Abstract
Objectives:
The Critical Care Choosing Wisely Task Force recommends that intensivists offer patients at high risk for death or severe functional impairment the option of pursuing care focused on comfort. We tested the a priori hypothesis that intensivists who are prompted to document patient prognosis are more likely to disclose prognosis and offer comfort-focused care.
Design:
Randomized controlled trial (clinicaltrials.gov:).
Setting:
High-fidelity Simulation Center in Baltimore, MD.
Participants:
One hundred sixteen intensivists from 17 states.
Intervention:
All intensivists reviewed a paper-based medical record for a hypothetical patient on ICU day 3 and answered four survey questions about the patient’s medical management. Intensivists randomized to the intervention group answered three additional questions about patient prognosis. Thereafter, each intensivist participated in a standardized, video-recorded, simulated family meeting with an actor performing a standardized portrayal of the patient’s daughter.
Measurements and Main Results:
Two blinded intensivists reviewed deidentified written transcripts of all simulated family meetings. The primary outcome was the blinded reviewers’ assessment that the intensivist had presented the option of care focused entirely on comfort. Secondary outcomes included disclosing risk of death. All outcomes were planned prior to data collection. Among the 63 intensivists randomized to the intervention, 50 (79%) expected the patient to die during the hospitalization and 58 (92%) expected the patient to have new functional impairments preventing independent living. Intensivists in the intervention versus control group were no more likely to offer the option of care focused on comfort (13% vs 13%; 95% CI, −13% to 12%; p = 1.0) but were more likely to inform the daughter that her father was sick enough to die (68% vs 43%; 95% CI, 5–44%; p = 0.01).
Conclusions:
Documenting prognosis may help intensivists disclose prognosis to ICU proxies, but in isolation, it is unlikely to change the treatment options offered during initial family meetings.
Keywords: communication, critical care, family, intensive care, prognosis, randomized trial
Americans are increasingly admitted to an ICU during their last month of life (1, 2). However, care in an ICU often does not align with patients’ preferences or help achieve patients’ valued goals (3–5). Protecting patients from unwanted treatment in an ICU can be challenging. In nationally representative studies, patients who participated in advance care planning were no less likely to be admitted to an ICU during their last month of life (6), and patients with advance directives limiting treatment were no less likely to receive life support during their last 6 months of life (7). Patients treated in hospitals with palliative care programs, the prevalence of which have grown dramatically in the last 2 decades (8), also do not have shorter ICU stays and receive mechanical ventilation, dialysis, and gastrostomy tubes at similar rates (9). When (or if) comfort care is offered in ICUs currently depends heavily on individual physician practice patterns (10, 11).
In response to this problem, the Critical Care Choosing Wisely Task Force issued the following evidence-based recommendation in 2014: “Do not continue life support for patients at high risk for death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort” (12). This recommendation was developed by a multidisciplinary task force that conducted in-depth evidence reviews and voted on potential recommendations using a National Institute of Health Style Scale (12). How best to foster adherence to this recommendation is unclear. In a randomized trial using written patient case studies, we previously demonstrated that U.S. critical care physicians (intensivists) were 49% more likely to report an intention to tell families about the option of withdrawing life support if the intensivist was required to consider and document the patient’s 3-month functional prognosis (13). However, it is unknown if the intentions reported in this randomized trial translate into action during family meetings. To answer this question, we designed a randomized trial to test the effect of requiring intensivists to document short- and long-term functional prognosis on their communication behaviors in a family meeting conducted with an actor in a well-controlled, high-fidelity, hospital-based Simulation Center. We hypothesized that intensivists randomized to document prognosis would be more likely to disclose prognosis to the patient’s proxy and to offer the alternative of care focused on entirely comfort.
METHODS
Trial Design
The “Simulated Communication with ICU Proxies” (SCIP) study was a double-blind randomized controlled trial (RCT) comparing intensivist communication behaviors with versus without documentation of prognosis for a hypothetical patient at high risk of death or severely impaired functional recovery. The Johns Hopkins Medicine Institutional Review Board (IRB) reviewed and approved the study (IRB 00082272). The SCIP study was registered at the clinicaltrials.gov ().
