Abstract
EUS-guided biliary drainage (EUS-BD) has been recognized as a new alternative to failed ERCP. The alternatives for failed/impossible ERCP in cases of difficult and selective bile duct cannulation include percutaneous transhepatic BD (PTBD) with precut papillotomy. EUS-BD is reportedly more convenient than PTBD and more successful than precut papillotomy, suggesting that EUS-BD is the next step following failed/impossible ERCP.
Keywords: EUS-guided biliary drainage, percutaneous transhepatic biliary drainage, precut papillotomy technique
INTRODUCTION
The transpapillary biliary approach using ERCP is recognized as the most standard biliary drainage (BD) therapy, with reported technical success rates of >90%. However, the procedure may fail due to anatomical and technical reasons such as surgically altered anatomy, upper intestinal obstruction, and duodenal papillary tumor invasion.[1,2,3] Percutaneous transhepatic BD (PTBD) has been widely used as an alternative procedure for patients with failed ERCP. However, PTBD involves an external fistula drainage system that drastically decreases patients' quality of life.[4,5,6] Another alternative is precut papillotomy, which is generally performed when deep bile duct cannulation fails during ERCP.
EUS-guided BD (EUS-BD) was first reported by Giovannini et al. in 2001;[7] it has gained substantial attention in recent years, and its efficacy has been demonstrated.[8,9,10,11,12] Unlike PTBD, EUS-BD involves an internal fistula between the biliary and gastrointestinal tracts, preserving patients' quality of life. In recent systematic reviews, the technical success rate for EUS-BD has been reported to be >90%,[13,14,15] suggesting its use as the standard treatment for BD in future.
The present study aimed to evaluate the efficacy of EUS-BD compared with that of conventional therapies in patients with failed selective bile duct cannulation.
EUS-BILIARY DRAINAGE VERSUS PERCUTANEOUS TRANSHEPATIC BILIARY DRAINAGE
PTBD has been the most common secondary BD treatment for cases of failed ERCP, but EUS-BD has been widely performed recently. To date, only ten studies have compared the efficacies of EUS-BD and PTBD after failed ERCP,[16,17,18,19,20,21,22,23,24,25] including seven retrospective studies[17,18,19,21,22,23,25] and three prospective, randomized, controlled trials[16,20,24] (two multicenter and eight single-center studies). Table 1 summarizes the results of these ten studies. Among the 530 patients included in these studies, 282 underwent EUS-BD and 248 underwent PTBD, with similar technical success rates obtained for EUS-BD (91% [256/282]) and PTBD (95% [236/248]). The clinical success rates for EUS-BD and PTBD were 84% (163/195) and 81% (137/169), respectively, in 364 patients in seven studies.[16,18,21,22,23,24,25] A systematic review and meta-analysis of nine studies[16,17,18,19,20,21,22,23,24] involving 483 patients found no difference in terms of technical success rate between EUS-BD and PTBD. However, EUS-BD showed a higher clinical success rate and significantly lower complication and reintervention rates than PTBD.[26] Although EUS-BD requires advanced techniques and it should be performed by experienced endoscopists, these results suggest that EUS-BD has several advantages over PTBD.
Table 1.
