Abstract
Objective:
To ascertain opinions regarding etiology and preventability of hospital-onset bacteremia and fungemia (HOB) and perspectives on HOB as a potential outcome measure reflecting quality of infection prevention and hospital care.
Design:
Cross-sectional survey.
Participants:
Hospital epidemiologists and infection preventionist members of the Society for Healthcare Epidemiology of America (SHEA) Research Network.
Methods:
A web-based, multiple-choice survey was administered via the SHEA Research Network to 133 hospitals.
Results:
A total of 89 surveys were completed (67% response rate). Overall, 60% of respondents defined HOB as a positive blood culture on or after hospital day 3. Central line-associated bloodstream infections and intra-abdominal infections were perceived as the most frequent etiologies. Moreover, 61% thought that most HOB events are preventable, and 54% viewed HOB as a measure reflecting a hospital’s quality of care. Also, 29% of respondents’ hospitals already collect HOB data for internal purposes. Given a choice to publicly report central-line–associated bloodstream infections (CLABSIs) and/or HOB, 57% favored reporting either HOB alone (22%) or in addition to CLABSI (35%) and 34% favored CLABSI alone.
Conclusions:
Among the majority of SHEA Research Network respondents, HOB is perceived as preventable, reflective of quality of care, and potentially acceptable as a publicly reported quality metric. Further studies on HOB are needed, including validation as a quality measure, assessment of risk adjustment, and formation of evidence-based bundles and toolkits to facilitate measurement and improvement of HOB rates.
Background
National surveillance data have documented a 50% decrease in central-line–associated bloodstream infections (CLABSIs) between 2008 and 2014.1 Reporting of CLABSIs to the Centers for Disease Control and Prevention’s National Healthcare Safety Network (CDC NHSN) and use of these data in the Centers for Medicare and Medicaid Services (CMS) pay-for-performance programs likely promoted enhanced infection prevention efforts and CLABSI reductions. Although this progress is encouraging, CLABSIs represent a subset of overall hospital-onset bacteremias and fungemias (HOB) that also include bacteremias due to other potentially preventable etiologies such as intra-abdominal infection, surgical site infections, healthcare-associated pneumonia, and common skin commensal organisms.
The use of HOB as a quality measure has several potential benefits. First, in addition to capturing NHSN CLABSI and MRSA laboratory events, secondary bacteremia events (eg, peripheral-line–associated infections, pneumonia, and urinary tract infections) would also be included, and a significant proportion of these could be preventable.2 Focusing infection preventionists and frontline clinical staff on preventing these additional bacteremias could enhance patient safety. Second, likely because of sustained improvement efforts, CLABSIs have significantly decreased nationally, and for most hospitals they are an uncommon event.1,3 A low number of NHSN reported CLABSI events can significantly change the summary statistic for inter-hospital comparisons, which uses an indirect standardization method (standardized infection ratios).4 However, HOB is a much more common event and therefore allows for greater discrimination in interhospital comparisons.5 Third, HOB events could be directly obtained from an electronic health record system without requiring an infection preventionist’s application of a surveillance definition, making HOB more objective and less labor intensive to measure.
There is currently no standardized surveillance definition for HOB. Hospital epidemiologist and infection preventionist input in the early stages of outcome metric development may provide valuable information and lead to more robust, informed, and practical metrics. The aim of this study is to ascertain hospital epidemiologist and infection preventionist opinions regarding etiology and preventability of HOB and their perspectives on HOB as a potential outcome measure reflecting quality of infection prevention and hospital care.
Methods
A survey was developed in conjunction with the Society for Healthcare Epidemiology of America (SHEA) Research Committee, reviewed and piloted by the SHEA Research Network Review and Research Committees.
The SHEA Research Network is a consortium of 133 US and international hospitals (at the time of the survey) that have successfully conducted multicenter projects in the field of healthcare epidemiology.5–8 A 14-question survey was designed based on expert opinion to evaluate perceptions regarding potential HOB definition, sources, preventability, and acceptability as a quality measure (supplement). On April 20, 2017, the survey was distributed via e-mail through the SHEA Research Network. Surveys were sent to 1 representative from each participating hospital. That representative, usually a healthcare epidemiologist, was instructed to either complete the survey or to assign it on to a professional colleague from their hospital who they deemed to be the most knowledgeable in this field. The initial email was followed by reminders at 1 and 2 weeks. Responses were submitted anonymously, with a unique identifier that could be linked back to baseline hospital demographics shared upon the time of joining the SHEA Research Network. Respondents were not required to answer every question. No payment or incentives were offered for survey completion. This study was approved by the Johns Hopkins University institutional review board as nonhuman subjects research. A descriptive analysis was performed using Excel version 16.12 software (Microsoft, Redmond, WA).
