Abstract
Objectives:
To identify comorbidity profiles of older patients last seen in primary care prior to a suicide attempt, and assess attempt and clinical factors (e.g., means and lethality of attempt) associated with these profiles.
Design:
Cohort study and latent class analysis using VA national data (2012–2014).
Setting:
All Department of Veterans Affairs (VA) medical centers in the United States.
Participants:
2,131 patients 65 years and older who were last seen by a primary care provider prior to a first documented suicide attempt.
Measurements:
Fatal suicide attempt and means were identified using the National Suicide Data Repository. Non-fatal attempt was defined using the National Suicide Prevention Applications Network. Medical and psychiatric diagnoses and other variables were determined from electronic medical records.
Results:
Patients (mean age 74.4, 98.2% male) were clustered into 5 classes based on medical and psychiatric diagnoses: Minimal Comorbidity (23.2%); Chronic Pain-Osteoarthritis (30.1%); Depression-Chronic Pain (22.9%); Depression–Medical Comorbidity (16.5%); and High Comorbidity (7.3%). The Minimal Comorbidity and Chronic Pain-Osteoarthritis classes were most likely to attempt fatally compared to classes with higher burden of comorbidities. Overall, 61% of the sample attempted fatally, and 82.5% of suicide decedents used firearms.
Conclusion:
This study provides evidence that the majority of comorbidity profiles (>50%) in primary care patients attempting suicide was characterized by minimal depression diagnoses and fatal attempts, mostly with firearms. These findings suggest that more than a depression diagnosis contributes to risk and that conversations about firearm safety by medical providers may play an important role in suicide intervention and prevention.
Keywords: late life suicide, comorbidity, primary care, firearms, epidemiology
INTRODUCTION
Late-life suicide is a pressing public health concern1, with greater lethality of attempts among older compared to younger adults2. Moreover, research indicates that 50–70% of older adults who attempt suicide see their primary care provider within one month of their attempt3,4. Although depression, physical illness and pain have been identified as separate risk factors for suicide attempt following a primary care visit among older adults5–7, little is known about the spectrum of medical and psychiatric comorbidities in these patients beyond this. The knowledge gap is important, as such comorbidity profiles may serve as valuable markers, uniquely characterizing those who may attempt in ways that a diagnosis alone is unable to capture.
There is a dearth of prior studies addressing complexities of comorbidities in late-life suicide attempters, with most studies focusing on predictive value of individual risk factors6 such as depression8, or retrospective data from suicide notes9 regarding characterization of attempters. The presence of medical illness burden in isolation from or in tandem with psychiatric comorbidity is less clear, particularly in larger samples, which may lead to mischaracterization of absent risk for certain patients. A focus on identifying comorbidity profiles rather than individual diagnoses10 has been indicated as a vital focus of future research in suicide prevention11. Further, perceptions that suicide risk is limited to those with diagnosed depression or co-occurring psychiatric conditions makes it challenging for providers to effectively assess risk among patients without those diagnoses8, especially given limited resources12. Broadening the evidence base about who is at risk for a suicide attempt in late life, and how to approach preventive intervention accordingly, is thus a vital priority.
The primary objective of our study was to identify medical and psychiatric comorbidity clusters within a sample of older patients who attempted suicide between 2012–2014, and were last seen in primary care prior to that attempt. Our secondary objective was to describe attempt and clinical factors such as means and lethality of attempt, related to those profiles. National data from the VA Health Care System, the largest integrated US healthcare system with a large proportion of geriatric patients, provides a unique opportunity to achieve these objectives.
METHODS
Data and Participants
A cohort of all patients 65 years and older who used VA health care services and had a first late-life suicide attempt between 2012 and 2014 was formed by linking four national databases: 1) National Patient Care Database (NPCD), which includes all VA inpatient and outpatient services; 2) Centers for Medicare and Medicaid Services (CMS) data, which includes medical claims/diagnoses; 3) Suicide Prevention Applications Network (SPAN), which contains information about suicide attempts documented beginning in 200813−15; and 4) Suicide Data Repository (SDR), containing information about cause of death16. Records were extracted for patients 65 and older seen at a VA healthcare facility in primary care between October 1, 2011 and December 31, 2014. The final sample included 2,131 patients who had a first documented late-life suicide attempt during this time period, no recent previous attempt between October 1, 2007 and September 30, 2011, and had a provider in VA primary care as their last point of contact prior to that attempt. Demographic information including age, gender, race and marital status was obtained from the NPCD and/or CMS database records, with education and socioeconomic status extrapolated from census data based on residential zip code at the time of the primary care visit. This study was approved by the institutional review boards of San Francisco VA Medical Center and the University of California, San Francisco.
