Abstract
Background
The clinical treatment of patients with severe diabetic foot (DF) is difficult. Recently, the First Affiliated Hospital of Guangxi Medical University began to apply tibial transverse transport (TTT) in patients with DF. This treatment has achieved significant effects, but its mechanism of action is unclear. Recently, microcirculation and the pathogenesis of diabetes have become the foci of research in this field. The evaluation of the possible mechanism of microcirculation reconstruction requires relevant indicators. The aim of this study was to investigate the value of computed tomography perfusion in evaluations of the curative effects of TTT and establish corresponding quantitative evaluation indicators.
Methods
Twelve patients with DF treated with TTT were recruited as the research participants. All diabetic feet were divided into the transport foot (TF) group and nontransport foot (NTF) group according to whether the patients underwent TTT. All patients underwent CT shuttle scanning preoperatively and 8 weeks after surgery. The shuttle scan data were transferred to Siemens VPCT body software and postprocessed with Customized Tumor2. We chose the TF posterior tibial artery from a distance of approximately 15 cm to the bifurcation of the plantar medial artery and the lateral plantar artery as the input artery. We selected the centre of the bilateral medial plantar muscle group on the coronal and axial regions of interest. We applied a deconvolution approach to obtain data from both sides of the plantar tissue perfusion. Skin temperature (ST) detection was performed with an ST gun to measure the average ST values in the dorsal and plantar areas, the first and fifth heads of the phalanges, and the medial and lateral malleolus points of both feet of patients with DF preoperatively and 8 weeks after surgery.
Results
The preoperative and postoperative ST values of the patients in the TF group were 30.73 ± 1.86 °C and 32.22 ± 1.51 °C, respectively. The preoperative and postoperative ST values for the patients in the NTF group were 30.93 ± 2.65 °C and 32.07 ± 2.09 °C, respectively. There were significant differences in the preoperative and postoperative data between the TF (P = 0.001) and NTF (P = 0.013) groups. In the patients with DF who underwent TTT, there were both preoperative and postoperative differences inside the medial plantar muscle group in the relative blood volume (rBV) value and relative mean transit time (rMTT) (P = 0.027, P = 0.026, respectively). The postoperative BV in the NTF group was increased compared with the preoperative BV (P = 0.006).
Conclusion
There were significant differences in relative BV, relative mean transit time, and ST between the two groups before and after surgery, and the postoperative BV in the NTF group and ST values in the two groups were increased compared with the preoperative values. The BV in the NTF group and the ST values in the two groups were effective indicators in evaluating the changes between preoperative and postoperative perfusion. These results indicate that TTT could increase plantar tissue perfusion as assessed by BV and ST; this increase was among the reasons for the surface healing of severe DF ulcers.
Translational potential of this article
Preoperative CT perfusion evaluation can provide relevant information of blood vessels and microcirculation for clinical operation, and postoperative CT perfusion evaluation can provide postoperative efficacy evaluation for clinical operation. All patients received information about the study and signed a specific informed consent. Approval for this study was granted by the regional ethics committee [Regional Ethics Committee of the First Affiliated Hospital of Guangxi Medical University, China [(2018-(KY-E-069].
Keywords: CT perfusion, Curative effect evaluation, Severe diabetic foot, Shuttle scan, Tibial transverse transport
Introduction
Diabetic foot (DF) is a common complication of diabetes, and microvascular disease represents the specific lesions that occur [1]; however, the current comprehensive treatment of [2], [3] DF Wagner grade III-V patients is still associated with a 21% amputation rate and some requirements for multiple amputations [4]. In recent years, some domestic scholars investigating bone external fixation technology have expanded the treatment modalities with Chinese elements and evaluated the Ilizarov tibial transverse transport (TTT) treatment for limb ischaemia [5], [6], [7]. However, currently, this technique is not widely used for the treatment of DF.
Our hospital has treated more than 100 patients with refractory Wagner III-V DF with TTT, and the limb salvage effects were remarkable [8]. However, the current basic theory of orthopaedics cannot satisfactorily explain the extraordinary efficacy of TTT in repairing the peculiar effects of diabetes, and relevant indicators need to be evaluated to determine the possible mechanism of microcirculation reconstruction [9].
Currently, there is no gold standard for evaluating microcirculatory function, and multimodality comprehensive evaluation methods are necessary. Computed tomography perfusion (CTP) imaging is a relatively developed, noninvasive, repeatable, quantitative, and semiquantitative functional imaging technique that can effectively assess the blood perfusion status and haemodynamic properties in living tissue. CTP can also reflect the microvascular characteristics of organized tissue [10] to a certain extent.
In this study, CTP was used to evaluate the blood perfusion status before and after TTT. The CTP technique was used to evaluate the curative effect of TTT under the guidance of the tension-stress rules of Ilizarov and provide a theoretical basis for evaluating the curative effect of TTT in DF.
