Abstract
Background
Recent randomized controlled clinical trials have provided solid evidence that mechanical thrombectomy (MT) coupled with best medical therapy (BMT) improve functional outcomes of acute ischemic stroke patients with large vessel occlusion compared with BMT alone. However, they provided inconclusive evidence on the benefit of MT on mortality.
Methods and Results
We evaluated the association of MT+BMT compared with BMT with the risk of 3‐month mortality using aggregate data from all available randomized controlled clinical trials. We also sought to identify potential predictors on the mortality risk and performed univariate meta‐regression analyses. Our literature search identified 11 eligible randomized controlled clinical trials, including a total of 2460 patients. The pooled rates of 3‐month mortality were 15% (95% CI:12%–19%) and 19% (95% CI:16%–23%), respectively, in the MT+BMT and BMT groups. In the overall analysis MT+BMT was associated with a significantly lower risk for 3‐month mortality compared with BMT (risk ratio=0.83, 95% CI:0.69–0.99; P=0.04), without heterogeneity across included studies (I2=3%, P for Cochran Q=0.41). No evidence of publication bias was present in funnel plot inspection and Egger statistical test (P=0.762). In meta‐regression analyses no moderating effect on the aforementioned association was detected with patient age (P=0.254), sex (P=0.702), admission systolic blood pressure (P=0.601), admission glucose (P=0.277), onset‐to‐groin puncture time (P=0.985), administration of intravenous alteplase before MT (P=0.804), MT under general anesthesia (P=0.735), and successful reperfusion following MT (P=0.663).
Conclusions
Our meta‐analysis provides evidence that MT+BMT reduces the risk of 3‐month mortality compared with BMT alone. This association appears not to be moderated by individual patient or procedural characteristics.
Keywords: ischemic stroke, mortality, thrombectomy
Subject Categories: Ischemic Stroke
Clinical Perspective
What Is New?
Recent randomized controlled clinical trials have provided inconclusive evidence on the benefit of mechanical thrombectomy (MT) on mortality of patients with acute ischemic stroke attributable to large vessel occlusion.
Our meta‐analysis provides evidence that MT reduces by 17% the risk of 3‐month mortality of acute ischemic stroke patients with large vessel occlusion.
The reduction of mortality risk with MT appears not to be moderated by individual patient or procedural characteristics.
What Are the Clinical Implications?
MT should be performed in 31 acute ischemic stroke patients with large vessel occlusion to save the life of 1 more patient.
MT is also associated with improved functional outcomes, and therefore the reduction in mortality by MT does not seem to be associated with increased likelihood for functional disability.
Introduction
Despite the significant decrease of stroke mortality risk during the past decade, stroke still remains the second global cause of mortality.1 Recent randomized controlled clinical trials (RCTs) have provided solid evidence that mechanical thrombectomy (MT) coupled with best medical therapy (BMT) improve functional outcomes of acute ischemic stroke (AIS) patients with large vessel occlusion (LVO) compared with BMT alone. However, except for one, they were inconclusive on the benefit of MT +BMT on mortality.2
In the present systematic review and meta‐analysis, we evaluated the association of MT+BMT compared with BMT alone with the risk of 3‐month mortality in AIS patients with LVO using data from eligible RCTs.
Methods
The present systematic review and meta‐analysis adheres to the Journal of the American Heart Association's (JAHA) implementation of the Transparency and Openness Promotion guidelines, and is presented according to the Preferred Reporting Items of Systematic Reviews and Meta‐Analyses statement.
We searched for RCTs providing 3‐month mortality rates in LVO patients randomized to MT+BMT or BMT alone. Literature search in MEDLINE, SCOPUS and CENTRAL (the Cochrane Central Register of Controlled Trials) was performed using the following terms in combination: “endovascular therapy,” “endovascular treatment,” “endovascular reperfusion therapy,” “mechanical thrombectomy,” “thrombectomy,” “acute ischemic stroke,” “cerebrovascular ischemia” and “stent retriever,” “thromboaspiration,” “stroke,” and “large vessel occlusion.” The complete algorithm used in MEDLINE database search is available in Data S1. Eligible studies were also sourced from the hand‐searching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. No language or other search restriction was applied. Last literature search was performed on June 11, 2019.
