Abstract
Purpose
To evaluate the correlation of corneal elevation and difference elevation with severity of keratoconus.
Methods
Anterior and posterior corneal elevations with both conventional and enhanced best-fit spheres (using rotating Scheimpflug camera) were measured. Front and back difference elevation were extrapolated from difference map of Belin/Ambrỏsio Enhanced Ectasia Display of the Scheimpflug system. Data from corneal elevations and difference elevations were correlated with maximum keratometry, minimal corneal thickness, and severity of keratoconus as assessed by Amsler-Krumiech classification of keratoconus.
Results
Ninety eyes of 55 keratoconus patients of different clinical stages were evaluated. There was a significant positive correlation between keratoconus severity and corneal elevations (anterior and posterior elevation as measured with both conventional and enhanced best-fit spheres) and also between keratoconus severity and corneal elevation differences (P < 0.001 and r > 0.625 for all). Maximum keratometry (Kmax), mean keratometry (Kmean), and all corneal elevations and difference elevations were highly correlated (P < 0.001 and r > 0.840 for all). A significant negative correlation was found between minimum corneal thickness and all corneal elevations and difference elevations (P < 0.001 and r < 0.711 for all). Receiver operating characteristic (ROC) curve analyses showed that anterior and posterior difference elevations have the best predictive accuracy for grading keratoconus severity.
Conclusion
Evaluation of corneal elevation and difference elevation data obtained from Scheimpflug corneal imaging is useful for grading severity of keratoconus.
Keywords: Keratoconus, Corneal elevation, Corneal difference elevation, Pentacam
Introduction
Keratoconus is a bilateral non-inflammatory corneal thinning disorder leading to cone-like protrusion of the central cornea and decreased vision because of myopia, irregular astigmatism, and corneal scarring. Keratoconus is diagnosed clinically with biomicroscopic examination of the cornea.1 Placido disk–based corneal topography which has been traditionally used to diagnose keratoconus evaluates only the anterior corneal surface.2
Evaluation of the posterior corneal surface which has been made possible by Scheimpflug imaging and slit-scanning topography is especially important for detection of subclinical and early keratoconus.3, 4, 5 Pentacam as a rotating Scheimpflug imaging instrument measures both surfaces’ elevation by fitting the best-possible sphere to both surfaces of the cornea, which can miss small protrusions on the posterior cornea because the cone or apical protrusion steepens the best fit sphere (BFS), and this steepened BFS minimizes the elevation difference between the apex of the cone and the BFS.6 A Software known as Belin/Ambrỏsio Enhanced Ectasia Display overcomes this problem by utilizing an enhanced reference which excludes thinnest portion of cornea from calculation of reference shape.7 In conical cornea, this enhanced reference results in a significantly flatter BFS based more on the normal peripheral cornea. The map generated this way is known as exclusion map. The difference maps (anterior and posterior) show the relative change in elevation from the baseline elevation map to the exclusion map. Although this software was originally invented to rule out the possibility of forme fruste keratoconus before laser keratorefractive surgeries, it seems that this software may have some other utilities, especially in keratoconus patients.
As different treatment modalities have been developed in recent years for management of keratoconus patients,8, 9, 10 precise assessment of keratoconus severity is important in the management of these patients. The aim of this study was to evaluate the correlation of corneal elevation and difference elevation as measured by Scheimpflug corneal imaging with severity of keratoconus. Corneal elevations were measured with both conventional and enhanced BFSs and difference elevations were extrapolated from difference map of Belin/Ambrỏsio Enhanced Ectasia Display of the Scheimpflug system.
Methods
In this cross-sectional study, patients referred to the Cornea Clinic, Amiralmomenin Hospital, Guilan University of Medical Sciences, were enrolled from September 2013 to February 2014. The study was performed in accordance with the Declaration of Helsinki, and the protocol of the study was approved by the Ethics Committee of Guilan University of Medical Sciences. All patients were provided informed consent.
Keratoconus was defined as at least one keratoconus sign (eg, stromal thinning, conical protrusion of the cornea at the apex, Fleischer ring, Vogt striae, or anterior stromal scar) on slit-lamp examination in addition to the topographic findings.
