ABSTRACT
Background: Humanitarian workers operate in traumatic contexts, putting them at an increased risk of adverse mental health outcomes. The quality of the support they receive from their organization, their supervisor, and team members are proposed as determinants of mental illness and well-being, via the stress-appraisal process.
Objective: Grounded in organizational support theory, we sought to understand the relationship between organizational factors, including perceived organizational support, supervisor support, and team support, and indicators of both adverse mental health and mental well-being among humanitarian volunteers. This relationship is hypothesized to be mediated by the perceived psychological stress.
Methods: A sample of 409 humanitarian volunteers from the Sudanese Red Crescent Society completed an online, anonymous, survey comprised of the Perceived Supervision, Perceived Organizational Support, Team Support, and Perceived Psychological Stress scales, as well as the Generalized Anxiety Disorder and Patient Health Questionnaire scales, (GAD-7 and PHQ- 8), and the Warwick-Edinburgh Mental Well-being Scale. Study objectives were tested using structural equation modelling (SEM) procedures.
Results: Perceived helplessness (PH) and perceived self-efficacy (PSE), as measures of psychological stress, were both found to fully mediate the relationship between perceived organizational support and mental health outcomes. Perceived organizational support was associated with PSE and inversely with PH. PH was associated with adverse mental health and inversely related to mental well-being. PSE was only associated with mental well-being. Perceived supervision was negatively associated with PSE.
Conclusions: Perceived organizational support is a key determinant of the mental health of humanitarian volunteers, with greater perceived support associated with lower distress symptomology and greater mental well-being. Humanitarian agencies should take actions to improve their internal organization support systems to mitigate the stress associated with working in traumatic contexts. Specifically, more attention should be paid to the organizational support of the volunteers as front-line workers in humanitarian settings.
KEYWORDS: Volunteer, humanitarian workers, organizational support, work-related stress, well-being, mental health, Sudan, emergency contexts
HIGHLIGHTS: • Perceived organizational support is associated with both negative and positive aspects of humanitarian volunteers’ mental health.• Perceived psychological stress factors, including perceived helplessness and perceived self-efficacy, mediate the relationship between perceived organizational support and mental health.• Supervision and team support, as key components of managerial systems, are essential contributors to perceived organizational support within the humanitarian sector.• Organizational support theory is a useful framework to understand how organizational factors contribute to the well-being of humanitarian workers, especially volunteers.
Antecedentes: Los trabajadores humanitarios operan en contextos traumáticos, lo que los pone en un mayor riesgo de resultados adversos para la salud mental. La calidad del apoyo que reciben de su organización, su supervisor, y los miembros del equipo han sido propuestos como determinantes importantes de las enfermedades mentales y el bienestar, a través del proceso de evaluación del estrés.
Objetivo: Basados en la teoría del apoyo organizacional, buscamos comprender la relación entre los factores organizacionales, incluyendo el apoyo organizacional percibido, el apoyo del supervisor, y el apoyo del equipo, y los indicadores de salud mental adversa y bienestar mental entre los voluntarios humanitarios. La hipótesis es que esta relación está mediada por el estrés psicológico percibido.
Métodos: Una muestra de 409 voluntarios humanitarios de la Sociedad de la Media Luna Roja Sudanesa completó una encuesta en línea, anónima, compuesta por las escalas de Supervisión Percibida, Apoyo Organizacional Percibido, Apoyo del Equipo, y Estrés Psicológico Percibido, así como las escalas de Trastorno de Ansiedad Generalizada y el Cuestionario de Salud del Paciente, (GAD-7 y PHQ-8 en sus siglas en inglés) y la Escala de Bienestar Mental Warwick-Edinburgh. Los objetivos del estudio se probaron utilizando procedimientos de modelo de ecuaciones estructurales (SEM en su sigla en inglés).
Resultados: Se encontró que la desesperanza percibida (DP) y la autoeficacia percibida (AP), como medidas de estrés psicológico, mediaron completamente la relación entre el apoyo organizacional percibido y los resultados de salud mental. El apoyo organizacional percibido se asoció con la DP (b = −0.60) y la AP (b = 0.56). La DP se asoció con salud mental adversa (b = 0.88) y se relacionó inversamente con el bienestar mental (b = −0.43). La AP solo se asoció con el bienestar mental (b = 0.41). La supervisión percibida se asoció negativamente con la AP (b = −0.33).
Conclusiones: El apoyo organizacional percibido es un determinante clave de la salud mental de los voluntarios humanitarios, con mayor apoyo percibido asociado con menor sintomatología de angustia y mayor bienestar mental. Las agencias humanitarias deberían tomar medidas para mejorar los sistemas de apoyo de su organización interna para mitigar el estrés asociado con el trabajo en contextos traumáticos. Específicamente, se debe prestar más atención al apoyo organizacional de los voluntarios como trabajadores de primera línea en entornos humanitarios.
PALABRAS CLAVE: Voluntario, trabajadores humanitarios, apoyo organizacional, estrés laboral, bienestar, salud mental, Sudán, contextos de emergencia
背景:人道主义工作者在创伤环境下工作,这使其产生不良心理健康结果的风险增加。通过压力评估过程,他们从组织, 管理者及团队成员获得的支持质量被认为是精神疾患和身心健康的重要决定因素。
目标:基于组织支持理论,我们试图了解组织因素之间的关系,包括组织支持感, 管理者支持和团队支持,以及人道主义志愿者的不良心理健康和心理健康指标。假设此关系受到心理压力感中介。
方法:样本为409名苏丹红新月会的人道主义志愿者。他们完成了一个在线匿名调查,包含感知监管,组织支持,团队支持与心理压力量表,广泛性焦虑障碍和患者健康问卷量表(GAD-7和PHQ-8)以及沃里克-爱丁堡心理健康量表。使用结构方程模型(SEM)程序对研究目标进行考查。
结果:作为心理压力量度的无助感(PH)和自我效能感(PSE),均被发现可以完全中介组织支持感与心理健康结果之间的关系。组织支持感与PH(b = −0.60)和PSE(b = 0.56)相关。 PH与不良心理健康相关(b = 0.88),与精神健康为负相关(b = −0.43)。 PSE仅与心理健康相关(b = 0.41)。感知监管与PSE呈负相关(b = −0.33)。
结论:组织支持感是人道主义志愿者心理健康的关键决定因素,支持感越强,痛苦症状越低,身心健康状况就越好。人道主义机构应采取行动,改善其内部组织支持系统,以减轻在创伤环境下工作带来的压力。具体而言,应更加重视作为人道主义环境一线工作者的志愿者获得的组织支持。
关键词: 志愿者, 人道主义工作者, 组织支持, 工作压力, 身心健康, 心理健康, 苏丹, 紧急情况
Working within the humanitarian sector is associated with an increased risk of adverse mental health outcomes (Connorton, Perry, Hemenway, & Miller, 2012). Specifically, humanitarian aid workers experience increased anxiety, posttraumatic stress disorder (PTSD), depression, burnout, compassion fatigue, general distress, hazardous alcohol consumption, subjective health complaints, and suicidal ideation (Lopes Cardozo et al., 2012, 2005; Connorton et al., 2012; Ehring, Razik, & Emmelkamp, 2011; Musa & Hamid, 2008; Thormar et al., 2014; Wang, Yip, & Chan, 2016). This elevated risk is, at least in part, attributed to the nature of humanitarian work, which includes responding to the immediate and long-term human needs following disasters, whether natural (e.g. floods, earthquakes, epidemic diseases) or human-made (e.g. wars and conflicts, forced displacement) (Antares Foundation, 2012). In addition to routine exposure to traumatic events (Strohmeier & Scholte, 2015), humanitarian workers experience demanding working conditions, long working hours, separation from family members, interpersonal conflicts within teams, negative response from communities they serve, safety and security concerns, and financial hardship (Cardozo et al., 2013; Ehrenreich & Elliott, 2004). Therefore, apart from traumatic exposure, those work-related demands with limited organizational support were shown to contribute explicitly to the humanitarian workers’ psycho-morbidity (Jachens, Houdmont, & Thomas, 2019).
