ABSTRACT
Hypertrophic cardiomyopathy (HCM) is a hereditary disease characterized by cardiac hypertrophy with diastolic dysfunction. Gene mutations causing HCM have been found in about half of HCM patients, while the genetic etiology and pathogenesis remain unknown for many cases of HCM. To identify novel mechanisms underlying HCM pathogenesis, we generated a cardiovascular-mutant medaka fish, non-spring heart (nsh), which showed diastolic dysfunction and hypertrophic myocardium. The nsh homozygotes had fewer myofibrils, disrupted sarcomeres and expressed pathologically stiffer titin isoforms. In addition, the nsh heterozygotes showed M-line disassembly that is similar to the pathological changes found in HCM. Positional cloning revealed a missense mutation in an immunoglobulin (Ig) domain located in the M-line–A-band transition zone of titin. Screening of mutations in 96 unrelated patients with familial HCM, who had no previously implicated mutations in known sarcomeric gene candidates, identified two mutations in Ig domains close to the M-line region of titin. In vitro studies revealed that the mutations found both in medaka fish and in familial HCM increased binding of titin to muscle-specific ring finger protein 1 (MURF1) and enhanced titin degradation by ubiquitination. These findings implicate an impaired interaction between titin and MURF1 as a novel mechanism underlying the pathogenesis of HCM.
KEY WORDS: Genetics, Familial hypertrophic cardiomyopathy, Titin, Ubiquitin, Myocardial stiffness
Summary: The authors identified and characterized a medaka mutation in titin that leads to a phenotype similar to hypertrophic cardiomyopathy. Similar mutations were also observed in human patients.
INTRODUCTION
Zebrafish is well established as a model vertebrate in gene function studies (Seeley et al., 2007; Xu et al., 2002). The medaka fish, Oryzias latipes, recently emerged as another important such model system because of its smaller genome size and larger genome diversity (Kasahara et al., 2007). In particular, medaka is an excellent model for studying the cardiovascular system because the embryos are transparent and able to tolerate an absence of blood flow under sufficient oxygen delivery by diffusion (Burggren and Pinder, 1991). It is therefore possible to attribute cardiac phenotype directly to particular genes by ruling out the secondary effect of hypoxia.
Hypertrophic cardiomyopathy (HCM) is characterized by cardiac hypertrophy accompanied by myofibrillar disarray and diastolic dysfunction. The first HCM-causing gene identified was a missense mutation in the cardiac β-myosin heavy chain gene (Geisterfer-Lowrance et al., 1990). Such causative mutations were also identified in genes encoding contractile apparatus of sarcomere, such as α-tropomyosin, cardiac troponin T and cardiac myosin-binding protein-C (Ho and Seidman, 2006), whereby HCM was thought to result from compensation for dysregulated sarcomeric contractile function. An HCM-associated mutation (Gerull et al., 2002; Satoh et al., 1999; Itoh-Satoh et al., 2002) identified in the titin gene (TTN) was the first causative gene not encoding contractile apparatus, which implied the existence of a novel pathogenesis without the compensation of systolic dysfunction.
Titin is the largest known single protein and, after myosin and actin, the third most abundant protein of vertebrate striated muscle. Titin connects the Z-disc to the M-line region, where titin filaments extending from the opposite sides of half-sarcomeres overlap (Ojima et al., 2005; LeWinter and Granzier, 2010). Titin provides a scaffold for the assembly of thick and thin filaments (Gregorio et al., 1999), and provides passive stiffness during diastole (Granzier and Irving, 1995). Recently, titin was proposed to function as a sarcomeric stretch sensor that regulates muscle protein expression and turnover (Lange et al., 2006, 2005; Miller et al., 2004). Titin carries a kinase domain at the M-line–A-band transition zone, and adjacent to the kinase domain is a binding site for muscle-specific ring finger protein 1 (MURF1) (Centner et al., 2001), where the mechanical load on the sarcomere is transmitted through titin and its interaction partners to the nucleus. Functional alteration due to the TTN mutations may increase passive tension upon stretching of the sarcomere (Satoh et al., 1999; Kimura, 2008). Titin is extensively modular in structure and can be thought of as a microscopic necklace comprising up to 166 copies of 90- to 95-amino-acid-residue repeats from the immunoglobulin (Ig) domains.
Generally, the Ig domains located in the highly repetitive A-band region of titin share high structural similarity (Müller et al., 2007). However, a subset of Ig domains close to the titin kinase has unique structural features. For instance, Ig-A169 provides a binding site for MURF1 (Centner et al., 2001; Müller et al., 2007), a sarcomere-associated E3 ubiquitin ligase that conjugates ubiquitin to proteins destined for proteolysis (Bodine et al., 2001; Kedar et al., 2004). MURF1 belongs to the MURF family of proteins, which are transcribed from three genes, form heterodimers (Centner et al., 2001) and interact with titin kinase. MURFs have also been proposed to regulate protein degradation and gene expression in muscle tissues (Lange et al., 2005).
Here, we identified the non-spring heart (nsh) medaka fish, a cardiovascular mutant with a missense mutation in an Ig domain located at the M-line–A-band transition zone of titin. The nsh fish show diastolic dysfunction and hypertrophic heart. To decipher the roles of titin in these pathological effects, we focused on the M-line–A-band transition zone and identified two mutations in other Ig domains of titin in familial HCM patients. These titin mutations both increased the binding of titin to MURF1 and enhanced the degradation of titin by ubiquitination. This is the first report suggesting that the impaired binding of MURF1 to titin is a newly identified pathogenesis causing HCM.
RESULTS
Medaka nsh mutants showed hypertrophic heart and disrupted sarcomeric structure
In a previous screening for N-ethyl-N-nitrosourea (ENU)-induced mutations of medaka fish, we identified several mutants with abnormal heart development phenotypes (Taneda et al., 2010). Among these, one mutant showed rigid hearts with hypertrophy. Because the mutant heart had lost elasticity and beat in a rigid manner, we designated it as non-spring heart (nsh). The nsh embryos were indistinguishable from their wild-type (WT) siblings up to the heart tube stage (48 h), and there was no difference in the heart rate. However, after 72 h, the nsh hearts showed increased thickening of the myocardial wall, especially in the atrium and even without blood flow (Fig. 1A,B). Despite these abnormalities, the mutant embryos survived until 8 days post-fertilization (dpf), a stage around hatching, in a relatively healthy condition without forming pericardial edemas.
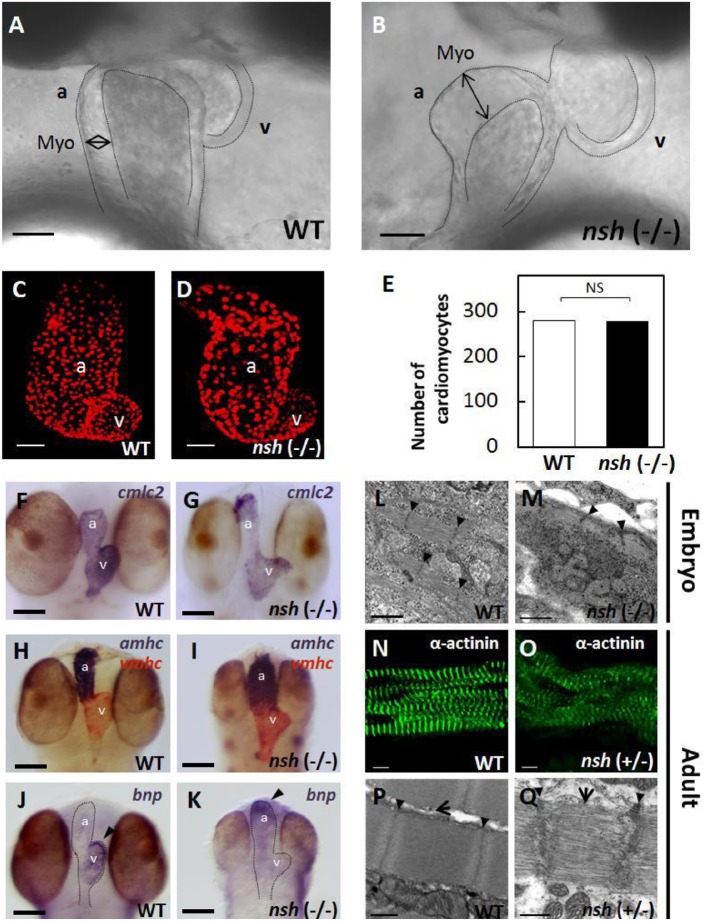
Fig. 1.
Hypertrophic myocardium and disrupted sarcomeric structure in the medaka nsh mutant heart. (A,B) Morphology of the wild-type (WT) and nsh mutant heart at 3 days post fertilization (dpf). The mutant showed hypertrophic heart, especially in the atrium (double-headed arrow). The nsh heart lost elasticity and showed increased passive stiffness. Due to diastolic inability (see Movie 2), the blood flow was very slow or clogged around 3 dpf. (C,D) Confocal z-stacked images of the WT and nsh mutant hearts at 3 dpf, in which cardiomyocytes were visualized by the Tg(cmlc2: DsRed2-nuc) signal. These reconstructed confocal images show approximately half of the total cardiomyocytes. (E) Quantification of cardiomyocytes using the transgenic line. Cell counting was performed on the optical slices to attain an accurate count. There was no difference in the number of cardiomyocytes between the WT and nsh mutant hearts. NS, statistically not significant (n=5 for WT and nsh). (F-K) In situ RNA hybridization analysis showing cardiac myosin light chain 2 (cmlc2) (F,G), and atrial and ventricular myosin heavy chains (amhc and vmhc, respectively) (H,I) in the WT and nsh mutant at 3 dpf. Normal sarcomeric protein expression was observed in the nsh mutant. (J,K) Strong expression of brain natriuretic peptide (bnp; arrowheads) was detected at 3 dpf in the WT ventricle (J), whereas bnp expression was strong in the atrium of nsh mutants (K). (L,M) Transmission electron microscopic findings of medaka embryonic cardiomyocytes at 5 dpf. Myofibrillar arrays were evident in the WT heart (L), but myofibrils were reduced with loosely arranged contractile filaments in the nsh mutant (nsh −/−) (M). Thick-filament structures and integrity of the M-line region were disrupted, and Z-discs were not parallel. (N,O) Medaka adult cardiac myocytes in the WT and nsh heterozygotes (nsh +/−) were stained for α-actinin. Expression of sarcomeric α-actinin was maintained in the nsh heterozygous mutant, but fewer striations and patchy staining was observed (O). (P,Q) Transmission electron microscopy showed the rupture of sarcomeric units, as well as irregular and widened Z-discs and M-lines in cardiomyocytes of the nsh heterozygotes. The integrity of the thick filaments is disrupted (Q) Z-discs (arrowheads) and M-lines (arrows) are indicated. a, atrium; v, ventricle; Myo, myocardium. Scale bars: 50 µm (A-D),100 µm (F-K), 1 µm (L,M), 5 µm (N,O), 0.5 µm (P,Q).