Measures
Fatal and non-fatal suicide attempt.
Data regarding first suicide attempt were obtained from the National SDR (fatal attempt) and SPAN (non-fatal attempt) data. The SDR data includes underlying (primary) cause of death information on all veterans using ICD-10 codes, including data from the CDC’s National Death Index. ICD-10 codes for fatal attempt or death by suicide included X60-X84 and Y87.0. In terms of non-fatal attempts, SPAN is a tracking system that uses a standardized method for recording suicide attempts, including attempt date, based on clinician reports from local databases13–15. The method used to identify attempts is the CDC’s Self-Directed Violence Classification System.
Medical and psychiatric diagnoses.
Diagnoses of common and major medical17 and psychiatric disorders18 were determined using ICD-9 codes included in NPCD and/or CMS database records at or within 2 years before the last primary care visit prior to the suicide attempt. Medical disorders included myocardial infarction (MI), congestive heart failure (CHF), stroke or TIA, chronic obstructive pulmonary disease (COPD), cancer, dementia, traumatic brain injury (TBI), hepatitis C, osteoarthritis, renal disease, chronic pain, and sleep disorder. Psychiatric disorders included depression, dysthymia, bipolar disorder, post-traumatic stress disorder (PTSD), generalized anxiety disorder (GAD), alcohol abuse, drug abuse, tobacco dependence, schizophrenia and personality disorder. ICD-9 codes of prior history of suicidal ideation was also included, along with information on suicidal ideation from the SPAN database.
Utilization variables.
Timing of the primary care visit relative to the suicide attempt, as well as type of primary care visit (telephone visit, in-person visit, and/or mental health primary care visit) were determined from NPCD data. Mental health primary care is an interdisciplinary service available in VA primary care settings (at VA hospitals, community-based outpatient clinics and in home-based primary care), whereby a patient may see a mental health provider with a health psychology focus in the primary care setting, rather than in mental health clinic19.
Statistical Analyses
Latent class analysis (LCA) was conducted in which all individuals were classified based on medical and psychiatric comorbidities described above. Several fit criteria are simultaneously assessed within LCA. Specifically, Akaike (AIC), Bayesian (BIC), and sample-size adjusted Bayesian information criterions, entropy values, G-squared deviance statistic (G2) and degrees of freedom (DF) were used, with lower values of Akaike and Bayesian information criteria and G2, and higher entropy values indicating better model fit and classification20,21. In order to determine the best-fitting number of classes, a combination of fit criteria, theoretical parsimony, and clinical interpretability were taken into consideration20, with models of increasing complexity compared until the best-fitting number of classes were identified22.
Once the best-fitting model comprising profiles of medical and psychiatric diagnoses was identified, the sample as a whole and the individual classes were described by attempt-related factors and utilization of health services within primary care, using bivariate analyses across classes. Factors describing the sample and individual classes were assessed using means and standard deviations or frequencies and proportions, with statistical significance of differences between the classes tested by F tests for continuous variables and chi-square tests for categorical variables.
All analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina), with statistical tests using a two-tailed p-value <.05 to indicate statistical significance.
RESULTS
A progressive number of classes were analyzed for relative model fit, beginning with a one-class model, through a six-class model (models for three through six classes are displayed in Table 1). The higher numbers of classes (up to five) were associated with improved model fit on the information criteria and entropy. However, the six-class model did not indicate a substantial improvement in information criteria, and resulted in one of the five classes being split into a barely distinguishable subgroup. Thus, interpretability and clinical utility of the five-class model was superior, as was theoretical parsimony. These factors together indicated that a five-class model of medical and psychiatric comorbidities best fit the data. Additionally, the latent classes were well-classified, as evidenced by low error proportions for classification of individuals in each class (standard error of the gamma estimate below 4% for each class in the final model).
Table 1.
