Abstract
Firefighters perform physically intensive jobs in suboptimal environments, making it even more important for them to maintain good functional postural balance or stability. As part of their training, firefighters are required to perform physically demanding tasks under high stress and high heat environments. These demanding tasks lead to increased physical fatigue which can then result in poor performance and/or postural instability. The objectives of this study were to 1) investigate the effect of live-firefighting training-induced heat stress on static postural balance, and 2) investigate the association between commonly monitored physiological responses (core body temperature, heart rate, oxygen saturation and blood pressure) and measures of static postural balance. Twenty-six firefighters (mean ± SD: age 36.0 years ±5.2, weight 216 lbs. ± 34, BMI 29.7 ± 4.2) participated in live firefighting training while performing following tasks: search and rescue, hose advancement, and backup. Prior to heat exposure (PRE) and following each scenario (POST1, POST2, POST3), firefighters’ postural balance was assessed with a wearable 3-D inertial sensor system quantifying time dependent changes in linear acceleration (LIN ACC) and angular velocity (AV) about three orthogonal axes [Anterior-Posterior (AP), Medial-Lateral (ML), and vertical (V)] during one foot balance tests for 30 seconds under eyes open and eyes closed conditions. The outcome variables from 3-D wearable sensors were used to create 3-D Phase-Plane based postural stability metrics. Physiological measurement of core body temperature (CBT) (measured with a radio pill) as well as perception of heat increased significantly during the live fire-training exercise. In addition, firefighters also perceived an increase in physical fatigue and respiratory distress. Angular combined stability parameters (ACSP), RMS angular velocity around ML axis were significantly correlated with CBT. In the multivariate analysis adjusted for the scenarios, height and weight of the firefighters, these measures of static postural balance were significantly associated with CBT. As per the model results, static postural balance, as indicated by ACSP, worsened with an increase in CBT. Future studies should place sensors at body extremities along with close to center of mass to capture the kinematic movements more comprehensively influencing postural balance.
Keywords: Postural Balance, Phase Plane Analysis, Live Burn, Firefighters, Heat Storage, Loss of Balance
Introduction
As one of the most physically demanding and dangerous occupations within a community, firefighting has become one of the largest contributors to work related deaths and injuries among all occupations. Firefighters perform physically intensive jobs in suboptimal environments, making it even more important for them to maintain good static and functional postural balance. One of the many contributing factors that can lead to on-duty deaths amongst firefighters is the exposure to heat. There are multiple sources for heat exposure including the environment. The personal protective equipment worn by firefighters not only reduces the body’s exposure to high temperatures, but it can also retain heat, preventing the body from naturally dissipating the large amount of heat generated during physically intense tasks. As part of their training as well as in real firefighting, the firefighters are asked to perform physically demanding tasks under high stress and high heat environments. These demanding tasks lead to increased physical fatigue which can then result in poor performance or postural instability. Fatigue due to excessive physical demand or heat stress can interfere with normal functioning of the central nervous system (CNS) [1,2]. The central nervous system as well as the peripheral nervous system work together to sustain balances [1]. Multiple physiological mechanisms are associated with heat storage in brain and muscle cells triggering fatigue [3–6]. Such disruptions in the normal functioning of the CNS due to factors such as heat stress or physical fatigue can impair one’s ability to maintain proper balance. This can lead to slips/trips, falls and other types of injuries.
The ability to sustain upright balance is a complex process that requires continual input from several sensory systems [1]. Proprioception, such as touch-pressure receptors in the soles of feet, is one dimension of the peripheral nervous system that is used to maintain proper balance. The other two include visual perception through the eyes/vision system as well as fluid and sensory organs within in the vestibular system. These physiological systems via afferent pathways send information to the brain about the body’s position in space. Disruption of the input sent from these afferents to the brain can decrease a person’s ability to maintain proper balance. It has been shown that prolonged physical exertion and fatigue can suppress the nervous system’s ability to regulate upright balance through these various physiological systems [5,7]. Reduced abilities to properly balance within a harsh work environment like that experienced by firefighters can increase the chances of injuries and even death.
Multiple factors can affect a firefighter’s ability to properly maintain balance. According to Sobeih, et al. [8], decreases in postural stability can be caused by long work shifts resulting in a high prevalence of slips and falls. Kincl, et al. [9] suggest that the use of PPE while having fatigued postural muscles can lead to a decrease in postural stability among workers. Firefighters wear turnout gear as well as a self-contained breathing apparatus (SCBA) when fighting a fire. The combination of turnout gear and SCBA can create an extra 80 pounds of workload that the firefighters must account for. The use of personal protective equipment (PPE) can lead to a decrease in postural stability; hence it is important to determine the effects of the combination of PPE and heat exposure that affect a firefighter’s ability to maintain upright posture. Other environmental effects such as smoky, dark environments or slippery floors due to spills, water discharge, and oil can affect the visual and proprioceptor systems used to maintain balance. They can also act as deterrents, forcing firefighters to work harder to maintain balance leading to more physical exertion and higher rates of fatigue.