Blood flow was very slow or clogged around 3 dpf in the mutants due to defects in diastole (see Movies 1,2). However, hemoglobin activity was normal in both WT embryos and nsh mutants at 3 dpf based on an o-dianisidine staining analysis (data not shown). After crossing with friend leukemia integration 1 transcription factor (fli1)-green fluorescent protein (GFP) transgenic medaka (Fig. S1), alkaline phosphatase staining analysis revealed normal vascular endothelial cells at 3 dpf and normal blood vessel formation in the nsh mutants. To estimate the number of cardiomyocytes, we crossed the nsh mutants with a transgenic medaka [Tg(cmlc2:DsRed2-nuc)] expressing DsRed in the cardiomyocyte nuclei (Fig. 1C,D). We counted the nuclei of cardiomyocytes using confocal images and found no difference in the numbers between WT and nsh mutants at 3 dpf (Fig. 1C-E).
In situ hybridization with cardiac-differentiation markers – atrial and ventricular myosin heavy chains and cardiac myosin light chain – demonstrated normal expression of sarcomeric proteins in the nsh mutant (Fig. 1F-I). A cardiac stretch marker, brain natriuretic peptide (bnp), is normally expressed at 3 dpf in the WT ventricle, but its expression was increased in the atrium of nsh mutants (Fig. 1J,K).
We then examined the sarcomeric structures of embryonic cardiomyocytes by transmission electron microscopy. Sarcomeric units of the WT cardiomyocytes at 5 dpf showed highly organized, precisely aligned thick and thin myofilaments, flanked by Z-discs and M-lines (Fig. 1L). In the nsh homozygotes, cardiomyocytes appeared abnormal with loosely arranged contractile filaments, where thick and thin filaments were disassembled and Z-discs were not parallel (Fig. 1M). We next analyzed the sarcomeric structure of adult cardiomyocytes in the WT and nsh heterozygotes (Fig. 1N,O). Expression of sarcomeric α-actinin was maintained in the nsh heterozygotes, although with fewer striations and patchy staining (Fig. 1O). Transmission electron microscopy demonstrated ruptured sarcomeric units with irregular and widened Z-discs and M-lines in the cardiomyocytes of nsh heterozygotes (Fig. 1P,Q). We have analyzed body:heart weight ratio in 3- to 4-month-old adult medaka fish. The hearts of nsh heterozygotes were heavier than WT hearts in relation to body weight (P=0.01, n=24) (Fig. S2). The nsh mutants did not show skeletal paralysis; however, the nsh homozygous embryos had a slightly smaller body, and skeletal myocytes demonstrated severely disturbed sarcomeric integrity with ruptured myofibrils (Fig. S3). Unlike in WT, staining for α-actinin was patchy in the nsh heterozygotes (Fig. S3). By transmission electron microscopy, the skeletal myofibrils of nsh heterozygotes demonstrated occasionally disrupted M-lines, although they displayed well-formed Z-discs and apparently mature myofibrils (Fig. S3). Body size, movement, lifespan and fertility of the nsh heterozygotes were not affected (data not shown), although the abnormal sarcomeric structure was inherited as an autosomal dominant trait.
TTN is the nsh gene
To identify the gene responsible for the nsh phenotype, we carried out positional cloning. We scored 2016 fishes from nsh×nsh/+ crosses and found that the nsh phenotype was linked to the medaka linkage group 21 (LG 21). Single-strand conformation polymorphism markers from introns 193 to 194 and the 3′UTR of TTN confined the nsh locus to a 19.0-kb critical region (Fig. 2A). TTN was the only transcript identified in the nsh critical region. Analysis of cDNAs from the nsh mutant and several WT strains revealed an adenine-to-thymine transversion causing the substitution of D (aspartic acid)-23186 to V (valine) in the nsh titin (Fig. 2B). Medaka titin is encoded by a single gene composed of 219 exons, and the nsh missense mutation was localized to TTN exon 204 near the MURF1-binding region that encodes an Ig domain (Fig. 2C). Alignment of titin from several species revealed that the nsh mutation occurred at an evolutionary highly conserved amino acid residue (Fig. 2D).
Fig. 2.
TTN is the nsh gene. (A) Genetic mapping of the nsh locus on the medaka linkage group 21 (LG 21). To define the nsh gene, we scored 2016 fish from nsh/+×nsh/+ mapping crosses. Single-strand conformation polymorphism markers from intron 193-194 and the 3′UTR of TTN confined nsh to a 19.0-kb critical region. (B) DNA sequence analysis of cDNAs from the nsh and WT strains revealed an adenine-to-thymine mutation in nsh, causing D (aspartic acid)-23186 to V (valine) mutation (red arrow), located in exon 204. (C) Modular structure of the M-line–A-band transition zone of titin contains a binding site for muscle-specific ring finger protein 1 (MURF1). The missense mutation identified in nsh was located in an Ig domain near this site. (D) Clustal W alignment of human, mouse, zebrafish and medaka TTN sequences. Medaka titin and human titin proteins share 62% similarity. GenBank or Ensembl accession numbers used for the analysis are as follows: human TTN (NM_133378), mouse Ttn (NP_035782), zebrafish ttna (DQ649453) and medaka TTN (ENSORLT00000022736). Alignment of titin protein from several species along with the nsh mutation showed that the mutation affected the evolutionary conserved amino acid residue (red asterisk). Identical and similar amino acids are indicated by dark blue and light blue boxes, respectively.
Protein turnover of the mutated-Ig-domain titin at the M-line–A-band transition zone was faster than that of WT-Ig-domain titin
To investigate the molecular mechanisms of TTN mutation as the nsh gene, we performed reverse-transcriptase PCR (RT-PCR) analysis of the TTN N-terminal, A-I junction, exon 204 and the titin kinase domain in WT and nsh mutant embryos at 3 dpf. This analysis revealed unchanged expression levels of TTN mRNA in the nsh mutant compared to WT (Fig. 3A).
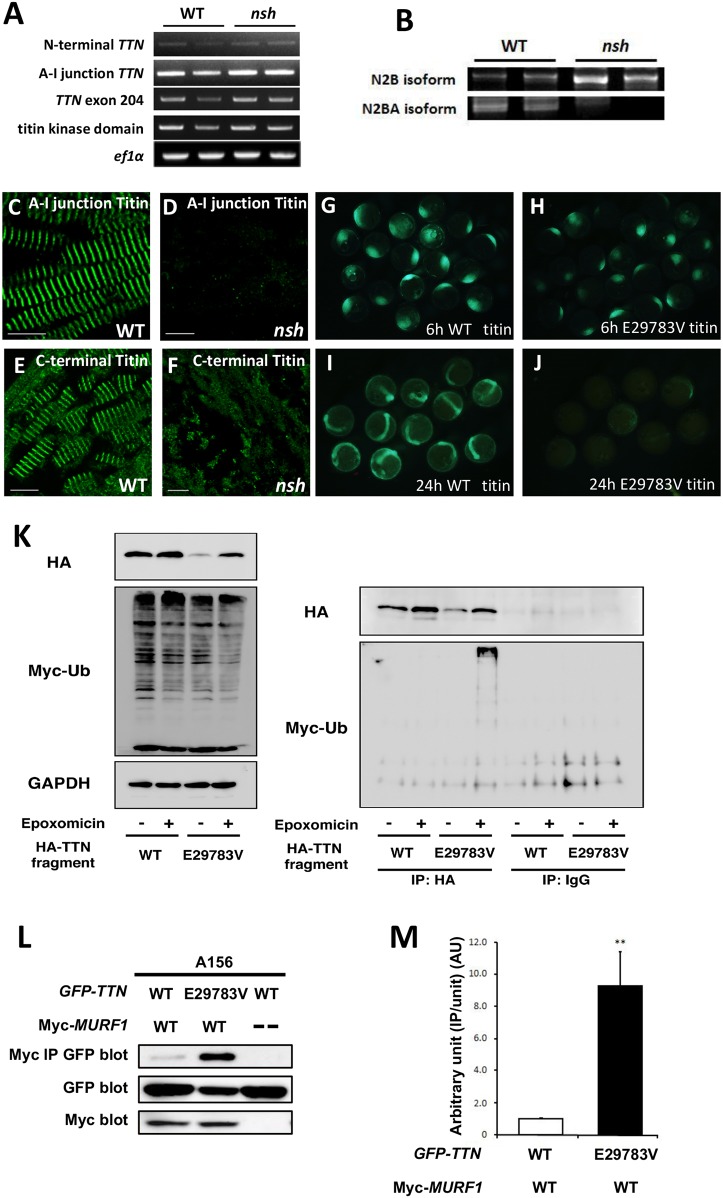
Fig. 3.
The mutant TTN Ig domain binds more strongly to MURF1 and is degraded faster than wild type, both in vitro and in vivo. (A) RT-PCR analysis of TTN for the N-terminal portion, A-I junction region, exon 204 and titin kinase domain in the WT and nsh mutant embryos at 3 dpf. Despite the presence of a missense mutation, the level of TTN mRNAs for these portions in the nsh mutant was similar to that in the WT. The ef1α transcript was used as a control. (B) RT-PCR analysis of titin N2B isoforms in the WT and nsh mutants. N2B isoforms were increased. (C-F) Embryonic skeletal muscle of the WT and nsh mutant at 3 dpf were stained with antibodies to A-I junction titin (C,D) and C-terminal titin (E,F). Despite the similar expression level of TTN mRNA, expression of titin containing the A-I junction isoform was reduced (D). Sarcomeric structures were disrupted in the nsh mutant (F). (G-J) WT and mutant (E29783V which was the equivalent of D23186V mutation in medaka) Ig fragments mRNA injection into medaka embryos. Despite the same amount of mRNA injection, mutant (E29783V) Ig fragments degraded faster than WT TTN Ig fragments. (K) Western blots (WBs) of HEK293FT cells transfected with HA-tagged WT and mutant (E29783V) Ig fragments with or without a proteosome inhibitor, epoxomicin. Myc-tagged ubiquitin was co-transfected to visualize ubiquitination. WBs of anti-HA IPs and control normal IgG IPs are shown. Note that the myc-labeled large molecules in mutant TTN transfectants were present only in the presence of epoxomicin. (L) GFP-tagged TTN-A156 domain co-precipitated with myc-tagged MURF1 are shown (top panel). Expression levels of GFP-tagged TTN-A156 (middle panel) and myc-tagged MURF1 (lower panel) was confirmed by WB of whole-cell lysates. Binding pairs were WT or E29783V mutant TTN-A156 in combination with MURF1. Dashes indicate no myc-tagged proteins (transfected only with pCMV-Tag3). (M) Densitometric data obtained from the co-IP assays. Bar graphs indicate the amount of IPs normalized to the input amount of GFP-TTN. Value for WT TTN-A156 with MURF1 was arbitrarily defined as 1.00 arbitrary unit (AU). Data are represented as means±s.e.m. (n=10). **P<0.001 versus WT. Scale bars: 50 µm.