Comparison of baseline modelsa
| Model | ||||
|---|---|---|---|---|
| Fit index | 3 clusters | 4 clusters | 5 clusters | 6 clusters |
| AIC | 10215.12 | 9854.91 | 9667.34 | 9519.93 |
| BIC | 10602.24 | 10372.98 | 10316.34 | 10299.87 |
| Adjusted BIC | 10386.20 | 10083.86 | 9954.15 | 9864.60 |
| Entropy | 0.71 | 0.68 | 0.71 | 0.72 |
| G2 | 10079.12 | 9672.91 | 9439.34 | 9245.93 |
| DF | 4194235 | 4194212 | 4194189 | 4194166 |
AIC = Akaike Information Criteria; BIC = Bayesian Information Criteria; G2 = G-squared; DF = degrees of freedom
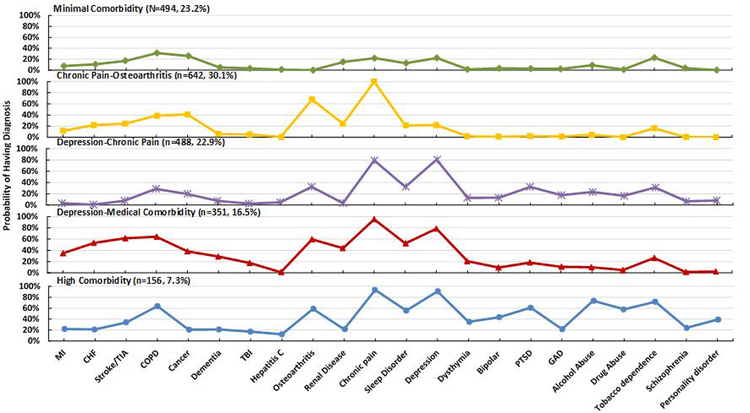
The five classes are described based on clinical characteristics of each comorbidity cluster, and shown in Figure 1 (each class individually displayed). Classes were, from “healthiest” (Minimal Comorbidity) to “most ill” (High Comorbidity) in terms of comorbidity profile, the Minimal Comorbidity Class (n = 494, 23.2% of sample), the Chronic Pain-Osteoarthritis Class (n = 642, 30.1%), the Depression-Chronic Pain Class (n = 488, 22.9%), the Depression-Medical Comorbidity Class (n = 351, 16.5%), and the High Comorbidity Class (n = 156, 7.3%). Numerical information and descriptive characteristics of each class, as well as the sample as a whole, are presented in Table 2.
Figure 1.
Distribution of Comorbidity Types among 5 Clusters
Table 2.
Demographic characteristics of 2,131 Veterans ages 65-years and older by Comorbidity Cluster
| Demographics | Total Sample (N=2,131) |
Minimal Comorbidity N=494 (23.18%) |
Chronic Pain-Osteoarthritis N=642 (30.13%) |
Depression-Chronic Pain N=488 (22.90%) |
Depression-Medical Comorbidity N=351 (16.47%) |
High Comorbidity N=156 (7.32%) | Pa |
|---|---|---|---|---|---|---|---|
| Age, mean (SD) | 74.38 (7.8) | 74.38 (7.5) | 78.91 (7.4) | 69.72 (5.5) | 75.34 (7.6) | 68.05 (3.3) | <.001 |
| Female, n (%)b | 39 (1.8) | 0 (0.0) | 7 (1.1) | 19 (3.9) | 7 (2.0) | 6 (3.9) | <.001 |
| Race | <.001 | ||||||
| Non-Hispanic White | 1,979 (92.9) | 458 (92.7) | 614 (95.6) | 451 (92.4) | 329 (93.7) | 127 (81.4) | |
| Non-Hispanic Black | 97 (4.6) | 24 (4.9) | 13 (2.0) | 24 (4.9) | 14 (4.0) | 22 (14.1) | |
| Hispanic/Other | 55 (2.6) | 12 (2.4) | 15 (2.3) | 13 (2.7) | 8 (2.3) | 7 (4.5) | |
| >25% college-educatedc | 833 (39.1) | 188 (38.1) | 235 (36.6) | 201 (41.2) | 147 (41.9) | 62 (39.7) | .411 |
| Median income tertilec | .766 | ||||||
| Low tertile (<$40,180) | 613 (28.8) | 146 (29.6) | 178 (27.7) | 140 (28.7) | 94 (26.8) | 55 (35.3) | |
| Middle tertile | 711 (33.4) | 161 (32.6) | 220 (34.3) | 163 (33.4) | 117 (33.3) | 50 (32.1) | |
| High tertile (>$52,546) | 807 (37.9) | 187 (37.9) | 244 (38.0) | 185 (37.9) | 140 (39.9) | 51 (32.7) | |
| Marital status | <.001 | ||||||
| Married | 1,087 (51.1) | 232 (47.0) | 378 (58.9) | 221 (45.3) | 204 (58.1) | 52 (33.3) | |
| Divorced/sep/widowed | 573 (26.9) | 131 (26.5) | 129 (20.1) | 174 (35.7) | 71 (20.2) | 68 (43.6) | |
| Never married | 205 (9.7) | 61 (12.4) | 36 (5.6) | 60 (12.3) | 23 (6.6) | 25 (16.0) | |
| Unknown | 266 (12.5) | 70 (14.2) | 99 (15.4) | 33 (6.8) | 53 (15.1) | 11 (7.1) |
P value based on F test for continuous variables and chi-squared test for categorical variables comparing across given clusters.