Using rotating Scheimpflug camera (Pentacam® HR Typ70900; oculus D-35582 Wetzlar, made in Germany), anterior and posterior corneal elevations with both conventional and enhanced BFS camera were measured. Enhanced BFS were calculated from Belin/Ambrỏsio Enhanced Ectasia Display software of Pentacam system. Elevation differences which are the differential change of elevation between the BFS and enhanced BFS were also extrapolated from this map. Exclusion criteria were eyes with post refractive surgery ectasia, pellucid marginal degeneration, pellucid like keratoconus, and any history of anterior segment surgery.
Severity of keratoconus was graded according to Amsler–Krumeich classification (Table 1).11 Data from corneal elevations and difference elevations were correlated with maximum keratometry, minimal corneal thickness, and severity of keratoconus using spearman correlation. A probability of 0.05 was regarded as statistically significant.
Table 1.
Amsler–Krumeich classification.11
| Severity | Mean keratometry (Kmean) (D) | Thickness (μ) | Spherical equivalent | Cornea |
|---|---|---|---|---|
| IV | >55 | <200 | Not measurable | Central scars |
| III | 54–55 | 200–400 | > − 8D | No central scars |
| II | 48–53 | 400–500 | [–5,−8]D | No central scars |
| I | <48 | >500 | < − 5D | No central scars |
D: Diopter.
Results
90 eyes of 55 keratoconus patients (63 male and 27 female eyes) of different clinical stages were enrolled in this cross-sectional study. Mean patient age was 24.16 ± 7.2 years. Considering Amsler–Krumeich classification, 30 eyes were in stage I, 25 in stage II, 26 in stage III, and 9 in stage IV of keratoconus severity. There was a significant positive correlation between keratoconus severity and corneal elevations (anterior and posterior elevation as measured with both conventional and enhanced BFS) and also between keratoconus severity and corneal elevation differences (P < 0.001 and r > 0.625 for all) (Table 2).
Table 2.
Correlation of cornea variables and keratoconus severity.
| Anterior elevation (Regular BFS) | Anterior elevation (Enhanced) | Posterior elevation (Regular BFS) | Posterior elevation (Enhanced) | Anterior elevation differences | Posterior elevation differences | ||
|---|---|---|---|---|---|---|---|
| Keratoconus severity | P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Spearman correlation | 0.683 | 0.727 | 0.625 | 0.730 | 0.786 | 0.771 | |
BFS: Best fit sphere.
The correlation between maximum keratometry (Kmax), mean keratometry (Kmean), minimal corneal thickness (as Pentacam indices of corneal severity assessment), and corneal elevations has been shown in Table 3. Kmax, Kmean, and all corneal elevations and difference elevations were highly correlated (P < 0.001 and r > 0.840 for all). A significant negative correlation was found between minimum corneal thickness and all corneal elevations and difference elevations (P < 0.001 and r < −0.711 for all).
Table 3.
Correlation of maximum keratometry (Kmax), mean keratometry (Kmean), minimum corneal thickness, and all corneal elevations and difference elevations.
| Variable | Kmax |
Kmean |
Thinnest point thickness |
|||
|---|---|---|---|---|---|---|
| Spearman correlation | P-value | Spearman correlation | P-value | Spearman correlation | P-value | |
| Anterior elevation (Regular BFS) | 0.916 | <0.001 | 0.844 | <0.001 | −0.743 | <0.001 |
| Posterior elevation (Regular BFS) | 0.895 | <0.001 | 0.844 | <0.001 | −0.711 | <0.001 |
| Anterior elevation (Enhanced) | 0.952 | <0.001 | 0.905 | <0.001 | −0.711 | <0.001 |
| Posterior elevation (Enhanced) | 0.931 | <0.001 | 0.905 | <0.001 | −0.730 | <0.001 |
| Anterior elevation differences | 0.950 | <0.001 | 0.933 | <0.001 | −0.756 | <0.001 |
| Posterior elevation differences | 0.921 | <0.001 | 0.916 | <0.001 | −0.718 | <0.001 |
BFS: Best fit sphere; Kmax: Maximum keratometry; Kmean: Mean keratometry.