Recruitment
Medical doctors were eligible to participate if they spent more than or equal to 4 weeks as an attending physician in an adult ICU during the previous 12 months, and primarily practiced in the United States. The study recruitment plan included advertisement by the American Thoracic Society’s Critical Care Assembly prior to their annual conference in Washington, DC, approximately 1 hour away. Recruitment materials directed physicians to complete a survey assessing their eligibility (supplemental digital material, Supplemental Digital Content 1, http://links.lww.com/CCM/E495). Appointments for eligible intensivists were scheduled at the Simulation Center between October 2016 and November 2017 where they provided written informed consent and received $500 in compensation.
Randomization and Blinding
To avoid biasing intensivists’ behavior and responses, the IRB approved the use of deception regarding the study design and hypothesis (14–17). Intensivists and actors were told that the objective of this study was to describe variability in how physicians treat patients.
A 1:1 randomization sequence was created by an independent study statistician using R (R Core Team, Vienna, Austria) (18). The allocation sequence was concealed using sequentially numbered opaque-sealed envelopes with aluminum foil inside the envelope according to published standards (19). Envelopes were opened by a research coordinator or the principal investigator after obtaining consent. All other study team members, including outcome assessors, were strictly blinded.
Intervention and Control
Intensivists were given as much time as needed to review the paper-based medical record of a hypothetical patient. This review occurred at a quiet desk immediately prior to start of the family meeting. Intensivists in both the intervention and control groups were asked four questions about their management plan for the hypothetical patient via a web-based survey on a study computer. Intensivists randomized to the intervention group also viewed three additional questions about the patient’s prognosis:
What do you believe is this patient’s most likely outcome 3 months from now? (free-text response)
Do you expect this patient to survive to hospital discharge? (binary choice: yes, no)
If this patient survives his current hospitalization, what do you believe is his most likely outcome 3 months from now? (response options in supplemental digital material, Supplemental Digital Content 1, http://links.lww.com/CCM/E495)
Participants were required to answer all questions before participating in a standardized, video- and audio-recorded, simulated family meeting in the Simulation Center, using specially trained and paid actors portraying the patient’s daughter.
Clinical Scenario
The hypothetical patient was an 81-year-old African American man who was admitted to the ICU and treated appropriately. By ICU day 3, he developed acute respiratory distress syndrome complicated by septic shock (supplemental digital material, Supplemental Digital Content 1, http://links.lww.com/CCM/E495). The scenario was adapted from an actual patient case. At admission, the patient’s in-hospital mortality probability, estimated using Acute Physiology and Chronic Health Evaluation III (20), was 64%, and by ICU day 3, it was 88% using the Mortality Probability Model II—72 hours (21, 22). Information on actor training, the study script (eTable 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E495), and the quality assurance process implemented to assure consistent performances is provided in the supplemental digital material (Supplemental Digital Content 1, http://links.lww.com/CCM/E495).
Data Collection
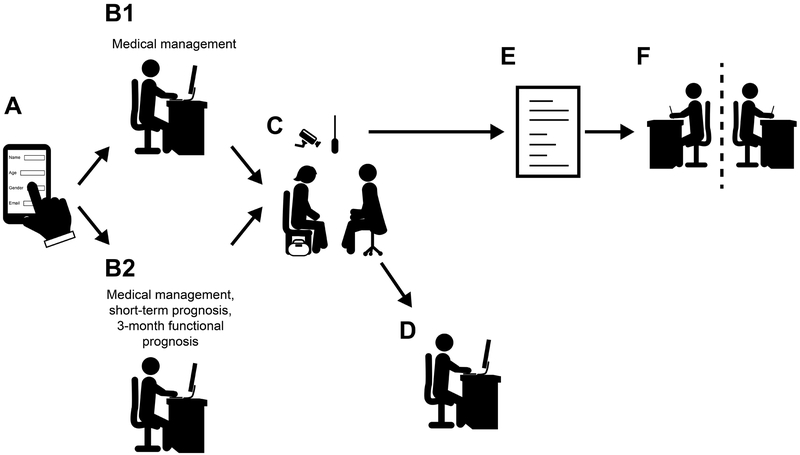
Data on intensivist demographics and professional experience were collected within the study eligibility survey (Fig. 1). At the Simulation Center, intensivists in both the intervention and control groups answered questions about how they intended to manage the hypothetical patient. Intensivists in the intervention group also answered questions about their assessment of the patient’s prognosis for survival and functional outcome. Immediately after the simulation, intensivists were asked to self-report on their communication behaviors and perceived conflict with the daughter during the simulated patient meeting. They also rated realism of the encounter using a previously validated instrument scored on a 0–10 scale, with 0 indicating “completely different” from their clinical experiences and 10 indicating “almost identical” to their clinical experiences (23). Audio recordings of all simulated meetings were transcribed and deidentified.
