Abstract
Melanocytoma is a deeply pigmented variant of melanocytic nevus that classically occurs in the optic disk, sometimes with contiguous involvement of the adjacent retina or choroid. Historically, this tumor was often confused with malignant melanoma both clinically and histopathologically. Today, however, it is generally recognized by its typical clinical features that differ from most melanomas and erroneous enucleation is rarely done. Histopathologically, melanocytoma is composed of intensely pigmented round to oval nevus cells with benign features. Although traditionally believed to be a relatively stationary lesion, it is now known to exhibit minor enlargement in 10--15% of cases and can cause minor visual loss by a variety of mechanisms. In rare instance, it can induce severe visual loss due to spontaneous necrosis of the lesion or compressive optic neuropathy. More importantly, it can exhibit malignant transformation into melanoma in 1--2% of cases. Ophthalmologists should be familiar with melanocytoma of the optic disk and affected patients should be followed periodically.
Keywords: Choroid, eye, magnocellular nevus, melanocytoma, melanoma, optic disk, optic nerve, pseudomelanoma, retina, tumor, uvea, uveal tract
This classic review article published in Survey of Ophthalmology is reprinted with permission from Elsevier. Copyright (2004). Shields JA, Demirci H, Mashayekhi A, Eagle Jr RA, Shields CL. Melanocytome of the Optic Disk: A Review. Surv Ophthalmol 2006;51:93-104.
General Considerations
Primary intraocular pigmented lesions can arise from melanocytes in the uveal tract or from the pigment epithelium of the iris, ciliary body, and retina. Uveal melanoma most often occurs in the choroid and is less frequent in the anterior uvea.[1,10,34,56,58,61,62,79,80,81] Tumors and related lesions of the pigment epithelium are considerably less common than uveal melanoma and have characteristic clinical and histopathologic features.[65] Melanocytic tumors can also occur in the optic disk and in the deeper portions of the optic nerve. Primary malignant melanoma of the optic disk is extremely rare with few well documented cases in the literature.[18,23] However, a benign tumor of the optic disk, which has been termed melanocytoma in the ophthalmic literature, is relatively common and well known.[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82]
A number of reports have also shown that lesions with similar histopathologic features can occur anywhere in the uveal tract separate from the optic disk.[50,61,74] Since the original descriptions of optic disk melanocytoma, many case reports, small series of cases, and two larger series have stressed new observations on optic disk melanocytoma.[34,58] This article is a comprehensive review of the historical aspects, clinical variations, natural course, pathology, pathogenesis, differential diagnosis, diagnostic approaches, and management of this unique ophthalmic tumor.
Historical perspectives
The lesion called melanocytoma of the optic disk is now well-known to ophthalmologists. The evolution of our current knowledge regarding this tumor is intriguing. Whereas melanocytoma of the optic disk was once believed to be a malignant neoplasm with lethal potential, it is now known to be a benign lesion that carries an excellent prognosis. Such changing concepts regarding the malignancy of a specific condition are rare in ophthalmology and oncology.
Prior to the elucidation of the nature of melanocytoma, there were a number of reports of pigmented lesions of the optic disk. This subject was summarized by Reese in 1933.[49] He found histopathologic evidence of normal pigmentation at the level of the lamina choroidalis and lamina scleralis in some heavily pigmented individuals. He showed three fundus drawings of small, pigmented lesions on the optic disk that he called melanoma of the optic disk. However, our review of the case description and illustrations indicates features typical of what is called a melanocytoma today.[49] Additionally, he correctly pointed out that juxtapapillary choroidal melanoma (generally called melanosarcoma at that time) can grow around the posterior termination of Bruch's membrane and give the false illusion of a primary optic disk tumor.
In 1935, Levine reported a 53-year-old Hispanic patient who underwent enucleation for a deeply pigmented lesion of the optic disk that was diagnosed clinically as a melanosarcoma.[39] On histopathologic examination, the small elevated tumor was mainly confined to the optic disk but extended for a short distance posterior to the lamina cribrosa. The patient refused subsequent orbital exenteration, and was treated with orbital irradiation. A review of that case also suggests that it was a typical melanocytoma of the optic disk.
In 1949, Cordes and Hogan reported a clinicopathologic correlation of a case of primary melanoma of the optic disk in an African-American woman.[14] The lesion was a small black tumor that occupied the inferior half of the optic disk and had finger-like projections into the adjacent sensory retina. Bleached histopathologic sections revealed slightly pleomorphic round cells that would be consistent with a melanocytoma. These authors described in some detail the 7 previously reported cases purported to be melanoma of the optic disk and judged that only 5 could be “proved” cases of melanoma. They believed that their case represented the sixth “proved” case. All of the reported cases mentioned above were small lesions confined to the disk and adjacent retina or choroid. Based on our review, we believe that all of them most certainly would be classified today as melanocytomas.
In 1954, deVeer reported a case of pigmented lesion of the optic disk and mentioned that 10 prior cases had been reported.[19] Based on his review, he concluded that none of those cases were absolutely proven to have originated in the optic disk. He believed that those previously reported tumors were probably all juxtapapillary choroidal melanomas with secondary invasion of the optic nerve. In a subsequent publication in 1961, deVeer reported an eye with a lesion that was shown on serial sections through the optic disk to be completely located within the disk and possibly benign.[20] He based his belief on the benignancy of the lesion on his knowledge that Zimmerman had mentioned several similar benign cases 1 year earlier.[79]
In 1957, Milosevic and Litrocin reported a clinicopathologic correlation of a small deeply pigmented, enlarging tumor that initially was believed to be a melanoma confined to the optic disk.[43] However, pathologic examination revealed a choroidal component, which prompted them to title their paper “Illusion of a primary melanoma of the optic disc.” They proposed that the tumor was a melanoma that arose from a small choroidal component and secondarily invaded the disk. A review of their case strongly suggests that the lesion was a melanocytoma of the optic disk with a juxtapapillary choroidal component, a feature that was subsequently found to be a common component of melanocytoma.
A number of the aforementioned cases, as well as other cases, were cited by Lorenz E. Zimmerman, MD, at the Armed Forces Institute of Pathology (AFIP) in Washington, DC. Dr. Zimmerman had carefully reviewed a series of eyes that were enucleated for melanoma of the optic disk and was impressed by their relatively benign histopathologic features, as compared to typical choroidal melanomas. Dr. Zimmerman surprised the ophthalmic community in his 1959 de Schweinitz Lecture in Philadelphia, when he proposed that there was a benign pigmented lesion of the optic disk that had previously been erroneously considered malignant by both clinicians and pathologists.[79]
Three years later, the data on melanocytoma collected at the AFIP were published by Zimmerman and Garron.[81] They reported 36 cases, 20 of which were clinicopathologic correlations on eyes enucleated for suspected melanoma. Enucleation was not performed on the remaining 14 cases because the patient declined or because the clinician elected to follow a small asymptomatic lesion without immediate removal of the eye. They presented a strong and convincing argument that this pigmented lesion of the optic disk was benign, rather that malignant, as had been previously believed. They stressed the fact that, in those eyes that were not enucleated, the lesions remained stable, sometimes for many years of follow-up. They also conducted a detailed histopathological review of available pathologic specimens and showed convincing evidence that the lesions were benign. They pointed out that prior pathologists had assumed that the lesion was malignant.
