Abstract
Background
Chronic psychological stress has been associated with hypertension, but few studies have examined this relationship in blacks. We examined the association between perceived stress levels assessed annually for up to 13 years and incident hypertension in the Jackson Heart Study, a community‐based cohort of blacks.
Methods and Results
Analyses included 1829 participants without hypertension at baseline (Exam 1, 2000–2004). Incident hypertension was defined as blood pressure≥140/90 mm Hg or antihypertensive medication use at Exam 2 (2005–2008) or Exam 3 (2009–2012). Each follow‐up interval at risk of hypertension was categorized as low, moderate, or high perceived stress based on the number of annual assessments between exams in which participants reported “a lot” or “extreme” stress over the previous year (low, 0 high stress ratings; moderate, 1 high stress rating; high, ≥2 high stress ratings). During follow‐up (median, 7.0 years), hypertension incidence was 48.5%. Hypertension developed in 30.6% of intervals with low perceived stress, 34.6% of intervals with moderate perceived stress, and 38.2% of intervals with high perceived stress. Age‐, sex‐, and time‐adjusted risk ratios (95% CI) associated with moderate and high perceived stress versus low perceived stress were 1.19 (1.04–1.37) and 1.37 (1.20–1.57), respectively (P trend<0.001). The association was present after adjustment for demographic, clinical, and behavioral factors and baseline stress (P trend=0.001).
Conclusions
In a community‐based cohort of blacks, higher perceived stress over time was associated with an increased risk of developing hypertension. Evaluating stress levels over time and intervening when high perceived stress is persistent may reduce hypertension risk.
Keywords: Blacks, blood pressure, chronic stress, hypertension, Jackson Heart Study
Subject Categories: Epidemiology, Race and Ethnicity, Hypertension, Mental Health
Clinical Perspective
What Is New?
In a community‐based cohort of blacks, high perceived stress over time was associated with a significantly higher risk of incident hypertension compared with sustained low stress.
This association was independent of demographic factors, clinical risk factors, lifestyle behaviors, and baseline stress levels.
What Are the Clinical Implications?
Studies are needed to determine whether stress management may be an effective approach to preventing hypertension in blacks.
Introduction
Psychosocial stress is thought to be implicated in the development of hypertension.1 Blacks experience greater exposure to specific chronic stressors, such as discrimination and low socioeconomic status, and report higher overall stress levels compared with whites.2, 3, 4, 5 However, strong evidence of a prospective association between stress and hypertension in blacks has been elusive.1, 6, 7, 8 For example, a previous analysis of the JHS (Jackson Heart Study), a community‐based cohort of blacks, found no association between multiple measures of stress and incident hypertension.6 Other large cohort studies have failed to demonstrate effects of perceived discrimination and job stress on incident hypertension among blacks.7, 8 Whether these findings suggest that effects of stress on hypertension differ in this population or reflect methodological limitations (eg, assessment of stress) is unknown. Chronic stressors often cluster, and the specific source(s) of stress may be less important than overall perceived stress level.2, 9, 10 Furthermore, most earlier studies have examined the association of stress assessed at a single occasion with incident hypertension, even though exposure to stressful events and circumstances can change over time. High levels of chronic stress over time are more likely than transient stress to contribute to sustained behavioral and physiological changes that increase hypertension risk.11, 12 It is also possible that there are sex differences in the effects of chronic stress on hypertension. In a previous cross‐sectional study of the JHS, higher stress was associated with a higher prevalence of hypertension, diabetes mellitus, and obesity in women, but not in men.13 Several prospective studies have also demonstrated stronger effects of stress on blood pressure (BP) and incident hypertension among women.14, 15, 16
Given the disproportionately high burden of hypertension in blacks,17, 18 determining whether chronic stress increases the risk of hypertension onset in this population is an important question that could inform nonpharmacological prevention strategies.19 We tested the association between chronic stress and incident hypertension using annual assessments of perceived stress over up to 13 years in the JHS, a community‐based cohort of blacks. We hypothesized that higher perceived stress over time (ie, chronic stress) would be associated with increased risk of incident hypertension, independent of baseline level of perceived stress. Moreover, given past evidence of sex differences in the experience and effects of stress,1, 14, 15, 16, 20 we conducted secondary analyses to explore whether the association between chronic stress and incident hypertension was stronger in women than in men.
Methods
The data, analytical methods, and study materials can be made available to other researchers for purposes of reproducing the results or replicating the procedure by following the JHS publications procedures and data‐use agreements found at: https://www.jacksonheartstudy.org/Research/Study-Data/Data-Access.
Study Population
The JHS is a cohort study designed to investigate the causes of cardiovascular disease in a community‐based sample of blacks. Details of the study design, recruitment approach, data collection, and measures have been previously published.21, 22, 23 Briefly, 5306 noninstitutionalized black adults aged ≥21 years were enrolled from the Jackson, Mississippi metropolitan tricounty area (Hinds, Madison, and Rankin counties) between 2000 and 2004 (Exam 1). Follow‐up visits were conducted between 2005 and 2008 (Exam 2) and between 2009 and 2012 (Exam 3). The current analysis included JHS participants with systolic BP (SBP)<140 mm Hg and diastolic BP (DBP)<90 mm Hg who were not taking antihypertensive medications at Exam 1 (n=2308). Participants who were missing medication and BP data at follow‐up were excluded (n=321), as were participants with <2 annual follow‐up assessments of stress between exams (n=158), because their chronic stress exposure could not be defined. After applying these exclusion criteria, the analytical sample was 1829 participants. The JHS was approved by the institutional review boards of the participating institutions: University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided written informed consent. Figure shows the study design and timing of measurements.