Studies on EUS-guided biliary drainage versus percutaneous transhepatic biliary drainage
| References | Study design | Number of patients | Technical success rate (%) | Clinical success rate (%) | Adverse event rate (%) | Reintervention rate (%) |
|---|---|---|---|---|---|---|
| Artifon et al.[16] | Prospective, RCT | EUS-BD: 13 PTBD: 12 |
13/13 (100) 12/12 (100) |
13/13 (100) 12/12 (100) |
2/13 (15) 3/12 (25) |
- |
| Bapaye et al.[17] | Retrospective | EUS-BD: 25 PTBD: 26 |
23/25 (92) 26/26 (100) |
- | 5/25 (20) 12/26 (46) |
- |
| Khashab et al.[18] | Retrospective | EUS-BD: 22 PTBD: 51 |
19/22 (86) 51/51 (100) |
19/19 (100) 47/51 (92) |
4/22 (18) 20/51 (39) |
3/19 (16) 23/51 (45) |
| Bill et al.[19] | Retrospective | EUS-BD: 25 PTBD: 25 |
19/25 (76) 25/25 (100) |
24/25 (96) 20/25 (80) |
7/25 (28) 9/25 (36) |
4/25 (16) 15/25 (60) |
| Giovannini et al.[20] | Prospective, RCT | EUS-BD: 20 PTBD: 21 |
19/20 (95) 17/21 (85) |
- | 7/20 (35) 12/21 (60) |
- |
| Sharaiha et al.[21] | Retrospective | EUS-BD: 47 PTBD: 13 |
43/47 (92) 11/13 (93) |
27/43 (63) 3/11 (27) |
5/47 (15) 11/13 (85) |
12/43 (28) 10/11 (91) |
| Torres-Ruiz et al.[22] | Retrospective | EUS-BD: 35 PTBD: 31 |
28/35 (81) 28/31 (90) |
25/28 (89) 19/28 (68) |
9/35 (26) 20/31 (65) |
2/28 (7) 8/28 (29) |
| Sportes et al.[23] | Retrospective | EUS-BD: 31 PTBD: 20 |
31/31 (100) 20/20 (100) |
25/31 (86) 15/20 (83) |
5/31 (16) 2/20 (10) |
2/31 (6) 4/21 (19) |
| Lee et al.[24] | Prospective, RCT | EUS-BD: 34 PTBD: 32 |
32/34 (94) 31/32 (97) |
28/32 (88) 27/31 (87) |
3/34 (9) 9/32 (28) |
11/32 (34) 29/31 (94) |
| Ogura et al.[25] | Retrospective | EUS-BD: 30 PTBD: 18 |
29/30 (97) 16/18 (89) |
26/29 (90) 14/16 (88) |
3/30 (10) 3/18 (17) |
- |
RCT: Randomized controlled trial, EUS-BD: EUS-guided biliary drainage, PTBD: Percutaneous transhepatic biliary drainage
Most PTBD cases involve the use of plastic stents, whereas most endoscopists performing EUS-BD prefer metal stents; this difference may be related to adverse events, such as bile leakage and stent occlusion. PTBD is often performed by radiologists, but EUS-BD is performed by endoscopists who have the advantage of immediately shifting to the secondary treatment after ERCP failure. Ngamruengphong et al. reported that the average number of interventions per patient was 3.44 for PTBD and 1.67 for EUS-BD, and that EUS-BD is more cost-effective than PTBD owing to its lower need for reintervention.[27]
In addition, endoscopists can choose among different EUS-BD routes and methods, whereas PTBD has the limitation of drainage route selection and does not offer these options. PTBD requires intrahepatic bile duct dilatation because only the intrahepatic bile ducts are its target. Conversely, EUS-BD can be achieved through both intrahepatic and extrahepatic bile duct approaches, and the selection of an appropriate drainage route may determine treatment effectiveness [Figure 1].
Figure 1.
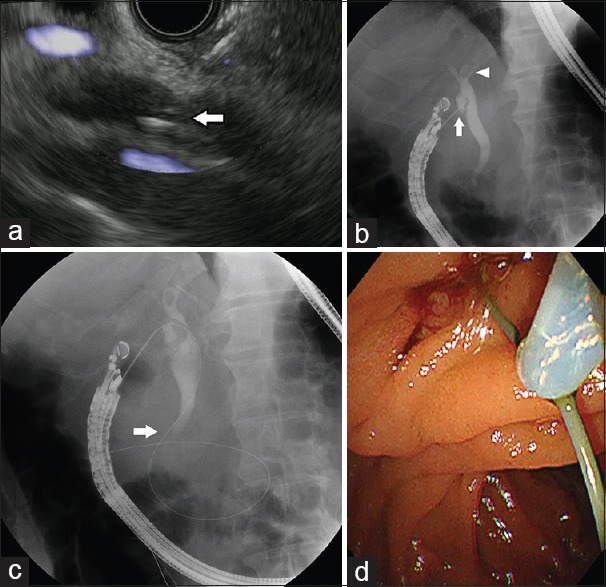
A case of choledocholithiasis, wherein EUS-rendezvous was performed without intrahepatic bile duct dilatation. (a) Puncture the extrahepatic bile duct using a 19G fine-needle aspiration needle under EUS guidance (white arrow). (b) Inject a contrast medium into the extrahepatic bile duct (white arrow) and then, confirm choledocholithiasis (white arrowhead). (c) Lead the guidewire successfully to the papilla side (white arrow) and advance it to the duodenum. (d) While retaining guidewire, remove the EUS scope and insert the ERCP scope to the duodenal papilla. Then, hold the soft parts of guidewire using a snare
A recent meta-analysis revealed no significant difference between the intrahepatic and extrahepatic bile duct approaches regarding efficacy and safety.[14] Tyberg et al. proposed an algorithm for the BD route in EUS-BD after ERCP failure,[28] which suggested that the procedure must be switched to the extrahepatic bile duct approach when drainage from intrahepatic bile ducts is unsuccessful. In this report, the use of multiple access routes and methods resulted in efficacy and safety superior to those reported in other studies. Minaga et al. reported no difference in terms of technical success rates between extrahepatic and intrahepatic bile duct approaches.[29] In addition, when one approach appears significantly challenging, readily switching to the other approach could increase the overall technical success rate.[29]
