Abstract
Rabies, the most lethal zoonotic disease, is caused by lyssaviruses, most often by rabies virus (RABV). Despite control efforts, sporadic outbreaks in wildlife populations are largely unpredictable, underscoring our incomplete knowledge of what governs viral transmission and spread in reservoir hosts. Furthermore, the evolutionary history of RABV and related lyssaviruses remains largely unclear. Robust surveillance efforts combined with diagnostics and disease modeling are now providing insights into the epidemiology and evolution of rabies. The contributions of host [G] immune status, nature of exposure and strain [G] differences all clearly influence infection and transmission dynamics. In this Review, we focus on wildlife rabies, and synthesize current knowledge in the rapidly-advancing fields of rabies epidemiology and evolution, and advocate for multi-disciplinary approaches to advance our understanding of this disease.
Subject categories: Biological sciences / Microbiology / Virology / Viral evolution[URI /631/326/596/2554], Biological sciences / Microbiology / Virology / Viral pathogenesis[URI /631/326/596/2555], Biological sciences / Microbiology / Virology / Virus–host interactions[URI /631/326/596/2557]
Much of the molecular virology of rabies virus has been well-characterized, and we are now gaining a better understanding of how nuanced infection dynamics and immune status relates to transmission. In this Review, Schnell and colleagues review our current knowledge of rabies virus transmission, spread and evolution, and they explore their determining factors.
Introduction
Rabies disease, a lethal encephalitis, of which the causative agent is believed to be rabies virus (RABV), has been documented in numerous historical records dating back at least 4000 years and spanning continents1–4. Despite substantial advances in understanding RABV biology, a vaccine regimen that can protect against disease both before and after exposure, and mass vaccination campaigns designed to diminish the circulation of RABV in wild and domestic carnivoran reservoirs [G] the virus continues to establish itself in new host species and geographical areas, threatening animal and human lives.
In the twentieth-century, efforts to defeat rabies were ostensibly successful: North America saw a drop in annual human deaths to single-digit numbers by the 1990s5, and Western Europe, where RABV infections in foxes was once rampant, is now considered ‘rabies free’6. However, in North America, epizootics in raccoons, skunks, foxes and bats belie progress made7–11. Moreover, RABV vampire bat variants [G] have spread in South America, new RABV lineages have been discovered, expanding the list of reservoir hosts, and efforts to eliminate RABV infections in domestic dogs have failed, posing a sustained threat of re-emergence10,12,13. In Europe, Africa, Asia and Australia, RABV-related lyssaviruses, which cause the same fatal disease as RABV, circulate in bats, and RABV-targeted control efforts do not always protect against these viruses11,14. Across the globe, particularly in Africa, Asia and India, domestic dog-adapted RABV wages a neglected epidemic that claims an estimated 59,000 human lives annually15,16.
How RABV establishes transmission cycles in new hosts is mostly unknown. Moreover, how such host shifts can be prevented remains an open question. There are dozens of RABV strains, each of which associate closely with a host mammal species in either the chiroptera or carnivora orders. Mechanisms of transmission and evolution may differ within each virus-host relationship. More importantly, it is unclear what prevents RABV from adapting to species of other mammalian orders. Although cross-species transmissions usually result in ‘dead-end’ infections, exceptional host shifts continue to occur in unpredicted ways. Although our understanding of RABV-related lyssaviruses continues to grow (Box 1)17–21, how lyssaviruses circulate and their potential for outbreak remain to be fully established, as their pathology is indistinguishable from that of RABV22. It is almost certain that infection with non-RABV lyssaviruses occurs but goes unnoticed based on the lack of discriminatory diagnostic tools in many countries23. This assumption is supported by the finding that even infection with RABV has been misdiagnosed as malaria encephalitis in children24. Importantly, some lyssaviruses are divergent enough to resist protection from current vaccines and rabies immunoglobulin (RIG)25–27.
Box 1: Discovery of rabies virus-related viruses.
In 1956, a pathogenic virus was discovered in the brains of fruit bats (Eidolon helvum) in Nigeria160. The serological tests available at the time identified it as related to, but distinct from, RABV. A similar result was found after a South African man died from a rabies-like illness following a bat bite in 1970161. The discovery of Lagos bat and Duvenhage lyssaviruses were the first in a series of discoveries of rabies virus (RABV)-related viruses that now comprise the lyssavirus genus, which includes RABV. There are fourteen members of the genus (see table), and two recently discovered lyssaviruses: Lleida bat lyssavirus (LLEBV) discovered in Spain in 2011 and Gannoruwa bat lyssavirus (GBLV) discovered in Sri Lanka in 201418,19. Lyssaviruses are further grouped into two phylogroups, an organization based on serum cross-reactivity against the viral proteins and thresholds in genetic sequence differences14,17. However, the divergence of Ikoma (IKOV) and West Caucasian bat (WCBV) lyssaviruses, which cluster with neither phylogroups, suggests that phylogroup organization may be more complex than originally proposed21,25. Non-RABV lyssaviruses have been traced almost exclusively to bats, with two notable exceptions: Mokola lyssavirus (MOKV) has been found across six African countries in shews162, domestic dogs and cats20,151, and was responsible for at least one human death163; Ikoma lyssavirus (IKOV) was recently discovered in Tanzania in an African civet, despite decades of local carnivore surveillance and research21,164. The persistent discovery of new lyssaviruses in Europe, Africa, Asia and Australia reflects the utility of continual RABV and lyssavirus surveillance and increasingly sensitive diagnostics, but also highlights potential unassessed risks. More members are likely to be discovered in coming years.
| Phylogroup | Species name | Abbreviation |
|---|---|---|
| Phylogroup I | Aravan lyssavirus | ARAV |
| Australian bat lyssavirus | ABLV | |
| Bokeloh bat lyssavirus | BBLV | |
| Duvenhage lyssavirus | DUVV | |
| European bat 1 lyssavirus | EBLV-1 | |
| European bat 2 lyssavirus | EBLV-2 | |
| Irkut lyssavirus | IRKV | |
| Khujand lyssavirus | KHUV | |
| Rabies lyssavirus | RABV | |
| Phylogroup II | Lagos bat lyssavirus | LBV |
| Mokola lyssavirus | MOKV | |
| Shimoni bat lyssavirus | SHIBV | |
| Unclassified | Ikoma lyssavirus | IKOV |
| West Caucasian bat lyssavirus | WCBV | |
| Lleida bat lyssavirus | LLEBV | |
| Gannoruwa bat lyssavirus | GBLV |
The current distribution and impact of RABV across the globe contrasts with how it has historically been studied: foundational understanding of RABV spread and transmission comes from studies on RABV infections in wildlife in North America and Western Europe, but RABV infections in canines in Africa and Asia, which is responsible for the vast majority of human fatalities, has been less studied. Similarly, our understanding of RABV biology largely stems from mouse models with a relatively small repertoire of strains. In both investigating the evolutionary history of lyssaviruses and working towards its elimination, our understanding benefits from a convergence of virology, epidemiology and ecology. In this Review, we first briefly discuss RABV biology for context, highlighting relevant new research. We then discuss RABV transmission, and explore enzootic maintenance and epizootic spread of the virus. Finally, we review molecular evolutionary dynamics, host adaptation and the origins of RABV.
Rabies virus biology
Molecular virology and life cycle.
RABV is a negative-stranded RNA virus of the Rhabdoviridae family28,29. RABV virions [G] are enveloped by a host cell-derived membrane and take on a bullet shape of about 200 nm by 80 nm. The bullet shape is likely influenced by the constraints of budding30 and viral uptake31. The relatively small RNA genome of the virus (~12 kb) encodes for five proteins: nucleoprotein (N), phosphoprotein (P), matrix protein (M), glycoprotein (G), and polymerase (L, in reference to the large size of the gene)28 (Figure 1A). The basic functions of lyssavirus proteins are well-conserved (Box 2).
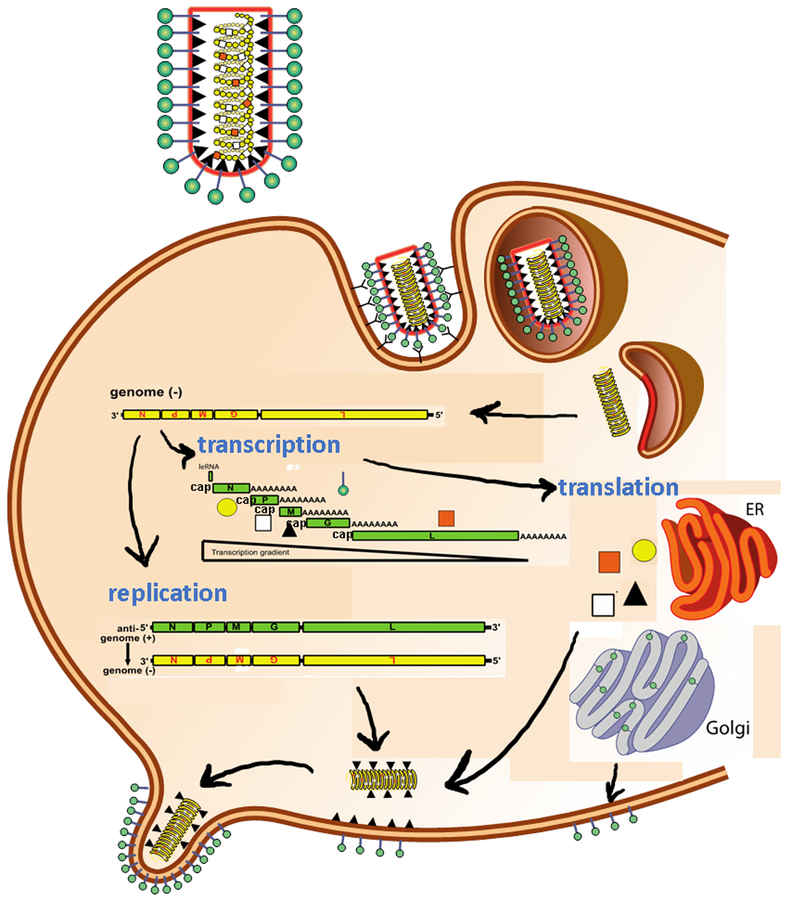
Figure 1a: Cellular life cycle of rabies virus.
In the first phase of the rabies virus (RABV) life cycle, the virus binds to the cell surface receptors via its glycoprotein and enters by endocytosis (step 1). Subsequently, the viral membrane fuses with the endosomal membrane to release the viral genome (uncoating, step 2). In the second phase, the encapsidated negative-stranded RNA genome is transcribed by the polymerase complex, starting with a short uncapped leader RNA (leRNA), followed by the transcription of 5′ end-capped (cap) and polyadenylated (A) mRNAs, and their translation into the viral proteins nucleoprotein (N), phosphoprotein (P), matrix protein (M), glycoprotein (G) and polymerase (L) (steps 3 and 4). Following replication, the full-length antigenomic RNA is encapsidated in the nucleoprotein protein along with the genomic RNA. The synthesized antigenome functions as a template for the synthesis of additional copies of genomic RNA (step 5). In the last phase, the viral components are assembled and the RABV virions bud and are released, starting a new round of infection (step 6).
Box 2: Basic functions of lyssavirus proteins.
N proteins encapsidate the genomic and antigenomic RNA. The resulting ribonucleoprotein (RNP) complex protects the RNA from degradation by RNAses. The phosphoprotein has at least two functions: it is the non-catalytic subunit of the polymerase complex, providing the connection between the RNP and viral polymerase protein, and antagonizes innate immunity in the infected host. The matrix protein coats the inside of the viral envelope, bridging the carboxy-terminal region of the glycoprotein and the RNP. Importantly, it sequesters the glycoprotein in a concentrated area of the cell membrane to aid in viral budding, although the role of the cytoplasmic region of the glycoprotein has been challenged by the finding that foreign glycoproteins with heterologous cytoplasmic sequences are well-incorporated into the budding virion39,165,166. The glycoprotein is a transmembrane protein which, in a trimer formation, constitutes the sole protein on the outer surface of the rabies virus (RABV) virion. The glycoprotein interacts with a host cell receptor and mediates pH-triggered fusion between the viral and host membranes, which results in the release of the RNP into the host cytoplasm. The glycoprotein is also the primary target for virus-neutralizing antibodies, which are necessary for protection against rabies disease. A unique feature of the rhabdoviral glycoprotein is that it can revert to its prefusion conformation once a neutral pH is restored167, unlike the permanent fusion conformation exhibited by other viral proteins. The fusion mechanism of the closely-related vesicular stomatitis virus (VSV) has recently been elucidated168; however a lack of structural information limits our full understanding of the glycoprotein of RABV. RABV encodes its own RNA-dependent RNA polymerase because mammalian cells are not equipped to transcribe negative-stranded RNA. Moreover and in contrast with plus-stranded RNA viruses, neither the RABV genome nor anti-genome are functional templates for the viral polymerase unless encapsidated by the nucleoprotein. Therefore, the virus requires its own polymerase to perform the primary transcription of mRNA from the anti-genomic RNP and initiate the viral life cycle within the infected cell. After a threshold of transcription has been achieved and a certain amount of viral proteins has been produced, the polymerase switches to replication mode in which it ignores stop and start signals used to produce single mRNAs and produces a single, positive-stranded encapsidated plus-sense RNA. This anti-genomic RNA serves as a template for more copies of the genomic viral RNA. Such newly produced RNP are assembled together with the matrix protein and the glycoprotein into new virions at the cell membrane.
