Abstract
Purpose
To compare the effect of amblyopia therapy on cases who received interactive binocular treatment (I-BiT™) with those who received standard patching of the dominant eye with placebo I-BiT™.
Methods
In this randomized clinical trial, 38 unilateral amblyopic children (3–10 years old) were studied. All unilateral amblyopic children who had best corrected visual acuity (BCVA) worse than 0.30 logMAR or a difference of two Snellen lines of BCVA between their two eyes were included, and children who did not complete at least 75% of amblyopia treatment were excluded from this study. Eventually, a total of 19 and 21 subjects were included in case and control groups, respectively. Cases played I-BiT™ games, while controls had standard patch therapy and played with placebo I-BiT™ games, both for one month. All subjects were examined at baseline and after one-month therapy.
Results
BCVA improved significantly in both groups after one-month treatment (case: P = 0.003, control: P < 0.001), while in comparison with each other, there was not any difference between them (P = 0.52). Although stereopsis improved in the case (P < 0.001) and control (P < 0.001), there was no significant difference between them pre and post-therapy. Our children played games for about 6 h total during one month in both groups, and their compliance was 87.5% and 76% in cases and controls, respectively. Two children were excluded due to their lower compliance of playing I-BiT™ games (n = 38).
Conclusions
I-BiT™ game and patching with placebo game had similar BCVA improvement in amblyopic children after one-month treatment. It is suggested to conduct further randomized clinical trials with a larger sample size and longer duration of study and assessment of its recurrence.
Keywords: Amblyopia, Interactive binocular treatment, I-BiT™, Patch therapy
Introduction
Amblyopia is defined as uni- or bilateral decreased best corrected visual acuity (BCVA) with no ocular pathologic or anatomic concern.1 It has been reported as the most common cause of unilateral reduced vision among children and young adults living in Central Europe.2 Amblyopia prevalence is varied from 0.51% to 3.67% based on different epidemiological reports.3 Amblyopia could be mild (20/25 to 20/40), moderate (20/50 to 20/100), and severe (worse than 20/100 logMAR).1, 2, 4
Although various therapies have been suggested for management of amblyopia, patching of the dominant eye is a gold standard modality which has been recommended as the first line of amblyopia treatment.5, 6 Lower compliance of children, necessity of long-term patching, and also lower rate of success in the severe amblyopic cases can be considered some drawbacks of ocular patching.7 In addition, occlusion of one eye causes disruption of the binocular fusion, and strabismus may be manifested consequently.8 Therefore, an updated modality of amblyopia therapy which is named interactive binocular treatment (I-BiT™) has been introduced based on different mechanisms of 1) presenting fine and movable stimulus to the amblyopic eye and the fixed targets or background to the dominant eye,7, 9 2) showing the half of one image to each eye simultaneously, 3) demonstrating identical images to both eyes with small retinal disparity. One of the advantages of I-BiT™ system is the possibility of adjusting its illumination and image contrast according to the patient's BCVA, and it is effective even in individuals aged beyond the limitation of amblyopia therapy.8 The simultaneous stimulus presentation to both eyes without ocular occlusion is the crucial positive point of I-BiT™ system for preserving of the binocular fusion.7, 8, 9, 10
In a study on 39 amblyopic patients, BCVA improvement was noted in 87% of cases after an average of 6 months of I-BiT™ treatment.7 In another study by the author, it was revealed that I-BiT™ can be beneficial as a complementary treatment of patching and no manifestation of amblyopia recurrence was noted after one month following cessation of I-BiT™ treatment.9 In the present study, we aimed to investigate the effect of amblyopia therapy on cases who received I-BiT™ without patching compared with those who received patching with placebo game.