Titin isoform shifts have been reported in pathological conditions (Lahmers et al., 2004; Neagoe et al., 2002; Opitz et al., 2004; Warren et al., 2004; Makarenko et al., 2004). In cardiac muscle, the elastic region expresses two types of titin isoform, termed N2B and N2BA, which arose from alternative splicing and result in titin molecules that contain either a unique N2B element and short PEVK region (N2B isoform) or unique N2B and N2A elements and a long PEVK region (N2BA isoform) (Miller et al., 2004). Predominant expression of the N2B isoform results in stiffer cardiac tissue, while the expression of the N2BA isoform results in more compliant cardiac myofibrils (Wu et al., 2002). Changes in the relative proportions of N2B and N2BA was paralleled by changes in diastolic stiffness (Ouzounian et al., 2008). The N2BA:N2B ratio in myocardium under conditions of diastolic heart failure is lower than that observed during systolic heart failure (van Heerebeek et al., 2006). We detected different titin N2B isoform shifts between the WT and nsh mutant titin in the nsh heart, which would be associated with less elasticity and increased passive stiffness (Fig. 3B).
Mutations in the TTN gene and protein have also been linked to disorders of skeletal muscles (Ojima et al., 2005; Gregorio et al., 1999). To analyze the expression of titin proteins in the nsh mutant, we conducted indirect immunofluorescence on the skeletal muscle of 3 dpf embryos using an antibody to the A-I junction portion of titin. In WT, titin appeared in a regularly striated pattern between the sarcomeres of adjacent myofibrils (Fig. 3C). However, the nsh mutants showed severely decreased titin immunofluorescence at the A-I junction (Fig. 3D). Analysis of the titin C-terminal region and α-actinin staining demonstrated an altered muscle organization, but there was no apparent decrease in expression of the titin C-terminal portion (Fig. 3E,F; Fig. S2). These findings indicated that certain titin isoforms at the A-I junction were selectively perturbed.
To further investigate the dominant-negative effect of mutant TTN in vivo, we overexpressed the Ig domain of TTN (GFP-tagged WT-TTN-A156 or E29783V-TTN-A156 construct, which was the equivalent of the D23186V mutation in medaka) (Fig. 3G-J) by injecting mRNA corresponding to exon 204, in which the missense mutation was found, fused with the GFP fragment into one-cell-stage medaka embryos. Overexpression of neither the WT nor nsh Ig domain induced a specific cardiac phenotype (n=200 in each case). However, in the nsh-Ig-domain-injected medaka embryos, the GFP signal disappeared faster than in the WT-Ig-domain-injected embryos (Fig. 3G-J), demonstrating that the nsh Ig domain was susceptible to degradation and/or was unstable in vivo. The nsh-Ig-domain fragments could not be observed 2 days after the injection, before the heart began beating, and this could explain why we could not replicate the nsh phenotype in the injected embryos (Fig. 3G-J).
Next, we examined the faster turnover of the nsh-Ig titin domain, focusing on the ubiquitin proteasome (UPS) system because of the proximity of the nsh mutation to the MURF1-binding site. We found that the nsh-Ig-domain protein was degraded faster via the UPS-dependent pathway in vitro than the WT Ig domain (Fig. 3K), and that this effect was rescued by the UPS inhibitor epoxomicin (Fig. 3K), indicating that the turnover of this specific titin Ig domain is controlled by the UPS. This regulation mechanism could involve MURF1 because it is thought to act in muscle as a rate-limiting E3 ligase to initiate UPS-mediated degradation.
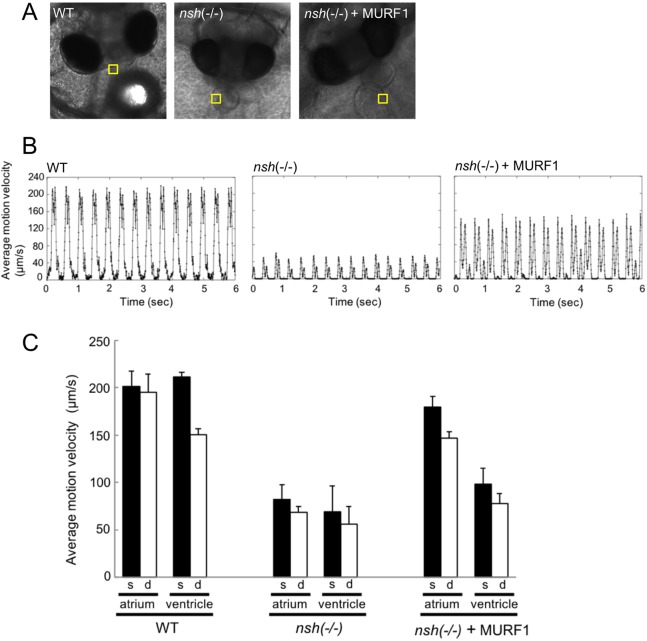
Medaka nsh mutants showed rigid hearts with normal heart rhythm
We quantified cardiac systolic and diastolic motion of WT and nsh mutants (see Movies 1,2) using high-speed video imaging and analysis with the motion vector prediction (MVP) method as described in the Materials and Methods section. This method could extract contraction and relaxation motions of cardiomyocytes non-invasively, and evaluate characteristics such as beating rate, orientation of contraction, beating homogeneity and wave propagation of contraction (da Silva Lopes et al., 2011). As shown in Fig. 4B,C, maximum systolic and diastolic velocities of atrium were decreased from ∼183 μm/s in WT embryos to ∼64 μm/s in nsh mutants, and from ∼140 μm/s in WT embryos to ∼35 μm/s in nsh mutants, respectively. Similarly, the maximum systolic and diastolic velocities of ventricles were decreased from ∼189 μm/s in WT embryos to ∼29 μm/s in nsh mutants, and from ∼136 μm/s in WT embryos to ∼22 μm/s in nsh mutant embryos, respectively. However, the heart rate between WT and nsh mutants was not changed significantly (Fig. 4B,C). These data demonstrated that the nsh mutated gene was not required for the establishment of cardiac rhythm, but rather for control of cardiac elasticity (Fig. 4B). As we had previously shown that the nsh-Ig-domain protein was degraded faster than the WT Ig domain (Fig. 3K), we hypothesized that cardiac rigidity might be due to excessive degradation of titin. To confirm our hypothesis, we performed a rescue experiment with morpholino knockdown of MURF1. After the injection of morpholino, we analyzed cardiac movement by motion vector analysis. The maximum systolic and diastolic velocities of both the atrium and ventricle was increased when nsh mutant embryos were microinjected with MURF1 morpholino, suggesting that cardiac elasticity was partially recovered (Fig. 4B,C). However, we still observed cardiac hypertrophy in MURF1-morpholino-injected nsh embryos. This may be because the effects of morpholinos generally only persist up to 3-4 dpf and the cardiac hypertrophy phenotype is developed at a later stage in nsh mutant embryos.
Fig. 4.
Medaka nsh mutants showed rigid hearts with normal heart rhythm. The beating motions of medaka atrium and ventricle were captured with a high-speed camera and were analyzed with the motion vector prediction (MVP) method. (A) Phase-contrast images of medaka embryos of WT (left), nsh mutant (middle) and nsh mutant+MURF1 morpholino (right). The yellow squares in the images indicate the regions of interest (ROI) employed for the motion vector calculation of atrium wall. (B) Typical beating profile of atrium observed for WT (left), nsh mutant (middle) and nsh mutant+MURF1 morpholino (right). Motion velocity (the vertical scale) represents averaged motion vector length in the ROI. In both figures, each large peak followed by a small peak represents a single beat of atrium. Since we obtained the vector lengths simply from the square root of x2+y2 (x and y represent the vector components), the systolic and diastolic peaks both had positive values. (C) Maximum velocities observed for systolic and diastolic motions in WT, nsh mutant and nsh mutant+MURF1 morpholino are shown for atrium and ventricle. Systolic and diastolic velocities were decreased in nsh mutants and were partially rescued by MURF1 morpholino, while the heart rate was not changed. Data are represented as means±s.e.m. (n=3).
Next, we investigated the binding between MURF1 and the Ig domain with or without the mutations using the coimmunoprecipitations (co-IPs) assays, and found that co-IPs from cells transfected with the myc-tagged MURF1 construct in combination with the GFP-tagged WT-TTN-A156 or E29783V-TTN-A156 construct revealed that the A156 domain bound MURF1 and that the E29783V mutation significantly increased the binding (9.23±2.11 AU; P<0.001) (Fig. 3L,M). Notably, the expression level of mutant-TTN-A156 was lower than that of WT-TTN-A156 (Fig. 3L).
Taken together, our data indicate that the Ig domain of the M-line–A-band transition zone of titin plays an important role in maintaining and organizing the myofibril structure. The severely reduced titin protein levels in combination with the genetic linkage data implicated the TTN mutation as being causative of the nsh phenotype. The alternations in N2B/N2BA titin isoforms in the nsh phenotype in turn underscored the probable key role of titin in regulating and maintaining cardiac muscle elasticity. The next logical step would have been to rescue the nsh phenotype by injecting full-length TTN mRNA. However, since the medaka TTN gene is very large, we were unable to clone the full-length cDNA (∼15 kb) to perform the rescue experiments, and as a result there remains a chance that the wrong variant has been identified.
Mutational analysis of the human TTN gene around the MURF1-binding domain in patients with familial HCM
The proximity of the nsh mutation to the titin-MURF1 binding domain and the cardiac phenotype in mutant medaka implicated the titin M-line–A-band transition zone as a candidate region for mutations associated with HCM in humans. We therefore analyzed a total of 96 genetically unrelated Japanese patients with familial HCM who carried apparent family history of HCM consistent with an autosomal dominant trait. They were diagnosed with HCM according to the diagnostic criteria as described previously (Arimura et al., 2009). They had been analyzed for mutations in the known disease genes for HCM, i.e. genes for contractile elements (MYH7, TNNT2, MYBPC3, TNNI3, MYL2, MYL3, ACTC1, TNNC1), Z-disc elements and I-band elements, and no disease-associated mutation was found (Arimura et al., 2009). Control subjects were 400 healthy Japanese individuals selected at random from non-HCM patients at Tokyo Medical and Dental Hospital.
