particular, there is a need for reliable estimates of the prevalence of NSSI in these populations, so as to ascertain with precision the magnitude of this issue among sexual and gender minority individuals and to monitor progress in addressing disparities in the occurrence of this clinical phenomenon.
There are unique challenges, however, accurately to determining the prevalence of NSSI in these populations. Specifically, decisions regarding how LGBT status is operationalized may influence estimates of NSSI prevalence. Indeed, even for estimates LGB prevalence, significant differences have been found depending on how sexual orientation is defined (Meyer & Wilson, 2009; Savin-Williams, 2006). Some studies of NSSI have based sexual minority status on same-sex behavior. Yet, relying entirely on this approach is not without its complications. A substantial proportion of individuals who identify as a member of a sexual minority group may not (yet) have engaged in same-sex behavior. This consideration is of particular relevance to assessing sexual minority outcomes in adolescence, a period of development in which lower rates of lifetime engagement in sexual behavior would reasonably be expected (Mustanski & Liu, 2013). Also especially pertinent to basing sexual minority status on sexual behavior in studies of negative health-related outcomes in youth is that early lifetime onset in sexual behavior is a risky sexual behavior, which itself has been associated with negative mental-health outcomes, including NSSI (Hilt, Nock, Lloyd-Richardson, & Prinstein, 2008; Wichstrøm, 2009). For this reason, using same-sex behavior as the sole index of sexual minority status introduces a methodological confound that may artificially inflate estimates of NSSI prevalence in sexual minority youth. An alternative index adopted in other studies, self-identified sexual orientation circumvents these issues regarding same-sex behavior. It is important to note, however, that not everyone who has engaged in same-sex behavior necessarily self-identifies as a sexual minority individual (Mustanski & Liu, 2013), meaning that a subset of potentially at-risk individuals may be missed when relying entirely on this index of sexual orientation. Indeed, there is recent evidence that individuals whose sexual identity is discordant with their sexual behavior may be an especially at-risk group for engaging in self-injurious behaviors (Annor et al., 2018). Finally, same-sex attraction has been used as another index of sexual minority status. Yet, not everyone with same-sex attraction necessarily self-identifies as a sexual minority individual. It is therefore important to consider multiple indices of sexual orientation accurately and comprehensively to estimate the prevalence of NSSI in sexual minority populations.
In addition to the need for precise NSSI prevalence estimates to determine the scope of this clinical phenomenon and to monitor temporal trends in sexual and gender minority groups, identifying correlates of NSSI in these populations is necessary for characterizing potential risk and protective factors for this behavior among LGBT individuals. Such knowledge is invaluable insofar as it may inform risk stratification strategies. Moreover, correlates may be promising candidates for future investigation as potential prospective predictors of NSSI in these populations, and thus potential targets for the development of future clinical interventions.
At a more general level, the study of correlates of NSSI in LGBT populations is needed to provide resolution to the fundamental question of why sexual and gender minority groups are at greater risk for engaging in NSSI. Of direct relevance to this question, the minority stress model and the gender minority stress model adapted for transgender individuals, posit that stigma, discrimination, and prejudice create a hostile and stressful environment that increases the risk for negative mental health outcomes among sexual and gender minority individuals (Meyer, 2003; Testa et al., 2016). Particularly, these models suggest specific stress processes associated uniquely with LGBT individuals that confer additional risk for mental health disorder including, but not limited to, experience of prejudice, discrimination, victimization, rejection, nondisclosure of sexual minority status, and internalized homophobia or transphobia (Meyer, 2003; Testa et al., 2016). In contrast, adaptive coping mechanisms targeting stressful circumstances and increases in social support present important protective factors against negative mental health outcomes among minority populations (Meyer, 2003). Although many clinical interventions address adaptive coping mechanisms, the minority stress model would suggest specific modifications to coping that specifically target coping with societal stigma and discrimination. In the minority stress model, risk factors for mental health conditions specific to LGBT populations exist on a continuum from the environment (i.e., distal factors) to the internal/self (i.e., proximal factors), with societal stigma representing the most environmental to internalized homophobia and transphobia the most internal risk factor. In a word, based on the sexual and gender minority stress models, LGBT populations may be at elevated risk for NSSI because in addition to general risk factors that both they and heterosexual/cisgender compeers experience, they are subject to risk factors uniquely related to their minority status.
To date, there have been a prior meta-analysis (Batejan et al., 2015) and a qualitative review (Jackman et al., 2016) examining sexual orientation and/or gender minority status in relation to NSSI. Both reviews were consistent in finding higher risk for NSSI among sexual and/or gender minority individuals relative to heterosexual and/or cisgender peers. Although of clear value for providing the first quantitative review in this area, the prior meta-analysis included only 11 publications, a minority of the currently available studies, was unable to perform moderator analyses or analyses of NSSI correlates, and did not provide prevalence estimates of NSSI among sexual minority individuals. Also of note, studies of transgender individuals were not included, and thus no prior meta-analysis exists with this population. Although the more recent narrative review included transgender samples and a greater number of studies (k = 26), 10 of these studies did not distinguish NSSI from suicidal behavior and/or did not include a systematic assessment of NSSI, complicating interpretations of its findings. The studies included in this prior narrative review therefore still represented a minority of the existing empirical literature.
The current review provides a systematic quantitative synthesis of the existing empirical literature on NSSI in sexual and gender minority populations. In doing so, it aimed to provide (i) a substantial update to the aforementioned literature reviews; (ii) prevalence estimates of NSSI among sexual minority and gender minority individuals, respectively; (iii) direct comparisons of prevalence and risk for NSSI among sexual and gender minority individuals and heterosexual/cisgender peers; (iv) moderator analyses for the prevalence and risk for NSSI among sexual and gender minority individuals; and (v) an assessment of correlates of NSSI in sexual and gender minority groups, with particular focus on both LGBT-specific and non-specific risk and resilience correlates. Additionally, as cultural and societal attitudes towards LGBT individuals change over time, NSSI in sexual and gender minority groups may similarly change (Newcomb & Mustanski, 2010, 2011). For this reason, analyses will be conducted to evaluate whether prevalence of NSSI among LGBT individuals and the risk for NSSI in these individuals change as a function of the year each study was conducted or year of publication. Finally, given aforementioned considerations regarding the operationalization of sexual minority status, sensitivity analyses will be conducted whenever possible based on this consideration.
2. Method
2.1. Search strategy and eligibility criteria
A systematic search of the literature was conducted in PsycINFO, MEDLINE, and Embase to identify studies relevant to the current review published from inception to July 19, 2019. The following search string was applied: (suicid* OR parasuicid* OR self-harm OR NSSI OR self-injur* OR self-cut* OR self-mutilat*) AND (pansexual* OR transgender* OR transsexual* OR intersex OR gay OR homosexual* OR “men who have sex with men” OR lesbian* OR queer OR bisexual* OR GBL OR GBLT OR LGBTQI OR LGB OR LGBT OR LGBTQ OR “sexual orientation”“ OR “sexual minority” OR “sexual minorities”) NOT “laparoscopic gastric bypass.” Selection of search terms for LGBT and NSSI, respectively, was informed in part by a recent systematic review of LGBT terminology used in the empirical literature (Lee, Ylioja, & Lackey, 2016) and prior meta-analyses of the NSSI literature (Liu, Cheek, & Nestor, 2016; Liu, Scopelliti, Pittman, & Zamora, 2018; Liu, Trout, Hernandez, Cheek, & Gerlus, 2017). Search results were limited to: (i) English-language publications and (ii) peer-reviewed journals. This search was supplemented by a search of the references of the prior systematic reviews of NSSI among sexual and gender minority individuals (Batejan et al., 2015; Jackman et al., 2016), again limiting eligible studies to English-language publications in peer-reviewed journals. This approach yielded a total of 2,778 articles, of which, 1,980 were unique reports. In cases where the eligibility of an article could not be ruled out based on title and abstract, the full text was also examined. Each search result was independently reviewed for eligibility by two of the authors, with discrepancies independently resolved by a third author.
The study inclusion criteria were: (i) sexual and/or gender minority status was determined systematically; (ii) NSSI was assessed separately from other constructs (e.g., suicidal behavior); (iii) NSSI was assessed systematically; (iv) presented data on prevalence of NSSI among LGBT individuals, and/or provided sufficient quantitative data for meta-analysis on LGBT status or an aspect of LGBT experiences (e.g., age of coming out) in relation to any aspect of NSSI (e.g., NSSI occurrence, age of first onset of NSSI), and/or provides quantitative data on correlates of NSSI among LGBT individuals; and (v) in studies providing data on correlates of NSSI, these correlates were assessed systematically among LGBT individuals separate from heterosexual and/or cisgender individuals. Additionally, in the case of studies where more information on the measurement of the constructs of interest (e.g., NSSI) was needed to determine study eligibility, every effort was made to obtain further details in other publications describing the measure (e.g., other publications based on the same dataset) or by contacting the corresponding author of the study.
2.2. Data extraction
Data on eight study characteristics were extracted. These included four sample characteristics: (i) mean age of sample; (ii) sample age group (i.e., adolescent, adult); (iii) sample type (i.e., community, at-risk/mixed, and clinical); and (iv) percentage of female participants in the sample.1 Data for four study design characteristics were also extracted: (i) method of determining sexual minority status (i.e., attraction, behavior, self-identification, or no information provided); (ii) NSSI measure type (i.e., self-report versus interview); (iii) time-frame covered by NSSI assessment (e.g., past year); and (iv) year of data collection.
2.3. Data analysis
All analyses were conducted with Comprehensive Meta-Analysis Version 3.3.070 (Biostat, 2014). The standardized mean difference (SMD; Cohen’s d) was used as the primary index of effect size for analyses of: (i) sexual minority status and NSSI and (ii) risk/protective correlates in a sexual and/or gender minority sample and NSSI. Cohen’s d of .20 is interpreted as a small effect size, .50 as medium, and .80 as large (Kraemer et al., 2003). All pooled effects were calculated such that values greater than zero reflected a positive association between: (i) sexual and/or gender minority status and NSSI; and (ii) risk/resilience correlates in sexual and/or gender minority samples and NSSI.
For all analyses, random-effects models were generated in preference to fixed-effects models, to account for the high expected heterogeneity across studies resulting from differences in samples, measures, and design (Borenstein, Hedges, Higgins, & Rothstein, 2009). Random-effects models are more appropriate than fixed-effects models in cases where there is high heterogeneity, in that they account for this heterogeneity by including both sampling and study-level errors, with the pooled effect size representing the mean of a distribution of true effect sizes instead of a single true effect size. In contrast, fixed-effects models approximate only within-study variance, as it assumes that a single true effect size exists across all studies and any variance detected is due strictly to sampling error. Heterogeneity across the studies was evaluated using the I2 statistic. I2 indicates the percentage of the variance in an effect estimate that is due to heterogeneity across studies rather than sampling error (i.e., chance). Low heterogeneity is indicated by I2 values of around 25%, and moderate heterogeneity by I2 values of 50%. Substantial heterogeneity that is due to real differences in study samples and methodology is indicated by an I2 value of 75%, which suggests that the observed heterogeneity is more than would be expected with random error (Higgins, Thompson, Deeks, & Altman, 2003).
High heterogeneity indicates the need to conduct moderator analyses to account for potential sources of this heterogeneity. Each potential moderator was first assessed separately, with the effect size at each level of the moderator estimated in the case of categorical moderators. When significance was detected for multiple moderators, a multivariate meta-regression with a random-effects model and unrestricted maximum likelihood was conducted simultaneously evaluating all moderators found to be significant in univariate analyses.
The possibility of publication bias is a common concern in conducting meta-analyses. Studies with small effect sizes or non-significant findings are less likely to be published, and thus may be more likely to be excluded from meta-analyses, resulting in a potentially inflated estimate of the overall effect size. The following publication bias indices were calculated to assess for the presence of potential publication bias: Duval and Tweedie’s trim-and-fill analysis (Duval & Tweedie, 2000) and Egger’s regression intercept (Egger, Davey Smith, Schneider, & Minder, 1997). Duval and Tweedie’s trim-and-fill analysis produces an estimate of the number of missing studies based on asymmetry in a funnel plot of the standard error of each study in a meta-analysis (based on the study’s sample size) against the study’s effect size. This analysis also calculates an effect size estimate and confidence interval, adjusting for these missing studies. It is important to note that this method assumes homogeneity of effect sizes. Consequently, its results must be interpreted with a degree of caution in cases where significant heterogeneity exists. Egger’s regression intercept also provides an estimate of potential publication bias using a linear regression approach weighing study effect sizes relative to their standard error.
