Abstract
Background
Off‐hour presentation can affect treatment delay and clinical outcomes in endovascular therapy (EVT) for acute ischemic stroke. We aimed to examine the treatment delays and clinical outcomes of EVT between on‐ and off‐hour admission and to evaluate the effect of hospital procedure volume and the number of neurointerventionalists on off‐hour EVT.
Methods and Results
From a multicenter registry, we identified patients who were treated with EVT within 12 hours of symptom. Annual hospital procedure volume was divided as low (<30), medium (30–60), and high (>60). The effect of the number of neurointerventionalists and annual hospital procedure volume on clinical outcome was estimated by the generalized estimation equation. Of the 31 133 stroke patients, 1564 patients met the eligibility criteria (mean age: 69±12 years; median baseline National Institutes of Health stroke scale score, 15 [interquartile range, 10–19]). Of 1564 patients, 893 (57.1%) arrived during off‐hour. The off‐hour patients had greater median door‐to‐puncture time (110 versus 95 minutes; P<0.001) compared with on‐hour patients. Despite the treatment delay, the functional outcome at 3 months did not differ between off‐ and on‐hour (odds ratio with 95% CI for 3‐month modified Rankin Scale 0–2, 0.99 [0.78–1.25]; P=0.90). The presence of three neurointerventionalists was significantly associated with favorable outcomes at 3 months during on‐ and off‐hour (2.07 [1.53–2.81]; P<0.001). The association was not observed for annual hospital procedural volume and the functional outcomes.
Conclusions
The number of neurointerventionalists was more crucial to effective around‐the‐clock EVT for acute stroke patients than hospital procedural volume.
Keywords: hospital performance, interventional neuroradiology, stroke, stroke care, thrombectomy
Subject Categories: Quality and Outcomes, Ischemic Stroke, Revascularization, Cerebrovascular Procedures
Clinical Perspective
What Is New?
The greater number of neurointerventionalists per hospital was associated with increased emergent endovascular therapy (EVT) service with reduced door‐to‐puncture time during off‐hour for patients with acute ischemic stroke.
The increasing number of neurointerventionalists per hospital was also significantly associated with favorable clinical outcomes at 3 months after the EVT.
What Are the Clinical Implications?
At the hospital level, an appropriate number of neurointerventionalists are required to provide effective around‐the‐clock EVT for patients with acute ischemic stroke regardless of the time of day.
A balance between a sufficient case volume to maintain competence and an excessive case volume that could lead to exhaustion of neurointerventionalists should be considered in estimating the number of neurointerventionalists.
In addition to hospital procedural volume, a minimum number of neurointerventionalists providing EVT should be considered as a new requirement for designating comprehensive stroke center where the majority of EVT takes place.
Intravenous recombinant tissue plasminogen activator administered within 4.5 hours after symptom onset significantly improved clinical outcomes of patients with acute ischemic stroke, and earlier treatment with tissue plasminogen activator showed more‐significant benefit.1
Recently, endovascular therapy (EVT) showed significant clinical benefit among patients with acute ischemic stroke attributable to large vessel occlusion when the procedure was performed within 6 hours after the onset of stroke symptoms. The benefit correlated well with a lesser time delay from symptom onset to reperfusion.2 To be a successful EVT, it needs an experienced stroke endovascular team which is ready for 24/7. Because of a limited number of patients requiring such treatment among acute stroke patients, even large stroke centers could not have enough workforce responsible for around‐the‐clock EVT, which might lead to a treatment gap during off‐hour. Previous research reported delayed door‐to‐recanalization time or picture‐to‐recanalization time in patients who received EVT during off‐hour compared with those treated during on‐hour.3, 4, 5 Unfortunately, all the previous studies were small‐sized, single‐center research, and they had not investigated the effect of hospital procedure volume or number of neurointerventionalists on treatment delay and outcomes during off‐hour.
In the present study, we aimed to investigate the treatment delays and clinical outcomes of EVT between on‐ and off‐hour admission using a large multicenter stroke registry and also to evaluate the effect of hospital procedure volume and number of neurointerventionalists on off‐hour EVT.
Methods
The data and materials used in the present study are available from the corresponding author on request.
Study Design and Data Sources
In this study, we used data of consecutive patients enrolled in the CRCS‐K (Clinical Research Collaboration for Stroke in Korea). It is a web‐based, ongoing, prospective, multicenter registry of patients with acute ischemic stroke. The registry started enrolling patients since 2008, and as of January 2018, 15 academic or regional stroke centers in South Korea have participated in the registry. Design, structure, and case characteristics of the CRCS‐K registry have been published previously.6, 7 This study was approved by the institutional review boards of all participating centers with a waiver of informed consent of individual patients because of study subject anonymity and minimal risk to participants. Between January 2010 and December 2015, we identified study participants using the following criteria from 12 hospitals; (1) acute ischemic stroke ≥18 years; (2) treated with EVT at the study hospitals within 12 hours of symptom onset. We excluded patients (1) who did not have exact time information on EVT, (2) whose functional status at 3 months after the stroke was not available.