No time or protocol restrictions were implemented, and thus we included all RCTs providing mortality rates on the 3‐month follow‐up. Per study protocol we excluded from further evaluation all observational studies, case reports, case series, and studies not providing 3‐month mortality rates. We also excluded studies using first generation thrombectomy devices and studies with possibility of enrolling patients without LVO. Reference lists of all articles that met the inclusion criteria and of relevant review articles were examined to identify studies that may have been missed by the initial database search.
We performed quality control for each eligible study with the Cochrane risk of bias assessment tool. Literature search, data abstraction, and bias identification were independently performed by 2 authors (AHK, KM) and all emerging conflicts were resolved after consultation of the senior author (GT).
Using aggregate data from available RCTs we performed random‐effects meta‐analyses on the risk of 3‐month mortality and the probability of functional improvement at 3 months in the ordinal scale between patients randomized to MT+BMT or BMT alone. Mortality rates in each group were calculated after implementing the variance‐stabilizing double arcsine Freeman‐Tukey transformation. Heterogeneity was assessed with the I2 and Cochran Q statistics. Number needed to treat was calculated using the formula number needed to treat=1/[(1‐Risk Ratio) x mortality rate in BMT alone group].3
To identify potential predictors of mortality risk we performed univariable meta‐regression analyses for all baseline characteristics reported as percentages or mean values (for continuous variables) and being provided in ≥10 publications. Publication bias across individual studies was graphically evaluated by funnel plot inspection and with the Egger statistical test.
All statistical analyses were conducted using the Cochrane Collaboration's Review Manager (RevMan 5.3) Software Package (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and the Stata Statistical Software Release 13 for Windows (College Station, TX, StataCorp LP).
Data Availability Statement
All data used for analyses are available within the main manuscript and its associated supplemental file.
Results
Our literature search identified 11 eligible RCTs, including a total of 2460 patients (Figure S1).2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Excluded studies with reasons for exclusion are outlined in Table S1. Patient characteristics receiving MT+BMT or BMT alone are summarized in Table. Risk of bias was considered low in most domains, except for the risk of performance bias because of the open blinded design (Figures S2 and S3), while marked as unclear in the corresponding domains of one RCT that could not be sufficiently assessed because of the lack of full‐text publications at the time of our literature search.9
Table 1.
Characteristics of patients randomized to receive mechanical thrombectomy within included studies
| Study Name | Publishing, y | Enrollment, y | n, Patients | Mean Age (y) | Women (%) | Median NIHSS Score | Median ASPECTS Score | IVT Pretreatment (%) | General Anesthesia (%) | Mean/Median SBP | Mean/Median Glucose (mmol/L) | Mean/Median Onset to Groin Puncture (min) | Successful Reperfusion (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DAWN4 | 2017 | 2014 to 2017 | 107 | 69.4 | 61 | 17 | N/A | 5 | 10 | 147 | 6.9 | 768 | 84 |
| DEFUSE 35 | 2018 | 2016 to 2017 | 92 | 70 | 50 | 16 | 8 | 11 | 28 | N/A | N/A | 688 | 76 |
| ESCAPE2 | 2015 | 2013 to 2014 | 164 | 71 | 52.1 | 16 | 9 | 72.7 | 9.1 | 147 | 6.6 | 185 | 72.4 |
| EXTEND‐IA6 | 2015 | 2012 to 2014 | 35 | 70.2 | 51 | 13 | N/A | 100 | 36 | N/A | 7.6 | 210 | 86 |
| MR CLEAN7 | 2014 | 2010 to 2014 | 233 | 65.8 | 42.1 | 17 | 9 | 87.1 | 37.8 | 146 | N/A | 260 | 58.7 |