3. Results
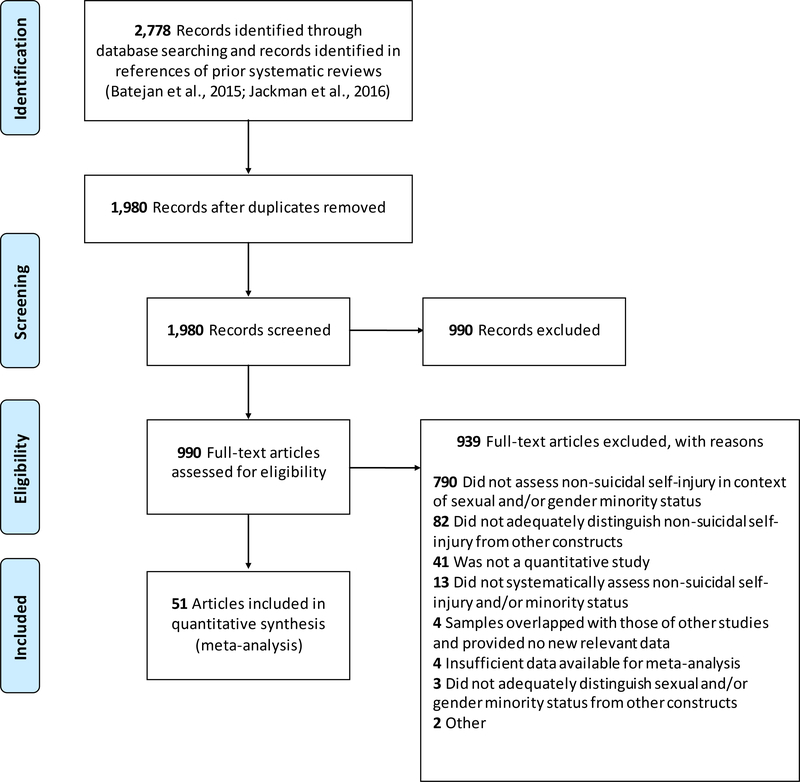
Out of the 1,980 unique records identified, we excluded 990 based on their titles and abstracts. Following this initial screen, we excluded an additional 935 articles based on full-text review, resulting in 55 articles that satisfied the eligibility criteria. For articles that did not provide sufficient data for meta-analysis, every effort was made to contact the study authors (i.e., first author, corresponding author, and senior author) to obtain the necessary data. This resulted in additional data required for meta-analysis being obtained from the authors of four of these studies (DeCamp & Bakken, 2016; Gollust, Eisenberg, & Golberstein, 2008; Serras, Saules, Cranford, & Eisenberg, 2010; Smith & Perrin, 2017). For studies meeting eligibility criteria but featuring overlapping samples, determination of which study to include in the meta-analysis was based, in descending order, on: (i) inclusion of sufficient reported data for meta-analysis; and (ii) largest sample size for the relevant analysis. In cases where two studies used overlapping samples but examined different associations (e.g., NSSI with different correlates), however, both studies were retained for the relevant analyses. Whenever it remained unclear after full-text inspection whether two studies reported on overlapping samples, the study authors were contacted to seek clarity on this issue. Fifteen articles featured overlapping samples and four were excluded at this stage, resulting in a final set of 51 articles, featuring 54 studies, included in the current review (see Figure 1 and Table 1).
Figure 1.
PRISMA flow chart of literature search
Table 1.
Study characteristics
| Study Author(s) (year) | Na | % Femalea | Mean Agea | Sample Type | Sexual Orientation and Gender Identity |
Non-Suicidal Self-Injury |
|||
|---|---|---|---|---|---|---|---|---|---|
| Minority Group(s) | Index/Indices | Measure(s) | Format | Time Frame(s) | |||||
| Arcelus et al. (2016)1 | 268 | 45.15 | 19.90 | Clinical | T | Self-Identification | SIQ | Q | Year, Lifetime |
| Balsam et al. (2005) | 1,254 | 64.19 | 36.54 | Community | LGB | Self-Identification | SSM | Q | Lifetime |
| Beard et al. (2017) | 441 | 58.08 | 34.42 | Clinical | LGB | Self-Identification | ISAS | Q | Lifetime |
| Benau et al. (2017) | 1,352 | 66.80 | 21.10 | Community | LGB | Self-Identification | SSM | Q | Lifetime |
| Bergero-Miguel et al. (2016) | 210 | 52.00 | 27.86 | Clinical | T | Self-Identification | SSM | Q | Lifetime |
| Brennan et al. (2017) | 83 | — | — | Community | T | Self-Identification | SSM | Q | Lifetime |
| Chakraborty et al. (2011) | 7,461 | — | — | Community | LGB | Behavior, Self-Identification | SSM | I | Lifetime |
| Claes, Bouman, et al. (2015)1 | 155 | 33.55 | 34.52 | Clinical | T | Self-Identification | SIQ | Q | Lifetime |
| Claes, Luyckx, et al. (2015) | 99 | 100 | 27.75 | Clinical | LGB | Self-Identification | SIQ | Q | Lifetime |
| Clark et al. (2014) | 7,805 | — | — | Community | T | Self-Identification | SSM | Q | Year |
| Davey et al. (2016)1 | 194 | 38.14 | 36.67 | Mixed | T | Self-Identification | SIQ | Q | Lifetime |
| Davis et al. (2017) | 244 | 67.21 | 22.40 | Community | LGB | No Information | DSHI | Q | Lifetime |
| Decamp & Bakken (2016) | 7,326 | 49.56 | — | Community | LGB | Self-Identification | SSM | Q | Year |
| Deliberto & Nock (2008) | 73 | 77.66 | 17.14 | Mixed | LGB | Self-Identification | SITBI | I | Lifetime |
| dickey et al. (2015) | 773 | 52.00 | 40.40 | Community | T | Self-Identification | ISAS | Q | Lifetime |
| Eisenberg et al. (2017)2 | 80,929 | — | — | Community | T | Self-Identification | SSM | Q | Year |
| Fox et al. (2018) Study 1 | 90 | 78.35 | 22.53 | Clinical | LGB | Self-Identification | SITBI | I | Lifetime |
| Fox et al. (2018) Study 2 | 153 | 58.89 | 24.50 | Clinical | LGB | Self-Identification | SITBI-Self Report | Q | Year |
| Fox et al. (2018) Study 3 | 174 | 86.89 | 25.16 | Clinical | LGB | Self-Identification | SITBI-Self Report | Q | Lifetime |
| Fox et al. (2018) Study 4 | 977 | 66.44 | 26.54 | Clinical | LGB | Self-Identification | SITBI-Self Report | Q | Lifetime |
| Fraser et al. (2018) | 1,791 | 56.67 | 15.16 | Community | LGB | Self-Identification | DSHI | Q | Lifetime |
| Gandhi et al. (2015) | 536 | 62.50 | 16.13 | Community | LGB | N/A | SIQ-Treatment Related | Q | Lifetime |
| Goldbach et al. (2017) | 346 | 56.36 | — | Community | LGB | No Information | SSM | Q | Year |
| Gollust et al. (2008) | 2,843 | 48.00 | — | Community | LGB | Self-Identification | SSM | Q | Month |
| Hickson et al. (2017) | 5,751 | 0 | — | Community | GB | Attraction, Behavior, Self-Identification | SSM | Q | Year |
| House et al. (2011) | 1,126 | 41.47 | 37.60 | Community | LGBT | Self-Identification | SSM | Q | Lifetime |
| Irish et al. (2019) | 2,222 | — | — | Community | LGB | Self-Identification | SSM | Q | Lifetime |
| Jackman et al. (2018) | 332 | 49.70 | 34.56 | Community | T | Self-Identification | SITBI | I | Year, Lifetime |
| Katz-Wise et al. (2017) | 452 | — | — | Community | T | Self-Identification | SSM | Q | Lifetime |
| Katz-Wise et al. (2018) | 33 | 60.61 | 15.18 | Community | T | Self-Identification | SSM | Q | Lifetime |
| Kidd et al. (2012) | 889 | 100 | 16.20 | Community | LB | Self-Identification | SSM | Q | Year |
| Lefevor et al. (2019) | 3,568 | — | 22.08 | Clinical | T | Self-Identification | SSM | Q | Lifetime |
| Liu (2019)3 | 21,213 | — | — | Community | LGB | Behavior, Self-Identification | SSM | Q | Year |
| Macrynikola et al. (2018) | 1,712 | 81.00 | 22.76 | Community | LGB | No Information | SSM | Q | Year, Lifetime |
| McDowell et al. (2019) | 150 | 100 | 27.50 | Community | T | Self-Identification | SIQ | Q | Year |
| Monto et al. (2018)3 | 48,485 | — | — | Community | LGB | Self-Identification | SSM | Q | Year |
| Muehlenkamp et al. (2015) | 137 | 74.00 | 19.86 | Community | LGBT | Self-Identification | ISAS | Q | Lifetime |
| Ray-Sannerud et al. (2015) | 345 | 28.70 | — | Community | LGB | Behavior | SITBI-Self Report | Q | Lifetime |
| Serras et al. (2010) | 5,530 | 61.84 | — | Community | LGB | Self-Identification | SSM | Q | Year |
| Silva et al. (2015) | 140 | 71.40 | 19.59 | Community | LGB | Self-Identification | SITBI-Self Report | Q | Lifetime |
| Smith & Perrin (2017) | 239 | 62.76 | 31.47 | Community | LGB | Self-Identification | SSM | Q | Year, Lifetime |
| Sornberger et al. (2013) | 414 | 61.62 | 19.52 | Community | LGB | Self-Identification | HIDS | Q | Lifetime |
| Staples et al. (2018) | 237 | 64.80 | 28.00 | Community | T | Self-Identification | DSHI | Q | Lifetime |
| Swannell et al. (2016) | 9,471 | 50.29 | 52.10 | Community | LGB | Self-Identification | DSHI, FASI, SHBQ | Q | Year |
| Taliaferro & Muehlenkamp (2017) | 77,758 | 49.80 | — | Community | LGB | Self-Identification | SSM | Q | Year |
| Taliaferro et al. (2019)2 | 1,340 | 65.60 | — | Community | T | Self-Identification | SSM | Q | Year |
| Taylor et al. (in press) | 709 | 75.20 | 23.05 | Community | LGB | Self-Identification | SITBI-Self Report | Q | Lifetime |
| Thorne et al. (2019) | 388 | 85.31 | 20.16 | Clinical | T | Self-Identification | SIQ | Q | Lifetime |
| Veale, Peter, et al. (2017)4 | 533 | — | — | Community | T | Self-Identification | SSM | Q | Year |
| Veale, Watson, et al. (2017)4 | 30,192 | — | — | Community | T | Self-Identification | SSM | Q | Year |
| Whitlock & Knox (2007) | 2,875 | 56.51 | — | Community | LGB | Self-Identification | NSSI-AT | Q | Lifetime |
| Whitlock et al. (2011) | 11,363 | 57.60 | — | Community | LGB | Self-Identification | NSSI-AT | Q | Lifetime |
| Wilcox et al. (2012) | 1,081 | 53.84 | — | Community | LGB | Self-Identification | NSSI-AT | Q | Lifetime |
| Zaki et al. (2017) | 411 | 100 | 16.91 | At-risk | LB | Self-Identification | DSHI | Q | Lifetime |
Note: DSHI = Deliberate Self-Harm Inventory; FASI = Functional Assessment of Self-Injury; HIDS = How I Deal With Stress Questionnaire; ISAS = Inventory of Statements About Self-Injury; NSSI-AT = Non-Suicidal Self-Injury Assessment Tool; SHBQ = Self-Harm Behaviour Questionnaire; SIQ = Self-Injury Questionnaire; SITBI = Self-Injurious Thoughts and Behaviors Inventory; SSM = study-specific measure
B = bisexual; G = gay; L = lesbian; T = transgender
I = Interview; Q = Questionnaire
Studies with identical superscripts were drawn from same or overlapping samples but presented unique data included in this review.
The sample size, mean age, and percentage female for participants included in relevant analyses, rather than of the entire study sample, are presented and were incorporated in moderator analyses whenever available. For ease of presentation, whenever the sample size, mean age, or percentage female varied across multiple relevant analyses within a study, data for the cumulative number of unique participants across these analyses are presented here, and the sample size used in each analysis was retained in the relevant meta-analysis for purposes of obtaining weighted effect sizes.