The rabies life cycle and its resulting pathogenesis have been extensively studied and reviewed32–35. Briefly, RABV, with its modest genome and single surface glycoprotein, can infiltrate an astonishing number of mostly neuronal tissues in almost any mammal to induce its lethal pathology. This might lead one to assume that the receptor that RABV uses to enter the cells is exceptionally conserved. However, debate surrounds RABV receptor binding (Fig. 1b). In vitro and knockout in vivo experiments have homed in on three primary candidates: the nicotinic acetylcholine receptor (nAChR), neural cell adhesion molecule (NCAM, also known as CD56), and the low-affinity neurotrophin receptor, p75NTR 36. Overall consensus holds that glycoprotein can bind flexibly to all three receptors, and possibly others, as needed in different stages of the life cycle or in different hosts. Recent studies on virus internalization confirm that RABV uptake is mediated by classic clathrin-mediated endocytosis (Fig. 1B)37,38.
Figure 1b: RABV entry and transport in neurons.
The nicotinic acetylcholine receptor (nAchR) is located at the postsynaptic muscle membrane. It has been suggested that the nAchR receptor enriches RABV at the neuromuscular junction (NMJ, synaptic cleft), enabling more efficient infection of the connected motor neurons. Other research suggests that initial virus amplification occurs in muscle (indicated by the question mark), which indicates that nAchRs might be used to infect muscle cells. RABV can enter neurons by binding to NCAM or another, unknown receptor. Following uptake by clathrin-mediated endocytosis, RABV virions are then transported within the vesicle and are released in the cell body of the infected neurons, where replication and transcription occurs (not shown). Parts a and b modified from Ref 34
Infection usually begins in muscle tissue following a bite from an infected animal. The virus then crosses neuromuscular junctions to peripheral nerves and uses retrograde axonal transport to reach the central nervous system (CNS)39. It was originally believed that RABV did not replicate in muscle, but evidence now shows that replication occurs in some instances in muscle40. It is still unclear why RABV is not detected immediately after exposure, especially if it is replicating in muscle tissue; strong immune evasion is likely to be responsible (see below). Evidence suggests that the virus takes multiple routes to reach the CNS (such as via motor or sensory neurons), depending on the site of inoculation and post-infection time41.
Whereas the initial spread of RABV is exclusively retrograde, at the end stage of infection, RABV reverses its direction of transport and migrates out of the CNS in an anterograde fashion towards the periphery42. Centrifugal spread, especially to the salivary glands where the virus can easily transmit through a bite, is essential to restart the cycle. For much of its life cycle, RABV infection is asymptomatic, and clinical signs of neuronal dysfunction present only at late stages of the disease. Rabies disease then rapidly deteriorates the health of the host and leads to death from respiratory or heart failure, usually within days35. A few unusual examples of survival have been reported in humans, but interventions have not proven repeatable43,44.
Neurological symptoms can manifest in different ways. Often, infected animals (including humans) exhibit the ‘furious’ form of rabies disease, which is characterized by agitation and aggression45. In other cases, the disease manifests as paralysis (paralytic rabies), and sometimes the two forms alternate during the course of disease45. Variations in immune responses may have a role in the manifestation of disease46. Recent studies using RABV isolates [G] from canines exhibiting furious and paralytic disease strengthen anecdotal evidence that strains may also contribute to these phenotypes47. A distinctive hallmark of rabies disease is hydrophobia, in which the patient is extremely resistant to consuming, or even encountering water or other liquids. The neuropathogenesis, diagnosis and management of rabies disease in humans has been reviewed previously48.
It is becoming increasingly clear that the pace of rabies infection is determined in part by viral factors that differ between strains49, and possibly between lyssavirus species. Recent work comparing bat- and carnivore-derived variants in mice found increased neuroinvasiveness and lethality of the bat variant50, a pattern which may ultimately influence the clinical outcome and diagnosis of rabies51. However, though well-established, the use of mouse models to test the pathogenicity and neuroinvasiveness of lyssaviruses from diverse reservoirs tells an incomplete story. Experimental infections in bats suggest that, upon RABV exposure, they develop strong but sometimes sub-detectable immunological memory52–54. Such experiments highlight both the utility of examining variant phenotype in a host closer to its natural reservoir, as well as suspected differences between bat and terrestrial mammal immunity(Figure 2)55. The dose of RABV administered during an exposure is also important52. Higher doses result in shorter incubation times (the time between exposure and the infectious period) and, consequently, more rapid deterioration of the host. Lower doses seem to lengthen the incubation time and possibly increase chances of an abortive infection, or an infection in which the virus enters the host but cannot replicate sufficiently to invade the CNS. Of note, the inoculation titers are likely to be lower in bats than in larger animals51,52,56.
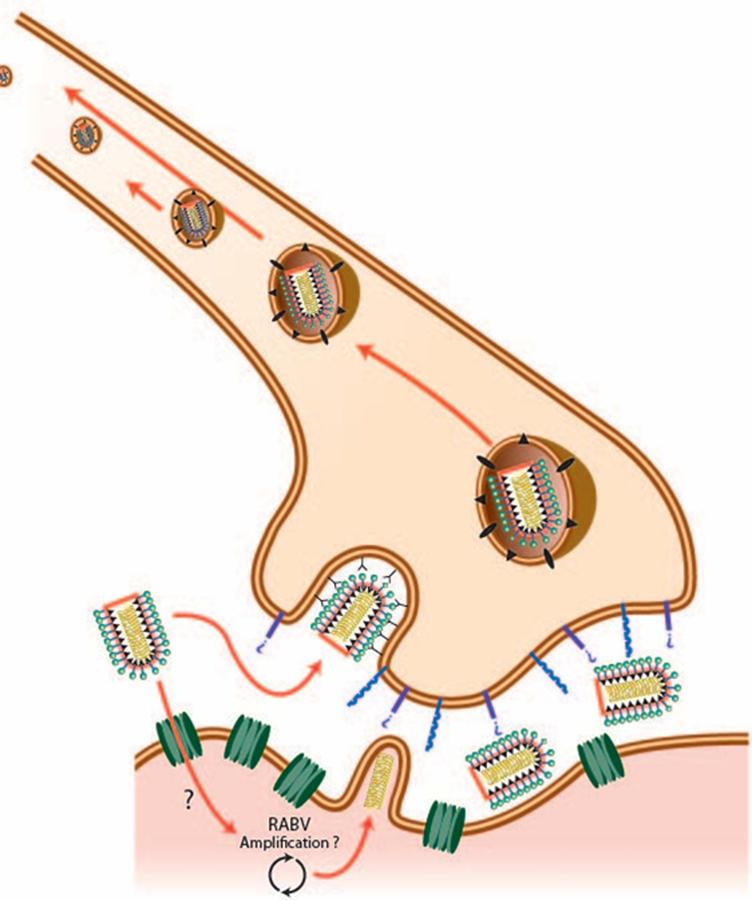
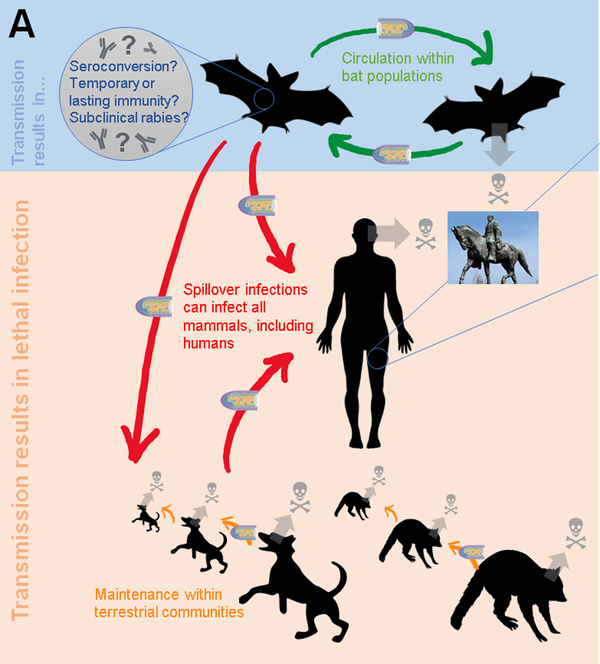
Figure 2: Lyssavirus transmission dynamics in bats and terrestrial animals.
Lyssaviruses seem to circulate more successfully in bats than in terrestrial mammals. A variety of factors contribute to maintenance, such as general and reservoir-specific viral factors, habitat factors and levels of human interaction. Host-specific factors, especially immune status in bats, are less understood. Although bats die upon clinical manifestation of disease, high rates of seroprevalence seen in healthy bats suggests a high frequency of abortive infection, which occurs through a combination of low exposure dosages, functional innate immune, and presence or development of neutralizing antibodies. Experimental infection studies have shown that bats can develop sub-detectable immunological memory (protection in the absence of neutralizing antibodies). However, there has never been evidence to suggest that a healthy but virus-secreting “carrier” state contributes to maintenance within bat populations. Seroprevalence in non-bats arising from natural exposure (not vaccination) are lower by comparison. Maintenance of RABV in wild and domestic carnivore reservoirs of RABV depends more heavily on variation in life history traits, population density, habitat use and degree of associations with humans. Spillover infections (in humans, for example) almost exclusively result in death before transmission to another host. The biological factors underpinning whether hosts survive or succumb to rabies, if naturally acquired VNAs are protective, and what role this has in the long-term perpetuation of RABV remain unclear.
Immune responses to RABV and immune evasion.
The skin is the first defense barrier against RABV. Except for relatively rare instances of intranasal inoculation57, a breach in the skin is essential for RABV to penetrate the host. After penetration, RABV infections elicit inadequate immune responses until late stages of the disease. Indeed, a major reason for the lack of symptoms during the incubation period is the absent immune response58. RABV adeptly evades innate immunity both actively at the cellular level59,60, and via its tropism to the immunologically-privileged nervous system.
Investigating direct and indirect immune evasion mechanisms of RABV has been a particularly active area of research in recent years (recently reviewed in REF.61). Each of the five proteins encoded in the RABV genome has been implicated in immune suppression either directly or indirectly, although phosphoprotein has a key role and can differ in its activity between strains62. Immune dysfunctions linked to RABV include inhibition of interferon (IFN) signaling, systemic immunosuppression, altered nitric oxide production and mitochondrial dysfunction61,63. RABV has also been shown to induce apoptosis, the benefit or detriment of which to the virus is currently debated61. As a consequence of the innate immune evasion mechanisms, the host does not mount an adaptive immune response against the virus until late stages of the disease, when the viral load is intractably high35. The lack of adaptive immunity until it this late stage of infection is particularly unfortunate as RABV is highly immunogenic when administered in a vaccine format and, furthermore, protective immunity is relatively straightforward.
Upon vaccination, T cell-dependent humoral immunity generates virus-neutralizing antibodies (VNAs) that are the critical correlate of protection, as determined by extensive experimental infection studies and clinical observations58,63. Although RABV can induce cytotoxic T cells, these cells do not to have a substantial role in protection from rabies disease58. Antibodies can be found against multiple RABV proteins, but only VNAs against glycoprotein are relevant for protection. VNA-mediated clearance is believed to function by coating the virion and blocking receptor binding, however cell-mediated antibody functions have never been definitely ruled out64. Understanding of RABV neutralization is complicated by the fact that infection occurs primarily in the nervous system, and uncertainty persists surrounding viral clearance from the CNS65. Those mechanisms will need elucidation before a therapeutic can be developed that works after the onset of symptoms (reviewed in REFS.58,63). Notably, similar to the study of lyssavirus strain pathogenicity, our understanding of lyssavirus-induced immunity mostly comes from mouse studies, which do not necessarily recapitulate natural infection. Nevertheless, well-established methods of assaying for VNAs66 informed the highly successful post-exposure prophylaxis (PEP) that has been widely used for decades.