Figure 1.
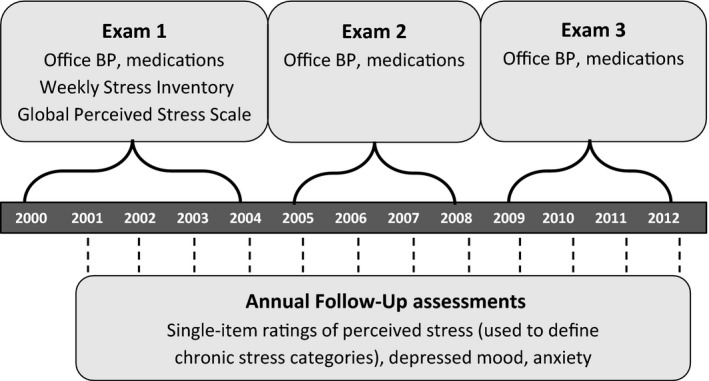
JHS study design and data collection timing. BP indicates blood pressure; JHS, Jackson Heart Study.
Data Collection
Data were collected during an in‐home interview and clinic examination at each study visit and at annual telephone follow‐up assessments between visits. Trained research staff measured height, weight, and BP, collected blood and urine samples, and administered questionnaires to collect data on sociodemographic factors, medical history, medication use, health behaviors, and psychosocial factors.
BP measurement
Clinic BP was measured at each exam following a standardized protocol. Specifically, after participants had rested for at least 5 minutes, trained staff performed 2 BP measurements, 1 minute apart, in the participant's right arm. The appropriate cuff size was determined from an arm circumference measurement. The 2 clinic BP measurements were averaged for analysis. Quality‐control procedures conducted by the JHS Coordinating Center included monitoring digit preference, comparing mean BP measurements within and between technicians, and technician recertification every 6 months.
A random‐zero sphygmomanometer (Hawksley and Sons, Ltd, London, UK) was used at Exams 1 and 2, and a semiautomatic oscillometric device (Omron HEM‐ 907XL; Omron Healthcare, Inc, Lake Forest, IL) was used at Exams 2 and 3. A BP comparability substudy was performed in 2115 participants who had their BP measured simultaneously with a random‐zero sphygmomanometer and the oscillometric device using a Y‐connector at Exam 2. As previously described, random‐zero BP measurements were calibrated to the semiautomated device using robust regression, and calibrated data were used in these cases.24 Clinic BP from the semiautomated device was used when available.
Incident hypertension was defined as the first follow‐up exam at which a participant had any of the following: SBP≥140 mm Hg, DBP≥90 mm Hg, or reported use of antihypertensive medication.25 Current antihypertensive medication use was defined as self‐reported use of antihypertensive medication in the 2 weeks preceding the exam. We did not use the BP threshold of SBP≥130 mm Hg or DBP≥80 mm Hg to define high BP, as recommended in the 2017 American College of Cardiology/American Heart Association BP guideline,26 given that these lower BP thresholds were not routinely recommended between 2000 and 2012 when the 3 JHS exams were conducted.
Chronic stress exposure
A longitudinal measure of chronic stress exposure was derived from responses to a single‐item measure of overall perceived stress administered during each annual follow‐up (AFU) assessment. The question asks: “How much stress have you experienced over the past year?” Respondents answered on a 6‐point Likert scale with the following options: “None,” “Very little,” “Mild stress,” “Moderate stress,” “A lot of stress,” or “Extreme stress.” Ratings from “None” to “Moderate” were coded as low perceived stress, and ratings of “A lot” or “Extreme” were coded as high perceived stress. This item is similar to a previously validated single‐item measure of stress experienced over the past year.27 The number of AFU assessments in an interval at risk of incident hypertension (ie, between Exams 1 and 2, between Exams 2 and 3, and between Exams 1 and 3 for participants missing Exam 2 data) in which participants reported high perceived stress was used to define 3 categories of chronic stress (ie, high perceived stress over time): (1) low chronic stress (0 AFU assessments with high perceived stress ratings); (2) moderate chronic stress (1 AFU assessment with high perceived stress ratings); and (3) high chronic stress (≥2 AFU assessments with high perceived stress ratings). The mean number of perceived stress ratings per interval was 3.25 (SD=0.99).
Baseline stress
The single‐item measure of stress used to define chronic stress was not administered at the JHS baseline exam, so we used 2 other measures to adjust for baseline stress in our analyses. The Weekly Stress Inventory (WSI) is a validated 87‐item checklist of minor stressors occurring in multiple life domains (eg, work, family, and finances).28 Participants indicated whether or not each event occurred during the previous week, and the number of stressful events was summed to create a score ranging from 0 to 87 (α=0.98). The Global Perceived Stress Scale (GPSS) is an 8‐item measure developed for the JHS that assesses domain‐specific stressors experienced over the previous 12 months: job, relationships, neighborhood, caregiving, legal, medical, racism and discrimination, and meeting basic needs.27 Scores range from 0 to 24, with higher scores indicating greater levels of stress. Because the WSI was associated with BP progression in a previous study of the JHS,6 this measure of baseline stress was selected as a covariate in the primary analysis. To examine whether results were sensitive to the definition of baseline stress, we replaced the WSI with the GPSS in a sensitivity analysis.