Values are presented as n (%) unless otherwise indicated
Zip code tabulation area from 2013 census.
The classes were significantly different from each other at p<.001 across multiple demographic and clinical variables (Tables 2 and 3). In terms of age, the Chronic Pain-Osteoarthritis Class had the oldest individuals among the groups (M = 78.91; SD = 7.42) and the High Comorbidity Class the youngest (M = 68.05; SD = 3.33). Regarding gender differences, no female patients were classified into the Minimal Comorbidity Class while the Depression-Chronic Pain Class had the most, at 3.89% of the group. Most classes were made up of predominantly non-Hispanic White individuals (> 92%). However, the High Comorbidity group had the most minority individuals, with 18.6% of individuals identified as African American or Hispanic. In terms of marital status, the Chronic Pain-Osteoarthritis Class had the highest proportion of married individuals (58.9%), and the High Comorbidity Class the lowest (33.3%).
Table 3.
Suicide Behaviors among 2,131 65-years and Older Veterans by Comorbidity Cluster
| Total Sample (N=2,131) |
Minimal Comorbidity N=494 (23.18%) |
Chronic Pain-Osteoarthritis N=642 (30.13%) |
Depression-Chronic Pain N=488 (22.90%) |
Depression-Medical Comorbidity N=351 (16.47%) |
High Comorbidity N=156 (7.32%) | Pa | |
|---|---|---|---|---|---|---|---|
| Last visit to attempt, days, mean (SD) | 76.3 (125.1) |
112.6 (155.8) | 100.5 (133.7) | 42.2 (82.5) | 51.8 (105.8) | 23.0 (50.4) | <.001 |
|
Prior suicidal ideation, n (%)b |
299 (14.0) |
13 (2.6) |
11 (1.7) |
96 (19.7) |
73 (20.8) |
106 (68.0) |
<.001 |
| Fatal attempt | 1,300 (61.0) | 363 (73.4) | 552 (86.0) | 189 (38.7) | 181 (51.6) | 15 (9.6) | <.001 |
| Fatal Suicide Method | |||||||
| Firearms | 1,072 (82.5) | 299 (82.4) | 481 (87.1) | 137 (72.5) | 148 (81.8) | 7 (46.7) | <.001 |
| Hanging | 104 (8.0) | 29 (8.0) | 30 (5.4) | 23 (12.2) | 20 (11.1) | 2 (13.3) | .016 |
| Drug overdose | 50 (3.9) | 10 (2.8) | 17 (3.1) | 14 (7.4) | 6 (3.3) | 3 (20.0) | <.001 |
| Poisoning | 27 (2.1) | 8 (2.2) | 12 (2.2) | 4 (2.1) | 2 (1.1) | 1 (6.7) | .654 |
| Jumping | 12 (1.0) | 4 (1.1) | 2 (0.4) | 6 (3.2) | 0 (0.0) | 0 (0.0) | .006 |
| Others | 35 (2.7) | 13 (3.6) | 10 (1.8) | 5 (2.7) | 5 (2.8) | 2 (13.3) | .056 |
P value based on chi-squared test for categorical variables comparing across given clusters.