Clinical Data and Outcomes
From the registry, we obtained demographic characteristics, vascular risk factors, prestroke medications, baseline National Institutes of Health Stroke Scale score, ischemic stroke subtypes, acute treatment, exact time information for hospital arrival, cranial imaging, groin puncture, final cerebral angiography at the end of the EVT, laboratory findings, symptomatic hemorrhagic transformation (SHT) during admission, and 3‐month modified Rankin Scale (mRS) score. The onset time for unclear‐onset stroke in this study was defined as the last‐seen‐normal time. Using the above time information, we calculated onset‐to‐door, door‐to‐puncture, door‐to‐image, image‐to‐puncture, and procedural time (from groin puncture to the final angiography). On‐hour was defined as weekdays between 8:00 am to 6:00 pm, and off‐hour was defined as 6:00 pm to 8:00 am for weekdays and all days for weekends and national holidays. Ischemic stroke was classified as large‐artery atherosclerosis, small‐vessel occlusion, cardioembolism, or undetermined etiology/other determined etiology using the TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification with slight modification.8, 9 The SHT was defined using the criteria suggested by the ECASS (European Cooperative Acute Stroke Study) III.10 Primary outcome was dichotomized 3‐month mRS score (mRS 0–2 versus mRS 3–6). For secondary outcomes, we used the distribution of the mRS score and SHT during admission. For ordinal scale analysis, the mRS scores were converted to 6 categories by collapsing Seok 5 and mRS 6 into a single level of extreme disability or death.
Hospital Procedural Volume and Number of Neurointerventionalists
Annual hospital EVT volume was calculated for each year, and it was classified as low (<30), medium (30–60), and high (>60) for the analyses. Low‐volume threshold was defined as at 30 EVT procedures in accord with the annual number of acute ischemic stroke treatments required for accreditation of a neuroendovascular surgery program in the United States.11 The number of neurointerventionalists, neurointerventional technologists, and dedicated nurses for EVT procedures was collected for each year from the hospitals. In South Korea, neurointerventionalists receive emergency calls only from the hospital where he or she is employed. If ≥2 patients who required the emergency procedure arrive at the hospital at the same time and the hospital has only 1 neurointerventionalist, 1 of the patients has to be transferred to another hospital where the treatment is possible.
Statistical Analysis
Data were summarized as mean±SD or median (interquartile range; IQR) for continuous variables and as number (%) for categorical variables. For missing values, simple imputation with median values was used for continuous variables with missing <10% of the total observations except for the time variables. Variables with missing >10% of total observations were excluded in the analysis. For the correlation between continuous variables, we used the Spearman test. Baseline characteristics between patients treated during on‐hour and those treated during off‐hour were compared using Pearson's chi‐square test, Fisher's exact test, Student's t test, or Wilcoxon's rank‐sum test according to the characteristics of the variables. For hospital‐level data analysis, we created a hospital‐year tier for each hospital for each year.
For unadjusted outcome analyses, the chi‐square test or Fisher's exact test was used for binary outcomes. We used a generalized estimation equation for the binary outcomes and a multilevel ordered logistic regression analysis for the ordinal outcome to evaluate the independent effects of hospital‐level variables on the outcomes, while also adjusting for patient‐level variables including on‐ versus off‐hour presentation. To investigate the possible mediation effect of shortened treatment time on the outcomes, a mediation analysis was done using ldecomp command, which was developed for estimating direct and indirect effects in a logit model.12 All statistical analyses were performed using Stata data analysis software (Version 15.1; StataCorp LP, College Station, TX). In all analyses, P<0.05 was considered statistically significant.
Results
Characteristics of the Patients
Of the 31 133 stroke patients who were admitted to 1 of the 12 participating centers between January 2010 and December 2015, 1564 patients met the eligibility criteria (Figure 1). They had a mean age of 69±12 years, and median baseline National Institutes of Health Stroke Scale score was 15 (IQR, 10–19). Of 1564 patients, 893 patients (57.1%) visited the hospitals during off‐hour. Compared with the patients visited during on‐hour, they were slightly younger and more frequently had unclear stroke onset time. However, they showed no significant differences in baseline National Institutes of Health Stroke Scale score, ischemic stroke subtype, and vascular risk factors except for atrial fibrillation (Table 1).
Figure 1.
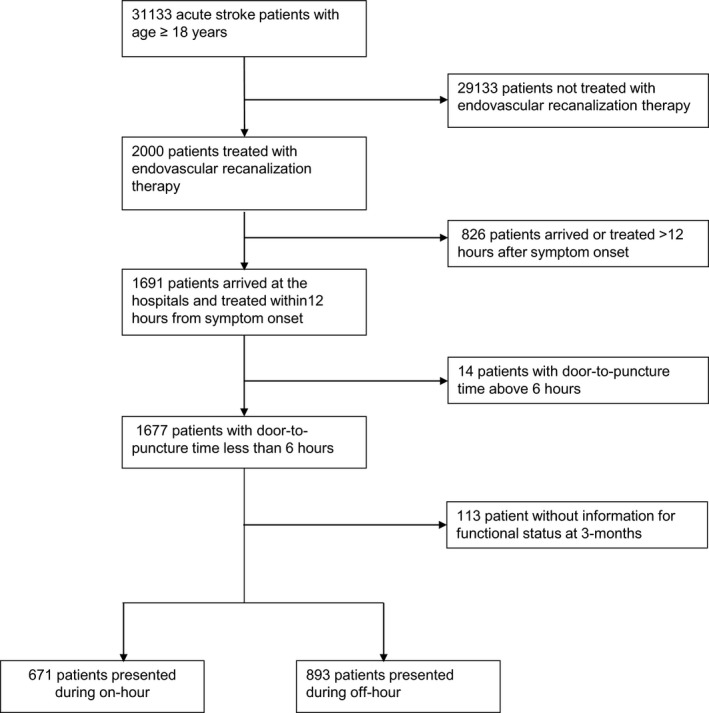
Flow diagram of enrollment.
Table 1.