Figure 1.
Data collection. A, Data on intensivist characteristics were collected via an online survey. Eligible intensivists then traveled to the Simulation Center where they reviewed the medical record of the hypothetical patient and were randomized (B1) to document their medical management plan or (B2) to document their medical management plan as well as estimates of the patient’s prognosis for in-hospital survival and 3-mo functional prognosis. C, Each intensivist then participated in a standardized, video- and audio-recorded, simulated family meeting with a trained actor portraying the patient’s daughter. D, Immediately following the simulation intensivists self-reported their own communication behaviors during the simulated meeting via a computer-based survey. E, Audio recordings of the meetings were transcribed and deidentified by a medical transcriptionist. F, Two blinded reviewers (both attending intensivists) independently read the resulting transcripts and assessed whether participating intensivists disclosed prognosis and offered the option of care focused on comfort during the simulated family meeting.
Outcomes
All outcomes were determined prior to the start of data collection. The primary outcome, as assessed by two blinded reviewers (M.M.H., R.G.B.) after reading the transcript of the simulated family meeting, was the proportion of intensivists who presented the option of care focused entirely on comfort to the patient’s daughter. As in prior studies (10, 24–27), deidentified transcripts were reviewed so that reviewers would not recognize colleagues. Reviewers worked independently and resolved any discrepancies via consensus. Secondary outcomes included the proportions of intensivists who disclosed patient survival and functional prognoses in the simulation as assessed by the two blinded reviewers, and two self-reported outcomes assessed immediately after the simulation: whether they disclosed survival and functional prognoses, and whether they presented the option of care focused entirely on comfort.
Sample Size
We estimated that 116 intensivists would be required to detect an effect size of 0.49 (as demonstrated in our prior scenario-based RCT [13]), with a two-tailed α of 0.05 and power of 0.80. This estimate assumed 50% of intensivists in the control group would present the option of comfort care based on the previous trial (13).
Statistical Analysis
Our analyses were performed using an intention-to-treat approach including all randomized intensivists. Intensivist characteristics and responses to multiple-choice questions about medical management, perceived conflict, and simulation realism were reported using descriptive statistics. To assess efficacy of the intervention, we evaluated the average treatment effect, defined as the difference in the proportion of intensivists who disclosed prognosis and offered the alternative of treatment focused solely on comfort in the intervention versus control arms. This average treatment effect was estimated using the sample proportions observed in each treatment arm, and the null hypothesis of zero average treatment effect was tested using the Fisher exact test. We also report the unadjusted risk difference in the proportion of intensivists achieving secondary outcomes in the intervention versus control arms. A sensitivity analysis excluding simulations in which the actor deviated from the simulation script was also planned on an a priori basis. A two-sided p value less than 0.05 signified statistical significance. All analyses were conducted using R (version 3.3.2; R Development Core Team, Vienna, Austria).