It is important to understand and be aware of a person’s postural balance because postural balance can be an indicator for decreased nervous system function and increased fatigue. Relationships between heat stress, physical fatigue, perceptions of physical exertion, and postural balance may be used to determine the likelihood of a firefighter falling resulting in an injury or worse.
The objectives of this study were to 1) investigate the effect of live-fire training induced heat stress on static postural balance of firefighters, and 2) investigate the association between commonly monitored physiological responses (core body temperature, heart rate, and blood pressure) and measures of static postural balance. The balance was quantified by collecting kinematics of the center of mass (at the navel area) and calculating established metrics for energy content in time-series data (2nd statistical moment) and stability parameters [10].
Methods
Participants
Twenty-six firefighters (25 males, 1 female, age range 24–43 years) recruited from two separate fire stations volunteered to participate in this study. Twenty-five of them were experienced full-time firefighters, and one participant was a part-time firefighter who worked at a designated fire station one to two shifts per week. All participants were screened and medically cleared by each fire station’s designated occupational medical officer. Every participant gave informed consent according to the study protocol approved through the University of Cincinnati’s Institutional Review Board.
Procedures
Live fire trainings were performed in order to expose firefighters to heat. A “burn house” was used to contain a fire composed of combustible materials in order to produce heat. The fire was set in a controlled burn room where temperature reached as much as 483°C. Three scenarios (or evolutions) were developed for each team of firefighters. The firefighters were required to enter the building, perform all necessary steps to complete the assigned tasks, then enter the burn room for about 30 seconds, and then exit the building. Each firefighter was required to wear firefighting suit with PPE including SCBA. At the start of their shift, about six hours before the start of live-burn training, firefighters ingested an FDA-approved CorTemp® radio pill (HQ Inc., Palmetto, FL) in order to track their core body temperature. The pill wirelessly transmits core body temperature as it travels through the digestive tract. Baseline measurements of heart rate, perceived exertion, and blood pressure were also taken according to methods described in a previous study [11].
Live-Fire Training Exercise
The live fire training exercise was divided into three scenarios (referred to as Sc1, Sc2 and Sc3). The scenarios represented real life firefighting activities, (e.g., fighting first and second floor fires). Each scenario was divided into three specific tasks (or evolutions). The evolutions were hose advancement, search and rescue, and backup. The firefighters had rest periods between consecutive scenarios. Following each scenario, firefighters took their gear off and drank cold fluids. Postural balance tests were performed prior to heat exposure and at the end of each scenario (Baseline, Post1, Post2, Post3, Post 4). Perceived ratings of physical exertion (BORG), thermal stress, and respiratory distress as well as heart rate and blood pressure metrics were collected between each scenario [11].
Instrument and Equipment
Balance measurements were recorded using wearable 6 channel sensors with triaxial accelerometer and triaxial gyroscope. Either one of two such sensors were used depending upon their availability: a) 3-Space Data Logging Sensor (YEI Technologies, Portsmouth, OH) or b) a wireless Inertia-Link sensor (Lord Micro-Strain, Williston, VT). The sensor was placed over the navel of each participant. Before placing the sensor, each participant removed the helmet, SCBA, and the over coat so that only a T-shirt, turnout pants, and boots were worn [12].
Balance Test Procedure
For the one-leg balance tests, each participant was asked to stand with any one foot off the ground for the duration of the test. The test was performed on a flat concrete surface about 15 meters from the bare wall of a building about 100 meters away from the burn building. The objective of the test was to maintain proper balance for 30 seconds while staring straight ahead at the bare wall. It was noted if a participant needed to place the raised foot back on the ground in order to regain balance during the test. After a few moments to recover, participants were then asked to look at the wall in order to get their bearings, close their eyes lift the same leg and maintain upright proper balance for 30 seconds. Again, it was noted if a participant placed the raised foot on the ground to regain balance during the test (considered a FALL) or if the participant opened their eyes to adjust or regain balance (considered a FALL) [12].
Data Collection
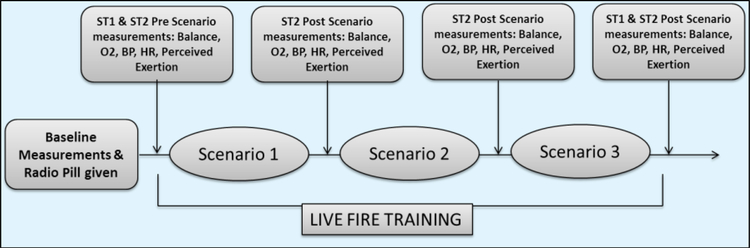
Baseline balance measurements were taken immediately upon the participants’ donning of turnout pants and boots. Participants then proceeded through the first scenario of live burn training. Upon completion, post scenario 1 balance tests were performed. This was repeated for post scenario 2 and post scenario 3 measurements (Figure 1) [11,13].