Results
Overall, 89 surveys were completed (response rate, 67%), with varying response frequency per question (71 minimum, 89 maximum). Among all 89 respondents, 70 (79%) represented US hospitals, while 18 respondents (20%) represented hospitals outside the United States (1 respondent did not specify country of origin). In addition, 57 respondents (64%) identified as a healthcare epidemiologists, 15 (17%) identified as infection preventionists, and 35 respondents (39%) also served as an infection committee chair. Furthermore, 67 respondents (75%) were from academic-affiliated hospitals: 56 (63%) from academic or teaching hospitals, 11 (12%) from community hospitals with academic affiliations, 4 (4%) from community hospitals without academic affiliations, 3 (3%) from Veterans Affairs hospitals, 1 (1%) from a freestanding pediatric hospital, and the remaining 14 (16%) were from other categories. A small number of respondents (4 of 89, 44%) represented hospitals with 0–100 beds, whereas most respondents represented medium-sized hospitals with 101–500 beds (40 of 89, 45%), and large hospitals with ≥500 beds (39 of 89, 44%), and 6 (7%) did not specify.
Definition of HOB
When asked the appropriate number of days post hospital admission that a positive blood culture should qualify as ‘hospital onset,’ 53 of 89 (60%) responded on hospital day 3 or later. Nearly all respondents (75 of 76, 99%) agreed that a single patient could contribute >1 HOB event during the same hospitalization. However, opinions regarding what constituted a new event differed: 23 of 76 (30%) would require a different organism; 22 of 76 (29%) would require an interval of time between positive cultures; 2 weeks was the interval most frequently selected (12 of 22, 55%), and 6 of 76 (8%) would require negative blood cultures between HOB events. Of 77 respondents, 47 (61%) indicated that common skin commensal organisms should only be included if at least 2 sets of blood cultures were positive with the same organism within 24 hours. Of 77 respondents, 71 (92%) favored inclusion of Enterococcus. However, criteria differed among respondents: 27 of 77 of respondents (35%) would require ≥2 Enterococcus-positive blood cultures to document an Enterococcus HOB; 26 of 77 (34%) would require only a single Enterococcus-positive blood culture, and 13 of 77 (16%) would require documentation of a simultaneous infection at another body site.
Etiology of HOB
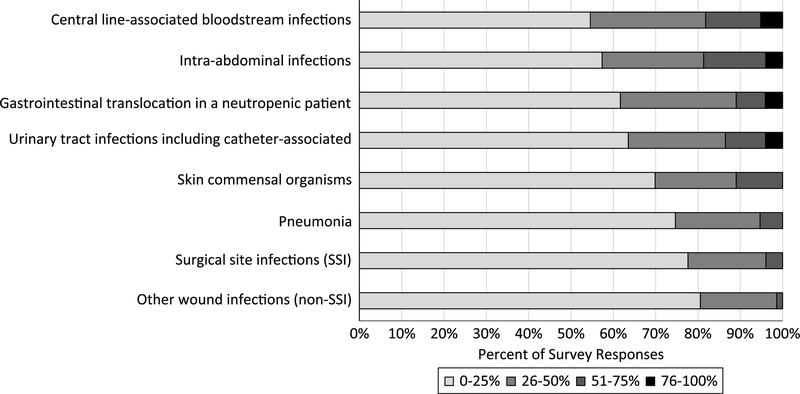
CLABSI and intra-abdominal infections were perceived to be the most frequent sources of HOB, with ~20% of respondents stating that >50% their HOB were due to either of these 2 etiologies (Fig. 1). Other perceived HOB sources included (in descending order of likelihood): gastrointestinal translocation in a neutropenic patient, urinary tract infections including catheter-associated, skin commensal organisms, pneumonia, surgical site infections, and other wound infections (Fig. 1).