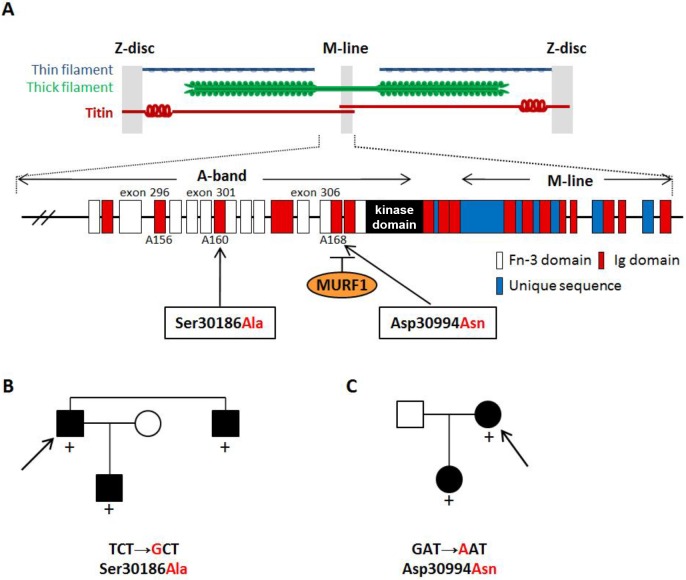
Exon 204 of medaka TTN, containing the nsh mutation, corresponds to exon 297 of human TTN; thus, we searched for mutations in the patients by direct sequencing of exons 296-307 of TTN (GenBank accession no. NM_133378), which encoded for the M-line–A-band transition region of titin, including the titin kinase domain. We identified two disease-associated missense mutations (Fig. 5A): TCT→GCT, leading to the replacement of serine with alanine at position 30186 (S30186A) in exon 301 (Fig. 5B), and GAT→AAT, with the exchange of aspartic acid for asparagine at position 30994 (D30994N) in exon 306 (Fig. 5C). The proband patients and their affected relatives were heterozygous for the mutations, and both mutations affected highly conserved amino acids. Quite interestingly, the latter mutation in the M-line–A-band transition zone of titin was mapped within the binding site for MURF1. It should be noted here that all three mutations found in the medaka nsh mutant and human HCM patients were located in the Ig domains (Fig. 5A).
Fig. 5.
Mutations in the Ig domains of titin are associated with HCM. (A) Schematic structure of titin at the C-terminal A-band and M-line region. C-terminal ends of titin meet in the M-line. Arrows indicate the position of two mutations found in familial HCM. The nsh missense mutation corresponds to exon 297 of human titin. Fn-3 indicates fibronectin type 3. (B,C) Pedigrees of Japanese families with HCM; affected and unaffected members are indicated by black and white symbols, respectively. Upon screening for mutations in exons 296-307 of TTN, which encode for the A-band region of titin, including the titin-kinase domain, two disease-associated mutations, S30186A (B) and D30994N (C), were identified. The latter mutation is located at the edge of the M-line region of titin and within a binding site for MURF1. Both mutations were found in the Ig domains of titin as indicated by red boxes in A. The proband patient of each family is indicated by the arrow. Presence (+) of the mutations is noted.
Altered binding of titin to MURF1 caused by the TTN mutations
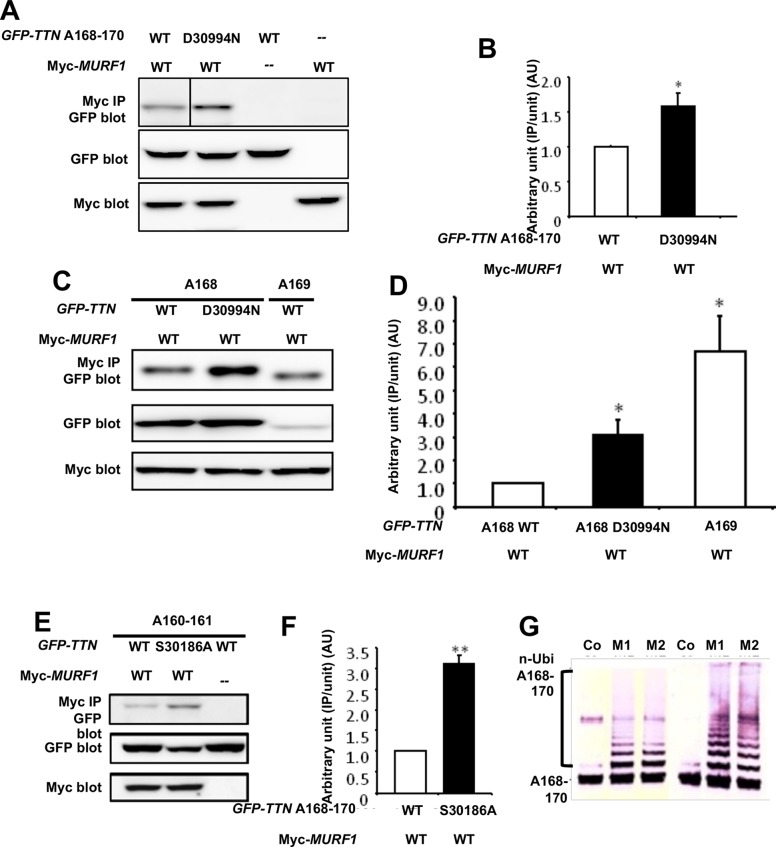
Based on the D30994N mutation being located in the MURF1-binding Ig domain of titin, A168-170, we investigated a possible functional change in binding to MURF1 due to the mutation. GFP-tagged WT- or D30994N-TTN-A168-170 construct was co-transfected with a myc-tagged MURF1 construct into COS-7 cells. Western blot (WB) analysis of co-IPs of the transfected cells using anti-myc antibody demonstrated that the D30994N mutation significantly increased binding to MURF1 (1.58±0.19 AU; P<0.01) (Fig. 6A,B). The A168-170 domain contains two Ig domains, A168 and A169, of which the A169 domain is the predominant binder of MURF1 (Müller et al., 2007), despite the D30994N mutation being located in the A168 domain. To further characterize the increased binding of titin to MURF1 in the presence of the D30994N mutation, we performed additional WB analyses of co-IPs from the cells transfected with the myc-tagged MURF1 construct in combination with GFP-tagged WT-TTN-A168, D30994N-TTN-A168 or WT-TTN-A169 constructs. WT-TTN-A169 showed significantly higher binding to MURF1 than WT-TTN-A168 (6.69±1.53 AU; P<0.01) (Fig. 6C,D). On the other hand, the D30994N mutation also significantly increased the binding of the A168 domain to MURF1 (3.06±0.68 AU; P<0.01) (Fig. 6C,D).
Fig. 6.
Altered binding of titin and MURF1 caused by the TTN mutations. (A) GFP-tagged TTN-A168-170 domain co-immunoprecipitated with myc-tagged MURF1 is shown (top panel). Expression levels of GFP-tagged TTN-A168-170 (middle panel) and myc-tagged MURF1 (lower panel) were evaluated by WB of whole-cell lysates. Binding pairs were WT or D30994N mutant TTN-A168-170 in combination with MURF1. Dashes indicate no GFP-tagged or myc-tagged proteins (transfected only with pEGFP-C1 or pCMV-Tag3, respectively). (B) Densitometric data obtained from the co-IP assays. Bar graph indicates the amount of precipitate normalized to the input amount of GFP-TTN. Value for WT TTN-A168-170 with MURF1 was arbitrarily defined as 1.00 AU. *P<0.01 versus WT. (C) GFP-tagged TTN-A168 or TTN-A169 domains co-immunoprecipitated with myc-tagged MURF1 are shown (top panel). Expression levels of GFP-tagged TTN-A168 or TTN-A169 (middle panel) and myc-tagged MURF1 (lower panel) were evaluated by WB of whole-cell lysates. Binding pairs were WT or D30994N mutant TTN-A168 in combination with MURF1, and WT TTN-A169 in combination with MURF1. (D) Densitometric data obtained from the co-IP assays. Bar graph indicates the amount of precipitate normalized to the input amount of GFP-TTN. Value for WT TTN-A168 with MURF1 was arbitrarily defined as 1.00 AU. Data are represented as means±s.e.m. (n=10). *P<0.01 versus WT. (E) GFP-tagged TTN-A160-161 domains co-precipitated with myc-tagged MURF1 are shown (top panel). Expression levels of GFP-tagged TTN-A160-161 (middle panel) and myc-tagged MURF1 (lower panel) was confirmed by WB of whole-cell lysates. Binding pairs were WT or S30186A mutant TTN-A160-161 in combination with MURF1. Dashes indicate no myc-tagged proteins (transfected only with pCMV-Tag3). (F) Densitometric data obtained from the co-IP assays. Bar graph indicates the amount of IPs normalized to the input amount of GFP-TTN. Value for WT TTN-A160-161 with MURF1 was arbitrarily defined as 1.00 AU. Data are represented as means±s.e.m. (n=10). **P<0.001 versus WT. (G) Titin A168-170 was ubiquitinated by MURF1 and MURF2. The titin fragment A168-170 containing the MURF1-binding site was used as a substrate for in vitro ubiquitination assays. Addition of recombinant MURF1 or MURF2 catalyzes multi-ubiquitination of titin fragments. Lanes: Co, control (no E3 ligase added); M1, inclusion of MURF1; M2, inclusion of MURF2. After incubation, A168-170 fragments were detected by WB, using specific antibodies to titin A169 (left), and A168-170 (right).