Methods
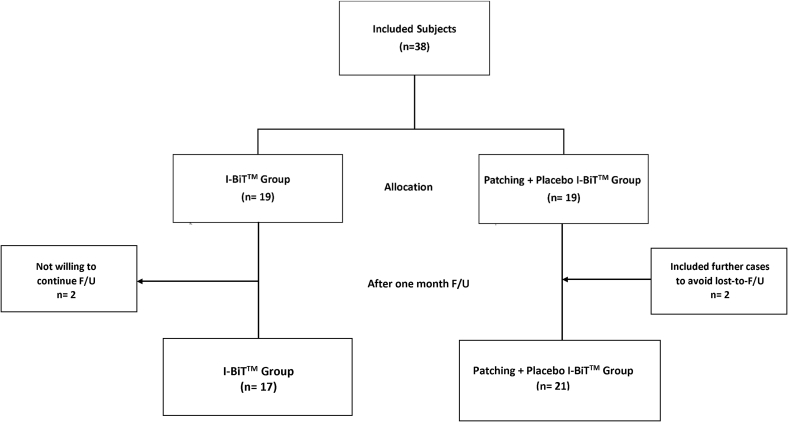
In this randomized clinical trial, 38 unilateral amblyopic children (3–10 years) referring to the tertiary referral center from January 2017 to March 2018 were studied. The study was approved by the Ethics Committee of the School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran. An informed consent, which explained the details of our project, was signed by parents of these children before any intervention. This study conformed to all local rules and complied with the principles of Declaration of Helsinki. Our study was registered at https://register.clinicaltrials.gov by a registration number of NCT03940222. All functional amblyopic children who had BCVA less than 20/30 (0.3 logMAR) in one eye or a difference of two lines of Snellen between their two eyes were included in this study and randomly divided into the case (n = 19) and control (n = 21) groups (Fig. 1). According to the literature, the difference of two lines of BCVA between two eyes was defined as amblyopia. We also defined similar decreased vision for amblyopia in each eye. For instance, the left eye was considered amblyopic for BCVA 20/20 and 20/30 in right and left eyes, respectively, since it has two lines less BCVA on Snellen chart. Moderate amblyopia definition was between BCVAs from 20/50 to 20/100.4
Fig. 1.
Flowchart of our study. I-BiT™: Interactive binocular treatment; F/U: Follow-up; n: Number.
Children with a history of penalization one month prior to the study, bilateral amblyopia, BCVA less than 20/200, eccentric fixation, nystagmus, ocular deviation more than 10 prism diopter (pd), and organic amblyopia, as well as uncooperative children who were not eager to play the games or those with mental and physical disability and systemic diseases were excluded from our study. Any child who did not complete at least 75% of treatment in both groups was excluded as well. Cases had I-BiT™ games, while controls had patching with placebo game for one month.
In the present study, randomization was performed using the permuted-block method with the block length variation between 2 and 6. This study step was conducted using a computer program, and the sequence of randomization was not revealed to investigators.
To have a power of 80% to detect 0.10 logMAR difference between the two groups when the standard deviation of BCVA between them was assumed to be 0.11 logMAR, a sample size of 19 in each group was calculated.
Initially, all study subjects underwent cycloplegic refraction 30–45 min after instillation of one drop of cyclopentolate 1% and tropicamide 1% with 5 min interval. Afterwards, BCVA was measured 48 h following cycloplegia using a Yang Vision Tester instrument (SIFI Diagnostic S.P.A-Via Castellana, 70/e−31100 T revise-Italy) with the Snellen E-chart containing 5 letters in each line at a 6 m distance under daylight condition. Anisometropia was defined as spherical equivalent difference ≥1.50 diopter (D) between the two eyes. Ocular alignment was evaluated using an alternative prism cover test or Krimsky method (for uncooperative cases) at both far (6 m) and near (33 cm) distances. In addition, the function of extraocular muscles was assessed through duction and version movements by the scale of −4 underaction to +4 overaction grades. Furthermore, fixation quality was evaluated by monocular visuoscope examination. Finally, the anterior and posterior ocular segments were evaluated by slit-lamp and indirect ophthalmoscope (HEINE BETA 200; US) in order to diagnose pathologic lesions. Stereopsis was also measured by Titmus steroacuity test at near distance under day light condition. The BCVA and stereopsis measurements were repeated after one month of I-BiT™ and patching treatments and were compared with their initial value(s) in each group and between the two groups as well.
Four months after wearing new prescription if amblyopia was already left, the patient began the study, while this period was reduced to one month for patients who did not need any new prescription but had previous patching. In the case group, they were recommended to play the games using red-green glasses, 20–30 min per a day for at least five days in a week for one month (total hours = 6).
In the control group, 2 and 4 h patching of dominant eye per a day were recommended for mild and moderate amblyopia, respectively, accompanied by I-BiT™ games with no red-green glasses, 20–30 min per a day for at least five days in a week for one month. I-BiT™ software was designed according to the known strategy in which the dominant eye sees the fixed target, but the amblyopic eye follows the moving object through the conjugate colored filters, including red (Wratten≠25) and green (Wratten≠58), that are positioned in the glasses in order to dissociate the eyes of each subject while both eyes are watching simultaneously. In children with corrective glasses, the filters were set on their glasses. Software was designed the same as the previous study9 although more games (n = 7) with higher diversity were applied in this study to attract the child's cooperation. (The previous study had only 3 games.)