While stressors exist among all humanitarian workers, considerable differences are found across different humanitarians. Notably, differences in psychological morbidity are reported between volunteer and professional personnel, with the former experiencing worse outcomes (Hagh-Shenas, Goodarzi, Dehbozorgi, & Farashbandi, 2005; Lee et al., 2017). Despite their increased risk however, comparatively little research has been conducted with humanitarian volunteers, resulting in the majority of our understanding of humanitarian work psychopathology being generated from samples of paid, expatriate (international), or national staff (Strohmeier & Scholte, 2015). Given that volunteers make up the vast majority of the humanitarian workforce, paid humanitarian workers are, therefore, not representative of this entire population. For example, the International Federation of the Red Cross and Red Crescent Societies (IFRC) alone posts a workforce of approximately 13.7 million volunteers globally, compared to 465,000 paid staff (IFRC, 2019). The study of humanitarian volunteers is further warranted given that their working conditions differ from those of paid staff.
According to the IFRC, a volunteer is the ‘person who carries out volunteering activities with a National Society [humanitarian organization], occasionally or regularly. It [volunteering activity] is carried out by people motivated by free will, and not by a desire for material or financial gain, or by external social, economic or political pressure’ (Hazeldine & Baillie Smith, 2015). In emergencies, volunteers are locals who deliver aids, arrange shelters and provide primary health care for the affected populations. They are, therefore, vastly different from paid staff who are formally contracted to work for humanitarian agencies based on their technical expertise. As non-professionals, volunteers tend to have fewer resources in terms of security, insurance, support mechanisms and access to help (Griffiths et al., 2018). Volunteers also tend to be less prepared for humanitarian work challenges, which has been shown to be a crucial contributor to worker resilience (Brooks, Dunn, Amlôt, Greenberg, & Rubin, 2016). In parallel, volunteers are often part of the affected communities they serve, and therefore face the same disaster-related experiences and hardships (Thormar et al., 2010).
Research on paid humanitarian workers suggests that organizational factors, such as supervision, relationship with managers, and positive team support, can mitigate the development of mental distress and promote well-being among staff. A high level of perceived organizational support was associated with lower symptoms of anxiety, depression and PTSD among a sample of local humanitarian staff working in Sri Lanka in the aftermath of the country’s civil war (Cardozo et al., 2013). Similarly, strong team cohesion was associated with lower levels of emotional exhaustion among humanitarian workers in Northern Uganda (Ager et al., 2012). Among volunteers, a lack of perceived support from the organization and team leaders were associated with higher depression rates after disasters (Thormar et al., 2013). More recently, a study conducted by Young, Pakenham (Young, Pakenham, & Norwood, 2018) found that one’s relationship with colleagues, a lack of teamwork, poor management and difficult supervisors, as well as the perceived lack of organizational support were the most common stressors reported by humanitarian workers.
According to organizational support theory (OST) (Eisenberger, Huntington, & Hutchison, 1986), Perceived Organizational Support (POS) represents the level to which ‘employees’ believe that their organization cares about their well-being and values their contributions. Following the norm of reciprocity, ‘employees’ trade their personal efforts and commitment towards achieving the organization’s goals, in exchange for both tangible benefits (e.g. incentives) and intangible benefits (e.g. esteem and caring), leading to better performance and a stronger belief in the organization’s goals (Baran, Shanock, & Miller, 2012). In the case of volunteers, where tangible benefits are very limited or do not exist, the trade-off should lean more towards intangible benefits. However, and though OST is one of the leading theories used to explain a wide spectrum of job-related outcomes such as commitment, retention, strain, performance and satisfaction (Kurtessis et al., 2015), its application has yet to be investigated among humanitarian volunteers. The current study therefore sought to explore the utility of OST to explain mental health outcomes among volunteer humanitarian workers.
Evidently, stress is an important contributor to the psycho-morbidity of humanitarians, whereby exposure to chronic stressors has been shown to be associated with mental ill-health (Strohmeier, Scholte, & Ager, 2018). Similarly, reduced exposure to stressors has been shown to be associated with better mental health outcomes (Ager et al., 2012), and there is some evidence to support the effectiveness of stress management interventions (de Fouchier & Kedia, 2018) and psychoeducation (Okanoya et al., 2015) in improving mental health outcomes for humanitarian workers. However, and while the appraisal process of stressors (i.e. perceived psychological stress) has been found to mediate the effects of work-related stressors on mental ill-health (Lee, Joo, & Choi, 2013), this relationship has yet to be investigated among humanitarian workers, and more specifically, among volunteers. This study therefore further aims to explore the relationships between organizational factors, including perceived organizational support, supervision, and team support and adverse mental health and well-being among humanitarian volunteers, mediated by perceived psychological stress.
A dual continua model is widely used to explain the nature of mental health (Schönfeld, Brailovskaia, & Margraf, 2017; Westerhof & Keyes, 2010). The dual continua is characterized by a positive continuum (i.e. hedonic feelings, functionality, and social relationships) and a negative one (i.e. existence or absence of symptoms). While the link between organizational factors and the negative continuum of mental health has been studied among humanitarians, no research to date has investigated the link between organizational factors and the positive continuum of mental health.
We hypothesized that organizational factors (organizational support, supervision, and team support) would be negatively associated with adverse mental health outcomes and positively associated with mental well-being among humanitarian volunteers. We further hypothesized that these relationships would be mediated by perceived psychological stress. These hypotheses are reflected in the study’s theoretical model, represented in Figure 1.
Figure 1.
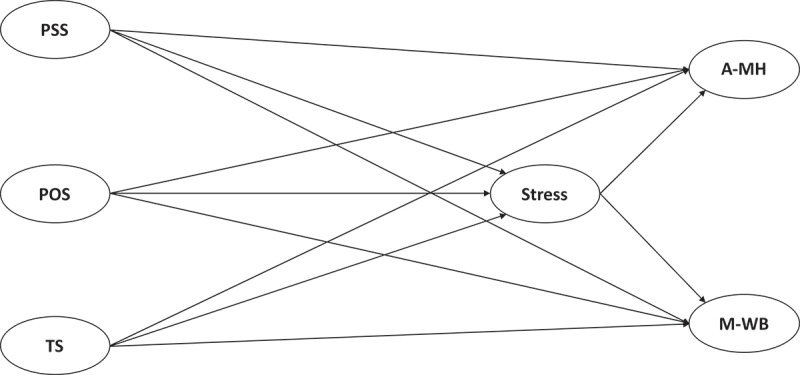
The study hypotheses.
POS: Perceived Organizational Support; PSS: Perceived Supportive Supervision; TS: Team Support; Stress: Perceived Psychological Stress; A-MH: Adverse Mental Health; M-WB: Mental Well-being.