There is a tendency to regard RABV infection in a binary fashion: virus neutralization by antibodies if they are present, and lethal infection if they are not. Infection dynamics are likely more nuanced, as a combination of low exposure dosages, functional innate immunity, and neutralizing antibodies can result in abortive infection. A high frequency of abortive infection is clearly seen in the presence of antibody in healthy bats67–69, spanning many species and geographic areas52. VNAs in non-bats are less well-established, but have been detected at varying levels in diverse reservoir and non-reservoir species, including human, cow, and mongoose45,70–72. These findings highlight major unanswered questions: what are the biological factors underpinning whether hosts survive or succumb to rabies? and if naturally acquired VNAs are protective, what role do they have in the long-term perpetuation of RABV? It remains unclear why lethality, which seems unlikely to benefit the virus, is highly permissible in its transmission dynamics.
Transmission, maintenance and spread
RABV transmission.
Transmission of RABV, and indeed all lyssaviruses, occurs through contact between infectious saliva and broken skin or mucous membranes, typically via bites, but also through scratches or licks. Transmission through consumption of carcasses or infected animals may also occur, but neutralization of RABV in the gastro-intestinal tract means that abrasions in the oral cavity are likely to be required to give the virus passage into innervated muscle or neuronal tissue73,74. Experimental infection directly into the intestine resulted in neither clinical rabies disease nor development of VNAs75. Examples of aerosol transmission have been limited to extraordinary situations involving high concentrations of virus, such as in the largest aggregations of free-tailed bats (numbering in the millions) or in laboratory settings57,76,77, which suggests this route is unlikely to be important for natural virus circulation. In regions where RABV infection in human is rare, there have been instances of misdiagnosis and subsequent RABV transmission via organ transplantation upon death of the patient78,79.
The host immune status and the nature of the exposure (for example, dose, location, and depth of inoculation) can influence whether an exposure results in a lethal or abortive infection. Strain-level differences among RABVs that influence the outcome of exposures are increasingly evident, particularly in comparisons between bat and terrestrial carnivore-associated variants51. For example, silver-haired bat rabies virus (SHBRV), but not dog-derived RABV isolates, are capable of hematogenous spread in mice after intravenous inoculations, which suggests that viremia could be an alternate route to the CNS in some strains80. SHBRV also replicates better at lower temperatures in epithelial cells than carnivore RABVs, which may indicate the adaptation to the relatively shallow bites of small insectivorous bats81. In mice, bat-derived RABVs generally seem to be less neurotropic and less uniformly lethal than carnivore RABVs, which may explain why the rare instances of human survival of clinical rabies mostly involved bat variants82. Mechanistic explanations for differences in pathogenesis and virulence at the cellular and molecular level remain largely elusive, limiting our ability to understand the risks posed by newly discovered or emergent strains. Combining new genomics technologies with classic phenotypic studies may enable researchers to identify how viral genomic backgrounds interact with host transcriptomic responses to infection, ultimately leading to the identification of factors that influence the outcomes of rabies infections.
Enzootic maintenance of RABV.
RABV is an obligately lethal pathogen that infects relatively long-lived, slow-reproducing mammalian hosts, has an infectious period spanning less than 1 week (and typically only 2–4 days), and relies on transmission among members of the same specifics to be maintained at the population level. In theory, this combination of characteristics would be expected to rapidly deplete susceptible individuals and cause host and/or virus extinction83. Indeed, estimates of the basic reproductive number (R0, the number of secondary infections generated from a single infection in an entirely susceptible population) of RABV are near or below the theoretical limit precluding epidemic spread (R0 = 1) in domestic dogs, wild carnivores and bats, suggesting that RABV should be prone to stochastic extinctions and sensitive to control measures7,84,85. Explaining how RABV is perpetuated over long time periods has therefore been a major conundrum that directly affects policies for rabies control through vaccination and culling of reservoir hosts.
Fortunately, the remarkable volume and quality of data collected on RABV through public health and veterinary surveillance systems has made the virus a model system for understanding the epidemiological dynamics of zoonoses within their animal reservoirs (Box 3). On the basis of multi-annual epidemic cycles, early studies suggested that the maintenance of RABV was driven by an interaction between density-dependent transmission and rabies-induced mortality, whereby reduction of host populations owing to lethal infection dampened transmission and enabled the recovery of susceptible hosts86–88. However, the consistent failure of population reduction (that is, culling) to control RABV transmission and weak or absent empirical relationships between population density and measures of RABV transmission84,89,90 raised doubts that a simple relationship between density and transmission exists. Moreover, a recent synthesis highlighted alternative mechanisms, including demographic structure and spatial structure, that could generate observed epidemic cycles in the absence of density dependence91. Individual-level variation in host dispersal or propensity to bite during infection is poorly understood but could also have a crucial role in the maintenance of RABV by creating ‘super-spreaders’ of infection84,92.
Box 3: Rabies virus as a model system for epidemiology and evolution.
Mathematical models are invaluable tools to understand the mechanisms underlying contemporary and historical patterns of infectious disease transmission and to quantify the potential effectiveness of interventions for prevention and control83. The distinctive symptoms of rabies virus (RABV) and its global importance for human and animal health contributed to the early development of surveillance systems that recorded dates and geographic locations of incidence or exposure, information about the host and results from laboratory diagnostics. This unusual wealth of data for a non-human disease, often spanning decades and thousands of observations, has made rabies an exceptional system for modeling zoonotic infectious disease dynamics that has delivered applied and theoretical advances169. Foundational epidemiological models of rabies used a deterministic ‘SEI’ model, in which individuals were classified as susceptible (S), infected and incubating RABV (‘exposed’ (E)) or infected and infectious (I) with transmission governed by host density86,170. This simple model explained the observed epidemiological cycles for RABV infections in foxes and guided eventual strategies for elimination from Western Europe171. Since then, increasingly sophisticated models have captured diverse epidemiological features of RABV in domestic and wild reservoirs, including seasonality118, individual heterogeneity in infectiousness84, spatial dynamics111, and the role of naturally acquired immunity among many others172. Similar modeling frameworks have been applied more recently to understand the dynamics of RABV infections in bats85,97. A critical application of models is in areas where rabies has not yet spread. For example, a recent model for the spread of canine rabies in Australia (currently RABV-free) highlighted geographic regions where research was needed to define parameters governing dog movements and behavior to prepare for the possible introduction of canine RABV173,174. Similar models of the spread of RABV in raccoons in Ohio, USA, provided rapid, high resolution recommendations for localities requiring vaccine delivery and enhanced surveillance efforts following a breach in a vaccine barrier175.
The increasing availability of sequence data from RABV isolates is now driving the development of models that combine epidemiological and evolutionary data to better understand RABV transmission. RABVs are a reliable system for these models due to a combination of factors: its small single-stranded, non-segmented genome and its evolution on epidemiological timescales by point mutation (that is, without recombination or strong antigenic selection) enable for relatively simple evolutionary models; and its transmission dynamics (direct transmission, single species reservoirs, lack of arthropod vectors) remove much of the complexity typical to animal diseases. Consequently, RABV has been at the forefront of the development of statistical models in spatial phylogeography176–178 and molecular inference of cross-species transmission116,179. Second generation sequencing is now expanding the depth and size of RABV molecular datasets. These data are providing insights into rabies transmission and evolution at unprecedented spatial and temporal scales180. The ability to characterize sub-consensus viral populations has enabled researchers to understand how genetic diversity in local reservoirs contributes to host shifts to novel species132. Mechanistic models that link phylogenomic or sub-consensus distributions of sequence variants are now needed to fully exploit this new generation of data.
It is now evident that RABV has evolved both general and reservoir host-specific maintenance mechanisms to avoid extinction. Across RABV reservoirs, transmission is aided by the aggressive behavior of rabid animals. Disease-induced aggression may facilitate transmission at low host population densities and for reservoirs that have infrequent natural contacts with conspecifics (for example, solitary bat species) or territorial carnivores that live in small groups (for example, arctic foxes). Variable incubation periods are another general feature that may help RABV avoid extinction. Although incubation periods are typically 1–3 months, deaths in wild-caught, captive bats show longer delays (>200 days) are likely to occur in nature52,93,94, which might promote viral dispersal to new host populations or the recovery of susceptible hosts through births or immigration93,95. Finally, across many reservoirs, transmission dynamics and prospects for control of host populations can be profoundly influenced by the spatial structure, such as induced by rivers, mountains and other landscape barriers, vaccination campaigns or reliance on human-provided resources96.
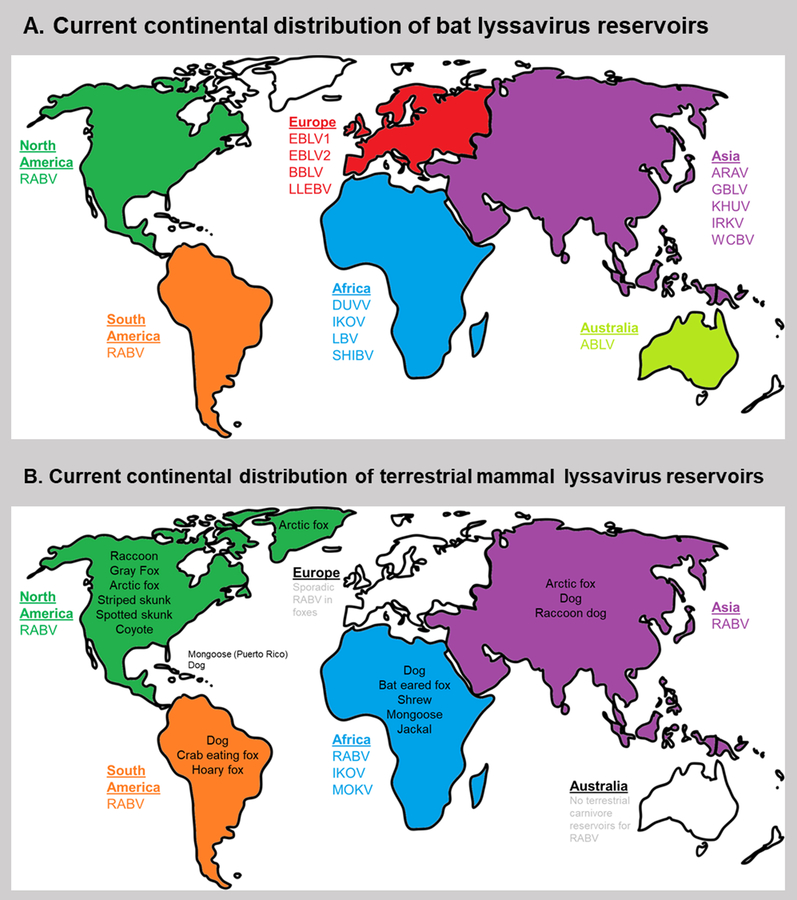
Given the diverse ecologies of its bat and carnivore reservoirs, it is not surprising that RABV has evolved distinctive strategies for enzootic maintenance in different reservoirs (Fig. 3, Fig. 4). For example, in temperate, hibernating bats, RABV overwinters by slowing replication, thereby prolonging the incubation until spring birth pulses replenish susceptible individuals to the population97–99. By contrast, for tropical bats that are transmitted throughout the year, spatial processes such as metapopulation dynamics seem to prevent host or virus extinction85. Maintenance mechanisms for bat colonies comprising hundreds of thousands to millions of individuals remain unclear. These colonies sustain high seroprevalence [G], suggesting optimal conditions for spread, yet no die-offs from RABV have been observed69,100. Studies on European bat lyssavirus (EBLV) suggested extended infectious periods or carrier states might explain persistence in large colonies without overt mortality101; however, experimental models in both EBLV and RABV have not generated infections that produce long-term shedding without death52,102,103, raising doubts on the existence or epidemiological relevance of a healthy carrier state. Among the wild and domestic carnivore reservoirs of RABV, variation in life history traits, population density, habitat use and degree of associations with humans also exert pressures that are important for maintaining viral transmission through extinction-recolonization dynamics or age-structured transmission91,104. The ability of RABV to maintain independent transmission cycles in such a diverse set of hosts is a remarkable testament to its epidemiological plasticity. Important questions for understanding the changing ecological niche of RABV include how this plasticity alters viral molecular evolution and whether strategies in some reservoirs predispose establishment in novel host species or landscapes.