Because the other mutation (S30186A) also located in the Ig domain (A160), we also investigated the binding between MURF1 and the A160 Ig domain with or without the mutation using the co-IP assays. The co-IPs from cells transfected with the myc-tagged MURF1 construct in combination with GFP-tagged WT- or S30186A-TTN-A160-161 construct revealed that the A160-161 domains also bound MURF1 and that the S30186A mutation significantly increased the binding (3.11±0.71 AU; P<0.001) (Fig. 6E,F). Notably, the expression level of mutant-TTN-A160-161 was lower than that of WT-TTN-A160-161 (Fig. 6E). These data suggested that mutations in the Ig domains of the M-line–A-band transition zone enhanced the interactions with MURF1. This raises an interesting possibility that the association of MURFs with the M-line regions could link ubiquitin-transfer pathways to the titin filament system, which may relate to the physiological turnover of titin in myofibrils. To test this hypothesis, we performed an in vitro ubiquitination assay of titin fragment. The titin fragment A168-170, containing the MURF1-binding site, was used as a substrate. Addition of recombinant MURF1 or MURF2 indeed catalyzed multi-ubiquitination of titin fragment (Fig. 6G). Moreover, to confirm this idea, we also performed immuno-electron microscopy with anti-ubiquitin antibodies in WT and MURF1-knockout mice (Bodine et al., 2001). Ubiquitin signals were detected at the Z-line, central I-band and M-line regions in WT sarcomere. It was hard to quantify the signals; however, ubiquitin seemed to be reduced in MURF1-knockout mice at the M-line region (data not shown). Endogenous MURF1 levels were tightly regulated (Centner et al., 2001), in combination with ubiquitination of the titin A168-170 fragment by MURFs (Fig. 6G), and increased binding of titin and MURF1 (Fig. 3L; A,C,E) suggested that the interactions of MURF1 with titin are critical for maintaining the stability of titin.
DISCUSSION
We generated a cardiovascular-mutant nsh medaka fish by ENU mutagenesis that developed hypertrophy and diastolic dysfunction. We identified a causative mutation in a region of titin around the MURF1-binding site. The nsh homozygous fish showed loosely arranged contractile units, and died around 8 dpf. The nsh heterozygotes showed normal lifespan and fertility, but they exhibited M-line disassembly in myofibrils, indicating that the phenotype of M-line disassembly was inherited as a dominant trait.
Due to the extremely large size and presence of multiple isoforms, it has been difficult to study the structure and function of titin. A knock-in mouse of eGFP to the titin gene showed that sarcomeric titin is more dynamic than previously suggested (da Silva Lopes et al., 2011). The large cardiac titin N2BA isoform is rapidly replaced by the smaller N2B isoform both after birth and with re-expression of the fetal gene program in cardiac pathological conditions (Lahmers et al., 2004; Neagoe et al., 2002; Opitz et al., 2004; Warren et al., 2004; Makarenko et al., 2004). The isoform switch plays an important role in adjusting diastolic function. It has been used with knockout technology to gain insight into the roles of titin in sarcomere assembly, stability and mechanotransduction during muscle pathophysiology (Weinert et al., 2006; Radke et al., 2007; Granzier et al., 2009). Based on these studies, it was proposed that titin provides a scaffold for the developing sarcomere (Gregorio et al., 1999), and that passive forces maintain the correct localization of M-lines and tether various signaling and structural molecules (LeWinter and Granzier, 2010). Multiple interacting proteins integrate titin into the sarcomere and modulate the titin filament via links to basic cellular functions, including trophic signaling and energy balance.
Herman et al. (2012) recently showed by next-generation sequencing that TTN-truncating mutations are the most common known genetic cause of dilated cardiomyopathy (DCM). Their findings revealed that mutations associated with DCM were overrepresented in the titin A-band, but were absent around the M-band regions of titin. One may therefore speculate that some truncated titin peptides are degraded via the RNA- and protein-surveillance pathways in DCM. The consequently decreased titin levels could limit sarcomere formation, resulting in cardiac dysfunction. However, this is not the case for previously reported TTN mutations that delete only part of the M-band portion of titin (Carmignac et al., 2007); immunohistochemical studies showed that some of these C-terminal-truncated titin proteins are integrated into the sarcomere. If more-proximal TTN-truncating mutations caused DCM through haploinsufficiency, the distribution of such mutations would be rather uniform across the susceptible portion of titin.
The current study of our HCM families found point mutations around the M-line–A-band transition zone, which is implicated in sensing and modulating sarcomeric force. These mutations also induced high binding affinity between titin and MURF1. Using the medaka fish and our in vitro system, we showed that mutated titin fragments are degraded faster by ubiquitination. This study indicates that titin proteins found in families with HCM, as in the C-terminal titin truncations studied, are integrated into sarcomeres and cause HCM via a dominant-negative mechanism. Our results indicated that titin protein mutations in HCM families could be incorporated into the sarcomere and impair MURF1 binding, resulting in HCM through disturbance of the normal turnover of titin and abnormal sarcomere stiffness.
Until now, altered binding of MURF1 to titin has not been identified to be closely associated with human HCM or diastolic dysfunction. In this study, we analyzed exons 296-307 (M-line–A band transition zone) of TTN for mutations in patients with familial HCM and identified two disease-associated missense mutations in the Ig domains. One of the TTN mutations in familial HCM was in a binding site for MURF1. Although MURF1 binds to the Ig domain of the M-line–A-band transition region, A168-170, MURF1 was not considered to target titin for degradation (Centner et al., 2001). Data in this study and previous studies indicate that MURF1 may regulate the turnover of critical sarcomeric proteins (Kedar et al., 2004) including some titin isoforms (Bodine et al., 2001; McElhinny et al., 2002). We also found that all the TTN mutations associated with HCM both in medaka and human in the Ig domains of the M-line–A-band transition zone increased the binding of MURF1 to titin (Fig. 6A,C,E). In addition, the TTN constructs carrying the HCM-associated mutations expressed less protein when they were injected into medaka embryos and transfected into cells (Fig. 3G-J). Although the molecular mechanisms underlying this reduced expression remain to be clarified, it seems to be caused by accelerated degradation by the ubiquitin proteasome pathway (Figs 3K and 6G). Further, the knockdown of MURF1 in nsh mutants partially recovered the cardiac systolic and diastolic velocity. These studies therefore suggests the inhibition of MURF1 function as a therapeutic intervention for HCM patients.
In summary, we have identified TTN mutations that increased the binding of titin to MURF1 in a medaka model and in patients with HCM. There are several pathways underlying the pathogenesis of HCM, including abnormal power generation, power transmission, calcium sensitivity, energy homeostasis and stretch response. MURF1 may be involved with a novel pathway responsible for both the regulation of myofibril turnover and isoform shift as well as muscle gene expression, because MURF1 exists in multiple locations within the cell, including the cytosol, sarcomere and nucleus. Our observations suggest that pathogenic mechanisms underlying HCM cases that are related to mutations in the titin M-line–A-band transition zone might be a consequence of abnormal protein turnover and impaired adjustment of diastolic function regulated by titin and MURF1.
MATERIALS AND METHODS
Fish strains and maintenance
Medaka fish (Oryzias latipes) were maintained at 28.5°C in a recirculating system with a 14-h day and 10-h night cycle. The Qurt strain, derived from the southern Japanese population, was used for the genetic screen. Another strain, Kaga, which came from the northern population in Japan, was used for the mapping cross. The medaka heart mutant non-spring heart (nsh) was isolated by mutational screening (Sakamoto et al., 2004). Fertilized eggs were collected and then incubated at 28.5°C in medaka Ringer's solution (0.65% NaCl, 0.04% KCl, 0.011% CaCl2, 0.01% MgSO4, 0.01% NaHCO3 and 0.0001% Methylene Blue). Developmental stages were determined by their morphology according to the medaka stage table described by Iwamatsu (2004). The fli1-GFP transgenic line was kindly gifted by Dr A. Kudo (Moriyama et al., 2010). All experimental procedures and protocols were approved by the Animal Care and Use Committee of Keio University and conformed to the current NIH Guidelines for the Care and Use of Laboratory Animals.
Counting cardiomyocytes in vivo
The DsRed2-nuc gene under control of the zebrafish cardiac myosin light chain 2 (cmlc2) promoter transgenic strain (Taneda et al., 2010) was used for scoring cardiomyocyte numbers. The WT and nsh homozygous hearts carrying Tg(cmlc: DsRed2-nuc) were dissected, fixed with 4% paraformaldehyde (PFA) in phosphate-buffered saline (PBS) overnight at 4°C, and then mounted in 1% agarose gel. We routinely prepared 50-100 optical sections from one heart sample, and counted cells on the merged images from one in every 25 sections. Data were presented as mean±s.e.m. Student's t-test was used to test statistical significance.
Whole-mount RNA in situ hybridization (ISH) analysis
Whole-mount ISH analysis was performed as described previously (Thisse and Thisse, 2008). After staining, tissues were fixed with 4% PFA in PBS for color preservation, equilibrated with 80% glycerol and then mounted on slide glass for microscopic observation. The following primers were used for cloning the probes by PCR: for cmlc2, F 5′-AATGTCTTTTCCATGTTTGAGC-3′ and R 5′-CTCCTCTTTCTCATCCCCATG-3′; for atrium myosin heavy chain (amhc), F 5′-TGCACTGATGGCTGAATTTG-3′ and R 5′-ACTTGATCTACACCTTGGCC-3′; for ventricular myosin heavy chain (vmhc), F 5′-GCTGAGATGTCCGTGTATGGTGC-3′ and R 5′-GCTCCTCACGAGGCCTCTGCTTG-3′; and for brain natriuretic peptide (bnp), F 5′-GATCCATCCATCCATCATCC-3′ and R 5′-TGATACTTTAAAGACACAATGTCCAA-3′. The PCR products were cloned into standard vectors and used to prepare the digoxigenin (dig)-labeled RNA probes.
Histology and electron microscopy
We fixed medaka embryos with 4% PFA in PBS overnight at 4°C, before dehydrating them in 70% ethanol, mounting in paraffin and sectioning at 5 µm thickness. Sections were stained with hematoxylin and eosin (H&E) and viewed using a BIOREVO optical microscope (BZ-9000; Keyence, Japan). For transmission electron microscopy, samples were prepared as described previously (Rottbauer et al., 2001), sectioned using an RMC MT6000 ultramicrotome and visualized using the JEM-1230 (JEOL) electron microscope.
Immunohistochemistry
Medaka embryos were fixed in 4% PFA/PBS overnight at 4°C. Following fixation and removal of the egg chorion with forceps, samples were cryoprotected in sucrose at 4°C overnight, embedded in OCT compound (Sakura Finetec) and snap-frozen in hexane at −80°C. The sections were incubated in primary antibodies (see below) overnight at 4°C, washed three times for 5 min each in PBS and then incubated in the appropriate secondary antibodies (Invitrogen) for 1 h at room temperature. Stained samples were observed by confocal laser-scanning microscopy (LSM510; Carl Zeiss, Jena, Germany). The following primary antibodies were used at the indicated dilutions: anti-α-actinin (Sigma-Aldrich; A7811) at 1:300, anti-A-I junction Titin [T11 (Sigma-Aldrich; T9030)] at 1:100, and anti-C-terminal Titin [Titin H-300 (Santa Cruz Biotechnology; sc-28536)] at 1:100. Secondary antibodies were goat anti-rabbit IgG-FITC (sc-2012, 1:100) and goat anti-mouse IgG H&L–Alexa-Fluor-488 (ab150113, 1:100).