These studies suggest that EUS-BD is more useful for patients with ERCP failure than PTBD because of its favorable clinical outcomes and lower adverse event and reintervention rates. In addition, the option of selecting the bile duct approach route is considered as an advantage.
EUS-GUIDED BILIARY DRAINAGE VERSUS PRECUT PAPILLOTOMY
According to a meta-analysis on the success rate for ERCP, the selective deep bile duct cannulation rate is approximately 89%, and precut papillotomy is generally performed when deep bile duct cannulation fails.[30] Bile duct cannulation has been successful in >65% of cases, in which precut papillotomy was performed when ERCP failed.[30,31,32,33,34,35,36] Currently, two precut methods are available: one using a needle knife, and the other using a papillotome. Needle knife precut papillotomy has been performed since the 1980s.[37] The papillotome precutting method was first reported by Goff in 1995 as transpancreatic precut sphincterotomy.[38] A prospective randomized controlled trail study that compared the outcomes of transpancreatic precut sphincterotomy and needle knife precut papillotomy concluded that the former method increases the rate of selective biliary cannulation and shortens the examination time without increasing the risk of complications.[39]
To the best of our knowledge, only two retrospective studies have compared the efficacy of precut papillotomy and EUS-BD in patients with failed bile duct cannulation.[11,40] Table 2 summarizes the results of these two studies.[11,40] Lee et al. conducted a retrospective, multicenter, cohort study on patients with selective bile duct cannulation failure who underwent precut papillotomy plus EUS-BD or precut papillotomy alone. They showed that the failure rate for ERCP was significantly lower, and technical success rate was higher in the precut papillotomy plus EUS-BD group than those in the precut papillotomy alone group.[40]
Table 2.
Studies of EUS-guided biliary drainage versus precut papillotomy
| References | Study design | Number of patients | Technical success rate (%) | Complications rate (%) |
|---|---|---|---|---|
| Dhir et al.[11] | Retrospective | EUS-BD: 58 Precut: 144 |
57/58 (98) 130/144 (90) P=0.038 |
2/58 (3) 10/144 (7) P=0.27 |
| Lee A et al.[40] | Retrospective | EUS-BD: 61 Precut: 142 |
58/61 (95) 107/142 (75) P<0.001 |
- |
EUS-BD: EUS-guided biliary drainage
In a single-center, retrospective study, Dhir et al. compared technical success and complication rates between EUS-guided rendezvous technique (EUS-RV) and precut papillotomy in patients with failed selective bile duct cannulation and found that the technical success rate was significantly higher in the EUS-RV group (57/58, 98.3%) than in the precut papillotomy group (130/144, 90.3%).[11] There was no significant difference in terms of complication rate between the groups, although one patient in the precut papillotomy group experienced severe pancreatitis requiring prolonged hospitalization.[11]
Taken together, these results suggest that EUS-BD has a higher technical success rate than precut papillotomy. In cases of malignant biliary obstruction caused by carcinoma of the head of the pancreas, distal bile duct, or papilla of Vater; tumor invasion into the papilla of Vater and duodenal stenosis cause challenges while performing precut papillotomy; further, precut papillotomy is associated with a high complication risk. For particularly, such cases, EUS-BD allows the selection of a tumor-free drainage route; therefore, it is considered to be associated with a lower complication risk than precut papillotomy [Figure 2].