Figure 3A: Current continental distribution of bat lyssaviruses.
Rabies disease-causing lyssaviruses circulate on all continents except Antarctica. In the Americas, all variants to date are strains of RABV. By contrast, RABV is largely absent from bats in the rest of the world, but 14 other lyssaviruses have been found in bats, including in Australia and Europe which are otherwise considered RABV-free.
3B: Current continental distribution of terrestrial mammal lyssavirus reservoirs. Most terrestrial lyssavirus reservoirs circulate strains of RABV, except in Africa, where IKOV and MOKV have been found. Europe is considered free of terrestrial RABV on account of vaccination efforts. Rabies in terrestrial mammals has never been reported in Australia. Common reservoirs are indicated.
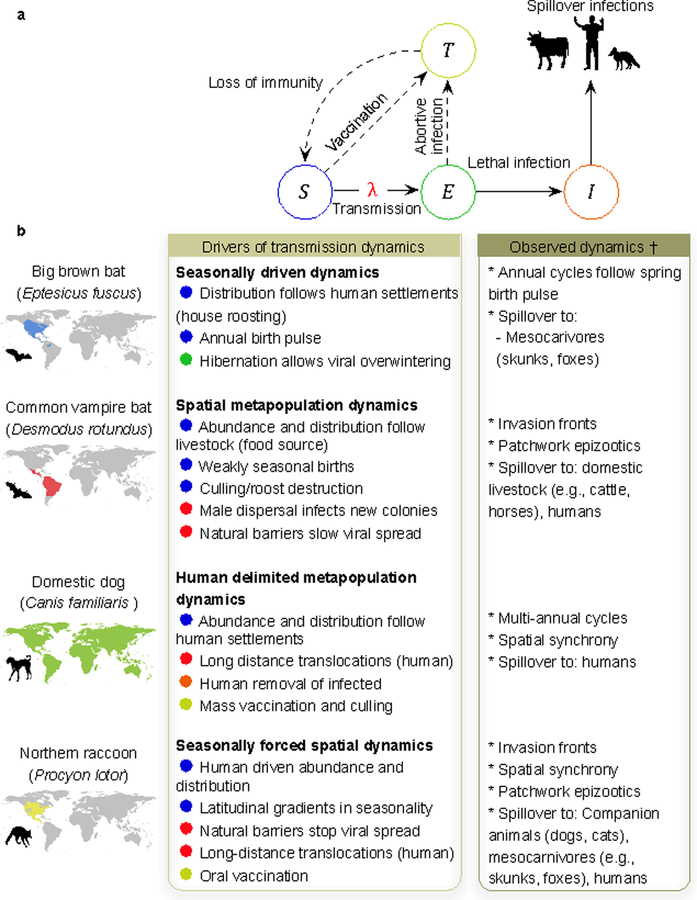
Figure 4: The influence of reservoir host ecology on the epidemiology of rabies.
a| The ‘SEI’ model for rabies epidemiology represents transitions of hosts between individuals that are classified as susceptible (S), infected and incubating RABV (‘exposed’ (E), infected and infectious (I) and temporarily immune (T). Both intraspecific transmission and spillover infections to non-reservoir hosts arise from infectious reservoirs in the I class. The force of infection (λ) depends on the frequency of susceptible and infected and infectious individuals in the population, total population size and transmission rate. Solid arrows indicate portions of the transmission cycle that are common to all RABV reservoirs. Dashed arrows may only occur for some reservoir hosts, depending on pathbiological relationships with rabies (see Fig. 2) or human interventions such as the presence of vaccination campaigns. b| Variation in reservoir host ecology influences different phases of the transmission cycle, causing reservoir host-specific transmission dynamics and maintenance mechanisms. Maps show the geographic range of four of the best-studied RABV reservoir hosts, although RABV may be absent from some parts of each species’ range, for example because of changing viral distributions or local eradication efforts. The drivers of transmission dynamics are mapped for each reservoir host to the compartmental model in panel a, to illustrate how ecology affects transmission dynamics. The epidemiological dynamics observed in each reservoir are summarized.
Of note, spillover infections to a broad range of species occur from each reservoir; shown are the principle spillover hosts infected by each reservoir.
Epizootic spread of rabies.
Despite the challenges of enzootic persistence, RABV has repeatedly demonstrated sudden opportunist epizootic spread when introduced to naive host populations. Although such spread occasionally follows cross-species transmission105 (see below), the best-studied examples of landscape-level viral invasions from point source introductions (that is, ‘travelling or epizootic waves’) involve translocations of the virus into new populations of existing reservoirs by human movement of incubating animals or natural host dispersal87. Wavefront velocities have been quantified in foxes86, skunks8, raccoons7 and vampire bats10,106 and generally advance between 10 km and 40 km per year. Mathematical models and phylogeographic analyses of these invasions have revealed key facets of the transmission dynamics of RABV. For example, the spread of RABV among raccoons in eastern North America was partly contained by mountain ranges and rivers, enabling these natural landscape barriers to complement oral vaccination campaigns and limit western spread107. Invasions in other reservoirs, such as skunks and bats, have proceeded at more regular velocities along routes defined by host population structure8,108. In principle, predictable wavefronts enable forecasting of risk and vaccination of reservoirs, humans and domestic animals prior to viral invasion, but strategic planning in unaffected areas from model forecasts remains relatively uncommon. Moreover, intentional or unintentional translocation of synanthropic species (for example, dogs and raccoons) reduces predictability and can compromise natural or vaccine-generated barriers109–112. Fully understanding viral spread at the landscape level will require answers to fundamental questions: what ecological, climatic or anthropogenic factors trigger viral invasions to new areas? What explains different spread velocities within the same reservoir hosts in different geographic locations or time points in the invasion process7,8,10? Will RABV persist indefinitely or fade out from newly invaded areas? New technologies for studying animal movement, such as GPS tagging and nano-scale radio-transmitters, together with the comprehensive epidemiological and genomic datasets collected through surveillance systems provide exciting opportunities to resolve these questions and enlighten programs for rabies prevention and control.
Evolution and host shift
In rare instances, spillover infections [G] of RABV are maintained over long time scales in new host species. These events are important for public health because they create new reservoirs for human exposures113,114 and can affect wildlife conservation when new transmission cycles occur in threatened or endangered species115 or increase spillover to those species. Most novel transmission cycles have been established in previously known hosts of RABV, such as bats, skunks and foxes105,116. However, evidence of sustained transmission in non-traditional hosts has reinforced the need to understand how RABV overcomes evolutionary barriers to establish novel reservoirs. These non-traditional hosts include marmosets12 and kinkajous (primates)117, greater kudu antelope (artiodactyl)118, and coatis119, mongooses120,121 and ferret badgers122 (carnivores).
The need for host adaptation in RABV.
Despite the apparent capacity of rabies to infect any mammal, numerous lines of evidence imply that RABV must adapt to establish in new host species123. From an epidemiological perspective, RABVs that use multiple host species for long-term maintenance are conspicuously absent. In vivo and in vitro studies suggest this absence may reflect genetic fine tuning of RABV to specific hosts. Phenotypic differences among genetic variants of RABV are commonly observed81, and infections in heterologous hosts show altered patterns of infectivity and pathogenesis that would be expected to limit onward transmission. For example, raccoons inoculated with homologous RABV manifest acute clinical rabies after a long incubation period, but show subtle clinical signs such as lethargy followed by death or abortive infection when inoculated with dog or skunk-origin viruses124,125. Phylogenetic comparative studies provide another line of evidence that host barriers exist and must be overcome by viral evolution. In bats, both cross-species transmission and historical host shifts occurred more often between closely related species than between species with extensive geographic range or ecological overlap116. This suggests that although ecological opportunity is a prerequisite for emergence, physiological or immunological barriers that correlate with host relatedness influence the likelihood of successful host adaptation. Non-random clustering of RABV reservoirs on the carnivore phylogeny could reflect a similar predominance of host shifts among related hosts or variation in susceptibility among clades of carnivores126,127.
Molecular evolutionary dynamics of rabies host shifts.
Given that RABV must evolve to efficiently infect and establish transmission in new host species, it is surprising that classic molecular evolutionary signatures of positive selection (dn/ds ratios >1) have been only rarely described in RABV. The overwhelming force on the RABV genome is purifying selection, and until recently positive selection was only detected in a small number of amino acid positions in the ectodomain of the glycoprotein17,128. Selection on the RABV genome may be difficult to detect, given that available sequences are typically limited to the genes encoding the nucleoprotein and glycoprotein and span only a small fraction of viral evolutionary history129. Moreover, potential host shifts may be driven to extinction by control efforts, such as vaccination, before adaptation occurs105. Another possible explanation is that most studies have used computational methods that assumed pervasive selection across all branches of viral phylogenies, an assumption that is unlikely to hold for a virus experiencing a sudden change in environment following long periods of relative evolutionary stasis. Indeed, more recent studies have shown pulsed episodes of positive selection on diverse sites in the nucleoprotein, glycoprotein and polymerase130,131. Repeated host shifts between the same donor and recipient species have shown that the adaptive evolution of RABV can even be repeatable. Independent host shifts from domestic dogs into ferret-badgers in Asia resulted in parallel substitutions in the genes encoding nucleoprotein and polymerase130. In the southwestern USA, three independent outbreaks of bat-associated RABV in skunks were associated with six parallel changes across the viral genome, but did not overlap with those observed in ferret-badgers105. Similarly, among 30 host shifts between American bats that represented different combinations of donor and recipient species, combinations of positively selected changes were largely unique to each host shift131. It therefore seems likely that the adaptive changes necessary for each host shift are driven by the interaction between the genetic background of the infecting virus and the identity of the host species involved.
The importance of viral genetic background implies that the degree of viral preadaptation to a particular host can make some host shifts more likely to occur than others. For example, bat viruses with threonine in position 242 of the glycoprotein have caused more outbreaks in carnivores than those of other genetic backgrounds105. Deep sequencing has revealed sub-consensus viral populations as another source of genomic diversity that can be selected during host shifts. For example, changes that became fixed following a host shift from skunks to foxes in California were present as low frequency variants for years before outbreaks in foxes began132. As a potentially important consequence of the increasing diversity of reservoirs, the virus may be exposed to previously unexplored areas of host genomic space, increasing the likelihood of rare, preadapted variants that facilitate further host range expansions, perhaps even to reservoirs outside of bats and carnivores. This ‘snowball effect’ hypothesis predicts an increasing frequency of future host shifts123.
The unsolved mystery of rabies origins.
Phylogenetic studies have shown that the evolutionary history of RABV is dominated by host shifts, predominately within bats and within carnivores, but more rarely between these mammalian orders17,130. As the vast majority of lyssavirus diversity occurs in Old World bats (Figure 3A), RABV was commonly assumed to have evolved in Old World bats, shifted to carnivores and subsequently spread globally133. However, unexplained observations have plagued the bat-to-dog hypothesis and complicate our understanding of the evolutionary history of RABV. Most notably, Old World bats carry diverse RABV-related lyssaviruses but not RABV, whereas New World bats exclusively carry RABV (Figure 3A). By contrast, carnivores maintain RABV in both the New and Old Worlds (Figure 3B). The absence of RABV from its putative origin (Old World bats) raises the important question of how carnivores in the Old World acquired RABV. Conceivably, RABV evolved around the time of the origin of bats (~62 mya134) and moved with bats as they colonized the Americas from Africa or North Asia. However, this would require a RABV host shift from bats into ancestral or modern carnivores, followed by RABV extinction from Old World bats amid conditions that favored the persistence of RABV in New World bats. A more controversial alternative is that RABV evolved in carnivores following a host shift of a non-RABV lyssavirus from Old World bats, spread to the New World RABV infected dogs during European colonization, and more recently jumped from carnivores to bats in the New World. Although cross-species RABV transmission from carnivores to bats is unlikely, given that rabid carnivore bites would likely kill comparatively smaller bats before they contract rabies, it is worth noting that all bat RABV variants are monophyletic130, so such an event would only need to occur once. Moreover, the recent discovery of a carnivore-related RABV in a bat in Sri Lanka may represent the first evidence of a carnivore-to-bat exposure that resulted in successful RABV infection, setting a precedent that a similar transmission event might have occurred in the New World135. Less speculative evidence for a more recent origin of RABV in the Americas comes from studies suggesting that RABV is not at equilibrium within American bat communities, as might be expected for an ancient virus. This evidence includes the fact that American bat RABVs are still diversifying their host range136, geographically isolated populations of established reservoirs are rabies-free (suggesting arrival of rabies after host vicariance)108, and ongoing invasion fronts into historically rabies-free areas resemble those observed for recent introductions10. This evidence suggests a more recent introduction to New World bats, but it is biased by the enhanced detection abilities of modern surveillance programs and by the changing environmental conditions that could alter the abundance and distribution of RABV reservoirs137.