Depressed mood and anxiety over time
Longitudinal measures of depressed mood and anxiety were derived from the annual follow‐up items: “How often have you felt sad or depressed over the past year?” and “How often have you felt nervous or tense over the past year?” Respondents answered on a 6‐point Likert scale with the following options: “Almost never,” “Seldom,” “Sometimes,” “Often,” “Very often,” or “Constantly.” Following the approach used for perceived stress, the 4 lowest ratings (ie, from “Almost never” to “Often”) were coded as low depressed mood or low anxiety and the 2 highest ratings (ie, “Very often,” “Constantly”) were coded as high depressed mood or high anxiety. The percentage of AFU assessments in which participants reported high levels of depressed mood and high anxiety, respectively, in an interval at risk of incident hypertension were calculated and included in a sensitivity analysis.
Covariates
Additional covariates were selected based on known associations with incident hypertension and included age, sex, education (less than high school versus high school or greater), marital status (married versus unmarried), parental history of hypertension, baseline SBP, baseline DBP, baseline body mass index, diabetes mellitus, reduced estimated glomerular filtration rate (eGFR), smoking, alcohol use, physical activity, and diet. Diabetes mellitus was defined by self‐report of taking diabetes mellitus medication or fasting glucose ≥126 mg/dL or glycated hemoglobin≥6.5%. Reduced eGFR was defined as <60 mL/min/1.73 m2. Current smoking was defined as having smoked at least 400 cigarettes in one's lifetime and self‐report of currently smoking.29 Alcohol consumption was defined as: “none” being 0 alcoholic beverages per week, “moderate” consumption being 1 to 14 and 1 to 7 alcoholic beverages per week for men and women, respectively, and “heavy” consumption being >14 and >7 alcoholic beverages per week for men and women, respectively.30 Physical activity was assessed using a modified Baecke questionnaire that was validated in the JHS and provided number of minutes per week of moderate or vigorous exercise.31 Diet was assessed using a 158‐item food frequency questionnaire that was validated in the JHS.32 Physical activity and diet were coded as poor, intermediate, or ideal based on the American Heart Association's Life's Simple 7 guidelines.33, 34
Statistical Analysis
Baseline characteristics of the sample were calculated overall and stratified by incident hypertension status. The association of chronic stress exposure during each interval at risk and incident hypertension at the following exam was determined. Specifically, perceived stress ratings from AFU assessments between Exams 1 and 2 were used to predict incident hypertension at Exam 2. Perceived stress ratings from AFU assessments between Exams 2 and 3 were used to predict incident hypertension at Exam 3 among participants who did not develop hypertension by Exam 2. For participants missing Exam 2 data, AFU assessments between Exams 1 and 3 were used to predict incident hypertension at Exam 3. The association between chronic perceived stress category and incident hypertension was then tested using repeated‐measures generalized estimating equations with a Poisson distribution.35 As recommended for Poisson regressions with binary outcome data, a robust covariance matrix was specified.36 Interval‐censored cox regression was not used because measurement of the exposure (longitudinally assessed stress) would overlap with the outcome. We calculated risk ratios (RRs) for incident hypertension associated with chronic perceived stress exposure (moderate versus low, high versus low) adjusting for age, sex, and years between exams (model 1). Subsequent models (models 2–4) included progressive adjustment for other demographics and hypertension risk factors (education, marital status, parental history of hypertension, baseline SBP, baseline DBP, body mass index, diabetes mellitus, and reduced eGFR), baseline stress (WSI), and behavioral factors that are in the hypothesized causal pathway between stress and hypertension (smoking, alcohol use, physical activity, and diet). Missing values of covariates were imputed using multiple imputation with full conditional specification. To test the hypothesis that the association of high perceived stress over time with incident hypertension would be stronger in women than men, we examined the chronic stress category×sex interaction. We also examined effects of chronic perceived stress on incident hypertension stratified by sex.
Sensitivity analyses
To examine whether the association between high perceived stress over time and incident hypertension was sensitive to the definition of baseline stress, we performed a sensitivity analysis in which the GPSS replaced the WSI as a covariate in model 3. A second sensitivity analysis was performed in which the percentage of AFU assessments with high depressed mood and high anxious mood were included as covariates to determine whether the effect of chronic stress was independent of these related psychosocial factors.37, 38, 39, 40 A third sensitivity analysis was performed to examine whether results were influenced by the definition of the chronic stress variable developed from AFU ratings. We revised the variable as follows using a higher threshold to define the high chronic stress category: low chronic stress (0 AFU ratings of high perceived stress in a follow‐up interval); moderate chronic stress (1–2 AFU ratings of high perceived stress); and high chronic stress (≥3 AFU ratings of high perceived stress). This approach required participants to have ≥3 AFU stress ratings in an interval at risk of hypertension, which reduced the sample size to 1423 participants who contributed 1875 intervals in this sensitivity analysis. A final sensitivity analysis was performed in which incident hypertension was defined by initiation of antihypertensive medication use only, regardless of BP level, to address the limitation of definining incident hypertension based on BP measurements from a single visit.
P<0.05 were considered statistically significant. Analyses were conducted using SPSS software (v24; IBM Corp, Armonk, NY).
Results
Participant Characteristics
Sample characteristics are shown in Table 1. Mean (±SD) age was 49.3±11.9 years, and 40.0% of participants were male. Average baseline SBP and DBP were 118.6±10.6 and 73.9±7.3 mm Hg, respectively. Participants who developed versus did not develop incident hypertension were older, less likely to have a high school education, had higher baseline SBP, DBP, and body mass index, and were more likely to have diabetes mellitus and reduced eGFR. They were also more likely to be current smokers, not use alcohol, and had lower physical activity levels. Baseline stress level did not differ significantly between those who did versus did not develop hypertension (35.93±23.52 versus 36.28±23.15; P=0.785). Compared with participants included in the analysis sample, the 479 participants who were free of hypertension at baseline, but excluded because of missing exposure or follow‐up data, had lower education, were less likely to be married, were more likely to have diabetes mellitus and reduced eGFR, were more likely to be smokers, and had lower levels of physical activity (Table S1). The 2 groups did not differ significantly on baseline BP or baseline stress levels.