3.1. Prevalence of NSSI among sexual and gender minority individuals
Weighted lifetime and past-year prevalence rates were calculated for all sexual and gender minority groups combined (i.e., LGBT), sexual minority groups combined (i.e., LGB), bisexual individuals, and gender minority groups alone. For reference, weighted prevalence rates were also calculated for heterosexual and/or cisgender individuals. These data are presented in Table 2. Only two studies provided data on past-year prevalence among gay individuals alone (Hickson, Davey, Reid, Weatherburn, & Bourne, 2017; Swannell, Martin, & Page, 2016), one study for lifetime prevalence among gay individuals alone (Balsam, Beauchaine, Mickey, & Rothblum, 2005), as well as one study each for lifetime (Balsam et al., 2005) and past-year prevalence (Swannell et al., 2016) among lesbian individuals alone. Therefore, pooled prevalence rates were not calculated for gay or lesbian individuals alone, respectively. Lifetime and past-year prevalence rates were quite elevated among sexual and gender minority individuals, ranging from 29.68% for sexual minority individuals to 46.65% for gender minority individuals in the case of lifetime prevalence, and from 24.68% for sexual minority individuals to 46.61% for gender minority individuals in the case of past-year prevalence. In contrast, lifetime and past-year prevalence rates were 14.57% and 10.64%, respectively, among heterosexual and/or cisgender peers.
Table 2.
Prevalence rates for non-suicidal self-injury by sexual orientation and gender identity.
| Sample Type | k | N | Prevalence Estimates |
Heterogeneity Analyses |
Publication Bias Analyses |
||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | I2 | p | Egger’s regression test p | Trim-and-fill |
||||
| % | 95% CI | ||||||||
| Lifetime Prevalence | |||||||||
| LGBT | 40 | 11,587 | 36.53% | 30.94% – 42.51% | 97.01% | <.001 | — | — | — |
| LGB | 24 | 6,726 | 29.68% | 24.38% – 35.59% | 94.32% | <.001 | .75 | 29.68% | 24.38% – 35.59% |
| Bisexual | 7 | 895 | 41.47% | 36.45% – 46.66% | 41.54% | .11 | .22 | 41.47% | 36.45% – 46.66% |
| Transgender | 15 | 4,724 | 46.65% | 39.35% – 54.10% | 94.97% | <.001 | .18 | 46.65% | 39.35% – 54.10% |
| Heterosexual/Cisgender | 19 | 27,947 | 14.57% | 11.10% – 18.89% | 98.36% | <.001 | .62 | 14.57% | 11.10% – 18.89% |
| Past-Year Prevalence | |||||||||
| LGBT | 34 | 61,364 | 31.52% | 24.45% – 39.56% | 99.36% | <.001 | — | — | — |
| LGB | 22 | 57,774 | 24.68% | 18.65% – 31.91% | 99.19% | <.001 | .06 | 25.44% | 19.29% – 32.75% |
| Bisexual | 11 | 2,258 | 41.20% | 27.18% – 56.82% | 97.25% | <.001 | .11 | 36.53% | 24.60% – 50.38% |
| Transgender | 12 | 3,590 | 46.61% | 35.45% – 58.12% | 97.15% | <.001 | .44 | 46.61% | 35.46% – 58.12% |
| Heterosexual/Cisgender | 17 | 158,393 | 10.64% | 9.10% – 12.41% | 99.05% | <.001 | <.05 | 8.91% | 6.67% – 11.80% |
Note: CI = confidence interval; k = number of unique effects; N = total number of participants included in pooled analyses;
B = bisexual; G = gay; L = lesbian; T = transgender
There was a sufficient number of studies to conduct sensitivity analyses with sexual minority status based solely on self-identification in the case of lifetime and past-year NSSI among sexual minority individuals and past-year NSSI among bisexuals alone (see Supplemental Table 1). The NSSI prevalence rates in all cases were generally comparable to the corresponding rates in Table 2. In addition, sensitivity analysis was not possible for lifetime NSSI among bisexuals alone as indexed solely by self-identification, as there were too few studies for analysis. For this reason too, sensitivity analysis was not conducted for sexual minority status indexed solely by same-sex behavior or gender minority status.
Direct comparisons were also conducted between groups in lifetime and past-year prevalence of NSSI (see Table 3). Identical patterns emerged for lifetime and past-year prevalence rates. In particular, all sexual and gender minority groups had significantly higher prevalence rates than did heterosexual and/or cisgender individuals (p ≤ .001). Transgender and bisexual groups did not differ from each other in NSSI prevalence (pLifetime = .26; pPast Year = .58), but prevalence rates were higher among transgender individuals than all sexual minority groups combined (p < .001).
Table 3.
Between-groups comparisons of lifetime and past-year prevalence of non-suicidal self-injury.
| LGB | Bisexual | Transgender | Heterosexual/Cisgender | |
|---|---|---|---|---|
| LGB | — | N/A | Transgender; p <.001 | LGB; p <.001 |
| Bisexual | N/A | — | p = .26 | Bisexual; p <.001 |
| Transgender | Transgender; p = .001 | p = .58 | — | Transgender; p <.001 |
| Heterosexual/Cisgender | LGB; p <.001 | Bisexual; p <.001 | Transgender; p <.001 | — |
| Lifetime Prevalence | 29.68% | 41.47% | 46.65% | 14.57% |
| Past-Year Prevalence | 24.68% | 41.20% | 46.61% | 10.64% |
Note. Values above the diagonal reflect comparisons of lifetime-prevalence and values below the diagonal comparisons of past-year prevalence. Where significant differences in prevalence rates were detected, the group with the higher prevalence rate is presented next to the corresponding p value. Lifetime and past-year prevalence are also presented to facilitate comparisons between groups.