RESULTS
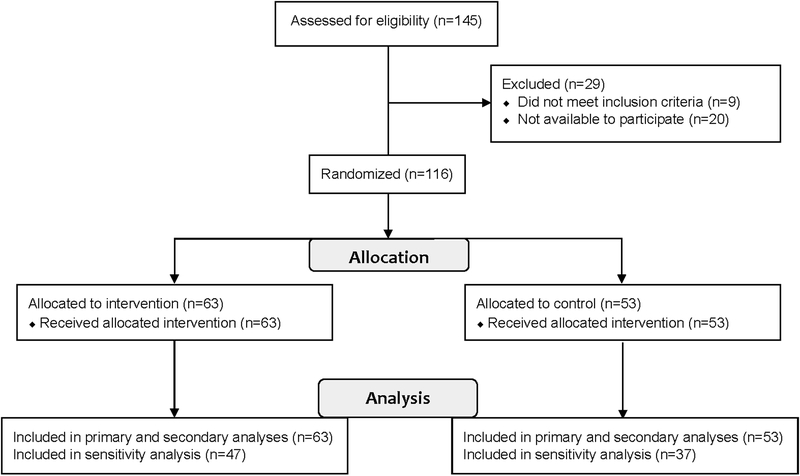
Out of 145 physicians assessed for eligibility, 116 met the inclusion criteria, were randomized, and completed the study (Fig. 2). Half of participants completed fellowship greater than or equal to 7 years ago (interquartile range [IQR], 2–13), and 80 (69%) were male (Table 1). Participants worked in hospitals in 17 states within the United States and reported working a median of 14 weeks (IQR, 8–22 wk) in the ICU during the previous year. There were 53 participants (45%) randomized to the control group and 63 (55%) in the intervention group, with similar distributions of baseline characteristics between the two groups (eTable 2, Supplemental Digital Content 1, http://links.lww.com/CCM/E495). The number of intensivists in the control and intervention groups was not equal because blocking was not used during randomization. No participants were lost to follow-up.
Figure 2.
Flow of intensivists through the Simulated Communication with ICU Proxies (SCIP) trial.
TABLE 1.
Characteristics of Enrolled Intensivists
| Characteristics | n = 116 |
|---|---|
| Age, median (IQR) | 40 (36–46) |
| Male, n (%) | 80 (69) |
| Hispanic or Latino, n (%)a | 11 (9) |
| Race, n (%)a | |
| White | 81 (70) |
| Asian | 23 (20) |
| > 1 race | 6 (5) |
| Black | 4 (3) |
| Primary hospital location | |
| Outside Maryland, n (%)b | 32 (28) |
| No. of weeks worked in the ICU last year, median (IQR) | 14 (8–22) |
| Critical care fellowship completed in the United States, n (%) | 109 (94) |
| Years since completing critical care fellowship, median (IQR) | 7 (2–13) |
| Type of ICU, n (%) | |
| Medical | 55 (47) |
| Mixed medical and surgical | 33 (28) |
| Surgical | 15 (13) |
| Trauma | 2 (2) |
| Neurologic | 2 (2) |
| Multiple types | 9 (8) |
| Hospital financial model, n (%)c | |
| Nonprofit | 105 (91) |
| For profit | 13 (11) |
| Hospital teaching status, n (%)c | |
| University | 81 (70) |
| Non-university teaching | 34 (29) |
| Nonteaching | 11 (9) |
| Current religion, n (%)a | |
| Catholic | 31 (27) |
| Agnostic/atheist/no religious affiliation | 29 (25) |
| Jewish | 15 (13) |
| Protestant | 15 (13) |
| Hindu | 8 (7) |
| Other | 11 (9) |
| How important is religion in your life? n (%)a | |
| Extremely/very important | 22 (19) |
| Moderately important | 23 (20) |
| Slightly/not at all important | 66 (57) |
IQR = interquartile range.
Missing values: race = 2, Hispanic = 2, religion = 7, importance of religion = 5.
Thirty-two participants (28%) practice outside of Maryland in the following 17 states: California, District of Columbia, Delaware, Hawaii, Illinois, Kentucky, Massachusetts, Michigan, Minnesota, North Carolina, New Jersey, New York, Pennsylvania, South Carolina, Utah, Vermont, Washington.