Table 1.
Baseline Characteristics of JHS Participants Without Hypertension
| Characteristic | Overall (n=1829) | Did Not Develop Hypertension (n=942) | Developed Hypertension (N=887) | P Valuea |
|---|---|---|---|---|
| Age, y | 49.32 (11.89) | 46.73 (11.81) | 52.06 (11.36) | <0.001 |
| Men, % | 732 (40.0%) | 391 (41.5%) | 341 (38.4%) | 0.181 |
| Less than high school education, % | 218 (12.0%) | 85 (9.1%) | 133 (15.0%) | <0.001 |
| Married, % | 1085 (59.5%) | 551 (58.7%) | 534 (60.3%) | 0.488 |
| Systolic BP, mm Hg | 118.55 (10.64) | 114.26 (9.89) | 123.11 (9.45) | <0.001 |
| Diastolic BP, mm Hg | 73.86 (7.31) | 72.20 (6.75) | 75.62 (7.47) | <0.001 |
| BMI, kg/m2 | 30.59 (6.96) | 29.76 (6.68) | 31.47 (7.16) | <0.001 |
| Parental history of hypertension, % | 1220 (69.0%) | 615 (67.4%) | 605 (70.8%) | 0.131 |
| Diabetes mellitus, % | 154 (8.5%) | 40 (4.3%) | 114 (13.0%) | <0.001 |
| Reduced eGFR, % | 24 (1.3%) | 6 (0.6%) | 18 (2.1%) | 0.009 |
| Current smoking, % | 245 (13.6%) | 95 (10.2%) | 150 (17.1%) | <0.001 |
| Current alcohol use, % | ||||
| None | 841 (64.6%) | 393 (61.0%) | 448 (68.2%) | 0.024 |
| Low | 384 (29.5%) | 211 (32.8%) | 173 (26.3%) | |
| High | 76 (5.8%) | 40 (6.2%) | 36 (5.5%) | |
| Physical activity, % | ||||
| Poor | 760 (41.6%) | 348 (37.0%) | 412 (46.4%) | <0.001 |
| Intermediate | 649 (35.5%) | 342 (36.4%) | 307 (34.6%) | |
| Ideal | 418 (22.9%) | 250 (26.6%) | 168 (18.9%) | |
| Diet, % | ||||
| Poor | 1029 (62.8%) | 515 (61.8%) | 514 (63.9%) | 0.095 |
| Intermediate | 598 (36.5%) | 310 (37.2%) | 288 (35.8%) | |
| Ideal | 11 (0.7%) | 9 (1.1%) | 2 (0.2%) | |
| Baseline stress (WSI) | 36.11 (23.32) | 36.28 (23.15) | 35.93 (23.52) | 0.785 |
Data presented as mean (SD) or n (%). BMI indicates body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate; JHS, Jackson Heart Study; WSI, Weekly Stress Inventory.
P values for comparisons were generated using independent‐samples t tests for continuous variables and chi‐squared tests for categorical variables.
The 1829 participants in the analytical sample contributed data to 2711 intervals at risk of incident hypertension. Specifically, 1744 participants had sufficient data to define chronic perceived stress for the first analysis interval (Exams 1–2 or Exams 1–3 if Exam 2 was missed). In addition, 967 participants who did not develop hypertension by Exam 2 contributed data to the second analysis interval (Exams 2–3). Of the 2711 intervals at risk of hypertension, 1704 (62.9%) were classified as low chronic stress, 512 (18.9%) moderate chronic stress, and 495 (18.3%) high chronic stress. Older age, female sex, higher body mass index, lower baseline SBP, parental history of hypertension, being unmarried, current smoking status, and higher baseline stress were each associated with higher categories of chronic perceived stress (Ps<0.01).
Chronic Perceived Stress and Incident Hypertension
Over a median follow‐up of 7.0 years, 887 (48.5%) participants developed incident hypertension (587 at Exam 2 and 300 at Exam 3). As shown in Table 2, higher perceived stress over time was associated with a greater risk of incident hypertension. In model 1, the age‐, sex‐, and time‐adjusted RRs associated with moderate and high chronic stress compared with low chronic stress were 1.19 (95% CI, 1.04–1.37) and 1.37 (95% CI, 1.20–1.57), respectively (P trend<0.001). This association between higher perceived stress over time and incident hypertension remained statistically significant after adjustment for hypertension risk factors in model 2 (moderate versus low, RR=1.18, 95% CI, 1.04–1.34; high versus low, RR=1.27, 95% CI, 1.12–1.45; P trend<0.001), additional adjustment for baseline stress in model 3 (moderate versus low, RR=1.17, 95% CI, 1.02–1.33; high versus low, RR=1.24, 95% CI, 1.09–1.42; P trend<0.001), and further adjustment for health behaviors in model 4 (moderate versus low, RR=1.15, 95% CI, 1.01–1.31; high versus low, RR=1.22, 95% CI, 1.07–1.39; P trend=0.001).
Table 2.