Each child was detected by one code and monitored by the office of engineer who was going to check all dates and time of playing. Compliance of our cases and controls were also recorded by the mentioned system and parents' response.
BCVA and stereopsis of all patients in both groups were measured one month after I-BiT and patching with placebo game therapy.
To assess the normal distribution of data, Kolmogorove-Smirnov test and Q-Q plot were used. To present data, we used mean, standard deviation, median and range, frequency, and percent. To compare the baseline characteristics of participants, we used T-test, Mann-Whitney U test, Chi-Square, and Fisher Exact Test. To assess the improvement within the groups, we used linear mixed model (LMM) and multiple comparison considered by the Bonferroni method. All statistical analysis was performed by SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). P-value less than 0.05 was considered statistically significant.
Results
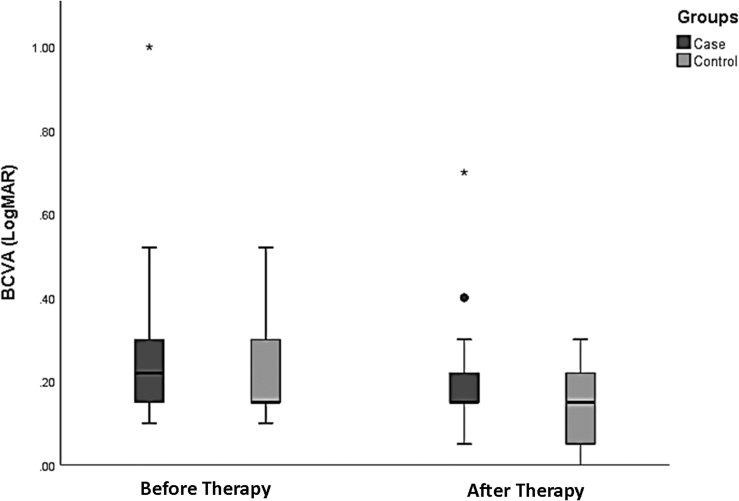
In this study, 38 unilateral amblyopic children with the mean age of 7.08 ± 1.82 years old were studied in both the case (6.5 ± 2.01 years) and control (7.55 ± 1.55 years) groups. As shown in Table 1, there was not any difference between both groups regarding their age, sex, BCVA, spherical equivalent, ocular alignment, and history of previous patching of non-amblyopic eye. The mean spherical, cylindrical, and spherical equivalent of refractive error of our patients were +3.00, −2.00, and +2.00 D, respectively. Anisometropia was seen in 11.8% of cases and 19% of controls. In the present study, 15% of cases and 20% of controls needed a new prescription. Compliances were 87.5% and 76% for case and control groups, respectively. BCVA improved significantly in both groups after one-month treatment (case: P = 0.003, control: P < 0.001), while in comparison with each other, there was not any difference between them (P = 0.52, Fig. 2).
Table 1.
Epidemiologic characteristics of the amblyopic children in case and control groups.