Values are presented as n (%) unless otherwise indicated
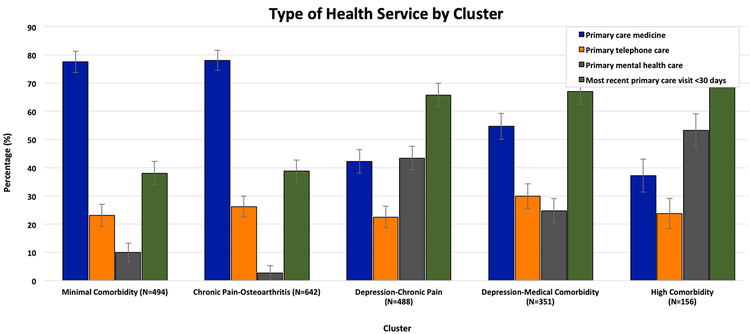
They also differed at p<.001 in utilization, with significant differences in location of last visit (Figure 2). Specifically, the High Comorbidity Class was more likely to have been seen by primary care mental health than all other classes (53.2% of visits, compared to 2.7% of visits with mental health primary care in the Chronic Pain-Osteoarthritis Class). Furthermore, the High Comorbidity class was significantly more likely to have seen a provider <30 days prior to their attempt, compared to all other classes, with the Minimal Comorbidity and Chronic Pain-Osteoarthritis classes averaging 3–4 months between last visit and attempt (see Table 3).
Figure 2.
Type of Health Service Seen in Last Visit by Cluster
The classes further differed in the means and lethality of their suicide attempts. Attempts were fatal in 61% of the sample, with the highest proportion of fatal attempts in the Chronic Pain-Osteoarthritis class (86.0%) and the Minimal Comorbidity class (73.4%), with the lowest in the High Comorbidity class (9.6%). Despite the lower proportion of fatal attempts in the High Comorbidity Class, these individuals were more likely to have prior suicidal ideation documented in their medical record compared to all other classes (at p<.001). Means used in a fatal attempt also differed between classes (Table 3). Most notably, the Minimal Comorbidity, Chronic Pain-Osteoarthritis, and Depression-Medical Comorbidity used firearms in over 80% of fatal attempts, compared to 46.7% of those in the High Comorbidity Class (p<.001). This trend is striking in the sample overall, with 82.5% of all fatal attempts made using firearms.
DISCUSSION
Latent class analysis characterized five distinct comorbidity clusters of older patients who were last seen in primary care before attempting suicide; 1) Minimal Comorbidity (23.2%); 2) Chronic Pain-Osteoarthritis (30.1%); 3) Depression-Chronic Pain (22.9%); 4) Depression-Medical Comorbidity (16.5%); and 5) High Comorbidity (7.3%). These findings were surprising given the literature on late-life suicide – specifically regarding the prevailing belief that those who go on to die by suicide have diagnoses of depression, and attendant idea that screening for depression symptoms is therefore central to identification of those at risk. Further, patients in the High Comorbidity group were most likely to have been seen by mental health in primary care, as well as least likely to have a fatal attempt. Those in the low depression diagnosis groups (Minimal Comorbidity and Chronic Pain-Osteoarthritis) were most likely to attempt fatally, with majority (>80%) using firearms.
As important, the high documentation of previous suicidal ideation for the High Comorbidity group may reflect engagement with mental health providers in addition to medical services through VA, a possible protective factor related to lethality of attempt given significant efforts in VA mental health to address firearm safety and access to lethal means; implementing a safety plan when suicidal ideation is endorsed. Additionally, the fact that this group was most likely to have been seen <30 days prior to their attempt may reflect more consistent engagement with care overall. However, it is also possible that veterans with similarly high rates of psychiatric and medical comorbidity may have been less likely to survive to older age, and may have either passed away or attempted fatally earlier in life. Finally, the finding that 20% of fatal attempters in the High Comorbidity cluster died by overdose may inform greater attention to medication management and prescribing practices for providers across disciplines seeing older veterans with multiple comorbidities.
Surprisingly, over half of suicide attempters in this sample did not have a diagnosis of depression at the time of their attempt. As noted, this is concerning because the approach to risk assessment in most primary care settings is to use presence of depression or mental health treatment to identify potentially suicidal patients23. In fact, the U.S. Preventive Services Task Force concludes that there is insufficient evidence of preventive benefits to recommend suicide screening in primary care above and beyond previous mental health diagnoses and suicide attempts3. They further recommend for limiting access to lethal means among those with previous suicide attempts. Yet, as evidenced in the present study, the high rate of lethal first attempt shows this is too little too late for many older patients.