Percentages do not sum to 100% because some intensivists work in multiple hospitals.
In the intervention group, 50 intensivists (79%) said that they did not expect the patient to survive to hospital discharge, and 58 (92%) expected him to have new impairments that would prevent a return to independent living if he survived to 3-month follow-up (Table 2). A total of 54 participants (47%) selected palliative care from a list of possible consults to request as part of their medical management plan (Table 2).
TABLE 2.
Responses After Reviewing Patient Chart and Before Simulated Meeting With Patient’s Family
| Questions Asked of Intensivists Before Simulated Meeting | Intervention n = 63 | Control n = 53 |
|---|---|---|
| Are there any consults that you would like to order for this patient today? n (%) | ||
| Cardiology | 0 (0) | 0 (0) |
| Physical therapy | 15 (24) | 20 (38) |
| Palliative care | 28 (44) | 26 (49) |
| Other consult | 7 (11) | 3 (6) |
| Do you expect this patient to survive to hospital discharge? n (%) | ||
| No | 50 (79) | NA |
| Yes | 13 (21) | |
| If this patient survives his current hospitalization, what do you believe is his most likely outcome 3 mo from now? | ||
| Able to live independently; no physical or cognitive decline | 0 (0) | NA |
| Able to live independently; some physical or cognitive decline | 5 (8) | |
| Dependent in ≥ 1 ADL; unable to live independently | 36 (57) | |
| Dependent in all ADLs; unable to live independently | 18 (29) | |
| Deceased | 4 (6) | |
ADL = activities of daily living, NA = not applicable.
Intensivists randomized to the intervention group were no more likely to offer the option of care focused entirely on comfort (13% vs 13%; difference, 0% [95% CI, −13% to 12%]; p = 1.0), but more likely to inform the daughter that her father was sick enough to die as a result of his current illness (68% vs 43%; difference, 25% [95% CI, 5–44%]; p = 0.01) as determined by the blinded reviewers (Table 3). Clear communication that the patient might have new functional impairments if he survived was rare in both groups (3% vs 4%; difference, 1% [95% CI, −8% to 7%]; p = 1.0). Excluding simulations in which an actor deviated from the script did not have a material effect on the study results, and the study outcomes did not differ significantly across actors (eTables 3–6, Supplemental Digital Content 1, http://links.lww.com/CCM/E495).
TABLE 3.
Trial Outcomes, as Assessed by Blinded Intensivists and by Participant Self-Report
| Outcome | Intervention n = 63 | Control n = 53 | Difference in Proportions (95% CI) | p | Effect Size |
|---|---|---|---|---|---|
| Assessment of two blinded intensivistsa | |||||
| “Did this intensivist…” (n [%] responding “yes”) | |||||
| Communicate that the patient may die as a result of his current illness despite treatment? | 43 (68) | 23 (43) | 25% (5–44%) | 0.01 | 0.51 |
| Clearly communicate that the patient may experience new functional impairments if he survives? | 2 (3) | 2 (4) | −1% (−8% to 7%) | 1.0 | 0.03 |
| Offer the alternative of care focused entirely on comfort either now or as a possibility in the future? | 8 (13) | 7 (13) | 0% (−13% to 12%) | 1.0 | 0.02 |
| Intensivist self-report | |||||
| “During the simulation, did you.” (n [%] responding “Done”)b | |||||
| Convey prognosis for risk of death? | 58 (92) | 36 (68) | 24% (8–40%) | 0.002 | 0.64 |
| Convey prognosis for risk of postdischarge functional impairment? | 43 (68) | 26 (49) | 19% (0–39%) | 0.06 | 0.40 |
| Offer the alternative of care focused entirely on comfort? | 15 (24) | 17 (32) | −8% (−26% to 10%) | 0.43 | 0.18 |
Disagreements were resolved through discussion and consensus.
Response options to questions starting with “During the simulation, did you” were: done, not done, don’t remember, and not applicable.
