ABSTRACT
Maxillofacial fractures in the pediatric population consist of less than 15% of all facial fractures. Road traffic accidents, sport-related injury, and fall constitutes most common causes for the facial injury. Incidence of the facial fractures is comparatively higher in boys than in girls. In the management of the maxillofacial fractures in pediatric patients, we have to take into consideration the variation in anatomy and physiology between children and adults, as well as the particular stage of growth and dental development. Treatment options can vary from closed reduction to open reduction and internal fixation. In this article, the authors successfully managed the pediatric mandibular fractures by performing bridle wiring with the help of an orthodontic ligature wire.
How to cite this article
Sharma A, Patidar DC, et al. Mandibular Fracture in Children: A New Approach for Management and Review of Literature. Int J Clin Pediatr Dent 2019;12(4):356–359.
Keywords: Bridle wiring, Orthodontic ligature wire, Pediatric facial fracture
INTRODUCTION
Maxillofacial fractures in the pediatric population consist of less than 15% of all facial fractures.1 Their incidences are rare below age five (0.6–1.4%), raises as children commence school and peaks throughout puberty and adolescence owing to increased sport and unsupervised physical activity.1,2
The incidence of facial fractures is higher in boys than in girls all over the world in all age groups. Road traffic accidents, sports injuries, and fall comprise the most frequent causes of facial fractures in children.2,3 Facial fractures are also seen in victims of child abuse.1,2
The aim of the treatment was to achieve the bony union, normal occlusion, restoration of normal form and function, and to avoid impediments to normal growth. Children differ from adults in that the definitive result is determined not solely by the initial management but also by the effect that growth has on form and function over time.4 To achieve the goals of treatment in pediatric maxillofacial fractures, minimal manipulation of the facial skeleton or noninvasive procedures are advisable.4–7
Growth and Development Consideration
The effect of the trauma or treatment on growth and development is the utmost concern while managing the pediatric patients. Also, anatomical and psychological aspect is equally significant, and can have diverse effects on management.6
At birth, the ratio between the cranium and face is 8:1 (which declines to 4:1 by the age of 5 years) and in adults it becomes 2.5:1. In infants, the large cranium protects the face; as the child grows, the cranium-to-face ratio decreases, making the child more prone to facial fractures. During the mixed dentition period, with increasing age and growth of the facial skeleton in a downward and forward direction, the maxillofacial region becomes more prominent and the occurrence of facial fractures rises. Frontal prominence reduces and the facial bones emerge from the shelter of the cranial base.2,8–10
Distinctive to the pediatric growing jaw is the concern of dental development and potential complications and morbidity that occur as a result from the surgical manipulation in the developing teeth region.8 Pediatric maxillofacial complex is also malleable owing to a greater cancellous-to-cortical ratio. Greenstick fractures are more common in children. The osteogenic and bone remodeling potential is also greater in children than in adults.8
CASE DESCRIPTION
In this pediatric maxillofacial trauma series, the authors successfully managed the mandible fracture noninvasively by bridle wiring with the help of an orthodontic ligature wire (28 gauge), which is a novel technique for the management of displaced mandible fracture in children. The details of all cases are given in tabulate form (Table 1).
Table 1.
Series of cases treated by bridle wiring
| S. no. | Patients age (years) | Gender | Mandible fracture site | Left/right | Displacement |
|---|---|---|---|---|---|
| 1 | 7 | M | Parasymphysis | Bilateral | Mild |
| 2 | 6 | M | Parasymphysis | Bilateral | Mild |
| 3 | 6 | M | Parasymphysis | L | Severe |
| 4 | 7 | F | Parasymphysis | L | Mild |
| 5 | 5 | F | Symphysis | NA | Severe |
| 6 | 5 | F | Symphysis | NA | Mild |
| 7 | 6 | M | Parasymphysis | L | Moderate |
| 8 | 8 | M | Symphysis | NA | Moderate |
| 9 | 3 | F | Symphysis | NA | Mild |
| 10 | 3 | F | Parasymphysis | L | Mild |
Case 1
A 7-year-old boy was reported to the emergency department on 16/03/2016 with the chief complaint of pain in the lower jaw. A history of fall from height one day back, no history of loss of consciousness, a seizure or ENT bleed but 2–3 episodes of vomiting were reported. On an extraoral examination, a bruise present over the chin region and a deviation of chin towards the right side was seen. On an intraoral examination, lacerated wound with respect to 72 73 and 82 83 regions was noted (Fig. 1), and on palpation, step deformity was felt with respect to the same region. Malocclusion was present and sublingual hematoma was also noted. After a thorough clinical and radiographic examination (Fig. 2), the patient was diagnosed as having a bilateral mandible parasymphysis fracture and it was planned to manage the condition nonsurgically by means of placing bridle wiring with the help of a ligature wire. Bridle wiring performed with respect to 72 73, 74 75, and 82 83, 84 85 with the help of a 28-gauge orthodontic ligature wire (Figs 3 and 4). The patient was kept on a soft diet and regularly followed up for 3–4 weeks.
