Abstract
Background
Improving postoperative recovery is important, with a national focus on postacute care, but the volume and quality of evidence in this area are not well characterized. We conducted a systematic review to characterize studies on postoperative recovery after adult cardiac surgery using patient‐reported outcome measures.
Methods and Results
From MEDLINE and Web of Science, studies were included if they prospectively assessed postoperative recovery on adult patients undergoing cardiac surgery using patient‐reported outcome measures. Six recovery domains were defined by prior literature: nociceptive symptoms, mental health, physical function, activities of daily living, sleep, and cognitive function. Of the 3432 studies, 105 articles met the inclusion criteria. The studies were small (median sample size, 119), and mostly conducted in single‐center settings (n=81; 77%). Study participants were predominantly men (71%) and white (88%). Coronary artery bypass graft was included in 93% (n=98). Studies commonly selected for elective cases (n=56; 53%) and patients with less comorbidity (n=67; 64%). Median follow‐up duration was 91 (interquartile range, 42–182) days. Studies most commonly assessed 1 domain (n=42; 40%). The studies also varied in the instruments used and differed in their reporting approach. Studies commonly excluded patients who died during the follow‐up period (n=48; 46%), and 45% (n=47) did not specify how those patients were analyzed.
Conclusions
Studies of postoperative patient‐reported outcome measures are low in volume, most often single site without external validation, varied in their approach to missing data, and narrow in the domains and diversity of patients. The evidence base for postoperative patient‐reported outcome measures needs to be strengthened.
Keywords: recovery, surgery, systematic review
Subject Categories: Cardiovascular Surgery, Quality and Outcomes
Clinical Perspective
What Is New?
This systematic review identified that studies of postoperative patient‐reported outcomes are low in volume, narrow in domains and diversity of patients, and varied significantly in instruments used and ways in which outcomes were reported.
What Are the Clinical Implications?
For efforts to improve postoperative recovery to be data‐driven, study methodology must be standardized and improve in its rigor.
Introduction
Postoperative recovery is a complex, time‐dependent process with multiple relevant domains, including physiological, nociceptive, mental health, cognitive, sleep, mobility, and activities of daily living.1, 2, 3 Understanding postoperative recovery after cardiac surgery is pertinent, as there is increasing emphasis on readmission and outcomes of postacute care, with implementation of national publicly reported measures and incentive systems, such as bundled payments and the Hospital Readmissions Reduction Program.4, 5 There are increasing calls for the use of patient‐reported outcome measures (PROMs) to improve recovery, as well as digital health tools to assess function and activity.3, 6 In fact, the Centers for Medicare and Medicaid Services is now paying for such remote monitoring.7 However, the quality and volume of the evidence base guiding this effort in the cardiac surgery population are unknown.
To inform strategies to study and improve postoperative recovery, it is important to systematically evaluate the volume, quality, and content of existing literature. Of particular interest is the use of standardized methods to assess various domains relevant to recovery and inclusion of diverse patient populations. Additionally, characterizing approaches to reporting PROM scores is important, as variable reporting of raw measured scores, relative change from the preoperative measurements, or other ways may impede generalizable synthesis of the literature. However, to date, there is no extensive review of the magnitude and quality of the studies, how prior studies have used PROM instruments, and what patient populations are being studied.
Accordingly, we performed a systematic review to (1) describe the methods used in existing studies that evaluated postoperative recovery after cardiac surgery using PROMs and (2) assess the populations studied. The findings will help prioritize future research by identifying areas of postoperative recovery that currently lack data.
Methods
The data that support the findings of this study are available from the first author (makoto.mori@yale.edu) upon reasonable request.
Search Strategy and Study Selection
We developed the protocol according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement.8 To identify prospective studies on the cardiac surgical population that evaluated postoperative recovery using PROMs, publications were searched on Medline and Web of Science using a combination of key terms and index headings related to cardiac surgery and postoperative recovery. We consulted a librarian experienced in systematic review on methodology and refining search terms. We did not include specific PROM terms or domain terms to increase the search sensitivity. We reviewed all publications indexed through January 10, 2019. The list of MeSH terms (permutations of “postoperative,” “cardiac surgery,” and “recovery”) and other search strategies are outlined in Data S1. We reviewed search results to confirm inclusion of 5 validation articles9, 10, 11, 12, 13, 14 that we identified before the search.
We included only prospective studies in adult patients (age 18 years or older) who underwent any type of cardiac surgery that reported any PROMs following surgery. We excluded case reports and review articles. We excluded studies including patients who underwent left ventricular assist device implantation, extracorporeal membrane oxygenation support, orthotopic heart transplant, and congenital or adult congenital patients, as these populations likely experience distinct recovery trajectories different from the majority of adult cardiac surgical populations, which are those undergoing coronary artery bypass grafting (CABG) and valve and aortic operations. We also excluded studies with follow‐up durations of fewer than 4 postoperative days, as the aim of this study was to characterize the recovery beyond the acute phase of care. To focus on studies evaluating patient‐centered recovery, we excluded studies not reporting PROMs, with the exception of studies measuring physical function using accelerometers. Additionally, studies measuring PROMs at unspecified time points were not included. We added this criterion to exclude studies that obtained PROMs at undefined time points from the index operation, which can have a considerable time range and is challenging to interpret considering the time‐dependent nature of recovery.
Screening and Data Collection
We organized the articles using Endnote 8 (Clarivate Analytics, Philadelphia, PA), and 2 authors (MM and SA) screened the titles and abstracts of all search results to locate potentially eligible articles for full‐text review. Both authors then reviewed the full text to identify the final list of eligible articles, and all disagreements were resolved by consensus.