Indeed, the two classes with minimal depression diagnoses that made up over half of attempters were also significantly more likely to have a fatal attempt than any other group, specifically with a firearm. Overall, over 80% of all fatal attempts in the sample used firearms – with the percentage in the Chronic Pain-Osteoarthritis group nearly 90%. Use of firearms among this population of older veterans is higher than the recent average for veterans and civilians of all ages who took their own lives (over 80% compared to 67.9% and 52.2%, respectively24), with an increase in firearm use across the board since 2001. Given the striking number of completed attempts using firearms and the low rates of other diagnostic factors which would allow for sensitive and specific detection of suicide risk, preventive intervention by way of lethal means safety counseling in primary care may be a logical and necessary next step in attempting to reduce suicide.
Recently, calls to action have been issued by professional medical associations for physicians to speak out about the public health crisis of firearms25–28. At the same time, research has uncovered an imbalance between physician perception of need for patient counseling about firearm safety29 and the current occurrence of follow-up in this area30. Indeed, while most internist respondents believe it is appropriate for physicians to counsel patients about firearm safety, 77% say they have never discussed these issues with a patient30. However, the potential preventive effects of such interventions are promising31, given data to suggest that patients are open to providers discussing firearm safety with them in clinic, particularly if they believe that owning a firearm heightens suicide risk32. Thus, the combination of education about firearms and suicide risk33 and lethal means counseling in primary care may be of greatest benefit to all, including those either with undiagnosed depression or without depressive symptoms who may attempt with a firearm.
Disseminating evidence to providers about the heterogeneous comorbidity profiles of late-life attempters, especially in regards to prevailing ideas that only those with a diagnosis of depression or other psychiatric conditions are at risk of suicide30, is imperative to late-life suicide prevention. The significance of primary care as a point of intervention is enormous. Our findings support this, highlighted by the proportion of late-life attempters without a depression diagnosis and with minimal medical comorbidity who may not regularly see any health care professional other than their primary care provider34. Further, trusted relationships with primary care providers may facilitate conversations about gun safety and restricting access to lethal means with older adults and their families – an intervention which may have the greatest preventive impact35. Lethal means counseling is rarely addressed in primary care30, especially in the absence of a mental health diagnosis. Based on the findings of our study, educating and encouraging primary care providers to discuss firearm safety and lethal means access36 with their patients and patients’ families, even those who may not “appear” to be at risk, is important. These discussions can include the distribution of locks and education for family members and caregivers about the rates of suicide attempt with a firearm among older adults with minimal medical and psychiatric comorbidities. Finally, the necessity of all providers taking responsibility for suicide prevention may assist in preventing first attempts among older patients at risk of falling through the cracks.
The present study has several strengths. It is the first study to characterize comorbidity profiles of late-life suicide attempters last seen in primary care. This study is a necessary and important first step that informs and sets the stage for future research efforts to examine comorbidity profiles in older primary care patients as longitudinal predictors of late-life fatal and non-fatal suicide attempts. Other strengths include linking of diagnostic, utilization and lethality data from a large national sample within an integrated healthcare system. Linking of the SPAN data with other VA data sources adds greatly to the literature on clinical factors proximal to an attempt by providing an exact attempt date as recorded by clinicians, rather than relying on ICD-9 codes of suicide behavior coded at subsequent visits. Further, the strengths of VA interfacing between primary care medicine and mental health, as well as national mandated programs to improve mental health and suicide screening across facilities increases the likelihood that these patients had a better opportunity to be identified as ‘at risk’ by their medical provider compared to non-VA settings. Yet, this would also suggest that in other medical settings older patients falling through the ‘at risk’ cracks is an even more pervasive problem.
This study also has limitations. First, it may not be generalizable to non-veterans, women, and those whose racial backgrounds are not well reflected by the older veteran population. Second, although the final class solution was chosen based on a combination of fit statistics, theoretical interpretability, and parsimony, our findings should be carefully interpreted and confirmed in future research. Third, means of attempt data were only available for suicide decedents, thus limiting the understanding of non-fatal attempts. In addition, previous non-lethal attempts may have been unidentified in the present study due to the lack of available attempt data prior to 2008, and the possibility that previous attempts that were not medically serious may never have been disclosed. Fourth, we did not have information on potentially salient factors such as social support and other psychosocial variables that may relate to suicide behavior. Given potential positive impact of social factors on suicide risk37, assessing for relevant protective factors and developing interventions to bolster these social factors, including partnerships with family and caregivers and community organizations is an important area for future research38.Finally, information was limited on severity of psychiatric (e.g., depression) and medical comorbidities, as well as detailed measures of disability.