Fig. 1.
Perceived etiologies of hospital-onset bacteremia and fungemia (HOB) among hospital epidemiologists and infection control practitioners.*n = 76.
*Survey respondents were asked: “Most facilities do not assess the etiology of hospital-onset bacteremia; however, in your opinion, for your facility overall, what proportion of hospital-onset bacteremia/fungemia do you think is attributable to: (these categories are not mutually exclusive and do not need to add to 100%)”
Preventability of HOB
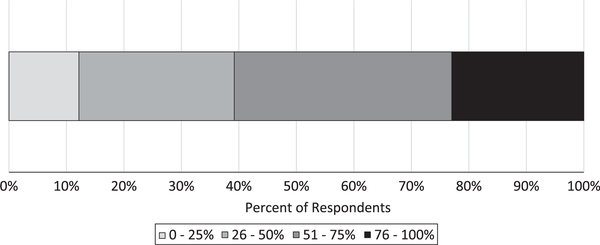
Most respondents (45 of 74, 61%) perceived ≥50% of HOB events as preventable under current practices; 17 of 74 (23%) considered ≥75% of HOB events preventable (Fig. 2). Among possible clinical sources of HOB, respondents ranked CLABSI as most likely to be preventable, followed by urinary tract infection (including catheter-associated), skin and soft-tissue infections, skin commensals and pneumonia. Gastrointestinal translocation was ranked as least preventable.
Fig. 2.
Proportion of hospital-onset bacteremia and fungemia (HOB) perceived as preventable under current infection prevention and clinical practices.*n = 74.
*Survey respondents were asked: “A proportion of hospital-onset bacteremia/fungemia at your facility is likely preventable with current infection prevention and clinical practice. In your opinion, at your institution, what would the increase be in hospital-onset bacteremia rate if current infection prevention and clinical practices were removed?”
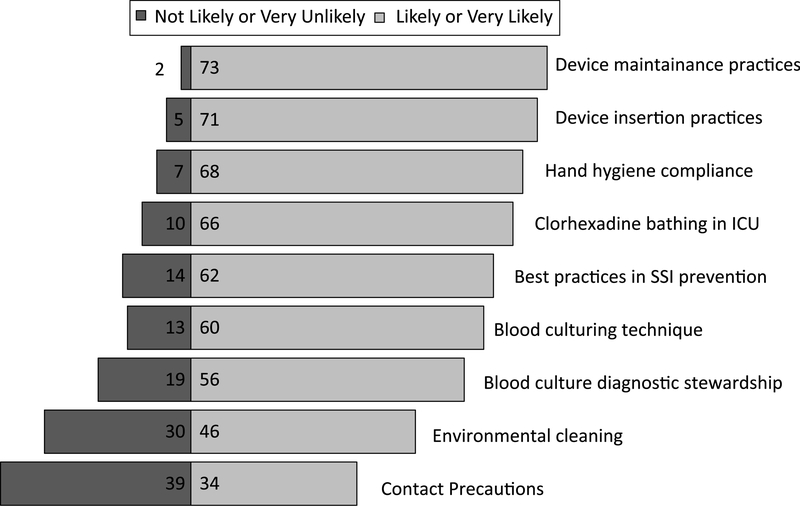
Improving indwelling device maintenance practices was ranked as most likely to reduce HOB, followed by device insertion practices and hand hygiene compliance. Most respondents indicated that enhanced patient environment cleaning and improved adherence to contact precautions were unlikely to reduce HOB events (Fig. 3).
Fig. 3.
Infection prevention improvement initiatives perceived as most likely to reduce hospital-onset bacteremia and fungemia (HOB).*n = 76.
*Survey respondents were asked: “In your opinion, how likely are the following specific infection practices to reduce hospital-onset bacteremia/fungemia?”
HOB as a metric of quality of hospital care
Among 76 respondents, 41 (54%) indicated that HOB reflects quality of care provided at a hospital, 14 of 76 (18%) disagreed, 21 of 76 (28%) neither agreed nor disagreed. Opinions differed regarding the possible reaction of frontline healthcare providers to use of HOB if used as an outcome measure. Moreover, 41 of 76 (46%) anticipated that it would be well received, 30% 23 of 76 (30%) anticipated that it would not be well received, and 18 of 76 (23%) anticipated a neutral reception. There were no statistically significant differences in these results when the data were stratified by academic affiliation, hospital size, or US versus non-US hospitals.