Figure 1:
Study Design: Schematic showing progression of live-fire training and data collection procedure (Adapted from Reference 11, 13).
Outcome Variables
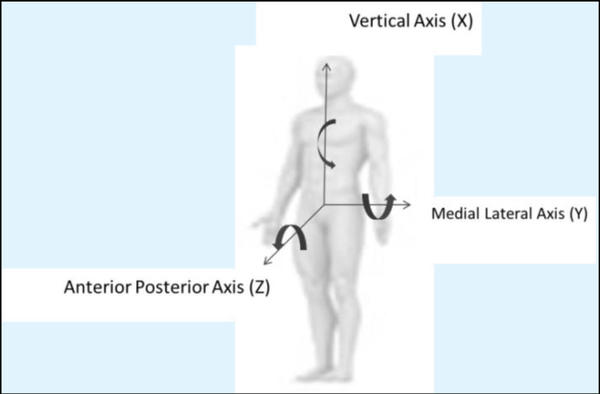
Physiological responses measured to quantify the effects of heat stress in this study were heart rate (HR), core body temperature (CBT), blood pressure and oxygen saturation (SaO2). Psychophysical responses included perceptions of physical exertion (PE), thermal stress (TS), and respiratory distress (RD). Time dependent changes in acceleration and angular velocity (AV) about three orthogonal axes [Anterior-Posterior (AP), Medial-Lateral (ML), and vertical (V)] were collected using the wearable sensors, as shown in Figure 2. Reaction times at baseline and after each scenario were also measured.
Figure 2:
Schematic showing sensor placement and reference frame for data collection.
Data Analysis
Descriptive Analyses and Transformation of Data
Mean (standard error), maximum and minimum values of the untransformed outcome variables were calculated. Untransformed variables were checked for normality of distribution. To meet the assumptions of normality during linear regression analyses, the variables that were not normally distributed were log-transformed. In addition, BMI was calculated from the height and weight of the participants and heat storage (discussed in the next section) was calculated from the weight and change in core body temperature.
Calculation of Heat Storage between Baseline and Scenarios
After completion of the baseline data collection, the balance data collected during rest periods at the end of scenarios 1–3 were used to investigate the buildup of heat or heat storage. Heat storage (HS) is calculated using the following equation [14]:
where, HS = Heat Storage (watts per hour)
BW = Body Weight (kg)
ΔCBT = Change in Core Body Temperature (°C)
ρ = specific heat capacity of body tissue (0.97 watts per hour/kg °C)
Effect of heat storage as a fixed effect on the postural balance measures, psychological and physiological responses were determined using a repeated measure mixed model linear regression analysis (SAS®, Cary, NC) adjusted for the height of the firefighters and using the scenarios as a random effect.
Balance Data Analysis
The data obtained from the sensors were processed by creating phase plane plots between AV and angular displacement (AD) about three axes as well as ACC and linear velocity (VEL) plots. Within the body based local coordinate system, human body segment with respect to its adjacent segment move in the angular mode around the referenced joint. Therefore, such segmental angular motions are instrumental in contributing toward the positional changes in whole body center of mass and potentially impacting subjects’ balance characteristics during the postural balance test. In addition, such phase plane analysis approach provides information about neuromuscular control of two adjacent body segments influencing the whole-body postural balance [15]. In addition, such an approach of analysis may provide further insights into the status of coordinated movement between body segments [10,15]. AD and VEL values were calculated using the integration of the AV and ACC values over time of the test. This was performed using MATLAB software version R2012a. Using 2nd statistical moment of data [root mean square (RMS)] as well as an adapted direct stability parameter and combined stability from Riley (1995) [10] each test was analyzed for the energy content in signal and stability and variance in postural sway.
Root Mean Square Linear Acceleration Component
| (1) |
| (2) |
Phase plane plots were initially developed, comparing angular velocity data to angular displacement data. In order to determine the angular position of the subject within each axis, the angular velocity was integrated through a MATLAB program among each individual axis. Taking the time derivation of angular velocity in each axis against the time derivative of angular displacement (position) in each axis, a phase plane plot was created. This was also carried out for linear acceleration. Using MATLAB integration versus time of tests within each axis, linear velocity was determined. Phase plane plots were created to show the variance of each parameter as compared to one another versus time. Using these phase plane plots, a set of parameters were created that relate one balance test to another through root mean square variance of angular position and velocity as well as linear velocity and acceleration. These parameters are called stability values. Stability values can represent the difference in stability between two tests. Calculations for stability parameters used following equations.