Fig. 1.

Preoperative photograph
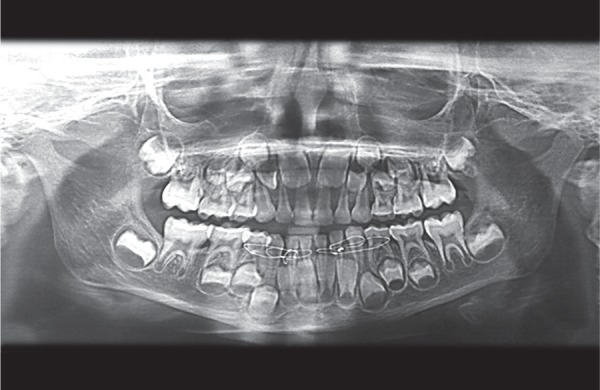
Fig. 2.

Preoperative panoramic radiograph
Fig. 3.

Intraoperative photograph
Fig. 4.
Intraoperative panoramic radiograph
Case 2
A 6-year-old boy was brought to the emergency department with the chief complaint of bleeding from the mouth. The history revealed a fall during playing. On examination, a lacerated wound was present bilaterally in between 72 73 and 82 83, also a sublingual hematoma is noted. The patient was diagnosed to have a bilateral mandible parasymphysis fracture and the condition was successfully managed by bridle wiring with the help of an orthodontic ligature wire.
DISCUSSION
Various studies reported almost a similar data of a lower occurrence of mandibular fractures in children than in adults, ranging from 1% to 15%.1,2,5 The gender allocation exhibited a prominence of boys in all age groups. The incidence raises from birth to 16 years of age.1,2,11 Mandibular fracture is the most common pediatric facial fracture, among them mandibular condyle is the frequently injured site.6,11 The higher occurrence of condylar fractures in children when compared to adults may be described by the high fraction of medullary bone content along with a thin periphery of cortex.1 Concomitant injuries are observed in 25–75% of the children with maxillofacial fractures.1
General considerations for the young injured patient include airway maintenance, fluid and electrolyte balance, and rational nutritional intake throughout treatment.2,12 The same as every trauma patients, primary evaluation and resuscitation must pursue the “ABCs” of advanced trauma life support, with a centre of attention on the unique differences in pediatric anatomy and physiology.6,13,14
Management of the mandibular fracture in pediatric patients is dependent upon the type of fracture and the phase of dental as well as skeletal development. Mandibular growth and development of dentition are the main concerns while treating the pediatric mandible fracture.1,2,5,7,12 The small jaw size, the presence of developing permanent tooth buds, and existing active growth centres significantly increases the risk for managing pediatric mandible fracture.7,11
Children have a higher osteogenic potential and a rapid healing rate when compared to adults. Thus, anatomic reduction must be achieved earlier and immobilization periods must be lesser (two weeks instead of four–six weeks for adults).1,2,12,15 Depending on the type of fracture and the patient's stage of development, immobilization and fixation of the fracture segments can be achieved by means of maxillomandibular fixation (MMF) or internal skeletal fixation or a combination of both these methods.1,2,6,12
Intermaxillary fixation (IMF) using the teeth in pediatric facial fracture patient may be more complex than adults. This may be due to less availability of teeth, resorption of roots of deciduous teeth, surfaces of the teeth are not retentive for etching procedure, and unfavorable form of the crowns of deciduous teeth for the fixation of interdental wires and arch bars.2,7,16 Posnick stated that approximately 42% of mandibular fractures in his series were managed by closed reduction, mainly with the help of maxillomandibular fixation (MMF).3,12
Currently, open reduction and internal fixation (ORIF) have become the standard care for the treatment of displaced pediatric mandible fractures.2,4,7,16 This uses fixation with miniplates, microplates, or bio-degradable plates. Although ORIF provides three-dimensional stability, promotes primary healing, and shortens the treatment time, but several risks are associated with the ORIF for the management of the pediatric mandibular fracture such as damage to the developing tooth buds; however, in a specific age group, plate fixation is possible at the inferior border of the mandible away from the developing tooth germs.7,11 Additionally this also carries the risk of interference with growth, plate migration, and stress shielding owing to the placement of the hardware. Allergic reaction to the metal leads to inflammatory sequelae, which necessitates further elimination of the plating hardware.7,8 Corrosion and freeing of metal ions can also be a cause to take away the internal fixation devices.
However with the use of resorbable osteosynthesis, the risks associated with the use of metal internal fixation devices can be evaded, but still there is a risk of harm to the developing tooth buds owing to drilling for the placement of plating hardware for the fixation of fracture segments.7,17,18
Complications such as postoperative infection, non-union, and malunion are infrequent in children owing to the higher osteogenic potential, rapid healing rate, and less common necessity for open reduction and rigid internal fixation. In addition, a large number of fractures are minimally displaced to undisplaced. However, TMJ dysfunction, restricted condylar translation, deviation upon mouth opening and growth disturbances such as hypoplasia of mandible or asymmetry, and secondary midface deformity usually occur with severe comminuted fractures in pediatric patients.2,7
In conclusive mandibular fractures in a young child, disruption of the periosteum may have an erratic effect on the growth; therefore, whenever intervention is needed, close reduction is favored.7 In a younger pediatric patient, an acrylic splint fixed to the mandible with the help of circummandibular wiring can successfully eliminate the need of IMF.1,11 But to accomplish this, making of impression, acrylic splint, and fixation of this splint through circummandibular wiring are needed, which constitute again an invasive procedure.