Data Extraction
For each article, we recorded publication characteristics (first author, year of publication, and journal), study characteristics (instruments used to evaluate recovery, such as the 36‐Item Short Form Health Survey [SF‐36],15 Quality of Recovery score,16 or battery of neurocognitive tests; number of assessments performed; longest time of patient follow‐up; timing of each follow‐up in terms of days since the operation; the domains of recovery evaluated; inclusion/exclusion criteria; enrollment approach; missing data treatment; and how death during the follow‐up was analyzed), and patient characteristics (age, sex, race, number of patients in the study, and cardiac surgery type). Patient follow‐up duration was defined as the duration between the operation and the time when the latest PROM recording was obtained. Values for the timing of measurement were collected in days since the operation. To assign a numeric value for visual representation of when the measurements were taken, the timing of measurements obtained at hospital discharge was defaulted to postoperative day 7, if the study did not report specific timing of postoperative discharge. Day 7 was chosen on the basis of the mean postoperative length of stay of 6.9 days reported by the national Society of Thoracic Surgeons database for patients undergoing isolated CABG.17 Journal type was grouped into 6 categories: nursing, surgical, psychology/behavioral, anesthesia, cardiology, and other. We categorized journals on the basis of the journal title including the name of the specialty (eg, anesthesiology, nursing) and professional society's affiliations to the journal (Table S1).
PROM Domains
Six domains that characterize postoperative recovery were identified on the basis of a previous literature review3: Nociceptive symptoms, physical function, activities of daily living, sleep, cognitive function, and mental health domains. Depression, anxiety, and psychosocial function were categorized into the mental health domain. The nociceptive symptoms domain included reporting of pain, physical discomfort, shortness of breath, and nausea. The physical function domain included measurement obtained using either objective tools, such as accelerometer, or PROMs. This criterion was set to avoid excluding studies that used a more rigorous tool to measure the domains. Similarly, studies using polysomnography for sleep were included to capture studies on postoperative sleep pattern, although polysomnography is likely not applicable for clinical home monitoring.
Definition of Outcomes Reporting Methodology
To evaluate how PROM values are analyzed and reported, we categorized reportings into the following 7 categories: raw score, percentage of patients with or without symptoms or dysfunction (according to each study's definition of categorizations), difference from baseline values, percentage of patients achieving baseline values, frequency of symptoms, fitting a model over raw scores, and others. To the best of our knowledge, there is no existing categorization of PROM reporting for the postoperative period. Therefore, we identified common reporting patterns by (1) reviewing the reporting of all included studies, (2) defining major categories, and (3) conducting a second review to categorize the studies by reporting approaches. Raw score indicates reporting of mean/median value of the PROM score obtained at a given time point and represents the simplest form of reporting. All other reporting categories involve processing of the raw score, such as calculating relative changes from baseline, or proportion of the patients reaching the baseline value at given time points.
Patient Characteristics, Enrollment Approach, and Inclusion/Exclusion Criteria
We then evaluated demographic data, enrollment approach, and inclusion/exclusion criteria to characterize the breadth of patient populations studied. Enrollment approach was categorized into convenience sampling, consecutive enrollment, or unspecified. Inclusion and exclusion criteria of interests were those specifically outlining age, sex, comorbidity criteria, and whether studies excluded patients on the basis of case acuity status (elective versus nonelective).
Treatment of Death and Missing Data
Finally, we evaluated how patients who died during the follow‐up period were treated in the analysis, to understand common analytical practice and existing knowledge of the recovery process before death. To characterize potential bias attributable to missing data, we recorded how missing data were being handled because in longitudinal studies with decline in study participation over time, the population retained to the completion of the study may represent a biased cohort.18
Analysis
Studies were summarized using descriptive statistics by the sample size, procedure types, duration and timing of follow‐up, number of measurements obtained, and the number of domains evaluated. Each variable was summarized either by the percentage or by the median, interquartile range, and range. Distributions of the studies in each component were summarized in a bubble plot. The most frequently used PROM instruments were selected to visualize the timing in days from operation and frequency of measurements obtained.
Results
Selected Studies
The search criteria yielded 3432 studies that potentially addressed postoperative recovery after cardiac surgery. Title and abstract screening excluded 3267 studies. Common reasons for exclusion included studies addressing the congenital heart disease population, animal studies, and studies not assessing PROMs. The remaining 165 potentially eligible articles underwent full‐text review. This process excluded an additional 60 studies, consisting of studies with measures obtained at inconsistent time points, studies without full text, follow‐up duration <4 days, and those evaluating the same study sample used in other included publications. Finally, 105 articles were included for analyses (Figure 1).
Figure 1.
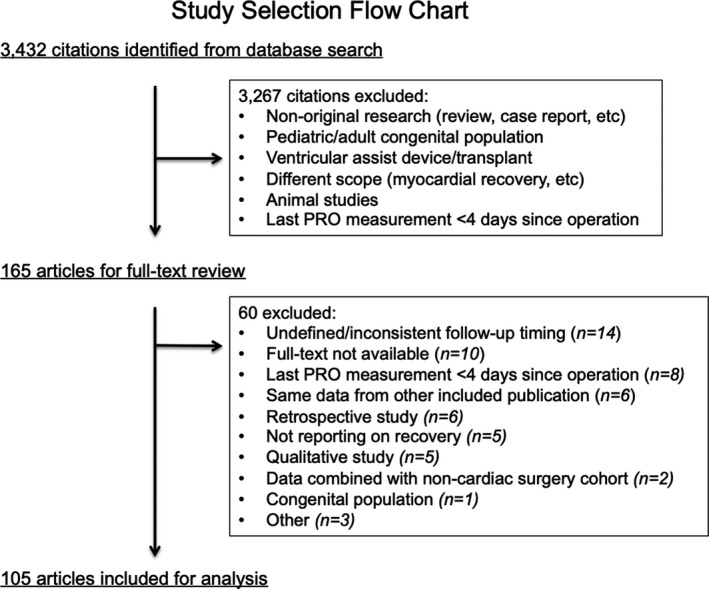
Study selection flow chart. Study selection process to arrive at the 110 articles analyzed. Studies were excluded on the basis of case types (ventricular assist device or heart transplant) and patient population (congenital, adult congenital) because the course of recovery may differ in these populations compared with common adult cardiac surgical population. PRO indicates patient‐reported outcomes.