1. Methods
1.1. The study context, participants and procedures
As part of CONTEXT project (Vallières et al., 2017), the study took place in Sudan, a country with numerous years of unstable economic and political status. That included a protracted civil war lasting from 1983–2005, which eventually led to the secession of South Sudan in 2011, and by the conflict in Darfur (Ryle & Willis, 2011). Since 2013, the ongoing civil war in South Sudan has led to large numbers of South Sudanese seeking refuge in Sudan. Additionally, Sudan is regularly affected by seasonal floods and epidemics (UNOCHA, 2018). More recently, rising inflation sparked a series of protests, and the eventual end to President Omar al-Bashir’s 30-year rule, marred by violent clashes. As a member of the International Federation of the Red Cross and Red Crescent Societies, the Sudanese Red Crescent Society (SRCS) engages approximately 80,000 volunteers providing humanitarian aid in disaster-response and development (http://data.ifrc.org/fdrs/societies/the-sudanese-red-crescent) across all of Sudan’s 18 states.
Humanitarian volunteers were recruited from (SRCS) to complete an online-based, self-report survey, using Google Forms. The survey link was sent to all reachable volunteers through their SRCS branch, along with a participation information leaflet. A total number of four hundred nine volunteers (N = 409) successfully filled the survey after giving their consent electronically. Data collection took place between June and August 2018, and with the challenges to reach all areas in Sudan, respondents represented only 14 out of the 18 Sudanese states. Approximately 44.5% (n = 179) were female, all volunteers were aged over 18 (M = 29.42, SD = 8.54), volunteering for their local SRCS branch for an average of six years (M = 6.67, SD = 5.21). Volunteers worked an average of 11.14 hours per week across a number of different tasks including first aid (n = 231), primary health care (n = 326), emergency response (n = 213), nutrition (n = 168), water and sanitation services (n = 154), restoring family links (n = 108), child protection and psychosocial support (n = 81), and dead bodies management (n = 26). About half of the participants (52.32%, n = 214) were employed elsewhere. Further employment and demographic profiles of the participants can be found in the supplemental materials.
1.2. Measures
The following tools were used to measure organizational, perceived stress, and mental health factors after translating them by the lead author (native Arabic speaker) and refining the translation by other two native Arabic professionals (an academic and a psychologist). Similarly, in the instance where scales were already available in Arabic, these were reassessed for consistency. Scales then were piloted with members of the SRCS prior to being made available online.
1.2.1. Organizational measures
Organizational Support was measured using the eight-item version of Perceived Organizational Support (POS) Scale (Eisenberger et al., 1986). The scale was adapted to complement the context of the study by replacing the term ‘my organization’ with ‘the Sudanese Red Crescent Society’ and the term ‘employee’ with the term ‘volunteer’. The POS scale is comprised of four positively-worded and four reversed scored items, answered on a seven-point Likert scale ranging from 0 (Strongly disagree) to 6 (Strongly agree) (Cronbach’s α = .83).
Supervisor support was measured using the perceived supervision scale (PSS) (Vallières et al., 2018), a six-item scale scored on a five-point Likert-type scale ranging from 1 (Strongly disagree) to 5 (Strongly agree) (Cronbach’s α = .89).
Finally, Team Support was measured using the scale developed by Rodwell, Kienzle (Rodwell, Kienzle, & Shadur, 1998), which contains seven-items, each scored on a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree) (Cronbach’s α = .66).
1.2.2. Mental health measures
Mental well-being was assessed using the short version of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) (Tennant et al., 2007), which measures the positive aspects of mental health using seven positively phrased statements. Each statement is answered on a five-point Likert-type scale ranging from 1 (Not all the time) to 5 (All the time) (Cronbach’s α = .75).
Adverse mental health was measured using: a) the GAD-7 (Spitzer, Kroenke, Williams, & Löwe, 2006) scale of generalized anxiety disorder symptoms (Cronbach’s α = .93), b) the Patient Health Questionnaire (PHQ-8) Scale (Kroenke et al., 2009) for major depressive disorder symptoms (Cronbach’s α = .86). Both GAD-7 and PHQ-8 are scored on a four-point Likert-type scale ranging from 0 (Not at all) to 3 (Nearly every day). To measure the adverse mental health, the total scores on the PHQ-8 and the GAD-7 were ultimately modelled as two observed variables, loading onto a single latent construct, termed Adverse Mental Health (A-MH).
1.2.3. Perceived stress
Perceived stress was assessed using the 10-item version of Perceived Psychological Stress scale, designed to measure life conditions which are appraised as stressful (Cohen, Kamarck, & Mermelstein, 1983). The items are scored on a five-point Likert-type scale ranging from 0 (Never) to 4 (Very Often) (α = .79). The scale’s factor structure, however, is debated within the literature. While some argue for a unidimensional model of perceived stress scale (Perera et al., 2017), others argue for a two-factor solution whereby perceived stress is comprised of perceived helplessness and perceived self-efficacy (Roberti, Harrington, & Storch, 2006).
1.3. Ethics
Ethical approval was obtained from the Health Policy & Management/Centre for Global Health Research Ethics Committee, Trinity College Dublin, Ireland as well as from the research directorate in the Federal Ministry of Health, Sudan.
1.4. Data analysis
The relationships between organizational factors, stress, and mental health outcomes, as outlined in Figure 1, were tested using structural equation modelling (SEM) procedures. SEM is a statistical approach comprised of (a) measurement modelling and (b) structural modelling (Byrne, 2012). The measurement model describes the relationship between the observed and hypothesized latent variables (factor analysis), and the structural component incorporates the relationship that links the latent variables (path analysis, regression). Within this model, the structural and measurement components can be estimated simultaneously, thereby determining the psychometric properties of the measurements employed and the relationships between the latent variables (Byrne, 2012). Therefore, unlike ‘traditional’ linear modelling techniques, structural equation models are more general and flexible, can correct for measurement error, and test for the ability of the model to explain the observed pattern of data (Preacher & Hayes, 2008).
A two-phase modelling approach was therefore followed. First, confirmatory factor analysis (CFA) was used to assess the factor structure of the individual scales. Optimal fit indicators were sought and therefore items demonstrating poor loadings (<0.3) were removed. Second, a structural analysis, was used to determine the nature of the direct, and indirect effects of organizational support on volunteer mental health outcomes (Morrison, Morrison, & McCutcheon, 2017). Data analyses were carried out using SPSS (Version 25) and Mplus (Version 7.4: Muthén & Muthén, 1998–2017). The CFA was conducted using a Robust Maximum Likelihood estimator (MLR). However, in the structural phase, when testing multiple mediators, we used the bootstrapping technique as recommended by Preacher and Hayes (Preacher & Hayes, 2008) to estimate the standard errors of direct and indirect effects using the maximum likelihood estimator. Hence, estimations were calculated based on bootstrapping for 1000 replications.
Two competing models were tested, (i) the fully mediated and (ii) the partially mediated via the perceived psychological stress constructs. Goodness of fit was assessed using a number of widely recognized fit indices (Hu & Bentler, 1998, 1999) including: a non-significant chi-square (χ2), Comparative Fit Index (CFI:Bentler, 1990) and Tucker Lewis Index (TLI: Tucker & Lewis, 1973) values above 0.95 reflect excellent fit, while values above .90 reflect acceptable fit; Root-Mean-Square Error of Approximation with 90% confidence intervals (RMSEA 90% CI: Steiger & Lind, 1980), and Standardized Root-Mean-Square Residual (SRMR: Jöreskog & Sörbom, 1996) values of 0.06 or less reflect excellent fit while values less than 0.08 reflect acceptable fit. For the models based on MLR estimation, the Bayesian Information Criterion (BIC: Schwarz, 1978) was used to evaluate and compare models, with the smallest value indicating the best fitting model.