In 1965, Zimmerman provided a scholarly publication of the Jonas S. Friedenwald Memorial Lecture that he had presented in the prior year. In that publication, entitled “Melanocytes, melanocytic nevi, and melanocytomas,” he challenged the prior publications of malignant melanoma of the optic disk, and stated his belief that they were all cases of melanocytoma of the optic disk.[81] He also defended his choice of the term melanocytoma, a subject to be considered next.
Terminology
The term melanocytoma was originally coined by Zimmerman to define the tumor that is the subject of this review. He chose that term because he thought that the appearance of the tumor cells on bleached sections was remarkably similar to the cells that he had observed to diffusely thicken the uveal tract in patients with ocular melanocytosis. He did acknowledge the shortcomings of that name, because melanocytoma is a general term that could refer any tumor composed of melanocytes, including malignant melanoma. He mentioned that at a prior meeting, Cogan had challenged the term melanocytoma and had proposed the term magnocellular nevus of the optic nerve.[13] However, that term, which does seem more appropriate, has not been perpetuated and the term melanocytoma has attained widespread usage.
We have also been concerned about the term melanocytoma and would have preferred a more accurate term such as hyperpigmented magnocellular nevus of the optic disk (HMNOD) because it is scientifically more correct. However, like many other terms that are not entirely accurate, but deeply engrained in our terminology, the name melanocytoma most likely will continue to be used.
Subsequent to the aforementioned series from the AFIP, numerous case reports, two review articles,[50,56] and two sizable series[34,58] on melanocytoma of the optic disk have been reported. These reports have expanded our knowledge of the clinical variations, clinical behavior, and local complications of optic disk melanocytoma. Melanocytoma is now best defined as a specific variant of melanocytic nevus, located in the optic disk or anywhere in the uveal tract, characterized clinically by a dark brown to black color, and composed histopathologically of intensely pigmented round to oval cells with copious quantities of cytoplasm and small, round, uniform, bland nuclei.[58,80,81]
Other ocular locations
Many tumors with histopathologic features identical to optic disk melanocytoma cell type have been reported in extrapapillary locations throughout the uveal tract, including the iris, ciliary body, and choroid.[61,74] These lesions generally are deeply pigmented and represent a specific variant of uveal melanocytic nevus.
Demographics
Based on numerous case reports and three reported series of optic disk melanocytoma, reasonably accurate demographic information is now available.[34,58] Because melanocytoma was traditionally confused with melanoma both clinically and histopathologically, it is important to mention the similarities and differences of these two lesions.
Age
The mean age at diagnosis of optic disk melanocytoma is 50 years with a median of 52 and range of 1–91 years.[58] This is generally similar to the age at diagnosis of uveal melanoma. However, we believe that most melanocytomas are probably present for many years before being discovered during a routine ocular examination. The melanocytoma diagnosed at age 1 year is exceptional and that diagnosis has been the source of some debate, as to whether the lesion was a true tumor or simple flat pigmentation of the optic disk.[8,57] It is possible that melanocytoma is a congenital lesion but may not become clinically apparent until later in life, perhaps due to acquisition of pigment in a previously amelanotic lesion.[67]
Race
An important difference between uveal melanoma and optic disk melanocytoma is that melanocytoma appears to have an equal incidence in all races, whereas uveal melanoma is uncommon in African Americans and Asians.[47] It is often stated that melanocytoma is more common in African Americans and Asians. However, in our clinical practice and our literature search, we have been unable to find support for that statement. In the series of Zimmerman and Garron, there was an equal distribution between white subjects and African Americans.[81] In the large clinical studies of Joffe and associates and Shields and associates, there was a preponderance of white patients, which the authors believe could partly reflect referral bias.[34,58] There is not enough data on this uncommon tumor to be certain about its racial distribution. We have no explanation for the different race distribution of melanocytoma and melanoma.
Sex
Optic disk melanocytoma appears to have a slight predilection for females. In the AFIP series 63% of the 35 cases were in women[81] and in the Wills Eye Hospital series 62% of 115 cases were women.[58] We have no explanation for this apparent sex predisposition.
Clinical Features
Laterality
Melanocytoma is usually unilateral. Bilateral cases have been rarely reported, usually in children.[27,76] There has been some controversy as to whether these are true melanocytomas or actually disc pigmentation in association with other congenital disk abnormalities.[8,9]
Multifocality
On occasion, optic disk melanocytoma and uveal melanocytoma can occur in the same eye. Such multiple melanocytomas may be more frequent than realized, because we are aware of cases of multiple melanocytomas found in eyes enucleated for other reasons and as a coincidental finding in autopsy eyes (personal observations).
Visual acuity
Most melanocytomas do not cause significant visual impairment.[58,81] However, slight visual loss caused by the tumor can occur in about 26%, usually due to mild exudative retinal exudation involving the fovea or neuroretinitis from tumor necrosis.[2,28] More severe visual loss can rarely occur, secondary to central retinal vein obstruction and/or spontaneous tumor necrosis[16,64,77,81] or malignant transformation.[1,58,61,63] When profound visual loss has occurred, most eyes have been enucleated because of suspicion of malignant transformation. In some cases, enucleation was not performed and visual acuity recovered, suggesting that there was transient ischemic necrosis or inflammation in the tumor.[28,77]
Pupillary changes
Osher and associates assessed pupillary reactions in the patients reported by Joffe and associates.[46] They found that 6 patients (30%) with optic disk melanocytomas had an afferent pupillary defect (Marcus Gunn pupil; APD) in the involved eye. An important clinical point is that APD can occur even in presence of excellent visual acuity. Optic disk melanocytoma is one of the few conditions in which this paradoxical pupillary reaction can occur. It is probably due to mild compression of the optic disk fibers by the melanocytoma cells, a factor that also explains the associated visual field defect.
