Abstract
Background
Drug use is prevalent among electronic dance music (EDM) party attendees, but research is needed to determine the extent of adverse drug-related outcomes in this population in order to better inform prevention and harm reduction efforts.
Method
1,029 adults were surveyed entering EDM parties in New York City in 2018. Those reporting past-year use of a drug were asked if they experienced a harmful or very unpleasant effect after use in which they were concerned about their immediate safety. They were also asked about co-use of other drugs and whether they sought help.
Results
We estimate that a third (33.5%) of EDM attendees has experienced a drug-related adverse effect in the past year. Two-thirds (67.8%) of adverse effects involved use of alcohol. Relative to use, adverse effects most commonly resulted from use of opioids (e.g., prescription opioid misuse, 41.1%) or alcohol (33.9%). Concomitant use of other drugs was common, particularly among users of cocaine (55.7%), LSD (55.7%), ketamine (56.5%), LSD (41.2%), and ecstasy/MDMA/Molly (47.7%). Adverse effects resulting from synthetic cathinone (“bath salt”) use were most likely to result in a hospital visit (57.1%), followed by opioids (e.g., prescription opioids: 14.3%).
Conclusion
Adverse effects from drug use are common among those in the EDM scene and polydrug use appears to be a common risk factor. More research is needed, however, to determine the extent of event-specific adverse outcomes. Results can inform prevention and harm reduction efforts in this population.
Keywords: club drugs, new psychoactive substances, adulterants, dance music
Introduction
Electronic dance music (EDM) parties, commonly held at nightclubs and large festivals, have gained popularity in the United States (US) and globally over the past decade (Watson, 2018). Individuals who attend these parties, where use of party drugs such as ecstasy (MDMA) is particularly prevalent, are known to be at high risk for drug use (Hughes, Moxham-Hall, Ritter, Weatherburn, & MacCoun, 2017; Palamar, Acosta, Ompad, & Cleland, 2017; Palamar, Griffin-Tomas, & Ompad, 2015). However, while prevalence of drug use in this population is well-documented, research on the extent to which use is associated with acute adverse health effects is lacking.
It is particularly important to focus on drug-related adverse effects in the US as drug-related deaths are exponentially higher in the US than in other areas such as Europe (United Nations Office on Drugs and Crime [UNODC], 2018; European Monitoring Centre for Drugs and Drug Addiction, 2018). For example, in 2015, 300 per million individuals in the US died from a drug as the primary cause of death compared to 75 per million in the United Kingdom (UNODC, 2018). More specifically, in the US in 2016, there were 17,087 deaths (5.2 per 100,000) related to use of prescription opioids, 10,375 deaths (3.2 per 100,000) related to cocaine use, and 7,542 deaths (2.4 per 100,000) related to use of other psychostimulants (Seth, Scholl, Rudd, & Bacon, 2018). In 2016, alcohol was involved in over 50,000 drug-related poisonings in the US, though approximately 85% involved co-use of other drugs (Gummin et al., 2017). Over 16,000 poisonings in the US involved amphetamines, 8,100 involved oxycodone, 7,841 involved heroin, 7,384 involved marijuana, 5,374 involved cocaine, and 2,026 involved hallucinogenic amphetamines (Gummin et al., 2017). Given the high prevalence of drug use among EDM attendees, it seems warranted to investigate the prevalence of adverse outcomes associated with drug use among individuals in this scene as they may be at higher risk than the general population. At least 137 drug-related deaths at dance festivals have occurred (worldwide) since 1999 (Turris, Jones, & Lund, 2018; Turris & Lund, 2017) and only a few reports have examined poisonings and deaths at EDM parties in the US (Chhabra, Gimbar, Walla, & Thompson, 2018); thus, more research on adverse drug effects in this population is needed.
Although event-level prevalence of adverse effects experienced at such parties would be most ideal to inform prevention and harm reduction efforts, data on adverse drug-related outcomes among those who attend such parties can indeed help fill in this data gap. Such information can also likely improve preparation for and responses to adverse outcomes for party or festival staff, as well as emergency department (ED) providers. In this study, we queried drug use and adverse effects related to drug use via a survey of this at-risk population.