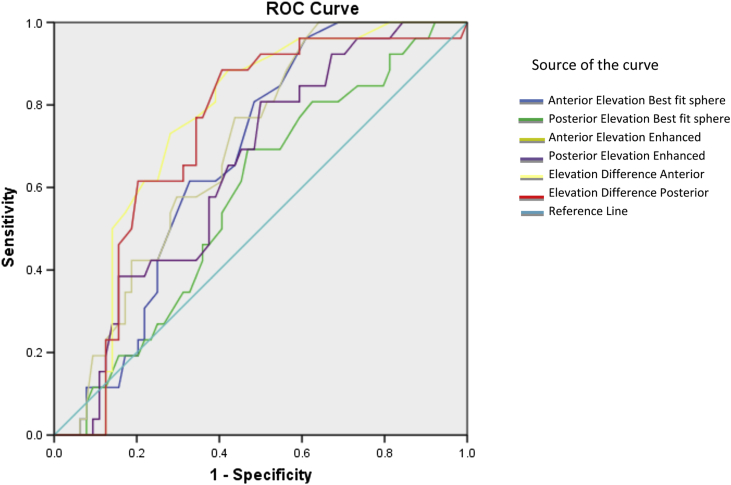
Fig. 1 shows receiver operating characteristic (ROC) curve analyses of all corneal elevations and difference elevations with reference to keratoconus staging (according to the Amsler–Krumeich classification) and indicates that anterior and posterior difference elevations have the best area under curve (AUC) in this regard.
Fig. 1.
Receiver operating characteristic (ROC) curve showed the sensitivity and specificity of the elevation differences. Data points in the upper left portion of the graph represent higher sensitivity and specificity. Area under curve (AUC) as close as 1.0 is better in diagnostic ability.
We preformed ROC curve analyses to assess the predictive accuracy of anterior and posterior corneal elevation differences in discriminating different stages of keratoconus, the result of which is shown in Table 4. The results indicate that its predictive accuracy is good for discriminating stage II from III and III from IV but not stage I from II.
Table 4.
Receiver operating characteristic (ROC) curve analyses of anterior and posterior corneal elevation differences in discriminating different stages of keratoconus.
| Area under the curve |
Sensitivity | Specificity | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Keratoconus severity | Variables | Area | Std. errora | Asymptotic Sig.b | Asymptotic 95% confidence interval |
Cut off optimal | |||
| Lower bound | Upper bound | ||||||||
| Grade i-ii | Elevation difference anterior | 0.454 | 0.058 | 0.496 | 0.339 | 0.568 | – | – | – |
| Elevation difference posterior | 0.483 | 0.059 | 0.801 | 0.367 | 0.599 | – | – | – | |
| Grade ii-iii | Elevation difference anterior | 0.753 | 0.052 | 0.000 | 0.651 | 0.855 | 19.5 μm | 73% | 72% |
| Elevation difference posterior | 0.730 | 0.056 | 0.001 | 0.621 | 0.840 | 37.5 μm | 80% | 63% | |
| Grade iii-iV | Elevation difference anterior | 0.995 | 0.006 | 0.000 | 0.982 | 1.000 | 32 μm | 100% | 96% |
| Elevation difference posterior | 0.991 | 0.010 | 0.000 | 0.972 | 1.000 | 64 μm | 100% | 92% | |
Standard deviation error.
Asymptotic significant.
Discussion
Although Amsler–Krumeich classification has been traditionally used for grading keratoconus severity, recently many other methods including topographic data,12, 13, 14, 15 higher-order aberrations,11 combinations of topographic pattern, and slit-lamp evaluation have been evaluated in this regard.16
As mentioned above, the aim of this study was to evaluate the correlation of corneal elevation and difference elevation (extrapolated from Belin/Ambrỏsio EnhancedEctasia Display of the Scheimpflug system) with severity of keratoconus. The result of this study demonstrates significant positive correlation between keratoconus severity and corneal elevations (anterior and posterior elevation as measured with both conventional and enhanced best-fit spheres) and also between keratoconus severity and corneal elevation differences. ROC curve analyses showed that anterior and posterior difference elevations have the best AUC with reference to keratoconic staging, indicating that corneal elevation differences extrapolated from BAD display of Pentacam have the best predictive accuracy for keratoconus grading.