Historical records and phylogenetic studies provide little resolution of these evolutionary uncertainties. Ancient records in the Old World make reference only to rabid dogs, not bats4,138. In the New World, there is no clear evidence of indigenous bat or dog rabies139,140, and the first confirmed reports of bat rabies appeared around the start of the sixteenth century as colonization began1. Rabies was not reported in North American bats until the 1950s141. However, the bias of record availability is worth noting; the Mayans were the only pre-Columbian Old World civilization to develop sophisticated writing, and most of their records were destroyed upon Spanish settlement139. Phylogenetic studies have clarified some aspects of the biogeography and evolution of lyssaviruses, but leave much uncertain for RABV in particular. At the genus level, a recent phylogeographic study rejected the expected African origin of lyssaviruses in favor of a Palearctic origin with multiple radiations creating the different phylogroups [G]142. For RABV, most studies put the most recent common ancestor of bat RABV within the timescale of European colonization (~500y, consistent with a carnivore-to-bat host shift); however, molecular clock methods based on contemporary sequences are unlikely to be able to estimate the true timing of ancient host shifts because of strong purifying selection and the lack of sequences from extinct lineages130,143. It has been suggested that paleovirological studies of endogenous viral elements (EVEs) in host genomes might clarify the time scale of RABV origins129. Although rhabdoviral or rhabdovirus-like EVEs exist in insect and plant genomes144, the absence of lyssavirus-related EVEs despite extensive screening of mammalian genomes, casts doubt on this approach to resolve RABV origins145. New virus discoveries and/or analytical methods may eventually solve the riddle of rabies origins.
Surveillance, Diagnostics, and Vaccines
As discussed above, traits unique to RABV have long spurred far-reaching surveillance efforts yielding large, comprehensive data sets. These datasets have, in turn, enabled advances in disease modeling which may eventually enable accurate predictions about the movements of RABV in host populations. However, the current situation requires even more than just monitoring the dozens of known RABV strains. In the past decade, numerous novel RABVs were discovered in Latin America that form species-associated genetic clusters in unusual host species, including non-human primates12,117 and coati119. In Taiwan, outbreaks of RABV in ferret-badgers have raised major public health concerns as a wildlife reservoir would compromise the long-term sustainability of dog vaccination for RABV elimination113. Whether these discoveries reflect spillovers from unknown reservoirs or emergent host shifts is unknown, as is the relative virulence of these viruses in humans or domestic animals.
Another frontier for surveillance lies in non-RABV lyssaviruses. At present, the discovery of RABV-related viruses [G] is usually attributed to either unusual exposures or fastidious surveillance efforts that endeavor to distinguish between strains (Box 1). The recent discovery of lyssaviruses in Spain18 and Sri Lanka19 highlights a potentially vast lyssavirus diversity that will continue to be discovered as surveillance systems and diagnostics become more accessible. Statistical approaches, such as machine learning, have been useful to identify unknown sources of disease in other systems146,147 and could accelerate the search for novel lyssaviruses by predicting potential reservoirs from the traits of known reservoirs.
Apart from detection, the threat to animal and human health posed by non-RABV lyssaviruses remains unsettled. Lyssaviruses cause the same zoonotic disease but are incompletely protected by rabies vaccines or biologics, which were designed to target only RABV14,22,25. All current human and animal vaccines have been developed against RABV; there is limited, incidental cross-reactivity among viruses of phylogroup I and no cross-reactivity between phylogroups26,27,148. Rabies is responsible for an estimated 59,000 global human deaths annually15, and an estimated 15 million people receive PEP annually for exposures149. However, the true disease burden of non-RABV lyssaviruses is unknown because clinical signs are indistinguishable from RABV infections and discriminatory diagnostics are rarely available for either human cases or animal surveillance22. Thus, although only 12 human deaths have been confirmed as being caused by six non-RABV lyssaviruses22, this number is likely to be a large underestimation. A study in Ethiopia showed that 1% of animals diagnosed with rabiesdisease were actually infected with Mokola virus (MOKV)23.
Investment in RABV vaccines has been touted as one of the lowest cost but highest impact tradeoffs among vaccine-preventable infectious diseases150. Yet, canine RABV still causes tens of thousands of human fatalities on multiple continents because mass vaccination of dogs is not sufficiently adopted and post-exposure prophylaxis of humans is either unavailable or inaccessible15. Looking forward, host shifts to new reservoirs bring new challenges. Lyssaviruses circulate in bats in Europe, Africa, Asia and Australia and have infected terrestrial mammals numerous times, raising the risk of novel non-RABV lyssaviruses in carnivores or other terrestrial mammals. Indeed, the absence of MOVK and IKOV from bats but presence in other species may indicate that such host shifts have already occurred21,151. Such shifts could have devastating effects given the absence of pre- or post-exposure vaccines that protect against these lyssaviruses, which are phylogenetically and antigenically divergent from RABV. Investment in studying lyssaviruses and developing a pan-lyssavirus vaccine is currently lacking, leaving the world unprepared in the event of an outbreak.
Given their prominence as reservoirs, bat populations are perhaps an attractive target for lyssavirus control. As noted, culling efforts in Latin America have failed to change RABV seroprevalence levels within the population and may even be counterproductive90. Mass bat vaccination has never been implemented, as it has been for terrestrial wildlife, but experimental vaccinations have been performed in captive bats, testing inactivated RAVB in Brazilian free-tailed bats54, vaccinia-vectored live vaccines in vampire bats152–154, and raccoonpox-vectored live vaccines in big brown bats155 and Brazilian free-tailed bats156. These and other studies of bat responses to RABV52,53 repeatedly find low or undetectable long-term antibody titers, as measured using conventional virus neutralization assay protection cutoffs defined for humans. Nevertheless, vaccines administered to bats through various routes, including topical, oral and intramuscular, protect against RABV challenge. Combined with our limited knowledge of bat immunity to rabies55, these findings highlight the need for defined bat-specific correlates of protection before investing in mass bat vaccination. The feasibility of scalable and effective mass vaccination of wild bats must also be resolved. For social and gregarious bat species, vaccines could be applied topically and spread through social interactions (that is, allo-grooming) to maximize coverage, akin to strategies currently used to poison common vampire bats157,158. However, field studies and epidemiological models are needed to determine what vaccination coverage may be expected with this dissemination vehicle and what proportion of colonies would need to be treated to meaningfully reduce rabies circulation in bat populations.
The changing epidemiological face of rabies creates new challenges for using molecular data and models to inform decisions for prevention and control. Where domestic dog rabies is approaching elimination, rapid sequencing will be paramount to determine whether resurgent outbreaks represent chains of previously undetected local transmission or re-introductions from still enzootic areas. New technologies mean that rapid diagnostics and genome sequencing (that is, MinION portable, real-time DNA and RNA sequencer) can be carried out in the field in affected countries159. Appropriate investments to strengthen local analytical and laboratory capacity are therefore paramount for elimination.
Conclusions
Despite its long history, rabies remains an important but neglected infectious disease. Much of the molecular virology of RABV has been well-characterized, and we are now gaining appreciation of how nuanced infection dynamics and immune status relates to transmission. Enzootic maintenance of rabies within a population depends on transmission within precariously narrow windows, and it is now clear that the virus avoids extinction by both general and reservoir host-specific mechanisms with remarkable epidemiological plasticity. At the landscape level, mathematical models and phylogeographic analyses provide a sketch of epizootic rabies spread, but questions surrounding ecological, climatic, and anthropogenic factors remain. At an evolutionary level, there is evidence that strong barriers prevent RABV from establishing in new host species, and both ecological opportunities and viral adaptation are needed to overcome these barriers. Nevertheless, host shifts occur, and the study of molecular evolutionary dynamics has revealed the role of purifying selection and the importance of viral and host genetic backgrounds in such shifts. Further study of contemporary host shifts will likely shed light on rabies’ unknown origin.
Examination of modern rabies has revealed subtleties in our understanding of how the virus moves within and among its animal reservoirs. The convergence of insights gained from field research with molecular virology studies will be key to fully elucidating rabies. Building upon the carnivore vaccination programs of the twentieth century, the next steps will be to devise strategies and technologies to similarly manage rabies within bat reservoirs; further integrate diagnostics that can rapidly differentiate strains into surveillance efforts; hone our predictive power to detect outbreaks; and coordinate local resources to halt the spread of this lethal zoonosis.
Online only:
With much of the molecular virology characterized, we are now gaining appreciation of how nuanced rabies virus infection dynamics are and how immune status relates to transmission.
The growing number of recognized rabies-virus related lyssaviruses highlights shortcomings in our discriminatory diagnostics and raises questions about their impact on human health. The lack of therapeutics for some of these lyssaviruses is a major concern.
Enzootic maintenance of rabies virus within a population depends on transmission within narrow windows. The virus avoids extinction by both general and reservoir host-specific mechanisms with remarkable epidemiological plasticity.
Features of rabies biology, ecology and evolution have made rabies a model pathogen for disease ecology and evolution. Recent work using mathematical models and phylodynamic analyses have allowd reconstruction and forecasting of epizootic rabies spread at the landscape level.
At an evolutionary level, there is evidence that strong barriers prevent RABV from establishing in new host species, and both ecological opportunities and viral adaptation are needed to overcome these barriers. Studies of rabies virus molecular evolutionary dynamics have revealed the role of purifying selection and the importance of viral and host genetic backgrounds in host shifts. Further study of contemporary host shifts will likely shed light on rabies’ unknown origin.
We suggest that efforts be put into developing strategies and technologies to manage rabies viruses within bat reservoirs as has been previously done with carnivores, integrate diagnostics that can rapidly differentiate strains into surveillance efforts, hone our predictive power to detect outbreaks, and coordinate local resources to halt the spread of this lethal zoonosis.
Acknowledgements:
The authors thank Jennifer Wilson (Thomas Jefferson University, Philadelphia, PA, USA) for her critical reading and editing of the manuscript. M.J.S is supported in part by NIH grant 1R01AI127823, 1R21AI128175 and 5P40OD010996-12 (Peter Strick, University of Pittsburgh, subcontract M.J.S.) and the Jefferson Vaccine Center. D.S. was supported by a Sir Henry Dale Fellowship, jointly funded by the Wellcome Trust and Royal Society (102507/Z/13/Z).
Glossary:
- Host
An individual or animal infected with a virus, such as a lyssavirus
- Strain
A viral population maintained within a particular reservoir, often in a geographically defined area that can be genetically distinguished from other sympatric viral populations
- Reservoirs
Animal pools that perpetuates the long-term transmission of a rabies virus strain. Sometimes called a reservoir host or maintenance host
- Variants
Viral strains with small genetic differences that may or may not be detectable by antigenic characterization
- Virions
Infectious particles, complete with the viral genome and viral proteins, capable of transmission to a new cell or host
- Isolates
Viral samples that have been obtained from an infected individual or animal host
- Seroprevalence
proportion of animals or individuals presenting virus-specific antibodies in their serum, indicative of exposure to either the virus or vaccine
- Spillover infections
Transmission events in which a lyssavirus strain successfully infects an animal of a non-reservoir species
- Phylogroups
Subgeneric classification of lyssavirus species grouped by genetic and immunologic characteristics
- Rabies virus-related lyssaviruses
Virus of the lyssavirus genus of RNA viruses other than the prototypical member, rabies virus.
Footnotes
There is NO Competing Interest.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nature Reviews Microbiology thanks Monique Lafon, and the other anonymous reviewer(s), for their contribution to the peer review of this work.