Study Characteristics
For the 105 included articles, the sample size of the studies tended to be small with a median of 119 patients (interquartile range, 62–229; range, 14–7321). Thirty‐five percent (n=37) of the studies were intervention‐based, comparing recovery between the specific intervention and control groups. Twenty‐five percent of the studies (n=26) were randomized controlled clinical trials, in all of which the interventions were hypothesized to improve recovery, including less invasive surgical approach19 and the use of special undergarments for women's incisional discomfort.20 Seventy‐seven percent (n=81) were conducted in single‐center settings. Median follow‐up duration was 91 (interquartile range, 42–182) days. Frequent follow‐ups (measurements at ≥5 time points) were obtained in 15% (n=15). Studies most commonly assessed 1 domain (n=42; 40%). The nociceptive symptom domain was the most commonly measured (n=60; 57%), followed by the mental health (n=58; 55%) domain. One study that met the inclusion criteria evaluated postoperative taste change,21 which did not meet any of our prespecified domain categories (Table 1). Of note, studies with the largest sample size (N=7321) evaluated only 1 domain, with 1 study having only 2 follow‐ups,22 while another had 7 follow‐ups but spanned only 7 days (Study 17; Table S2).
Table 1.
Study Characteristics of 105 Studies
| Variables | N or Median | % or Q1–Q3 (range) |
|---|---|---|
| Sample size (n) | 119 | 62–29 (14–7321) |
| Randomized trial | 26 | 25% |
| Intervention‐baseda | 37 | 35% |
| Multicenter study | 24 | 23% |
| Follow‐up duration (d) | 91 | 42–182 (4–1825) |
| Number of follow‐ups | ||
| 1 | 7 | 7% |
| 2 | 27 | 26% |
| 3 | 35 | 33% |
| 4 | 21 | 20% |
| 5 | 7 | 7% |
| 6–9 | 8 | 8% |
| Domains | ||
| Nociceptive symptoms | 60 | 57% |
| Activities of daily living | 51 | 49% |
| Cognitive | 18 | 17% |
| Mental health | 58 | 55% |
| Physical function | 55 | 52% |
| Sleep | 11 | 10% |
| Number of domains assessed | ||
| 1 | 42 | 40% |
| 2 | 14 | 13% |
| 3 | 17 | 16% |
| 4 | 23 | 22% |
| 5 | 8 | 8% |
| 6 | 0 | 0% |
IQR indicates interquartile range.
Intervention‐based refers to studies that examined patient‐reported outcome measures according to different process of care (robotic vs. sternotomy approach, telehealth follow‐up vs. usual care, etc.).
Studies were most commonly published in nursing journals (n=30; 30%), followed by surgical journals (n=25; 24%) (Table S3). The oldest study was published in 1980, and 88% and 40% of the included studies were published after 2000 and 2010, respectively (Figure S1).
Reporting Methodology
Of the 105 studies, 71 (68%) reported only the raw scores obtained from measurement tools. Fourteen (13%) defined presence of symptoms or dysfunction in a binary form and reported proportion of patients experiencing the symptoms or dysfunction at each time point. Ten (10%) studies reported measurement values in relation to the baseline values, either as the absolute or relative difference or proportion of patients achieving the baseline value at each measured time points (Table 2). Only 60 (57%) studies obtained the first measurement before the operation (Figure 2).
Table 2.
Outcomes Reporting Methodology
| Reporting Methods | N (%) |
|---|---|
| Raw score valuesa | 71 (68) |
| Percentage of patients with and without symptoms/dysfunction | 14 (13) |
| Difference from baseline | 6 (6) |
| Percentage of patients achieving baseline | 4 (4) |
| Function‐based (fit over raw score values) | 4 (4) |
| Frequency of symptom | 3 (3) |
| Other | 3 (3) |
Raw score values include 1 study reporting number of steps measured by a tracker.
Figure 2.
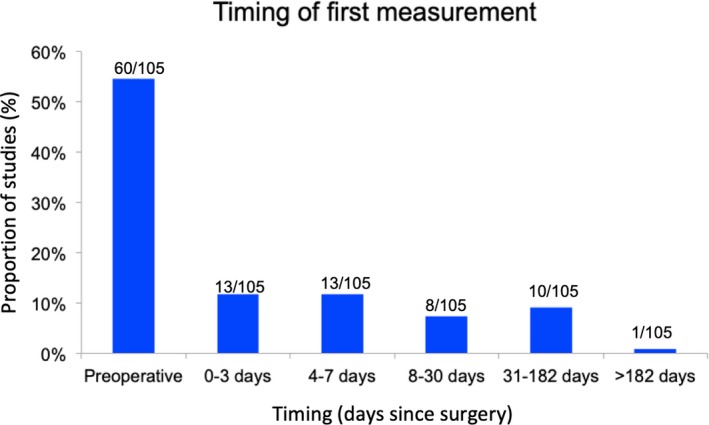
Timing of the first measurement obtained. Distribution of the timing of first measurement reported by the studies. Fifty‐seven percent of the studies obtained the first measurement before surgery.
Most of the studies with 1 to 2 follow‐up assessments examined duration of <30 days. Three studies reported 5 measurements within a 50‐day period,11, 13, 23 representing the highest temporal resolution (Figure 3 and Figure S2).
Figure 3.
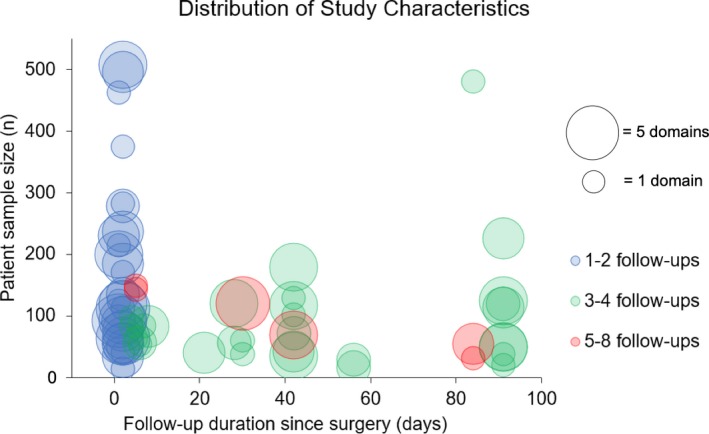
Bubble chart of studies by the study characteristics. Studies by the duration of follow‐up (x axis) up to 100 days, sample size (y axis) up to 500 patients, number of domains evaluated (bubble size), and number of follow‐ups at which time the measurements were obtained (color). Six possible domains are: nociceptive symptoms, activities of daily living, cognitive, sleep, mental health, and physical function.