| PISTE8 | 2017 | 2013 to 2015 | 33 | 67 | 61 | 18 | 9 | 100 | 31 | 147 | 8 | 209 | 87 |
| RESILIENT9 | N/A | 2017 to 2019 | 111 | 65 | 46 | 18 | 8 | 69 | N/A | N/A | N/A | 170 | 75 |
| REVASCAT10 | 2015 | 2012 to 2014 | 103 | 65.7 | 46.6 | 17 | 7 | 68 | 6.7 | 142 | 6.8 | 269 | 65.7 |
| SWIFT PRIME11 | 2015 | 2012 to 2014 | 98 | 65 | 45 | 17 | 9 | 100 | 37 | N/A | 7.3 | 224 | 88 |
| THERAPY12 | 2016 | 2012 to 2014 | 50 | 67 | 38 | 17 | 7.5 | 100 | 64 | 148 | 6.2 | 227 | 73 |
| THRACE13 | 2016 | 2010 to 2015 | 202 | 66 | 43 | 18 | N/A | 100 | 49 | 140 | 6.7 | 250 | 69 |
ASPECTS indicates Alberta stroke program early CT score; DAWN, DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake‐Up and Late Presenting Strokes Undergoing Neurointervention with Trevo; DEFUSE, Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke; ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times; EXTEND‐IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra‐Arterial; IVT, intravenous thrombolysis; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; N/A, not available; NIHSS, National Institutes of Health Stroke Scale; PISTE, Pragmatic Ischaemic Stroke Thrombectomy Evaluation; RESILIENT, Randomisation of endovascular treatment with stent‐retriever and/or thromboaspiration versus best medical therapy with acute ischaemic stroke due to large vessel occlusion; REVASCAT, Randomized Trial of Revascularization with Solitaire FR Device versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset; SBP, systolic blood pressure; SWIFT PRIME, Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System’s Safety and Effectiveness in the Treatment of Acute Stroke; THRACE, Thrombectomie des Artères Cerebrales.
In the overall analysis, MT+BMT was associated with a significantly lower risk of all‐cause mortality at 3 months compared with BMT alone (risk ratio=0.83, 95% CI: 0.69–0.99; P=0.04; Figure 1), without heterogeneity across the included studies (I2=3%, P for Cochran Q=0.41). No evidence of publication bias was present in both funnel plot inspection (Figure S4) and Egger statistical test (P=0.762). The pooled rates of 3‐month mortality were 15% (95% CI: 12%–19%; Figure S5) and 19% (95% CI: 16%–23%; Figure S6), respectively, in the MT+BMT and BMT alone groups. MT+BMT was also associated with a higher probability of functional improvement in the whole distribution of the modified Rankin Scale scores at 3 months (common odds ratio=2.13, 95% CI: 1.77–2.57), with no significant heterogeneity within studies (I2=38%, P for Cochran Q=0.10; Figure 2).
Figure 1.
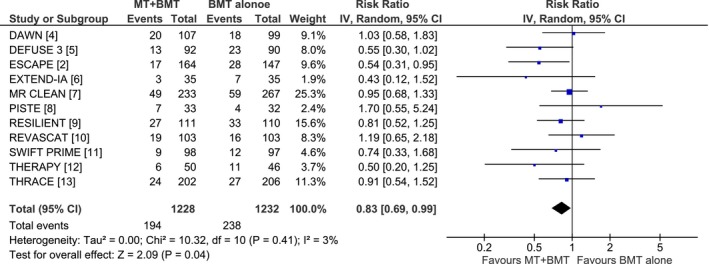
Forest plot on the risk of all‐cause mortality at 3 months between patients randomized to mechanical thrombectomy plus best medical treatment or best medical treatment alone. BMT indicates best medical therapy; DAWN, DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake‐Up and Late Presenting Strokes Undergoing Neurointervention with Trevo; DEFUSE, Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke; ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times; EXTEND‐IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra‐Arterial; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; MT, mechanical thrombectomy; PISTE, Pragmatic Ischaemic Stroke Thrombectomy Evaluation; RESILIENT, Randomisation of endovascular treatment with stent‐retriever and/or thromboaspiration versus best medical therapy with acute ischaemic stroke due to large vessel occlusion; REVASCAT, Randomized Trial of Revascularization with Solitaire FR Device versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset; SWIFT PRIME, Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System's Safety and Effectiveness in the Treatment of Acute Stroke; THRACE, Thrombectomie des Artères Cerebrales.