2. Results
2.1. Initial bivariate analysis
Bivariate correlations are presented in Table 1. All bivariate relationships were significant, whereby the three independent variables (POS, PSS, team support) were positively associated with mental well-being, and negatively associated with anxiety (GAD-7), depressive symptoms (PHQ-8), and perceived stress. Perceived stress was positively associated with adverse mental health indicators and negatively associated with mental well-being.
Table 1.
The coefficients of correlation between scales.
| Variables | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1- The Mental Well-being (M-WB) | 30.56 | 3.76 | - | ||||||||
| 2- Generalized Anxiety Disorder (GAD-7) | 3.64 | 4.1 | −.437** | - | |||||||
| 3- Patient Health questionnaire (PHQ-8) | 4.14 | 4.33 | −.426** | .835** | - | ||||||
| 4- Perceived Psychological Stress (Per.S) | 12.89 | 6.13 | −.500** | .720** | .663** | - | |||||
| 5- Perceived Supportive Supervision (PSS) | 34.33 | 4.91 | .223** | −.182** | −.215** | −.233** | - | ||||
| 6- Perceived Organizational Support (POS) | 36.55 | 9.7 | .401** | −.366** | −.446** | −.433** | .520** | - | |||
| 7- Team support (TS) | 28.82 | 3.76 | .354** | −.283** | −.339** | −.386** | .463** | .478** | - | ||
| 8-Adeverse Mental Health (A-MH) | 7.62 | 7.94 | −.455** | .955** | .961** | .720** | −.212** | −.430** | −.317** | - | |
| 9-Perceived Self-efficacy (PSE) | 5.23 | 2.79 | .394** | −.301** | −.281** | −.687** | .158** | .295** | .293** | −.311** | - |
| 10-Pereived Helplessness (PH) | 7.37 | 4.65 | −.424** | .762** | .707** | .900** | −.213** | −.393** | −.337** | .763** | .302** |
SD: Standard deviation
** Correlation is significant at the 0.01 level (2-tailed).
2.2. Measurement modelling (CFA)
Results from the CFA across all measurements can be found in the supplemental materials. All scales demonstrated acceptable model fit, with the exception of the team support scale whereby two items loaded weakly on their latent variable (<0.3) and therefore were removed. Moreover, post-hoc model comparison using latent variable modelling techniques suggested the presence of a method effect for POS scale, whereby all negatively worded items loaded onto a single factor, and all 8 items were grouped onto a general factor (POS) to get an acceptable model fit. Therefore, the sum of the four positively worded items and the sum of the four negatively worded items were subsequently regrouped into two observed variables, loading onto a single latent factor, POS, and brought forward in the structural modelling phase.
Results of the measurement modelling of the perceived stress scale (Cohen et al., 1983) supported a two-dimensional factor structure, consistent with the findings of Roberti, Harrington (Roberti et al., 2006) and Taylor (Taylor, 2015). Perceived helplessness and perceived self-efficacy were therefore introduced to mediate relationships between the organizational factors and mental health outcomes.
2.3. The structural phase
Table 2 presents the model fit indices for both competing models. The fully mediated model was preferred, given its lower BIC and the non-significant relationships between the independent and dependent variables in the partially mediated one. The preferred model is depicted in Figure 2, and its results are presented in Table 3.
Table 2.
Fully VS. partially mediation competing models fit indices.
| Model | χ2 | df | CFI | TLI | RMSEA[90% CI] | SRMR | BIC |
|---|---|---|---|---|---|---|---|
| Partially mediation model | 967.344* | 444 | 0.897 | 0.885 | 0.054[0.049–0.058) | 0.058 | 35,210.502 |
| Fully mediation model | 989.529* | 450 | 0.894 | 0.883 | 0.054[0.050–0.059] | 0.060 | 35,196.635 |
χ2: Chi square, df = degrees of freedom; CFI: comparative fit index; TLI: Tucker Lewis index, RMSEA: root-mean-square error of approximation, CI: confidence interval, SRMR: standardized square root mean residual, BIC: Bayesian information criterion, * Significant Chi square test.
Note: In Fully mediation model, there are no direct effects from independent to dependent variables. In contrast, in the partially mediation one, direct effects between independent and dependent variables were examined.
Figure 2.
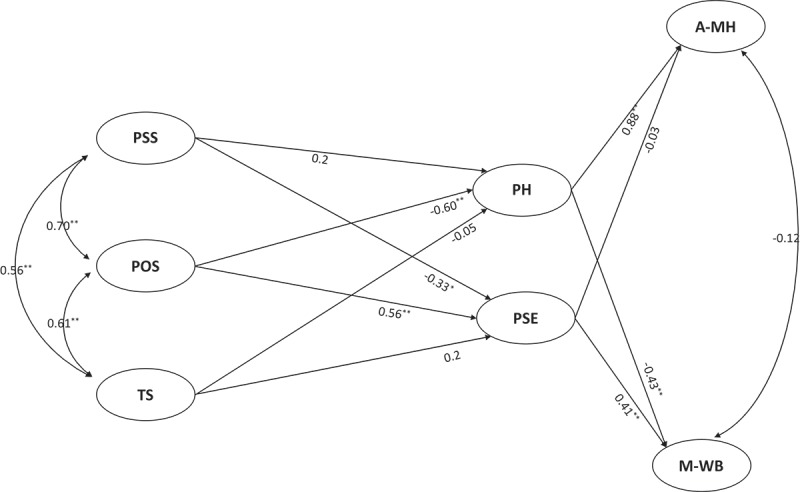
The model results.
POS: Perceived Organizational Support; PSS: Perceived Supportive Supervision; TS: Team Support; PH: Perceived helplessness; PSE: Perceived Self-efficacy; A-MH: Adverse Mental Health; M-WB: Mental Well-being. * p < 0.05, ** p < 0.01.
Table 3.
Standardized and unstandardized regression weights for the relationship between variables in structural equation modelling.
| β | B | SE | |
|---|---|---|---|
| Direct effects | |||
| ● POS ⇒ PH | −0.6** | −0.12 | 0.12 |
| ● POS ⇒ PSE | 0.56** | 0.08 | 0.17 |
| ● PSS ⇒ PH | 0.20 | 0.21 | 0.12 |
| ● PSS ⇒ PSE | −0.33* | −0.26 | 0.13 |
| ● TS ⇒ PH | −0.05 | −0.10 | 0.12 |
| ● TS ⇒ PSE | 0.2 | 0.27 | 0.12 |
| ● PH ⇒ A-MH | 0.88** | 4.27 | 0.02 |
| ● PSE ⇒ A-MH | −0.03 | −0.21 | 0.04 |
| ● PH ⇒ M-WB | −0.43** | −0.20 | 0.07 |
| ● PSE ⇒ M-WB | 0.41** | 0.25 | 0.09 |
| Indirect Effects | |||
| ● POS ⇒ M-WB via PH | 0.26** | 0.02 | 0.08 |
| ● POS ⇒ M-WB via PSE | 0.23* | 0.02 | 0.1 |
| ● POS ⇒ A-MH via PH | −0.53** | −0.52 | 0.16 |
| ● POS ⇒ A-MH via PSE | −0.01 | −0.01 | 0.02 |
| ● PSS ⇒ M-WB via PH | −0.08 | −0.04 | 0.05 |
| ● PSS ⇒ M-WB via PSE | −0.13* | −0.06 | 0.06 |
| ● PSS ⇒ A-MH via PH | 0.18 | 0.93 | 0.11 |
| ● PSS ⇒ A-MH via PSE | 0.01 | 0.05 | 0.01 |
| ● TS ⇒ M-WB via PH | 0.02 | 0.02 | 0.05 |
| ● TS ⇒ M-WB via PSE | 0.08 | 0.07 | 0.05 |
| ● TS ⇒ A-MH via PH | −0.05 | −0.45 | 0.11 |
| ● TS ⇒ A-MH via PSE | −0.007 | −0.06 | 0.01 |
R-square
M-WB R2 = 0.44, SE = 0.07, p < 0.001.