Materials and methods
Ethical approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patients
Hospitalized patients with severe DF younger than 70 years whose diabetes course was not limited were recruited from December 2015 to February 2017 at the First Affiliated Hospital of Guangxi Medical University and the Affiliated Hospital of Guilin Medical University for orthopaedic surgery. Diabetes was diagnosed by a diabetes specialist and staged by Wagner staging. The diabetes diagnosis was based on the 2005 World Health Organization Diabetes Expert Committee on Diabetes Diagnostic Criteria.
Inclusion criteria
Patients with severe DF (Wagner grade III or above) with TTT surgical indications were assessed for orthopaedic surgery. The patients signed an informed consent before the operation.
Exclusion criteria
The surgical exclusion criteria included any of the following contraindications: (1) recent severe chronic diabetic complications or other stress conditions, such as acute myocardial infarction and cerebrovascular accidents; (2) severe liver dysfunction; (3) severe lung infection, cardiopulmonary dysfunction, poor control, or heart failure; (4) severe hypoproteinaemia or haemoglobin less than 90 g/L; and (5) peripheral arterial lesions in the lower extremity arteries, including lesions to the upper level of the popliteal artery that cannot be recommunicated (preoperative ultrasound examination was performed to exclude these lesions) as clinical data show that such artery occlusion in the knee joint cannot be recanalized, and TTT surgery is not effective.
The CTP exclusion criteria were as follows: (1) branches of the bilateral popliteal artery lesions leading to severe vascular wall sclerosis (perfusion values were not detectable because of severe vascular wall calcification); (2) contrast agent allergies or patients in whom vascular puncture was difficult to perform because of swelling, bleeding, or other adverse reactions; and (3) kidney dysfunction (creatinine clearance (Ccr): 70 ml/min-20 ml/min).
TTT surgical method
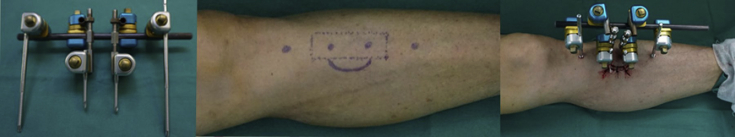
The installation of the bone transfer frame was performed using the following protocol. After anaesthesia, two 2.5-cm arc incisions were performed in the middle of the tibia, and the interval between the two incisions was 3 cm. After the separation of the subcutaneous tissue, two 3.5-cm × 1.5-cm bone windows were created at the two incisions with the principle of a “moving skin window”; a minimally invasive 2-cm perforated osteotomy device, or “日”-type osteotomy to effectively reduce the complications of fracture after osteotomy. A 60 × 4-mm Shashi needle (Double Medical Technology Co., Ltd., Residence: No. 18 Shanbian Hongdong Road, Haicang District, Xiamen City, China, Phone: +86 400-860-2618, double-medical.com) was screwed into each of the two bone windows to remove them. In addition, two 120 × 4-mm external fixation needles were screwed into the distal and proximal ends of the surgical area, the fixation needle and external tibia removal frame were screwed, the nut and connecting rod were adjusted and tightened, the direction and location of the bone removal were marked, skin silk suturing was performed, and the dressing was wrapped and removed [11]. The framework of the external fixation and the basic surgical methods are shown in Figure 1.
Figure 1.
Flow chart of TTT. TTT = tibial transverse transport.
ST measurement method
The air conditioning temperature was set to 25 °C; the doors, windows, and curtains were closed; and the lower limbs were exposed for 30 min before performing the ST measurement. ST detection was performed with an ST gun to measure the average ST values of the dorsal and plantar areas, the first and fifth heads of the phalanges, and the medial and lateral malleolus points of both feet of patients with DF preoperatively and 8 weeks after surgery.
Test grouping
All diabetic feet were divided into the transport foot (TF) and nontransport foot (NTF) groups according to whether the patients underwent TTT. The two groups were evaluated in preoperative and postoperative comparative studies.
CT scan
All patients with DF underwent a double lower extremity CT plain scan and shuttle scanning with a Siemens 64 CT scanner preoperatively and 8 weeks after surgery. All patients with DF signed an informed consent form. Radioprotection, fixation, and other preparatory work were completed.
Double lower extremity CT plain scan
The range included the abdominal aorta from the beginning of the plantar area with a layer thickness of 5 mm, a pitch of 0.6 mm, a voltage of 120 KV, and a current of 35 mAs.