Characteristics of the Patients
| On‐Hour (N=671) | Off‐Hour (N=893) | Total (N=1564) | P Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, y | 69.6±11.8 | 68.4±11.9 | 68.9±11.8 | 0.045 |
| Male | 356 (53.1) | 512 (57.3) | 868 (55.5) | 0.092 |
| Risk factors | ||||
| Hypertension | 420 (62.6) | 592 (66.3) | 1012 (64.7) | 0.13 |
| DM | 170 (25.3) | 237 (26.5) | 407 (26.0) | 0.59 |
| Hyperlipidemia | 173 (25.8) | 214 (24.0) | 387 (24.7) | 0.41 |
| Smoking | 124 (18.5) | 184 (20.6) | 308 (19.7) | 0.296 |
| Atrial fibrillation | 321 (47.8) | 476 (53.3) | 797 (51.0) | 0.032 |
| History of stroke | 111 (16.5) | 177 (19.8) | 288 (18.4) | 0.098 |
| History of CAD | 76 (11.3) | 104 (11.6) | 180 (11.5) | 0.845 |
| Laboratory finding | ||||
| Systolic blood pressure, mm Hg | 139.9±26.2 | 142.6±26.5 | 141.5±26.4 | 0.048 |
| Hemoglobin, g/dL | 13.3±2.0 | 13.5±1.9 | 13.4±2.0 | 0.112 |
| Fasting glucose, mg/dL | 127.5±48.1 | 129.3±52.8 | 128.6±50.8 | 0.496 |
| BUN, mg/dL | 17.7±8.3 | 17.3±7.9 | 17.5±8.1 | 0.399 |
| Creatinine, mg/dL | 1.1±1.2 | 1.0±0.7 | 1.0±0.9 | 0.076 |
| Platelet count, k/mm3 | 214.0±70.3 | 206.7±69.8 | 209.8±70.1 | 0.041 |
| LDL cholesterol, mg/dL | 102.1±31.5 | 99.6±34.5 | 100.7±33.2 | 0.148 |
| Stroke characteristics | ||||
| Clear onset | 514 (76.6) | 599 (67.1) | 1113 (71.1) | <0.001 |
| Onset to arrival time, min | 149 (53–208) | 172 (54–247) | 162 (54–224) | 0.002 |
| Baseline NIHSS score | 14 (10–19) | 15 (10–19) | 15 (10–19) | 0.206 |
| Ischemic stroke classification | 0.234 | |||
| LAA | 146 (21.8) | 196 (21.9) | 342 (21.9) | |
| Cardioembolism | 349 (52.0) | 495 (55.4) | 844 (54.0) | |
| Others | 176 (26.2) | 202 (22.6) | 378 (24.2) | |
| IV‐tPA use | 436 (65.0) | 570 (63.8) | 1006 (64.3) | 0.639 |
| Door‐to‐needle timea, min | 38 (28–52) | 39 (29–57) | 38 (29–55) | 0.404 |
Data are N (%), mean±SD or median (IQR). Data were compared using Pearson's chi‐square test, Student's t test, or Wilcoxon's rank‐sum test according to the characteristics of the variables. BUN indicates blood urea nitrogen; CAD, coronary artery disease; DM, diabetes mellitus; IV‐tPA, intravenous tissue plasminogen activator; LAA, large artery atherosclerosis; LDL, low‐density lipoprotein; NIHSS, National Institutes of Health Stroke Scale.
The exact time was not available for 12 patients among 1006 patients who received IV‐tPA.
Off‐Hour Effects on Treatment Delay
The patients that arrived during off‐hour had significantly greater median door‐to‐puncture‐time (DTPT; 110 versus 95 minutes; P<0.001) and resultant greater median onset to puncture time (250 [176–360] versus 220 [160–317] minutes; P<0.001). Exact image time was available for 1052 patients. Median door‐to‐image time did not differ significantly between off‐ and on‐hour (19 [12–29] versus 19 [11–30] minutes; P=0.74). However, the image‐to‐puncture time was delayed ≈17 minutes during off‐hours (90 [67–117] versus 73 [49–105] minutes; P<0.001). Procedure times were available for all patients except for 13, and the median procedure times were also significantly higher in patients that arrived during off‐hour (75 [46–110] versus 67 [41–100] minutes; P<0.001; Table 2).
Table 2.
Time Delays During On‐ and Off‐Hour
| On‐Hour (N=671) | Off‐Hour (N=893) | P Valuea | |
|---|---|---|---|
| Onset‐to‐puncture | |||
| Median (IQR) | 220 (160–317) | 250 (176–360) | <0.001 |
| Mean±SD | 251±128 | 290±152 | <0.001 |
| Door‐to‐puncture | |||
| Median (IQR) | 95 (72–123) | 110 (89–137) | <0.001 |
| Mean±SD | 101±44 | 118±45 | <0.001 |
| Door‐to‐image timeb | |||
| Median (IQR) | 19 (11–30) | 19 (12–29) | 0.74 |
| Mean±SD | 25±22 | 24±22 | 0.65 |
| Image‐to‐puncture timeb | |||
| Median (IQR) | 73 (49–105) | 90 (67–117) | <0.001 |
| Mean±SD | 81±47 | 96±44 | <0.001 |
| Procedural timec | |||
| Median (IQR) | 67 (41–100) | 75 (46–110) | <0.001 |
| Mean±SD | 76±48 | 85±54 | <0.001 |
Data are minutes. IQR indicates interquartile range.
Wilcoxon's rank‐sum test was used for comparing median values, and Student's t test was used for mean values.
Exact image time was available for 1052 patients (460 patients during on‐hour and 592 patients during off‐hour).
Procedure time was available for all patients except for 13 patients.
Effects of Hospital Procedural Volume on Off‐Hour EVT
Median annual hospital EVT volume was 15 (IQR, 6–33), and 34.1% of the patients treated at the hospitals with a volume of the EVT below 30 procedures per year, 23.3% at 30 to 60 procedures per year, and 42.6% at the hospitals offering >60 procedures per year. The annual number of the EVT procedures per hospital showed a significant negative correlation with average DTPT at the hospital level (Spearman's rho=−0.720; P<0.001). Both the DTPT during on‐ and off‐hour showed a significant negative correlation with hospital EVT volume (on‐hour, Spearman's rho=−0.518;P<0.001; off‐hour, Spearman's rho=−0.712; P<0.001). In particular, low‐volume hospitals showed significantly delayed DTPT compared with high‐volume hospitals during both on‐ and off‐hour. However, the DTPT showed a significant difference between low‐ and medium‐volume center only during off‐hour (Figure 2).