Directional Stability Parameters
| (3) |
| (4) |
Combined Stability Parameter
| (5) |
| (6) |
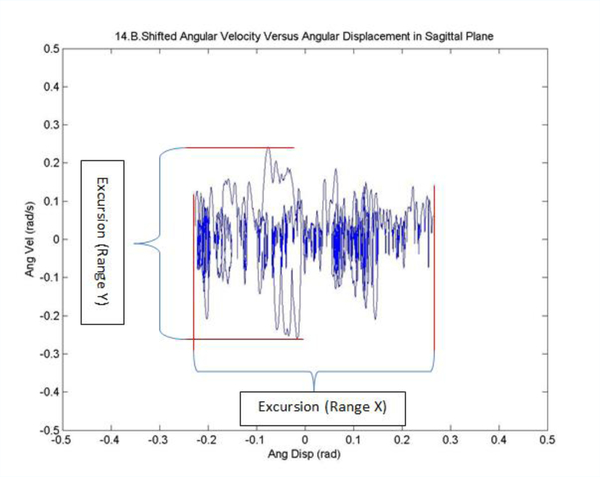
Excursion (Range)
Excursion or range of a set of values is the difference between the greatest value and the least value for each parameter listed above. The postural balance characteristics were also quantified by the size (max excursions about three axes) of the phase plane plots, as seen in the Figure 3.
Figure 3:
Sample phase plane plot for angular velocity.
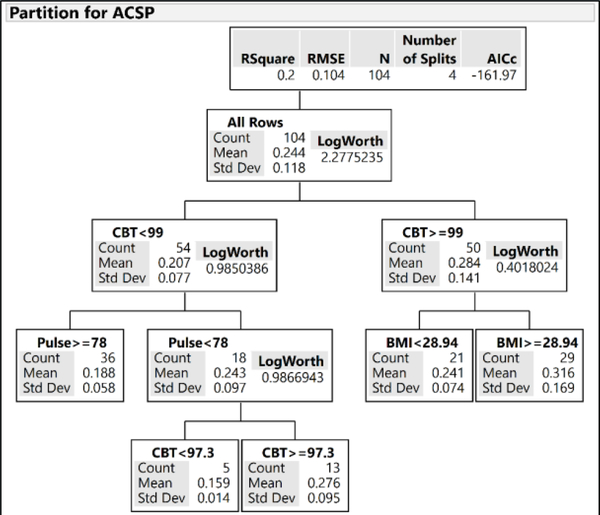
Recursive Partitioning Analysis of Angular Combined Stability Parameter
Using recursive partitioning analysis (RPA), a method for creating regression tree according to most significant determinants at each step of the decision node, the physiological parameters such as CBT, pulse rate, and BMI, were used to analyze their effect on and predict the angular CSP. With this method a decision tree was created by recursively partitioning data according to a relationship between the predictors and response values. The best response is predicted using the partition algorithm that selects optimum splits from several possible splits. A tree of decision rules is formed through recursive partitioning or splitting of the data until the desired fit is achieved [16].
Results
Descriptive Analyses of Postural Balance Measures, Psychological and Physiological Responses
Descriptive analyses of the postural balance measures, psychological and physiological responses in this study are shown in Table 1. Heat storage, indicative of heat stress due to heat stored within the body between two time-points in the study, increased progressively between baseline vs. Sc1, and Sc1 vs. Sc2; but decreased between Sc2 and Sc3. These differences in the heat storage between the time-points were statistically significant (p<0.0001). In addition, the differences in most of the psychological and physiological responses from baseline were statistically significant.
Table 1:
Summary of the Physiological and Stability Parameters among Firefighters at Baseline and Post-Training Scenarios.
| Outcomes [Mean (SE), Max, Min] | Baseline | Post-Scenario 1 | Post-Scenario 2 | Post-Scenario 3 | P-value |
|---|---|---|---|---|---|
| Heat Storage | Reference | 194.4 (25.5) | 211.3 (33.9) | 148.2 (32.3) | <0.0001 |
| Postural Balance Measures | |||||
| Angular Combined Stability Parameter | 0.23 (0.02), 0.42, 0.14 | 0.24 (0.02), 0.40, 0.10 | 0.30 (0.02), 0.50, 0.14 | 0.25 (0.03), 1.0, 0.13 | 0.18 |
| Linear Combined Stability Parameter | 8.60 (0.30), 9.90, 3.50 | 9.10 (0.10), 10.60, 8.30 | 8.90 (0.20), 9.60, 5.60 | 8.70 (0.3), 10.3, 2.40 | 0.23 |
| RMS Angular Velocity X-axis | 0.09 (0.01), 0.28, 0.02 | 0.07 (0.01), 0.17, 0.02 | 0.08 (0.01), 0.30, 0.02 | 0.10 (0.03), 0.63, 0.02 | 0.38 |