A-MH R2 = 0.79, SE = 0.03, p < 0.001.
PH R2 = 0.26, SE = 0.08, p < 0.01.
PSE R2 = 0.27, SE = 0.09, p < 0.01.
Fit indices
χ2 = 989.52**, df = 450, CFI = 0.894, TLI = 0.883, RMSEA = 0.054 [90% CI = 0.050–0.059], SRMR = 0.060.
POS: Perceived Organizational Support. PH: Perceived Helplessness. PSE: Perceived Self-efficacy. PSS: Perceived Supportive Supervision. TS: Team Support. A-MH: Adverse Mental Health. M-WB: Mental Well-being. β: Standardized weights. B: Unstandardized weights . SE: Standard Error (for standardized estimations). RMSEA: root-mean-square error of approximation. CI: confidence interval. df: degrees of freedom. CFI: comparative fit index. TLI: Tucker Lewis index. SRMR: standardized square root mean residual. * p < 0.05, ** p < 0.01.
The model displayed borderline acceptable fit indices (χ2 = 989.52, df = 450, CFI = 0.894, TLI = 0.883, RMSEA = 0.054 [90% CI = 0.050–0.059], SRMR = 0.060). The model explained 79% of the variance in adverse mental health, 44% of the variance in mental well-being, and 26% and 27% of the variance in perceived helplessness and perceived self-efficacy, respectively.
As noted in Table 3, perceived helplessness was positively associated with adverse mental health (β = 0.88, p < 0.01) and negatively associated with mental well-being (β = −0.43, p < 0.01). Similarly, perceived self-efficacy was positively associated with mental well-being (β = 0.41, p < 0.01), but was not associated with adverse mental health. Perceived organizational support was associated with both perceived stress factors (β = −0.6, p < 0.01 and β = 0.56, p < 0.01, for perceived helplessness and perceived self-efficacy, respectively). Perceived supervision was negatively associated with perceived self-efficacy (β = −0.33, p < .05), whereas team support was not associated with perceived stress factors. All three organizational factors (POS, PSS, Team support) were positively and significantly correlated (r = 0.56–0.70), whereas adverse mental health was uncorrelated with mental well-being.
Significant indirect positive effects were observed between perceived organizational support and mental well-being, through perceived psychological stress factors (β = 0.26, p < 0.01 for perceived helplessness and β = 0.23, p < 0.05 for perceived self-efficacy), and negative effects on adverse mental health, via perceived helplessness (β = −0.53, p < 0.01). Indirect negative effects were also observed between perceived supervision and mental well-being through perceived self-efficacy (β = −0.13, p < 0.05).
3. Discussion
The study results show that perceived organizational support was positively associated with mental well-being and negatively associated with adverse mental health. However, against what was hypothesized, team support was unrelated to mental health outcomes when controlling for POS and PSS. Also, supervision associated negatively with mental well-being. Furthermore, perceived psychological stress factors, perceived helplessness and perceived self-efficacy, fully mediate the relationship between POS and mental health of humanitarian volunteers.The dual continua model of mental health is confirmed, with two distinguished constructs of adverse mental health and mental well-being. Perceived psychological stress was, however, associated with them both, consistent with previous research (Lee et al., 2013; Urquijo, Extremera, & Villa, 2016). Specifically, perceived helplessness was associated with both positive and negative mental health, whereas perceived self-efficacy was associated with only positive mental health (i.e. mental well-being). The relationship between self-efficacy and positive mental health is highlighted in other organizational studies (Fu, Liang, An, & Zhao, 2018; Milam, Cohen, Mueller, & Salles, 2019), and our findings support that this relationship also applies to volunteers working in humanitarian contexts. Moreover, and given the large standardized regression weight (0.88) of perceived helplessness on adverse mental health, these results support the role of self-appraised stress on the psychological morbidity (Cohen et al., 1983; Lazarus, 1974) as a mechanism of linking stressful events with mental health outcomes among volunteers.
Preliminary bivariate correlation results for the association between supervision and mental health outcomes were consistent with the existing literature suggesting a direct correlation between these two variables. Specifically, supervision has been found to be an important contributor to mental health and well-being among other types of first responders including ambulance staff (Petrie et al., 2018), and poor supervision has been identified as a common stressor among humanitarians (Young et al., 2018). However, and when controlling for perceived organizational support, supervision was found to be negatively associated with perceived self-efficacy in the current sample. One plausible explanation for this observation is that supervisor support acts as a component of perceived organizational support (r = 0.7), such that, and as suggested by the OST literature, supervisors are seen as agents of the organization (Eisenberger, Stinglhamber, Vandenberghe, Sucharski, & Rhoades, 2002; Kurtessis et al., 2015; Rhoades & Eisenberger, 2002). Therefore, introducing POS in the model may reveal a ‘well-being trade-off’, whereby more engagement in work occurs at the expense of additional stress and exhaustion. This phenomenon has been documented within the paid staff literature (Inceoglu, Thomas, Chu, Plans, & Gerbasi, 2018; Nielsen & Daniels, 2016). The nature of the relationship between POS, PSS and mental well-being however, remains complex and further research is needed in this area.
Consistent with the literature on humanitarian workers, (Ager et al., 2012), bivariate correlations suggested a positive relationship between team support and mental well-being, and a negative association between team support and adverse mental health and perceived stress. However, team support was no longer significantly associated with these variables when the covariates of perceived organizational support and supervision were controlled for. Similar to perceived supervision, team support was highly correlated with perceived organizational support (r = 0.61). This finding may reflect that team support was also perceived as an important component of perceived organizational support (Kurtessis et al., 2015) and supports that this relationship also holds for volunteers.
In general, results are consistent with the OST literature, where POS has been found to predict a number of positive psychological outcomes within staff-based organizations including less emotional exhaustion (Alexander Hamwi, Rutherford, & Boles, 2011), less stress (Butts, Vandenberg, DeJoy, Schaffer, & Wilson, 2009), subjective well-being (Panaccio & Vandenberghe, 2009), and general health and job satisfaction (Bradley & Cartwright, 2002). Our results are consistent with previous studies which found that a lack of support from humanitarian organizations was accompanied by psycho-morbidity among humanitarian workers (Thormar et al., 2013).