Double lower extremity CT shuttle scanning
A Siemens Somatom definition Flash scan (Global Siemens Healthcare Headquarters, siemens AG, Healthcare Sector, Imaging and IT Division, Henkestr. 127, 91052 Erlangen, Germany, Phone:+49 9131 84-0, www.siemens.com/healthcare) was used with a voltage of 80 kV, a current of 100 mAs [12], [13], a 4D range of 284 mm, a Dynamic 4D shuttle scan dose length product of 1806.7 mGycm, a scan time of 69.53 s, a dynamic scan of 27 phases, and 370 mg/ml iopromide as the contrast agent at a dose of 90 ml. The injection speed was 4.5 ml/s, and the contrast agent was administered with a Nemoto-type high-pressure double-tube syringe (Nemoto Kyorindo Co.,Ltd., 2-27-20, Hongo, Bunkyo-Ku., Tokyo, 113-0033, Japan) in the anterior elbow vein group. The shuttle scan of the lower limbs (from the plantar area to the middle tibial area) was initiated 18 s after the contrast agent injection.
Image analysis
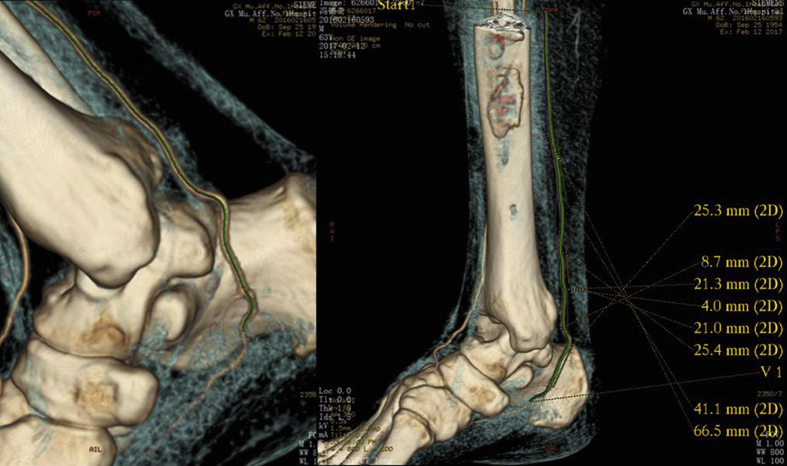
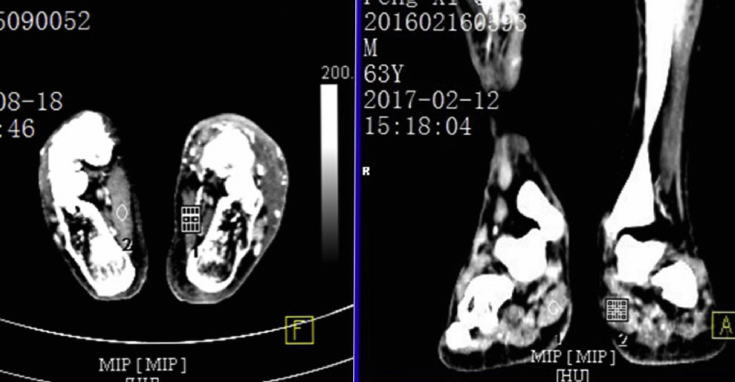
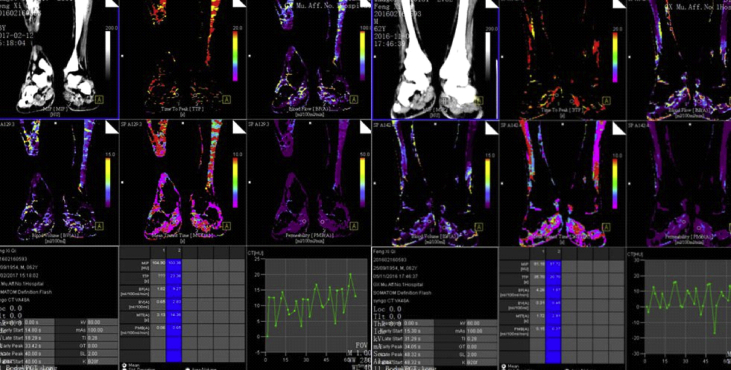
The 27-sequence shuttle scan data were transferred to Siemens VPCT body software (Global Siemens Healthcare Headquarters, siemens AG, Healthcare Sector, Imaging and IT Division, Henkestr. 127, 91052 Erlangen, Germany, Phone:+49 9131 84-0, www.siemens.com/healthcare) and postprocessed with Customized Tumor2 (Global Siemens Healthcare Headquarters, siemens AG, Healthcare Sector, Imaging and IT Division, Henkestr. 127, 91052 Erlangen, Germany, Phone:+49 9131 84-0, www.siemens.com/healthcare). We used a “Patlak” tracer kinetic model. The perfusion organization threshold was defined in the range of −50 Hu to 150 Hu after the motion artefact correction. We chose the TF posterior tibial artery from a distance of approximately 15 cm to the bifurcation of the plantar medial artery and the lateral plantar artery as the input artery (Figure 2). We selected the centre of the bilateral medial plantar muscle group on coronal and axial images as the region of interest (Figure 3, Figure 4). A deconvolution approach was applied to evaluate the perfusion parameters, including blood flow (BF), blood volume (BV), mean transit time (MTT), time to peak (TTP), permeability, and maximal intensity projection, of both sides of the plantar tissues, and a corresponding function diagram was obtained based on the targeted blood vessel's time–density curve (Figure 5, Figure 6). The patients with DF in this group all had unilateral foot ulcers, and the transport side was the ulcer side. TTT may play a role in both feet; therefore, we first evaluated the difference between the two feet before and after surgery with the relative value as follows: R=(TF perfusion value-NTF perfusion value)/NTF perfusion value.