| RMS Angular Velocity Y-axis | 0.06 (0.01), 0.17, 0.02 | 0.06 (0.01), 0.15, 0.02 | 0.06 (0.01), 0.14, 0.03 | 0.07 (0.01), 0.30, 0.03 | 0.3 |
| RMS Angular Velocity Z-axis | 0.04 (0.01), 0.14, 0.01 | 0.03 (0.003), 0.07, 0.01 | 0.04 (0.01), 0.18, 0.01 | 0.05 (0.01), 0.30, 0.01 | 0.04 |
| Excur_AngPos X-axis | 0.40 (0.05), 0.90, 0.10 | 0.40 (0.004), 0.9, 0.14 | 0.46 (0.06), 1.17, 0.13 | 0.45 (0.13), 3.21, 0.09 | 0.05 |
| Excur_AngPos Y-axis | 0.53 (0.03), 0.90, 0.25 | 0.59 (0.04), 0.94, 0.33 | 0.64 (0.05), 1.20, 0.25 | 0.56 (0.04), 1.0, 0.20 | 0.53 |
| Excur_AngPos Z-axis | 0.27 (0.03), 0.56, 0.12 | 0.29 (0.03), 0.54, 0.14 | 0.32 (0.03), 0.61, 0.13 | 0.31 (0.04), 0.97, 0.11 | 0.36 |
| Psychological (Perception) Responses | |||||
| BORG | 6.50 (0.20), 9.00, 6.00 | 12.40 (0.40), 17.00, 8.00 | 13.2 (0.4), 17.50, 8.00 | 13.30 (0.60), 18.00, 8.00 | <0.0001 |
| RESP | 1.20 (0.10), 3.00, 1.00 | 2.60 (0.20), 5.00, 1.00 | 3.10 (0.10), 5.00, 2.00 | 3.00 (0.20), 6.00, 1.00 | <0.0001 |
| THERM | 3.70 (0.10), 4.50, 2.00 | 5.40 (0.20), 7.50, 4.00 | 5.60 (0.10), 7.00, 5.00 | 5.80 (0.20), 8.00, 4.70 | |
| Physiological Responses | |||||
| Core Body Temperature | 97.70 (0.10), 98.60, 96.00 | 99.30 (0.19), 101.0, 97.3 | 99.7 (0.2), 103.0, 98.0 | 99.2 (0.2), 101.1, 97.5 | <0.0001 |
| Systolic BP | 125.6 (2.4), 158.0, 107.0 | 139.0 (3.3), 187.0, 111.0 | 134.3 (2.9), 161.0, 102.0 | 137.5 (3.6), 176.0, 108.0 | 0.001 |
| Diastolic BP | 78.1 (1.9), 105.0, 58.0 | 83.0 (2.2), 113.0, 65.0 | 80.2 (1.7), 102.0, 60.0 | 82.0 (2.2), 108.0, 55.0 | 0.03 |
| Pulse | 75.7 (3.1), 113.0, 51.0 | 114.8 (3.7), 156.0, 85.0 | 124.6 (4.5), 160.0, 65.0 | 122.4 (3.6), 153.0, 70.0 | <0.0001 |
| Oxygen Saturation (SaO2) | 97.5 (0.2), 99.00, 95.00 | 96.7 (0.20), 99.00, 95.00 | 96.8 (0.2), 99.0, 95.0 | 96.7 (0.2), 99.0, 94.0 | 0.03 |
| Maximum Reaction Time | 0.45 (0.03) | 0.39 (0.02) | 0.39 (0.02) | 0.40 (0.02) | 0.006 |
| Mean Reaction Time | 0.33 (0.01) | 0.31 (0.01) | 0.30 (0.01) | 0.31 (0.01) | 0.001 |
| Minimum Reaction Time | 0.28 (0.01) | 0.26 (0.01) | 0.26 (0.01) | 0.28 (0.02) | 0.007 |
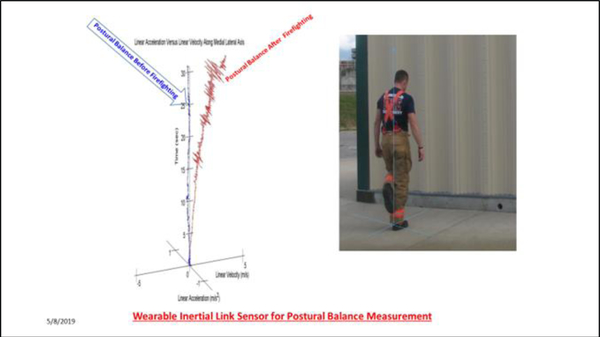
Figure 4 shows an example of a 3D phase plane plot of a Baseline and Post Scenario 3 one-foot balance test for a single firefighter. This figure represents the change in postural balance before and after heat exposure (associated with firefighting) with changes in linear velocity and linear acceleration with respect to time. Since the sensor was placed over the navel area, the graph represents the aggregate contributions of torso/head/arm motion deviations influencing postural balance after three scenarios of firefighting compared to the baseline.
Figure 4:
3D phase plane plot of a Baseline and Post Scenario 3 one-foot balance test for a single firefighter.