Methods
Procedure and Participants
Time-space sampling was utilzied to survey participants in this study (MacKellar et al., 2007). Each week, parties (primarily at nightclubs) were randomly selected to survey attendees. Specifically, each week, a list of upcoming EDM parties in NYC (located primarily in Brooklyn and Manhattan) was created. The list was based on EDM party ticket websites, party listings on social media, and recommendations from key informants. We considered parties from ticket websites eligible for random selection if at least 15 tickets were purchased for the party by mid-week. Parties were randomly selected using R software (R Development Core Team, 2013). Recruitment was typically limited to one to two nights per week on Thursday through Sunday. Time slots, however, were not randomly selected with recruitment for night parties typically conducted between 11:30pm and 2:30am because the majority of parties ended at 4am (with very few parties ending at 5am or 6am). While most participants were surveyed outside of nightclubs, participants were also surveyed outside of two large daytime festivals, which were not randomly selected.
Individuals were eligible if they were 1) 18–40 years old, and 2) about to enter the randomly-selected party. Recruiters approached passersby (who were alone or in groups), and if eligible, they were asked if they would be willing to take a drug survey. Surveys were self-administered on electronic tablets after informed consent was provided. The survey response rate was 73% with 1029 participants taking the survey. Participants were compensated $10 USD upon survey completion and recruitment was conducted from June through September of 2018. This study was approved by the New York University Langone Medical Center Institutional Review Board.
Measures
This epidemiological survey queried past-year use of a variety of drugs in separate sections. Specifically, after being asked about demographic characteristics, participants were then asked about use of 1) prescription opioids (e.g., Vicodin®, OxyContin® [nonmedical use]); followed by use of 2) other opioids (e.g., heroin, fentanyl and its analogs), 3) NBOMe (e.g., 25i-NBOMe), 4) alcohol and/or marijuana, 5) other common illegal drugs (e.g., LSD, GHB, PCP, ketamine, nonmedical amphetamine use), 6) synthetic cathinones (“bath salts”; e.g., methylone), 7) ecstasy/MDMA/Molly, 8) 2C series drugs (e.g., 2C-B), 9) new dissociatives (e.g., MXE), 10) tryptamines (e.g., 4-AcO-DMT), 11) benzodiazepines (e.g., Xanax® [nonmedical use]), 12) synthetic cannabinoids (e.g., “Spice”, “K2”), and 13) “unknown” powders (‘mystery’ powders used to get high). Nonmedical use of prescription drugs was defined for participants as using without a prescription or in a manner in which it was not prescribed—for example, to get high.
Those reporting past-year use of a drug were asked whether they had experienced a harmful or very unpleasant effect after using the drug in the past 12 months. The survey further explained that this referred to a drug effect in which the user was concerned about his or her immediate safety. Our definition of adverse effect was based on definitions in previous sources in which the drug effect was perceived to be harmful and/or unpleasant (Edwards & Aronson, 2000). Those answering affirmatively were asked follow-up questions. Specifically, they were asked: whether they asked someone for help after using the drug and not feeling well; if they felt they needed to go to the hospital or ED; and if they went to the hospital or ED. It was noted to participants that if more than one adverse effect from the drug occurred that they should answer questions regarding the most recent time this happened. To confirm recency of the event we asked how long ago it happened (e.g., within the past month, within the past six months). Those answering “over a year ago” were coded as not reporting an adverse effect in the past year; however, those answering ‘unsure’ were still coded as experiencing an adverse effect in the past year as they originally reported that the event occurred in the past 12 months. Those reporting an adverse effect were further asked if they used more than one drug (including alcohol) within a few hours of this happening. Those responding affirmatively were asked to type in the name of the other drug(s) used concomitantly. These type-in responses were later double-coded by two independent raters to ensure correct coding of drugs and this continued until 100% agreement was reached.