Risk Ratios for Incident Hypertension Associated With Chronic Stress
| Chronic Stress Categorya | n Cases of Incident Hypertension/n Intervals at Risk | Risk Ratio (95% CI) | |||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Low | 521/1704 (30.6%) | REF | REF | REF | REF |
| Moderate | 177/512 (34.6%) | 1.19 (1.04–1.37) | 1.18 (1.04–1.34) | 1.17 (1.02–1.33) | 1.15 (1.01–1.31) |
| High | 189/495 (38.2%) | 1.37 (1.20–1.57) | 1.27 (1.12–1.45) | 1.24 (1.09–1.42) | 1.22 (1.07–1.39) |
| P trend | 0.004 | <0.001 | <0.001 | <0.001 | 0.001 |
Model 1, adjusted for age, sex, and time between exams. Model 2, model 1 plus education, marital status, parental history of hypertension, systolic BP, diastolic BP, body mass index, diabetes mellitus, and reduced eGFR. Model 3, model 2 plus baseline stress (Weekly Stress Inventory). Model 4, model 3 plus current smoking, alcohol use, physical activity, and diet. BP indicates blood pressure; eGFR, estimated glomerular filtration rate.
Low, 0 annual follow‐up (AFU) ratings of high perceived stress; moderate, 1 AFU rating of high perceived stress; high, ≥2 AFU ratings of high perceived stress.
Stress by sex interaction was not statistically significant in unadjusted (P=0.782) or fully adjusted models (P=0.695). In analyses stratified by sex (Table 3), higher levels of chronic stress were associated with a higher risk of incident hypertension in both groups, but the association was statistically significant in women and not in men in fully adjusted models (model 4). The adjusted RRs (Model 4) associated with moderate and high chronic stress compared with low chronic stress among women were 1.19 (95% CI, 1.01–1.39) and 1.25 (95% CI, 1.08–1.46), respectively (P trend=0.002). Among men, the adjusted RRs (model 4) associated with moderate and high chronic stress compared with low chronic stress were 1.12 (95% CI, 0.89–1.41) and 1.17 (95% CI, 0.91–1.51), respectively (P trend=0.172).
Table 3.
Risk Ratios for Incident Hypertension Associated With Chronic Stress, Stratified by Sex
| Chronic Stress Categorya | n Cases of Incident Hypertension/n Intervals at Risk | Risk Ratio (95% CI) | |||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| Men (n=1098) | |||||
| Low | 233/781 (29.8%) | REF | REF | REF | REF |
| Moderate | 59/181 (32.6%) | 1.20 (0.95–1.52) | 1.16 (0.92–1.45) | 1.14 (0.90–1.43) | 1.12 (0.89–1.41) |
| High | 49/136 (36.0%) | 1.40 (1.10–1.79) | 1.23 (0.95–1.59) | 1.19 (0.91–1.54) | 1.17 (0.91–1.51) |
| P trend | 0.314 | 0.004 | 0.075 | 0.141 | 0.172 |
| Women (n=1613) | |||||
| Low | 288/923 (31.2%) | REF | REF | REF | REF |
| Moderate | 118/331 (35.6%) | 1.19 (1.00–1.40) | 1.20 (1.03–1.41) | 1.19 (1.02–1.40) | 1.19 (1.01–1.39) |
| High | 140/359 (39.0%) | 1.36 (1.16–1.60) | 1.29 (1.11–1.50) | 1.27 (1.09–1.48) | 1.25 (1.08–1.46) |
| P trend | 0.022 | <0.001 | <0.001 | 0.001 | 0.002 |
Model 1, adjusted for age, time between exams. Model 2,‐model 1 plus education, marital status, parental history of hypertension, systolic BP, diastolic BP, body mass index, diabetes mellitus, and reduced eGFR. Model 3, model 2 plus baseline stress (Weekly Stress Inventory). Model 4, model 3 plus current smoking, alcohol use, physical activity, and diet. BP indicates blood pressure; eGFR, estimated glomerular filtration rate.
Low, 0 annual follow‐up (AFU) ratings of high perceived stress; moderate, 1 AFU rating of high perceived stress; high, ≥2 AFU ratings of high perceived stress.
In a sensitivity analysis in which we replaced the WSI with the GPSS to adjust for baseline stress, the chronic stress category remained associated with incident hypertension (P trend=0.006; model 4). In a second sensitivity analysis, the association between chronic stress category and incident hypertension remained statistically significant after adjustment for depressed mood and anxiety over time (Table S2). In a third sensitivity analysis using a higher threshold to define high chronic stress in a subset of participants (n=1423), chronic stress was associated with incident hypertension after adjustment for demographics, hypertension risk factors, and baseline stress in model 3 (P=0.029), but became marginally significant after adjustment for behavioral factors in model 4 (P=0.056; Table S3).
To address the limitation of obtaining BP measurements at a single visit for each study exam, we examined the proportion of participants who were classified as having incident hypertension based on BP alone versus antihypertensive medication use. Of the 587 participants who developed hypertension at Exam 2, 430 (73.3%) were taking antihypertensive medication and 157 (26.7%) had elevated BP, but were not taking antihypertensive medication. Of the latter group who completed Exam 3 (n=132), 108 (81.8%) continued to meet criteria for hypertension at Exam 3. In a sensitivity analysis in which incident hypertension was defined by initiation of antihypertensive medication use alone, results were virtually unchanged and remained statistically significant in all 4 models (model 4: moderate versus low, RR=1.28, 95% CI, 1.10–1.48; high versus low, RR=1.22, 95% CI, 1.03–1.43; P trend=0.004).
Discussion
In this community‐based cohort of blacks, moderate and high perceived stress over time were associated with a 15% and 22% increased risk of developing hypertension over a median of 7 years, respectively, compared with sustained low perceived stress. The association was independent of traditional sociodemographic and hypertension risk factors, health behaviors, and baseline stress level. The effect of chronic perceived stress was also independent of depressed mood and anxiety over time. This finding is notable given that earlier studies did not adjust for these related psychosocial factors, which may have resulted in overestimation of the effect of stress.37, 38 Overall, the present findings suggest that among blacks, higher perceived stress over time independently contributes to hypertension onset.