Figure 2.
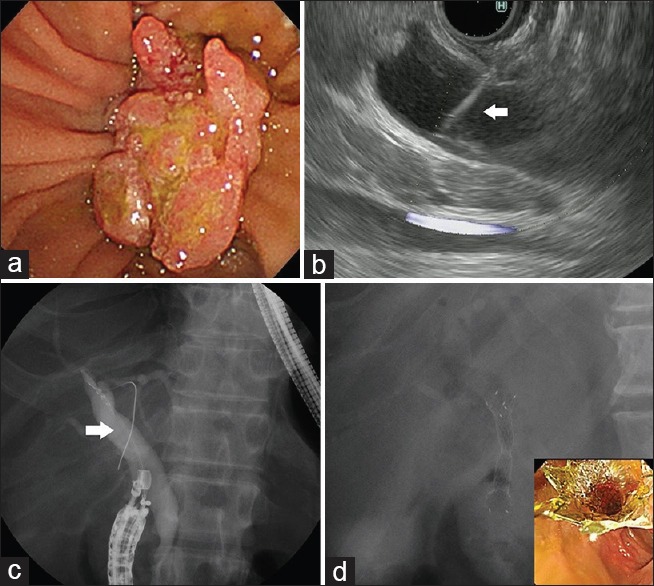
A case of failed ERCP for carcinoma of the duodenal papilla. (a) Papillary orifice cannot be recognized due to carcinoma of the papilla of Vater. (b) Puncture the extrahepatic bile duct from the duodenal bulb (white arrow). (c) Followed by cholangiography, advances the guidewire into the hilar bile duct. Then, insert the stent delivery system (white arrow). (d) The stent is deployed completely
Taken together, our literature review suggests that EUS-BD is a more effective treatment than conventional precut papillotomy for patients with failed selective bile duct cannulation.
CONCLUSION
PTBD and precut papillotomy have been often performed in cases of failed selective bile duct cannulation; however, EUS-BD is more convenient than conventional therapies. For EUS-BD to be recognized as a standard therapy in future, more studies confirming these findings are warranted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Enochsson L, Swahn F, Arnelo U, et al. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish registry for gallstone surgery and ERCP. Gastrointest Endosc. 2010;72:1175–84. doi: 10.1016/j.gie.2010.07.047. 1184.e1-3. [DOI] [PubMed] [Google Scholar]
- 2.Tonozuka R, Itoi T, Tsuchiya T, et al. EUS-guided biliary drainage is infrequently used even in high-volume centers of interventional EUS. Gastrointest Endosc. 2016;84:206–7. doi: 10.1016/j.gie.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: Effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296–301. doi: 10.1055/s-2007-995566. [DOI] [PubMed] [Google Scholar]
- 4.Yee AC, Ho CS. Complications of percutaneous biliary drainage: Benign vs. malignant diseases. AJR Am J Roentgenol. 1987;148:1207–9. doi: 10.2214/ajr.148.6.1207. [DOI] [PubMed] [Google Scholar]
- 5.Oh HC, Lee SK, Lee TY, et al. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731–6. doi: 10.1055/s-2007-966577. [DOI] [PubMed] [Google Scholar]
- 6.Winick AB, Waybill PN, Venbrux AC. Complications of percutaneous transhepatic biliary interventions. Tech Vasc Interv Radiol. 2001;4:200–6. doi: 10.1016/s1089-2516(01)90026-5. [DOI] [PubMed] [Google Scholar]
- 7.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui AA, Sreenarasimhaiah J, Lara LF, et al. Endoscopic ultrasound-guided transduodenal placement of a fully covered metal stent for palliative biliary drainage in patients with malignant biliary obstruction. Surg Endosc. 2011;25:549–55. doi: 10.1007/s00464-010-1216-6. [DOI] [PubMed] [Google Scholar]
- 9.Hara K, Yamao K, Hijioka S, et al. Prospective clinical study of endoscopic ultrasound-guided choledochoduodenostomy with direct metallic stent placement using a forward-viewing echoendoscope. Endoscopy. 2013;45:392–6. doi: 10.1055/s-0032-1326076. [DOI] [PubMed] [Google Scholar]
- 10.Komaki T, Kitano M, Sakamoto H, et al. Endoscopic ultrasonography-guided biliary drainage: Evaluation of a choledochoduodenostomy technique. Pancreatology. 2011;11(Suppl 2):47–51. doi: 10.1159/000323508. [DOI] [PubMed] [Google Scholar]
- 11.Dhir V, Bhandari S, Bapat M, et al. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos) Gastrointest Endosc. 2012;75:354–9. doi: 10.1016/j.gie.2011.07.075. [DOI] [PubMed] [Google Scholar]