Correlation between Angular Combined Stability Parameter and Core Body Temperature or Oxygen Saturation
Among the stability parameters, angular CSP was correlated positively with CBT (r= 0.299, p-value= 0.002), negatively with SaO2 (r= −0.286, p-value=0.003) and with maximum reaction time (r=−0.22, p=0.046). Moreover, CBT was negatively correlated with SaO2 (r= −0.249, p-value= 0.01). Linear CSP was negatively correlated with body weight (r=−0.29, p=0.005) and with minimum reaction time (r=−0.24, p=0.03).
Multivariate Linear Regression Analyses
Effect of Heat Storage on Postural Balance Measures
Table 2 describes the effect of heat stress induced by live fire training on the postural balance measures. Neither the linear CSP nor the angular CSP was associated with heat storage during the training.
Table 2:
Effect of Heat Stress, Measured by Heat Storage, on the Static Postural Balance of Firefighters During Live Fire Training.
| Postural Stability Parameters | Estimate | SE | P-value |
|---|---|---|---|
| Log(Angular Combined Stability Parameter) | −0.0002 | 0.0001 | 0.07 |
| Log(Linear Combined Stability Parameter) | −0.00005 | 0.00004 | 0.2 |
| Log(RMS_AngVelX) | −0.0005 | 0.0003 | 0.1 |
| Log(RMS_AngVelY) | −0.0003 | 0.0002 | 0.1 |
| Log(RMS_AngVelZ) | −0.0005 | 0.0002 | 0.01 |
| Log(Excur_AngPosX) | −0.0001 | 0.0003 | 0.78 |
| Log(Excur_AngPosY) | −0.00003 | 0.0002 | 0.81 |
| Log(Excur_AngPosZ) | −0.0002 | 0.0001 | 0.12 |
Effect of Heat Storage on Physiological and Psychological Responses
Among the physiological and psychological responses measured in this study, all these responses except for systolic blood pressure and pulse rate were significantly associated with heat storage (Table 3). Among these measures, the rating on perceived or symptomatic breathlessness (RESP) was most significantly associated with heat storage (estimate=0.0013, p<0.0001); perceived exertion (BORG) was also significantly associated but to a lesser extent than breathlessness. Increase in heat storage was also associated significantly with an increase in diastolic blood pressure (p= 0.004) and with a decrease in oxygen saturation (p=0.05).
Table 3:
Effect of Heat Stress, Measured by Heat Storage, on the Physiological and Psychological Responses of Firefighters during Live Fire Training.
| Parameters | Estimate | SE | P-value |
|---|---|---|---|
| SBP | 0.002 | 0.007 | 0.83 |
| DBP | 0.011 | 0.004 | 0.004 |
| Pulse | 0.011 | 0.007 | 0.11 |
| SaO2 | −0.0012 | 0.0006 | 0.05 |
| Log(BORG Scale) | 0.0001 | 0.00006 | 0.1 |
| THERM Scale | 0.0009 | 0.0004 | 0.02 |
| RESP Scale | 0.0013 | 0.0003 | < 0.0001 |
Effect of Core Body Temperature on Postural Balance Measures
Table 4 describes the associations between core body temperatures with the postural balance measures. Increase in core body temperature significantly increased the angular CSP (estimate = 0.07, p=0.006), and RMS angular velocity on ML-axis (estimate=0.1, p=0.005).
Table 4:
Associations between Core Body Temperature during Live Fire Training and Postural Balance Measures Adjusted for Height and Weight of Firefighters.
| Postural Stability Parameters | Estimate | SE | P-value |
|---|---|---|---|
| log(Angular Combined Stability Parameter) | 0.026 | 0.01 | 0.02 |
| Log(Linear Combined Stability Parameter) | −0.002 | 0.01 | 0.76 |
| Log(RMS_AngVelX) | 0.08 | 0.05 | 0.13 |
| Log(RMS_AngVelY) | 0.08 | 0.03 | 0.01 |
| Log(RMS_AngVelZ) | 0.006 | 0.05 | 0.89 |
Recursive Partitioning Analysis Results
As shown in Figure 5, according to the RPA tree the best angular CSP (mean: 0.16) was observed in firefighters with CBT<97.3°F and pulse rate <78/minute. The worst angular CSP (mean: 0.316) was measured in firefighters with CBT≥99°F and BMI ≥28.9. These variables (i.e., CBT, pulse rate, and BMI) explain ~20% of the variances in the angular CSP.
Figure 5:
Regression Tree for Angular Combined Stability Parameter.
Discussion
Effects of Heat Stress on Physiological Response and Perceived Measures of Stress
Physiological measurement of CBT as well as perception of heat increased significantly during the live fire-training exercise. In addition, firefighters also perceived an increase in physical fatigue and respiratory distress (Table 3). These findings are consistent with those reported in literature [13,17]. This is important to consider given that the training exercises are in controlled environments with short rest periods built into the training exercise. Other fire stations might conduct live fire-training exercises that are longer with less opportunities to hydrate and recuperate. Real life scenarios of firefighting may not allow for intermediate rests either. Hence the increase in the reported physiological and perceived indicators of stress should be considered lower bounds on the actual increase one might see in real-life firefighting.