Figure 2.
Measurement of the length of the target vessel. 2D = two-dimensional.
Figure 3.
Map of the medial plantar muscle groups (abductor muscles).
Figure 4.
Perfusion ROI in the axial and coronal positions of the bilateral medial plantar muscle group. ROI = region of interest.
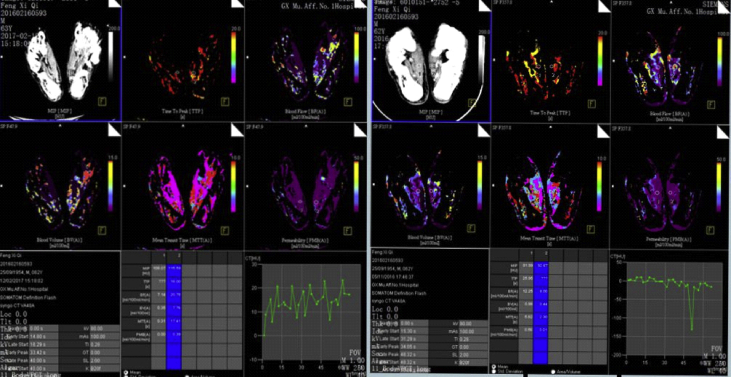
Figure 5.
Coronal shuttle scanning perfusion images with contrast of the bilateral medial plantar muscle groups (the left picture is postoperative and the right is preoperative). There were differences between the preoperative and postoperative BV and MTT values in the bilateral medial plantar muscle groups, and the postoperative BV in the NTF group was increased compared with the preoperative BV in the same group. BV = blood volume; MTT = mean transit time; NTF = nontransport foot.
Figure 6.
Double inside medial plantar muscle group shuttle scanning perfusion contrast on axial imaging (the left picture is postoperative and the right is preoperative). The image is approximately the same as the coronal image.
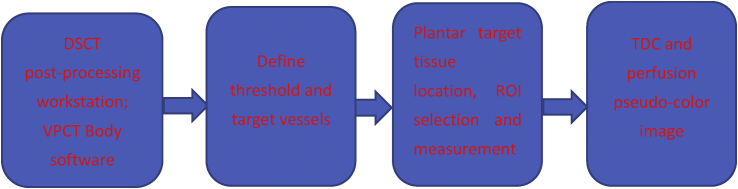
The postprocessing of the CT shuttle scan perfusion data is shown in the following figure:
Statistical analysis
All data in the study included measurement variables and were analysed using SPSS Statistics 17.0 statistical software (SPSS Inc., 233 South Wacker Drive, llth Floor, Chicago, IL 60606-6412, Phone:(312)651-3000, Fax:(312)651-3668, www.spss.com). We used P-P figures to test where the data were normally distributed, and paired t tests were used to test for statistically significant differences between the groups; the data are presented as the mean ± standard deviation. A P value < 0.05 was considered statistically significant.
Results
General characteristics of the patients with DF
In total, 12 patients (10 men and 2 women) were included in this study. The average age was 55 ± 7 years. All patients had unilateral foot ulcers (10 left and 2 right), and 12 patients underwent TTT for the ulcerated foot. Five patients had Wagner's grade IV DF ulcers, and 7 patients had Wagner's grade III DF ulcers. In 7 patients, the ulcerated area was less than 5 cm × 5 cm, and in 5 patients, the ulcerated area was greater than 5 cm × 5 cm. Eleven patients experienced healing of their DF ulcers, except for 1 patient who developed a fracture after TTT and did not heal.
The ST values preoperatively and eight weeks after surgery among the patients in the TF group were 30.73 ± 1.86 °C and 32.22 ± 1.51 °C, respectively. The ST values preoperatively and eight weeks after surgery among the patients in the NTF group were 30.93 ± 2.65 °C and 32.07 ± 2.09 °C, respectively. There was a significant difference between the preoperative and postoperative data in the TF group (P = 0.001). There was also a significant difference between the preoperative and postoperative data in the NTF group (P = 0.013). See Table 1 for details.
Table 1.