According to OST (Kurtessis et al., 2015; Rhoades & Eisenberger, 2002), plausible mechanisms through which POS impacts on the mental health among volunteers include the fulfilment of the volunteers’ socio-emotional needs such as affiliation, emotional support, and esteem. According to this mechanism, and supported by our findings, POS should strengthen self-efficacy. Another proposed mechanism is via an enriched self-enhancement process, leading to increases in anticipation of help, when needed (Kurtessis et al., 2015). This corresponds to our finding that POS is negatively associated with perceived helplessness. Self-enhancement processes can also lead to developing shared values within the organization (Kurtessis et al., 2015) which, in turn, might increase the feeling of community and the collective efficacy among volunteers. Shared values and collective-efficacy have been shown to be related to higher well-being (Cicognani, Pietrantoni, Palestini, & Prati, 2009) and to better organizational commitment (Meyer, Becker, & Van Dick, 2006).
In summary, the study results offer further support that perceived organizational support contributes to volunteer humanitarian mental health through its effect on perceived stress and proposes OST as a valuable theory through which to conceptualize these relationships. Therefore, underlying the role of POS in the volunteers’ mental health, these findings can be utilized into implications for humanitarian organizations to strengthen their organizational support.
A supportive working environment where volunteers receive favourable treatment from their organization including proper supervision, fair and equal treatment and reliable volunteer management systems is essential to enhance POS (Kurtessis et al., 2015). Prioritizing the volunteers’ safety, protection and well-being, and preparing them better for their work should also be considered as part of strategic planning and budgeting within humanitarian responses (Dinesen, 2018). Moreover, while working, volunteers should be provided with food, water and safe sleeping spaces. Volunteers also need clear job descriptions, where they know about their mission, and are made aware of their specific working hours and are given time to rest. Lack of these aspects accompanied with reduced perception of support and greater psycho-morbidity among humanitarian workers (Brooks et al., 2016; Hearns & Deeny, 2007; Thormar et al., 2013). POS can also be enhanced through involving volunteers in the decision-making process; promoting transparency and accountability within organizations, where volunteers can easily express their concerns and challenges; and building team spirit, where volunteers can receive social support from their peers (Ager et al., 2012; Ghodsi, Jazani, Sohrabizadeh, & Kavousi, 2019; Lopes Cardozo et al., 2013; Nencini, Romaioli, & Meneghini, 2016; Waikayi, Fearon, Morris, & McLaughlin, 2012).
Finally, from an OST perspective, implementing well-being promotion programmes (e.g. Caring for Volunteers: IFRC PS Centre, 2012) is important to not only mitigate the effects of stress and traumatic exposure on volunteers (Okanoya et al., 2015), but also to bring the trust that organizations are making their best efforts to protect their volunteers. A similar conclusion from humanitarian paid staff literature suggested their needs for equality, self-enhancement, and improving access to psychosocial support in order to feel better supported by their organizations (Strohmeier, Scholte, & Ager, 2019).
Consequently, based on the norm of reciprocity, investing in organizational support should enhance work-related behaviours among volunteers, including performance and organizational commitment, both of which are essential to delivering humanitarian assistance and to retaining a volunteer workforce (Rhoades & Eisenberger, 2002; Walker, Accadia, & Costa, 2016).
3.1. Limitations
The present study is not without limitations. As a cross-sectional study, it is impossible to identify causation processes and/or mechanisms of action for how organizational factors impact on humanitarian volunteers’ mental health. Indeed, while the theoretical model suggests unidirectional relationships between variables, the interaction between these is likely bidirectional. Moreover, the use of self-report measures, rather than clinical interviews does not allow us to estimate the prevalence of mental disorders among the study population. Given that internet access remains challenging in Sudan, using an internet-based survey platform may have also acted as a barrier in reaching all volunteers. Finally, adverse mental health was conceptualized using only two measures (i.e. depression and anxiety), omitting other known symptomologies of psychological distress (e.g. PTSD), and other workplace stress-related syndromes (e.g. burnout).
3.2. Conclusions and future research
In agreement with existing research, the present study indicates that organizational support is a vital resource to mitigate mental illness among humanitarian volunteers. Specifically, perceived organizational support is associated with lower perceived stress and greater mental well-being in the volunteers, both of which are important for the performance of volunteers and to achieve the goals of an organization. The relationship between organizational support factors, perceived stress and mental health however is complex and further research is required to understand how these factors interact to impact on humanitarian volunteers. Identifying how these mechanisms may work differently in different contexts is also required. Lastly, future research should continue to explore the utility of OST as an explanatory model for humanitarian worker well-being.
Funding Statement
This work was supported by the European Union’s Horizon 2020, MSCA Actions [722523].
Acknowledgments
This research has received funding from the European Union’s Horizon 2020 research and innovation programme as part of CONTEXT project (http://www.psychotraumanetwork.com) under the Marie Skłodowska-Curie grant agreement No 722523. The authors thank Dr Ayat Abu-agla and Ahlem Cheffi for contributing to the Arabic translation of the instruments, Fabio Beltramini and Sanja Pupacic from the Danish Red Cross delegation in Sudan, and Aida Sayed Abdalla Elsayed, Khalid El-Omer and Osama Mustafa Suliman from SRCS for facilitating the research activities. The authors gratefully thank all SRCS volunteers who participated in the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Ager A., Pasha E., Yu G., Duke T., Eriksson C., & Cardozo B. L. (2012). Stress, mental health, and burnout in national humanitarian aid workers in Gulu, Northern Uganda. Journal of Traumatic Stress, 25(6), 713–12. [DOI] [PubMed] [Google Scholar]
- Alexander Hamwi G., Rutherford B. N., & Boles J. S. (2011). Reducing emotional exhaustion and increasing organizational support. Journal of Business & Industrial Marketing, 26(1), 4–13. [Google Scholar]
- Antares Foundation (2012). Managing stress in humanitarian workers, Guidelines for good practice. Amsterdam: Author. Retrieved from https://www.antaresfoundation.org/filestore/si/1164337/1/1167964/managing_stress_in_humanitarian_aid_workers_guidelines_for_good_practice.pdf?etag=4a88e3afb4f73629c068ee24d9bd30d9
- Baran B. E., Shanock L. R., & Miller L. R. (2012). Advancing organizational support theory into the twenty-first century world of work. Journal of Business and Psychology, 27(2), 123–147. [Google Scholar]
- Bentler P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238. [DOI] [PubMed] [Google Scholar]
- Bradley J. R., & Cartwright S. (2002). Social support, job stress, health, and job satisfaction among nurses in the United Kingdom. International Journal of Stress Management, 9(3), 163–182. [Google Scholar]