Figure 2.
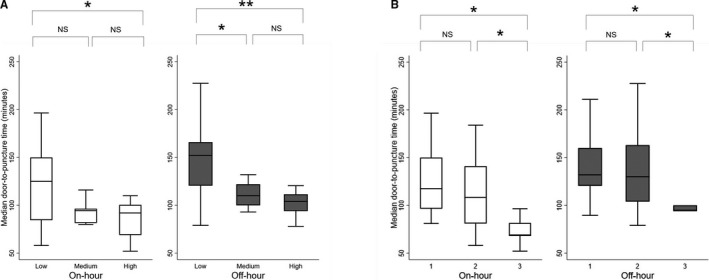
Boxplot showing door‐to‐puncture time (DTPT) during on‐ and off‐hour by annual hospital procedural volume (A) and by the number of neurointerventionalists (B). The DTPT did not show a significant difference between medium‐ and high‐volume centers during both on‐ and off‐hour. The off‐hour DTPT did not show a significant difference between hospitals with a single neurointerventionalist and 2 neurointerventionalists, but showed a significant difference between 1 or 2 neurointerventionalists and 3 neurointerventionalists per hospital. *P<0.05; **P<0.01. NS indicates not nignificant.
Effects of Number of Neurointerventionalists on Off‐Hour EVT
The number of neurointerventionalists per hospital ranged from 1 to 3 per hospital, and the median number of neurointerventional technologists and dedicated nurses for 64 hospital‐year was 2.0 (2.0–4.5) and 2.5 (2.0–4.0). The number of neurointerventional technologists and dedicated nurses did not differ between the hospitals with a single neurointerventionalist and 2 neurointeventionalists. However, the total number of technologists and dedicated nurses were significantly greater for the hospitals with 3 neurointerventionalists than those with 1 or 2 neurointerventionalists (median with IQR, 14 [14–14] versus 4 [3.5–8]; P=0.002). Of 1564 patients, 36.3% of the total EVT procedures were done at hospitals with a single neurointerventionalist, 41.6% at hospitals with 2 neurointerventionalists, and 22.2% at hospitals with 3 neurointerventionalists. The average annual volume of the EVT procedures per neurointerventionalist varied widely for a single neurointerventionalist (median annual procedure of 9 [IQR 4–42]), and 32% of the single neurointerventionalists were categorized as medium or high annual hospital procedural volume. The DTPT did not show a significant difference between hospitals with a single neurointerventionalist and 2 neurointerventionalists, but showed a significant difference between 1 or 2 neurointerventionalists and 3 neurointerventionalists per hospital both during on‐ and off‐hour (Figure 2). Interestingly, the proportion of the EVT procedures during off‐hour increased significantly with the number of neurointerventionalists per hospital (P<0.001), but it did not show a significant correlation with hospital EVT volume (P=0.42; Figure 3).
Figure 3.
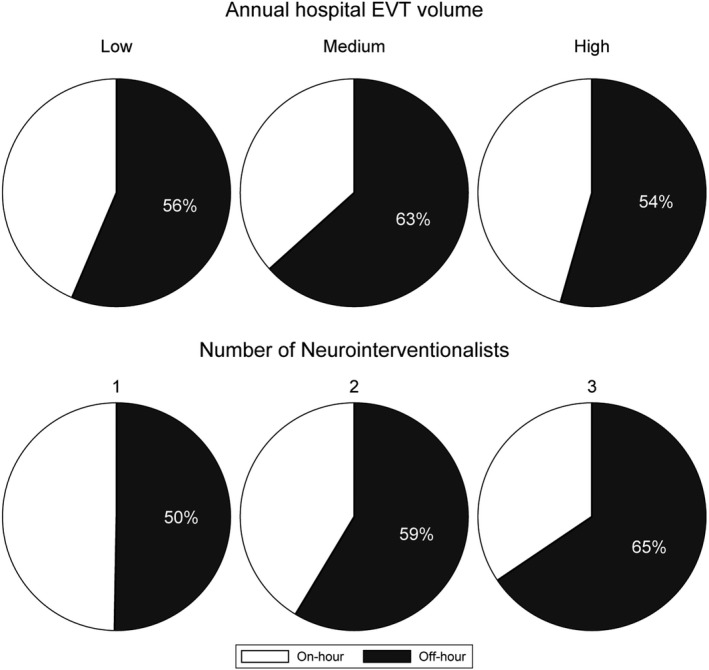
The proportion of the EVT procedures during off‐hour. The proportion increased significantly with the number of neurointerventionalists per hospital (P<0.001), but not with the hospital EVT volume (P=0.47). EVT indicates endovascular therapy.
Outcome Analyses
Despite those significant treatment delays in patients arrived hospitals during off‐hour, they exhibited no significant differences in functional outcomes at 3 months and SHT compared with those patients arrived hospital during on‐hour (odds ratio for off‐ versus on‐hour, 95% CI 3‐month mRS 0 to 2, 0.99 [0.78–1.25], P=0.90; ordinal mRS, 1.00 [0.83–1.21], P=0.98; SHT, 1.06 [0.73–1.54], P=0.76; Figure 4). In the regression analyses adjusted for hospital‐level variables, the presence of 3 neurointerventionalists, but not 2 neurointerventionalists, was associated with significantly better functional outcomes at 3 months during on‐hour compared with a single neurointerventionalist (2.74 [1.57–4.79]; P<0.001). However, both 2 and 3 neurointerventionalists were associated with significantly improved outcomes at 3 months during off‐hour compared with a single neurointerventionalist (2 neurointerventionalists, 1.78 [1.07–2.96]; P=0.026; 3 neurointerventionalists, 1.69 [1.08–2.64]; P=0.021). Overall, the presence of 3 neurointerventionalists was associated with a >2‐fold increased chance of achieving a favorable clinical outcome at 3‐month (2.07 [1.53–2.81]; P<0.001; Table 3). Annual hospital procedural volume was not associated with any clinical outcome in the entire patient population.