B = bisexual; G = gay; L = lesbian
N/A = not applicable
With the exception of lifetime prevalence of NSSI among bisexual individuals, heterogeneity was quite high across all prevalence analyses, and moderator analyses were therefore appropriate. Moderator analyses were conducted separately for lifetime prevalence of NSSI among sexual and gender minority individuals, respectively. Age as a continuous variable, percentage of natal female participants in each sample, sample type, and year of data collection were evaluated as potential moderators of lifetime prevalence of NSSI (see Table 4). NSSI measure type was excluded from moderator analyses because only one sexual minority study (Chakraborty, McManus, Brugha, Bebbington, & King, 2011) and one gender minority study (Jackman, Dolezal, Levin, Honig, & Bockting, 2018) used interview-based measures to assess lifetime prevalence of NSSI. For similar reasons, method of determining sexual minority status was not included in moderator analyses; only two eligible studies used same-sex behavior as an index (Chakraborty et al., 2011; Ray-Sannerud, Bryan, Perry, & Bryan, 2015) and no studies based sexual minority status on same-sex attraction. Finally, age as a categorical variable was also excluded from moderator analyses, as only one eligible study featured an adolescent-only sample for sexual minority (Fraser et al., 2018) and gender minority studies (Katz-Wise, Ehrensaft, Vetters, Forcier, & Austin, 2018), respectively.
Table 4.
Moderator analyses for lifetime prevalence of non-suicidal self-injury among sexual and gender minorities.
| Moderator | k | N | b | SE | p |
|---|---|---|---|---|---|
| LGB | |||||
| Age (Continuous) | 6 | 1,683 | −.20 | .04 | <.001 |
| Sex (% Female) | 10 | 1,968 | <.01 | <.01 | .01 |
| Sample Typea | — | — | — | — | — |
| Year of Study Data Collection | 12 | 5,366 | .07 | .05 | .15 |
| Transgender | |||||
| Age (Continuous) | 7 | 2,073 | −.03 | .03 | .36 |
| Sex (% Female) | 11 | 2,462 | .01 | .01 | <.01 |
| Sample Type | 15 | 4,724 | — | — | .69 |
| Year of Study Data Collection | 8 | 3,299 | .11 | .06 | .10 |
Note: k = number of unique effects; N = total number of participants included in pooled analyses
B = bisexual; G = gay; L = lesbian
All studies analyzed lifetime prevalence of non-suicidal self-injury in community samples, and thus moderator analysis was not conducted.
In moderator analyses for sexual minority samples, a negative association was found between age as a continuous variable and lifetime prevalence (b = −.20, p < .001), indicating that samples with lower mean age tended to have higher lifetime rates of NSSI. Sex was also a significant moderator; samples with more females generally had higher lifetime rates of NSSI (b < .01, p = .01). No association was found between year of study data collection and lifetime NSSI prevalence. A multivariate meta-regression analysis was not conducted, as doing so with age as a continuous variable and percentage of female participants would have resulted in only six unique effects included in the analysis. In moderator analyses for gender minority samples, only percentage of female participants was associated with lifetime NSSI prevalence, a positive relation indicating that samples with more female participants tended to have higher lifetime rates of NSSI (b = .01, p < .01). Age as a continuous variable, sample type, and year of study collection were not significant moderators of lifetime NSSI prevalence among gender minority individuals.
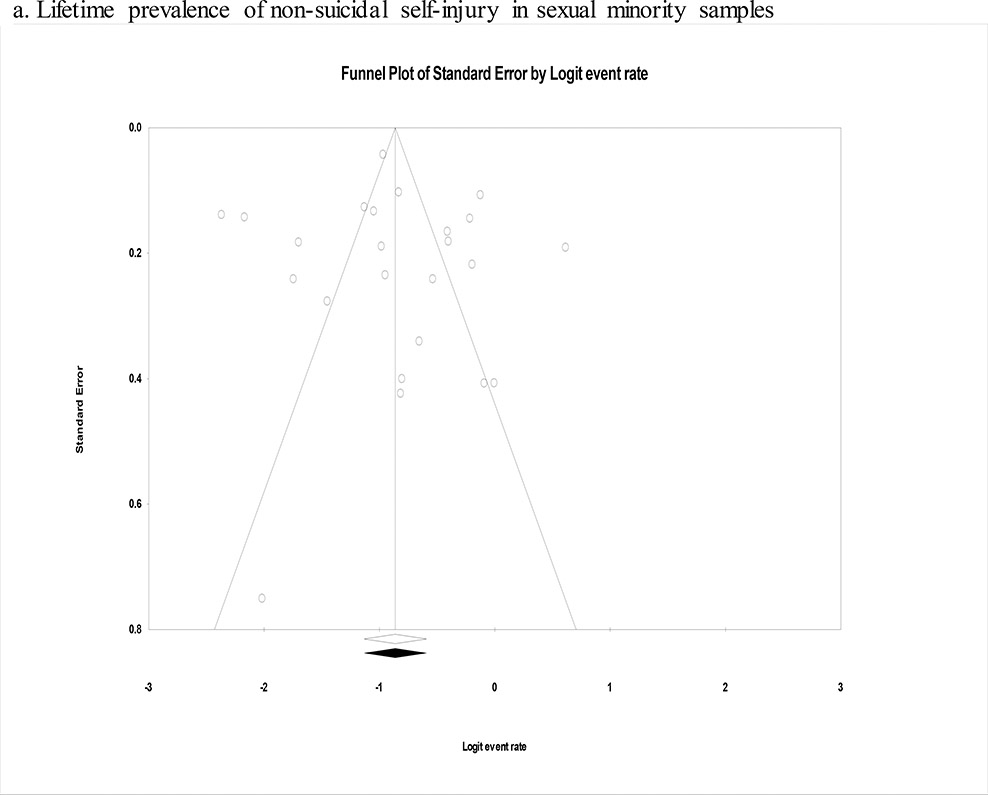
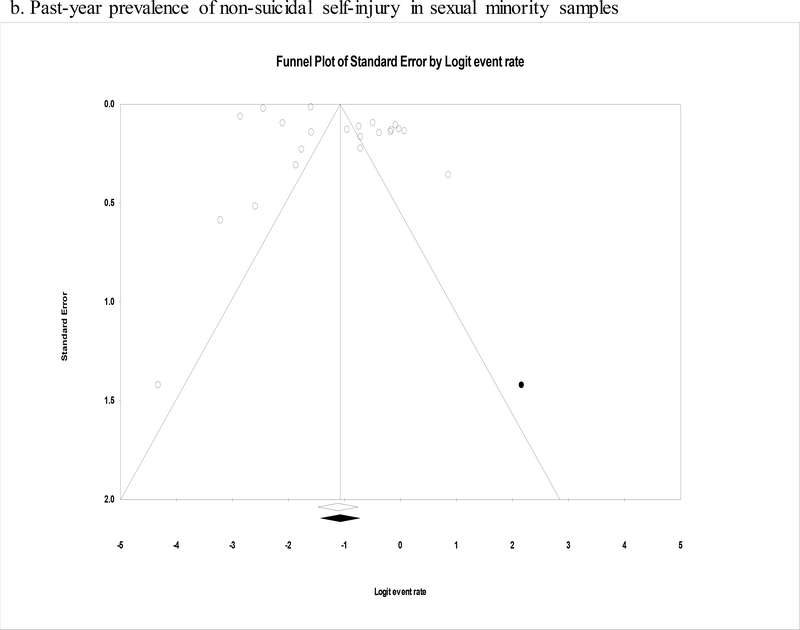
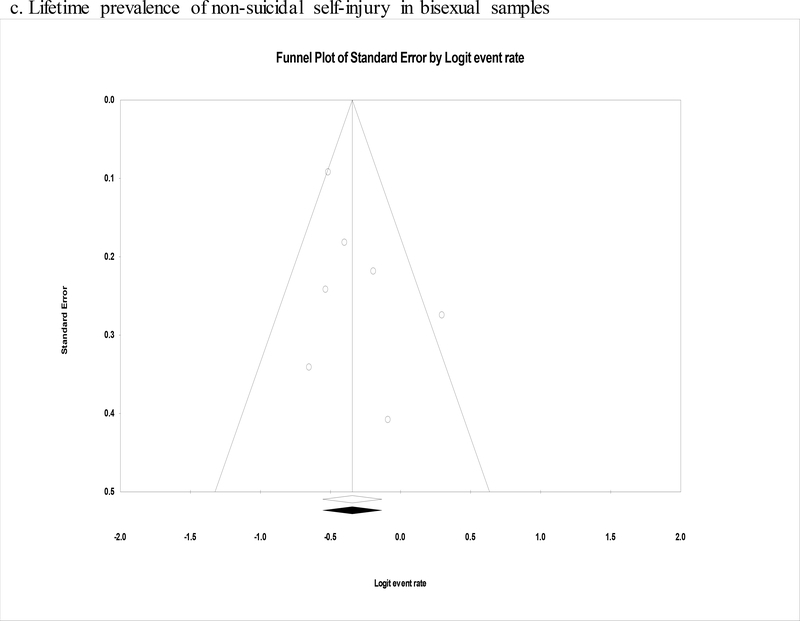
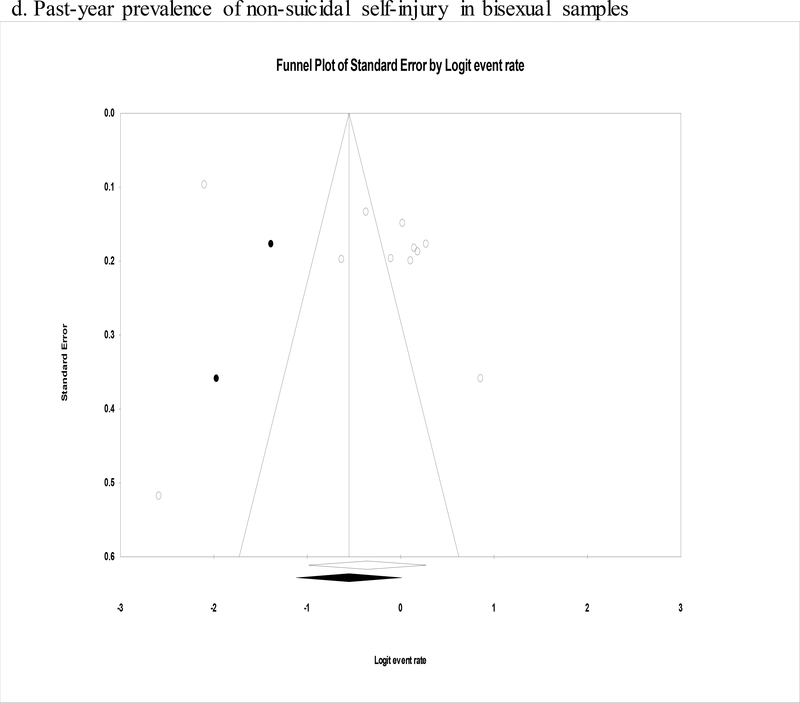
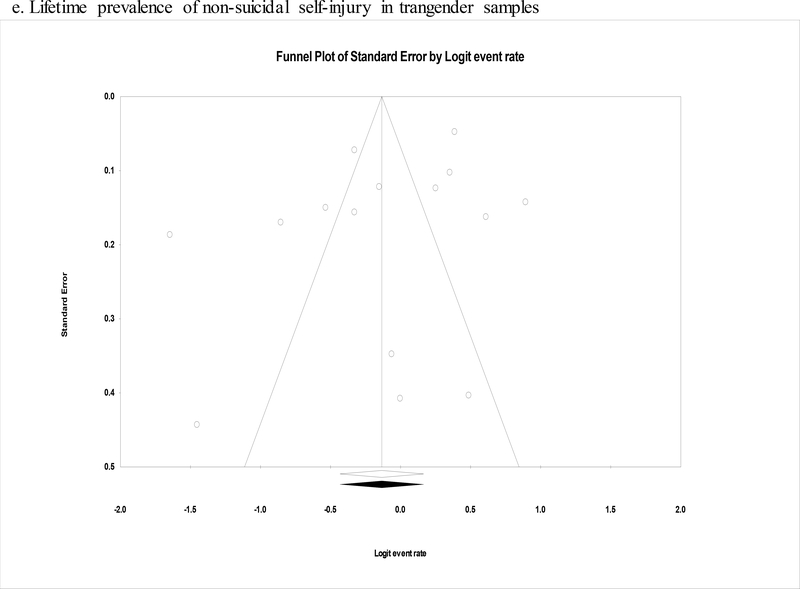
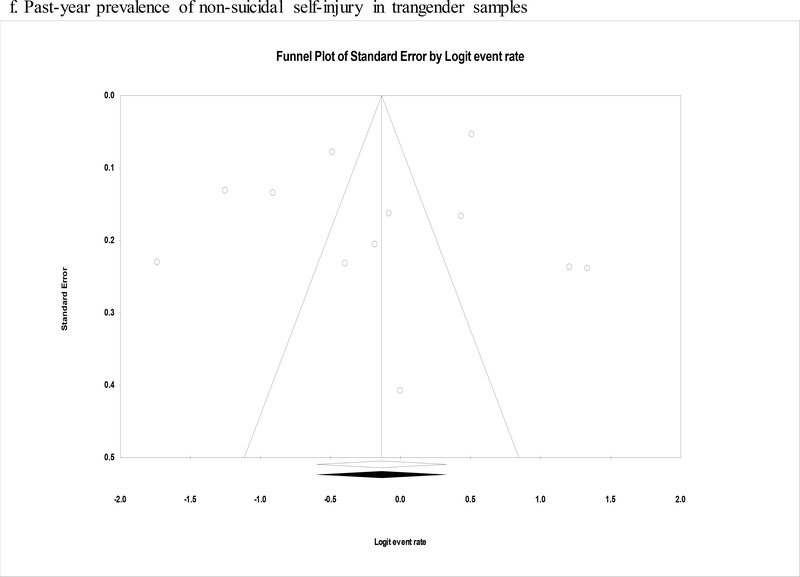
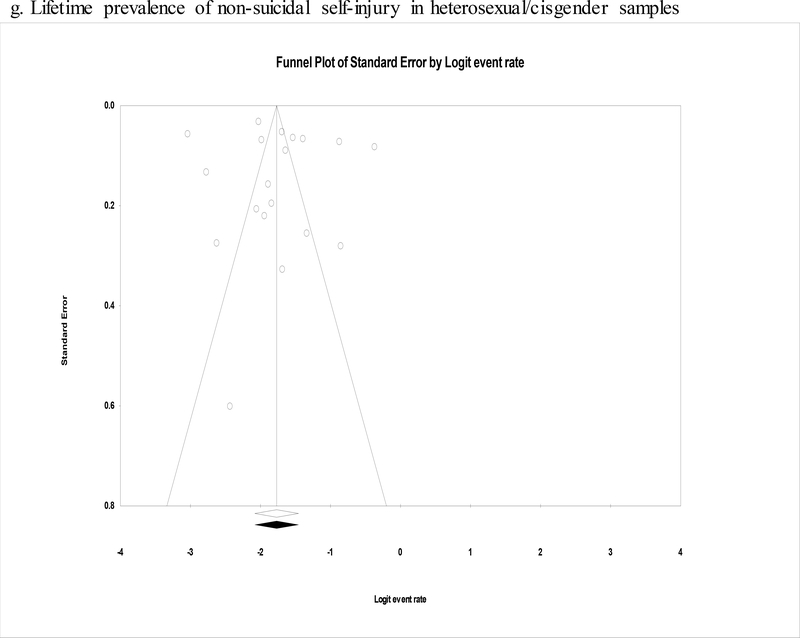
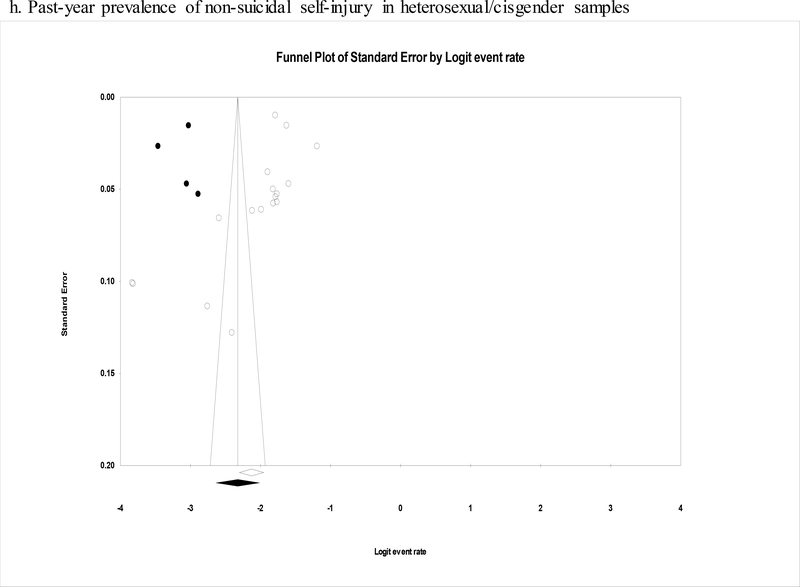
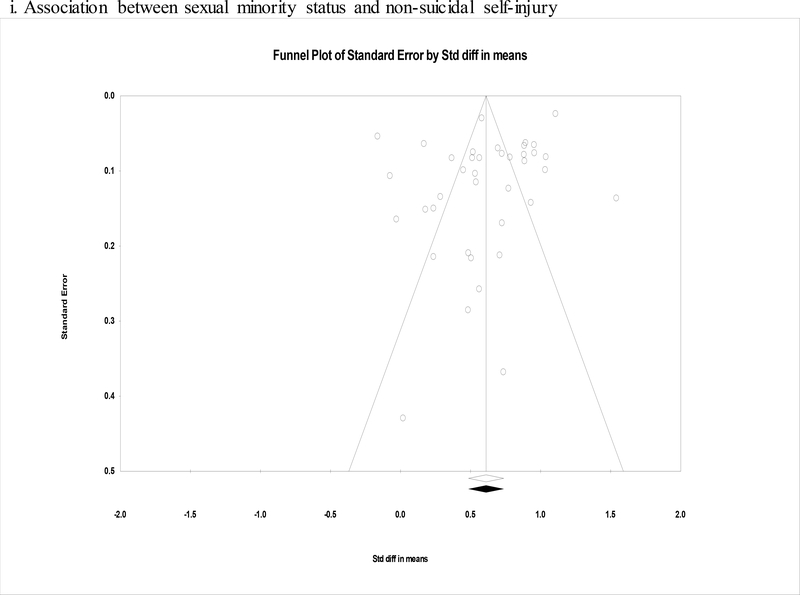
Analyses of publication bias were conducted for both lifetime and past-year NSSI for sexual minority, bisexual-only, and gender minority samples. Publication bias analyses were also conducted for the heterosexual and/or cisgender reference group. In general, there was modest evidence of publication bias across all analyses (See Table 2). With the exception of past-year prevalence of NSSI among heterosexual and/or cisgender individuals, Egger’s regression test yielded no evidence of publication bias. Trim-and-fill analyses did not produce changes in pooled prevalence estimates for lifetime NSSI across all groups. The adjusted pooled estimates yielded by trim-and-fill analyses for past-year NSSI across all groups were not substantially different from unadjusted estimates. Other than in the case of past-year prevalence among heterosexual and/or cisgender individuals, funnel plots were essentially symmetrical (see Figures 2a through 2h).
Figure 2.
Funnel plots for effect sizes in the meta-analyses. The vertical line indicates the weighted mean effect. Open circles indicate observed effects for actual studies, and closed circles indicate imputed effects for studies believed to be missing due to publication bias. The clear diamond reflects the unadjusted weighted mean effect size, whereas the black diamond reflects the weighted mean effect size after adjusting for publication bias.