Intensivists in the intervention group were no more likely than intensivists in the control to report that they offered care focused entirely on comfort (24% vs 32%; difference, −8% [95% CI, −26% to 10%]; p = 0.43). However, intensivists randomized to the intervention group were more likely to self-report that they conveyed prognosis for risk of death (92% vs 68%; difference, 24% [95% CI, 8–40%]; p = 0.002) and conveyed prognosis for risk of postdischarge functional impairment (68% vs 49%; difference, 19% [95% CI, 0–39%]; p = 0.06). The majority of intensivists in both groups perceived no disagreement or conflict during the simulated meeting, with 102 (88%) of all 116 intensivists rating conflict less than 3 on a 0–10 scale (eFigs. 1 and 2, Supplemental Digital Content 1, http://links.lww.com/CCM/E495). Intensivists rated conversations and emotions in the simulations as highly realistic (eFigs. 3–8, Supplemental Digital Content 1, http://links.lww.com/CCM/E495).
DISCUSSION
In this RCT, requiring intensivists to document expected in-hospital survival and 3-month functional prognosis of a critically ill patient at high risk of death or severe functional impairment resulted in intensivists being more likely to disclose prognosis for survival to the patient’s family within a well-controlled, high-fidelity medical simulation but had no effect on offering the option of care focused on comfort. This is encouraging because the majority of families want intensivists to disclose prognosis even when there is a high level of uncertainty (28). The intervention was designed to leverage the focusing effect (29–31), described as the human tendency to place more importance on factors we are prompted to consider. In this case, prompting intensivists to think about and document the patient’s in-hospital mortality and 3-month functional prognosis likely increased the importance of these outcomes in intensivists’ minds.
These findings contrast with results of our previous trial in which intensivists randomized to document 3-month functional prognosis for patients presented in online written vignettes were 49% (95% CI, 20–85%) more likely to self-report they would bring up the option of withdrawing life support in a subsequent family meeting (13). We offer four explanations that may help explain why prompting intensivists to consider a patient’s functional prognosis did not result in more intensivists informing families of the option of comfort-focused care in our trial.
First, some intensivists may have felt uncomfortable offering comfort care during a first meeting with family proxy. We could not observe the effect of prompting after a longer length of ICU stay, or on subsequent family meetings when there may have been a higher likelihood of offering comfort care. However, the study script directed actors to portray a passive, grateful, and trusting proxy who was open to hearing about comfort-focused care during a first meeting. A second possible explanation is that disclosing prognosis is a basic communication skill, whereas presenting the option of comfort-focused care for critically ill patients is a more advanced skill (32, 33). Intensivists may have intended to discuss comfort-focused care, but been unable to undertake this discussion in the presence of an actor performing emotion after learning about her father’s poor prognosis. Third, intensivists may have been comfortable discussing comfort care, but intentionally chosen not to inform the proxy, at this point in time, that comfort-focused care was an option. The clinical scenario was developed so that the patient was almost assured of an impaired functional recovery, and in-hospital death was highly probable but not certain. If intensivists intentionally do not offer the choice to forego critical care interventions without complete confidence that a patient will die, then most critically ill patients are unlikely to have access to comfort-focused care until their final days or hours of life. Finally, the actor portrayed an African American with low health literacy in Baltimore where high end-of-life treatment intensity is common (34).
There were substantial differences between the communication behaviors intensivists self-reported performing, and the behaviors that blinded intensivist reviewers identified in written transcripts. This difference may be partly attributable to differences in the wording of questions, with intensivists asked “did you convey prognosis?” and reviewers asked if prognosis was “clearly communicated.” This was particularly true for communication about future functional impairment, for which blinded reviewers only coded as “occurring” if the intensivist clearly explained that the patient might not be able to perform self-care or have new physical or cognitive impairments.