Figure 4.

Distribution of modified Rankin Scale score at 3 months after the index stroke by the admission hour. Functional outcomes did not differ significantly between on‐ and off‐hour (P=0.25).
Table 3.
Effect of the Number of Neurointerventionalists on Clinical Outcomes in Regression Analyses
| Clinical Outcome | No. of Neurointerventionalists | On‐Hour | Off‐Hour | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | OR | 95% CI | P Value | ||
| 3‐mo mRS 0 to 2 | Single | Reference | Reference | Reference | ||||||
| 2 | 1.01 | 0.61 to 1.65 | 0.98 | 1.78 | 1.07 to 2.96 | 0.026 | 1.43 | 0.97 to 2.11 | 0.073 | |
| 3 | 2.74 | 1.57 to 4.79 | <0.001 | 1.69 | 1.08 to 2.64 | 0.021 | 2.07 | 1.53 to 2.81 | <0.001 | |
| Ordinal 3‐mo mRS | Single | Reference | Reference | Reference | ||||||
| 2 | 1.01 | 0.69 to 1.49 | 0.95 | 1.61 | 1.14 to 2.26 | 0.007 | 1.34 | 1.04 to 1.72 | 0.025 | |
| 3 | 2.76 | 1.78 to 4.30 | <0.001 | 1.79 | 1.24 to 2.59 | 0.002 | 2.08 | 1.57 to 2.75 | <0.001 | |
| SHT | Single | Reference | Reference | Reference | ||||||
| 2 | 1.30 | 0.44 to 3.83 | 0.63 | 0.97 | 0.46 to 2.04 | 0.93 | 1.09 | 0.57 to 2.08 | 0.80 | |
| 3 | 1.45 | 0.56 to 3.77 | 0.45 | 0.80 | 0.38 to 1.69 | 0.56 | 0.98 | 0.51 to 1.86 | 0.95 | |
All analyses were adjusted for age, sex, prestroke modified Rankin Scale, initial NIHSS score, fasting blood glucose, hemoglobin, hypertension, diabetes mellitus, smoking, atrial fibrillation, use of intravenous tPA, use of a statin, onset to puncture time, procedure time, and annual hospital procedural volume. A generalized estimation equation was used for 3‐month mRS and SHT analyses and a multilevel mixed‐effects ordered logistic regression analysis was used for ordinal 3‐month mRS analyses. mRS indicates modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio; SHT, symptomatic hemorrhagic transformation; tPA, tissue plasminogen activator.
In the mediation analysis, the reduced time from door to finish of the procedure was responsible for around 17.5% (95% CI, 7.1–27.8; P=0.003) of the total effect of the number of neurointeventionalists on the favorable outcomes. The mediation effect was small and nonsignificant during off‐hour (Table 4).
Table 4.
Summary of the Mediation Analysis
| On‐Hour | Off‐Hour | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Indirect effect | 1.28 | 1.12 to 1.47 | <0.001 | 1.09 | 1.02 to 1.17 | 0.015 | 1.13 | 1.07 to 1.21 | <0.001 |
| Direct effect | 1.92 | 1.21 to 3.03 | 0.005 | 1.79 | 1.23 to 2.61 | 0.002 | 1.83 | 1.38 to 2.42 | <0.001 |
| Total effect | 2.46 | 1.56 to 3.88 | <0.001 | 1.95 | 1.34 to 2.84 | <0.001 | 2.09 | 1.57 to 2.77 | <0.001 |
| Mediated proportion | 0.27 | 0.03 to 0.52 | 0.026 | 0.13 | −0.02 to 0.27 | 0.084 | 0.18 | 0.07 to 0.28 | 0.003 |
The effects are ORs for modified Rankin Scale score 0 to 2 at 3 months except for the mediated proportion. OR indicates odds ratio.
Discussion
In the current study of consecutive stroke patients who underwent EVT at 12 stroke centers in South Korea, we found that onset‐to‐puncture, DTPT, and procedural time were significantly longer for patients undergoing treatment during off‐hour, compared with those receiving treatment during on‐hour. Despite this treatment delay during off‐hour, we found no significant difference in clinical outcomes at 3 months after the stroke between on‐ and off‐hour. At the hospital level, the DTPT was correlated well with hospital procedural volume and the number of neurointerventionalists per hospital. The proportion of the EVT procedures during off‐hour increased significantly with the number of neurointerventionalists, but not with the hospital EVT volume. Finally, the presence of ≥2 neurointerventionalists was associated with significantly improved outcomes at 3 months during off‐hour compared with a single neurointerventionalist.
Because the benefit of thrombolytic therapy is significantly associated with time from symptom onset to reperfusion, the treatment should be performed as soon as possible regardless of the time of the patient's visit to the hospital. This study showed an average of a 15‐minute delay of the DTPT during off‐hour. The treatment delay for EVT during off‐hour is frequent in other reports,3, 4 but not universal.5 In this study, the delay would represent the time spent for a commute of the neurointerventionalists and other interventional staffs from their residence to the hospital during off‐hour because the door‐to‐image time and door‐to‐needle time was not different between on‐ and off‐hour in this study. Despite the inevitable treatment delays during off‐hour, the functional outcomes at 3 months did not differ significantly between the patients treated during on‐hour and those treated during off‐hour. Our findings are consistent with the previous research that also found no significant differences in clinical outcomes between on‐ and off‐hour regardless of the presence of treatment delay.3, 4, 5 The patients with unclear‐onset stroke were more frequent during off‐ than on‐hour, and previous studies have already suggested that the substantial proportion of strokes that are evident after sleep occurred in the last few hours before awakening.13, 14 Therefore, the most probable reason could be that the actual onset‐to‐arrival time of patients with unclear‐onset stroke in this study could be shorter than the last‐seen‐normal‐to‐arrival time used in this study.