Association between Physiological Responses and Measures of Static Postural Balance
Angular CSP, RMS angular velocity on ML-axis were significantly correlated with core body temperature in the correlational analysis (Supplementary Table 1). In the multivariate analysis adjusted for the scenarios, height and weight of the firefighters, these measures of static postural balance were significantly associated with CBT. As per the model results, static postural balance, as indicated by ACSP, can worsen with an increase in CBT. The model included only the height, weight and CBT as explanatory variables. These variables could explain only about 10% and 8% of the variance in the angular CSP and RMS angular velocity on ML-axis respectively. Certain other variables, not measured in this study, could account for the development of a better model. No significant association was determined in the multivariate analysis with Linear CSP as the dependent variable. This is not surprising as previous authors have also shown that physiological parameters typically do not provide a clearer explanation for the state of postural balance [1].
However, it should be noted that the lack of associations found through univariate analysis here and in previous studies may be, partially, due to averaging of data across different study participants. Such averaging would not account for varying levels of physical fitness the firefighters might have. While BMI is not an accurate measurement of physical fitness, the variation in BMI was quite large (mean 30, min 22.8, maximum 37.2). To comprehensively account for different levels of physical fitness in firefighters, one would also need access to performance numbers from recently performed fitness tests. This data was not available to the authors.
Since variations between different firefighters, from a fitness perspective, could not be accounted for statistically, a non-parametric approach was chosen to look for sub-groups of firefighters that showed worse static postural balance as compared to others. This analysis was done by a recursive binary partitioning method called regression trees. The regression tree analysis demonstrated that the firefighters with CBT > 99°F and BMI >= 28.94 had the highest value of ACSP (mean = 0.316; std dev = 0.169) indicating that they had the highest deterioration in postural balance as a result of the live-fire training. This result points to the finding that firefighters with higher BMI may be more susceptible to decrease in postural balance. Other studies have found fat content and BMI to be significantly associated with poorer balance in a different population [18,19]. Another sub-group of interest identified was firefighters with pulse < 78 beats/min, and CBT between 97.3°F and 99°F. This sub-group had lower values of ACSP (mean = 0.159; std dev = 0.014) indicating comparatively smaller decline in postural balance as a result of the live-fire training.
Effects of Heat Stress on Static Postural Balance
When averaged across all study participants, there was no significant change in the overall energy content for kinematics measurements along the individual directions: vertical, medio-lateral and anterior-posterior. The resultant (combined) measure of stability ACSP was found to increase significantly with rise in CBT. Given that the IMU sensor was placed close to center of mass, angular measures might be more sensitive than translation. Future studies should place sensors at body extremities along with close to center of mass to capture the kinematic movements more comprehensively. The linear combined measure, LCSP, did not change significantly with rise in CBT. Enough data was not present to divide the study participants in sub-groups and repeat the analysis.
Conclusion
Core body temperatures were significantly elevated as compared to the baseline measurements after each training scenarios (p < 0.001) (Table 1).
Core body temperature was found to be significant in explaining a portion of variation in the angular combined stability parameter (p = 0.035) (Table 4). This regression results show that static postural balance, as indicated by ACSP, can worsen with rising CBT.
Pulse, BMI and blood pressure were not found to be significantly associated with ACSP in a regression model.
Recursive binary partitioning done using a regression tree demonstrated that the firefighters with CBT > 99°F and BMI >= 28.94 had the highest value of ACSP (mean = 0.316; std dev = 0.169) indicating that they had the highest deterioration in postural balance as a result of the live-fire training (Figure 5).
The firefighters with pulse < 78/min, and CBT < 97.3°F recorded lower values of ACSP (mean = 0.159; std dev = 0.014) indicating comparatively smaller decline in postural balance as a result of the live-fire training.
Only 20% of the variance in ACSP was explained by the regression tree model, which shows that merely monitoring the physiological responses of the firefighters may not be enough to accurately gauge their postural balance in physically demanding situations. We need to leverage sensors to monitor the kinematics of center of body motion to quantify changes in balance and stability.
Future work should explore the question if implementing a consistent scheme for micro-breaks would break the trend of declining static postural balance as a result of the live-fire training.
Supplementary Material
Acknowledgements
We thank Fire Chief, Donald G. Bennett, Chief BJ Jetter, Captain Russell L. Kammer and all participating firefighters from the two fire stations for their participation and co-operation in this research study. We also thank Diane Busch James, RN, MSN, JD, COHN-S, Chris Scott Sparks, MS, Peter Sandwell, MS, Kent Bennett, DO, and Kevin He, PhD for their help with the study.
Funding
This research was partially funded by the NIOSH ERC grant #T42OH008432 (2014).
Footnotes
Conflicts of Interest
All authors declare no conflict of interest.