References
- 1.Baer GM The natural history of rabies. (CRC press, 1991). [Google Scholar]
- 2.Yuhong W Rabies and rabid dogs in Sumerian and Akkadian literature. Journal of the American Oriental Society, 32–43 (2001). [Google Scholar]
- 3.Tarantola A Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure. Tropical Medicine and Infectious Disease 2, 5(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baer GM in Rabies (ed Wunner William H Jackson Alan C) Ch. 1, 1–22 (2007). [Google Scholar]
- 5.Belotto A, Leanes L, Schneider M, Tamayo H & Correa E Overview of rabies in the Americas. Virus research 111, 5–12 (2005). [DOI] [PubMed] [Google Scholar]
- 6.Ribadeau-Dumas F et al. Travel-Associated Rabies in Pets and Residual Rabies Risk, Western Europe. Emerging Infectious Diseases 22, 1268–1271, doi: 10.3201/eid2207.151733 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biek R, Henderson JC, Waller LA, Rupprecht CE & Real LA A high-resolution genetic signature of demographic and spatial expansion in epizootic rabies virus. Proceedings of the National Academy of Sciences of the United States of America 104, 7993–7998 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study established rabies as a model for viral phylodynamics, demonstrating that the dynamics of viral invasions can be estimated to high resolution from spatially and temporally annotated viral sequences.
- 8.Kuzmina NA et al. The phylogeography and spatiotemporal spread of south-central skunk rabies virus. PloS one 8, e82348(2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez-Burnes J et al. An outbreak of vampire bat-transmitted rabies in cattle in northeastern Mexico. The Canadian Veterinary Journal 38, 175(1997). [PMC free article] [PubMed] [Google Scholar]
- 10.Benavides JA, Valderrama W & Streicker DG Spatial expansions and travelling waves of rabies in vampire bats. Proceedings of the Royal Society B: Biological Sciences 283, doi: 10.1098/rspb.2016.0328 (2016). [DOI] [Google Scholar]
- 11.Birhane MG et al. Rabies surveillance in the United States during 2015. Journal of the American Veterinary Medical Association 250, 1117–1130 (2017). [DOI] [PubMed] [Google Scholar]
- 12.Favoretto SR, de Mattos CC, Morais NB, Araujo FAA & de Mattos CA Rabies in marmosets (Callithrix jacchus), Ceara, Brazil. Emerging Infectious Diseases 7, 1062–1065 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castillo-Neyra R et al. Barriers to dog rabies vaccination during an urban rabies outbreak: Qualitative findings from Arequipa, Peru. PLoS neglected tropical diseases 11, e0005460(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banyard AC, Evans JS, Luo TR & Fooks AR Lyssaviruses and bats: emergence and zoonotic threat. Viruses 6, 2974–2990, doi: 10.3390/v6082974 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]; This review reports on the detection, transmission, and maintenance of rabies-related lyssaviruses in bats.
- 15.Human rabies: 2016 updates and call for data. Releve epidemiologique hebdomadaire 92, 77–86 (2017). [PubMed] [Google Scholar]
- 16.Hampson K et al. Estimating the global burden of endemic canine rabies. PLoS neglected tropical diseases 9, e0003709(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badrane H, Bahloul C, Perrin P & Tordo N Evidence of two Lyssavirus phylogroups with distinct pathogenicity and immunogenicity. J Virol 75, 3268–3276, doi: 10.1128/JVI.75.7.3268-3276.2001 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ceballos NA et al. Novel lyssavirus in bat, Spain. Emerging infectious diseases 19, 793(2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gunawardena PS et al. Lyssavirus in Indian Flying Foxes, Sri Lanka. Emerging infectious diseases 22, 1456(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coertse J et al. New isolations of the rabies-related Mokola virus from South Africa. BMC veterinary research 13, 37, doi: 10.1186/s12917-017-0948-0 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marston DA et al. Ikoma lyssavirus, highly divergent novel lyssavirus in an African civet. Emerg Infect Dis 18, 664–667 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evans JS, Horton DL, Easton AJ, Fooks AR & Banyard AC Rabies virus vaccines: is there a need for a pan-lyssavirus vaccine? Vaccine 30, 7447–7454, doi: 10.1016/j.vaccine.2012.10.015 (2012). [DOI] [PubMed] [Google Scholar]
- 23.Mebatsion T, Cox JH & Frost JW Isolation and characterization of 115 street rabies virus isolates from Ethiopia by using monoclonal antibodies: identification of 2 isolates as Mokola and Lagos bat viruses. Journal of Infectious Diseases 166, 972–977 (1992). [DOI] [PubMed] [Google Scholar]; This study focused on prevalence of phylogroup II lyssaviruses in terrestrial mammals.
- 24.Mallewa M et al. Rabies encephalitis in malaria-endemic area, Malawi, Africa. Emerging infectious diseases 13, 136(2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanlon CA et al. Efficacy of rabies biologics against new lyssaviruses from Eurasia. Virus Research 111, 44–54 (2005). [DOI] [PubMed] [Google Scholar]
- 26.Liu Y et al. Evaluation of rabies biologics against Irkut virus isolated in China. J Clin Microbiol 51, 3499–3504, doi: 10.1128/JCM.01565-13 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Benedictis P et al. Development of broad‐spectrum human monoclonal antibodies for rabies post‐exposure prophylaxis. EMBO molecular medicine 8, 407–421 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Conzelmann KK, Cox JH, Schneider LG & Thiel HJ Molecular cloning and complete nucleotide sequence of the attenuated rabies virus SAD B19. Virology 175, 485–499 (1990). [DOI] [PubMed] [Google Scholar]
- 29.Tordo N, Poch O, Ermine A, Keith G & Rougeon F Walking along the rabies genome: is the large G-L intergenic region a remnant gene? Proc Natl Acad Sci U S A 83, 3914–3918 (1986). [DOI] [PMC free article] [PubMed] [Google Scholar]; This was the first study to report a complete rabies virus genome sequence.
- 30.Ge P et al. Cryo-EM model of the bullet-shaped vesicular stomatitis virus. Science 327, 689–693 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cureton DK, Massol RH, Saffarian S, Kirchhausen TL & Whelan SP Vesicular stomatitis virus enters cells through vesicles incompletely coated with clathrin that depend upon actin for internalization. PLoS pathogens 5, e1000394(2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson AC in Rabies (eds Jackson Alan C & Wunner William H) Ch. 8, 341–372 (Academic Press, 2007). [Google Scholar]
- 33.Rossiter JP & Jackson AC in Rabies (eds Jackson Alan C & Wunner William H) Ch. 9, 383–403 (Academic Press, 2007). [Google Scholar]
- 34.Schnell MJ, McGettigan JP, Wirblich C & Papaneri A The cell biology of rabies virus: using stealth to reach the brain. Nature reviews. Microbiology 8, 51–61, doi: 10.1038/nrmicro2260 (2010). [DOI] [PubMed] [Google Scholar]
- 35.Dietzschold B, Li J, Faber M & Schnell M Concepts in the pathogenesis of rabies. (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]; This work provides an overview of viral factors which affect the pathogenicity of rabies virus.
- 36.Lafon M Rabies virus receptors. Journal of neurovirology 11, 82–87 (2005). [DOI] [PubMed] [Google Scholar]
- 37.Piccinotti S & Whelan SP Rabies Internalizes into Primary Peripheral Neurons via Clathrin Coated Pits and Requires Fusion at the Cell Body. PLoS pathogens 12, e1005753(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu H et al. Real-time imaging of rabies virus entry into living vero cells. Scientific reports 5, 11753(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis BD, Rall GF & Schnell MJ in Annual Review of Virology Vol. 2 (ed DiMaio Dermody Enquist) 51–71 (Annual Reviews, 2015). [Google Scholar]; This work is a comprehensive review of rabies virus and rabies virus infection.
- 40.Yamaoka S et al. Involvement of the rabies virus phosphoprotein gene in neuroinvasiveness. Journal of virology 87, 12327–12338 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Velandia-Romero ML, Castellanos JE & Martínez-Gutiérrez M In vivo differential susceptibility of sensory neurons to rabies virus infection. Journal of neurovirology 19, 367–375 (2013). [DOI] [PubMed] [Google Scholar]
- 42.Jackson AC et al. Extraneural organ involvement in human rabies. Laboratory investigation; a journal of technical methods and pathology 79, 945–951 (1999). [PubMed] [Google Scholar]
- 43.de Souza A & Madhusudana SN Survival from rabies encephalitis. Journal of the neurological sciences 339, 8–14 (2014). [DOI] [PubMed] [Google Scholar]
- 44.Wunner WH & Jackson AC Rabies: scientific basis of the disease and its management. (Academic Press, 2010). [Google Scholar]
- 45.Hanlon CA, Niezgoda M & Rupprecht CE Rabies in terrestrial animals. Jackson AC, Wunner WH. Rabies 2, 201–258 (2013). [Google Scholar]
- 46.Hemachudha T et al. Immunologic study of human encephalitic and paralytic rabies: preliminary report of 16 patients. The American journal of medicine 84, 673–677 (1988). [DOI] [PubMed] [Google Scholar]
- 47.Shuangshoti S et al. Intracellular Spread of Rabies Virus Is Reduced in the Paralytic Form of Canine Rabies Compared to the Furious Form. PLoS neglected tropical diseases 10, e0004748(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hemachudha T et al. Human rabies: neuropathogenesis, diagnosis, and management. The Lancet Neurology 12, 498–513 (2013). [DOI] [PubMed] [Google Scholar]
- 49.Katz ISS et al. Delayed progression of rabies transmitted by a vampire bat. Archives of virology 161, 2561–2566 (2016). [DOI] [PubMed] [Google Scholar]
- 50.Mesquita LP et al. A rabies virus vampire bat variant shows increased neuroinvasiveness in mice when compared to a carnivore variant. Archives of Virology, 1–9 (2017). [DOI] [PubMed] [Google Scholar]
- 51.Begeman L et al. Comparative pathogenesis of rabies in bats and carnivores, and implications for spillover to humans. The Lancet Infectious Diseases (2017). [DOI] [PubMed] [Google Scholar]
- 52.Jackson FR et al. Experimental rabies virus infection of big brown bats (Eptesicus fuscus). Journal of Wildlife Diseases 44, 612–621 (2008). [DOI] [PubMed] [Google Scholar]
- 53.Obregón-Morales C et al. Experimental infection of Artibeus intermedius with a vampire bat rabies virus. Comparative Immunology, Microbiology and Infectious Diseases (2017). [DOI] [PubMed] [Google Scholar]
- 54.Turmelle AS et al. Response to vaccination with a commercial inactivated rabies vaccine in a captive colony of Brazilian free-tailed bats (Tadarida brasiliensis). Journal of Zoo and Wildlife Medicine 41, 140–143 (2010). [DOI] [PubMed] [Google Scholar]
- 55.Baker M, Schountz T & Wang LF Antiviral immune responses of bats: a review. Zoonoses and public health 60, 104–116 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Messenger SL, Smith JS, Orciari LA, Yager PA & Rupprecht CE Emerging pattern of rabies deaths and increased viral infectivity. Emerging infectious diseases 9, 151(2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Constantine DG, Emmons RW & Woodie JD Rabies Virus in Nasal Mucosa of Naturally Infected Bats. Science 175, 1255 LP–1256 (1972). [DOI] [PubMed] [Google Scholar]
- 58.Lafon M in Rabies (ed Wunner William H Jackson Alan C) Ch. 12, 489–504 (2007). [Google Scholar]
- 59.Brzózka K, Finke S & Conzelmann K-K Identification of the rabies virus alpha/beta interferon antagonist: phosphoprotein P interferes with phosphorylation of interferon regulatory factor 3. Journal of virology 79, 7673–7681 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yang J, Koprowski H, Dietzschold B & Fu ZF Phosphorylation of rabies virus nucleoprotein regulates viral RNA transcription and replication by modulating leader RNA encapsidation. Journal of virology 73, 1661–1664 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Scott TP & Nel LH Subversion of the Immune Response by Rabies Virus. Viruses 8, 231(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rieder M & Conzelmann K-K Interferon in rabies virus infection. Advances in virus research 79, 91(2011). [DOI] [PubMed] [Google Scholar]; This review covers the interplay between the innate immune response and rabies virus’s strategies to antagonize it.