Ishii et al.17 evaluated the correlation between anterior and posterior elevation differences and keratoconus severity and showed positive correlation between them (Pearson correlation coefficient, r = 0.66; P < 0.001; r = 0.74; P < 0.001, respectively. Their study revealed a significant correlation between Keratoconus Severity Index (KSI) and Amsler–Krumeich classification and the elevation differences, but they did not evaluate correlation of corneal elevations with keratoconus severity. Du et al.18 reported that in the subclinical stage of keratoconus, posterior elevation value (PEV), thickness, and posterior I-S had important diagnostic values, and elevation values remained most efficient when keratoconus developed to the moderate stage. The anterior curvature indices were most characteristic when keratoconus became severe. Keratoconus first appeared in the inferior cornea of posterior surface, but the feature of protrusion formed at the moderate stage.
In the study performed by Miháltz et al.,19 the keratometric, pachymetric, and elevation parameters of keratoconic and normal corneas (all measured by Pentacam) were evaluated. ROC curve analyses showed the best predictive accuracy for posterior and anterior elevation (area under the curve, 0.97 and 0.96) followed by minimal and central pachymetry (0.89 and 0.88), again emphasizing the clinical significance of elevation data. Falavarjani et al.20 stated that in normal population, the mean interocular difference was 2.17 μm for maximum anterior elevation and 3.62 μm for maximum posterior elevation. One study previously reported that corneal elevation differences were significantly correlated with the keratoconus severity index, suggesting that corneal height information was also useful for indicating keratoconus severity.17 Piñero et al. reported that the anterior and posterior BFS measurements were highly correlated in the healthy eyes and subclinical groups, but that the correlation was weaker in the two clinical keratoconus groups.21
In conclusion, according to our study, the measurements of anterior and posterior elevation differences were effective indices in aiding for grading severity of keratoconus in moderate and advanced stages (II-IV). Our study also showed the best predictive accuracy is for anterior and posterior difference elevations in this regard.
Acknowledgements
Authors would like to acknowledge Shila Kianmehr, the manager of Eye Research Center, Guilan University of Medical Sciences, for her great contribution to this study.
Footnotes
We state that our only interest is academic and we have no financial interest in this publication and our research is not funded from any organization.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Soltani Moghadam R., Akbari M., Alizadeh Y., Medghalchi A., Dalvandi R. The outcome of corneal collagen cross-linking in patients with advanced progressive keratoconus: a 2-year follow-up study. 2019;26(1):11–16. doi: 10.4103/meajo.MEAJO_101_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krachmer J.H., Feder R.S., Belin M.W. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 3.Rao S.N., Raviv T., Majmudar P.A., Epstein R.J. Role of Orbscan II in screening keratoconus suspects before refractive corneal surgery. Ophthalmology. 2002;109(9):1642–1646. doi: 10.1016/s0161-6420(02)01121-1. [DOI] [PubMed] [Google Scholar]
- 4.Schlegel Z., Hoang-Xuan T., Gatinel D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg. 2008;34(5):789–795. doi: 10.1016/j.jcrs.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 5.de Sanctis U., Loiacono C., Richiardi L., Turco D., Mutani B., Grignolo F.M. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminate keratoconus/subclinical keratoconus. Ophthalmology. 2008;115(9):1534–1539. doi: 10.1016/j.ophtha.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 6.Belin M.W., Khachikian S.S. An introduction to understanding elevation-based topography: how elevation data are displayed – a review. Clin Exp Ophthalmol. 2009;37(1):14–29. doi: 10.1111/j.1442-9071.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 7.Belin M.W., Khachikian S.S. New Advances and Technology With Pentacam. Oculus Optikgerate GmbH; Wetzlar, Germany: 2013. Keratoconus/ectasia detection with the Oculus Pentacam: Belin/Ambrosi_o enhanced ectasia display; pp. 3–7.http://www.oculus.de/en/downloads/dyn/oculus/presse/158/oculus_low_res.pdf Available at: [Google Scholar]