The limitations of the SCIP study include randomizing a convenience sample of U.S. intensivists and using a single standardized clinical scenario. Developing a single scenario prohibits us from making inferences about the effect of documenting functional prognosis for patients with different pre-ICU health states or prognoses, or at different time points in the ICU stay. However, using a standardized scenario eliminated important sources of variability in understanding the effect of the intervention. The trial’s strengths include testing a no-cost intervention designed to leverage a known behavioral phenomenon (29–31) to increase compliance with evidence-based practice recommendations from the Critical Care Choosing Wisely Task Force (12). We employed deception in accord with accepted ethical standards for experimental psychologic studies (14–17) to minimize social desirability bias from participants and actors. The insights gained from this controlled approach are not possible in pragmatic real-world clinical trials and help clearly elucidate the intervention’s mechanistic effects.
In conclusion, this RCT demonstrates that requiring intensivists to document in-hospital survival and 3-month functional prognoses for a critically ill patient at high risk of death or severely impaired functional recovery significantly increased their disclosure of survival prognosis to the patient’s family. However, the intervention did not make intensivists more likely to offer the option of care focused entirely on comfort, even though most intensivists believed the patient would not survive hospitalization or return to independent living. Further research in real-world clinical settings is needed to fully assess the impact of prompting intensivists to consider prognosis. Meanwhile, practicing intensivists should consider routinely asking themselves: “What is this patient’s most likely outcome 3 months from now?” and “Does the patient/family know they have the option of comfort care?”
Supplementary Material
ACKNOWLEDGMENTS
We thank the critical care physicians who participated in this study. Special thanks to the study actors Barbara King, Hiawatha Howard, and Kecia Campbell for their hard work and dedication. We also thank the staff at the Johns Hopkins Simulation Center for their technical expertise. Thanks to the Critical Care Assembly of the American Thoracic Society for their assistance with recruitment. Finally, thanks to Leeza Faraone, BS, Gabriel Ukwuoma, and An To, MS, for research assistance and administrative support.
Supported, in part, by grant from the Gordon and Betty Moore Foundation.
Dr. Turnbull, Ms. Basyal, and Dr. Needham’s institutions received funding from the Gordon and Betty Moore Foundation. Dr. Brower received funding from Theravance and Applied Clinical Intelligence. Dr. White’s institution received funding from the National Institutes of Health and Greenwall Foundation, and he received funding from UptoDate. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
See also p. 865.
REFERENCES
- 1.Teno JM, Gozalo PL, Bynum JP, et al. : Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013; 309:470–477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teno JM, Gozalo P, Trivedi AN, et al. : Site of death, place of care, and health care transitions among US medicare beneficiaries, 2000–2015. JAMA 2018; 320:264–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fried TR, Bradley EH, Towle VR, et al. : Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002; 346: 1061–1066 [DOI] [PubMed] [Google Scholar]
- 4.Somogyi-Zalud E, Zhong Z, Hamel MB, et al. : The use of life-sustaining treatments in hospitalized persons aged 80 and older. J Am Geriatr Soc 2002; 50:930–934 [DOI] [PubMed] [Google Scholar]
- 5.Fischer S, Min SJ, Cervantes L, et al. : Where do you want to spend your last days of life? Low concordance between preferred and actual site of death among hospitalized adults. J Hosp Med 2013; 8: 178–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bischoff KE, Sudore R, Miao Y, et al. : Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc 2013; 61:209–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicholas LH, Langa KM, Iwashyna TJ, et al. : Regional variation in the association between advance directives and end-of-life medicare expenditures. JAMA 2011; 306:1447–1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dumanovsky T, Augustin R, Rogers M, et al. : The growth of palliative care in U.S. hospitals: A status report. J Palliat Med 2016; 19:8–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hua M, Ma X, Morrison RS, et al. : Association between the availability of hospital-based palliative care and treatment intensity for critically ill patients. Ann Am Thorac Soc 2018; 15:1067–1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schenker Y, Tiver GA, Hong SY, et al. : Association between physicians’ beliefs and the option of comfort care for critically ill