- 12.Vila JJ, Pérez-Miranda M, Vazquez-Sequeiros E, et al. Initial experience with EUS-guided cholangiopancreatography for biliary and pancreatic duct drainage: A Spanish National Survey. Gastrointest Endosc. 2012;76:1133–41. doi: 10.1016/j.gie.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Khan MA, Akbar A, Baron TH, et al. Endoscopic ultrasound-guided biliary drainage: A systematic review and meta-analysis. Dig Dis Sci. 2016;61:684–703. doi: 10.1007/s10620-015-3933-0. [DOI] [PubMed] [Google Scholar]
- 14.Wang K, Zhu J, Xing L, et al. Assessment of efficacy and safety of EUS-guided biliary drainage: A systematic review. Gastrointest Endosc. 2016;83:1218–27. doi: 10.1016/j.gie.2015.10.033. [DOI] [PubMed] [Google Scholar]
- 15.Moole H, Bechtold ML, Forcione D, et al. A meta-analysis and systematic review: Success of endoscopic ultrasound guided biliary stenting in patients with inoperable malignant biliary strictures and a failed ERCP. Medicine (Baltimore) 2017;96:e5154. doi: 10.1097/MD.0000000000005154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Artifon EL, Aparicio D, Paione JB, et al. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: Endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768–74. doi: 10.1097/MCG.0b013e31825f264c. [DOI] [PubMed] [Google Scholar]
- 17.Bapaye A, Dubale N, Aher A. Comparison of endosonography-guided vs. percutaneous biliary stenting when papilla is inaccessible for ERCP. United European Gastroenterol J. 2013;1:285–93. doi: 10.1177/2050640613490928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khashab MA, Valeshabad AK, Afghani E, et al. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557–65. doi: 10.1007/s10620-014-3300-6. [DOI] [PubMed] [Google Scholar]
- 19.Bill JG, Darcy M, Fujii-Lau LL, et al. A comparison between endoscopic ultrasound-guided rendezvous and percutaneous biliary drainage after failed ERCP for malignant distal biliary obstruction. Endosc Int Open. 2016;4:E980–5. doi: 10.1055/s-0042-112584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giovannini M, Napoleon B, Barthet M, et al. Multicenter randomized phase II study: Percutaneous biliary drainage vs. EUS guided biliary drainage: Results of the intermediate analysis [abstract] Gastrointest Endosc. 2015;81:AB174. [Google Scholar]
- 21.Sharaiha RZ, Kumta NA, Desai AP, et al. Endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage: Predictors of successful outcome in patients who fail endoscopic retrograde cholangiopancreatography. Surg Endosc. 2016;30:5500–5. doi: 10.1007/s00464-016-4913-y. [DOI] [PubMed] [Google Scholar]
- 22.Torres-Ruiz MF, De La Mora-Levy JG, Alonso-Larraga JO, et al. Biliary drainage in malignant obstruction: A comparative study between EUS-guided vs. percutaneous drainage in patients with failed ERCP [abstract] Gastrointest Endosc. 2016;83:AB356. [Google Scholar]
- 23.Sportes A, Camus M, Grabar S, et al. Comparative trial of EUS-guided hepatico-gastrostomy and percutaneous transhepatic biliary drainage for malignant obstructive jaundice after failed ERCP [abstract] Gastrointest Endosc. 2016;83:AB522–3. [Google Scholar]
- 24.Lee TH, Choi JH, Park do H, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2016;14:1011–9. doi: 10.1016/j.cgh.2015.12.032. [DOI] [PubMed] [Google Scholar]
- 25.Ogura T, Okuda A, Miyano A, et al. EUS-guided versus percutaneous biliary access in patients with obstructive jaundice due to gastric cancer. Dig Liver Dis. 2019;51:247–52. doi: 10.1016/j.dld.2018.09.015. [DOI] [PubMed] [Google Scholar]