3.2. Associations between sexual and gender minority status and NSSI
Pooled effects were calculated for the association between sexual and gender minority status and NSSI, with heterosexual and/or cisgender individuals serving as the reference group in all instances (see Table 5). The association between sexual minority status, when combined with gender minority status or assessed alone, and NSSI yielded medium-to-large effects (ds = .61 to .65). Large effects were found in the case of bisexual (d = .92, 95% CI .75 – 1.08) and transgender individuals (d = .91, 95% CI .72 – 1.11), respectively. Where possible, sensitivity analyses were conducted for sexual minority status based solely on self-identification and same-sex behavior (see Supplemental Table 2). In these analyses, pooled effects were largely unchanged regardless of whether restricted to samples basing sexual minority status on self-identification and same-sex behavior, respectively. In direct comparisons, the weighted effect for transgender individuals was significantly larger than that for all sexual minority groups combined (p = .01) but not bisexuals alone (p = .97).
Table 5.
Correlates of non-suicidal self-injury.
| Correlate | k | N | d | 95% CI | p |
|---|---|---|---|---|---|
| Sexual and Gender Minority Status | |||||
| LGBT | 45 | 282,043 | .65 | .54 – .76 | <.001 |
| LGB | 39 | 159,962 | .61 | .49 – .74 | <.001 |
| Bisexual | 20 | 127,490 | .92 | .75 – 1.08 | <.001 |
| Transgender | 6 | 122,081 | .91 | .72 – 1.11 | <.001 |
| Sociodemographic Characteristics | |||||
| Age (Continuous) | 8 | 8,604 | −.52 | −.80 – −.24 | <.001 |
| Sex (Female) | 20 | 78,686 | .41 | .33 – .49 | <.001 |
| Race (White) | 6 | 8,264 | −.15 | −.24 – −.07 | <.001 |
| Educational attainment (Low) | 5 | 8,116 | .27 | .19 – .35 | <.001 |
| Financial status (Low) | 7 | 9,556 | .37 | .04 – .70 | .03 |
| Clinical Correlates | |||||
| Overall Psychopathology | 7 | 2,902 | .55 | .46 – .65 | <.001 |
| Depression | 6 | 2,692 | .49 | .34 – .64 | <.001 |
| Anxiety | 6 | 1,562 | .52 | .41 – .63 | <.001 |
| General Risk Correlates | |||||
| Overall | 7 | 3,681 | .47 | .29 – .65 | <.001 |
| Aggression and Hostility | 3 | 1,495 | .59 | .02 – 1.16 | .04 |
| LGBT-Specific Risk Correlates | |||||
| Overall | 14 | 5,784 | .32 | .22 – .43 | <.001 |
| Intrapersonal (Distress over LGBT Identity) | 6 | 3,322 | .35 | .20 – .50 | <.001 |
| Interpersonal (LGBT Stigma, Discrimination, and Victimization) | 12 | 3,457 | .32 | .21 – .43 | <.001 |
| Resilience Correlates | |||||
| Overall | 7 | 2,397 | −.15 | −.23 – −.06 | <.01 |
| Intrapersonal | 4 | 644 | −.30 | −.49 – −.12 | <.01 |
| Self-Esteem | 3 | 403 | −.32 | −.61 – −.03 | .03 |
| Transgender Social Support: Overall | 5 | 2,075 | −.03 | −.09 – .03 | .35 |
| Transgender Social Support: Family | 5 | 2,282 | −.24 | −.41 – −.06 | .01 |
| Transgender Social Support: Friends | 5 | 2,123 | −.02 | −.19 – .16 | .84 |
| Transgender Community Connectedness | 3 | 558 | −.05 | −.15 – .06 | .38 |
Note: CI = confidence interval; k = number of unique effects; N = total number of participants included in pooled analyses
B = bisexual; G = gay; L = lesbian; T = transgender
Weighted effects were also calculated for sexual minority status in relation to lifetime onset of NSSI, self-reported desire no longer to engage in NSSI, and self-perceived likelihood of future engagement in NSSI, respectively (see Supplemental Table 3). Sexual minority individuals who engaged in NSSI were more likely to initiate this behavior at a younger age, and saw themselves as more likely to engage in NSSI again in the future than were heterosexual peers. No differences based on sexual minority status were found, however, for the desire to cease future engagement in NSSI.
Heterogeneity was assessed for the association between sexual minority status and NSSI and was found to be high (I2 = 95.67%, p < .001), indicating that moderator analysis was appropriate. Although a high degree of heterogeneity was also observed for the relation between gender minority status and NSSI (I2 = 89.43, p <.001), there were too few effects (k = 6) for meaningful moderator analyses. For the association between sexual minority status and NSSI, age as a categorical and continuous variable, respectively, percentage of natal female participants in each sample, sample type, NSSI measure type, and year of data collection were evaluated as candidate moderators (see Table 6). In univariate analyses, age as a categorical, but not continuous, was a significant moderator, with larger effects observed among adolescent samples (d = .93, 95% CI .84 – 1.01) than adult ones (d = .47, 95% CI .34 – .60). The strength of the association between sexual minority status and NSSI also changed as a function of the sample type, with larger effects found for community (d = .69, 95% CI .56 – .82) than clinical samples (d = .30, 95% CI .06 – .55). Larger effects were also observed for questionnaire-based measures of NSSI (d = .62, 95% CI .49 – .75) than interview-based ones (d = .37, 95% CI .22 – .52). Percentage of natal female participants and year of study data collection were not significant moderators. In a meta-regression analysis that included age as a categorical variable, sample type, and NSSI measure type as candidate moderators, only age remained a significant moderator (b = .40, p < .001), with the association between sexual minority status and NSSI being stronger among adolescents than adults. This multivariate model accounted for 58% of the variance in the effect sizes for sexual minority status in relation to NSSI.
Table 6.
Moderator analyses for the association between sexual minority status and non-suicidal self-injury.
| Moderator | k | N | Univariate Analyses |
Multivariate Meta-Regression Analysisb |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | d | 95% CI | p | b | SE | p | |||
| Age (Categorical) | 38 | 159,551 | <.001 | |||||||
| Adolescent | 13 | 108,602 | .93 | .84 – 1.01 | <.001 | .40 | .10 | <.001 | ||
| Adulta | 25 | 50,949 | .47 | .34 – .60 | <.001 | |||||
| Age (Continuous) | 18 | 10,922 | <.01 | .01 | .82 | |||||
| Sex (% Female) | 27 | 43,383 | <.01 | <.01 | .60 | |||||
| Sample Type | 37 | 159,478 | <.01 | |||||||
| Clinicala | 6 | 1,933 | .30 | .06 – .55 | <.01 | |||||
| Community | 31 | 157,545 | .69 | .56 – .82 | <.001 | .21 | .13 | .12 | ||
| NSSI Measure | 39 | 159,962 | .01 | |||||||
| Interviewa | 3 | 7,623 | .37 | .22 – .52 | <.001 | |||||
| Questionnaire | 36 | 152,339 | .62 | .49 – .75 | <.001 | .13 | .21 | .53 | ||
| Year of Study Data Collection | 26 | 155,225 | <.01 | .02 | .64 | |||||
Note: CI = confidence interval; k = number of unique effects; N = total number of participants included in pooled analyses
NSSI = non-suicidal self-injury
The category with the smallest effect size in univariate moderator analysis served as the reference group in the corresponding meta-regression analysis.
R2 = .58
In a set of analyses, no evidence of publication bias was found for sexual minority status in relation to NSSI. Specifically, Egger’s regression test did not indicate the existence of significant publication bias (intercept = −2.57, p = .06), the pooled effect size remained unchanged after trim-and-fill analysis, and the funnel plot was symmetrical (see Figure 2i).
3.3. Correlates of NSSI among sexual and gender minority individuals
Weighted effects were calculated for correlates of NSSI among sexual and gender minority samples (see Table 5). Sociodemographic correlates of NSSI had pooled effect sizes ranging from small-to-medium to medium. Female sex, racial minority status, and indices of low socioeconomic status (i.e., education and financial health) were positively associated with NSSI (ds = .15 to .41), whereas age was negatively correlated with this outcome (d = −.52, 95% CI −.80 – −.24), meaning that NSSI was more prevalent among younger LGBT individuals than older ones.
Across clinical correlates, including overall psychopathology, depression, and anxiety, pooled effects were consistently in the medium range (ds = .49 to .55). For general risk correlates, overall risk yielded a medium pooled effect size (d = .47, 95% CI .29 – .65) whereas aggression and hostility were found to have a medium-to-large pooled effect size (d = .59, 95% CI .02 – 1.16). LGBT-specific risk correlates, both intrapersonal and interpersonal ones, consistently produced small-to-medium pooled effects (ds = .32 to .35). Finally, mixed results were observed for resilience correlates of NSSI in sexual and gender minority samples. Intrapersonal resilience correlates yielded small-to-medium negative associations with NSSI (ds = −.30 to −.32). Contrastingly, among interpersonal resilience correlates, only family social support yielded a significant negative association with NSSI (d = −.24, 95% CI −.41 – −.06), although it should be noted that analyses of interpersonal resilience correlates were limited to transgender samples and thus do not characterize interpersonal resilience among sexual minority individuals.
4. Discussion
The current effort provides a comprehensive review of the empirical literature on the nature of the relation between LGBT status and NSSI. That is, it provided estimates of the prevalence of NSSI among sexual and gender minority individuals, as well as comparisons in these pooled estimates of NSSI prevalence between minority groups and heterosexual and/or cisgender peers. It also quantified the strength of the association between sexual and/or gender minority status and NSSI, as well as whether the size of the association differed between different sexual and gender minority groups. These findings, along with prevalence estimates, are critical for accurately evaluating the scale of this clinical concern in these at-risk populations as well as the magnitude of disparities relative to heterosexual and/or cisgender counterparts. Finally, the current effort also provided a systematic meta-analytic review of correlates of NSSI among sexual and gender minority individuals so as to characterize risk and resilience for NSSI in these populations. Such data are of value for their potential to aid in identifying which individuals within these populations are at particular risk for NSSI as well as correlates that may serve as meaningful targets for future investigation in the prospective prediction of NSSI. Moreover, insofar as these correlates are modifiable and temporally predictive of NSSI, they may ultimately lead to advances in the development of intervention strategies with these at-risk populations.
Prevalence analyses yielded consistently and markedly elevated rates of NSSI among all sexual and gender minority groups, ranging in the case of lifetime estimates from 30% in sexual samples combined to 47% in gender minority samples. These pooled estimates were two to three times that for heterosexual and/or cisgender individuals (15%), and are thus indicative of pronounced disparities in prevalence of NSSI. The lifetime prevalence rate for this reference group, heterosexual and/or cisgender individuals, is consistent with those in a prior meta-analysis of NSSI prevalence in general, non-clinical samples, which found lifetime estimates ranging from 13.4% among young adults to 17.2% among adolescents (Swannell, Martin, Page, Hasking, & St John, 2014), an age span that includes the mean sample age of most of the studies in the current review. It is also important to note that the high lifetime rates of NSSI among sexual and gender minority individuals in the current meta-analysis did not appear to be inflated by the inclusion of clinical samples in the pooled estimates. Indeed, it was not possible to evaluate sample type as a moderator of lifetime prevalence of NSSI among sexual minority indiviudals because only community samples were included in estimates of NSSI prevalence. Additionally, in the case of gender minority samples, moderator analyses indicated that prevalence estimates did not differ between clinical and community samples. Congruent with these prevalence findings, pooled correlational analyses of the strength of the association between sexual and gender minority status and NSSI yielded medium-to-large and large effects. These findings on prevalence and the relation between minority status and NSSI generally held true, regardless of how sexual minority status was operationalized (e.g., based on self-identification or same-sex behavior).
In direct comparisons across groups, results for prevalence and correlational analyses were essentially identical. Specifically, in both sets of analyses, bisexual and transgender individuals were consistently the groups most likely to engage in NSSI and did not differ from each other in this regard. Sexual minority individuals were more likely than heterosexual peers in these analyses to engage in NSSI, but were also significantly less likely to do so than transgender peers. The findings that bisexual and transgender individuals appear to be at highest risk for NSSI are particularly notable. There may be several potential explanations for these findings. Specifically, bisexual individuals may feel stigmatized by heterosexual, gay, and lesbian peers (Israel & Mohr, 2004), and report lower perceived social support than to lesbian and gay counterparts (Balsam & Mohr, 2007). Bisexual individuals are also less likely to disclose their sexual orientation than are lesbian and gay peers (Balsam & Mohr, 2007; Gates, 2010). Of direct relevance to the current findings regarding lower educational attainment and racial minority status being associated with greater risk for NSSI, bisexual individuals are less likely to complete high school and more likely to be members of racial minority groups than are lesbian and gay peers (Gates, 2010). Finally, bisexual individuals appear more likely than lesbian and gay counterparts to have several of the psychiatric correlates strongly associated in the current review to be associated with NSSI (e.g., depression and anxiety; Jorm, Korten, Rodgers, Jacomb, & Christensen, 2002). When taken together, these findings are suggestive of strategies for identifying at-risk individuals (e.g., bisexual individuals who are members of a racial minority group) as well as potential avenues worth evaluating to decrease risk in bisexual populations (e.g., increasing general social support as well as connectedness and acceptance in LGBT communities).