A recent study of the JHS found that baseline stress was associated with BP progression (increase by 1 BP stage as defined by JNC7) through Exam 2, but not with incident hypertension or with changes in BP.6 A strength of the current study is the use of annual assessments of stress, which allows identification of those exposed to high chronic stress over time. Acute stress is known to affect BP, and this sympathetic nervous system reactivity is 1 mechanism underlying the association between stress and hypertension.12, 41 However, short‐term or mild levels of stress are unlikely to have sustained effects on behavioral and pathophysiological processes that contribute to the development of hypertension.11, 12 In the present study, higher baseline stress was associated with more‐frequent reports of high stress over time, but baseline stress was not significantly different in participants who did and did not develop hypertension. Our findings support the hypothesis that determining chronic stress exposure over time identifies individuals at higher risk of developing hypertension.
These findings are consistent with earlier studies that demonstrated associations between sustained or increasing stress levels over time and incident hypertension.15, 39, 42, 43, 44 In the CARDIA (Coronary Artery Risk Development in Young Adults) study, increasing job strain over time and both baseline and continued financial hardship were associated with an increased risk of incident hypertension among young adults.42, 44 The CARDIA study included black and white participants, but race‐stratified results were not reported. Other studies that have tested longitudinal measures of stress and distress included few blacks.39, 43 The present study extends earlier findings by demonstrating that chronic stress over time was associated with incident hypertension among middle‐aged blacks. Furthermore, these findings suggest the importance of overall perceived stress levels, which reflect the cumulative burden of multiple stress exposures (eg, job, financial, and discrimination).
In stratified analyses, there was an association between higher levels of chronic stress and incident hypertension in both women and men, but after multivariable adjustment the association was statistically significant only in women. Although these findings should be interpreted cautiously given that the stress×sex interaction was not statistically significant, the possibility that women may be more vulnerable to the effects of chronic stress is in line with previous research. In an earlier cross‐sectional study of the JHS, higher stress was associated with a higher prevalence of hypertension, diabetes mellitus, and obesity in women, but not in men.13 Several prospective studies have also demonstrated stronger effects of stress on BP and incident hypertension among women.14, 15, 16 There are a number of possible explanations for these findings. Women might be exposed to more‐stressful events than men, and they may appraise life events as more stressful.20, 45 Women are also more likely than men to engage in rumination, or persistent negative thinking about stressful experiences, which can prolong adverse emotional and physiological stress responses associated with hypertension.46, 47, 48, 49 Given increasing recognition of cardiovascular disease risk in black women, further exploration of the possible contribution of stress in this population is warranted.50
The JHS is 1 of the largest longitudinal cohort studies of blacks, and its design enabled us to examine effects of perceived stress levels reported annually over several years. Despite these strengths, the present findings should be considered in light of several limitations. First, the measure of chronic stress used in this study is derived from single‐item ratings of perceived stress and does not characterize the type of stress participants experienced. This measure is conceptually similar to that of the widely used Perceived Stress Scale (Cohen),9 which captures the cumulative burden of stress from any source and has been associated with cardiovascular disease incidence and outcomes.51, 52, 53 Although longer, validated measures have advantages, the approach used in the JHS is more feasible for collecting annual assessments of multiple psychosocial domains. This allowed us to distinguish participants with high perceived stress over time from those with high stress at only 1 time point, and to evaluate the effect of chronic perceived stress while controlling for levels of anxiety and depressed mood during the same period of time. Second, because the single‐item stress rating was not administered at baseline, we were limited to the measures administered when controlling for baseline stress (ie, WSI and GPSS). These measures were significantly associated with perceived stress over time, but are conceptually distinct in the type of stress being assessed. Third, incident hypertension was identified based on BP measurements taken at a single visit. This approach is common in epidemiological research, but clinical guidelines recommend diagnosing hypertension based on elevated BP at ≥2 visits.25, 26 This limitation is partly mitigated by the use of a standardized protocol to measure BP. Furthermore, most cases of incident hypertension were identified based on initiation of antihypertensive medication rather than clinic BP level alone, and a sensitivity analysis in which incident hypertension was defined only by medication use showed virtually unchanged results. Fourth, although we controlled for many potential confounders, lifestyle behaviors were assessed by self‐report rather than objective measures, and we could not account for changes in behavior over time. Finally, the results may not be generalizable to black populations beyond the Jackson, Mississippi metropolitan area.
Conclusions
In the current study, higher stress over time was associated with incident hypertension in a community‐based sample of blacks. It has been hypothesized that exposure to chronic stress accounts, in part, for disparities in hypertension and cardiovascular disease between blacks and whites, though few studies have directly tested this hypothesis.2, 5 Some of the chronic stressors that disproportionately affect blacks (eg, discrimination, low socioeconomic status) are difficult to intervene on,54, 55 but stress appraisals and responses to stressful events and circumstances can be modified. Interventions that teach more‐adaptive coping responses may mitigate the adverse cardiovascular effects of chronic stress exposure. For example, fostering mindfulness may buffer stress‐related emotional and pathophysiological processes that contribute to the development of hypertension.56, 57, 58 The results of the current study suggest that it is important to evaluate chronic stress over time, rather than at a single occasion, and to intervene when it is persistent. Identifying effective, culturally sensitive stress management interventions may support primary prevention of hypertension and subsequent cardiovascular disease risk among blacks.