While we asked about adverse effects for each individual drug queried, we collapsed some specific drugs into categories. For example, we collapsed all prescription opioid-related adverse effect data into a prescription opioid category rather than presenting data for drugs such as oxycodone (e.g., OxyContin®) separately. Data were also cross-checked for multiple reporting of the same drugs that were used concomitantly. Only two cases contained the same pair of drugs co-used within the same time frame (and these also had identical responses for other questions) so we removed these two repeated cases. When multiple drugs were used before an adverse outcome we recoded the data so that responses to the adverse outcome were associated with each separate drug reported (rather than just the drug entered as leading to the adverse outcome). This was done because answering affirmatively about an adverse effect from a drug combination may have been based on order in which drug use was queried (e.g., alcohol was queried earlier in the survey) rather than by which drug was believed to “cause” the adverse effect. Sensitivity tests were conducted comparing results according to whether a single drug or multiple drugs were reported and results were similar. Therefore, we report statistics with data coded with responses applying to each drug reported when polydrug use occurred.
Analyses
While the main aim of this report was to provide descriptive information about adverse drug effects in this population, we also estimated the prevalence and correlates of individuals in this population experiencing an adverse drug outcome. To compute these estimates, selection probabilities were computed, which were composed of frequency of self-reported party attendance and number of party attendees (tracked via a clicker) who passed a predetermined recruitment line near the party entrance (MacKellar et al., 2007). For frequency of party attendance, weights were inversely proportional to frequency of attendance. For the component considering number of party attendees, weights were inversely proportional to the party-level response rate. The two weight components were combined via multiplication and normalized. This up-weighting of participants believed to have a lower probability of selection and down-weighting of those believed to have a higher probability of selection has been used in other studies utilizing venue-based sampling (Jenness et al., 2011; MacKellar et al., 2007). These probability weights were utilized when estimating prevalence and correlates of experiencing an adverse drug effect, to account for differential selection probability and clustering of participants entering each party.
Bivariable comparisons were conducted using chi-square, then we then fit all covariates simultaneously into separate multivariable generalized linear models using Poisson and log link with self-reported experience of any adverse outcome (yes/no) as the outcome. This generated adjusted prevalence ratios (aPRs) for each covariate. We also examined self-report of any adverse outcome according to frequency of self-reported attendance (utilizing unweighted data) and we tested for a trend by estimating odds of experiencing an adverse effect as a linear function of attendance as a continuous predictor.