Physician or hospital case volume is a well‐established factor affecting clinical outcomes in percutaneous coronary intervention as well as carotid stenting or endarterectomy.15, 16, 17, 18 However, only a few studies have examined the role of the number of physicians on the clinical outcome after acute cardiovascular diseases so far. In Japanese patients with acute heart failure and acute myocardial infarction, in‐hospital mortality showed a significant negative correlation with the number of cardiologists per hospital, but not with physician case volume.19, 20 Their results seem to be contrary to the established relationship between case volume and outcome reported in the earlier studies. They speculated that the total number of cardiologists per hospital could better explain the improved quality of care in the urgent illness that required specialized team care. In this study, we found that the number of neurointerventionalists was correlated with shortened DTPT, the proportion of the EVT procedures during off‐hour, and favorable clinical outcome at 3 months after the index stroke. Although hospital EVT volume was correlated with DTPT, it was not independently associated with overall clinical outcome in this study. It should also be noted that the hospital EVT volume was not correlated well with the number of neurointerventionalists in this study because a single neurointerventionalist showed a wide range of case volume. In this study, the hospitals had, at most, 3 neurointerventionalists because EVT procedures are usually required for a very limited number of stroke patients even in a tertiary hospital. In this unique situation, the number of physicians could be a more‐important factor for a patient's outcome than the hospital case volume because it must be a challenging mission for a small number of neurointerventionalists to deal with 24/7 interventional consultations and procedures for patients with acute ischemic stroke.
Currently, the exact number of neurointerventionalists required for 24/7 coverage of endovascular ischemic stroke therapy has not been defined in the recommendation for a comprehensive stroke center.21 A balance between a sufficient case volume to maintain competence and an excessive case volume that could lead to exhaustion of neurointerventionalists should be considered in estimating the number of neurointerventionalists and their minimum volume of cases at both the hospital and physician level.22 Although the DTPT was correlated well with both hospital procedural volume and the number of neurointerventionalists per hospital in this study, the proportion of EVT volume performed during off‐hours did not reach 60% in hospitals with fewer than 3 neurointerventionalists, even though off‐hours would account for >75% of the total hours. Interestingly, the presence of ≥2 neurointerventionalists was associated with significantly improved outcomes at 3 months during off‐hour compared with a single neurointerventionalist, although the number of neurointerventional technologists and dedicated nurses was not different between institutions with a single neurointerventionalist and 2 neurointerventionalists. Therefore, this study showed that an appropriate number of neurointerventionalists was crucial to reducing treatment delay as well as providing effective treatment even during off‐hour.
In this study, the reduced DTPT alone was not able to explain the entire relationship between the number of neurointerventionalists and clinical outcome because the mediation analysis found only a partial mediation effect of the reduced treatment time on the clinical outcomes. It is well known that a physician is vulnerable to burnout, and the physician's burnout can lead to increased medical errors.23, 24 In general, work factors that contribute to physician burnout include excessive workloads, long working hours, specialty choice, frequent call duties (night call or weekend call), time spent at home on work‐related factors, and risk of malpractice suits.24 Among a broad spectrum of medical specialties, neurointerventionalists are experiencing a high rate of burnout recently because of frequent nighttime consultations and procedures that are chased by time for a faster DTPT with the expansion of the EVT indication.25, 26, 27, 28 In addition to reduced treatment time, other factors that led to improved outcome in hospitals with a higher number of neurointerventionalists, such as reduced workload, less chance of burnout, or improved collaboration with other medical staff, should be investigated further in future research.
This study has several limitations. First, though the CRCS‐K registry includes geographically diverse hospitals with annual stroke volumes ranging from 300 to 1000, our results may not be generalizable to other countries with different regional stroke care systems. Nevertheless, the CRCS‐K is the largest, most comprehensive current registry of acute stroke patients available in South Korea. Second, detailed EVT information, such as recanalization status, collateral status, and procedural complications, that may affect the functional outcome was not available in the current analysis. Third, our conclusions may be limited by the lack of assessment of ischemic stroke lesions on computed tomography or magnetic resonance imaging using the Alberta Stroke Program Early CT Score before deciding EVT.
Conclusions and Policy Implications
Onset to treatment time was significantly longer for patients undergoing treatment during off‐hour, and it was correlated well with hospital procedural volume and the number of neurointerventionalists per hospital. The proportion of the EVT procedures during off‐hour increased significantly with the number of neurointerventionalists, but not with hospital EVT volume. Our research is the first to highlight the association between the number of neurointerventionalists and clinical outcome among patients treated with EVT. Therefore, efforts to improve the quality of EVT should ensure that the proportion of patients receiving EVT and clinical outcomes is achieved regardless of the time of day. In addition to hospital procedural volume, a minimum number of neurointerventionalists providing EVT should be considered as a new requirement for designating a comprehensive stroke center where the majority of EVT takes place.
Appendix
Clinical Research Collaboration for Stroke in Korea (CRCS‐K) Investigators
Participating stroke centers and site investigators
Seoul National University Bundang Hospital: Hee‐Joon Bae (director), Moon‐Ku Han, Beom Joon Kim, Jihoon Kang.
Nowon Eulji Medical Center, Eulji University: Jong‐Moo Park, Kyusik Kang.