Regarding public reporting, 27 of 77 (35%) would like HOB to be used in addition to CLABSI, 26 (34%) would prefer CLABSI alone, 17 of 77 (22%) would favor HOB over CLABSI reporting, and 7 (9%) replied “other,” with most free-text responses stating that more studies were needed to decide. There were no statistically significant differences in these results when the data were stratified by academic affiliation, hospital size, or US versus non-US hospitals.
Nearly all respondents stated that the required elements for a HOB measure could be extracted electronically from a hospital database, including the date of blood culture (75 of 77, 97%), the causative organism (73 of 77, 95%), and the location or unit where the culture was collected (69 of 77, 90%). Of 77 respondents, 22 (29%) stated that their hospital already measures HOB, and 12 of 77 (22%) already use HOB to guide performance improvement efforts.
Discussion
Even at this exploratory stage of HOB measure development, with no consensus definition, most hospital epidemiologists and infection preventionists supported HOB as a measure of quality of care provided at acute-care hospitals. They perceived HOB to be potentially preventable with basic infection prevention practice improvements, such as adherence to correct device insertion and maintenance practices, hand hygiene compliance, chlorhexidine bathing in intensive care units, and surgical site infection prevention practices. The survey responses supported the feasibility of HOB for reporting; nearly all believed that data for HOB can be extracted electronically from hospital databases and electronic medical records. Interestingly, nearly one-quarter of respondents currently use HOB to direct performance improvement efforts despite lack of regulatory requirement, benchmarks for interhospital comparison, or a standardized surveillance definition. This finding may be attributable to respondents’ varying interpretation of what constitutes HOB, the practice of reviewing all bacteremias as part of CLABSI surveillance, or infection prevention programs expanding the NHSN methicillin-resistant Staphylococcus aureus (MRSA) laboratory event definition to include other organisms for internal surveillance. Most respondents thought HOB was appropriate for public reporting, either concurrently with CLABSI or in lieu of CLABSI.
The potential benefits and unintended consequences of routine HOB surveillance require further exploration. If HOB rates are shown to be a reliable indicator of healthcare-associated infection (HAI) burden, then HOB surveillance could inform broad measures to improve infection control in conjunction with other HAI data, potentially resulting in measurably improved patient outcomes. HOB data collection and reporting burden would likely be low given the ubiquity and functionality of current EHRs, in contrast to NHSN CLABSI and other measures that call for substantial investments of time and effort in manual reviews of healthcare records.9,10 For HOB surveillance to efficiently contribute to improved quality of care, any guidelines for interpreting and acting upon HOB data should minimize the need to perform in-depth chart review, as this could be burdensome to infection control programs at a time when many are already underresourced.11 Ideally, EHR-based tools could be created to ascertain indicators of various HOB etiologies, therefore allowing infection control programs to direct resources toward prevention activities. Additionally, measurement of HOB is likely to be influenced by local blood culturing practices. The introduction of HOB surveillance could potentially influence providers to reduce blood culturing, even when it is clinically indicated, which could lead to patient harm. Blood-culturing practices may need to be monitored and potentially adjusted when measuring HOB. Finally, one-third of respondents indicated that they anticipate resistance to this measure by frontline clinicians. Qualitative research, such as focus groups involving frontline clinicians, nurses, infection preventionists, hospital epidemiologists. and other healthcare workers would be needed to understand barriers and benefits to using this measure for performance improvement.