Visual fields
Optic disk melanocytoma can cause a variety of visual field defects.[22,46,75] In the same series of patients in whom the pupillary findings were studied, there were 20 patients who underwent Goldman perimetry. The visual field was normal in 10% and abnormal in 90%. Abnormal fields included minimal enlargement of the blind spot in 3 patients (15%), and a greatly enlarged blind spot in 15 patients (75%), of whom 10 had concomitant nerve fiber bundle defects including nasal step (10%), relative nerve fiber bundle defect (20%), and an absolute arcuate defect (20%). The blind spot enlargement appeared to be related to the amount of tumor extension beyond the disk margin and the arcuate defects appeared to be related to compression of axons in the optic disk. It is of interest that the scotomas usually occurred in patients with normal visual acuity.[46] A similar incidence of 90% visual fields defects was demonstrated by Usui and associates in 11 Japanese patients.[75]
Ophthalmoscopic features
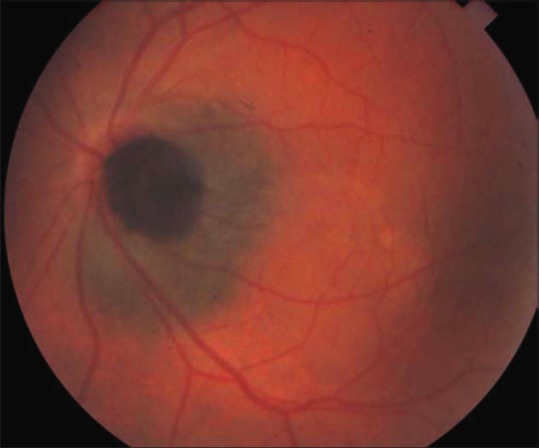
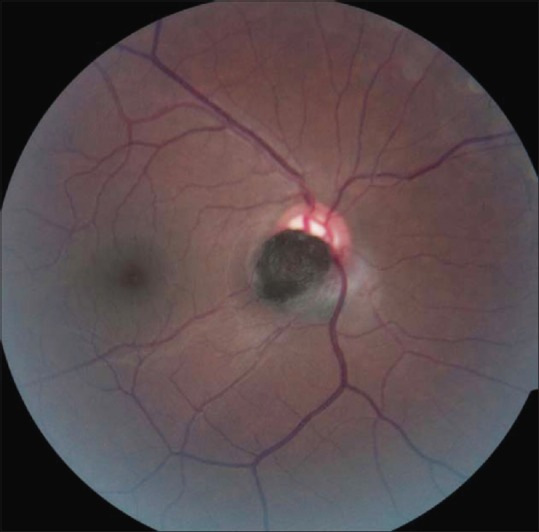
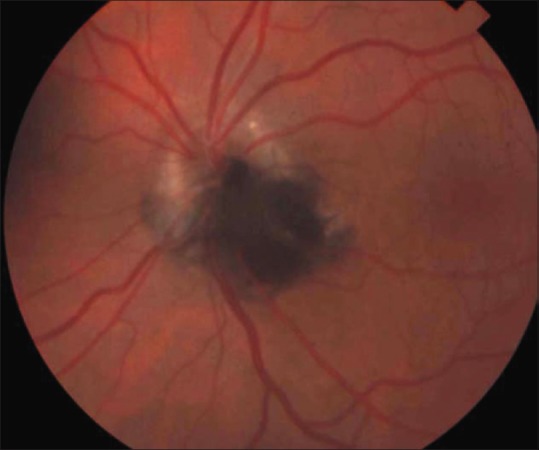
The ophthalmoscopic features of optic disk melanocytoma can vary considerably from case to case. It is characteristically a dark brown to black lesion that is located entirely or partly in the optic disk. It is relatively small and confined to the disk in 15% of cases (Fig. 1). More characteristically, it extends over the margin of the optic disk to involve the adjacent choroid (54%) (Fig. 2) or into the adjacent sensory retina (30%) (Fig. 3).[18] In some cases, the choroidal component is more pronounced than the optic disk component.[7,34,58]
Figure 1.
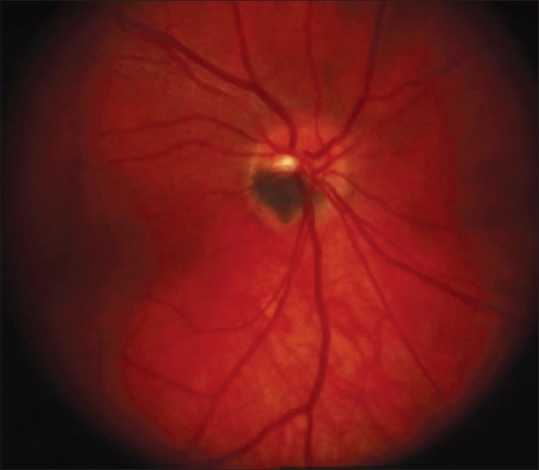
Optic disk melanocytoma confined to the optic disk
Figure 2.
Optic disk melanocytoma with choroidal component
Figure 3.
Optic disk melanocytoma with prominent retinal component
Ocular associations
In a recent review of 115 patients, the only significant ocular association was ocular melanocytosis, which was present in 8%.[58] This is greater than would be expected in the general population. Other rare associations, such as racial melanosis, optic disk hypoplasia, retinitis pigmentosa, and congenital hypertrophy of the retinal pigment epithelium, were probably coincidental. The finding of ipsilateral ocular melanocytosis appears to be more than coincidental, since Zimmerman chose the term melanocytoma because the cells were so similar to those that diffusely thicken the uveal tract in ocular melanocytosis.[80]
Systemic associations
Optic disk melanocytoma is generally an isolated entity with no proven associations with any systemic diseases. A recent study showed solitary cases of neurofibromatosis type 2, basal cell carcinoma, and vitiligo, but these seem to be coincidental.[58] Optic disk melanocytoma has also been associated with intracranial meningioma.[69,76]
Clinical Course
Local complications
Although optic disk melanocytoma generally is believed to have few local complications, a recent study showed the presence of disk edema (25%) (Fig. 4), intraretinal edema (16%), subretinal fluid (14%), yellow intraretinal exudation (12%), focal hemorrhage (5%), vitreous seeds (4%), and retinal vein obstruction (3%). These local complications can produce visual symptoms or visual loss in 26% of cases.[58] The statistical risk factors for visual loss include retinal extension of the tumor and the presence of subretinal fluid.[58] As mentioned earlier, the complications are generally minor, and severe visual loss is exceptional. Vitreous seeds from necrosis of the melanocytoma can extend into the anterior chamber, sometimes producing a black pseudohypopyon. As mentioned above, melanocytoma rarely causes focal subretinal or intraretinal hemorrhage, and, if it does, it is usually small and insignificant. Although it is not always clearly seen clinically or histopathologically, we strongly suspect that juxtapapillary choroidal neovascularization is the most likely cause of such hemorrhage. One tumor with adjacent subretinal hemorrhage was followed for 16 years without change and the eye was enucleated when a large hematoma developed beneath the RPE. The enucleated eye showed fibroglial tissue adjacent to the disk that was probably the source of the hemorrhage.[33] Retinal vascular occlusion secondary to optic disk melanocytoma (Fig. 5) can cause severe visual loss and usually is due to ischemic necrosis in the tumor or vascular compression of the tumor.[38,64,70] Some eyes affected by this complication have been enucleated, one of which had developed neovascular glaucoma secondary to the retinal ischemia. In one case the melanocytoma was obscured by disk edema, central retinal artery obstruction developed, and the disk edema subsequently resolved allowing visualization of the optic disk tumor.[73]
Figure 4.
Optic disk melanocytoma with secondary disk edema
Figure 5.