With regards to transgender individuals, the existing literature is considerably more modest. The greater prevalence of NSSI in transgender populations may in part be due to stigma related to the DSM diagnosis of gender dysphoria (previously gender identity disorder) leading to transgender individuals less likely to seek mental health care (Drescher, 2010). There is a need for research directly assessing differences between transgender and sexual minority peers with regards to candidate risk factors (e.g., stigma and discrimination) related to self-injurious behaviors (Haas et al., 2011).
Compounding these issues, at least in the case of bisexual populations, is the possibility that common psychotherapeutic interventions (e.g., cognitive behavior therapy and dialectic behavior therapy) may be less effective for addressing thoughts of NSSI among members of this population than other sexual minority and heterosexual peers (Beard et al., 2017). In the context of this possibility, the current findings underscore the need to develop new therapies or tailor existing cognitive behavioral interventions to address the specific needs of bisexual and transgender individuals. Assessment of identity-specific risk correlates within the context of treatment and development of treatments addressing minority stress may be crucial to this end. Indeed, various LGBT affirmative treatments that explicitly include content related to internalized stigma and minority stress factors have been developed for this purpose (Craig & Austin, 2016; Pachankis, Hatzenbuehler, Rendina, Safren, & Parsons, 2015). The results of the current study underscore the importance of rigorous testing among bisexual and transgender individuals of such interventions in comparison to existing treatments developed to address NSSI behaviors.
How lesbian and gay individuals fair with regards to NSSI could not be precisely determined, as there were only two studies in the current review providing prevalence data for the former (lifetime in Balsam et al., 2005; past-year in Swannell et al., 2016) and three studies for the latter (lifetime in Balsam et al., 2005; past-year in Hickson et al., 2017; Swannell et al., 2016). With the exception of the analysis of sex as a moderator of the association between LGB status and NSSI, however, all analyses involving sex as a moderator or correlate indicated a significant positive association for female sex with NSSI. These findings are consistent with the broader NSSI literature, in which females are generally at greater risk for this clinical outcome (Bresin & Schoenleber, 2015). Taken together, these findings therefore suggest that lesbians may be more likely to engage in NSSI than are gay men, who it could then be assumed would also be at significantly lower risk for NSSI than bisexual and transgender individuals based on the aforementioned differences between sexual minority groups combined and transgender individuals. Direct evaluation is required fully to assess these possibilities, however, and is important for determining relative allocation of resources for assessing risk in sexual and gender minority populations.
Correlations analyses may at least in part provide an account of these elevations in NSSI in LGBT populations. First, in line with sexual and gender minority stress models (Meyer, 2003; Testa et al., 2016), the current review yielded evidence consistent the view that experiences specific to being a member of these minority groups may confer unique risk to negative mental health outcomes such as NSSI. In particular, intrapersonal (e.g., internalized homophobia) and interpersonal experiences (e.g., stigma and discrimination) both had significant and sizable effects in relation to NSSI. In addition to these unique experiences, however, traditional correlates of risk that have been identified in non-minority populations (e.g., psychopathology and aggression) were also pertinent to sexual and gender minority groups, with medium to large effects in all cases. What is particularly notable about these general risk correlates is that several of them have, themselves, also been found in prior studies to be more common among sexual and gender minority individuals relative to heterosexual and cisgender peers (Becerra-Culqui et al., 2018; Liu, Stevens, Wong, Yasui, & Chen, 2019; Lucassen, Stasiak, Samra, Frampton, & Merry, 2017; Ross et al., 2018). LGBT individuals may therefore be potentially “twice hit” in terms of risk for NSSI, having vulnerabilities specific to their identity as well as experiencing more general vulnerabilities at higher levels than is found in the general population. As such, specifically addressing the needs of this vulnerable population would enhance existing treatments for reduction of NSSI such as cognitive behavior therapy and dialectical behavior therapy. Future research is necessary to identify evidence-based, cognitive-behaviorally informed processes for targeting identity-specific cognitive vulnerabilities (e.g., internalized homophobia), affective vulnerabilities (e.g., LGBT related distress), and environmental stressors (e.g., stigma). As it currently stands, no specific assessment of or intervention on sexual- or gender-minority related correlates of risk is conducted as a part of well-established treatment protocols.
The current evidence base for resilience correlates for NSSI was decidedly more modest, with strongest support in terms of effect size appearing for self-esteem, albeit based on just three effects. Additionally, all existing studies of social support were conducted with transgender samples, with only a small-to-medium pooled effect detected in the case of family support, and thus the relevance of this correlate to NSSI in sexual minority populations is currently unknown. Greater focus on this currently underdeveloped area of research is particularly critical for the development of intervention aimed at reducing risk in these vulnerable populations. In particular, just as LGBT-specific and general risk factors have been empirically evaluated and appear both to be relevant to the higher prevalence of NSSI in sexual and gender minority populations, future studies should identity and evaluate whether (i) potential general resilience factors (e.g., general social support) are less common among LGBT individuals, and (ii) both general and LGBT-specific resilience factors (e.g., LGBT community connectedness) both prospective predict lower rates of NSSI among LGBT populations.
Concerning the question of whether the relation between LGBT status and NSSI has changed over time, analyses of the year of study data collection as a moderator of NSSI prevalence in sexual and gender minority samples, respectively, suggest that rates of this clinical phenomenon have not experience a decline within these populations. In the case of sexual minority individuals, these findings are in line with those of a recent study of temporal trends, in which sexual minority youth had consistently heightened and unchanging rates of NSSI relative to heterosexual peers over a 13-year period (Liu, 2019). In addition to these findings, year of study data collection did not moderate the strength of the association between sexual minority status and NSSI, suggesting that disparities in this outcome have not improved over time. Collectively, these findings are concerning and striking, given that the persistently elevated rates of NSSI in sexual and gender minority populations allow for greater opportunity for improvement in this clinical outcome (e.g., natural regression) which does not appear to have occurred.
Also of concern was the pattern of findings relating to age in moderator analyses and as a correlate of NSSI. More specifically, younger age was associated with greater prevalence of NSSI in sexual minority individuals. Consistent with this finding, in analyses of correlates of NSSI, age was again negatively associated with this behavior among sexual and gender minority individuals. By itself, these findings are perhaps not all that unexpected, given the considerable body of literature demonstrating that NSSI is more common among adolescents than adults in the general population (Nock, 2010; Plener, Schumacher, Munz, & Groschwitz, 2015; Swannell et al., 2014). What makes these findings particularly concerning, however, is that age, at least when stratified by adolescent and adult samples, also significantly moderated the strength of the association between sexual minority status and NSSI, with this association being stronger among adolescents than adults, the large effect size for the former (d = .93) being essentially double that of the latter (d = .47).2 This age difference among sexual minority individuals appears to be robust, being the one moderator that remained significant in multivariate meta-regression analysis. That is, these findings indicate that even with NSSI already particularly prevalent among youth in general, the disparity in NSSI between sexual minority youth and their heterosexual counterparts is still greater than that between sexual minority and heterosexual adults. When considered together, these findings highlight LGB youth as an especially at-risk group among sexual minority populations. That many adolescents who engage in NSSI cease to do so by adulthood (Whitlock, Eckenrode, & Silverman, 2006) does not make this pattern of findings any less consequential, as even a single instance of NSSI may be linked with greater risk for negative mental health outcomes later in life (Whitlock, 2010; Whitlock et al., 2006).
There are several limitations worth mentioning. First, only two studies included in the current review employed a longitudinal design (Irish et al., 2019; Wilcox et al., 2012). In both of these studies, however, the analyses relevant to sexual minority status were nonetheless cross-sectional in nature (i.e., the association between sexual minority status and lifetime NSSI). Studies reporting longitudinal findings of the association between LGBT status and NSSI are necessary for characterizing the course of this behavior over time (e.g., persistence and chronicity). Such studies would aid in the determination, for example, of whether, in addition to being more prevalent, NSSI may also follow a more severe trajectory in these populations than among heterosexual and/or cisgender peers. Furthermore, studies of currently identified correlates in relation to prospectively occurring NSSI in sexual and gender minority groups may refine our understanding of the nature of their association with NSSI inasmuch as they would allow for disambiguating concomitants of NSSI from its risk factors (Kazdin, Kraemer, Kessler, Kupfer, & Offord, 1997; Kraemer et al., 1997). The translational value of this research lies in the potential for identified risk factors with large effects to inform our ability to identify which individuals in sexual and gender minority populations are at particular risk and how to intervene with these individuals insofar as stable risk factors may be relevant to risk stratification and state-sensitive or malleable risk factors be candidates for targeted intervention. Finally, a related need is for research aimed at reducing general NSSI risk factors that are more prevalence among LGBT populations as well as studies focused on addressing ones specific to these populations.
In summary, the findings of the current review collectively provide clear and robust evidence that NSSI is highly prevalent among sexual and gender minority groups, with transgender and bisexual populations being at greatest risk, and that disparities in prevalence with heterosexual and/or cisgender individuals are striking. These differences may in large measure be due to LGBT-specific experiences associated with risk (e.g., stigma and discrimination) combined with higher levels of more general risk correlates than in heterosexual and/or cisgender populations. Sexual minority youth also emerged as an especially vulnerable population. Furthermore, the available evidence suggests that, despite sustained efforts by the National Institute of Health and the National Academy of Medicine since the turn of the century to promote research addressing health disparities among sexual and gender minority populations, particularly in the case of self-injurious behaviors (Institute of Medicine, 2011; National Action Alliance for Suicide Prevention: Research Prioritization Task Force, 2014; National Institutes of Health, 2001, 2006, 2012, 2017), the prevalence of NSSI among sexual and gender minority groups has not improved over time. Therefore, not only is there a continued need for research in general to address this pressing priority, especially in terms of identifying which correlates are prospectively predictive of NSSI among LGBT individuals, but this need may be particular acute in the case of developing and implementing treatments effectively tailored for sexual and gender minority populations (Beard et al., 2017).
Supplementary Material
Highlights.
We conducted a meta-analysis of the association between LGBT status and NSSI
Sexual and gender minorities are at elevated risk for NSSI
Transgender and bisexual individuals are at greatest risk for NSSI
General and LGBT-specific factors likely account for this greater risk
Longitudinal and treatment studies are needed
Acknowledgements
Preparation of this manuscript was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Numbers R01MH101138, R01MH115905, and R21MH112055, as well as by the American Psychological Foundation Wayne F. Placek Grant. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Disclosures
Role of Funding Sources
Preparation of this manuscript was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Numbers R01MH101138, R01MH115905, and R21MH112055, as well as by the American Psychological Foundation Wayne F. Placek Grant. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Conflict of Interest
None
With the exception of studies including transgender participants, the studies included in the current review generally did not differentiate between sex and gender in reporting data on the proportion of the sample that was female. For percentage of female participants in the sample for studies with transgender participants, we extracted data on natal sex.
Although age treated as a continuous variable was not a significant moderator of this same association, this may have been due to there being only three out of the 18 studies reporting mean sample age having purely adolescent samples. In contrast, when age was treated as a categorical variable, 13 out of 38 samples included in moderator analysis featured purely adolescent samples.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
* Articles marked with an asterisk were included in the meta-analysis.