Mandibular fracture without any displacement or malocclusion are treated by means of close observation, a liquid-to-soft diet, prevention of physical activities, and medications.1,6 Here the authors have successfully managed the mandibular symphysis or parasymphysis fracture by performing the bridle wiring with the help of a ligature wire, which is a very simple procedure and easy to perform without any need of surgical intervention.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Glazer M, Joshua BZ, et al. Mandibular fracture in children: Analysis of 61 cases and review of the literature. Int J Pediatr Otorhinolaryngol. 2011 Jan;75(1):62–64. doi: 10.1016/j.ijporl.2010.10.008. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Zimmermann CE, Troulis MJ, et al. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2006;35:2–13. doi: 10.1016/j.ijom.2005.09.014. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Posnick JC. Peterson LP, Indresano AT, et al. Principles of oral and maxillofacial surgery. Philadelphia: WB Saunders; 1992. Diagnosis and management of pediatric craniomaxillofacial fractures. pp. 623–640. [Google Scholar]
- 4.Myall RW. Management of Mandibular fractures in children. Oral Maxillofacial Surg Clin North Am. 2009;21(2):197–201. doi: 10.1016/j.coms.2008.12.007. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Singhal R, Singh V, et al. Pediatric maxillofacial injuries-If a new look is required? Int J Pediatr Otorhinolaryngol. 2013;77:1333–1336. doi: 10.1016/j.ijporl.2013.05.028. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Haug HR, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol. 2000;90(2):126–134. doi: 10.1067/moe.2000.107974. DOI: [DOI] [PubMed] [Google Scholar]
- 7.John B, John RR, et al. Management of mandibular body fractures in pediatric patients: A case report with review of literature. Contemp Clin Dent. 2010 Oct;1(4):291–296. doi: 10.4103/0976-237X.76406. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aziz SR, Ziccardi VB. Fonseca RJ. Oral and Maxillofacial Trauma, 4th ed., Missouri: Elsevier St. Loius; 2013. Management of Pediatric Facial Fractures. pp. 735–748. [Google Scholar]
- 9.McGraw BL, Cole RR. Pediatric maxillofacial trauma. Age-related variations in injury. Arch Otolaryngol Head Neck Surg. 1990;116:41–45. doi: 10.1001/archotol.1990.01870010045014. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Koltai PJ, Rabkin D. Management of facial trauma in children. Pediatr Clin North Am. 1996;43:1253–1275. doi: 10.1016/s0031-3955(05)70518-6. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Infante Cossio P, Espin Galvez F, et al. Mandibular fractures in children. A retrospective study of 99 fractures in 59 patients. Int J Oral Maxillofac Surg. 1994;23:329–331. doi: 10.1016/s0901-5027(05)80047-5. DOI: [DOI] [PubMed] [Google Scholar]
- 12.Kaban LB. Diagnosis and treatment of fractures of the facial bones in children, 1943–1993. J Oral Maxillofac Surg. 1993;51:722–729. doi: 10.1016/s0278-2391(10)80409-4. DOI: [DOI] [PubMed] [Google Scholar]
- 13.Chameides L, Hazinski MF. Pediatric advanced life support. Dallas: American Heart Association; 1997. pp. 8-1–8-9. [Google Scholar]
- 14.Cummins RO. Advanced cardiac life support. Dallas: American Heart Association; 1997. pp. 1-60–1-68. [Google Scholar]
- 15.Cole P, Kaufman Y, et al. Principles of pediatric mandibular fracture management. Plast Reconstr Surg. 2009;123:1022–1024. doi: 10.1097/PRS.0b013e318199f695. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Joshi S, Kshirsagar R, et al. Clinical efficacy of open reduction and semirigid internal fixation in management of displaced pediatric mandibular fractures: A series of 10 cases and surgical guidelines. J Indian Soc Pedod Prev Dent. 2015 Apr-Jun;33(2):161–165. doi: 10.4103/0970-4388.155135. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Yerit KC, Hainich S, et al. Biodegradable fixation of mandibular fractures in children: Stability and early results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:17–24. doi: 10.1016/j.tripleo.2004.11.013. DOI: [DOI] [PubMed] [Google Scholar]
- 18.Jingang A, Jia P, et al. Application of biodegradable plates for treating pediatric mandibular fractures. J Craniomaxillofac Surg. 2015;43:515–520. doi: 10.1016/j.jcms.2015.03.002. DOI: [DOI] [PubMed] [Google Scholar]