- Brooks S. K., Dunn R., Amlôt R., Greenberg N., & Rubin G. J. (2016). Social and occupational factors associated with psychological distress and disorder among disaster responders: A systematic review. BMC Psychology, 4(1), 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butts M. M., Vandenberg R. J., DeJoy D. M., Schaffer B. S., & Wilson M. G. (2009). Individual reactions to high involvement work processes: Investigating the role of empowerment and perceived organizational support. Journal of Occupational Health Psychology, 14(2), 122. [DOI] [PubMed] [Google Scholar]
- Byrne B. M. (2012). Structural equation modeling with Mplus: Basic concepts, applications, and programming. Hove, East Sussex: Routledge Taylor & Francis Group. [Google Scholar]
- Cardozo B. L., Holtz T. H., Kaiser R., Gotway C. A., Ghitis F., Toomey E., & Salama P. (2005). The mental health of Expatriate and Kosovar Albanian humanitarian aid workers. Disasters, 29(2), 152–170. [DOI] [PubMed] [Google Scholar]
- Cardozo B. L., Sivilli T. I., Crawford C., Scholte W. F., Petit P., Ghitis F., … Eriksson C. (2013). Factors affecting mental health of local staff working in the Vanni Region, Sri Lanka. Psychological Trauma-theory Research Practice and Policy, 5(6), 581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicognani E., Pietrantoni L., Palestini L., & Prati G. (2009). Emergency workers’ quality of life: The protective role of sense of community, efficacy beliefs and coping strategies. Social Indicators Research, 94(3), 449. [Google Scholar]
- Cohen S., Kamarck T., & Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Connorton E., Perry M. J., Hemenway D., & Miller M. (2012). Humanitarian relief workers and trauma-related mental illness. Epidemiologic Reviews, 34(1), 145–155. [DOI] [PubMed] [Google Scholar]
- de Fouchier C., & Kedia M. S. (2018). Trauma-related mental health problems and effectiveness of a stress management group in national humanitarian workers in the Central African Republic. Intervention, 16(2), 103. [Google Scholar]
- Dinesen C. (2018). Mental health and psychosocial support: Who cares for the volunteers? Humanitarian Exchange, (72), 52–54. Retrieved from https://odihpn.org/wp-content/uploads/2018/06/HE-72-web.pdf [Google Scholar]
- Ehrenreich J. H., & Elliott T. L. (2004). Managing stress in humanitarian aid workers: A survey of humanitarian aid agencies’ psychosocial training and support of staff. Peace and Conflict: Journal of Peace Psychology, 10(1), 53–66. [Google Scholar]
- Ehring T., Razik S., & Emmelkamp P. M. G. (2011). Prevalence and predictors of posttraumatic stress disorder, anxiety, depression, and burnout in Pakistani earthquake recovery workers. Psychiatry Research, 185(1), 161–166. doi: 10.1016/j.psychres.2009.10.018 [DOI] [PubMed] [Google Scholar]
- Eisenberger R., Huntington R., & Hutchison S. (1986). Perceived organizational support. Journal of Applied Psychology, 71, 500–507. [Google Scholar]
- Eisenberger R., Stinglhamber F., Vandenberghe C., Sucharski I. L., & Rhoades L. (2002). Perceived supervisor support: Contributions to perceived organizational support and employee retention. Journal of Applied Psychology, 87(3), 565. [DOI] [PubMed] [Google Scholar]
- Fu F., Liang Y., An Y., & Zhao F. (2018). Self-efficacy and psychological well-being of nursing home residents in China: The mediating role of social engagement. Asia Pacific Journal of Social Work and Development, 28(2), 128–140. [Google Scholar]
- Ghodsi H., Jazani R. K., Sohrabizadeh S., & Kavousi A. (2019). The resiliency of humanitarian aid workers in disasters: A qualitative study in an Iranian context. Iranian Red Crescent Medical Journal, 21(2), e80366. doi: 10.5812/ircmj.80366 [DOI] [Google Scholar]
- Griffiths M., Smith M. B., Paz B. V., Agerhem S., Cadesky J., & Fadel B. (2018). Theme paper 6: Trauma and psychosocial support. Stockholm: SRC. [Google Scholar]
- Hagh-Shenas H., Goodarzi M. A., Dehbozorgi G., & Farashbandi H. (2005). Psychological consequences of the Bam earthquake on professional and nonprofessional helpers. Journal of Traumatic Stress, 18, 477–483. doi: 10.1002/jts.20055 [DOI] [PubMed] [Google Scholar]
- Hazeldine S., & Baillie Smith M. (2015). IFRC global review of volunteering. Geneva: IFRC. [Google Scholar]
- Hearns A., & Deeny P. (2007). The value of support for aid workers in complex emergencies: A phenomenological study. Disaster Management & Response, 5(2), 28–35. [DOI] [PubMed] [Google Scholar]
- Hu L.-T., & Bentler P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424. [Google Scholar]
- Hu L.-T., & Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- IFRC (2019). Everyone counts. May 2019 issue Geneva: The International Federation of Red Cross and Red Crescent Societies. [Google Scholar]
- IFRC PS Centre (2012). Caring for volunteers, a psychosocial support toolkit: IFRC reference centre for psychosocial support. Copenhagen: IFRC PS Centre. Retrieved from http://legacy.pscentre.org/wp-content/uploads/volunteers_EN.pdf
- Inceoglu I., Thomas G., Chu C., Plans D., & Gerbasi A. (2018). Leadership behavior and employee well-being: An integrated review and a future research agenda. The Leadership Quarterly, 29(1), 179–202. [Google Scholar]
- Jachens L., Houdmont J., & Thomas R. (2019). Effort–Reward imbalance and burnout among humanitarian aid workers. Disasters, 43(1), 67–87. [DOI] [PubMed] [Google Scholar]
- Jöreskog K. G., & Sörbom D. (1996). LISREL 8: User’s reference guide. Lincolnwood, IL: Scientific Software International. [Google Scholar]
- Kroenke K., Strine T. W., Spitzer R. L., Williams J. B. W., Berry J. T., & Mokdad A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. [DOI] [PubMed] [Google Scholar]
- Kurtessis J. N., Eisenberger R., Ford M. T., Buffardi L. C., Stewart K. A., & Adis C. S. (2015). Perceived organizational support: A meta-analytic evaluation of organizational support theory. Journal of Management, 43(6), 1854–1884. [Google Scholar]
- Lazarus R. S. (1974). Psychological stress and coping in adaptation and illness. The International Journal of Psychiatry in Medicine, 5(4), 321–333. [DOI] [PubMed] [Google Scholar]
- Lee J. S., Joo E. J., & Choi K. S. (2013). Perceived stress and self‐esteem mediate the effects of work‐related stress on depression. Stress and Health, 29(1), 75–81. [DOI] [PubMed] [Google Scholar]
- Lee J.-Y., Kim S.-W., Bae K.-Y., Kim J.-M., Shin I.-S., & Yoon J.-S. (2017). Factors associated with posttraumatic stress disorder symptoms among community volunteers during the Sewol ferry disaster in Korea. Comprehensive Psychiatry, 77, 38–44. [DOI] [PubMed] [Google Scholar]
- Lopes Cardozo B., Sivilli T. I., Crawford C., Scholte W. F., Petit P., Ghitis F., … Eriksson C. (2013). Factors affecting mental health of local staff working in the Vanni region, Sri Lanka. Psychological Trauma: Theory, Research, Practice, and Policy, 5(6), 581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes Cardozo B., Gotway Crawford C., Eriksson C., Zhu J., Sabin M., Ager A., ... Simon, W (2012). Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: A longitudinal study. PLoS One, 7(9),e44948. doi: 10.1371/journal.pone.0044948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J. P., Becker T. E., & Van Dick R. (2006). Social identities and commitments at work: Toward an integrative model. Journal of Organizational Behavior, 27(5), 665–683. [Google Scholar]
- Milam L. A., Cohen G. L., Mueller C., & Salles A. (2019). The relationship between self-efficacy and well-being among surgical residents. Journal of Surgical Education, 76(2), 321–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison T. G., Morrison M. A., & McCutcheon J. M. (2017). Best practice recommendations for using structural equation modelling in psychological research. Psychology, 8(9), 1326. [Google Scholar]
- Musa S. A., & Hamid A. A. R. M. (2008). Psychological problems among aid workers operating in Darfur. Social Behavior & Personality: An International Journal, 36(3), 407–416. [Google Scholar]
- Muthén L. K., & Muthén B. O. (1998–2017). Mplus User’s Guide (8th ed.). Los Angeles, CA: Muthén & Muthén.