- 63.Johnson N, Cunningham AF & Fooks AR The immune response to rabies virus infection and vaccination. Vaccine 28, 3896–3901 (2010). [DOI] [PubMed] [Google Scholar]
- 64.Moore SM & Hanlon CA Rabies-specific antibodies: measuring surrogates of protection against a fatal disease. PLoS neglected tropical diseases 4, e595(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hooper DC, Phares TW, Fabis MJ & Roy A The production of antibody by invading B cells is required for the clearance of rabies virus from the central nervous system. PLoS neglected tropical diseases 3, e535(2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith J, Yager P & Baer G in Laboratory Techniques in Rabies (eds Meslin FX, Kaplan MM, & Koprowski H) 181–192 (World Health Organization, 1996). [Google Scholar]
- 67.De Thoisy B et al. Bioecological drivers of rabies virus circulation in a Neotropical bat community. PLoS neglected tropical diseases 10, e0004378(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Streicker DG, Franka R, Jackson FR & Rupprecht CE Anthropogenic roost switching and rabies virus dynamics in house-roosting big brown bats. Vector-Borne and Zoonotic Diseases 13, 498–504 (2013). [DOI] [PubMed] [Google Scholar]
- 69.Turmelle AS et al. Ecology of rabies virus exposure in colonies of Brazilian free-tailed Bats (Tadarida brasiliensis) at natural and man-made roosts in Texas. Vector-Borne and Zoonotic Diseases 10, 165–175, doi: 10.1089/vbz.2008.0163 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Everard C & Everard J Mongoose rabies in the Caribbean. Annals of the New York Academy of Sciences 653, 356–366 (1992). [DOI] [PubMed] [Google Scholar]
- 71.Gilbert A et al. Antibody response of cattle to vaccination with commercial modified live rabies vaccines in Guatemala. Preventive veterinary medicine 118, 36–44 (2015). [DOI] [PubMed] [Google Scholar]
- 72.Gilbert AT et al. Evidence of rabies virus exposure among humans in the Peruvian Amazon. The American journal of tropical medicine and hygiene 87, 206–215 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ramsden RO & Johnston DH Studies on the oral infectivity of rabies virus in carnivora. Journal of wildlife diseases 11, 318–324 (1975). [DOI] [PubMed] [Google Scholar]
- 74.Bell JF & Moore GJ Susceptibility of carnivora to rabies virus administered orally. American journal of epidemiology 93, 176–182 (1971). [DOI] [PubMed] [Google Scholar]
- 75.Charlton K & Casey G Experimental rabies in skunks: oral, nasal, tracheal and intestinal exposure. Canadian Journal of Comparative Medicine 43, 168(1979). [PMC free article] [PubMed] [Google Scholar]
- 76.Winkler WG, Fashinell TR, Leffingwell L, Howard P & Conomy JP Airborne rabies transmission in a laboratory worker. Jama 226, 1219–1221 (1973). [PubMed] [Google Scholar]
- 77.Gibbons RV Cryptogenic rabies, bats, and the question of aerosol transmission. Annals of Emergency Medicine 39, 528–536, doi: 10.1067/mem.2002.121521 (2002). [DOI] [PubMed] [Google Scholar]
- 78.Srinivasan A et al. Transmission of rabies virus from an organ donor to four transplant recipients. New England Journal of Medicine 352, 1103–1111 (2005). [DOI] [PubMed] [Google Scholar]
- 79.Hellenbrand W, Meyer C, Rasch G, Steffens I & Ammon A Cases of rabies in Germany following organ transplantation. Euro surveillance: bulletin Europeen sur les maladies transmissibles= European communicable disease bulletin 10, E050224–050226 (2004). [DOI] [PubMed] [Google Scholar]
- 80.Preuss MA et al. Intravenous inoculation of a bat-associated rabies virus causes lethal encephalopathy in mice through invasion of the brain via neurosecretory hypothalamic fibers. PLoS pathogens 5, e1000485(2009). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides evidence that bat-derived rabies virus spreads differently than classical rabies virus.
- 81.Morimoto K et al. Characterization of a unique variant of bat rabies virus responsible for newly emerging human cases in North America. Proceedings of the National Academy of Sciences of the United States of America 93, 5653–5658 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jackson AC Current and future approaches to the therapy of human rabies. Antiviral research 99, 61–67 (2013). [DOI] [PubMed] [Google Scholar]
- 83.Keeling MJ & Rohani P Modeling infectious diseases in humans and animals. 366 (2008). [Google Scholar]
- 84.Hampson K et al. Transmission dynamics and prospects for the elimination of canine rabies. PLoS biology 7, e1000053(2009). [DOI] [PMC free article] [PubMed] [Google Scholar]; By estimating the first field-derived estimates of the basic reproductive number of dog rabies from contact tracing and mathematical models, this study showed that rabies might be eliminated through sustained dog vaccination programs.
- 85.Blackwood JC, Streicker DG, Altizer S & Rohani P Resolving the roles of immunity, pathogenesis, and immigration for rabies persistence in vampire bats. Proceedings of the National Academy of Sciences of the United States of America 110, 20837–20842, doi: 10.1073/pnas.1308817110 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study combined longitudinal field studies with mathematical models to show that the long term maintenance of rabies in vampire bats relies on spatial dynamics and immunizing abortive infections.
- 86.Anderson RM, Jackson HC, May RM & Smith AM Population dynamics of fox rabies in Europe. Nature 289, 765–771 (1981). [DOI] [PubMed] [Google Scholar]
- 87.Childs JE et al. Predicting the local dynamics of epizootic rabies among raccoons in the United States. Proceedings of the National Academy of Sciences of the United States of America 97, 13666–13671, doi: 10.1073/pnas.240326697 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Courtin F, Carpenter TE, Paskin RD & Chomel BB Temporal patterns of domestic and wildlife rabies in central Namibia stock-ranching area, 1986–1996. Preventive Veterinary Medicine 43, 13–28 (2000). [DOI] [PubMed] [Google Scholar]
- 89.Coleman PG & Dye C Immunization coverage required to prevent outbreaks of dog rabies. Vaccine 14, 185–186, doi: 10.1016/0264-410X(95)00197-9 (1996). [DOI] [PubMed] [Google Scholar]
- 90.Streicker DG et al. Ecological and anthropogenic drivers of rabies exposure in vampire bats: implications for transmission and control. Proceedings of the Royal Society B: Biological Sciences 279, 3384–3392, doi: 10.1098/rspb.2012.0538 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provided the first evidence that culling vampire bats may be ineffective for rabies elimination.
- 91.Morters MK et al. Evidence-based control of canine rabies: a critical review of population density reduction. Journal of Animal Ecology 82, 6–14, doi: 10.1111/j.1365-2656.2012.02033.x (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]; This review assesses the evidence for various mechanism through which animal culls are hypothesized to be effective strategy for rabies control and concludes that vaccination should be the preferred strategy.
- 92.Lloyd-Smith JO, Schreiber SJ, Kopp PE & Getz WM Superspreading and the effect of individual variation on disease emergence. Nature 438, 355–359 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Davis AD, Dupuis M & Rudd RJ Extended incubation period of rabies virus in a captive big brown bat (Eptesicus fuscus). Journal of wildlife diseases 48, 508–511, doi: 10.7589/0090-3558-48.2.508 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides evidence for long incubation times when bat-derived rabies virus infects its natural host (bats).
- 94.Moore GJ & Raymond GH Prolonged incubation period of rabies in a naturally infected insectivorous bat, Eptesicus foscus (beauvois). Journal of wildlife diseases 6, 167–168 (1970). [DOI] [PubMed] [Google Scholar]
- 95.Smith JS, Fishbein DB, Rupprecht CE & Clark K Unexplained Rabies in Three Immigrants in the United States a Virologic Investigation. New England journal of medicine 324, 205–211 (1991). [DOI] [PubMed] [Google Scholar]
- 96.Beyer HL et al. Metapopulation dynamics of rabies and the efficacy of vaccination. Proceedings of the Royal Society B: Biological Sciences 278, 2182–2190, doi: 10.1098/rspb.2010.2312 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.George DB et al. Host and viral ecology determine bat rabies seasonality and maintenance. Proceedings of the National Academy of Sciences of the United States of America 108, 10208(2011). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used mathematical models and field studies to show that the observed seasonal dynamics of rabies in temperate bats may be achieved through long incubation periods during hibernation and birth pulses.
- 98.Davis AD et al. Overwintering of Rabies Virus in Silver Haired Bats (Lasionycteris noctivagans). Plos One 11, e0155542, doi: 10.1371/journal.pone.0155542 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Streicker DG, Lemey P, Velasco-Villa A & Rupprecht CE Rates of viral evolution are linked to host geography in bat rabies. PLoS Pathogens 8, e1002720(2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Steece RR & Altenbach JSJS Prevalence of rabies specific antibodies in the Mexican free-tailed bat (Tadarida brasiliensis mexicana) at Lava Cave, New Mexico. Journal of Wildlife Diseases 25, 490–496, doi: 10.7589/0090-3558-25.4.490 (1989). [DOI] [PubMed] [Google Scholar]
- 101.Amengual B, Bourhy H, López-Roíg M & Serra-Cobo J Temporal dynamics of European bat lyssavirus type 1 and survival of Myotis myotis bats in natural colonies. PLoS ONE 2, doi: 10.1371/journal.pone.0000566 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fooks AR, Brookes SM, Johnson N, McElhinney LM & Hutson AM European bat lyssaviruses: an emerging zoonosis. Epidemiology and Infection 131, 1029–1039, doi: 10.1017/S0950268803001481 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Franka R et al. Susceptibility of North American big brown bats (Eptesicus fuscus) to infection with European bat lyssavirus type 1. Journal of General Virology 89, 1998–2010, doi: 10.1099/vir.0.83688-0 (2008). [DOI] [PubMed] [Google Scholar]
- 104.Carey AB & McLean RG The ecology of rabies: evidence of co-adaptation. Journal of Applied Ecology, 777–800 (1983). [Google Scholar]
- 105.Kuzmin IV et al. Molecular inferences suggest multiple host shifts of rabies viruses from bats to mesocarnivores in Arizona during 2001–2009. PLoS Pathogens 8, e1002786, doi: 10.1371/journal.ppat.1002786 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed that rabies outbreaks in terrestrial carnivores arose from recurrent re-introductions from bats, but found little evidence of adaptive evolution within carnivores.
- 106.Lord RD et al. Observations on the epizootiology of vampire bat rabies. Bulletin of the Pan American Health Organization 9, 189–195 (1975). [PubMed] [Google Scholar]
- 107.Slate D et al. Oral rabies vaccination in North America: Opportunities, complexities, and challenges. PLoS Neglected Tropical Diseases 3, e549, doi: 10.1371/journal.pntd.0000549 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Streicker DG et al. Host–pathogen evolutionary signatures reveal dynamics and future invasions of vampire bat rabies. Proceedings of the National Academy of Sciences, 201606587(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Talbi C et al. Phylodynamics and human-mediated dispersal of a zoonotic virus. PLoS pathogens 6, e1001166(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nettles VF, Shaddock JH, Keith Sikes R & Reyes CR Rabies in translocated raccoons. American Journal of Public Health 69, 601–602, doi: 10.2105/AJPH.69.6.601 (1979). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Smith DL, Lucey B, Waller LA, Childs JE & Real LA Predicting the spatial dynamics of rabies epidemics on heterogeneous landscapes. Proceedings of the National Academy of Sciences of the United States of America 99, 3668–3672, doi: 10.1073/pnas.042400799 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Horton DL et al. Complex epidemiology of a zoonotic disease in a culturally diverse region: phylogeography of rabies virus in the Middle East. PLoS neglected tropical diseases 9, e0003569(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang S et al. Rabies in ferret badgers, Southeastern China. Emerging Infectious Diseases 15, 946–949, doi: 10.3201/eid1506.081485 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Leslie MJ et al. Bat-associated rabies virus in skunks. Emerging infectious diseases 12, 1274(2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Randall DA et al. Rabies in endangered Ethiopian wolves. Emerging infectious diseases 10, 2214(2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Streicker DG et al. Host phylogeny constrains cross-species emergence and establishment of rabies virus in bats. Science (New York, N.Y.) 329, 676–679, doi: 10.1126/science.1188836 (2010). [DOI] [PubMed] [Google Scholar]
- 117.Condori-Condori RE, Streicker DG, Cabezas-Sanchez C & Velasco-Villa A Enzootic and epizootic rabies associated with vampire bats, Peru. Emerging Infectious Diseases 19, 1463–1469, doi: 10.3201/eid1909.130083 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Duke-sylvester SM et al. Strong seasonality produces spatial asynchrony in the outbreak of infectious diseases. Journal of the Royal Society, Interface / the Royal Society 8, 817–825, doi: 10.1098/rsif.2010.0475 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Arechiga-Ceballos N et al. New rabies virus variant found during an epizootic in white-nosed coatis from the Yucatan Peninsula. Epidemiology and Infection 138, 1586–1589 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nadin-Davis S et al. A molecular epidemiological study of rabies in Cuba. Epidemiology & Infection 134, 1313–1324 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nel L et al. Mongoose rabies in southern Africa: a re-evaluation based on molecular epidemiology. Virus research 109, 165–173 (2005). [DOI] [PubMed] [Google Scholar]
- 122.Chiou H-Y et al. Molecular characterization of cryptically circulating rabies virus from ferret badgers, Taiwan. Emerging infectious diseases 20, 790(2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mollentze N, Biek R & Streicker DG The role of viral evolution in rabies host shifts and emergence. Current opinion in virology 8, 68–72 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hamir AN, Moser G & Rupprecht CE Clinicopathologic variation in raccoons infected with different street rabies virus isolates. Journal of Veterinary Diagnostic Investigation 8, 31–37 (1996). [DOI] [PubMed] [Google Scholar]
- 125.Sikes RK Pathogenesis of rabies in wildlife. I. Comparative effect of varying doses of rabies virus inoculated into foxes and skunks. American Journal of Veterinary Research 23, 1041–1047 (1962). [PubMed] [Google Scholar]
- 126.Huang S, Bininda‐Emonds OR, Stephens PR, Gittleman JL & Altizer S Phylogenetically related and ecologically similar carnivores harbour similar parasite assemblages. Journal of Animal Ecology 83, 671–680 (2014). [DOI] [PubMed] [Google Scholar]
- 127.Longdon B, Brockhurst MA, Russell CA, Welch JJ & Jiggins FM The evolution and genetics of virus host shifts. PLoS pathogens 10, e1004395(2014). [DOI] [PMC free article] [PubMed] [Google Scholar]; This comprehensive review discusses barriers to viral host shifts between species.