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association. [Google Scholar]
- Annor FB, Clayton HB, Gilbert LK, Ivey-Stephenson AZ, Irving SM, David-Ferdon C, & Kann LK (2018). Sexual orientation discordance and nonfatal suicidal behaviors in U.S. high school students. American Journal of Preventive Medicine, 54, 530–538. doi: 10.1016/j.amepre.2018.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Arcelus J, Claes L, Witcomb, Marshall, & Bouman (2016). Risk factors for non-suicidal self-injury among trans youth. Journal of Sexual Medicine, 13, 402–412. doi: 10.1016/j.jsxm.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, Vitiello B, et al. (2011). Suicide attempts and nonsuicidal self-injury in the Treatment of Resistant Depression in Adolescents: Findings from the TORDIA study. Journal of the American Academy of Child & Adolescent Psychiatry, 50, 772–781. doi: 10.1016/j.jaac.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Balsam KF, Beauchaine TP, Mickey RM, & Rothblum ED (2005). Mental health of lesbian, gay, bisexual, and heterosexual siblings: Effects of gender, sexual orientation, and family. Journal of Abnormal Psychology, 114, 471–476. doi: 10.1037/0021-843X.114.3.471 [DOI] [PubMed] [Google Scholar]
- Balsam KF, & Mohr JJ (2007). Adaptation to sexual orientation stigma: A comparison of bisexual and lesbian/gay adults. Journal of Counseling Psychology, 54, 306–319. [Google Scholar]
- Batejan KL, Jarvi SM, & Swenson LP (2015). Sexual orientation and non-suicidal selfinjury: A meta-analytic review. Archives of Suicide Research, 19, 131–150. doi: 10.1080/13811118.2014.957450 [DOI] [PubMed] [Google Scholar]
- *.Beard C, Kirakosian N, Silverman AL, Winer JP, Wadsworth LP, & Björgvinsson T (2017). Comparing treatment response between LGBQ and heterosexual individuals attending a CBT- and DBT-skills-based partial hospital. Journal of Consulting and Clinical Psychology, 85, 1171–1181. doi: 10.1037/ccp0000251 [DOI] [PubMed] [Google Scholar]
- Becerra-Culqui TA, Liu Y, Nash R, Cromwell L, Flanders WD, Getahun D, Giammattei SV, et al. (2018). Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics, 141, 1–11. doi: 10.1542/peds.2017-3845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Benau EM, Jenkins AL, & Conner BT (2017). Perceived parental monitoring and sexual orientation moderate lifetime acts of non-suicidal self-injury. Archives of Suicide Research, 21, 322–340. doi: 10.1080/13811118.2016.1182092 [DOI] [PubMed] [Google Scholar]
- *.Bergero-Miguel T, García-Encinas MA, Villena-Jimena A, Pérez-Costillas L, Sánchez-Álvarez N, de Diego-Otero Y, & Guzman-Parra J (2016). Gender dysphoria and social anxiety: An exploratory study in Spain. Journal of Sexual Medicine, 13, 1270–1278. doi: 10.1016/j.jsxm.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Biostat. (2014). Comprehensive Meta-Analysis Version 3. Englewood, NJ: Biostat. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2009). Introduction to Meta Analysis. Chichester, England: John Wiley & Sons, Ltd. doi: 10.1002/9780470743386 [DOI] [Google Scholar]
- *.Brennan SL, Irwin J, Drincic A, Amoura NJ, Randall A, & Smith-Sallans M (2017). Relationship among gender-related stress, resilience factors, and mental health in a Midwestern U.S. transgender and gender-nonconforming population. International Journal of Transgenderism, 18, 433–445. doi: 10.1080/15532739.2017.1365034 [DOI] [Google Scholar]
- Brent D (2011). Nonsuicidal self-injury as a predictor of suicidal behavior in depressed adolescents. American Journal of Psychiatry, 168, 452–454. doi: 10.1176/appi.ajp.2011.11020215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K, & Schoenleber M (2015). Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clinical Psychology Review, 38, 55–64. doi: 10.1016/j.cpr.2015.02.009 [DOI] [PubMed] [Google Scholar]
- Calati R, & Courtet P (2016). Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. Journal of Psychiatric Research, 79, 8–20. doi: 10.1016/j.jpsychires.2016.04.003 [DOI] [PubMed] [Google Scholar]
- *.Chakraborty A, McManus S, Brugha TS, Bebbington P, & King M (2011). Mental health of the non-heterosexual population of England. British Journal of Psychiatry, 198, 143–148. doi: 10.1192/bjp.bp.110.082271 [DOI] [PubMed] [Google Scholar]
- *.Claes L, Bouman WP, Witcomb G, Thurston M, Fernandez-Aranda F, & Arcelus J (2015). Non-suicidal self-injury in trans people: associations with psychological symptoms, victimization, interpersonal functioning, and perceived social support. Journal of Sexual Medicine, 12, 168–179. doi: 10.1111/jsm.12711 [DOI] [PubMed] [Google Scholar]
- *.Claes L, Luyckx K, Bijttebier P, Turner B, Ghandi A, Smets J, Norre J, et al. (2015). Non-suicidal self-injury in patients with eating disorder: Associations with identity formation above and beyond anxiety and depression. European Eating Disorders Review, 23, 147–155. doi: 10.1002/erv.2341 [DOI] [PubMed] [Google Scholar]
- *.Clark TC, Lucassen MFG, Bullen P, Denny SJ, Fleming TM, Robinson EM, & Rossen FV (2014). The health and well-being of transgender high school students: Results from the New Zealand adolescent health survey (youth’12). Journal of Adolescent Health, 55, 93–99. doi: 10.1016/j.jadohealth.2013.11.008 [DOI] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. doi: 10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig SL, & Austin A (2016). The AFFIRM open pilot feasibility study: A brief affirmative cognitive behavioral coping skills group intervention for sexual and gender minority youth. Children and Youth Services Review, 64, 136–144. doi: 10.1016/j.childyouth.2016.02.022 [DOI] [Google Scholar]
- *.Davey A, Arcelus J, Meyer C, & Bouman WP (2016). Self-injury among trans individuals and matched controls: prevalence and associated factors. Health and Social Care in the Community, 24, 485–494. doi: 10.1111/hsc.12239 [DOI] [PubMed] [Google Scholar]
- *.Davis LT, Weiss NH, Tull MT, & Gratz KL (2017). The relation of protective factors to deliberate self-harm among African-American adults: moderating roles of gender and sexual orientation identity. Journal of Mental Health, 26, 351–358. doi: 10.1080/09638237.2017.1340610 [DOI] [PubMed] [Google Scholar]
- *.DeCamp W, & Bakken NW (2016). Self-injury, suicide ideation, and sexual orientation: differences in causes and correlates among high school students. Journal of Injury & Violence, 8, 15–24. doi: 10.5249/jivr.v8i1.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Deliberto TL, & Nock MK (2008). An exploratory study of correlates, onset, and offset of non-suicidal self-injury. Archives of Suicide Research, 12, 219–231. doi: 10.1080/13811110802101096 [DOI] [PubMed] [Google Scholar]
- *.dickey l. m., Reisner SL, & Juntunen CL (2015). Non-suicidal self-injury in a large online sample of transgender adults. Professional Psychology: Research and Practice, 46, 3–11. doi: 10.1037/a0038803 [DOI] [Google Scholar]
- Drescher J (2010). Transsexualism, gender identity disorder and the DSM. Journal of Gay and Lesbian Mental Health, 14, 109–122. doi: 10.1080/19359701003589637 [DOI] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56, 455–463. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Eisenberg ME, Gower AL, McMorris BJ, Rider GN, Shea G, & Coleman E (2017). Risk and protective factors in the lives of transgender/gender nonconforming adolescents. Journal of Adolescent Health, 61, 521–526. doi: 10.1016/j.jadohealth.2017.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Fox KR, Hooley JM, Smith DMY, Ribeiro JD, Huang X, Nock MK, & Franklin JC (2018). Self-injurious thoughts and behaviors may be more common and severe among people identifying as a sexual minority. Behavior Therapy, 49, 768–780. doi: 10.1016/j.beth.2017.11.009 [DOI] [PubMed] [Google Scholar]
- *.Fraser G, Wilson MS, Garisch JA, Robinson K, Brocklesby M, Kingi T, O’Connell A, et al. (2018). Non-suicidal self-injury, sexuality concerns, and emotion regulation among sexually diverse adolescents: A multiple mediation analysis. Archives of Suicide Research, 22, 432–452. doi: 10.1080/13811118.2017.1358224 [DOI] [PubMed] [Google Scholar]
- *.Gandhi A, Luyckx K, Maitra S, & Claes L (2015). Non-suicidal self-injury and identity distress in Flemish adolescents: Exploring gender differences and mediational pathways. Personality and Individual Differences, 82, 215–220. doi: 10.1016/j.paid.2015.03.031 [DOI] [Google Scholar]
- Garofalo R, Wolf RC, Wissow LS, Woods ER, & Goodman E (1999). Sexual orientation and risk of suicide attempts among a representative sample of youth. Archives of Pediatrics & Adolescent Medicine, 153, 487–493. doi: 10.1001/archpedi.153.5.487 [DOI] [PubMed] [Google Scholar]
- Gates GJ (2010). Sexual minorities in the 2008 General Social Survey: Coming out and demographic characteristics. Los Angeles, CA. [Google Scholar]
- *.Goldbach JT, Schrager SM, & Mamey MR (2017). Criterion and divergent validity of the sexual minority adolescent stress inventory. Frontiers in Psychology, 8, 1–13. doi: 10.3389/fpsyg.2017.02057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gollust SE, Eisenberg D, & Golberstein E (2008). Prevalence and correlates of self-injury among university students. Journal of American College Health, 56, 491–498. doi: 10.3200/JACH.56.5.491-498 [DOI] [PubMed] [Google Scholar]
- Haas AP, Eliason M, Mays VM, Mathy RM, Cochran SD, D’Augelli AR, Silverman MM, et al. (2011). Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: Review and recommendations. Journal of Homosexuality, 58, 10–51. doi: 10.1080/00918369.2011.534038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hickson F, Davey C, Reid D, Weatherburn P, & Bourne A (2017). Mental health inequalities among gay and bisexual men in England, Scotland and Wales: A large community-based cross-sectional survey. Journal of Public Health, 39, 266–273. doi: 10.1093/pubmed/fdw021 [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilt LM, Nock MK, Lloyd-Richardson EE, & Prinstein MJ (2008). Longitudinal study of nonsuicidal self-injury among young adolescents: Rates, correlates, and preliminary test of an interpersonal model. Journal of Early Adolescence, 28, 455–469. doi: 10.1177/0272431608316604 [DOI] [Google Scholar]
- *.House AS, van Horn E, Coppeans C, & Stepleman LM (2011). Interpersonal trauma and discriminatory events as predictors of suicidal and nonsuicidal self-injury in gay, lesbian, bisexual, and transgender persons. Traumatology, 17, 75–85. doi: 10.1177/1534765610395621 [DOI] [Google Scholar]
- Institute of Medicine. (2011). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- *.Irish M, Solmi F, Mars B, King M, Lewis G, Pearson RM, Pitman A, et al. (2019). Depression and self-harm from adolescence to young adulthood in sexual minorities compared with heterosexuals in the UK: a population-based cohort study. Lancet Child and Adolescent Health, 3, 91–98. doi: 10.1016/S2352-4642(18)30343-2 [DOI] [PubMed] [Google Scholar]
- Israel T, & Mohr JJ (2004). Attitudes toward bisexual women and men: Current research, future directions In Fox RC (Ed.), Current research on bisexuality (pp. 117–134). Binghamton, NY: Harrington Park Press/Haworth Press. [Google Scholar]
- *.Jackman KB, Dolezal C, Levin B, Honig JC, & Bockting WO (2018). Stigma, gender dysphoria, and nonsuicidal self-injury in a community sample of transgender individuals. Psychiatry Research, 269, 602–609. doi: 10.1016/j.psychres.2018.08.092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackman K, Honig J, & Bockting W (2016). Nonsuicidal self-injury among lesbian, gay, bisexual and transgender populations: an integrative review. Journal of Clinical Nursing, 25, 3438–3453. doi: 10.1111/jocn.13236 [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Rodgers B, Jacomb PA, & Christensen H (2002). Sexual orientation and mental health: Results from a community survey of young and middle-aged adults. British Journal of Psychiatry, 180, 423–327. doi: 10.1192/bjp.180.5.423 [DOI] [PubMed] [Google Scholar]
- *.Katz-Wise SL, Ehrensaft D, Vetters R, Forcier M, & Austin SB (2018). Family functioning and mental health of transgender and gender-nonconforming youth in the trans teen and family narratives project. Journal of Sex Research, 55, 582–590. doi: 10.1080/00224499.2017.1415291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Katz-Wise SL, Reisner SL, White Hughto JM, & Budge SL (2017). Self-reported changes in attractions and social determinants of mental health in transgender adults. Archives of Sexual Behavior, 46, 1425–1439. doi: 10.1007/s10508-016-0812-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Kraemer HC, Kessler RC, Kupfer DJ, & Offord DR (1997). Contributions of risk-factor research to developmental psychopathology. Clinical Psychology Review, 17, 375–406. [DOI] [PubMed] [Google Scholar]
- *.Kidd JD, White JL, & Johnson RM (2012). Mental health service contacts among sexual minority and heterosexual girls in boston public high schools. Journal of Gay and Lesbian Mental Health, 16, 111–123. doi: 10.1080/19359705.2012.653907 [DOI] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, & Kupfer DJ (1997). Coming to terms with the terms of risk. Archives of General Psychiatry, 54, 337–343. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Morgan GA, Leech NL, Gliner JA, Vaske JJ, & Harmon RJ (2003). Measures of clinical significance. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1524–1529. doi: 10.1097/00004583-200312000-00022 [DOI] [PubMed] [Google Scholar]