Central retinal vein obstruction secondary to melanocytoma of optic disk
A noteworthy local complication that often occurs in melanocytoma is acute ischemic necrosis. This can lead to abrupt and severe visual loss with signs of unilateral optic neuritis, secondary retinal vein obstruction, and vitreous seeding. Foci of necrosis have been demonstrated in a number of eyes that came to enucleation because of suspicion of malignant transformation.[16,64,81] Focal necrosis in the tumor is also believed to account for cases of melanocytoma that caused seeding of tumor cells into the vitreous and anterior chamber.[38,78]
Growth
Melanocytoma of the optic disk traditionally was believed to be a stable lesion with no tendency to grow.[11,25,29,31,34,58] However, serial fundus photographs have documented that 10–15% of them show subtle enlargement over several years. This mild growth should not be considered a sign of malignant transformation.[34,58] Mansour and associates reported a progressively growing melanocytoma which after enucleation proved to be benign, despite extensive growth and visual loss.[41] Recent analysis has shown that the main predictive risk factor for growth is an initial thickness of 1.5 mm or greater at the time of first diagnosis.[58] Some tumors can grow slowly and produce ischemic optic neuropathy associated with tumor necrosis, resulting in severe visual loss. Others can cause central retinal vein obstruction and visual loss (Fig. 5).[16,64] In rare cases the tumor can present as neovascular glaucoma secondary to retinal vein obstruction.[16]
Malignant transformation
Extensive involvement of the optic nerve with severe visual loss is a dramatic event that suggests malignant transformation of optic disk melanocytoma.[1,16,28,34,42,55,58] However, severe necrosis of a benign melanocytoma can sometimes produce similar signs and symptoms.[16,64,81] Malignant change is estimated to occur in about 1–2% of cases.[58] A few convincing cases of malignant melanoma arising from an optic nerve melanocytoma with histopathologic confirmation have been reported.[1,42,63,82] The characteristic features of malignant transformation of optic disk melanocytoma are an initial lesion originating exclusively from optic nerve without juxtapapillary choroidal involvement, with progressive growth and visual loss. Histologically, malignant change is characterized by spindle-shaped melanoma cells adjacent to the typical melanocytoma cells. The melanocytoma cells and the spindle-melanoma cells are often interwoven without interseptal or interstitial tissue. However, growth and visual loss do not always imply malignant transformation and such changes can occur from ischemic necrosis in the lesion or other complications.[30,41,70,77] Fluorescein angiography and indocyanine green angiography may sometimes be helpful in identifying the nature of the lesion but they have limitations because of the deep pigmentation of the lesion. The differential diagnosis of malignant melanoma and primary malignant melanoma of the optic nerve simulating a melanocytoma have been reported.[23,40]
Extensive involvement of the optic disk with severe visual loss are dramatic events that suggest malignant transformation of optic disk melanocytoma [Fig. 5].[1,16,28,34,42,55,58] Malignant change is estimated to occur in about 1–2% of cases.[58] Only a few convincing cases of transformation into melanoma with histopathologic confirmation have been reported.[1,63,82] However, growth and visual loss do not always imply malignant transformation and such changes can occur from ischemic necrosis in the lesion.[30,41,64,77]
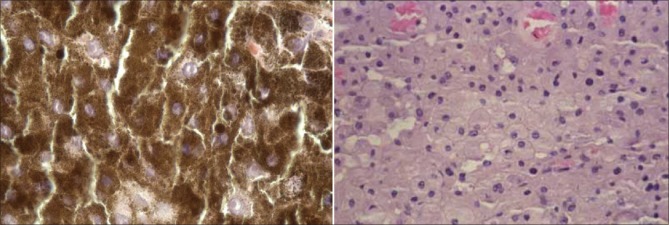
Pathology
Histopathologically, melanocytoma of the optic disk has a characteristic appearance. It is an intensely pigmented mass that occupies the optic disk and extends for a variable distance into the optic disk itself (Fig. 6). The most distinguishing characteristics are the intense cytoplasmic pigmentation, the low nuclear cytoplasmic ratio, and the uniform size of the cells and nuclei.[61,62,73,79,80,81] Although the copious quantities of cytoplasmic pigment typically obscure nuclear and cellular details, bleached preparations reveal the cells to be oval or round with abundant cytoplasm, relatively small nuclei, and few prominent nucleoli, similar to those which occur throughout the uvea in patients with ocular melanocytosis (Fig. 7). In some cases of otherwise typical optic disk melanocytoma, spindle-shaped cells admixed with the more typical round cells have been observed.[35] Tumors composed of similar cells have also been recognized in the iris, ciliary body, choroid, conjunctiva,[61] and meninges.[48,69]
Figure 6.
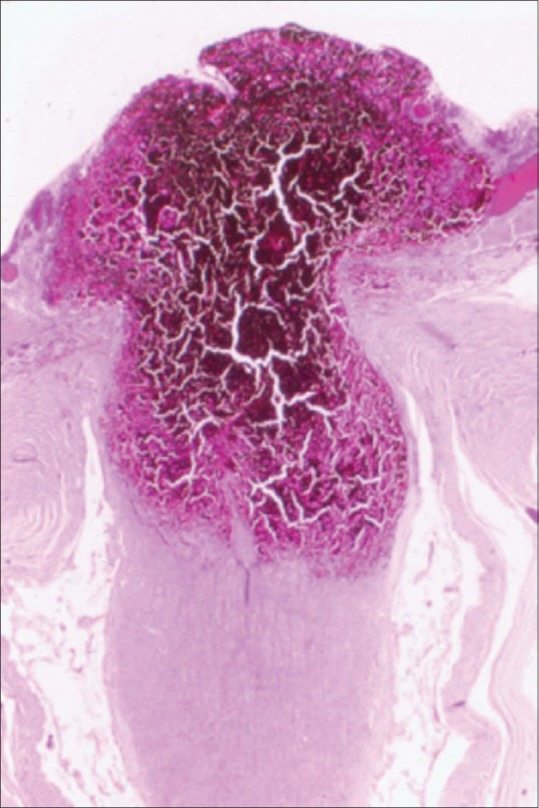
Low magnification photomicrograph of optic disk melanocytoma (hematoxylin-eosin 3 10). (Courtesy of Armed Forces Institute of Pathology)
Figure 7.
Cytologic features of optic disk melanocytoma. Left: Unbleached section (hematoxylin-eosin 3 100). Right: Bleached section (bleached; hematoxylin-eosin 3 100)
Ultrastructural studies of optic disk melanocytoma have been reported.[16,35] The plump round cells seen by light microscopy contained giant round cytoplasmic melanosomes with relative sparsity of other cytoplasmic organelles. In contrast, spindle nevus cells had more prominent nucleoli, the melanosomes were rod-shaped, and there were more cytoplasmic organelles.[35] Juarez and Tso classified these two variants as type 1 and type 2, respectively. The authors believed that the large round cells were better differentiated as compared to the spindle cells.[35]
Pathogenesis
The pathogenesis of optic disk melanocytoma is unknown. It is generally assumed to be a congenital lesion, but, like most uveal nevi, it is rarely seen in young children. It has developed in an adult fundus that was previously documented photographically to be normal, raising speculation that it is either acquired or occurs as an amelanotic lesion that later becomes pigmented and clinically visible.[67] The rare association of optic disk melanocytoma with neurofibromatosis and meningioma could be of pathogenetic interest since the lesions in both entities are of neural crest origin, similar to uveal melanocytes that comprise melanocytoma and ocular melanocytosis.[69,77]
Differential Diagnosis
The differential diagnosis of melanocytoma of the optic disk includes juxtapapillary choroidal melanoma, choroidal nevus, hyperplasia of the RPE, combined hamartoma of the retina and RPE and adenoma of the RPE, metastatic melanoma to optic disk, epipapillary vitreous hemorrhage, and other conditions.[48,61,62] The detailed clinical features of these lesions are described elsewhere[61] and will only be highlighted here.