Eulji University Hospital: Soo Joo Lee, Jae Guk Kim.
Dong‐A University Hospital: Jae‐Kwan Cha, Dae‐Hyun Kim.
Seoul Medical Center: Tai Hwan Park, Sang‐Soon Park, Moo‐Seok Park.
Soonchunhyang University Hospital Seoul: Kyung Bok Lee.
Yeungnam University Medical Center: Jun Lee.
Inje University Ilsan Paik Hospital: Yong‐Jin Cho, Keun‐Sik Hong, Hong‐Kyun Park.
Hallym University Sacred Heart Hospital: Mi‐Sun Oh, Kyung‐Ho Yu, Byung‐Chul Lee.
Dongguk University Ilsan Hospital: Dong‐Eog Kim, Wi‐Sun Ryu.
Chonnam National University Hospital: Joon‐Tae Kim, Ki‐Hyun Cho, Kangho Choi.
Jeju National University Hospital: Jay Chol Choi, Joong‐Goo Kim.
Ulsan University Hospital: Wook‐Joo Kim, Jee Hyun Kwon.
Chungbuk National University Hospital: Dong‐Ick Shin, Kyu Sun Yum.
Keimyung University Dongsan Medical Center: Sung Il Sohn, Jeong‐Ho Hong, Joonsang Yoo.
Hallym University Dongtan Sacred Heart Hospital: Min Uk Jang.
Hallym University Chuncheon Sacred Heart Hospital: Lee Sang‐Hwa.
Chung‐Ang University Hospital: Kwang Yeol Park.
Statistical advisors
June‐Young Lee (Department of Biostatistics, Korea University College of Medicine).
Ji Sung Lee (Clinical Trial Center, Asan Medical Center).
Sources of Funding
This work was supported by a research grant from the Jeju National University Hospital Research Fund of Jeju National University in 2016.
Disclosures
None.
Acknowledgments
Choi conceptualized and designed the study. Choi and J.‐G. Kim reviewed the articles and collected the data. Choi, Bae, S.‐J. Lee, Jong‐Moo Park, T.H. Park, Cho, K.B. Lee, J. Lee, D.‐E. Kim, Jae‐Kwan Cha, J.‐T. Kim, and B.‐C. Lee recruited patients. Choi and D.J. Kim analyzed the data. All authors contributed to data interpretation, write‐up, editing, and revisions of the final manuscript. All authors have contributed to the production of the final version of this manuscript.
(J Am Heart Assoc. 2019;8:e011933 DOI: 10.1161/JAHA.119.011933.)
Contributor Information
Jay Chol Choi, Email: jaychoi@jejunu.ac.kr.
on the behalf of CRCS‐K Investigators:
Moon‐Ku Han, Beom Joon Kim, Jihoon Kang, Kyusik Kang, Jae Guk Kim, Dae‐Hyun Kim, Sang‐Soon Park, Moo‐Seok Park, Keun‐Sik Hong, Hong‐Kyun Park, Mi‐Sun Oh, Kyung‐Ho Yu, Wi‐Sun Ryu, Ki‐Hyun Cho, Kangho Choi, Wook‐Joo Kim, Jee Hyun Kwon, Dong‐Ick Shin, Kyu Sun Yum, Sung Il Sohn, Jeong‐Ho Hong, Joonsang Yoo, Min Uk Jang, Lee Sang‐Hwa, Kwang Yeol Park, June‐Young Lee, and Ji Sung Lee
References
- 1. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, Grotta J, Howard G, Kaste M, Koga M, von Kummer R, Lansberg M, Lindley RI, Murray G, Olivot JM, Parsons M, Tilley B, Toni D, Toyoda K, Wahlgren N, Wardlaw J, Whiteley W, del Zoppo GJ, Baigent C, Sandercock P, Hacke W; Stroke Thrombolysis Trialists’ Collaborative Group . Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta‐analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millan M, Davis SM, Roy D, Thornton J, Roman LS, Ribo M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG; HERMES collaborators . Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. [DOI] [PubMed] [Google Scholar]
- 3. Almekhlafi MA, Hockley A, Desai JA, Nambiar V, Mishra S, Volny O, Eesa M, Demchuk AM, Menon BK, Goyal M. Overcoming the evening/weekend effects on time delays and outcomes of endovascular stroke therapy: the Calgary Stroke Program experience. J Neurointerv Surg. 2014;6:729–732. [DOI] [PubMed] [Google Scholar]
- 4. Mpotsaris A, Kowoll A, Weber W, Kabbasch C, Weber A, Behme D. Endovascular stroke therapy at nighttime and on weekends‐as fast and effective as during normal business hours? J Vasc Interv Neurol. 2015;8:39–45. [PMC free article] [PubMed] [Google Scholar]
- 5. Nikoubashman O, Probst T, Schurmann K, Othman AE, Matz O, Brockmann MA, Muller M, Wiesmann M, Reich A. Weekend effect in endovascular stroke treatment: do treatment decisions, procedural times, and outcome depend on time of admission? J Neurointerv Surg. 2017;9:336–339. [DOI] [PubMed] [Google Scholar]
- 6. Kim BJ, Han MK, Park TH, Park SS, Lee KB, Lee BC, Yu KH, Cha JK, Kim DH, Lee J, Lee SJ, Ko Y, Park JM, Kang K, Cho YJ, Hong KS, Cho KH, Kim JT, Kim DE, Lee JS, Jang MS, Broderick JP, Yoon BW, Bae HJ. Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. Int J Stroke. 2014;9:514–518. [DOI] [PubMed] [Google Scholar]
- 7. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, Cha JK, Kim DH, Nah HW, Han MK, Park TH, Park SS, Lee KB, Lee J, Hong KS, Cho YJ, Lee BC, Yu KH, Oh MS, Kim DE, Ryu WS, Cho KH, Kim JT, Choi JC, Kim WJ, Shin DI, Yeo MJ, Sohn SI, Hong JH, Lee JS, Yoon BW, Bae HJ. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke‐fifth division registry in South Korea. J Stroke. 2015;17:38–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE III. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- 9. Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, Park TH, Park SS, Cho YJ, Hong KS, Lee KB, Lee J, Kim DE, Kim DH, Cha JK, Kim JT, Choi JC, Shin DI, Lee JS, Lee J, Yu KH, Lee BC, Bae HJ. MRI‐based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014;16:161–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. [DOI] [PubMed] [Google Scholar]