Figure 4 summarizes the measurement timing and frequencies by the studies using the SF‐36,10, 13, 14, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 which was the most commonly used tool among the studies analyzed. Among the studies using the SF‐36, the total number of measurements obtained ranged from 1 to 6, with highly variable timing of measurements among the studies. Preoperative, 42 days (6 weeks), 91 days (3 months), and 182 days (6 months) after surgery were common time points to obtain the measurement.
Figure 4.
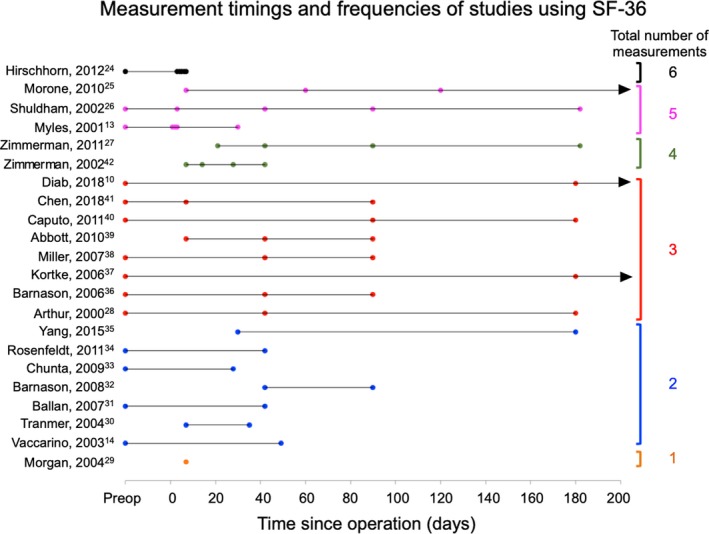
Measurement timings and frequencies of studies using the 36‐Item Short‐Form Health Survey (SF‐36). Each horizontal line represents a study, and each dot represents the time point at which measurements were obtained. Last name of the first author and publication years are displayed in the left column. Studies are clustered by the total number of measurements obtained during the study (right column). Arrows indicate follow‐up >200 days.
Patient Characteristics, Selection Criteria, and Missing Values
Of the 100 studies that reported sex, men represented 71% (n=27,308) of the patients. Only 26% (n=27) of the studies reported race, and of those that reported race, white race comprised 88% (n=4852). The most common procedure type evaluated was isolated or concomitant CABG only (n=60; 57%), followed by studies including both CABGs and other non‐CABG procedures (n=38; 36%); studies focusing solely on valve surgery cohort comprised 6% of the studies (n=6). Studies commonly excluded patients who died during the follow‐up period (46%) and 45% did not specified how people who died were analyzed (Table 3). Only one study evaluated recovery in relation to mortality as an outcome.22
Table 3.
Study Population Characteristics
| Criteria | N (%) |
|---|---|
| Sex reported | 100 (95) |
| Male (of sex reported) | 27 308/38 567 (71) |
| Race reported | 27 (26) |
| White (of race reported) | 4852/5509 (88) |
| Procedure type | |
| CABG only | 60 (57) |
| CABG+other | 38 (36) |
| Valve only | 6 (6) |
| Other | 1 (1) |
| Death treatment | |
| Unspecified | 47 (45) |
| Excluded | 48 (46) |
| No death occurred | 7 (7) |
| Other | 3 (3) |
| Enrollment approach | |
| Unspecified | 55 (52) |
| Convenience | 19 (18) |
| Consecutive | 31 (30) |
| Inclusion/exclusion criteria to select for | |
| Elective case only | 56 (53) |
| Nonelective case only | 0 (0) |
| Less comorbidity | 67 (64) |
| More comorbidity | 4 (4) |
| Older age (>60 years old) | 10 (10) |
| Younger age (<80 years old) | 10 (10) |
| Female sex only | 5 (5) |
Total N is 105, except for male and white numbers, which are specified in the table. Older and younger ages were defined by different thresholds to identify studies that focused on extremes of patient age (ie, “older” referred to the exclusion of extremely young population and vice versa). CABG indicates coronary artery bypass grafting.
Over half of the studies did not specify whether enrollment was consecutive or on a convenience basis. Studies commonly set criteria to select for elective cases (53%) and patients with less comorbidity (64%). Ten percent of the studies set criteria to select for an older patient population (age ≥60 years), and 5% of the studies specified inclusion of women only (Table 3).
Study Findings
The variability in methodologies used across studies precluded synthesis of the existing evidence. Therefore, we summarized interventions and clinical characteristics associated with postoperative recovery that studies identified (Table S4), although interpretation of such claims is difficult in the context of limited quality of studies included in this analysis.
Discussion
In this systematic review, we identified that the body of literature on postoperative recovery after cardiac surgery is small (105 studies) and limited in quality, mostly single‐center studies focusing on narrow diversity of patients. Patients studied were predominantly men, and of 26% of the studies reporting race, 88% were white. Measurement and reporting methods varied widely among the studies, with no standardized use of instruments. Although studies reported predictors of recovery, most lacked external validation, were low in quality, and limited in breadths of the population studied. A significant implication of our findings is in highlighting the need for high‐quality research using a standardized approach so that recovery can be measured and improved on evidence‐based fashion, especially with the current focus on the postacute phase of care.