High-speed video microscopy
Medaka embryos were placed in a bottom of the well (24-multiwell plate) and incubated with 500 μl of medaka Ringer's solution. Embryos were arranged to direct their heart towards the bottom of the plate so that the cross-sectional heart images for each embryo can be observed from a similar direction. A high-speed digital CMOS camera (KP-FM400WCL, Hitachi Kokusai Electric, Tokyo, Japan) was mounted on an inverted microscope (Eclipse TE2000, Nikon, Tokyo, Japan), which was equipped with an xy scanning stage (Bios-T, Sigma Koki, Tokyo, Japan). The microscope was also equipped with a stage-top mini-incubator (WSKM, Tokai Hit, Shizuoka, Japan), which maintained the temperature of the culture plate at 28.5°C. Videos of medaka embryos were recorded as sequential phase-contrast images with a 10× or 20× objective at a frame rate of 150 fps, a resolution of 2048×2048 pixels and a depth of 8 bits.
Evaluation of beating heart with MVP algorithm
To evaluate cardiac systolic and diastolic motion of the medaka heart from the high-speed video imaging of the embryos, we have applied the MVP method as previously reported (Hayakawa et al., 2012; Ghanbari, 1990). Briefly, each frame was divided into square blocks of N×N pixels (Fig. S4). Then, for a maximum motion displacement of w pixels per frame, the current block of pixels was matched to the corresponding block at the same coordinates in the previous frame within a square window of width N+2w. (Optimal values of N and w for the cardiac motion detection may vary with the observation magnification and resolution of the employed camera. Here, we set N=16 and w=4. These values were determined empirically based on the throughput speed of calculation and accuracy of the block-matching detection.) The best match on the basis of a matching criterion yielded the displacement. The mean absolute error (MAE) was used as the matching criterion. The matching function is given by
 |
where ft(m,n) represents the intensity at coordinates (m,n) in the current block of N×N pixels and ft-1(m+i,n+j) represents the intensity at new coordinates (m+i,n+j) in the corresponding block in the previous frame. We performed this calculation for every 4×4 pixels in the region of interest (ROI).
Genetic mapping and positional cloning
Genetic mapping was performed as described previously (Kimura et al., 2005). Briefly, an nsh mutant on the Qurt genetic background was crossed with the Kaga strain to obtain F1 offspring, which were then crossed to obtain the nsh mutant embryos for mapping. A pooled bulk segregation analysis was performed to localize the nsh mutation on the medaka linkage group (Kimura et al., 2005). Further mapping was also done using custom-designed markers based on the sequence polymorphisms that differed between the Qurt and Kaga strains. The following primers and restriction enzymes were used for the mapping: for TTN exon 90, F 5′-AACTTCACAGGCTTCAGGTC-3′ and R 5′-CAGCATCTGTGACGTAGCTC-3′ (HaeIII); for TTN intron 193-194, F 5′-CCGTGTAACCAACCTCACTG-3′ and R 5′-GGCTTGGTCCATTCAAGTGT-3′ (HaeIII); for TTN 3′UTR, F 5′-CAGGAATTGGTCCTGAAAGG-3′ and R 5′-TCGACTTGGGTGTTTTCAGA-3′; for LG 21_30057841, F 5′-AATAGGTTGAGGCTGCATGG-3′ and R 5′-TTCACTGGTTCTTGGCGTTC-3′ (HaeIII). The reference coding sequence of TTN cDNA was in the Ensembl DNA sequence database under the accession number ENSORLT00000022736.
RT-PCR analysis
Hearts were harvested from WT and nsh mutant embryos (n=50 for each) at 3 dpf. Total RNA was extracted using Trizol reagent (Invitrogen). For RT-PCR analysis, we carried out oligo-dT primed reverse transcription on aliquots (1 µg) of total RNA and used 1/10 of the single-strand cDNA products for each PCR amplification. Gene-specific primers were designed based on published sequences. ef1α was used as an internal control. The following primers were used for RT-PCR analysis: for N-terminal TTN, F 5′-GCTCTGCACAAAGAGCTGTC-3′ and R 5′-GCAAGATGTGCTGATGGTTC-3′; for A-I junction TTN, F 5′-GCAAGCCAAGAACAAGTTTGA-3′ and R 5′-AGAAAAGGTCGGGACAGAGG-3′; for TTN exon 204, F 5′-TTGTTCATGTCCATCGTGGT-3′ and R 5′-GCTCCTCTGGAGTTGATTGC-3′; for titin kinase domain, F 5′-AATGTTGCAAGGCACAAAAA-3′ and R 5′-AGCCTCAAGGCTAATGTCCT-3′; for ef1α, F 5′-ATCGTTGCTGCTGGTGTTG-3′ and R 5′-AGGCGATGTGAGCTGTGTG-3′; for N2B isoform, F 5′-TATGCCACAACAGCAGGAGA-3′ and R 5′-AAGCCTTGCAGGTGTATTCG-3′; for N2BA isoform, F 5′-TATGCCACAACAGCAGGAGA-3′ and R 5′-TTTGGTCTTTGCAGCCTCTT-3′.
Overexpression of TTN Ig domain
A WT TTN cDNA fragment covering A156 (from bp89426 to bp89711 of NM_133378 corresponding to aa29735-aa29829) or TTN mutants carrying the A-to-T change (E29783V mutation equivalent of the medaka mutation D23186V) was cloned into the pCS2+ expression vector (Turner and Weintraub, 1994). A capped RNA linked to the cDNA for GFP was synthesized by an MMESSAGE mMACHINE Kit (Ambion) and injected into the cytoplasm of one-cell-stage embryos at a final concentration of 500 ng/µl.
Cloning of titin fragment
We prepared fragments of human TTN by PCR from a TTN A156 Ig domain construct as templates. A WT TTN cDNA fragment covering the A156 (from bp89426 to bp89711 of NM_133378 corresponding to aa29735-aa29829) domain was obtained by PCR from cDNAs prepared from total heart RNA, and the A-to-T substitution mutant (E29783V mutation equivalent of the medaka mutation D23186V) was created by the primer-mediated mutagenesis method.
Constructs for epitope-tagged proteins
The cDNA fragments of WT and mutant TTN were cloned into 3HA-tagged pcDNA3-NTAP. Full-length MURF1 fragment in a Myc-tagged pCMV-Tag3B construct (McElhinny et al., 2002) was cloned into Flag-tagged pcDNA3-NTAP. The Myc-tagged ubiquitin construct was a kind gift from Dr Nakada (Osaka University, Osaka, Japan). These constructs were sequenced to ensure that no errors were introduced.
Cellular transfection, protein extraction and immunoprecipitation
A total of 8 µg of plasmid DNA was transfected into semi-confluent HEK293FT cells on 6-cm-diameter culture dishes using Lipofectamine 2000 (Invitrogen). Epoxomicin or DMSO was added to the culture 4 h before lysate preparation. At 24 h after transfection, cells were lysed in 400 µl RIPA buffer [25 mM Tris-HCl pH 7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate, 0.1% sodium dodecyl sulfate (SDS)] with protease inhibitor, incubated on ice for 30 min and centrifuged at 15,000 rpm (16,000 g) for 30 min. Supernatants were subjected to WB and immunoprecipitation (IP). For IP, lysates were diluted 1:10 using TGN buffer (50 mM Tris-HCl pH7.5, 150 mM NaCl, 1% Tween-20, 0.3% NP40) and precleaned by protein G PLUS-Agarose (Santa Cruz Biotechnology). The precleaned lysates were incubated with 1 µg anti-HA high-affinity (3F10, Roche) or normal IgG (GE Healthcare) for 3 h and combined with 20 µl protein G PLUS-Agarose (Santa Cruz Biotechnology). The lysates with agarose-bead complexes were incubated overnight with rotation. The bead complexes were washed in TGN four times and twice in PBS. The beads were suspended in 2×Laemmli sample buffer (Bio-Rad) containing 15% 2-mercaptoethanol and boiled for 10 min.
Western blotting
Cellular lysates and IPs were separated by SDS-PAGE and transferred to polyvinylidene fluoride (PVDF) membranes. After a pre-incubation with 3% skim milk in Tris-buffered saline (TBS), the membrane was incubated with primary antibody overnight. After TBS washing, the membrane was incubated with an appropriate secondary antibody {anti-rabbit or anti-mouse IgG HRP-conjugated Ab (1:10,000 in 3% skim milk in TBS; GE Healthcare), mouse TrueBlot ULTRA: anti-mouse Ig HRP [1:1000 in 3% skim milk in TBS containing 0.1% Tween-20 (TBST)]} for 1 h. After five more washes in TBST, signals were visualized using the Chemi-Lumi One Super (Nacalai) and Luminescent Image Analyzer LAS-3000 mini (Fujifilm, Tokyo, Japan).
Antibodies
We used the following primary antibodies: first antibodies: anti-Flag (1:1000 in 5% BSA/TBST, M2, F7425, Sigma-Aldrich), anti-HA (1:2000 in 3% skim milk/TBST, clone HA-7, H9658 Sigma-Aldrich), myc (1:400 in 5% BSA/TBST, clone 9E10, sc-40, Santa Cruz Biotechnology) and GAPDH (1:1000 in 5% BSA/TBST, 14C10, rabbit mAb; Cell Signaling Technology); second antibodies: ECL anti-mouse IgG, peroxidase-linked species-specific F(ab’)2 fragment (from sheep) (1:10,000 in 3% skim milk/TBST, NA9310; GE Healthcare), ECL anti-rabbit IgG, peroxidase-linked species-specific F(ab’)2 fragment (from donkey) (1:10,000 in 3% skim milk/TBST, NA9340; GE Healthcare), and mouse TrueBlot ULTRA: anti-mouse Ig HRP (1:1000 in 3% skim milk/TBST; eBioscience). IPs used the anti-HA high-affinity (3F10; Roche) normal mouse IgG (GE Healthcare).
Clinical subjects
We studied 96 genetically unrelated Japanese patients with HCM, who carried apparent family history of HCM consistent with an autosomal dominant trait. They were diagnosed with HCM according to the diagnostic criteria as described previously (Arimura et al., 2009). They had been analyzed for mutations in the known disease genes for HCM, i.e. genes for contractile elements, Z-disc elements and I band elements, and no disease-associated mutation was found (Arimura et al., 2009). Control subjects were 400 healthy Japanese individuals selected at random from non-HCM patients at Tokyo Medical and Dental Hospital. Blood samples were obtained from the subjects after written informed consent and the research protocol was approved by the Ethics Review Committee of Medical Research Institute, Tokyo Medical and Dental University, Japan.