Comparison of the average ST values in the two feet of patients with DF preoperatively and postoperatively (x ± s).
| Groups | Preoperative ST | Postoperative ST | t | p |
|---|---|---|---|---|
| TF group | 30.73 ± 1.86 °C | 32.22 ± 1.51 °C | −4.616 | 0.001 |
| NTF group | 30.93 ± 2.65 °C | 32.07 ± 2.09 °C | −2.940 | 0.013 |
NTF = nontransport foot; ST = skin temperature; TF = transport foot.
Comparison of the relative values of the perfusion parameters in the medial plantar muscle groups preoperatively and postoperatively
The preoperative and postoperative values of the relative BV (rBV) were 1.375 ± 1.974 and −0.225 ± 0.491, respectively, and the preoperative and postoperative values of the relative MTT were 0.150 ± 0.653 and −0.555 ± 0.382, respectively. The relative values of the postoperative rBV and relative MTT values were significantly lower than those before surgery and were statistically significantly different (P = 0.027 and P = 0.026, respectively). See Table 2 for details.
Table 2.
Comparison of the relative perfusion parameters of the medial plantar muscle groups preoperatively and postoperatively (x ± s).
| Relative perfusion parameters | Preoperatively | Postoperatively | t | p |
|---|---|---|---|---|
| rBF | 1.282 ± 1.531 | 1.542 ± 2.379 | −0.342 | 0.739 |
| rBV | 1.375 ± 1.974 | −0.225 ± 0.491 | 2.584 | 0.027 |
| rMTT | 0.150 ± 0.653 | −0.555 ± 0.382 | 2.613 | 0.026 |
| rPMB | 2.266 ± 2.276 | 0.744 ± 0.446 | 1.827 | 0.098 |
| rTTP | −0.042 ± 0.294 | −0.174 ± 0.127 | 1.148 | 0.278 |
| rMIP | −0.174 ± 0.446 | −0.237 ± 0.417 | 1.338 | 0.211 |
rPMB = relative permeability; rBF = relative blood flow; rBV = relative blood volume; rMIP = relative maximal intensity projection; rMTT = relative mean transit time; rTTP = relative time to peak.
Each relative perfusion parameter value, including the rBF, rBV, rMTT, rPMB, rMIP, and rTTP, had a ratio of 1.
Comparison of the perfusion parameters in the medial plantar muscle groups preoperatively and postoperatively
TF group
The preoperative and postoperative BF values in the TF group were 9.830 ± 5.450 and 37.601 ± 39.844, respectively. The postoperative BF value was significantly higher than the preoperative BF value, and the difference was statistically significant (P = 0.044). However, because the postoperative BF value was statistically discrete (the standard deviation was greater than the mean), we could not use the BF value in the TF group to evaluate the perfusion changes before and after TTT.
The postoperative BV value (1.997 ± 1.898) was higher than the preoperative BV value (1.426 ± 1.155), but the difference was not statistically significant (P = 0.247). See Table 3 for details.
Table 3.
Comparison of the perfusion parameters of the medial plantar muscle groups preoperatively and postoperatively (x ± s).
| Groups | Perfusion parameters | Preoperatively | Postoperatively | t | p |
|---|---|---|---|---|---|
| TF group | BF | 9.830 ± 5.450 | 37.601 ± 39.844 | −2.306 | 0.044 |
| BV | 1.426 ± 1.155 | 1.997 ± 1.898 | −1.231 | 0.247 | |
| MTT | 11.454 ± 10.406 | 4.532 ± 3.418 | 2.087 | 0.063 | |
| PMB | 2.524 ± 1.863 | 4.395 ± 4.370 | −1.450 | 0.178 | |
| MIP | 69.904 ± 38.955 | 63.524 ± 39.627 | 1.468 | 0.173 | |
| TTP | 27.721 ± 9.402 | 25.392 ± 5.822 | 0.763 | 0.463 | |
| NTF group | BF | 5.881 ± 3.998 | 22.221 ± 22.394 | −2.742 | 0.021 |
| BV | 0.956 ± 0.561 | 2.770 ± 1.561 | −3.443 | 0.006 | |
| MTT | 9.590 ± 10.590 | 11.923 ± 8.153 | −0.570 | 0.581 | |
| PMB | 0.859 ± 0.563 | 3.661 ± 5.787 | −1.640 | 0.132 | |
| MIP | 86.611 ± 10.763 | 86.558 ± 13.795 | 0.012 | 0.990 | |
| TTP | 28.547 ± 9.308 | 29.975 ± 3.767 | −0.510 | 0.622 |
BF = blood flow; BV = blood volume; MIP = maximal intensity projection; MTT = mean transit time; NTF = nontransport foot; PMB = permeability; TF = transport foot; TTP = time to peak.
The units of the perfusion parameters were as follows: BF, ml/100 ml/min; BV, ml/100 ml; MTT, s; PMB, ml/100 ml/min; MIP, HU; and TTP, s.