Choroidal melanoma
Although extremely rare, primary malignant melanoma can occur in the optic disk and may be difficult to impossible to differentiate clinically from melanocytoma.[18,23] In rare instances a juxtapapillary melanoma has extended around the posterior termination of Bruch's membrane and invaded the sensory retina causing a fibrillary margin similar to melanocytoma and leading to diagnostic confusion.[40]
Choroidal nevus
It should be stressed that an optic disk melanocytoma is a variant of melanocytic nevus that happens to be located partly over the optic disk. However, there has been a tendency to classify choroidal nevus and optic disk melanocytoma as separate entities because of their different location and clinical appearance. In general, a typical pigmented juxtapapillary choroidal nevus has clinical features that serve to differentiate it from optic disk melanocytoma. It is a flat, or minimally elevated choroidal lesion that lies outside the disk and does not overlie the disk. However, as mentioned earlier, many melanocytomas have a juxtapapillary choroidal component that is identical to choroidal nevus. We have seen cases of sizable juxtapapillary choroidal nevi that have a very small optic disk component. It may be difficult to decide whether such a lesion should be classified primarily as a choroidal nevus or as an optic disk melanocytoma.[61]
Hyperplasia of retinal pigment epithelium
Hyperplasia of the RPE at the disk margin can also be similar to melanocytoma. In general, there is a history of ocular trauma or inflammation and the lesion is more irregular with evidence of chorioretinal scarring.[61]
Combined hamartoma of retina and RPE
Juxtapapillary combined hamartoma of the retina and RPE can be very similar to a melanocytoma. However, it usually does not involve the disk itself, but may extend from its juxtapapillary location onto the disk margin. In contrast to melanocytoma, it is associated with overlying retinal gliosis, which causes traction on the retinal vessels causing stretched or corkscrew vascular changes that are not seen with melanocytoma. It does not have a juxtapapillary choroidal component or feathery invasion of the nerve fiber layer of the retina.[51]
Adenoma of RPE
Juxtapapillary adenoma of the RPE can also closely resemble melanocytoma.[60] It can also extend onto the disk margin but does not show a feathery margin. It is more likely than melanoma to show adjacent yellow retinal exudation. In contrast to melanocytoma, it can occasionally be clinically amelanotic.[59] An optic disk tumor reported as a melanocytoma later proved to be an adenoma of the RPE when eye was studied histopathologically after the patient died from unrelated causes.[10,60]
Metastatic melanoma to optic disk
Metastatic cutaneous melanoma to the optic disk is extremely rare and could resemble a melanocytoma. However it tends to grow more rapidly and to diffusely infiltrate the optic disk, resembling papilledema or acute papillitis. A distinct black mass usually is not seen.[68]
Diagnostic Approaches
The diagnosis of a melanocytoma of the optic disk usually can be made by ophthalmoscopic recognition of its characteristic clinical features. Ancillary procedures like fundus photography, fluorescein angiography, and visual field examination can facilitate the diagnosis and provide help in follow-up evaluations.
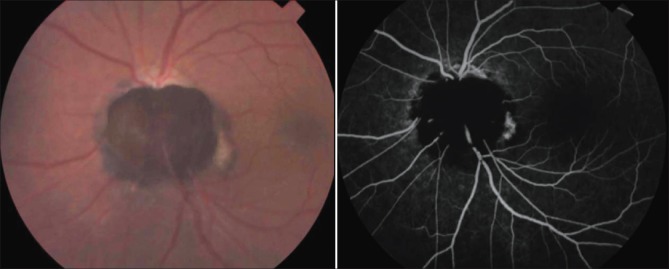
In most cases, fluorescein angiography of a melanocytoma of the optic disk demonstrates hypofluorescence throughout the angiogram (Fig. 8).[27,58,61] This is presumably because the cells are deeply pigmented and closely compact with relatively little vascularity. In cases with optic disk edema, there is hyperfluorescence of the edematous portion of the optic disk. Indocyanine green angiography also shows the lesion to be generally hypofluorescent.[36]
Figure 8.
Fluorescein angiography optic disk melanocytoma. Left: Clinical appearance of lesion. Right: Angiogram in mid venous phase showing hypofluorescence of lesion
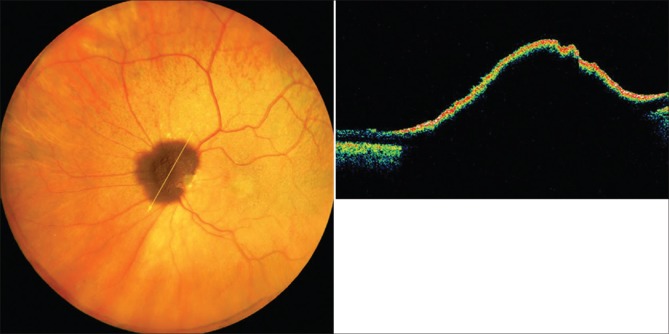
If a melanocytoma is greater than 0.5 mm in elevation, it often can be demonstrated with ultrasonography or computed tomography (CT) but these techniques cannot easily differentiate melanocytoma from other elevated lesions of the optic disk. Furthermore, ultrasonography cannot detect microscopic extension of the tumor into the retrolaminar portion of the optic nerve. Magnetic resonance imaging (MRI) can help determine the extent of gross involvement in the retrolaminar portion of the optic nerve, but is unlikely to detect microscopic extension. Optical coherence tomography is a new technique that has been used to evaluate optic disk melanocytoma (Fig. 9). Although the melanocytoma itself has no specific features with OCT, the technique appears to be useful in determining the extent of subretinal fluid and cystoid retinal edema, findings that cannot be easily detected with other methods.
Figure 9.
Optical coherence tomography (OCT) of optic disk melanocytoma. Left: Panoret image shows the darkly pigmented optic disk mass with adjacent retinal infiltration. Right: OCTshows a thin, delicate, echogenic line delineating the anterior aspect of the melanocytoma with abrupt and complete shadowing behind, obscuring all details of the optic disk and adjacent retina
Management
Because melanocytoma of the optic disk can rarely evolve into malignant melanoma, examination and fundus photography should be done yearly. Small degrees of growth may not signify malignant change. However, more progressive growth and visual loss should suggest malignant transformation and enucleation should be considered.