This study has several limitations. For this early exploratory survey, there was no consensus on some aspects of HOB definition, including hospitalization date to qualify as hospital-onset, repeat event definitions, and interpretation of skin commensals and Enterococcus, highlighting areas of controversy that need further evaluation. However, some responses may have differed in the setting of a clearly defined HOB definition. Although we had a high response rate, respondents were mostly affiliated with academic hospitals; therefore, results may not be generalizable to other settings. Because HOB is not currently in widespread use as a quality measure, responses are based on opinion and perceptions of preventability and potential use, rather than objective clinical data. Further research and validation are needed to determine whether HOB would be a valid hospital quality measure. This includes (1) the need to standardize and validate a HOB surveillance definition that accounts for a variety of patient populations (eg, adult and pediatric, high risk populations such as neutropenic and burn patients), diverse clinical settings (academic, community, resource-limited), emerging non-culture diagnostic testing, and potentially previous healthcare exposures (2) the need to evaluate whether reductions in HOB events lead to other benefits for patients, such as decreased mortality, shorter hospitalizations, or decreased cost (3) the need to create evidence-based guidance and tools for clinicians and infection preventionists to improve hospital HOB rates, and (4) the need to develop robust risk adjustment methods to facilitate fair public reporting. Further studies aimed at validating an HOB surveillance definition and understanding HOB etiologies and preventability are now underway within the CDC Prevention Epicenters Program. If these studies, and additional field testing, can address knowledge gaps in surveillance methods and preventability and operational requirements for EHR-based differentiation of HOB etiologies, then HOB surveillance in acute-care hospitals could be standardized and implemented through the NHSN. The use of the NHSN for HOB surveillance, in turn, could facilitate broad uptake of a promising new metric, could enable national benchmarks to be set and applied at the hospital level and all geographic levels, and could provide further impetus for HAI prevention.
Acknowledgments.
The findings and conclusions presented here are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support. C.R., A.M.M., A.D.H., and S.L. are supported by the Centers for Disease Control Prevention Epicenters Program. A.D.H. is also supported by a grant from the national Institutes of Health (NIH grant no. 5K24AI079040–05).
Footnotes
Conflicts of interest. The authors report no financial conflicts of interest related to this work.
References
- 1.National and state healthcare associated infections progress report. Centers for Disease Control and Prevention website. https://www.cdc.gov/hai/pdfs/progress-report/hai-progress-report.pdf. Published 2016. Accessed February 15, 2019.
- 2.Dantes RB, Rock C, Milstone AM, et al. Preventability of hospital onset bacteremia and fungemia: a pilot study of a potential new indicator of healthcare-associated infections. Presented at IDWeek 2017. on October 5, 2017; San Diego, CA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pronovost PJ, Watson SR, Goeschel CA, Hyzy RC, Berenholtz SM. Sustaining reductions in central line-associated bloodstream infections in Michigan intensive care units: a 10-year analysis. Am J Med Qual 2016;31:197–202. [DOI] [PubMed] [Google Scholar]
- 4.The NHSN standardized infection ratio (SIR). Centers for Disease Control and Prevention website. https://www.cdc.gov/nhsn/pdfs/ps-analysisresources/nhsn-sir-guide.pdf. Published 2018. Accessed February 15, 2019.
- 5.Rock C, Thom KA, Harris AD, et al. A multicenter longitudinal study of hospital-onset bacteremia: time for a new quality outcome measure? Infect Control Hosp Epidemiol 2016;37:143–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan DJ, Meddings J, Saint S, et al. Does nonpayment for hospital-acquired catheter-associated urinary tract infections lead to overtesting and increased antimicrobial prescribing? Clin Infect Dis 2012;55:923–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drees M, Pineles L, Harris AD, Morgan DJ. Variation in definitions and isolation procedures for multidrug-resistant gram-negative bacteria: a survey of the Society for Healthcare Epidemiology of America Research Network. Infect Control Hosp Epidemiol 2014;35:362–366. [DOI] [PubMed] [Google Scholar]
- 8.Harris AD, Pineles L, Belton B, et al. Universal glove and gown use and acquisition of antibiotic-resistant bacteria in the ICU: a randomized trial. JAMA 2013;310:1571–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell BG, Hall L, Halton K, MacBeth D, Gardner A. Time spent by infection control professionals undertaking healthcare associated infection surveillance: A multi-centred cross sectional study. Infection, Disease & Health 2016;21:36–40. [Google Scholar]
- 10.Parrillo SL. The Burden of National Healthcare Safety Network (NHSN) reporting on the infection preventionist: a community hospital perspective. Am J Infect Control 2015;43(6):S17. [Google Scholar]
- 11.Bryant KA, Harris AD, Gould CV, et al. Necessary infrastructure of infection prevention and healthcare epidemiology programs: a review. Infect Control Hosp Epidemiol 2016;37:371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]