NTF group
The preoperative and postoperative BF values in the NTF group were 5.881 ± 3.998 and 22.221 ± 22.394, respectively, and the preoperative and postoperative rBV values were 0.956 ± 0.561 and 2.770 ± 1.561, respectively. The postoperative BF and BV values were significantly higher than the preoperative values, and the differences were statistically significant (P = 0.021 and P = 0.006, respectively). Therefore, we could use the BV value in the NTF group to evaluate the perfusion changes before and after TTT but could not use the BF value in the NTF group because the postoperative BF value was statistically discrete. See Table 3 for details.
Discussion
VPCT body perfusion measurement software has been widely and fully used in mature applications, such as in pancreatic organs [14], [15], [16], [17]. In this study, Siemens VPCT body perfusion software was also used for lower limb CTP. Owing to the complex settings of the lower limb CTP parameters, long scanning time, and relatively difficult data collection, clinical applications and scientific research are rare. In this study, our perfusion data were consistent with the clinical symptoms and signs, confirming the credibility of the lower limb CTP.
Characteristics and significance of perfusion of the medial plantar muscle groups before and after TTT
Skin temperature
ST is closely related to the microcirculatory perfusion involved in BF and tissue metabolism [18], [19]. The preoperative ST in the TF group was significantly lower than that in the NTF group, and the postoperative ST in the TF group was higher than the preoperative ST in the same group. These two sets of data were statistically significant. This result indicates that the preoperative BF in the TF group was lower than that in the NTF group and that TTT could effectively improve perfusion as assessed by BF.
Blood flow
BF is measured by BV in blood vessels per unit time and is directly related to the body's BV, tissue oxygen consumption, and the patency of venous and lymphatic drainage. In this study, in both the NTF and TF groups, the postoperative BF value of the plantar medial muscle groups was significantly higher than the preoperative BF value of these muscle groups, and both groups demonstrated significant differences. The variance in the BF value between the two groups was greater than the mean; thus, the data were discrete, and the rBF was statistically meaningless; therefore, BF could not be used to evaluate the curative effect of TTT.
Blood volume
BV is the volume of blood in tissue and blood vessels, reflects the microcirculation of tissues, and includes the size and number of functional capillaries. In this study, the postoperative BV value in the NTF group was higher than the preoperative BV value in the same group, and this difference was statistically significant (Table 3). The comparison of the preoperative and postoperative rBV values was statistically significant. These results show that BV is an effective perfusion index in evaluating TTT because TTT could increase the perfusion capacity of the plantar tissues and may increase the opening of functional capillaries.
In this study, the reasons for the increase in the BF and BV values after the TTT surgery were first considered to be related to the increase in or recanalization of blood vessels caused by the surgery and the improvement in microcirculation. Second, the disappearance of ulcer foot oedema after the TTT surgery was considered, and the measured BF and BV values were changed. According to the literature, the BF and BV values in volume perfusion computed tomography (VPCT) examinations of pancreatic inflammatory oedema tissue are decreased compared with those in normal tissue [15], [16], [17].
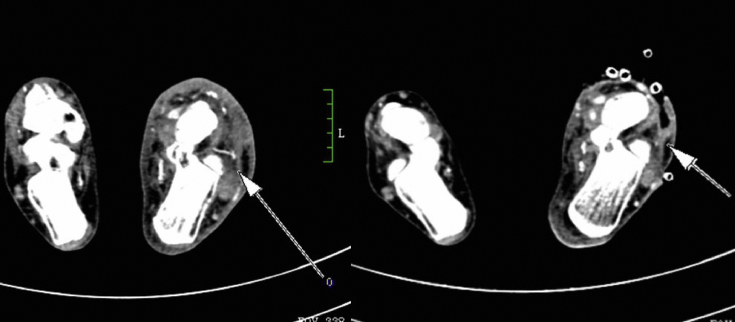
Possible mechanism
In our study, 12 cases of severe DF ulcers were healed after surgery, the skin temperature of both feet was higher than that before surgery, and the postoperative perfusion of both feet was higher than that before surgery. To some extent, the perfusion energy is known to reflect the characteristics of microcirculation and blood oxygen content [14], [20]. However, there was a typical case in which the bottom of the left transport foot showed a new small blood vessel after surgery (see Figure 7). Microcirculation angiogenesis and recanalization after TTT and changes in blood vessels have been suggested to directly lead to physiological changes, especially in perfusion BV [20]. Thus, microcirculation can be improved, limb blood supply can be restored, sufficient oxygen and nutrition supplies can be guaranteed, and ulcer wound healing or regeneration and repair can be promoted. The relationship between tension pressure conduction regulation and microcirculation reconstruction was considered. This relationship is consistent with the idea of the tension-stress law proposed by Birch [21]. Interestingly, in our study, the postoperative perfusion BF and BV values and the increase in skin temperature were bilateral, and the measurements were performed only on the side of the foot ulcer. We speculate that the following reasons could explain this result. On the one hand, diabetes is a systemic disease. The healing of a severe DF ulcer on one side and the improvement of limb microcirculation may have an impact on the whole body. On the other hand, some scholars believe that distraction osteogenesis technology has currently entered the stage of distraction histogenesis [22], [23]. The transport can stimulate the regeneration of the periosteum and tibial marrow [24]. Bone formation during distraction osteogenesis is accompanied by a robust induction of factors associated with angiogenesis [25]. If the ulcer surface does not heal but tissue regeneration occurs, the Ilizarov “tension-stress law” biological theory hypothesis [22] has very good rationality, that is, “biological tissues under a sustained, stable, and slow pull can stimulate cell division and generate tissues, which can repair various body defects”. This hypothesis needs to be further studied in animal experiments.