This review has marked implications to researchers and funding bodies, as it revealed how limited the evidence on postoperative recovery is when significant interest exists in readmission reduction and improving the quality of postacute care. The Centers for Medicare and Medicaid Services is developing PROMs as part of its Quality Payment Program to relate patient experience to hospital reimbursement.43 This signals the need for the science behind measuring the patient experience to catch up to the practice, and that need is not being fulfilled by current literature. A major implication to clinicians is that interventions to optimize postoperative recovery are based on little evidence at this point, and drawing clinical guidance on this topic from the literature is challenging.
Measurement Methodologies
Significant heterogeneity and methodological weaknesses were noted in the duration of follow‐ups, the frequency of measurement, tools used to assess recovery, and the domains that were assessed. Even among 22 studies using the same SF‐36 instrument, there was a high variation in when, in relation to the time of surgery, and how frequently the assessments were obtained. Because such variation complicates interpretation of the results across studies, a priority area in studying postoperative recovery may be to identify the standard approach to measurement frequency and timings. In addition, although accounting for individual variations in preoperative level of measurement may be important to contextualize postoperative recovery, measurement of preoperative values was inconsistent, with only 57% of the studies performing preoperative measurement. Furthermore, the review highlighted the low temporal granularity in measurement, with 8 and 9 being the highest numbers of measurements obtained over a relatively long period of 6 months12 to 1 year.44 Because digital platforms may allow for a high‐frequency measurement of PROM, as frequent as on a daily basis,45 leveraging such technology provides novel opportunities to obtain granular insights into the process of recovery.
Reporting Methodologies
Reporting of PROMs varied across studies, representing another element that requires standardization to promote cohesive interpretation of the evidence. A majority of the studies (67%) reported results as raw scores, often as the group‐level mean or median and standard deviations, without any further processing of the score. Other studies sought to provide more clinically intuitive values, such as the proportion of patients reaching the preoperative values in the measured domains or items.9, 10 Defining the recovery as the time that one reaches preoperative level of function in each of global domains3, 9 may be useful in the clinical setting in providing an estimate of the time it takes for a certain proportion of the cohort to achieve “recovery.” However, this approach to reporting may not be as useful in assessing domains that do not have a clear improving or declining trajectory, such as the mental health domain,10 and is also not possible when the preoperative (baseline) values are not measured. Additionally, the binary categorization of the scores limits the interpretation of recovery to that at the group level and obscures distributional properties, such as the standard deviation, of the raw scores. Furthermore, improvement of scores beyond baseline are not reflected in this reporting.
Raw scores measured via instruments calibrated to certain population‐based distributions may be difficult to interpret in a highly selective cohort, such as those recovering after cardiac surgery, because the clinical characteristics of specific subpopulations may not match that of the population from which the calibration was obtained. The SF‐36 score was linearly transformed to have a mean score of 50 and SD of 10,46 and has been validated by the original authors across 24 patient populations with variable sociodemographic characteristics and disease severity.47 However, whether this norm holds true in a highly specific subpopulation, such as a postoperative cohort after high‐acuity operations recovering from a critical care setting, is uncertain. Taken together, standardization of reporting is needed, which may entail reporting of both raw scores obtained by the instruments and any postprocessing of the scores if they provide additional interpretive advantages.
Underrepresented Population
We identified underrepresented populations in this review. As the vast majority of the studies (92%) selected for CABG or a mixture of CABG and other operations, existing data on postoperative recovery after non‐CABG operations are limited. Only 6 studies exclusively evaluated valve operations. Because the mortality and complication incidences vary across case types,48 the process of recovery is expected to also vary and likely represents an important area of investigation. Expectedly, nonwhite and female patients were underrepresented, but more importantly, only 26% of the studies reported race data. The recovery process is reported to be more protracted in female patients,14 and racial differences in recovery and the underlying causes likely warrant investigation. Most studies excluded or did not specify the treatment of mortality that occurred during the follow‐up. While exclusion may be a practical approach to handling missing data, excluding deceased patients leaves the trajectory or recovery before death unknown. Similarly, a large number of studies excluded patients undergoing nonelective procedures with higher comorbidity levels and enrolled patients on a convenience basis. Although such approaches may improve response rates, they obscure the recovery process of sicker patients. Measuring recovery of this population requires patient engagement and creatively devising ways to simplify patient response.
Design and Domain
The use of an objective mobility tracker device in this population was infrequent (3 studies). As the prognostic value of objectively measured mobility has been demonstrated in oncologic49 and noncardiac surgical populations,6 it may be an important aspect of global recovery assessment. Sleep and cognitive domains represented the least frequently assessed domains, although both domains undergo significant disturbances postoperatively.50, 51 This relative infrequency may be attributable to the challenge related to resource‐intensive cognitive function testing and polysomnography being the gold standards.52 To generate evidence in a large cohort representing a wide spectrum of patient populations, the use of subjective surrogate measures, such as self‐perceived sleep quality and duration, may be a practical alternative.
Limitations
This systematic review should be interpreted in the context of several potential limitations. First, the analysis was dependent on the available published data and is limited by publication bias and applicability of historical publications to contemporary clinical and research practice. However, we evaluated the temporal trend in the publication of included studies to assess contemporariness and found that almost 90% of the eligible studies were published after the year 2000. Second, although we worked with an experienced librarian to define the inclusive search terms and searched 2 large databases, it is possible that relevant studies may not have been identified. Third, the heterogeneity of studies in methodology and reporting precluded meta‐analysis. We reported a qualitative summary of the studies in the form of predictors of recovery reported. Fourth, although a systematic review typically includes a risk‐of‐bias assessment, this study focused on the synthesis of meta‐data of broad types of studies, and the heterogeneity of study types precluded systematic assessment of risk of bias applicable to all studies. As the main aim of the study was to describe the characteristics of all existing studies on this topic, we believe the metrics we used to characterize the studies provide a unified view of existing literature.
Conclusions
Our systematic review on postoperative, patient‐centered outcomes after adult cardiac surgery revealed that studies are limited in what they assess, most often single site without external validation, varied in their approach to missing data, and narrow in terms of the diversity of patients. The evidence base regarding postoperative patient‐centered outcomes needs to be strengthened to guide data‐driven improvement of postoperative recovery. Priority areas include augmenting the volume and quality of studies, improving and standardizing the methods and PROM instruments, and focused recruitment of minority populations.