References
- 1.Seliga R, Bhattacharya A, Succop P, Wickstrom R, Smith D, et al. (1991) Effect of workload and respirator wear on postural stability. American Industrial Hygiene Association Journal 52(10): 417–422. [DOI] [PubMed] [Google Scholar]
- 2.Nybo L (2008) Hyperthermia and fatigue. J Appl Physiol 104(3): 871–878. [DOI] [PubMed] [Google Scholar]
- 3.Ross JA, Shipp EM, Trueblood AB, Bhattacharya A (2016) Ergonomics and Beyond: Understanding How Chemical and Heat Exposures and Physical Exertions at Work Affect Functional Ability, Injury and Long-Term Health. Human Factors & Ergonomics 58(5): 777–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nybo L (2010) CNS fatigue provoked by prolonged exercise in the heat. Front Biosci 2: 779–792. [DOI] [PubMed] [Google Scholar]
- 5.Nybo L (2012) Brain temperature and exercise performance. Exp Physiol 97(3): 333–339. [DOI] [PubMed] [Google Scholar]
- 6.Nybo L, Jensen T, Nielsen B, Gonzalez-Alonso J (2001) Effects of marked hyperthermia with and without dehydration on VO(2) kinetics during intense exercise. J Appl Physiol (1985) 90(3): 1057–1064. [DOI] [PubMed] [Google Scholar]
- 7.Nybo L, Nielsen B, Blomstrand E, Moller K, Secher N (2003) Neurohumoral responses during prolonged exercise in humans. J Appl Physiol (1985) 95(3): 1125–1131. [DOI] [PubMed] [Google Scholar]
- 8.Sobeih TM, Davis KG, Succop PA, Jetter WA, Bhattacharya A (2006) Postural balance changes in on-duty firefighters: effect of gear and long work shifts. J Occup Environ Med 48(1): 68–75. [DOI] [PubMed] [Google Scholar]
- 9.Kincl LD, Bhattacharya A, Clark S, Rice C, Succop PA (2002) The use of postural sway measurement as a safety monitoring technique for workers wearing personal protective equipment. Applied Industrial and Environmental Hygiene 17(4): 256–266. [DOI] [PubMed] [Google Scholar]
- 10.Riley PO, Benda BJ, Gillbody KM, Krebs DE (1995) Phase plane analysis of stability in quiet standing. Journal of Rehabilitation Research and Development 32(3): 227–235. [PubMed] [Google Scholar]
- 11.Mani A, Musolin K, James K, Kincer G, Alexander B, et al. (2013) Risk factors associated with live fire training: buildup of heat stress and fatigue, recovery and role of micro-breaks. Occupational Ergonomics 11(2,3): 109–121. [Google Scholar]
- 12.James K, Mani A, Kincer G (2013) Effects of Heat Stress on Firefighters’ Postural Balance During Live Fire Fighting. Presented at the American Industrial Hygiene Annual Conference, Montreal, Canada, pp: 18–23: [Google Scholar]
- 13.Mani A, Rao M, James K, Bhattacharya A (2015) Individualized Prediction of Heat Stress in Firefighters: A Data-driven Approach using Classification and Regression Trees. J Occup Env Hygiene 12(12): 845–854. [DOI] [PubMed] [Google Scholar]
- 14.Van Gelder CM, Pranger LA, Wiesmann WP, Stachenfeld N, Bogucki S (2008) An experimental model of heat storage in working firefighters. Prehosp Emerg Care 12(2): 225–235. [DOI] [PubMed] [Google Scholar]
- 15.Spinelli BA, Wattananon P, Silfies S, Talaty M, Ebaugh D (2016) Using Kinematics and a Dynamical Systems Approach to Enhance Understanding of Clinically Observed Aberrant Movement Patterns. Man Ther 20(1): 221–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fors MM, Viada CE, Gonzalez P (2017) Use of Recursive Partitioning Analysis in Clinical Trials and Meta-Analysis of Randomized Clinical Trials, 1990–2016. Rev Recent Clin Trials 12(1): 3–7. [DOI] [PubMed] [Google Scholar]
- 17.Smith DL, Petruzzello SJ, Chludzinski MA, Reed JJ, Woods JA (2005) Selected hormonal and immunological responses to strenuous live-fire firefighting drills. Ergonomics 48(1): 55–65. [DOI] [PubMed] [Google Scholar]
- 18.Delfa-de-la-Morena JM, Rojo Tirado MA, Aparecida-de-Castro E, Gil Arias A, Miangolarra-Page JC, et al. (2018) Relationship of physical activity level and body composition on postural control in male adults. Nutr Hosp 35(6): 1416–1423. [DOI] [PubMed] [Google Scholar]
- 19.do Nascimento JA, Silva CC, Dos Santos HH, de Almeida Ferreira JJ, de Andrade PR (2017) A preliminary study of static and dynamic balance in sedentary obese young adults: the relationship between BMI, posture and postural balance. Clin Obes 7(6): 377–383. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.