Figure 7.
The bottom of the left transport foot showing a new small blood vessel after surgery (the left picture is postoperative and the right is preoperative).
Our study had some limitations. First, some additional radiation exposure was inevitable. We minimized this exposure by using the lowest tube voltage and tube setting (80 kV and 100 mAs, respectively) that still provides adequate image quality for perfusion maps. The estimated effective radiation dose in our perfusion series was approximately 0.90335 mSv, which is lower than the annual public radiation dose of 1.0 mSv. Second, the number of cases in our study was small because case collection was relatively difficult as CTP tests were required to exclude severe diabetic feet with impaired renal function. Third, the contrast agent should be heated to body temperature to maximally ensure the accuracy of the perfusion measurement.
Acknowledgements
This work was supported by the National Natural Science Fund of China (grant No. 81660287).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2019.04.005.
Contributor Information
Zisan Zeng, Email: zengzisan@aliyun.com.
Yan Dong, Email: 894367097@qq.com.
Qikai Hua, Email: hqk100@yeah.net.
XiaoCong Kuang, Email: kuangxiaocong@gxmu.edu.cn.
Kai Li, Email: 806390953@qq.com.
Xianyu Deng, Email: 848129850@qq.com.
Shaohua Qiu, Email: 1203356864@qq.com.
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
Author's contribution
Zisan Zeng, Yan Dong, and Qikai Hua contributed to the conception and design of study. Yan Dong, Xianyu Deng, and Shaohua Qiu contributed to acquisition of data. Yan Dong, Kai Li, Xiaocong Kuang and Zisan Zeng contributed to the analysis and/or interpretation of data. Yan Dong, Zisan Zeng, and Xianyu Deng contributed to drafting of the manuscript. Qikai Hua, Xiaocong Kuang, and Kai Li contributed to revising the manuscript critically for important intellectual content. Zisan Zeng, Yan Dong, Qikai Hua, Xiaocong Kuang, Kai Li, Xianyu Deng, and Shaohua Qiu approved the version of the manuscript to be published (the names of all authors must be listed).
Appendix 1. Supplementary data
The following is the supplementary data to this article:
References
- 1.Goldstone R.L. 2000. Diabetes mellitus[M]//Medical selection of life risks. [Google Scholar]
- 2.Guideline on the diagnosis and treatment of diabetic foot. J Interv Radiol. 2013;09:705–708. [Google Scholar]
- 3.Ferguson J.Y., Sutherland M., Pandit H.G., McNally M. The rate of symptomatic venous thromboembolism in patients undergoing elective Ilizarov surgery and the cost of chemical prophylaxis. Bone Joint Lett J. 2014;96-B(3):426–430. doi: 10.1302/0301-620X.96B3.32939. [DOI] [PubMed] [Google Scholar]
- 4.Costa R.H.R., Cardoso N.A., Procópio R.J., Navarro T.P., Dardik A., Ligia D.L.C. Diabetic foot ulcer carries high amputation and mortality rates, particularly in the presence of advanced age, peripheral artery disease and anemia. Diabetes Metab Syndrome: Clin Res Rev. 2017 doi: 10.1016/j.dsx.2017.04.008. S1871402117300826. [DOI] [PubMed] [Google Scholar]
- 5.Ramanujam C.L., Zgonis T. An overview of internal and external fixation methods for the diabetic charcot foot and ankle. Clin Podiatr Med Surg. 2017;34(1):25–31. doi: 10.1016/j.cpm.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Brandão R.A., Weber J.S., Larson D., Prissel M.A., Bull P.E., Berle G.C. New fixation methods for the treatment of the diabetic foot. Clin Podiatr Med Surg. 2017;35(1) doi: 10.1016/j.cpm.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Elalfy B., Ali A.M., Fawzy S.I. Ilizarov external fixator versus retrograde intramedullary nailing for ankle joint arthrodesis in diabetic charcot neuroarthropathy. J Foot Ankle Surg. 2017;56(2):309–313. doi: 10.1053/j.jfas.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Xian C., Zhao J.M., Su W., Lao S., Yang X., Hua Q.K. Ilizarov bone transport for repair of diabetic foot: a functional and imaging evaluation. Chinese J Tissue Eng Res. 2015;46:7539–7544. [In Chinese, English abstract] [Google Scholar]