| Factors | Level | Total | Groups |
P-value | |
|---|---|---|---|---|---|
| I-BiTTM (n = 17) | Patching with placebo game (n = 21) | ||||
| Age (yrs) | Mean ± SD | 7.08 ± 1.82 | 6.5 ± 2.01 | 7.55 ± 1.55 | 0.078a |
| Median (range) | 7 (3.5–10) | 7 (3.5–10) | 7 (4–10) | ||
| Sex (%) | female | 22 (57.9%) | 8 (47.1%) | 14 (66.7%) | 0.324d |
| male | 16 (42.1%) | 9 (52.9%) | 7 (33.3%) | ||
| Pre. BCVA (logMAR) | Mean ± SD | 0.26 ± 0.18 | 0.29 ± 0.22 | 0.23 ± 0.13 | 0.273a |
| Median (range) | 0.22 (0.1–1) | 0.22 (0.1–1) | 0.15 (0.1–0.52) | ||
| SE (D) | Mean ± SD | 2.27 ± 2.75 | 2.12 ± 2.70 | 2.40 ± 2.81 | 0.688a |
| Median (range) | 2.25 (−5.0 to 8.0) | 2.38 (−5.0 to 7.38) | 2.06 (−3.88 to 8.0) | ||
| Deviation Far (pd) | Mean ± SD | 1.16 ± 2.4 | 1.76 ± 2.99 | 0.67 ± 1.71 | 0.139b |
| Median (range) | 0 (0–10) | 0 (0–10) | 0 (0–6) | ||
| Ocular alignment | ET < 10 | 7 (18.4%) | 5 (29.4%) | 2 (9.5%) | 0.299c |
| XT < 10 | 2 (5.3%) | 1 (5.9%) | 1 (4.8%) | ||
| Ortho | 29 (76.3%) | 11 (64.7%) | 18 (85.7%) | ||
| Hx patching | Yes | 30 (78.9%) | 16 (94.1%) | 14 (66.7%) | 0.053c |
| No | 8 (21.1%) | 1 (5.9%) | 7 (33.3%) | ||
I-BiT™: Interactive binocular treatment; BCVA: Best corrected visual acuity; SE: Spherical equivalent; D: Diopter; pd: Prism diopter; Hx: History of; SD: Standard deviation; ET: Esotropia; XT: Exotropia; n: Number.
Based on independent T-test.
Based on Mann-Whitney U test.
Based on Fisher's exact test.
Based on Chi-square test.
Fig. 2.
Best corrected visual acuity (BCVA) before and after treatment in the both case and control groups. *Asterisks show the outlier BCVA data of our participants.
Although stereopsis improved in case (P < 0.001) and control (P < 0.001), there was no significant difference between them pre- and post-therapy (Table 2).
Table 2.
Best corrected visual acuity (BCVA) and stereopsis of the amblyopic children case and control groups.
| Factors | Level | Total | Groups |
P-value | |
|---|---|---|---|---|---|
| I-BiTTM (n = 17) | Patching with placebo Game (n = 21) | ||||
| Pre-BCVA (logMAR) | Mean ± SD | 0.26 ± 0.18 | 0.29 ± 0.22 | 0.23 ± 0.13 | 0.273a |
| Median (range) | 0.22 (0.1–1) | 0.22 (0.1–1) | 0.15 (0.1–0.52) | ||
| Post-BCVA (logMAR) | Mean ± SD | 0.17 ± 0.13 | 0.22 ± 0.16 | 0.14 ± 0.1 | 0.147a |
| Median (range) | 0.05 (0.0–0.7) | 0.08 (0.0–0.7) | 0.05 (0.0–0.3) | ||
| Change of BCVA (logMAR) | Mean ± SD | −0.08 ± 0.09 | −0.08 ± 0.09 | −0.09 ± 0.09 | 0.52a |
| P-value in each group | – | 0.003 | <0.001 | ||
| Pre-stereopsis (n) | Central (≤100 s/arc) | 4 (12.5%) | 2 (11.8%) | 2 (13.3%) | >0.999b |
| Peripheral (100–3000 s/arc) | 24 (75.0%) | 13 (76.5%) | 11 (73.3%) | ||
| Suppression (≥3000 s/arc) | 4 (12.5%) | 2 (11.8%) | 2 (13.3%) | ||
| Post-stereopsis (n) | Central (≤100 s/arc) | 7 (18.4%) | 3 (17.6%) | 4 (19.0%) | >0.999b |
| Peripheral (100–3000 s/arc) | 28 (73.7%) | 13 (76.5%) | 15 (71.4%) | ||
| Suppression (≥3000 s/arc) | 3 (7.9%) | 1 (5.9%) | 2 (9.5%) | ||
| P-value in each group | – | <0.001 | <0.001 | ||
| Logarithm of stereopsis (pre) | Mean ± SD | 2.52 ± 0.42 | 2.6 ± 1.78 | 3.48 ± 2.52 | 0.93 |
| Median (range) | 2.6 (1.78–3.48) | 2.6 (1.78–3.48) | 2.6 (1.78–3.48) | ||
| Logarithm of stereopsis (post) | Mean ± SD | 2.26 ± 0.42 | 2.3 ± 1.6 | 3.48 ± 2.19 | 0.231 |
| Median (range) | 2.3 (1.6–3.48) | 2.15 (1.78–2.6) | 2.3 (1.6–3.48) | ||
| P-value in each group | 0.05 | 0.051 | |||
I-BiT™: Interactive binocular treatment; BCVA: Best corrected visual acuity; D: Standard deviation; n: Number.