Figure 2.
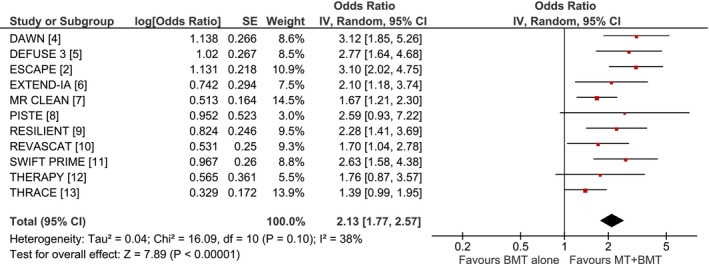
Forest plot on the probability of functional improvement at 3 months between patients randomized to mechanical thrombectomy plus best medical treatment vs best medical treatment alone. BMT indicates best medical therapy; DAWN, DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake‐Up and Late Presenting Strokes Undergoing Neurointervention with Trevo; DEFUSE, Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke; ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times; EXTEND‐IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra‐Arterial; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; MT, mechanical thrombectomy; PISTE, Pragmatic Ischaemic Stroke Thrombectomy Evaluation; RESILIENT, Randomisation of endovascular treatment with stent‐retriever and/or thromboaspiration versus best medical therapy with acute ischaemic stroke due to large vessel occlusion; REVASCAT, Randomized Trial of Revascularization with Solitaire FR Device versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset; SWIFT PRIME, Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System's Safety and Effectiveness in the Treatment of Acute Stroke; THRACE, Thrombectomie des Artères Cerebrales.
In meta‐regression analyses (Table S2) no moderating effect on the aforementioned association was detected with patient age (P=0.254), sex (P=0.702), admission systolic blood pressure (P=0.601), admission glucose (P=0.277), onset‐to‐groin puncture time (P=0.985), administration of intravenous alteplase before MT (P=0.804), MT under general anesthesia (P=0.735), and successful reperfusion following MT (P=0.663).
Discussion
Our meta‐analysis provides evidence that MT coupled with BMT reduce the risk of 3‐month mortality. This association appears not to be moderated by individual patient or procedural characteristics. Based on the risk reduction and pooled 3‐month mortality rates of BMT (19%) in the 11 RCTs, it appears that MT should be performed in 31 AIS patients with LVO in addition to BMT to save the life of 1 additional patient. MT was also associated with improved functional outcomes across all ranks of modified Rankin Scale (ordinal shift analysis), and therefore the reduction in mortality by MT does not seem to be associated with increased likelihood for functional disability.
Our results are in accordance with a previous nationwide US study suggesting a steady decrease in the mortality risk of AIS patients after the introduction of MT.14 Although numerous clinical and procedural parameters have been reported as potential predictors of all‐cause mortality risk following MT, we uncovered no moderating effect in our meta‐regression analyses. Despite the fact that futile recanalization was associated with increased mortality risk in a North‐American stroke registry, proximal vessel occlusion, high National Institutes of Health Stroke Scale scores, and the need for rescue therapy emerged as the only independent predictors of mortality, posing an increased risk independent of successful reperfusion.15
The present meta‐analysis is the first to date to have the adequate statistical power to answer the question on the impact of MT on 3‐month mortality (Table S3). Despite the strengths of the present report several limitations also need to be acknowledged. First, it should be highlighted that we combined studies with heterogeneous clinical and neuroimaging inclusion criteria to provide an estimate of the cumulative impact of MT on all‐cause mortality in different settings. Despite the disparities between study protocols of included studies, no evidence of heterogeneity was detected between study estimates. Second, it should be acknowledged that we were unable to assess the causes of mortality in included RCTs that further limited conducting subgroup analyses according to the corresponding cause (ie, cardiovascular mortality versus mortality associated with neurological deterioration). Finally, the lack of significant associations in meta‐regression analyses could also be attributed to the potential presence of aggregation bias (ecological fallacy).