- 9.Birch J.G., Osteosynthesis Transosseous. Theoretical and clinical aspects of the regeneration and growth of tissue. Ann R Coll Surg Engl. 1992;75(5):383. [Google Scholar]
- 10.Prezzi D., Khan A., Goh V. Perfusion CT imaging of treatment response in oncology. Eur J Radiol. 2015;84(12) doi: 10.1016/j.ejrad.2015.03.022. S0720048X15001448. [DOI] [PubMed] [Google Scholar]
- 11.Hua Q.K., Qin S.H., Zhao L.J., Zhou J., Kuang X.C., Zhao J.M. Transverse tibial bone transport by Ilizarov technique for treatment of diabetic foot. Orthop J China. 2017;25(4):303–307. [In Chinese, English abstract] [Google Scholar]
- 12.Wintermark M., Maeder P., Verdun F.R., Thiran J.P., Valley J.F., Schnyder P. Using 80 kVp versus 120 kVp in perfusion CT measurement of regional cerebral blood flow. Am J Neuroradiol. 2000;21(10):1881–1884. [PMC free article] [PubMed] [Google Scholar]
- 13.Smith A.B., Dillon W.P., Gould R., Wintermark M. Radiation dose-reduction strategies for neuroradiology CT protocols. Am J Neuroradiol. 2007;28(9):1628–1632. doi: 10.3174/ajnr.A0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park M.S.1, Klotz E., Kim M.J., Song S.Y., Park S.W., Cha S.W. Perfusion CT: noninvasive surrogate marker for stratification of pancreatic cancer response to concurrent chemo- and radiation therapy. Radiology. 2009;250:110–117. doi: 10.1148/radiol.2493080226. [DOI] [PubMed] [Google Scholar]
- 15.Tsuji Y., Hamaguchi K., Watanabe Y., Okumura A., Isoda H., Yamamoto N. Perfusion CT is superior to angiography in predicting pancreatic necrosis in patients with severe acute pancreatitis. J Gastroenterol. 2010;45(11):1155–1162. doi: 10.1007/s00535-010-0267-8. [DOI] [PubMed] [Google Scholar]
- 16.Grözinger G., Grözinger A., Horger M. The role of volume perfusion CT in the diagnosis of pathologies of the pancreas. RöFo - Fortschritte auf dem Gebiet der Röntgenstrahlen und der bildgebenden Verfahren. 2014;186(12):1082–1093. doi: 10.1055/s-0034-1384876. [DOI] [PubMed] [Google Scholar]
- 17.Delrue L., Blanckaert P., Mertens D., Meerbeeck S., Ceelen W., Duyck P. Tissue perfusion in pathologies of the pancreas: assessment using 128-slice computed tomography. Abdom Imag. 2012;37(4):595–601. doi: 10.1007/s00261-011-9783-0. [DOI] [PubMed] [Google Scholar]
- 18.Roback K. An overview of temperature monitoring devices for early detection of diabetic foot disorders. Expert Rev Med Devices. 2010;7(5):711–718. doi: 10.1586/erd.10.35. [DOI] [PubMed] [Google Scholar]
- 19.Minson C.T. Thermal provocation to evaluate microvascular reactivity in human skin. J Appl Physiol. 2010;109(4):1239–1246. doi: 10.1152/japplphysiol.00414.2010. PMID:20507974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miles K.A. Tumour angiogenesis and its relation to contrast enhancement on computed tomography: a review. Eur J Radiol. 1999;30(3):198–205. doi: 10.1016/s0720-048x(99)00012-1. PMID:10452718. [DOI] [PubMed] [Google Scholar]
- 21.Birch J.G., Osteosynthesis Transosseous. Theoretical and clinical aspects of the regeneration and growth of tissue. Ann R Coll Surg Engl. 1992;75(5):383. [Google Scholar]
- 22.Ilizarov G.A. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;238(239):263–285. [PubMed] [Google Scholar]
- 23.Ilizarov G.A. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238(238):249–281. [PubMed] [Google Scholar]
- 24.Zuo Q., Gao F., Song H., Zhou J. Application of Ilizarov transverse tibial bone transport and microcirculation reconstruction in the treatment of chronic ischemic diseases in lower limbs. Exp Ther Med. 2018;16(2):1355–1359. doi: 10.3892/etm.2018.6321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pacicca D.M., Patel N., Lee C., Salisbury K., Lehmann W., Carvalho R. Expression of angiogenic factors during distraction osteogenesis. Bone (N Y) 2003;33(6):0–898. doi: 10.1016/j.bone.2003.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.