patients. Intensive Care Med 2012; 38:1607–1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keating NL, Huskamp HA, Kouri E, et al. : Factors contributing to geographic variation in end-of-life expenditures for cancer patients. Health Aff (Millwood) 2018; 37:1136–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halpern SD, Becker D, Curtis JR, et al. ; Choosing Wisely Taskforce; American Thoracic Society; American Association of Critical-Care Nurses; Society of Critical Care Medicine: An official American Thoracic Society/American Association of Critical-Care Nurses/American College of Chest Physicians/Society of Critical Care Medicine policy statement: The Choosing Wisely® Top 5 list in Critical Care Medicine. Am J Respir Crit Care Med 2014; 190:818–826 [DOI] [PubMed] [Google Scholar]
- 13.Turnbull AE, Krall JR, Ruhl AP, et al. : A scenario-based, randomized trial of patient values and functional prognosis on intensivist intent to discuss withdrawing life support. Crit Care Med 2014; 42: 1455–1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boutron I, Guittet L, Estellat C, et al. : Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med 2007; 4:e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rhodes KV, Miller FG: Simulated patient studies: An ethical analysis. Milbank Q 2012; 90:706–724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCambridge J, Kypri K, Bendtsen P, et al. : The use of deception in public health behavioral intervention trials: A case study of three online alcohol trials. Am J Bioeth 2013; 13:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCambridge J, Kypri K, Elbourne D: In randomization we trust? There are overlooked problems in experimenting with people in behavioral intervention trials. J Clin Epidemiol 2014; 67: 247–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.R Core Team: R: A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing, 2016 [Google Scholar]
- 19.Doig GS, Simpson F: Randomization and allocation concealment: a practical guide for researchers. J Crit Care 2005; 20:187–191 [DOI] [PubMed] [Google Scholar]
- 20.Knaus WA, Wagner DP, Draper EA, et al. : The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991; 100:1619–1636 [DOI] [PubMed] [Google Scholar]
- 21.Lemeshow S, Teres D, Klar J, et al. : Mortality Probability Models (MPM II) based on an international cohort of intensive care unit patients. JAMA 1993; 270:2478–2486 [PubMed] [Google Scholar]
- 22.Lemeshow S, Klar J, Teres D, et al. : Mortality probability models for patients in the intensive care unit for 48 or 72 hours: A prospective, multicenter study. Crit Care Med 1994; 22:1351–1358 [DOI] [PubMed] [Google Scholar]
- 23.Chiarchiaro J, Schuster RA, Ernecoff NC, et al. : Developing a simulation to study conflict in intensive care units. Ann Am Thorac Soc 2015; 12:526–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White DB, Engelberg RA, Wenrich MD, et al. : Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med 2007; 35:442–448 [DOI] [PubMed] [Google Scholar]
- 25.White DB, Engelberg RA, Wenrich MD, et al. : The language of prognostication in intensive care units. Med Decis Making 2010; 30:76–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White DB, Malvar G, Karr J, et al. : Expanding the paradigm of the physician’s role in surrogate decision-making: An empirically derived framework. Crit Care Med 2010; 38:743–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uy J, White DB, Mohan D, et al. : Physicians’ decision-making roles for an acutely unstable critically and terminally ill patient. Crit Care Med 2013; 41:1511–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans LR, Boyd EA, Malvar G, et al. : Surrogate decision-makers’ perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med 2009; 179:48–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kahneman D, Krueger AB, Schkade D, et al. : Would you be happier if you were richer? A focusing illusion. Science 2006; 312:1908–1910 [DOI] [PubMed] [Google Scholar]
- 30.Schkade DA, Kahneman D: Does living in California make people happy? A focusing illusion in judgments of life satisfaction. Psychol Sci 1998; 9:340–346 [Google Scholar]
- 31.Halpern SD: Using default options and other nudges to improve critical care. Crit Care Med 2018; 46:460–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Back AL, Arnold RM, Baile WF, et al. : Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007; 167:453–460 [DOI] [PubMed] [Google Scholar]
- 33.Bays AM, Engelberg RA, Back AL, et al. : Interprofessional communication skills training for serious illness: Evaluation of a small-group, simulated patient intervention. J Palliat Med 2014; 17:159–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barnato AE, Chang CH, Lave JR, et al. : The paradox of end-of-life hospital treatment intensity among black patients: A retrospective cohort study. J Palliat Med 2018; 21:69–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.