Sources of Funding
This publication was made possible by the Yale Clinical and Translational Science Award, grant UL1TR001863, from the National Center for Advancing Translational Science, a component of the National Institutes of Health.
Disclosures
Dr Suter receives salary support from a contract to develop, implement, and maintain hospital performance outcome measures with the Centers for Medicare and Medicaid Services. Dr Chaudhry serves as a paid consultant for the CVS Caremark State of Connecticut Clinical Pharmacy Program. In the past 36 months, Dr Wallach has received research support through the Meta Research Innovation Center at Stanford and the Collaboration for Research Integrity and Transparency at Yale, which are funded by the Laura and John Arnold Foundation. Dr Krumholz works under contract with the Centers for Medicare and Medicaid Services to support quality measurement programs; was a recipient of a research grant, through Yale, from Medtronic and the US Food and Drug Administration to develop methods for postmarket surveillance of medical devices; was a recipient of a research grant with Medtronic; and is the recipient of a research grant from Johnson & Johnson, through Yale University, to support clinical trial data sharing; was a recipient of a research agreement, through Yale University, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion; collaborates with the National Center for Cardiovascular Diseases in Beijing; receives payment from the Arnold & Porter Law Firm for work related to the Sanofi clopidogrel litigation, from the Ben C. Martin Law Firm for work related to the Cook IVC filter litigation, and from the Siegfried and Jensen Law Firm for work related to Vioxx litigation; chairs a Cardiac Scientific Advisory Board for UnitedHealth; was a participant/participant representative of the IBM Watson Health Life Sciences Board; is a member of the Advisory Board for Element Science, the Advisory Board for Facebook, and the Physician Advisory Board for Aetna; and is the founder of HugoHealth, a personal health information platform, and cofounder of Refactor Health, an enterprise healthcare AI‐augmented data management company.
Supporting information
Data S1. Search Terms.
Table S1. Journal Categorization by Specialty
Table S2. List of Included Studies
Table S3. Number of Articles by Journal Category
Table S4. Qualitative Summary of Predictors and Interventions Associated With Improved Recovery
Figure S1. Number of publications by year. Number of articles published by 5‐year increment of calendar year. No publication published before 1980 met the inclusion criteria. The latest bin (2015–2018) includes only a 4‐year period.
Figure S2. Bubble chart of studies by the study characteristics up to 400 follow‐up days. Studies by the duration of follow‐up (x axis) up to 400 days, sample size (y axis) up to 600 patients, number of domains evaluated (bubble size), and number of follow‐ups at which time the measurements were obtained (color). Six possible domains are: nociceptive symptoms, activities of daily living, cognitive, sleep, mental health, and physical function.
Acknowledgments
We thank Alexandria Brackett, MA, MLIS, a librarian at Harvey Cushing/John Hay Whitney Medical Library at Yale School of Medicine for her assistance on refining literature search strategies and search terms.
(J Am Heart Assoc. 2019;8:e013546 DOI: 10.1161/JAHA.119.013546.)
References
- 1. Moore FD. Getting well: the biology of surgical convalescence. Ann N Y Acad Sci. 1958;73:387–400. [DOI] [PubMed] [Google Scholar]
- 2. Lee L, Tran T, Mayo NE, Carli F, Feldman LS. What does it really mean to “recover” from an operation? Surgery. 2014;155:211–216. [DOI] [PubMed] [Google Scholar]
- 3. Bowyer AJ, Royse CF. Postoperative recovery and outcomes—what are we measuring and for whom? Anaesthesia. 2016;71(suppl 1):72–77. [DOI] [PubMed] [Google Scholar]
- 4. Wadhera RK, Yeh RW, Joynt Maddox KE. The rise and fall of mandatory cardiac bundled payments. JAMA. 2018;319:335–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khera R, Dharmarajan K, Wang Y, Lin Z, Bernheim SM, Normand ST, Krumholz HM. Association of the hospital readmissions reduction program with mortality during and after hospitalization for acute myocardial infarction, heart failure, and pneumonia. JAMA Netw Open. 2018;1:e182777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daskivich TJ, Houman J, Lopez M, Luu M, Fleshner P, Zaghiyan K, Cunneen S, Burch M, Walsh C, Paiement G, Kremen T, Soukiasian H, Spitzer A, Jackson T, Kim HL, Li A, Spiegel B. Association of wearable activity monitors with assessment of daily ambulation and length of stay among patients undergoing major surgery. JAMA Netw Open. 2019;2:e187673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Medicare and Medicaid Services . Telehealth services. Available at: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf. Accessed March 3, 2019.