CONCLUSION
Distinct comorbidity profiles with different attempt-related characteristics are identifiable among older patients who attempt suicide and are last seen in primary care. The two clusters with relatively few physical and mental health comorbidities, including low rates of depression diagnosis but with high rates of lethal attempt using firearms, may represent individuals less likely to be flagged as high risk. These findings have significant implications for screening and intervention, particularly related to firearm safety counseling in primary care. Education of providers, patients, and the public about high risk of death by suicide using firearms in late life, as well as the development of interventions with clinical, psychosocial and legislative impacts39,40, are vital ways providers across medical and psychiatric specialties can address this public health crisis.
Acknowledgments
Support/Funding: This work was supported by Award Number I01 CX001119 from the Clinical Science Research & Development Service of the U.S. Department of Veterans Affairs (VA) Office of Research and Development (PI: Dr. Byers) and by the VA Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, Sierra Pacific Mental Illness Research Education and Clinic Centers (Dr. Morin). Dr. Whooley is supported by the Measurement Science QUERI, and Dr. Conwell is supported by CDC grant R49 CE002093 (PI: Dr. Caine). Support for the Suicide Data Repository (SDR) and Suicide Prevention Applications Network (SPAN) is provided by the VA Center of Excellence for Suicide Prevention. Support for VA/CMS data is provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02–237 and 98–004).
Sponsor’s Role: The sponsors had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript. Any opinions, findings, conclusions or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the views of the U.S. Government, or the U.S. Department of Veterans Affairs, and no official endorsement should be inferred. Dr. Byers and Ms. Li had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatric Clinics. 2011;34(2):451–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. American Journal of Public Health. 2000;90(12):1885–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LeFevre ML. Screening for suicide risk in adolescents, adults, and older adults in primary care: US Preventive Services Task Force recommendation statement. Annals of internal medicine. 2014;160(10):719–726. [DOI] [PubMed] [Google Scholar]
- 4.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry. 2002;159(6):909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeates C, LJ M, Paul D, et al. Completed Suicide Among Older Patients in Primary Care Practices: A Controlled Study. Journal of the American Geriatrics Society. 2000;48(1):23–29. [DOI] [PubMed] [Google Scholar]
- 6.Fässberg MM, Cheung G, Canetto SS, et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging & mental health. 2016;20(2):166–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeates C, Melanie R, CE D. Completed Suicide at Age 50 and Over. Journal of the American Geriatrics Society. 1990;38(6):640–644. [DOI] [PubMed] [Google Scholar]
- 8.McDowell AK, Lineberry TW, Bostwick JM. Practical Suicide-Risk Management for the Busy Primary Care Physician. Mayo Clinic Proceedings. 2011;86(8):792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung G, Merry S, Sundram F. Late-life suicide: Insight on motives and contributors derived from suicide notes. Journal of affective disorders. 2015;185:17–23. [DOI] [PubMed] [Google Scholar]
- 10.Dobscha SK, Denneson LM, Kovas AE, et al. Correlates of suicide among veterans treated in primary care: Case–control study of a nationally representative sample. Journal of general internal medicine. 2014;29(4):853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCarthy JF, Bossarte RM, Katz IR, et al. Predictive modeling and concentration of the risk of suicide: implications for preventive interventions in the US Department of Veterans Affairs. American journal of public health. 2015;105(9):1935–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. Jama. 2003;289(23):3145–3151. [DOI] [PubMed] [Google Scholar]
- 13.Bossarte RM, Knox KL, Piegari R, Altieri J, Kemp J, Katz IR. Prevalence and characteristics of suicide ideation and attempts among active military and veteran participants in a national health survey. American journal of public health. 2012;102(S1):S38–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kemp J, Bossarte RM. Surveillance of suicide and suicide attempts among veterans: addressing a national imperative. American journal of public health. 2012;102(Suppl 1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmire C, Stephens B, Morley S, Thompson C, Kemp J, Bossarte RM. VA Suicide Prevention Applications Network: A National Health Care System–Based Suicide Event Tracking System. Public Health Reports. 2016;131(6):816–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kemp J, Bossarte R. Suicide data report: 2012 Department of Veterans Affairs, Mental Health Services, Suicide Prevention Program Washington, DC; 2013. [Google Scholar]
- 17.Kazis LE, Ren XS, Lee A, et al. Health Status in VA Patients: Results from the Veterans Health Study. American Journal of Medical Quality. 1999;14(1):28–38. [DOI] [PubMed] [Google Scholar]
- 18.Zivin K, Pfeiffer PN, Szymanski BR, et al. Initiation of Primary Care—Mental Health Integration programs in the VA Health System: Associations with psychiatric diagnoses in primary care. Medical care. 2010:843–851. [DOI] [PubMed] [Google Scholar]
- 19.Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs health care system. Journal of clinical psychology in medical settings. 2008;15(1):73–78. [DOI] [PubMed] [Google Scholar]
- 20.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling. 2007;14(4):535–569. [Google Scholar]
- 21.Ram N, Grimm KJ. Methods and measures: Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International journal of behavioral development. 2009;33(6):565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lanza ST, Dziak JJ, Huang L, Xu S, Collins LM. Proc LCA & Proc LTA users’ guide (Version 1.3. 2) Penn State: University Park, The Methodology Center. 2011. [Google Scholar]
- 23.Rihmer Z, Belsö N, Kalmár S. Antidepressants and suicide prevention in Hungary. Acta Psychiatrica Scandinavica. 2001;103(3):238. [DOI] [PubMed] [Google Scholar]
- 24.Suicide Among Veterans and Other Americans, 2001–2014. 2017; https://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf.