- Lee JGL, Ylioja T, & Lackey M (2016). Identifying lesbian, gay, bisexual, and transgender search terminology: A systematic review of health systematic reviews. PloS One, 11, e0156210. doi: 10.1371/journal.pone.0156210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lefevor GT, Boyd-Rogers CC, Sprague BM, & Janis RA (2019). Health disparities between genderqueer, transgender, and cisgender individuals: an extension of minority stress theory. Journal of Counseling Psychology. doi: 10.1037/cou0000339 [DOI] [PubMed] [Google Scholar]
- Liu CH, Stevens C, Wong SHM, Yasui M, & Chen JA (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depression and Anxiety, 36, 8–17. doi: 10.1002/da.22830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Liu RT (2019). Temporal trends in the prevalence of nonsuicidal self-injury among sexual minority and heterosexual youth from 2005 through 2017. JAMA Pediatrics, 173, 790–791. doi: 10.1136/bmj.g5954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Cheek SM, & Nestor BA (2016). Non-suicidal self-injury and life stress: A systematic meta-analysis and theoretical elaboration. Clinical Psychology Review, 47, 1–14. doi: 10.1016/j.cpr.2016.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Scopelliti KM, Pittman SK, & Zamora AS (2018). Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry, 5, 51–64. doi: 10.1016/S2215-0366(17)30469-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Trout ZM, Hernandez EM, Cheek SM, & Gerlus N (2017). A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience and Biobehavioral Reviews, 83, 440–450. doi: 10.1016/J.NEUBIOREV.2017.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucassen MFG, Stasiak K, Samra R, Frampton CMA, & Merry SN (2017). Sexual minority youth and depressive symptoms or depressive disorder: A systematic review and meta-analysis of population-based studies. Australian and New Zealand Journal of Psychiatry, 51, 774–787. doi: 10.1177/0004867417713664 [DOI] [PubMed] [Google Scholar]
- *.Macrynikola N, Miranda R, & Soffer A (2018). Social connectedness, stressful life events, and self-injurious thoughts and behaviors among young adults. Comprehensive Psychiatry, 80, 140–149. doi: 10.1016/j.comppsych.2017.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B, Heron J, Crane C, Hawton K, Kidger J, Lewis G, Macleod J, et al. (2014). Differences in risk factors for self-harm with and without suicidal intent: findings from the ALSPAC cohort. Journal of Affective Disorders, 168, 407–414. doi: 10.1016/j.jad.2014.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.McDowell MJ, White Hughto JM, & Reisner SL (2019). Risk and protective factors for mental health morbidity in a community sample of female-to-male trans-masculine adults. BMC Psychiatry, 19, 1–12. doi: 10.1186/s12888-018-2008-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological bulletin, 129, 674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, & Wilson PA (2009). Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology, 56, 23–31. doi: 10.1037/a0014587 [DOI] [Google Scholar]
- *.Monto MA, McRee N, & Deryck FS (2018). Nonsuicidal self-Injury among a representative sample of US adolescents, 2015. American Journal of Public Health, 108, 1042–1048. doi: 10.2105/AJPH.2018.304470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Muehlenkamp JJ, Hilt LM, Ehlinger PP, & McMillan T (2015). Nonsuicidal self-injury in sexual minority college students: A test of theoretical integration. Child and Adolescent Psychiatry and Mental Health, 9, 1–8. doi: 10.1186/s13034-015-0050-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, & Liu RT (2013). A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Archives of Sexual Behavior, 42, 437–448. doi: 10.1007/s10508-012-0013-9 [DOI] [PubMed] [Google Scholar]
- National Action Alliance for Suicide Prevention: Research Prioritization Task Force. (2014). A prioritized research agenda for suicide prevention: An action plan to save lives. Rockville, MD: National Institute of Mental Health and the Research Prioritization Task Force. [Google Scholar]
- National Institutes of Health. (2001). Behavioral, social, mental health, and substance abuse research with diverse populations. Retrieved from https://grants.nih.gov/grants/guide/pa-files/PA-01-096.html
- National Institutes of Health. (2006). Health Research with Diverse Populations. Retrieved from https://grants.nih.gov/grants/guide/pa-files/PA-06-218.html
- National Institutes of Health. (2012). Research on the Health of LGBTI Populations. Retrieved from https://grants.nih.gov/grants/guide/pa-files/PA-12-111.html
- National Institutes of Health. (2017). The Health of Sexual and Gender Minority (SGM) Populations. Retrieved from https://grants.nih.gov/grants/guide/pa-files/PA-18-037.html
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30, 1019–1029. doi: 10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- Newcomb ME, & Mustanski B (2011). Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sexual Behavior, 40, 189–199. doi: 10.1007/s10508-009-9573-8 [DOI] [PubMed] [Google Scholar]
- Nock MK (2010). Self-injury. Annual Review of Clinical Psychology, 6, 339–363. doi: 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- O’Brien KHM, Liu RT, Putney J, Burke TA, & Aguinaldo L (2017). Suicide and non-suicidal self-injury In Smalley KB, Warren JC, & Barefoot KN (Eds.), LGBT Health: Meeting the Health Needs of Gender and Sexual Minorities (pp. 181–198). New York: Springer. [Google Scholar]
- Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, Wells M, et al. (2011). Lesbian, gay, bisexual, and transgender–related content in undergraduate medical education. JAMA, 306, 971–977. doi: 10.1001/jama.2011.1255 [DOI] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, & Asarnow JR (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 97–107.e2. doi: 10.1016/j.jaac.2014.10.009 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology, 83, 875–889. doi: 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakula B, Shoveller J, Ratner PA, & Carpiano R (2016). Prevalence and co-occurrence of heavy drinking and anxiety and mood disorders among gay, lesbian, bisexual, and heterosexual Canadians. American Journal of Public Health, 106, 1042–1048. doi: 10.2105/AJPH.2016.303083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plener PL, Schumacher TS, Munz LM, & Groschwitz RC (2015). The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personality Disorder and Emotion Dysregulation, 2, 2. doi: 10.1186/s40479-014-0024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ray-Sannerud BN, Bryan CJ, Perry NS, & Bryan AO (2015). High levels of emotional distress, trauma exposure, and self-injurious thoughts and behaviors among military personnel and veterans with a history of same sex behavior. Psychology of Sexual Orientation and Gender Diversity, 2, 130–137. doi: 10.1037/sgd0000096 [DOI] [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychological Medicine, 46, 225–236. doi: 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Salway T, Tarasoff LA, MacKay JM, Hawkins BW, & Fehr CP (2018). Prevalence of depression and anxiety among bisexual people compared to gay, lesbian, and heterosexual individuals: A systematic review and meta-analysis. Journal of Sex Research, 55, 435–456. doi: 10.1080/00224499.2017.1387755 [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC (2006). Who’s gay? Does it matter? Current Directions in Psychological Science, 15, 40–44. doi: 10.1111/j.0963-7214.2006.00403.x [DOI] [Google Scholar]
- *.Serras A, Saules KK, Cranford JA, & Eisenberg D (2010). Self-injury, substance use, and associated risk factors in a multi-campus probability sample of college students. Psychology of Addictive Behaviors, 24, 119–128. doi: 10.1037/a0017210 [DOI] [PubMed] [Google Scholar]
- *.Silva C, Chu C, Monahan KR, & Joiner TE (2015). Suicide risk among sexual minority college students: a mediated moderation model of sex and perceived burdensomeness. Psychology of Sexual Orientation and Gender Diversity, 2, 22–33. doi: 10.1037/sgd0000086 [DOI] [Google Scholar]
- *.Smith ER, & Perrin PB (2017). Structural equation modeling linking perceived heterosexism, mental health, and nonsuicidal self-injury in ethnically diverse sexual minority men and women. Traumatology, 23, 258–264. doi: 10.1037/trm0000111 [DOI] [Google Scholar]
- *.Sornberger MJ, Smith NG, Toste JR, & Heath NL (2013). Nonsuicidal self-injury, coping strategies, and sexual orientation. Journal of Clinical Psychology, 69, 571–583. doi: 10.1002/jclp.21947 [DOI] [PubMed] [Google Scholar]
- *.Staples JM, Neilson EC, Bryan AEB, & George WH (2018). The role of distal minority stress and internalized transnegativity in suicidal ideation and nonsuicidal self-injury among transgender adults. Journal of Sex Research, 55, 591–603. doi: 10.1080/00224499.2017.1393651 [DOI] [PubMed] [Google Scholar]
- *.Swannell S, Martin G, & Page A (2016). Suicidal ideation, suicide attempts and nonsuicidal self-injury among lesbian, gay, bisexual and heterosexual adults: Findings from an Australian national study. Australian and New Zealand Journal of Psychiatry, 50, 145–153. doi: 10.1177/0004867415615949 [DOI] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St John NJ (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide and Life-Threatening Behavior, 44, 273–303. doi: 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- *.Taliaferro LA, McMorris BJ, Rider GN, & Eisenberg ME (2019). Risk and protective factors for self-harm in a population-based sample of transgender youth. Archives of Suicide Research, 23, 203–221. doi: 10.1080/13811118.2018.1430639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Taliaferro LA, & Muehlenkamp JJ (2017). Nonsuicidal self-injury and suicidality among sexual minority youth: risk factors and protective connectedness factors. Academic Pediatrics, 17, 715–722. doi: 10.1016/j.acap.2016.11.002 [DOI] [PubMed] [Google Scholar]
- *.Taylor PJ, Dhingra K, Dickson JM, & McDermott E (n.d.). Psychological correlates of self-harm within gay, lesbian and bisexual uk university students. Archives of Suicide Research. doi: 10.1080/13811118.2018.1515136 [DOI] [PubMed] [Google Scholar]
- Testa RJ, Michaels MS, Bliss W, Rogers ML, Balsam KF, & Joiner T (2016). Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors. Journal of Abnormal Psychology, 126, 125–136. doi: 10.1037/abn0000234 [DOI] [PubMed] [Google Scholar]
- *.Thorne N, Witcomb GL, Nieder T, Nixon E, Yip A, & Arcelus J (2019). A comparison of mental health symptomatology and levels of social support in young treatment seeking transgender individuals who identify as binary and non-binary. International Journal of Transgenderism, 20, 241–250. doi: 10.1080/15532739.2018.1452660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Veale JF, Peter T, Travers R, & Saewyc EM (2017). Enacted stigma, mental health, and protective factors among transgender youth in canada. Transgender Health, 2, 207–216. doi: 10.1089/trgh.2017.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Veale JF, Watson RJ, Peter T, & Saewyc EM (2017). Mental health disparities among canadian transgender youth. Journal of Adolescent Health, 60, 44–49. doi: 10.1016/j.jadohealth.2016.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock J (2010). Self-injurious behavior in adolescents. PLOS Medicine, 7, e1000240. doi: 10.1371/journal.pmed.1000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock J, Eckenrode J, & Silverman D (2006). Self-injurious behaviors in a college population. Pediatrics, 117, 1939–1948. doi: 10.1542/peds.2005-2543 [DOI] [PubMed] [Google Scholar]
- *.Whitlock J, & Knox KL (2007). The relationship between self-injurious behavior and suicide in a young adult population. Archives of Pediatrics and Adolescent Medicine, 161, 634–640. doi: 10.1001/archpedi.161.7.634 [DOI] [PubMed] [Google Scholar]
- *.Whitlock J, Muehlenkamp J, Purington A, Eckenrode J, Barreira P, Baral Abrams G, Marchell T, et al. (2011). Nonsuicidal self-injury in a college population: General trends and sex differences. Journal of American College Health, 59, 691–698. doi: 10.1080/07448481.2010.529626 [DOI] [PubMed] [Google Scholar]
- Wichstrøm L (2009). Predictors of non-suicidal self-injury versus attempted suicide: Similar or different? Archives of Suicide Research, 13, 105–122. doi: 10.1080/13811110902834992 [DOI] [PubMed] [Google Scholar]
- *.Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, & O’Grady KE (2012). Longitudinal predictors of past-year non-suicidal self-injury and motives among college students. Psychological medicine, 42, 717–26. doi: 10.1017/S0033291711001814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, & Goodyer I (2011). Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). American Journal of Psychiatry, 168, 495–501. doi: 10.1176/appi.ajp.2010.10050718 [DOI] [PubMed] [Google Scholar]
- *.Zaki LF, Gross M, & Pachankis JE (2017). Help-seeking for nonsuicidal self-injury in sexual minority adolescent and young adult females. Journal of Gay and Lesbian Mental Health, 21, 171–187. doi: 10.1080/19359705.2016.1273156 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.