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG and Group P . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Royse CF, Saager L, Whitlock R, Ou‐Young J, Royse A, Vincent J, Devereaux PJ, Kurz A, Awais A, Panjasawatwong K, Sessler DI. Impact of methylprednisolone on postoperative quality of recovery and delirium in the steroids in cardiac surgery trial: a randomized, double‐blind. Placebo‐controlled substudy. Anesthesiology. 2017;126:223–233. [DOI] [PubMed] [Google Scholar]
- 10. Diab MS, Bilkhu R, Soppa G, Edsell M, Fletcher N, Heiberg J, Royse C, Jahangiri M. The influence of prolonged intensive care stay on quality of life, recovery, and clinical outcomes following cardiac surgery: a prospective cohort study. J Thorac Cardiovasc Surg. 2018;156:1906–1915.e3. [DOI] [PubMed] [Google Scholar]
- 11. Bowyer AJ, Heiberg J, Sessler DI, Newman S, Royse AG, Royse CF. Validation of the cognitive recovery assessments with the Postoperative Quality of Recovery Scale in patients with low‐baseline cognition. Anaesthesia. 2018;73:1382–1391. [DOI] [PubMed] [Google Scholar]
- 12. Petersen J, Vettorazzi E, Winter L, Schmied W, Kindermann I, Schäfers HJ. Physical and mental recovery after conventional aortic valve surgery. J Thorac Cardiovasc Surg. 2016;152:1549–1556.e2 [DOI] [PubMed] [Google Scholar]
- 13. Myles PS, Hunt JO, Fletcher H, Solly R, Woodward D, Kelly S. Relation between quality of recovery in hospital and quality of life at 3 months after cardiac surgery. Anesthesiology. 2001;95:862–867. [DOI] [PubMed] [Google Scholar]
- 14. Vaccarino V, Lin ZQ, Kasl SV, Mattera JA, Roumanis SA, Abramson JL, Krumholz HM. Gender differences in recovery after coronary artery bypass surgery. J Am Coll Cardiol. 2003;41:307–314. [DOI] [PubMed] [Google Scholar]
- 15. Ware JE, Sherbourne CD. The MOS 36‐Item Short‐Form Health Survey (SF‐36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 16. Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative quality of recovery score: the QoR‐40. Br J Anaesth. 2000;84:11–15. [DOI] [PubMed] [Google Scholar]
- 17. Badhwar V, Rankin JS, Thourani VH, D'Agostino RS, Habib RH, Shahian DM, Jacobs JP. The society of thoracic surgeons adult cardiac surgery database: 2018 update on research: outcomes analysis, quality improvement, and patient safety. Ann Thorac Surg. 2018;106:8–13. [DOI] [PubMed] [Google Scholar]
- 18. Heilbrun LK, Nomura A, Stemmermann GN. The effects of non‐response in a prospective study of cancer: 15‐year follow‐up. Int J Epidemiol. 1991;20:328–338. [DOI] [PubMed] [Google Scholar]
- 19. Grossi EA, Zakow PK, Ribakove G, Kallenbach K, Ursomanno P, Gradek CE, Baumann FG, Colvin SB, Galloway AC. Comparison of post‐operative pain, stress response, and quality of life in port access vs. standard sternotomy coronary bypass patients. Eur J Cardiothorac Surg. 1999;16(suppl 2):S39–S42. [PubMed] [Google Scholar]
- 20. King KM, Tsuyuki R, Faris P, Currie G, Maitland A, Collins‐Nakai RL. A randomized controlled trial of women's early use of a novel undergarment following sternotomy: the Women's Recovery from Sternotomy Trial (WREST). Am Heart J. 2006;152:1187–1193. [DOI] [PubMed] [Google Scholar]
- 21. Keith M, Mokbel R, San Emeterio M, Song J, Errett L. Evaluation of taste sensitivity in patients undergoing coronary artery bypass graft surgery. J Am Diet Assoc. 2010;110:1072–1077. [DOI] [PubMed] [Google Scholar]
- 22. Koch CG, Li L, Lauer M, Sabik J, Starr NJ, Blackstone EH. Effect of functional health‐related quality of life on long‐term survival after cardiac surgery. Circulation. 2007;115:692–699. [DOI] [PubMed] [Google Scholar]
- 23. Cook DJ, Thompson JE, Prinsen SK, Dearani JA, Deschamps C. Functional recovery in the elderly after major surgery: assessment of mobility recovery using wireless technology. Ann Thorac Surg. 2013;96:1057–1061. [DOI] [PubMed] [Google Scholar]
- 24. Hirschhorn AD, Richards DA, Mungovan SF, Morris NR, Adams L. Does the mode of exercise influence recovery of functional capacity in the early postoperative period after coronary artery bypass graft surgery? A randomized controlled trial. Interact Cardiovasc Thorac Surg. 2012;15:995–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morone NE, Weiner DK, Belnap BH, Karp JF, Mazumdar S, Houck PR, He F, Rollman BL. The impact of pain and depression on recovery after coronary artery bypass grafting. Psychosom Med. 2010;72:620–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shuldham CM, Fleming S, Goodman H. The impact of pre‐operative education on recovery following coronary artery bypass surgery. A randomized controlled clinical trial. Eur Heart J. 2002;23:666–674. [DOI] [PubMed] [Google Scholar]
- 27. Zimmerman L, Barnason S, Hertzog M, Young L, Nieveen J, Schulz P, Tu C. Gender differences in recovery outcomes after an early recovery symptom management intervention. Heart Lung. 2011;40:429–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low‐risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med. 2000;133:253–262. [DOI] [PubMed] [Google Scholar]
- 29. Morgan JA, Peacock JC, Kohmoto T, Garrido MJ, Schanzer BM, Kherani AR, Vigilance DW, Cheema FH, Kaplan S, Smith CR, Oz MC, Argenziano M. Robotic techniques improve quality of life in patients undergoing atrial septal defect repair. Ann Thorac Surg. 2004;77:1328–1333. [DOI] [PubMed] [Google Scholar]
- 30. Tranmer JE, Parry MJ. Enhancing postoperative recovery of cardiac surgery patients: a randomized clinical trial of an advanced practice nursing intervention. West J Nurs Res. 2004;26:515–532. [DOI] [PubMed] [Google Scholar]
- 31. Ballan A, Lee G. A comparative study of patient perceived quality of life pre and post coronary artery bypass graft surgery. Aust J Adv Nurs. 2007;24:24–28. [PubMed] [Google Scholar]
- 32. Barnason S, Zimmerman L, Nieveen J, Schulz P, Miller C, Hertzog M, Rasmussen D. Relationships between fatigue and early postoperative recovery outcomes over time in elderly patients undergoing coronary artery bypass graft surgery. Heart Lung. 2008;37:245–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chunta KS. Expectations, anxiety, depression, and physical health status as predictors of recovery in open‐heart surgery patients. J Cardiovasc Nurs. 2009;24:454–464. [DOI] [PubMed] [Google Scholar]