Mutational analysis
Genomic DNA extracted from blood samples of each individual was subjected to PCR in an exon-by-exon manner by using primer pairs specific to exons 296-307 of TTN (GenBank accession no. NM_133378), which encode for titin at the M-line–A-band transition zone including the titin-kinase domain. Sequences of primers and PCR conditions used in this study are listed in Table S1. PCR products were analyzed by direct sequencing using Big Dye Terminator chemistry (Applied Biosystems) and an ABI3100 DNA analyzer (Applied Biosystems).
Co-immunoprecipitation assay
We used cDNA fragments of human TTN and MURF1 by PCR from TTN A156, A160-161 and A168-170 Ig-like domain constructs and a MURF1 full-length construct, respectively, as templates for PCR. A WT TTN cDNA fragment covering the A156 (from bp89426 to bp89711 of NM_133378 corresponding to aa29735-aa29829), A160-161 (from bp90626 to bp91202 corresponding to aa30134-aa30326), A168 (from bp93006 to bp93287 corresponding to aa30928-aa31021), A169 (from bp93288 to bp93581 corresponding to aa31022-aa31119) or A168-A170 (from bp93006 to bp93908 corresponding to aa30928-aa31228) domains was obtained by PCR, and TTN mutants carrying A-to-T (E29783V mutation equivalent of the medaka mutation D23186V), T-to-G (an HCM-associated S30186A mutation) or T-to-A (another HCM-associated D30994N mutation) substitutions were created by the primer-mediated mutagenesis method. A full-length MURF1 cDNA fragment spanning from bp137 to bp1198 of GenBank Accession No. NM_032588 (corresponding to aa1-aa354) was obtained by PCR. The TTN cDNA fragment was cloned into pEGFP-C1 (Clontech, CA, USA), while the MURF1 cDNA fragment was cloned into myc-tagged pCMV-Tag3 (Stratagene, CA, USA). These constructs were sequenced to ensure that no errors were introduced.
Cellular transfection and protein extraction were performed as described previously (Arimura et al., 2009) and co-IP assays were done using the Catch and Release v2.0 Reversible Immunoprecipitation System according to the manufacturer's instructions. IPs were separated by SDS-PAGE and transferred to nitrocellulose membrane. After a pre-incubation with 3% skim milk in PBS, the membrane was incubated with primary rabbit anti-myc polyclonal or mouse anti-GFP monoclonal Ab (1:100, Santa Cruz Biotechnology), and with secondary goat anti-rabbit (for polyclonal Ab) or rabbit anti-mouse (for monoclonal Ab) IgG HRP-conjugated Ab (1:2000, Dako A/S, Glostrup, Denmark). Signals were visualized by Immobilon Western Chemiluminescent HRP Substrate (Millipore, MA, USA) and Luminescent Image Analyzer LAS-3000mini (Fujifilm, Tokyo, Japan), and their densities were quantified using Multi Gauge ver3.0 (Fujifilm, Tokyo, Japan). Numerical data were expressed as means±s.e.m. Statistical differences were analyzed using Student's t-test for paired values. A P-value of less than 0.05 was considered to be statistically significant.
In vitro ubiquitination assay
In vitro ubiquitination reactions contained as E1 ligase 100 nM UBE1 (Boston Biochem), and 1 µM UbcH5c as E2 ligase (Boston Biochem), 150 µM ubiquitin, 4 mM ATP and 2.5 µM recombinant titin A168-170 fragment. Reactions were started by addition of 2 µM MURF1 or MURF2, respectively. After incubation for 4 h at room temperature, samples were boiled in SDS loading buffer, and products were separated by SDS-PAGE and blotted onto nitrocellulose membranes. Titin-specific products were detected by using antibodies directed to titin A169 or titin A168-170.
Supplementary Material
Acknowledgements
We thank the National Bio Resource Project for supplying medaka strains and other support. We thank Dr T. Hayakawa and T. Kunihiro from Sony Corporation for their technical help in the high-speed video recording of medaka embryos and in the image analysis using the MVP method. We are also grateful to Ms Ono for maintenance of medaka.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Author contributions
Conceptualization: N.M., T.A., S.H.Y., M.O., H.E., R.K., F.H., T.S., A. Kawakami, A.G., T.F., S.L., S.M.; Methodology: Y.H., M.O., S.L., S.M.; Validation: S.M.; Formal analysis: Y.H., S.H.Y.; Investigation: Y.H., N.M., T.A., S.H.Y., M.O.; Resources: A. Kawakami; Data curation: F.H., S.M.; Writing - original draft: Y.H., N.M., R.K., A.G., S.L., S.M.; Writing - review & editing: N.M., H.E., F.H., T.S., A. Kimura, S.M.; Visualization: R.K., A.G., S.M.; Supervision: M.O., R.K., T.S., A. Kawakami, T.F., K.F., A. Kimura, S.M.; Project administration: T.S., A.G., K.F., A. Kimura, S.M.; Funding acquisition: T.S., T.F., K.F., A. Kimura, S.M.
Funding
This study was supported in part by the program for Grant-in-Aid for Scientific Research (21390248, 24390248, 16H05305, 25670397, 25293096 and 19590832) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, a research grant for Idiopathic Cardiomyopathy from the Ministry of Health, Labour and Welfare, Japan, and a grant for Basic Scientific Cooperation Program between Japan and Korea from the Japan Society for the Promotion of Science. It was also supported by the Joint Usage/Research Program of Medical Research Institute, a follow-up grant from the Tokyo Medical and Dental University and Association Française contre les Myopathies (Grant No. 15261). This investigation was also supported in parts by The Mochida Memorial Foundation for Medical and Pharmaceutical Research, The NOVARTIS Foundation (Japan) for the Promotion of Science, Japan Heart Foundation, the Institute of Life Science, KEIO Gijuku Academic Development Funds and Keio Kanrinmaru project, Japan.
Supplementary information
Supplementary information available online at http://dmm.biologists.org/lookup/doi/10.1242/dmm.041103.supplemental
References
- Arimura T., Bos J. M., Sato A., Kubo T., Okamoto H., Nishi H., Harada H., Koga Y., Moulik M., Doi Y. L. et al. (2009). Cardiac ankyrin repeat protein gene (ANKRD1) mutations in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 54, 334-342. 10.1016/j.jacc.2008.12.082 [DOI] [PubMed] [Google Scholar]
- Bodine S. C., Latres E., Baumhueter S., Lai V. K., Nunez L., Clarke B. A., Poueymirou W. T., Panaro F. J., Na E., Dharmarajan K. et al. (2001). Identification of ubiquitin ligases required for skeletal muscle atrophy. Science 294, 1704-1708. 10.1126/science.1065874 [DOI] [PubMed] [Google Scholar]
- Burggren W. W. and Pinder A. W. (1991). Ontogeny of cardiovascular and respiratory physiology in lower vertebrates. Annu. Rev. Physiol. 53, 107-135. 10.1146/annurev.ph.53.030191.000543 [DOI] [PubMed] [Google Scholar]
- Carmignac V., Salih M. A., Quijano-Roy S., Marchand S., Al Rayess M. M., Mukhtar M. M., Urtizberea J. A., Labeit S., Guicheney P., Leturcq F. et al. (2007). C-terminal titin deletions cause a novel early-onset myopathy with fatal cardiomyopathy. Ann. Neurol. 61, 340-351. 10.1002/ana.21089 [DOI] [PubMed] [Google Scholar]
- Centner T., Yano J., Kimura E., McElhinny A. S., Pelin K., Witt C. C., Bang M.-L., Trombitas K., Granzier H., Gregorio C. C. et al. (2001). Identification of muscle specific ring finger proteins as potential regulators of the titin kinase domain. J. Mol. Biol. 306, 717-726. 10.1006/jmbi.2001.4448 [DOI] [PubMed] [Google Scholar]
- Da Silva Lopes K., Pietas A., Radke M. H. and Gotthardt M. (2011). Titin visualization in real time reveals an unexpected level of mobility within and between sarcomeres. J. Cell Biol. 193, 785-798. 10.1083/jcb.201010099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisterfer-Lowrance A. A., Kass S., Tanigawa G., Vosberg H.-P., McKenna W., Seidman C. E. and Seidman J. G. (1990). A molecular basis for familial hypertrophic cardiomyopathy: a beta cardiac myosin heavy chain gene missense mutation. Cell 62, 999-1006. 10.1016/0092-8674(90)90274-I [DOI] [PubMed] [Google Scholar]
- Gerull B., Gramlich M., Atherton J., McNabb M., Trombitã¡S K., Sasse-Klaassen S., Seidman J. G., Seidman C., Granzier H., Labeit S. et al. (2002). Mutations of TTN, encoding the giant muscle filament titin, cause familial dilated cardiomyopathy. Nat. Genet. 30, 201-204. 10.1038/ng815 [DOI] [PubMed] [Google Scholar]
- Ghanbari M. (1990). The cross-search algorithm for motion estimation. IEEE Trans. Commun. 38, 950 10.1109/26.57512 [DOI] [Google Scholar]
- Granzier H. L. and Irving T. C. (1995). Passive tension in cardiac muscle: contribution of collagen, titin, microtubules, and intermediate filaments. Biophys. J. 68, 1027-1044. 10.1016/S0006-3495(95)80278-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granzier H. L., Radke M. H., Peng J., Westermann D., Nelson O. L., Rost K., King N. M. P., Yu Q., Tschöpe C., Mcnabb M. et al. (2009). Truncation of titin's elastic PEVK region leads to cardiomyopathy with diastolic dysfunction. Circ. Res. 105, 557-564. 10.1161/CIRCRESAHA.109.200964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregorio C. C., Granzier H., Sorimachi H. and Labeit S. (1999). Muscle assembly: a titanic achievement? Curr. Opin. Cell Biol. 11, 18-25. 10.1016/S0955-0674(99)80003-9 [DOI] [PubMed] [Google Scholar]