Sources of Funding
The JHS (Jackson Heart Study) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I/HHSN26800001), and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute for Minority Health and Health Disparities (NIMHD). Preparation of the manuscript was also supported by the National Institutes of Health grants R01HL117323, R01HL137818, and K24HL111315, R01DK108628‐05S1 and from UL1TR001873 and KL2TR001874 from the National Center for Advancing Translational Sciences. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosures
None.
Supporting information
Table S1. Characteristics of JHS Participants Without Hypertension at Baseline Who Were Included and Excluded From Analysis Sample
Table S2. Risk Ratios for Incident Hypertension Associated With Chronic Stress, Adjusted for Depressed Mood and Anxiety Over Time
Acknowledgments
The authors thank the staffs and participants of the JHS.
Dr Butler had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
(J Am Heart Assoc. 2019;8:e012139 DOI: 10.1161/JAHA.119.012139.)
A subset of the data contained in this article was presented at the American Heart Association Epi/Lifestyle Scientific Sessions, March 20 to 23, 2018, in New Orleans, LA.
References
- 1. Spruill TM. Chronic psychosocial stress and hypertension. Curr Hypertens Rep. 2010;12:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: how much does stress really matter? Du Bois Rev. 2011;8:95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burroughs Pena MS, Mbassa RS, Slopen NB, Williams DR, Buring JE, Albert MA. Cumulative psychosocial stress and ideal cardiovascular health in older women. Circulation. 2019;139:2012–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Neal WT, Qureshi W, Judd SE, Glasser SP, Ghazi L, Pulley L, Howard VJ, Howard G, Soliman EZ. Perceived stress and atrial ribrillation: the REasons for Geographic and Racial Differences in Stroke study. Ann Behav Med. 2015;49:802–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American Psychological Association, APA Working Group on Stress and Health Disparities . Stress and health disparities: contexts, mechanisms, and interventions among racial/ethnic minority and low‐socioeconomic status populations. 2017. Available at: http://www.apa.org/pi/health-disparities/resources/stress-report.aspx. Accessed December 13, 2018.
- 6. Ford CD, Sims M, Higginbotham JC, Crowther MR, Wyatt SB, Musani SK, Payne TJ, Fox ER, Parton JM. Psychosocial factors are associated with blood pressure progression among African Americans in the Jackson Heart Study. Am J Hypertens. 2016;29:913–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cozier Y, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Racial discrimination and the incidence of hypertension in US black women. Ann Epidemiol. 2006;16:681–687. [DOI] [PubMed] [Google Scholar]
- 8. Mezuk B, Kershaw KN, Hudson D, Lim KA, Ratliff S. Job strain, workplace discrimination, and hypertension among older workers: the Health and Retirement Study. Race Soc Probl. 2011;3:38–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 10. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer; 1984. [Google Scholar]
- 11. Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–2162. [DOI] [PubMed] [Google Scholar]
- 12. McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gebreab SY, Diez‐Roux AV, Hickson DA, Boykin S, Sims M, Sarpong DF, Taylor HA, Wyatt SB. The contribution of stress to the social patterning of clinical and subclinical CVD risk factors in African Americans: the Jackson Heart Study. Soc Sci Med. 2012;75:1697–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wiernik E, Nabi H, Pannier B, Czernichow S, Hanon O, Simon T, Simon JM, Thomas F, Ducolombier C, Danchin N, Limosin F, Consoli SM, Lemogne C. Perceived stress, sex and occupational status interact to increase the risk of future high blood pressure: the IPC cohort study. J Hypertens. 2014;32:1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gilbert‐Ouimet M, Brisson C, Vezina M, Milot A, Blanchette C. Repeated exposure to effort‐reward imbalance, increased blood pressure, and hypertension incidence among white‐collar workers: effort‐reward imbalance and blood pressure. J Psychosom Res. 2012;72:26–32. [DOI] [PubMed] [Google Scholar]
- 16. Mayne SL, Moore KA, Powell‐Wiley TM, Evenson KR, Block R, Kershaw KN. Longitudinal associations of neighborhood crime and perceived safety with blood pressure: the Multi‐Ethnic Study of Atherosclerosis (MESA). Am J Hypertens. 2018;31:1024–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 18. Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle‐aged and older adults: the multi‐ethnic study of atherosclerosis. Hypertension. 2011;57:1101–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, Fuchs FD, Hughes JW, Lackland DT, Staffileno BA, Townsend RR, Rajagopalan S; on behalf of the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity and Metabolism . Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61:1360–1383. [DOI] [PubMed] [Google Scholar]
- 20. Cohen S, Janicki‐Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42:1320–1334. [Google Scholar]
- 21. Taylor HA Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15(suppl 6):S6‐4–17. [PubMed] [Google Scholar]
- 22. Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez‐Mohammed ML, Calvin RL, Taylor HA Jr, Williams DR. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15(suppl 6):S6‐38–48. [PubMed] [Google Scholar]
- 23. Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, Taylor HA Jr. Recruiting African‐American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15(suppl 6):S6‐18–29. [PubMed] [Google Scholar]
- 24. Abdalla M, Booth JN III, Seals SR, Spruill TM, Viera AJ, Diaz KM, Sims M, Muntner P, Shimbo D. Masked hypertension and incident clinic hypertension among blacks in the Jackson Heart Study. Hypertension. 2016;68:220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; the National High Blood Pressure Education Program Coordinating Committee . Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 26. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 27. Littman AJ, White E, Satia JA, Bowen DJ, Kristal AR. Reliability and validity of 2 single‐item measures of psychosocial stress. Epidemiology. 2006;17:398–403. [DOI] [PubMed] [Google Scholar]