- 34. Rosenfeldt F, Braun L, Spitzer O, Bradley S, Shepherd J, Bailey M, van der Merwe J, Leong JY, Esmore D. Physical conditioning and mental stress reduction–a randomised trial in patients undergoing cardiac surgery. BMC Complement Altern Med. 2011;11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yang M, Yao M, Wang G, Xiao C, Wu Y, Zhang H, Gao C. Comparison of postoperative quality of life for patients who undergo atrial myxoma excision with robotically assisted versus conventional surgery. J Thorac Cardiovasc Surg. 2015;150:152–157. [DOI] [PubMed] [Google Scholar]
- 36. Barnason S, Zimmerman L, Nieveen J, Hertzog M. Impact of a telehealth intervention to augment home health care on functional and recovery outcomes of elderly patients undergoing coronary artery bypass grafting. Heart Lung. 2006;35:225–233. [DOI] [PubMed] [Google Scholar]
- 37. Körtke H, Stromeyer H, Zittermann A, Buhr N, Zimmermann E, Wienecke E, Körfer R. New East‐Westfalian Postoperative Therapy Concept: a telemedicine guide for the study of ambulatory rehabilitation of patients after cardiac surgery. Telemed J E Health. 2006;12:475–483. [DOI] [PubMed] [Google Scholar]
- 38. Miller C, Zimmerman L, Barnason S, Nieveen J. Impact of an early recovery management intervention on functioning in postoperative coronary artery bypass patients with diabetes. Heart Lung. 2007;36:418–430. [DOI] [PubMed] [Google Scholar]
- 39. Abbott AA, Barnason S, Zimmerman L. Symptom burden clusters and their impact on psychosocial functioning following coronary artery bypass surgery. J Cardiovasc Nurs. 2010;25:301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Caputo M, Alwair H, Rogers CA, Pike K, Cohen A, Monk C, Tomkins S, Ryder I, Moscariello C, Lucchetti V, Angelini GD. Thoracic epidural anesthesia improves early outcomes in patients undergoing off‐pump coronary artery bypass surgery: a prospective, randomized, controlled trial. Anesthesiology. 2011;114:380–390. [DOI] [PubMed] [Google Scholar]
- 41. Chen YC, Chen KC, Lu LH, Wu YL, Lai TJ, Wang CH. Validating the 6‐minute walk test as an indicator of recovery in patients undergoing cardiac surgery: a prospective cohort study. Medicine (Baltimore). 2018;97:e12925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zimmerman L, Barnason S, Brey BA, Catlin SS, Nieveen J. Comparison of recovery patterns for patients undergoing coronary artery bypass grafting and minimally invasive direct coronary artery bypass in the early discharge period. Prog Cardiovasc Nurs. 2002;17:132–141. [DOI] [PubMed] [Google Scholar]
- 43. Centers for Medicare and Medicaid Services . CMS Quality Measure Development Plan: supporting the transition to the Merit‐based Incentive Payment System (MIPS) and alternative payment models (APMs). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/Final-MDP.pdf. Accessed March 10, 2019.
- 44. Borkon AM, Muehlebach GF, House J, Marso SP, Spertus JA. A comparison of the recovery of health status after percutaneous coronary intervention and coronary artery bypass. Ann Thorac Surg. 2002;74:1526–1530; discussion 1530. [DOI] [PubMed] [Google Scholar]
- 45. Jaensson M, Dahlberg K, Eriksson M, Nilsson U. Evaluation of postoperative recovery in day surgery patients using a mobile phone application: a multicentre randomized trial. Br J Anaesth. 2017;119:1030–1038. [DOI] [PubMed] [Google Scholar]
- 46. Gandek B, Sinclair SJ, Kosinski M, Ware JE. Psychometric evaluation of the SF‐36 health survey in Medicare managed care. Health Care Financ Rev. 2004;25:5–25. [PMC free article] [PubMed] [Google Scholar]
- 47. McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36‐item Short‐Form Health Survey (SF‐36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. [DOI] [PubMed] [Google Scholar]
- 48. O'Brien SM, Feng L, He X, Xian Y, Jacobs JP, Badhwar V, Kurlansky PA, Furnary AP, Cleveland JC, Lobdell KW, Vassileva C, Wylervon Ballmoos MC, Thourani VH, Rankin JS, Edgerton JR, D'Agostino RS, Desai ND, Edwards FH, Shahian DM. The society of thoracic surgeons 2018 adult cardiac surgery risk models: part 2‐statistical methods and results. Ann Thorac Surg. 2018;105:1419–1428. [DOI] [PubMed] [Google Scholar]
- 49. Gresham G, Hendifar AE, Spiegel B, Neeman E, Tuli R, Rimel BJ, Figlin RA, Meinert CL, Piantadosi S, Shinde AM. Wearable activity monitors to assess performance status and predict clinical outcomes in advanced cancer patients. npj Digital Med. 2018;1:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Edéll‐Gustafsson UM, Hetta JE, Arén CB. Sleep and quality of life assessment in patients undergoing coronary artery bypass grafting. J Adv Nurs. 1999;29:1213–1220. [DOI] [PubMed] [Google Scholar]
- 51. Newman MF, Kirchner JL, Phillips‐Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA; Neurological Outcome Research Group and the Cardiothoracic Anesthesiology Research Endeavors Investigators . Longitudinal assessment of neurocognitive function after coronary‐artery bypass surgery. N Engl J Med. 2001;344:395–402. [DOI] [PubMed] [Google Scholar]
- 52. Van de Water AT, Holmes A, Hurley DA. Objective measurements of sleep for non‐laboratory settings as alternatives to polysomnography—a systematic review. J Sleep Res. 2011;20:183–200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Search Terms.
Table S1. Journal Categorization by Specialty
Table S2. List of Included Studies
Table S3. Number of Articles by Journal Category
Table S4. Qualitative Summary of Predictors and Interventions Associated With Improved Recovery
Figure S1. Number of publications by year. Number of articles published by 5‐year increment of calendar year. No publication published before 1980 met the inclusion criteria. The latest bin (2015–2018) includes only a 4‐year period.
Figure S2. Bubble chart of studies by the study characteristics up to 400 follow‐up days. Studies by the duration of follow‐up (x axis) up to 400 days, sample size (y axis) up to 600 patients, number of domains evaluated (bubble size), and number of follow‐ups at which time the measurements were obtained (color). Six possible domains are: nociceptive symptoms, activities of daily living, cognitive, sleep, mental health, and physical function.