Conclusions
MT combined with BMT provide survival benefits in addition to functional independence in AIS patients with LVO. The relative risk reduction in 3‐month mortality corresponds to 17% with a number needed to treat of 31.
Sources of Funding
Dr Katsanos has been supported by a European Academy of Neurology Research Fellowship.
Disclosures
Dr Cordonnier reports personal fees from Boehringer‐Ingelheim during the conduct of the study; personal fees from Biogen and grants from French ministry of health outside the submitted work; and is a member of the DSMB (Data and Safety Monitoring Board) for ATTEST‐2 (Alteplase‐Tenecteplase Trial Evaluation for Stroke Thrombolysis) trial (unpaid). Dr Schellinger received honoraria and speaker fees from Boehringer Ingelheim and Medtronic, as well as honoraria for service as expert witness appointed by German federal courts. Dr Tsivgoulis received honoraria and speaker fees from Boehringer Ingelheim and Medtronic. The remaining authors have no disclosures to report.
Supporting information
Data S1. Complete Search Algorithm Used in MEDLINE Search.
Table S1. Excluded Studies From the Meta‐Analysis With Reason(s) for Exclusion
Table S2. Meta‐Regression Analyses on the Association of all‐Cause Mortality at 3 Months With Patient and Procedure Characteristics
Table S3. Overview of Meta‐Analyses on the Association of Mechanical Thrombectomy With 3‐Month Mortality According to Sample Size
Figure S1. Flowchart presenting the selection of eligible studies.
Figure S2. Risk of bias summary that reviews authors’ judgments about each risk of bias item for each included study.
Figure S3. Risk of bias graph that reviews authors’ judgments about each risk of bias item presented as percentages across all included studies.
Figure S4. Funnel plot of included studies.
Figure S5. Mortality rate in patients receiving mechanical thrombectomy plus best medical treatment, calculated using double arcsine Freeman‐Tukey transformation.
Figure S6. Mortality rate in patients receiving best medical treatment alone, calculated using double arcsine Freeman‐Tukey transformation.
(J Am Heart Assoc. 2019;8:e014425 DOI: 10.1161/JAHA.119.014425.)
References
- 1. Thrift AG, Thayabaranathan T, Howard G, Howard VJ, Rothwell PM, Feigin VL, Norrving B, Donnan GA, Cadilhac DA. Global stroke statistics. Int J Stroke. 2017;12:13–32. [DOI] [PubMed] [Google Scholar]
- 2. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators . Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. [DOI] [PubMed] [Google Scholar]
- 3. Mendes D, Alves C, Batel‐Marques F. Number needed to treat (NNT) in clinical literature: an appraisal. BMC Med. 2017;15:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG; DAWN Trial Investigators . Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21. [DOI] [PubMed] [Google Scholar]
- 5. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega‐Gutierrez S, McTaggart RA, Torbey MT, Kim‐Tenser M, Leslie‐Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG; DEFUSE 3 Investigators . Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND‐IA Investigators . Endovascular therapy for ischemic stroke with perfusion‐imaging selection. N Engl J Med. 2015;372:1009–1018. [DOI] [PubMed] [Google Scholar]
- 7. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg‐Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20. [DOI] [PubMed] [Google Scholar]