- 28. Mosley TH Jr, Payne TJ, Plaud JJ, Johnson CA, Wittrock DA, Seville JL, Penzien DB, Rodriguez G. Psychometric properties of the Weekly Stress Inventory (WSI): extension to a patient sample with coronary heart disease. J Behav Med. 1996;19:273–287. [DOI] [PubMed] [Google Scholar]
- 29. The ARIC Investigators . The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 30. U.S. Department of Agriculture; U.S. Department of Health and Human Services . Dietary Guidelines for Americans, 2010, 7th ed. Washington, DC: U.S. Government Printing Office; December 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smitherman TA, Dubbert PM, Grothe KB, Sung JH, Kendzor DE, Reis JP, Ainsworth BE, Newton RL Jr, Lesniak KT, Taylor HA Jr. Validation of the Jackson heart study physical activity survey in African Americans. J Phys Act Health. 2009;6:S124–S132. [DOI] [PubMed] [Google Scholar]
- 32. Carithers T, Dubbert PM, Crook E, Davy B, Wyatt SB, Bogle ML, Taylor HA Jr, Tucker KL. Dietary assessment in African Americans: methods used in the Jackson Heart Study. Ethn Dis. 2005;15:S649–S655. [PubMed] [Google Scholar]
- 33. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD; ARIC Study Investigators . Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Booth JN III, Abdalla M, Tanner RM, Diaz KM, Bromfield SG, Tajeu GS, Correa A, Sims M, Ogedegbe G, Bress AP, Spruill TM, Shimbo D, Muntner P. Cardiovascular health and incident hypertension in blacks: JHS (the Jackson Heart Study). Hypertension. 2017;70:285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 36. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 37. Nabi H, Chastang JF, Lefèvre T, Dugravot A, Melchior M, Marmot MG, Shipley MJ, Kivimäki M, Singh‐Manoux A. Trajectories of depressive episodes and hypertension over 24 years: the Whitehall II prospective cohort study. Hypertension. 2011;57:710–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Meng L, Chen D, Yang Y, Zheng Y, Hui R. Depression increases the risk of hypertension incidence: a meta‐analysis of prospective cohort studies. J Hypertens. 2012;30:842–851. [DOI] [PubMed] [Google Scholar]
- 39. Raikkonen K, Matthews KA, Kuller LH. Trajectory of psychological risk and incident hypertension in middle‐aged women. Hypertension. 2001;38:798–802. [PubMed] [Google Scholar]
- 40. Kubzansky LD, Cole SR, Kawachi I, Vokonas P, Sparrow D. Shared and unique contributions of anger, anxiety, and depression to coronary heart disease: a prospective study in the normative aging study. Ann Behav Med. 2006;31:21–29. [DOI] [PubMed] [Google Scholar]
- 41. Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory‐induced stress in healthy populations: a quantitative review of 30 years of investigations. Psychol Bull. 2008;134:829–885. [DOI] [PubMed] [Google Scholar]
- 42. Markovitz JH, Matthews KA, Whooley M, Lewis CE, Greenlund KJ. Increases in job strain are associated with incident hypertension in the CARDIA Study. Ann Behav Med. 2004;28:4–9. [DOI] [PubMed] [Google Scholar]
- 43. Capistrant BD, Moon JR, Glymour MM. Spousal caregiving and incident hypertension. Am J Hypertens. 2012;25:437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Matthews KA, Kiefe CI, Lewis CE, Liu K, Sidney S, Yunis C; Coronary Artery Risk Development in Young Adults Study (CARDIA) . Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension. 2002;39:772–776. [DOI] [PubMed] [Google Scholar]
- 45. Matud MP. Gender differences in stress and coping styles. Pers Indiv Differ. 2004;37:1401–1415. [Google Scholar]
- 46. Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: a review of worry, prolonged stress‐related physiological activation, and health. J Psychosom Res. 2006;60:113–124. [DOI] [PubMed] [Google Scholar]
- 47. Nolen‐Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. 2012;8:161–187. [DOI] [PubMed] [Google Scholar]
- 48. Pasquali R. The hypothalamic‐pituitary‐adrenal axis and sex hormones in chronic stress and obesity: pathophysiological and clinical aspects. Ann N Y Acad Sci. 2012;1264:20–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Steptoe A, Kivimaki M, Lowe G, Rumley A, Hamer M. Blood pressure and fibrinogen responses to mental stress as predictors of incident hypertension over an 8‐year period. Ann Behav Med. 2016;50:898–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Muhajid MS, Palaniappan L, Taylor HA Jr, Willis M, Yancy CW; on behalf of the American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council . Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 51. Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta‐analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110:1711–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: long‐term mortality and health status outcomes. J Am Coll Cardiol. 2012;60:1756–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D'Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, Bueno H, Beltrame JF, Krumholz HM. Sex differences in perceived stress and early recovery in young and middle‐aged patients with acute myocardial infarction. Circulation. 2015;131:614–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lewis TT, Cogburn CD, Williams DR. Self‐reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol. 2015;11:407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shallcross AJ, Spruill TM. The protective role of mindfulness in the relationship between perceived discrimination and depression. Mindfulness. 2018;9:1100–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: systematic review and meta‐analysis. J Psychiatr Res. 2017;95:156–178. [DOI] [PubMed] [Google Scholar]
- 58. Woods‐Giscombe CL, Gaylord SA. The cultural relevance of mindfulness meditation as a health intervention for African Americans: implications for reducing stress‐related health disparities. J Holist Nurs. 2014;32:147–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of JHS Participants Without Hypertension at Baseline Who Were Included and Excluded From Analysis Sample
Table S2. Risk Ratios for Incident Hypertension Associated With Chronic Stress, Adjusted for Depressed Mood and Anxiety Over Time