Summary
Melanocytoma is a peculiar variant of nevus that classically occurs in the optic disk but can involve the uveal tract. Optic disk melanocytoma may be confined to the optic disk or it may have contiguous involvement of the choroid or sensory retina. It is important to differentiate this benign lesion from a malignant melanoma. Histologically the melanocytoma is composed of deeply pigmented round to oval nevus cells with benign cytologic features. Although melanocytoma is typically a relatively stationary lesion, it can show mild growth in 10–15% of cases and can cause visual loss due to a variety of mechanisms. It can undergo spontaneous necrosis leading to more severe visual loss. More importantly, it can exhibit malignant transformation into melanoma in 1–2% of cases. A patient with a melanocytoma of the optic disk should be examined annually.
Method of Literature Search
Literature selection for this review was based on a MEDLINE database search, using the terms melanocytoma, optic nerve, optic disk, magnocellular nevus, melanoma, pseudomelanoma, retina, uvea from the period 1966 to 2005. Pertinent articles from the English-language literature were primarily selected but highly pertinent articles from the non-English- language literature were also quoted. Articles and reports from the authors' reprint collections were also included.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Outline
-
General considerations
- Historical perspectives
- Terminology
- Other ocular locations
-
Demographics
- Age
- Race
- Sex
-
Clinical features
- Laterality
- Multifocality
- Visual acuity
- Pupillary changes
- Visual fields
- Ophthalmoscopic features
- Ocular associations
- Systemic associations
-
Clinical course
- Local complications
- Growth
- Malignant transformation
Pathology
Pathogenesis
-
Differential diagnosis
- Choroidal melanoma
- Choroidal nevus
- Hyperplasia of retinal pigment epithelium (RPE)
- Combined hamartoma retina and RPE
- Adenoma of RPE
- Metastatic melanoma to optic disk
Diagnostic approaches
Management
Summary
Method of literature search
References
- 1.Apple D.J, Craythorn JM, Reidy JJ, et al. Malignant transformation of an optic nerve melanocytoma. Can J Ophthalmol. 1984;19:320–325. [PubMed] [Google Scholar]
- 2.Archdale T.W, Magnus DE. Melanocytoma of the optic disc. J Am Optom Assoc. 1993;64:98–103. [PubMed] [Google Scholar]
- 3.Balestrazzi E. Melanocytoma of the optic disk. Ophthalmologica. 1973;166:289–292. doi: 10.1159/000306824. [DOI] [PubMed] [Google Scholar]
- 4.Bartlett H.M, Willoughby B, Mandava N. Polypoidal choroidal vasculopathy in a patient with melanocytoma of the optic nerve. Retina. 2001;21:396–399. doi: 10.1097/00006982-200108000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Besada E, Shechtman D, Barr RD. Melanocytoma inducing compressive optic neuropathy: The ocular morbidity potential of an otherwise invariably benign lesion. Optometry. 2002;73:33–38. [PubMed] [Google Scholar]
- 6.Bisceglia M, Carosi I, Fania M, et al. Nevus of Ota Presentation of a case associated with a cellular blue nevus with suspected malignant degeneration and review of the literature. Pathologica. 1997;89:168–174. [PubMed] [Google Scholar]
- 7.Borsetto P, Mantovani E. Melanocytoma of the optic disc. Metab Pediatr Syst Ophthalmol. 1990;13:101–103. [PubMed] [Google Scholar]
- 8.Brodsky MC. Melanocytoma or congenital optic disk pigmentation? Am J Ophthalmol. 137:208–9. doi: 10.1016/j.ajo.2003.09.018. author reply 209–10, 2004. [DOI] [PubMed] [Google Scholar]
- 9.Brodsky M.C, Phillips PH. Optic nerve hypoplasia and congenital hypopituitarism. J Pediatr. 2000;136:850. [PubMed] [Google Scholar]
- 10.Brown G.C, Shields JA. Tumors of the optic nerve head. Surv Ophthalmol. 1985;29:239–264. [PubMed] [Google Scholar]
- 11.Busse H, Schiffer H.P. Melanocytoma of the papilla. Ophthalmologica. 1978;177:245–247. doi: 10.1159/000308774. [DOI] [PubMed] [Google Scholar]
- 12.Chervin M, Pablo de Vecchi H. Melanocytoma of the optic disk Fluoretinographic study. Arch Oftalmol B Aires. 1970;45:509–514. [PubMed] [Google Scholar]
- 13.Cogan D. Discussion; pigmented ocular tumors. In: M Boniuk., editor. Ocular and Adnexal Tumors. New and Controversial Aspects. St. Louis: CV Mosby Co; 1964. p. 385. [Google Scholar]
- 14.Cordes F.C, Hogan MJ. Primary malignant melanoma of the optic disk. Am J Ophthalmol. 1949;32:1037–1047. doi: 10.1016/0002-9394(49)90645-5. [DOI] [PubMed] [Google Scholar]
- 15.Costa J, Vargas E, Mendonca AP, Barbosa MS. Growing optic disk melanocytoma: What to do. Neuro-Ophthalmol. 2002;27:39–43. [Google Scholar]
- 16.Croxatto J.O, Ebner R, Crovetto L, et al. Angle closure glaucoma as initial manifestation of melanocytoma of the optic disc. Ophthalmology. 1983;90:830–834. doi: 10.1016/s0161-6420(83)34482-1. [DOI] [PubMed] [Google Scholar]
- 17.Demirci H, Shields CL, Shields JA. Bilateral optic disk melanocytoma in a 10-month-old infant. Am J Ophthalmol. 2003;136:190–192. doi: 10.1016/s0002-9394(03)00088-6. [DOI] [PubMed] [Google Scholar]
- 18.De Potter P, Shields CL, Eagle RC, et al. Malignant melanoma of the optic nerve. Arch Ophthalmol. 1996;114:608–612. doi: 10.1001/archopht.1996.01100130600020. [DOI] [PubMed] [Google Scholar]
- 19.de Veer J.A. Juxtapapillary malignant melanoma of the choroid and so-called malignant melanoma of the optic disk, a pathologic study. Arch Ophthalmol. 1954;51:147–160. doi: 10.1001/archopht.1954.00920040149001. [DOI] [PubMed] [Google Scholar]
- 20.de Veer J.A. Melanotic tumors of the optic nerve. A pathologic study. Arch Ophthalmol. 1961;65:536–541. doi: 10.1001/archopht.1961.01840020538013. [DOI] [PubMed] [Google Scholar]
- 21.Dubielzig R.R, Aguirre GD, Gross SL, et al. Choroidal melanomas in dogs. Vet Pathol. 1985;22:582–585. doi: 10.1177/030098588502200612. [DOI] [PubMed] [Google Scholar]