- Hayakawa T., Kunihiro T., Dowaki S., Uno H., Matsui E., Uchida M., Kobayashi S., Yasuda A., Shimizu T. and Okano T. (2012). Noninvasive evaluation of contractile behavior of cardiomyocyte monolayers based on motion vector analysis. Tissue Eng. Part C Methods 18, 21-32. 10.1089/ten.tec.2011.0273 [DOI] [PubMed] [Google Scholar]
- Herman D. S., Lam L., Taylor M. R., Wang L., Teekakirikul P., Christodoulou D., Conner L., Depalma S. R., Mcdonough B., Sparks E. et al. (2012). Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med. 366, 619-628. 10.1056/NEJMoa1110186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C. Y. and Seidman C. E. (2006). A contemporary approach to hypertrophic cardiomyopathy. Circulation 113, e858-e862. 10.1161/CIRCULATIONAHA.105.591982 [DOI] [PubMed] [Google Scholar]
- Itoh-Satoh M., Hayashi T., Nishi H., Koga Y., Arimura T., Koyanagi T., Takahashi M., Hohda S., Ueda K., Nouchi T. et al. (2002). Titin mutations as the molecular basis for dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 291, 385-393. 10.1006/bbrc.2002.6448 [DOI] [PubMed] [Google Scholar]
- Iwamatsu T. (2004). Stages of normal development in the medaka Oryzias latipes. Mech. Dev. 121, 605-618. 10.1016/j.mod.2004.03.012 [DOI] [PubMed] [Google Scholar]
- Kasahara M., Naruse K., Sasaki S., Nakatani Y., Qu W., Ahsan B., Yamada T., Nagayasu Y., Doi K., Kasai Y. et al. (2007). The medaka draft genome and insights into vertebrate genome evolution. Nature 447, 714-719. 10.1038/nature05846 [DOI] [PubMed] [Google Scholar]
- Kedar V., McDonough H., Arya R., Li H.-H., Rockman H. A. and Patterson C. (2004). Muscle-specific RING finger 1 is a bona fide ubiquitin ligase that degrades cardiac troponin I. Proc. Natl. Acad. Sci. USA 101, 18135-18140. 10.1073/pnas.0404341102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura A. (2008). Molecular etiology and pathogenesis of hereditary cardiomyopathy. Circ. J. 72 Suppl. A, A38-A48. 10.1253/circj.CJ-08-0050 [DOI] [PubMed] [Google Scholar]
- Kimura T., Yoshida K., Shimada A., Jindo T., Sakaizumi M., Mitani H., Naruse K., Takeda H., Inoko H., Tamiya G. et al. (2005). Genetic linkage map of medaka with polymerase chain reaction length polymorphisms. Gene 363, 24-31. 10.1016/j.gene.2005.07.043 [DOI] [PubMed] [Google Scholar]
- Lahmers S., Wu Y., Call D. R., Labeit S. and Granzier H. (2004). Developmental control of titin isoform expression and passive stiffness in fetal and neonatal myocardium. Circ. Res. 94, 505-513. 10.1161/01.RES.0000115522.52554.86 [DOI] [PubMed] [Google Scholar]
- Lange S., Ehler E. and Gautel M. (2006). From A to Z and back? Multicompartment proteins in the sarcomere. Trends Cell Biol. 16, 11-18. 10.1016/j.tcb.2005.11.007 [DOI] [PubMed] [Google Scholar]
- Lange S., Xiang F. and Yakovenko A. (2005). The kinase domain of titin controls muscle gene expression and protein turnover. Science 308, 1599-1603. 10.1126/science.1110463 [DOI] [PubMed] [Google Scholar]
- Lewinter M. M. and Granzier H. (2010). Cardiac titin: a multifunctional giant. Circulation 121, 2137-2145. 10.1161/CIRCULATIONAHA.109.860171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makarenko I., Opitz C. A., Leake M. C., Neagoe C., Kulke M., Gwathmey J. K., del Monte F., Hajjar R. J. and Linke W. A. (2004). Passive stiffness changes caused by upregulation of compliant titin isoforms in human dilated cardiomyopathy hearts. Circ. Res. 95, 708-716. 10.1161/01.RES.0000143901.37063.2f [DOI] [PubMed] [Google Scholar]
- McElhinny A. S., Kakinuma K., Sorimachi H., Labeit S. and Gregorio C. C. (2002). Muscle-specific RING finger-1 interacts with titin to regulate sarcomeric M-line and thick filament structure and may have nuclear functions via its interaction with glucocorticoid modulatory element binding protein-1. J. Cell Biol. 157, 125-136. 10.1083/jcb.200108089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. K., Granzier H. and Ehler E. (2004). The sensitive giant: the role of titin-based stretch sensing complexes in the heart. Trends Cell Biol. 14, 119-126. 10.1016/j.tcb.2004.01.003 [DOI] [PubMed] [Google Scholar]
- Moriyama A., Inohaya K., Maruyama K. and Kudo A. (2010). Bef medaka mutant reveals the essential role of c-myb in both primitive and definitive hematopoiesis. Dev. Biol. 345, 133-143. 10.1016/j.ydbio.2010.06.031 [DOI] [PubMed] [Google Scholar]
- Müller S., Lange S., Gautel M. and Wilmanns M. (2007). Rigid conformation of an immunoglobulin domain tandem repeat in the A-band of the elastic muscle protein titin. J. Mol. Biol. 371, 469-480. 10.1016/j.jmb.2007.05.055 [DOI] [PubMed] [Google Scholar]
- Neagoe C., Kulke M., Del Monte F., Gwathmey J. K., de Tombe P. P., Hajjar R. J. and Linke W. A. (2002). Titin isoform switch in ischemic human heart disease. Circulation 106, 1333-1341. 10.1161/01.CIR.0000029803.93022.93 [DOI] [PubMed] [Google Scholar]
- Ojima K., Ono Y., Hata S., Koyama S., Doi N. and Sorimachi H. (2005). Possible functions of p94 in connectin-mediated signaling pathways in skeletal muscle cells. J. Muscle Res. Cell Motil. 26, 409-417. 10.1007/s10974-005-9023-8 [DOI] [PubMed] [Google Scholar]
- Opitz C. A., Leake M. C., Makarenko I., Benes V. and Linke W. A. (2004). Developmentally regulated switching of titin size alters myofibrillar stiffness in the perinatal heart. Circ. Res. 94, 967-975. 10.1161/01.RES.0000124301.48193.E1 [DOI] [PubMed] [Google Scholar]
- Ouzounian M., Lee D. S. and Liu P. P. (2008). Diastolic heart failure: mechanisms and controversies. Nat. Clin. Pract. Cardiovasc. Med. 5, 375-386. 10.1038/ncpcardio1245 [DOI] [PubMed] [Google Scholar]
- Radke M. H., Peng J., Wu Y., Mcnabb M., Nelson O. L., Granzier H. and Gotthardt M. (2007). Targeted deletion of titin N2B region leads to diastolic dysfunction and cardiac atrophy. Proc. Natl. Acad. Sci. USA 104, 3444-3449. 10.1073/pnas.0608543104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rottbauer W., Baker K., Wo Z. G., Mohideen M.-A. P. K., Cantiello H. F. and Fishman M. C. (2001). Growth and function of the embryonic heart depend upon the cardiac-specific L-type calcium channel alpha1 subunit. Dev. Cell 1, 265-275. 10.1016/S1534-5807(01)00023-5 [DOI] [PubMed] [Google Scholar]
- Sakamoto D., Kudo H., Inohaya K., Yokoi H., Narita T., Naruse K., Mitani H., Araki K., Shima A., Ishikawa Y. et al. (2004). A mutation in the gene for delta-aminolevulinic acid dehydratase (ALAD) causes hypochromic anemia in the medaka, Oryzias latipes. Mech. Dev. 121, 747-752. 10.1016/j.mod.2004.03.030 [DOI] [PubMed] [Google Scholar]
- Satoh M., Takahashi M., Sakamoto T., Hiroe M., Marumo F. and Kimura A. (1999). Structural analysis of the titin gene in hypertrophic cardiomyopathy: identification of a novel disease gene. Biochem. Biophys. Res. Commun. 262, 411-417. 10.1006/bbrc.1999.1221 [DOI] [PubMed] [Google Scholar]
- Seeley M., Huang W., Chen Z., Wolff W. O., Lin X. and Xu X. (2007). Depletion of zebrafish titin reduces cardiac contractility by disrupting the assembly of Z-discs and A-bands. Circ. Res. 100, 238-245. 10.1161/01.RES.0000255758.69821.b5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taneda Y., Konno S., Makino S., Morioka M., Fukuda K., Imai Y., Kudo A. and Kawakami A. (2010). Epigenetic control of cardiomyocyte production in response to a stress during the medaka heart development. Dev. Biol. 340, 30-40. 10.1016/j.ydbio.2010.01.014 [DOI] [PubMed] [Google Scholar]
- Thisse C. and Thisse B. (2008). High-resolution in situ hybridization to whole-mount zebrafish embryos. Nat. Protoc. 3, 59-69. 10.1038/nprot.2007.514 [DOI] [PubMed] [Google Scholar]
- Turner D. L. and Weintraub H. (1994). Expression of achaete-scute homolog 3 in Xenopus embryos converts ectodermal cells to a neural fate. Genes Dev. 8, 1434-1447. 10.1101/gad.8.12.1434 [DOI] [PubMed] [Google Scholar]
- Van Heerebeek L., Borbely A., Niessen H. W., Bronzwaer J. G. F., Van Der Velden J., Stienen G. J. M., Linke W. A., Laarman G. J. and Paulus W. J. (2006). Myocardial structure and function differ in systolic and diastolic heart failure. Circulation 113, 1966-1973. 10.1161/CIRCULATIONAHA.105.587519 [DOI] [PubMed] [Google Scholar]
- Warren C. M., Krzesinski P. R., Campbell K. S., Moss R. L. and Greaser M. L. (2004). Titin isoform changes in rat myocardium during development. Mech. Dev. 121, 1301-1312. 10.1016/j.mod.2004.07.003 [DOI] [PubMed] [Google Scholar]
- Weinert S., Bergmann N., Luo X., Erdmann B. and Gotthardt M. (2006). M line-deficient titin causes cardiac lethality through impaired maturation of the sarcomere. J. Cell Biol. 173, 559-570. 10.1083/jcb.200601014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Bell S. P., Trombitas K., Witt C. C., Labeit S., Lewinter M. M. and Granzier H. (2002). Changes in titin isoform expression in pacing-induced cardiac failure give rise to increased passive muscle stiffness. Circulation 106, 1384-1389. 10.1161/01.CIR.0000029804.61510.02 [DOI] [PubMed] [Google Scholar]
- Xu X., Meiler S. E., Zhong T. P., Mohideen M., Crossley D. A., Burggren W. W. and Fishman M. C. (2002). Cardiomyopathy in zebrafish due to mutation in an alternatively spliced exon of titin. Nat. Genet. 30, 205-209. 10.1038/ng816 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.