- 26.Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: A systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904–14. doi: 10.1016/j.gie.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 27.Ngamruengphong S, Hajiyeve G, Ismail A, et al. Cost-effectiveness analysis of endoscopic ultrasound-guided biliary drainage (EGBD) versus percutaneous transheptatic biliary drainage (PTBD) for malignant biliary obstruction after failed ERCP. Gastroenterology. 2016;150:S634. [Google Scholar]
- 28.Tyberg A, Desai AP, Kumta NA, et al. EUS-guided biliary drainage after failed ERCP: A novel algorithm individualized based on patient anatomy. Gastrointest Endosc. 2016;84:941–6. doi: 10.1016/j.gie.2016.05.035. [DOI] [PubMed] [Google Scholar]
- 29.Minaga K, Ogura T, Shiomi H, et al. Comparison of the efficacy and safety of endoscopic ultrasound-guided choledochoduodenostomy and hepaticogastrostomy for malignant distal biliary obstruction: Multicenter, randomized, clinical trial. Dig Endosc. 2019 doi: 10.1111/den.13406. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.DeBenedet AT, Elmunzer BJ, McCarthy ST, et al. Intraprocedural quality in endoscopic retrograde cholangiopancreatography: A meta-analysis. Am J Gastroenterol. 2013;108:1696–704. doi: 10.1038/ajg.2013.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kasmin FE, Cohen D, Batra S, et al. Needle-knife sphincterotomy in a tertiary referral center: Efficacy and complications. Gastrointest Endosc. 1996;44:48–53. doi: 10.1016/s0016-5107(96)70228-6. [DOI] [PubMed] [Google Scholar]
- 32.Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–18. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 33.Dhir V, Swaroop VS, Mohandas KM, et al. Precut papillotomy using a needle knife: Experience in 100 patients with malignant obstructive jaundice. Indian J Gastroenterol. 1997;16:52–3. [PubMed] [Google Scholar]
- 34.Rabenstein T, Ruppert T, Schneider HT, et al. Benefits and risks of needle-knife papillotomy. Gastrointest Endosc. 1997;46:207–11. doi: 10.1016/s0016-5107(97)70087-7. [DOI] [PubMed] [Google Scholar]
- 35.Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc. 1998;48:1–10. doi: 10.1016/s0016-5107(98)70121-x. [DOI] [PubMed] [Google Scholar]
- 36.Rollhauser C, Johnson M, Al-Kawas FH. Needle-knife papillotomy: A helpful and safe adjunct to endoscopic retrograde cholangiopancreatography in a selected population. Endoscopy. 1998;30:691–6. doi: 10.1055/s-2007-1001390. [DOI] [PubMed] [Google Scholar]
- 37.Siegel JH. Precut papillotomy: A method to improve success of ERCP and papillotomy. Endoscopy. 1980;12:130–3. doi: 10.1055/s-2007-1021728. [DOI] [PubMed] [Google Scholar]
- 38.Goff JS. Common bile duct pre-cut sphincterotomy: Transpancreatic sphincter approach. Gastrointest Endosc. 1995;41:502–5. doi: 10.1016/s0016-5107(05)80011-2. [DOI] [PubMed] [Google Scholar]
- 39.Zang J, Zhang C, Gao J. Guidewire-assisted transpancreatic sphincterotomy for difficult biliary cannulation: A prospective randomized controlled trial. Surg Laparosc Endosc Percutan Tech. 2014;24:429–33. doi: 10.1097/SLE.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 40.Lee A, Aditi A, Bhat YM, et al. Endoscopic ultrasound-guided biliary access versus precut papillotomy in patients with failed biliary cannulation: A retrospective study. Endoscopy. 2017;49:146–53. doi: 10.1055/s-0042-120995. [DOI] [PubMed] [Google Scholar]