- 22.Eckhardt B, Hütz W. Melanocytoma—a case report. Klin Monatsbl Augenheilkd. 1990;197:46–49. doi: 10.1055/s-2008-1046242. [DOI] [PubMed] [Google Scholar]
- 23.Erzurum S.A, Jampol LM, Territo C, et al. Primary malignant melanoma of the optic nerve simulating a melanocytoma. Arch Ophthalmol. 1992;110:684–686. doi: 10.1001/archopht.1992.01080170106034. [DOI] [PubMed] [Google Scholar]
- 24.Fischer P, Müller-Jensen K, Frenzel H. Peripapillary melanoma; 10-year follow-up. Klin Monatsbl Augenheilkd. 2000;217:363–366. doi: 10.1055/s-2000-9576. [DOI] [PubMed] [Google Scholar]
- 25.François J, De Laey JJ, Kluyskens J, et al. Melanocytoma of the optic papilla. Bull Soc Belge Ophtalmol. 1980;187:111–125. [PubMed] [Google Scholar]
- 26.François J, de Laey JJ, Kluyskens J, et al. Melanocytoma of the optic disc. Ophthalmologica. 1980;180:314–327. doi: 10.1159/000308994. [DOI] [PubMed] [Google Scholar]
- 27.Gahankari M.D, Jehangir R, Bhatti SS. Melanocytoma of the optic disc. J Postgrad Med. 1992;38:135–136. [PubMed] [Google Scholar]
- 28.García-Arumí J, Salvador F, Corcostegui B, et al. Neuroretinitis associated with melanocytoma of the optic disk. Retina. 1994;14:173–176. doi: 10.1097/00006982-199414020-00012. [DOI] [PubMed] [Google Scholar]
- 29.Girard E, Jallet G, Ebran JM, et al. Melanocytoma of the papilla: apropos of 3 cases. Bull Soc Ophtalmol Fr. 84:1295–8. 1301–3, 1984. [PubMed] [Google Scholar]
- 30.Gupta V, Gupta A, Dogra MR, et al. Progressive growth in melanocytoma of the optic nerve head. Indian J Ophthalmol. 1995;43:198–200. [PubMed] [Google Scholar]
- 31.Haye C, Chic F, Coat JP. Course of melanocytoma of the optic disk. Bull Soc Ophtalmol Fr. 86:971–2. 974, 1986. [PubMed] [Google Scholar]
- 32.Horodeński J. Pigmented tumor of the optic nerve head (melanocytoma) Klin Oczna. 1969;39:469–472. [PubMed] [Google Scholar]
- 33.Howard G.M, Forrest AW. Melanocytoma of the disc complicated by hematoma under retinal pigment epithelium. Trans Am Acad Ophthalmol Otolaryngol. 1966;70:281–285. [PubMed] [Google Scholar]
- 34.Joffe L, Shields JA, Osher RH, et al. Clinical and follow-up studies of melanocytomas of the optic disc. Ophthalmology. 1979;86:1067–1083. doi: 10.1016/s0161-6420(79)35421-5. [DOI] [PubMed] [Google Scholar]
- 35.Juarez C.P, Tso MO. An ultrastructural study of melanocytomas (magnocellular nevi) of the optic disk and uvea. Am J Ophthalmol. 1980;90:48–62. doi: 10.1016/s0002-9394(14)75076-7. [DOI] [PubMed] [Google Scholar]
- 36.Kadayifcilar S, Akman A, Aydin P. Indocyanine green angiography of optic nerve head melanocytoma. Eur J Ophthalmol. 1999;9:68–70. doi: 10.1177/112067219900900112. [DOI] [PubMed] [Google Scholar]
- 37.Kiratli H, Bilgiç S, Gedik S. Late normalization of melanocytomalytic intraocular pressure elevation following excision of iris melanocytoma. Graefes Arch Clin Exp Ophthalmol. 2001;239:712–715. doi: 10.1007/s004170100349. [DOI] [PubMed] [Google Scholar]
- 38.Lauritzen K, Augsburger JJ, Timmes J. Vitreous seeding associated with melanocytoma of the optic disc. Retina. 1990;10:60–62. [PubMed] [Google Scholar]
- 39.Levine J. Primary melanosarcoma of the optic disk. Arch Ophthalmol. 1935;14:229–238. [Google Scholar]
- 40.Loeffler K.U, Tecklenborg H. Melanocytoma-like growth of a juxtapapillary malignant melanoma. Retina. 1992;12:29–34. doi: 10.1097/00006982-199212010-00007. [DOI] [PubMed] [Google Scholar]
- 41.Mansour A.M, Zimmerman L, La Piana FG, et al. Clinicopathological findings in a growing optic nerve melanocytoma. Br J Ophthalmol. 1989;73:410–415. doi: 10.1136/bjo.73.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meyer D, Ge J, Blinder KJ, et al. Malignant transformation of an optic disk melanocytoma. Am J Ophthalmol. 1999;127:710–714. doi: 10.1016/s0002-9394(99)00065-3. [DOI] [PubMed] [Google Scholar]
- 43.Milosevic B, Liticin O. The illusion of a primary melanoma of the optic disk. Arch Ophthalmol. 1957;58:217–224. doi: 10.1001/archopht.1957.00940010229008. [DOI] [PubMed] [Google Scholar]
- 44.Naumann G. Observation of a benign melanocytoma of the optic nerve papilla. Doc Ophthalmol. 1966;20:468–483. doi: 10.1007/BF00165435. [DOI] [PubMed] [Google Scholar]
- 45.Nicolás El-Haddad M, Clement Fernández F, Pérez-Salvador E, et al. Polypoidal choroidal vasculopathy in a patient with a melanocytoma of the optic nerve. Arch Soc Esp Oftalmol. 2002;77:455–458. [PubMed] [Google Scholar]
- 46.Osher R.H, Shields JA, Layman PR. Pupillary and visual field evaluation in patients with melanocytoma of the optic disc. Arch Ophthalmol. 1979;97:1096–1099. doi: 10.1001/archopht.1979.01020010550008. [DOI] [PubMed] [Google Scholar]
- 47.Phillpotts B.A, Sanders RJ, Shields JA, et al. Uveal melanomas in black patients: a case series and comparative review. J Natl Med Assoc. 1995;87:709–714. [PMC free article] [PubMed] [Google Scholar]
- 48.Rahimi-Movaghar V, Karimi M. Meningeal melanocytoma of the brain and oculodermal melanocytosis (nevus of Ota): Case report and literature review. Surg Neurol. 2003;59:200–210. doi: 10.1016/s0090-3019(02)01052-2. [DOI] [PubMed] [Google Scholar]
- 49.Reese A.B. Pigmentation of the optic nerve. Arch Ophthalmol. 1933;9:560–570. [Google Scholar]
- 50.Reidy J.J, Apple DJ, Steinmetz RL, et al. Melanocytoma: Nomenclature, pathogenesis, natural history and treatment. Surv Ophthalmol. 1985;29:319–327. doi: 10.1016/0039-6257(85)90107-9. [DOI] [PubMed] [Google Scholar]
- 51.Schachat A.P, Shields JA, Fine SL, et al. Combined hamartomas of the retina and retinal pigment epithelium. Ophthalmology. 1984;91:1609–1615. doi: 10.1016/s0161-6420(84)34094-5. [DOI] [PubMed] [Google Scholar]
- 52.Schardt W.M, Milewski SA. Melanocytoma tumor. Conn Med. 1972;36:432–435. [PubMed] [Google Scholar]