- 8.Torquetti L., Ferrara G., Almeida F. Intrastromal corneal ring segments implantation in patients with keratoconus: 10-year follow-up. J Refract Surg. 2014;30(1):22–26. doi: 10.3928/1081597X-20131217-02. [DOI] [PubMed] [Google Scholar]
- 9.Raiskup F., Theuring A., Pillunat L.E., Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41(1):41–46. doi: 10.1016/j.jcrs.2014.09.033. [DOI] [PubMed] [Google Scholar]
- 10.Anwar M., Teichmann K.D. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002;21(4):374–383. doi: 10.1097/00003226-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Alió J.L., Shabayek M.H. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg. 2006;22(6):539–545. doi: 10.3928/1081-597X-20060601-05. [DOI] [PubMed] [Google Scholar]
- 12.Gupta N., Trindade B.L., Hooshmand J., Chan E. Variation in the best fit sphere radius of curvature as a test to detect keratoconus progression on a Scheimpflug-based corneal tomographer. J Refract Surg. 2018;34(4):260–263. doi: 10.3928/1081597X-20180206-03. [DOI] [PubMed] [Google Scholar]
- 13.Bae G.H., Kim J.R., Kim C.H., Lim D.H., Chung E.S., Chung T.Y. Corneal topographic and tomographic analysis of fellow eyes in unilateral keratoconus patients using Pentacam. Am J Ophthalmol. 2014;157(1):103–109. doi: 10.1016/j.ajo.2013.08.014. e1. [DOI] [PubMed] [Google Scholar]
- 14.Huseynli S., Abdulaliyeva F. Evaluation of Scheimpflug tomography parameters in subclinical keratoconus, clinical keratoconus and normal Caucasian eyes. Turk J Ophthalmol. 2018;48(3):99–108. doi: 10.4274/tjo.89587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safarzadeh M., Nasiri N. Anterior segment characteristics in normal and keratoconus eyes evaluated with a combined Scheimpflug/Placido corneal imaging device. J Curr Ophthalmol. 2016;28(3):106–111. doi: 10.1016/j.joco.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rabinowitz Y.S. Corneal Topography. In: Bennett E.S., Weissman B.A., editors. Clinical Contact Lens Practice. Lippincott, Wlliams and Wilkins; Philadelphia, PA: 2005. pp. 215–232. [Google Scholar]
- 17.Ishii R., Kamiya K., Igarashi A., Shimizu K., Utsumi Y., Kumanomido T. Correlation of corneal elevation with Severity of keratoconus by means of anterior and posterior topographic analysis. Cornea. 2012;31(3):253–258. doi: 10.1097/ICO.0B013E31823D1EE0. [DOI] [PubMed] [Google Scholar]
- 18.Du X.L., Chen M., Xie L.X. Correlation of basic indicators with stages of keratoconus assessed by Pentacam tomography. Int J Ophthalmol. 2015;8(6):1136–1140. doi: 10.3980/j.issn.2222-3959.2015.06.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miháltz K., Kovács I., Takács A., Nagy Z.Z. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with pentacam. Cornea. 2009;28(9):976–980. doi: 10.1097/ICO.0b013e31819e34de. [DOI] [PubMed] [Google Scholar]
- 20.Falavarjani K.G., Modarres M., Joshaghani M., Azadi P., Afshar A.E., Hodjat P. Interocular differences of the Pentacam measurements in normal subjects. Clin Exp Optom. 2010;93(1):26–30. doi: 10.1111/j.1444-0938.2009.00446.x. [DOI] [PubMed] [Google Scholar]
- 21.Piñero D.P., Alió J.L., Alesón A., Escaf Vergara M., Miranda M. Corneal volume, pachymetry, and correlation of anterior and posterior corneal shape in subclinical and different stages of clinical keratoconus. J Cataract Refract Surg. 2010;36(5):814–825. doi: 10.1016/j.jcrs.2009.11.012. [DOI] [PubMed] [Google Scholar]