- 25.Laine C, Taichman DB. The health care professional’s pledge: protecting our patients from firearm injury. Annals of internal medicine. 2017;167(12):892–893. [DOI] [PubMed] [Google Scholar]
- 26.Taichman D, Bornstein SS, Laine C. Firearm injury prevention: AFFIRMing that doctors are in our lane. Annals of internal medicine. 2018;169(12):885. [DOI] [PubMed] [Google Scholar]
- 27.Taichman DB, Bauchner H, Drazen JM, Laine C, Peiperl L. Firearm-related injury and death—a US health care crisis in need of health care professionals. Mass Medical Soc; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taichman DB, Laine C. Reducing firearm-related harms: time for us to study and speak out. Annals of internal medicine. 2015;162(7):520–521. [DOI] [PubMed] [Google Scholar]
- 29.Benjamin Wolk C, Van Pelt AE, Jager-Hyman S, et al. Stakeholder perspectives on implementing a firearm safety intervention in pediatric primary care as a universal suicide prevention strategy: A qualitative study. JAMA Network Open. 2018;1(7):e185309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butkus R, Weissman A. Internists’ attitudes toward prevention of firearm injury. Annals of internal medicine. 2014;160(12):821–827. [DOI] [PubMed] [Google Scholar]
- 31.Sarchiapone M, Mandelli L, Iosue M, Andrisano C, Roy A. Controlling access to suicide means. International journal of environmental research and public health. 2011;8(12):4550–4562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Betz ME, Azrael D, Barber C, Miller M. Public opinion regarding whether speaking with patients about firearms is appropriate: results of a national survey. Annals of internal medicine. 2016;165(8):543–550. [DOI] [PubMed] [Google Scholar]
- 33.Miller M, Hemenway D. Guns and suicide in the United States. New England Journal of Medicine. 2008;359(10):989–991. [DOI] [PubMed] [Google Scholar]
- 34.Simon GE, Johnson E, Lawrence JM, et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. American Journal of Psychiatry. 2018;175(10):951–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. Jama. 2005;294(16):2064–2074. [DOI] [PubMed] [Google Scholar]
- 36.Florentine JB, Crane C. Suicide prevention by limiting access to methods: a review of theory and practice. Social science & medicine. 2010;70(10):1626–1632. [DOI] [PubMed] [Google Scholar]
- 37.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr. The interpersonal theory of suicide. Psychological review. 2010;117(2):575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Orden KA, Stone DM, Rowe J, McIntosh WL, Podgorski C, Conwell Y. The Senior Connection: Design and rationale of a randomized trial of peer companionship to reduce suicide risk in later life. Contemporary Clinical Trials. 2013;35(1):117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anestis MD, Anestis JC, Butterworth SE. Handgun legislation and changes in statewide overall suicide rates. American journal of public health. 2017;107(4):579–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weinberger SE, Hoyt DB, Lawrence HC, et al. Firearm-related injury and death in the United States: a call to action from 8 health professional organizations and the American Bar Association. Annals of internal medicine. 2015; 162(7):513–516. [DOI] [PubMed] [Google Scholar]