- 11. Day AL, Siddiqui AH, Meyers PM, Jovin TG, Derdeyn CP, Hoh BL, Riina H, Linfante I, Zaidat O, Turk A, Howington JU, Mocco J, Ringer AJ, Veznedaroglu E, Khalessi AA, Levy EI, Woo H, Harbaugh R, Giannotta S. Training standards in neuroendovascular surgery: program accreditation and practitioner certification. Stroke. 2017;48:2318–2325. [DOI] [PubMed] [Google Scholar]
- 12. Buis ML. Direct and indirect effects in a logit model. Stata J. 2010;10:11–29. [PMC free article] [PubMed] [Google Scholar]
- 13. Costa R, Pinho J, Alves JN, Amorim JM, Ribeiro M, Ferreira C. Wake‐up stroke and stroke within the therapeutic window for thrombolysis have similar clinical severity, imaging characteristics, and outcome. J Stroke Cerebrovasc Dis. 2016;25:511–514. [DOI] [PubMed] [Google Scholar]
- 14. Dankbaar JW, Bienfait HP, van den Berg C, Bennink E, Horsch AD, van Seeters T, van der Schaaf IC, Kappelle LJ, Velthuis BK; on behalf of the DUST investigators . Wake‐up stroke versus stroke with known onset time: clinical and multimodality CT imaging characteristics. Cerebrovasc Dis. 2018;45:236–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Srinivas VS, Hailpern SM, Koss E, Monrad ES, Alderman MH. Effect of physician volume on the relationship between hospital volume and mortality during primary angioplasty. J Am Coll Cardiol. 2009;53:574–579. [DOI] [PubMed] [Google Scholar]
- 16. Hannan EL, Popp AJ, Tranmer B, Fuestel P, Waldman J, Shah D. Relationship between provider volume and mortality for carotid endarterectomies in New York state. Stroke. 1998;29:2292–2297. [DOI] [PubMed] [Google Scholar]
- 17. Strom JB, Wimmer NJ, Wasfy JH, Kennedy K, Yeh RW. Association between operator procedure volume and patient outcomes in percutaneous coronary intervention: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2014;7:560–566. [DOI] [PubMed] [Google Scholar]
- 18. Nallamothu BK, Gurm HS, Ting HH, Goodney PP, Rogers MA, Curtis JP, Dimick JB, Bates ER, Krumholz HM, Birkmeyer JD. Operator experience and carotid stenting outcomes in Medicare beneficiaries. JAMA. 2011;306:1338–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Park S, Sasaki N, Morishima T, Ikai H, Imanaka Y. The number of cardiologists, case volume, and in‐hospital mortality in acute myocardial infarction patients. Int J Cardiol. 2013;168:4470–4471. [DOI] [PubMed] [Google Scholar]
- 20. Sasaki N, Kunisawa S, Otsubo T, Ikai H, Fushimi K, Yasumura Y, Kimura T, Imanaka Y. The relationship between the number of cardiologists and clinical practice patterns in acute heart failure: a cross‐sectional observational study. BMJ Open. 2014;4:e005988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gorelick PB. Primary and comprehensive stroke centers: history, value and certification criteria. J Stroke. 2013;15:78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zaidat OO, Lazzaro M, McGinley E, Edgell RC, Nguyen T, Linfante I, Janjua N. Demand‐supply of neurointerventionalists for endovascular ischemic stroke therapy. Neurology. 2012;79:S35–S41. [DOI] [PubMed] [Google Scholar]
- 23. West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–1300. [DOI] [PubMed] [Google Scholar]
- 24. Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag J. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. [DOI] [PubMed] [Google Scholar]
- 25. Fargen KM, Arthur AS, Leslie‐Mazwi T, Garner RM, Aschenbrenner CA, Wolfe SQ, Ansari SA, Dabus G, Spiotta A, Mokin M, Linfante I, Mocco J, Hirsch JA. A survey of burnout and professional satisfaction among United States neurointerventionalists. J Neurointerv Surg. 2019. April 11. doi: 10.1136/neurintsurg-2019-014833. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26. Fargen KM, Hirsch JA. Neurointerventionalists, stroke and burnout. J Neurointerv Surg. 2018;10:811–812. [DOI] [PubMed] [Google Scholar]
- 27. Williams MM, Wilson TA, Leslie‐Mazwi T, Hirsch JA, Kellogg RT, Spiotta AM, De Leacy R, Mocco J, Albuquerque FC, Ducruet AF, Arthur A, Srinivasan VM, Kan P, Mokin M, Dumont TM, Reeves A, Singh J, Wolfe SQ, Fargen KM. The burden of neurothrombectomy call: a multicenter prospective study. J Neurointerv Surg. 2018;10:1143–1148. [DOI] [PubMed] [Google Scholar]
- 28. Mokin M, Ansari SA, McTaggart RA, Bulsara KR, Goyal M, Chen M, Fraser JF . Indications for thrombectomy in acute ischemic stroke from emergent large vessel occlusion (ELVO): report of the SNIS Standards and Guidelines Committee. J Neurointerv Surg. 2019;11:215–220. [DOI] [PubMed] [Google Scholar]