Based on independent T-test.
Based on Fisher's exact test.
Discussion
In our previous study, we applied I-BiT™ and patching to the case group and standard patching to the control group,9 since ethically we had no permission to study them separately in our first experience of I-BiT™ system. After achieving a better effect in our previous case group, we aimed to study them separately in a randomized clinical trial.
Our recent result also showed no BCVA difference between the two groups. In other words, I-BiT™ treatment has resulted in equal improvement of BCVA in comparison with patching with placebo game during one-month treatment.
Although stereopsis improved in the case (P < 0.001) and control (P < 0.001), there was no significant difference between them pre- and post-therapy. Up to April 2015 on Cochrane review by Tailor et al.,11 there was no clinical trial offering standardized evidence of the safety and effectiveness of binocular treatments, but the results of non-controlled cohorts were encouraging.
Holmes et al.12 compared BCVA in 385 unilateral amblyopic children aged 5–13 years old with BCVA from 20/40 to 20/200 who were treated by part-time patching and iPad games in multicenter randomized clinical trial study for 16 weeks. BCVA improved 1.05 and 1.35 lines in iPad games and patching groups, respectively. The author claimed that the difference was due to the lack of cooperation in game playing by some children (only 22% completed the 75% of game playing time). Their study showed a better result of patching while in our study there was no difference between them. Other reasons could be the short period of our study (4 versus 16 weeks) and exclusion of any child who did not complete at least 75% of treatment (game playing or patch time).
In the study by Mezad-Koursh et al.13 on 27 amblyopic children aged 4–8 years old, BCVA improved 0.2 logMAR with playing games (n = 19, P < 0.001) by one hour per day, 6 days per week for 12 weeks with 88% compliance in comparison with the sham group monitored for 4 weeks (n = 8, P = 0.28). The result of this study also showed that BCVA improvement of 0.2 logMAR was achieved in one month, and after that, it was approximately constant up to 12 weeks. In our study, we obtained about 0.1 logMAR BCVA improvement during one-month therapy. Less BCVA achievement in our study could be due to more time of playing in Mezad-Koursh et al.'s study (60 versus 30 days, 12 versus 4 weeks, and total hours of 72 versus 6).13
Kelly et al.14 studied 28 amblyopic children, 4–9 years old, 14 of whom played iPad games and 14 of whom had standard patching care with follow-up visits of 2 and 4 weeks. At two-week visit, BCVA improved in the case group more than the control group (0.15 versus 0.07 logMAR, P = 0.02). After two weeks, all children played the games. At 4-week visit, there was no difference between children who played 2 or 4 weeks (0.17 versus 0.16 logMAR, P = 0.73). This study showed more effect of binocular games compared to patch even sooner than 4 weeks. Our results are less than this study (case = 0.08 versus control = 0.09; P=NS). The reason might be due to less time of playing games per day (60 versus 30 min, 6 days versus 5 days per week).
In Li et al. study15 on 50 amblyopic children aged 4–12 years old, 25 in each group, BCVA improved from 0.47 to 0.39 logMAR (P = 0.08) after 4 weeks game playing (4 h per weeks, P < 0.001) in comparison with the sham group with no improvement, and BCVA was stable after 3 months of cessation of treatment. In our study, improvement of BCVA was the same (P = 0.08) in our case and control groups (P < 0.003).
Holmes et al.12 from Pediatric Eye Disease Investigator Group in the multicenter randomized clinical trial study on 138 ansiometropic, strabismimic, and mixed amblyopic children, 7–12 years old by comparison of iPad game playing groups, one hour per day, 5 days per week with only optical correction group for 8 weeks, came to conclusion that there was no difference between the two groups (1.3 versus 1.7 lines in the case and control) after 4 and 8 weeks with consideration of more than 50% of subjects completing the treatments. The reason of less BCVA improvement in our study compared to this study could be due to their longer duration of study (8 versus 4 weeks).
Regarding compliance for playing games, there are reports from 22% in Holmes et al.12 and 88% (50–100%) in Mezad-Koursh et al.'s13 study. Our result in this regard was in line with other studies. Total course of study was one month in order not to deal with the fatigue of our cases and their parents and to be in range with other studies.
Although stereopsis improved in the case (P < 0.001) and control groups (P < 0.001), there was no significant difference between them pre- and post-therapy.