- 53.Schroeder H, Schauer A. The so-called melanocytoma of the optic nerve head. Klin Monatsbl Augenheilkd. 1965;146:593–597. [PubMed] [Google Scholar]
- 54.Servodidio CA, Abramson DH, Romanella A. Melanocytoma. J Ophthalmic Nurs Technol. 9:255. 263, 1990. [PubMed] [Google Scholar]
- 55.Sharma P.M, Sangal K, Malik P, et al. Malignant transformation of optic disc melanocytoma? A clinical dilemma at presentation with a review of the literature. Ophthalmologica. 2002;216:292–295. doi: 10.1159/000063845. [DOI] [PubMed] [Google Scholar]
- 56.Shields J.A. Melanocytoma of the optic nerve head: A review. Int Ophthalmol. 1978;1:31–37. doi: 10.1007/BF00133275. [DOI] [PubMed] [Google Scholar]
- 57.Shields J.A, Demirci H, Shields CL. Melanocytoma or congenital optic disk pigmentation ([letter]) Am J Ophthalmol. 2004;137:209–210. doi: 10.1016/j.ajo.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 58.Shields J.A, Demirci H, Mashayekhi A, et al. Melanocytoma of optic disc in 115 cases: The 2004 Samuel Johnson Memorial Lecture, part 1. Ophthalmology. 2004;111:1739–1746. doi: 10.1016/j.ophtha.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 59.Shields J.A, Eagle RC, Barr CC, et al. Adenocarcinoma of retinal pigment epithelium arising from a juxtapapillary histoplasmosis scar. Arch Ophthalmol. 1994;112:650–653. doi: 10.1001/archopht.1994.01090170094029. [DOI] [PubMed] [Google Scholar]
- 60.Shields J.A, Eagle RC, Shields CL, et al. Pigmented adenoma of the optic nerve head simulating a melanocytoma. Ophthalmology. 1992;99:1705–1708. doi: 10.1016/s0161-6420(92)31734-8. [DOI] [PubMed] [Google Scholar]
- 61.Shields J, Shields C.L. Melanocytoma. In: J.A Shields, C.L Shields., editors. Intraocular Tumors. A Text and Atlas. Philadelphia: WB Saunders Co; 1992. pp. 101–115. [Google Scholar]
- 62.Shields J.A, Shields C.L. Melanocytoma. In: J.A Shields, C.L Shields., editors. Atlas of Intraocular Tumors. Philadelphia: Lippincott Williams and Williams; 1999. pp. 324–325. [Google Scholar]
- 63.Shields J.A, Shields CL, Eagle RC, et al. Malignant melanoma associated with melanocytoma of the optic disc. Ophthalmology. 1990;97:225–230. doi: 10.1016/s0161-6420(90)32601-5. [DOI] [PubMed] [Google Scholar]
- 64.Shields J.A, Shields CL, Eagle RC, et al. Central retinal vascular obstruction secondary to melanocytoma of the optic disc. Arch Ophthalmol. 2001;119:129–133. [PubMed] [Google Scholar]
- 65.Shields J.A, Shields CL, Gündüz K, et al. Neoplasms of the retinal pigment epithelium: The 1998 Albert Ruedemann, Sr, memorial lecture, Part 2. Arch Ophthalmol. 1999;117:601–608. doi: 10.1001/archopht.117.5.601. [DOI] [PubMed] [Google Scholar]
- 66.Shields J.A, Shields C, Lavrich J. Melanocytoma of optic disk in a patient with neurofibromatosis 2. Retina. 2002;22:222–223. doi: 10.1097/00006982-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 67.Shields J.A, Shields CL, Piccone M, et al. Spontaneous appearance of an optic disk melanocytoma in an adult. Am J Ophthalmol. 2002;134:614–615. doi: 10.1016/s0002-9394(02)01590-8. [DOI] [PubMed] [Google Scholar]
- 68.Shields J.A, Shields CL, Singh AD. Metastatic neoplasms in the optic disc: the 1999 Bjerrum Lecture: part 2 Arch. Ophthalmol. 2000;118:217–224. doi: 10.1001/archopht.118.2.217. [DOI] [PubMed] [Google Scholar]
- 69.Shinoda K, Hayasaka S, Nagaki Y, et al. Melanocytoma of the left optic nerve head and right retrobulbar optic neuropathy compressed by a tuberculum sellae meningioma. Ophthalmologica. 2000;214:161–163. doi: 10.1159/000027489. [DOI] [PubMed] [Google Scholar]
- 70.Shuey T.F, Blacharski PA. Pigmented tumor and acute visual loss. Surv Ophthalmol. 1988;33:121–126. doi: 10.1016/0039-6257(88)90164-6. [DOI] [PubMed] [Google Scholar]
- 71.Stroh E.M, Chen S, Jalkh AE. Melanocytoma with juxtapapillary nevus: premalignant or benign. Ann Ophthalmol. 1993;25:429–430. [PubMed] [Google Scholar]
- 72.Takahashi T. Clinicopathological findings of melanocytomas on the optic disc (author's transl) Klin Monatsbl Augenheilkd. 1979;175:47–55. [PubMed] [Google Scholar]
- 73.Takahashi T, Isayama Y, Okuzawa I. Unusual case of melanocytoma in optic disk. Jpn J Ophthalmol. 1984;28:171–175. [PubMed] [Google Scholar]
- 74.Thomas C.I, Purnell EW. Ocular melanocytoma. Am J Ophthalmol. 1969;67:79–86. doi: 10.1016/0002-9394(69)90011-7. [DOI] [PubMed] [Google Scholar]
- 75.Usui T, Shirakashi M, Kurosawa A, et al. Visual disturbance in patients with melanocytoma of the optic disk. Ophthalmologica. 1990;201:92–98. doi: 10.1159/000310133. [DOI] [PubMed] [Google Scholar]
- 76.Walsh T.J, Packer S. Bilateral melanocytoma of the optic nerve associated with intracranial meningioma. Ann Ophthalmol. 1971;3:885–888. [PubMed] [Google Scholar]
- 77.Wiznia R.A, Price J. Recovery of vision in association with a melanocytoma of the optic disk. Am J Ophthalmol. 1974;78:236–238. doi: 10.1016/0002-9394(74)90083-x. [DOI] [PubMed] [Google Scholar]
- 78.Yamaguchi K, Shiono T, Mizuno K. Pigment deposition in the anterior segment caused by melanocytoma of the optic disc. Ophthalmologica. 1987;194:191–193. doi: 10.1159/000309764. [DOI] [PubMed] [Google Scholar]
- 79.Zimmerman L.E. Pigmented tumors of the optic nerve head The 22nd Annueal de Schweinitz Lecture. Am J Ophthalmol. 1960;50:338. [Google Scholar]
- 80.Zimmerman L.E. Melanocytes, melanocytic nevi and melanocytomas. Invest Ophthalmol. 1965;4:11–41. [PubMed] [Google Scholar]
- 81.Zimmerman L.E, Garron LK. Melanocytoma of the optic disk. Int Ophthalmol Clin. 1962;2:431–440. [Google Scholar]
- 82.Zografos L, Uffer S, Gailloud C, et al. Malignant melanoma of the optic disk A case report (author's transl) Klin Monatsbl Augenheilkd. 1982;180:503–509. doi: 10.1055/s-2008-1055136. [DOI] [PubMed] [Google Scholar]