- 128.Holmes EC, Woelk CH, Kassis R & Bourhy H Genetic constraints and the adaptive evolution of rabies virus in nature. Virology 292, 247–257 (2002). [DOI] [PubMed] [Google Scholar]
- 129.Rupprecht C, Kuzmin I & Meslin F Lyssaviruses and rabies: current conundrums, concerns, contradictions and controversies. F1000Research 6 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Troupin C et al. Large-scale phylogenomic analysis reveals the complex evolutionary history of rabies virus in multiple carnivore hosts. PLoS pathogens 12, e1006041(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Streicker DG, Altizer SM, Velasco-Villa A & Rupprecht CE Variable evolutionary routes to host establishment across repeated rabies virus host shifts among bats. Proceedings of the National Academy of Sciences 109, 19715–19720 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Borucki MK et al. Ultra-Deep Sequencing of Intra-host Rabies Virus Populations during Cross-species Transmission. PLoS Neglected Tropical Diseases 7, e2555, doi: 10.1371/journal.pntd.0002555 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nel L & Rupprecht C in Wildlife and Emerging Zoonotic Diseases: The Biology, Circumstances and Consequences of Cross-Species Transmission 161–193 (Springer, 2007). [Google Scholar]
- 134.Eick GN, Jacobs DS & Matthee CA A nuclear DNA phylogenetic perspective on the evolution of echolocation and historical biogeography of extant bats (Chiroptera). Molecular Biology and Evolution 22, 1869–1886 (2005). [DOI] [PubMed] [Google Scholar]
- 135.Matsumoto T et al. Terrestrial animal-derived rabies virus in a juvenile Indian flying fox in Sri Lanka. Japanese Journal of Infectious Diseases, JJID. 20172249(2017). [DOI] [PubMed] [Google Scholar]
- 136.SHOJI Y et al. Genetic characterization of rabies viruses isolated from frugivorous bat (Artibeus spp.) in Brazil. Journal of veterinary medical science 66, 1271–1273 (2004). [DOI] [PubMed] [Google Scholar]
- 137.Lee DN, Papeş M & Van Den Bussche RA Present and potential future distribution of common vampire bats in the Americas and the associated risk to cattle. PLoS One 7, e42466(2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yuhong W Rabies and Rabid Dogs in Sumerian and Akkadian Literature. Journal of the American Oriental Society 121, 32–43, doi: 10.2307/606727 (2001). [DOI] [Google Scholar]
- 139.Vos A et al. The occurrence of rabies in pre-Columbian Central America: an historical search. Epidemiology & Infection 139, 1445–1452 (2011). [DOI] [PubMed] [Google Scholar]
- 140.Velasco-Villa A et al. The history of rabies in the Western Hemisphere. Antiviral research (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]; This review compiles historical information on rabies in the new world, with a focus on the importance of expanding dog populations following European colonization.
- 141.Scatterday JE Bat rabies in Florida. Journal of the American Veterinary Medical Association 124, 125(1954). [PubMed] [Google Scholar]
- 142.Hayman DT, Fooks AR, Marston DA & Garcia-R JC The global phylogeography of lyssaviruses-challenging the’out of Africa’hypothesis. PLoS neglected tropical diseases 10, e0005266(2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hughes GJ, Orciari LA & Rupprecht CE Evolutionary timescale of rabies virus adaptation to North American bats inferred from the substitution rate of the nucleoprotein gene. Journal of General Virology 86, 1467–1474 (2005). [DOI] [PubMed] [Google Scholar]
- 144.Chiba S et al. Widespread endogenization of genome sequences of non-retroviral RNA viruses into plant genomes. PLoS pathogens 7, e1002146(2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Katzourakis A & Gifford RJ Endogenous viral elements in animal genomes. PLoS genetics 6, e1001191(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Evans MV, Dallas TA, Han BA, Murdock CC & Drake JM Data-driven identification of potential zika virus vectors. eLife 6, 1–38, doi: 10.7554/eLife.22053 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Han BA, Schmidt JP, Bowden SE & Drake JM Rodent reservoirs of future zoonotic diseases. Proceedings of the National Academy of Sciences 112, 201501598, doi: 10.1073/pnas.1501598112 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nel LH in Sixth SEARG Meeting 80–86 (2001).
- 149.WHO. Rabies Fact Sheet, <http://www.who.int/mediacentre/factsheets/fs099/en/> (2017).
- 150.Rabies Vaccine Investment Strategy. (GAVI Alliance, 2013).
- 151.Sabeta CT et al. Mokola virus in domestic mammals, South Africa. Emerging infectious diseases 13, 1371(2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Almeida MF, Martorelli LF, Aires CC, Sallum P & Massad E Indirect oral immunization of captive vampires, Desmodus rotundus. Virus research 111, 77–82 (2005). [DOI] [PubMed] [Google Scholar]
- 153.Aguilar-Setién A et al. Vaccination of vampire bats using recombinant vaccinia-rabies virus. Journal of wildlife diseases 38, 539–544 (2002). [DOI] [PubMed] [Google Scholar]
- 154.Aguilar-Sétien A et al. Experimental rabies infection and oral vaccination in vampire bats (Desmodus rotundus). Vaccine 16, 1122–1126 (1998). [DOI] [PubMed] [Google Scholar]; This study first demonstrated the use of recombinant oral rabies vaccines in captive bats.
- 155.Stading B et al. Protection of bats (Eptesicus fuscus) against rabies following topical or oronasal exposure to a recombinant raccoon poxvirus vaccine. PLoS Neglected Tropical Diseases 11, e0005958(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Stading BR et al. Infectivity of attenuated poxvirus vaccine vectors and immunogenicity of a raccoonpox vectored rabies vaccine in the Brazilian Free-tailed bat (Tadarida brasiliensis). Vaccine 34, 5352–5358 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gomes MN, Uieda W & Latorre M. d. R. D. d. Influence of sex differences in the same colony for chemical control of vampire Desmodus rotundus (Phyllostomidae) populations in the state of Sao Paulo, Brazil. Pesquisa Veterinária Brasileira 26, 38–43 (2006). [Google Scholar]
- 158.Johnson N, Aréchiga-Ceballos N & Aguilar-Setien A Vampire bat rabies: ecology, epidemiology and control. Viruses 6, 1911–1928 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dürr S et al. Rabies diagnosis for developing countries. PLoS Neglected Tropical Diseases 2, e206, doi: 10.1371/journal.pntd.0000206 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Boulger L & Porterfield J Isolation of a virus from Nigerian fruit bats. Transactions of the Royal Society of Tropical Medicine and Hygiene 52, 421–424 (1958). [DOI] [PubMed] [Google Scholar]
- 161.Meredith C, Rossouw A & VAN PRAAG K An unusual case of human rabies thought to be of chiropteran origin. South African Medical Journal 45, 767–769 (1971). [PubMed] [Google Scholar]
- 162.Le Gonidec G, Rickenbach A, Robin Y & Heme G in Annales de microbiologie. 245–249. [PubMed] [Google Scholar]
- 163.Familusi J, Osunkoya B, Moore D, Kemp G & Fabiyi A A fatal human infection with Mokola virus. The American journal of tropical medicine and hygiene 21, 959–963 (1972). [DOI] [PubMed] [Google Scholar]
- 164.Lembo T et al. Exploring reservoir dynamics: a case study of rabies in the Serengeti ecosystem. Journal of Applied Ecology 45, 1246–1257 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Gomme EA, Wanjalla CN, Wirblich C & Schnell MJ Rabies virus as a research tool and viral vaccine vector. Advances in virus research 79, 139–164, doi: 10.1016/B978-0-12-387040-7.00009-3 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Prehaud C et al. Attenuation of rabies virulence: takeover by the cytoplasmic domain of its envelope protein. Science signaling 3, ra5, doi: 10.1126/scisignal.2000510 (2010). [DOI] [PubMed] [Google Scholar]; Neuronal survival after infection with rabies virus was linked to the interaction between a PDZ domain in the carboxy terminal tail of the rabies virus glycoprotein and cellular threonine kinases.
- 167.Gaudin Y, Tuffereau C, Segretain D, Knossow M & Flamand A Reversible conformational changes and fusion activity of rabies virus glycoprotein. J Virol 65, 4853–4859 (1991). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kim IS et al. Mechanism of membrane fusion induced by vesicular stomatitis virus G protein. Proc Natl Acad Sci U S A 114, E28–36, doi: 10.1073/pnas.1618883114 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lloyd-Smith JO et al. Epidemic dynamics at the human-animal interface. Science (New York, N.Y.) 326, 1362–1367, doi: 10.1126/science.1177345 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kermack WO & McKendrick AG Contributions to the mathematical theory of epidemics. I. Proc. R. Soc. Med 115A, 700–721 (1927). [DOI] [PubMed] [Google Scholar]
- 171.Freuling CM et al. The elimination of fox rabies from Europe: determinants of success and lessons for the future. Phil. Trans. R. Soc. B 368, 20120142(2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Panjeti VG & Real LA Mathematical models for rabies. Advances in Imaging and Electron Physics 79, 377–395 (2011). [DOI] [PubMed] [Google Scholar]
- 173.Dürr S & Ward MP Development of a novel rabies simulation model for application in a non-endemic environment. PLoS neglected tropical diseases 9, e0003876(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Johnstone-Robertson SP, Fleming PJ, Ward MP & Davis SA Predicted Spatial Spread of Canine Rabies in Australia. PLoS neglected tropical diseases 11, e0005312(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Russell CA, Smith DL, Childs JE & Real LA Predictive spatial dynamics and strategic planning for raccoon rabies emergence in Ohio. PLoS biology 3, e88(2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lemey P, Rambaut A, Drummond AJ & Suchard MA Bayesian phylogeography finds its roots. PLoS Computational Biology 5, e1000520, doi: 10.1371/journal.pcbi.1000520 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lemey P, Rambaut A, Welch JJ & Suchard MA Phylogeography takes a relaxed random walk in continuous space and time. Molecular Biology and Evolution 27, 1877–1885, doi: 10.1093/molbev/msq067 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Dellicour S, Rose R & Pybus OG Explaining the geographic spread of emerging viruses: a new framework for comparing viral genetic information and environmental landscape data. BMC Bioinformatics 17, 1–12, doi: 10.1186/s12859-016-0924-x (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Faria NR, Suchard MA, Rambaut A, Streicker DG & Lemey P Simultaneously reconstructing viral cross-species transmission history and identifying the underlying constraints. Philosophical transactions of the Royal Society of London. Series B, Biological sciences 368, 20120196, doi: 10.1098/rstb.2012.0196 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Brunker K et al. Elucidating the phylodynamics of endemic rabies virus in eastern Africa using whole-genome sequencing. Virus Evolution 1, 1–11, doi: 10.1093/ve/vev011 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]