- Nencini A., Romaioli D., & Meneghini A. M. (2016). Volunteer motivation and organizational climate: Factors that promote satisfaction and sustained volunteerism in NPOs. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations, 27(2), 618–639. [Google Scholar]
- Nielsen K., & Daniels K. (2016). The relationship between transformational leadership and follower sickness absence: The role of presenteeism. Work & Stress, 30(2), 193–208. [Google Scholar]
- Okanoya J., Kimura R., Mori M., Nakamura S., Somemura H., Sasaki N., ... Tanaka, K (2015). Psychoeducational intervention to prevent critical incident stress among disaster volunteers. Kitasato Medical Journal, 45, 62–68. [Google Scholar]
- Panaccio A., & Vandenberghe C. (2009). Perceived organizational support, organizational commitment and psychological well-being: A longitudinal study. Journal of Vocational Behavior, 75(2), 224–236. [Google Scholar]
- Perera M. J., Brintz C. E., Birnbaum-Weitzman O., Penedo F. J., Gallo L. C., Gonzalez P., & Llabre M. M. (2017). Factor structure of the perceived stress scale-10 (PSS) across English and Spanish language responders in the HCHS/SOL sociocultural ancillary study. Psychological Assessment, 29(3), 320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie K., Gayed A., Bryan B. T., Deady M., Madan I., Savic A., … Dalal K. (2018). The importance of manager support for the mental health and well-being of ambulance personnel. PLoS One, 13(5), e0197802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., & Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Rhoades L., & Eisenberger R. (2002). Perceived organizational support: A review of the literature. Journal of Applied Psychology, 87(4), 698. [DOI] [PubMed] [Google Scholar]
- Roberti J. W., Harrington L. N., & Storch E. A. (2006). Further psychometric support for the 10-item version of the perceived stress scale. Journal of College Counseling, 9(2), 135–147. [Google Scholar]
- Rodwell J. J., Kienzle R., & Shadur M. A. (1998). The relationships among work-related perceptions, employee attitudes, and employee performance: The integral role of communication. Australia, 37(3–4), 277–293. [Google Scholar]
- Ryle J., & Willis, J. (2011). Introduction: Many sudans. In J. Ryle, J. Willis, S. Baldo, & J. M. Jok (Eds.), The Sudan handbook (pp. 27–39). Woodbridge: James Currey. [Google Scholar]
- Schönfeld P., Brailovskaia J., & Margraf J. (2017). Positive and negative mental health across the lifespan: A cross-cultural comparison. International Journal of Clinical and Health Psychology, 17(3), 197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B. W., & Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Steiger J. H., & Lind, J. C. (1980). Statistically based tests for the number of common factors. In the annual meeting of the Psychometric Society, Iowa City, IA.
- Strohmeier H., & Scholte W. F. (2015). Trauma-related mental health problems among national humanitarian staff: A systematic review of the literature. European Journal of Psychotraumatology, 6(1), 28541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohmeier H., Scholte W. F., & Ager A. (2018). Factors associated with common mental health problems of humanitarian workers in South Sudan. PLoS One, 13(10), e0205333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohmeier H., Scholte W. F., & Ager A. (2019). How to improve organisational staff support? Suggestions from humanitarian workers in South Sudan. Intervention, 17(1), 40-49. doi: 10.4103/intv.Intv_22_18 [DOI]
- Taylor J. M. (2015). Psychometric analysis of the ten-item perceived stress scale. Psychological Assessment, 27(1), 90. [DOI] [PubMed] [Google Scholar]
- Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., … Stewart-Brown S. (2007). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Developmentand UK validation. Health & Quality of Life Outcomes, 5, 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thormar S. B., Gersons B. P. R., Juen B., Djakababa M. N., Karlsson T., & Olff M. (2013). Organizational factors and mental health in community volunteers. The role of exposure, preparation, training, tasks assigned, and support. Anxiety Stress and Coping, 26(6), 624–642. [DOI] [PubMed] [Google Scholar]
- Thormar S. B., Gersons B. P. R., Juen B., Djakababa M. N., Karlsson T., & Olff M. (2014). The impact of disaster work on community volunteers: The role of peri-traumatic distress, level of personal affectedness, sleep quality and resource loss, on post-traumatic stress disorder symptoms and subjective health. Journal of Anxiety Disorders, 28(8), 971–977. [DOI] [PubMed] [Google Scholar]
- Thormar S. B., Gersons B. P. R., Juen B., Marschang A., Djakababa M. N., & Olff M. (2010). The mental health impact of volunteering in a disaster setting: A review. The Journal of Nervous and Mental Disease, 198(8), 529–538. doi: 10.1097/NMD.0b013e3181ea1fa9 [DOI] [PubMed] [Google Scholar]
- Tucker L. R., & Lewis C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. [Google Scholar]
- UNOCHA (2018, January-December). Sudan 2018 humanitarian response plan. Retrieved from https://reliefweb.int/sites/reliefweb.int/files/resources/Sudan_2018_Humanitarian_Response_Plan.pdf
- Urquijo I., Extremera N., & Villa A. (2016). Emotional intelligence, life satisfaction, and psychological well-being in graduates: The mediating effect of perceived stress. Applied Research in Quality of Life, 11(4), 1241–1252. [Google Scholar]
- Vallières F., Hyland P., McAuliffe E., Mahmud I., Tulloch O., Walker P., & Taegtmeyer M. (2018). A new tool to measure approaches to supervision from the perspective of community health workers: A prospective, longitudinal, validation study in seven countries. BMC Health Services Research, 18(1), 806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallières F., Hyland P., Murphy J., Hansen M., Shevlin M., Elklit A., & Bramsen R. H. (2017). Training the next generation of psychotraumatologists: Collaborative network for training and excellence in psychoTraumatology (CONTEXT). European Journal of Psychotraumatology, 8(sup7), 1421001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waikayi L., Fearon C., Morris L., & McLaughlin H. (2012). Volunteer management: An exploratory case study within the British red cross. Management Decision, 50(3), 349–367. [Google Scholar]
- Walker A., Accadia R., & Costa B. M. (2016). Volunteer retention: The importance of organisational support and psychological contract breach. Journal of Community Psychology, 44(8), 1059–1069. [Google Scholar]
- Wang X. L., Yip P. S. F., & Chan C. L. W. (2016). Suicide prevention for local public and volunteer relief workers in disaster-affected areas. Journal of Public Health Management and Practice, 22(3), E39–E46. [DOI] [PubMed] [Google Scholar]
- Westerhof G. J., & Keyes C. L. M. (2010). Mental illness and mental health: The two continua model across the lifespan. Journal of Adult Development, 17(2), 110–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young T. K. H., Pakenham K. I., & Norwood M. F. (2018). Thematic analysis of aid workers’ stressors and coping strategies: Work, psychological, lifestyle and social dimensions. Journal of International Humanitarian Action, 3(1), 19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- UNOCHA (2018, January-December). Sudan 2018 humanitarian response plan. Retrieved from https://reliefweb.int/sites/reliefweb.int/files/resources/Sudan_2018_Humanitarian_Response_Plan.pdf