Applying a new style of amblyopia therapy and validity of study design (randomized clinical trial) were advantages of our study while a smaller sample size in each group, short-term therapy, and lack of follow-up were our limitations.
In conclusion, I-BiT™ game and patching with placebo game had similar BCVA improvements in amblyopic children after one-month treatment. It is suggested to conduct further randomized clinical trials with larger sample size and longer duration of study and assessment of its recurrence.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
Conflicts of interest: The authors have no conflict of interest with the subject matter of this manuscript.
References
- 1.Rajavi Z., Sabbaghi H., Baghini A.S. Prevalence of amblyopia and refractive errors among primary School children. J Ophthalmic Vis Res. 2015;10(4):408–416. doi: 10.4103/2008-322X.176909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schimitzek T., Haase W. Efficiency of a video-autorefractometer used as a screening device for amblyogenic factors. Graefes Arch Clin Exp Ophthalmol. 2002;240(9):710–716. doi: 10.1007/s00417-002-0524-5. [DOI] [PubMed] [Google Scholar]
- 3.Hashemi H., Pakzad R., Yekta A. Global and regional estimates of prevalence of amblyopia: a systematic review and meta-analysis. Strabismus. 2018:1–16. doi: 10.1080/09273972.2018.1500618. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 4.Petroysan T. Amblyopia: the Pathophysiology behind it and its Treatment. Am Optom Assoc. 2016 www.aoa.org Page 2. Retrieved from: [Google Scholar]
- 5.Cleary M. Effecicacy of occlusion for strabismic amblyopia: can an optimal duration be identified? Br J Ophthalmol. 2000;84(6):572–578. doi: 10.1136/bjo.84.6.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loudon S.E., Polling J.R., Simonsz H.J. A preliminary report of about the relation between visual acuity increase and compliance in patching therapy for amblyopia. Strabismus. 2002;10(2):79–82. doi: 10.1076/stra.10.2.79.8143. [DOI] [PubMed] [Google Scholar]
- 7.Waddingham P.E., Cobb S.V., Eastgate R.M., Gregson R.M. Virtual reality for interactive binocular treatment of amblyopia. Int J Disabil Hum Dev. 2006;5(2):155–162. [Google Scholar]
- 8.Eastgate R.M., Griffiths G.D., Waddingham P.E. Modified virtual reality technology for treatment of amblyopia. Eye. 2006;20(3):370–374. doi: 10.1038/sj.eye.6701882. [DOI] [PubMed] [Google Scholar]
- 9.Rajavi Z., Sabbaghi H., Amini Sharifi E., Behradfar N., Yaseri M. The role of Interactive Binocular Treatment system in amblyopia therapy. J Curr Ophthalmol. 2016 Aug 9;28(4):217–222. doi: 10.1016/j.joco.2016.07.005. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waddingham P.E., Butler T.K.H., Cobb S.V. Preliminary results from the use of the novel interactive Binocular Treatment (I-BiTTM) system, in the treatment of strabismic and anisometropic amblyopia. Eye. 2006;20(3):375–378. doi: 10.1038/sj.eye.6701883. [DOI] [PubMed] [Google Scholar]
- 11.Tailor V., Bossi M., Bunce C., Greenwood J.A., Dahlmann-Noor A. Binocular versus standard occlusion or blurring treatment for unilateral amblyopia in children aged three to eight years. Cochrane Database Syst Rev. 2015;8:CD011347. doi: 10.1002/14651858.CD011347.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes J.M., Manh V.M., Lazar E.L. Effect of a binocular iPad game vs part-time patching in children aged 5 to 12 Years with amblyopia: a randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1391–1400. doi: 10.1001/jamaophthalmol.2016.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mezad-Koursh D., Rosenblatt A., Newman H., Stolovitch C. Home use of binocular dichoptic video content device for treatment of amblyopia: a pilot study. J AAPOS. 2018;22(2):134–138. doi: 10.1016/j.jaapos.2017.12.012. e4. [DOI] [PubMed] [Google Scholar]
- 14.Kelly K.R., Jost R.M., Dao L., Beauchamp C.L., Leffler J.N., Birch E.E. Binocular iPad game vs patching for treatment of amblyopia in children: a randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1402–1408. doi: 10.1001/jamaophthalmol.2016.4224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li S.L., Jost R.M., Morale S.E. A binocular iPad treatment for amblyopic children. Eye (Lond) 2014;28(10):1246–1253. doi: 10.1038/eye.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]