- 8. Muir KW, Ford GA, Messow CM, Ford I, Murray A, Clifton A, Brown MM, Madigan J, Lenthall R, Robertson F, Dixit A, Cloud GC, Wardlaw J, Freeman J, White P; PISTE Investigators . Endovascular therapy for acute ischaemic stroke: the Pragmatic Ischaemic Stroke Thrombectomy Evaluation (PISTE) randomised, controlled trial. J Neurol Neurosurg Psychiatry. 2017;88:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Martins S, Mont'Alvern F, Pontes‐Neto O, Rebello LC, Silva GS, Lima F, Abud DG, de Sousa Mendes Parente B, Frudit ME, de Barros Faria M, de Carvalho JJF, Zetola VF, de Assis Barbosa L, Cardoso FB, de Souza AC, Carbonera LA, Filho JO, Bezerra D, Liebeskind D, Nogueira RG. Randomization of endovascular treatment with stent‐retriever and/or thromboaspiration vs. best medical therapy in acute ischemics stroke due to large vessel occlusion trial (RESILIENT): final results (ESOC19‐2403). Eur Stroke J. 2019;4:781. [Google Scholar]
- 10. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López‐Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez‐Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A; REVASCAT Trial Investigators . Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306. [DOI] [PubMed] [Google Scholar]
- 11. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators . Stent‐retriever thrombectomy after intravenous t‐PA vs. t‐PA alone in stroke. N Engl J Med. 2015;372:2285–2295. [DOI] [PubMed] [Google Scholar]
- 12. Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D, Frei D, Shownkeen H, Budzik R, Ajani ZA, Grossman A, Altschul D, McDougall C, Blake L, Fitzsimmons BF, Yavagal D, Terry J, Farkas J, Lee SK, Baxter B, Wiesmann M, Knauth M, Heck D, Hussain S, Chiu D, Alexander MJ, Malisch T, Kirmani J, Miskolczi L, Khatri P; THERAPY Trial Investigators . Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke. 2016;47:2331–2338. [DOI] [PubMed] [Google Scholar]
- 13. Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F; THRACE investigators . Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–1147. [DOI] [PubMed] [Google Scholar]
- 14. Villwock MR, Padalino DJ, Deshaies EM. Trends in mortality following mechanical thrombectomy for the treatment of acute ischemic stroke in the USA. J Neurointerv Surg. 2016;8:457–460. [DOI] [PubMed] [Google Scholar]
- 15. Linfante I, Walker GR, Castonguay AC, Dabus G, Starosciak AK, Yoo AJ, Abou‐Chebl A, Britz GW, Marden FA, Alvarez A, Gupta R, Sun CH, Martin C, Holloway WE, Mueller‐Kronast N, English JD, Malisch TW, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Janardhan V, Shaltoni H, Novakovic R, Chen PR, Kaushal R, Nanda A, Issa MA, Nogueira RG, Zaidat OO. Predictors of mortality in acute ischemic stroke intervention: analysis of the North American solitaire acute stroke registry. Stroke. 2015;46:2305–2308. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Complete Search Algorithm Used in MEDLINE Search.
Table S1. Excluded Studies From the Meta‐Analysis With Reason(s) for Exclusion
Table S2. Meta‐Regression Analyses on the Association of all‐Cause Mortality at 3 Months With Patient and Procedure Characteristics
Table S3. Overview of Meta‐Analyses on the Association of Mechanical Thrombectomy With 3‐Month Mortality According to Sample Size
Figure S1. Flowchart presenting the selection of eligible studies.
Figure S2. Risk of bias summary that reviews authors’ judgments about each risk of bias item for each included study.
Figure S3. Risk of bias graph that reviews authors’ judgments about each risk of bias item presented as percentages across all included studies.
Figure S4. Funnel plot of included studies.
Figure S5. Mortality rate in patients receiving mechanical thrombectomy plus best medical treatment, calculated using double arcsine Freeman‐Tukey transformation.
Figure S6. Mortality rate in patients receiving best medical treatment alone, calculated using double arcsine Freeman‐Tukey transformation.
Data Availability Statement
All data used for analyses are available within the main manuscript and its associated supplemental file.