All other analyses were descriptive in nature and we did not utilize probability weights for these analyses as many percentages (particularly for less prevalent drugs) were small, many participants reported more than one adverse effect, and shifting denominators across drugs made use of weights less feasible. We calculated the percentage of self-reporting past-year use of each drug, whether an adverse effect was experienced in the past year, and whether they sought help. We then calculated percentages for which drugs were most often used concomitantly with the drug the participant experienced the adverse effect on.
Results
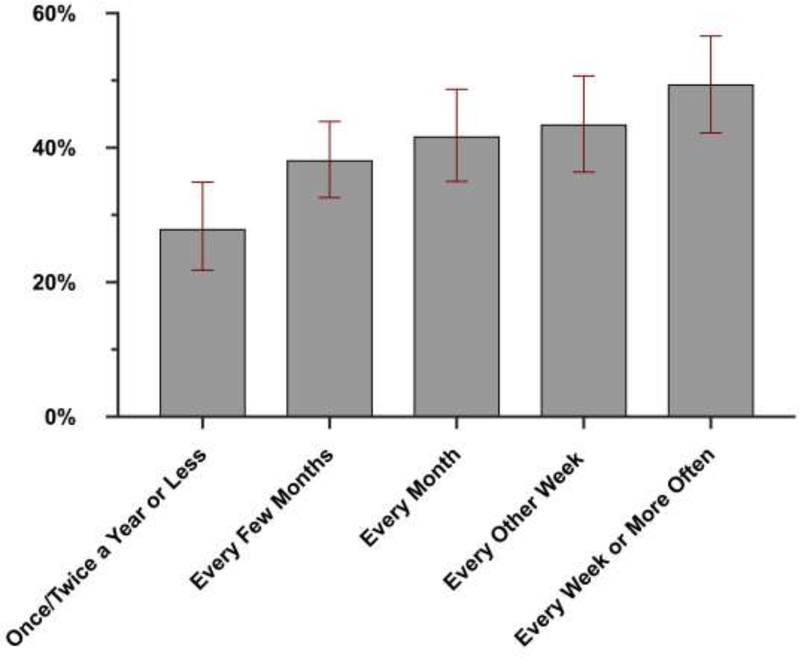
We estimate that a third (33.5%) of individuals in this population has experienced an adverse effect from a drug in the past year. While a total of 412 adverse effects were reported, 40.2% of those reporting an adverse effect reported experiencing an adverse effect on more than one instance (e.g., resulting from use of different drugs) over the past year. Specifically, while 56.6% (n=233) of those reporting an adverse effect reported experiencing one adverse effect in the past year, over a quarter (28.4%, n=117) reported two adverse outcomes, 9.7% (n=40) reported experiencing three, and 5.3% (n=22) reported experiencing four or more. As shown in Figure 1, as party attendance increased, so too did the percentage of participants reporting an adverse drug-related outcome (p for trend < .001). Specifically, half (49.5%) of those attending parties weekly or more often reported an adverse outcome compared to only about a quarter (27.9%) of very infrequent attendees (e.g., annual attendance) reporting such an outcome.
Figure 1.
Percentage of those reporting an adverse drug effect according to level of party attendance.
Sample characteristics and demographic correlates of reporting an adverse drug outcome within the full sample are presented in Table 1. In bivariable models, older participants (age 25–40) were more likely than younger participants (age 18–24) to report a drug-related adverse effect (p=.044), and males were more likely than females to report an adverse effect (p=.016). Those with a college degree were also more likely than those with lower education to report an adverse effect (p=.046). In the multivariable model, however, age and sex were no longer risk factors, and Asians were at low risk for reporting an adverse effect compared to white participants (aPR=0.69, p=.040), and those with a college degree (aPR=1.28, p=.041) and those identifying as “other” sexuality (aPR=2.43, p<.001) were at higher risk of reporting an adverse effect than those with lower education and heterosexuals, respectively.
Table 1.
Sample characteristics and demographic correlates of reporting an adverse drug effect in the past year
| Bivariable Comparisons | Multivariable Model | ||||
|---|---|---|---|---|---|
| Full Sample, Weighted % (n) | No Adverse Drug Effect, Weighted % | Adverse Drug Effect, Weighted % | aPR | (95% CI) | |
| Age | |||||
| 18–24 | 49.5 (504) | 69.6* | 30.4 | 1.00 | |
| 25–40 | 50.5 (525) | 63.4 | 36.6 | 1.07 | (0.83, 1.39) |
| Sex | |||||
| Male | 61.3 (604) | 62.6* | 37.4 | 1.00 | |
| Female | 38.7 (425) | 72.8 | 27.2 | 0.68 | (0.46, 1.01) |
| Race/Ethnicity | |||||
| White | 43.9 (494) | 62.0 | 38.0 | 1.00 | |
| Black | 10.0 (84) | 64.1 | 35.9 | 0.97 | (0.39, 2.41) |
| Hispanic | 22.1(207) | 67.8 | 32.2 | 0.88 | (0.67, 1.15) |
| Asian | 15.4 (159) | 75.8 | 24.2 | 0.69* | (0.49, 0.98) |
| Other/Mixed | 8.5 (85) | 72.7 | 27.3 | 0.72 | (0.41, 1.28) |
| Education | |||||
| Less than College | 41.4 (379) | 70.9* | 29.1 | 1.00 | |
| College Degree | 58.6(650) | 63.4 | 36.6 | 1.28* | (1.01, 1.63) |
| Weekly Income | |||||
| $0-$499 | 33.8 (368) | 68.1 | 31.9 | 1.00 | |
| $500-$999 | 37.5 (377) | 65.0 | 35.0 | 1.01 | (0.65, 1.56) |
| >$1,000 | 28.7 (284) | 66.5 | 33.5 | 0.87 | (0.56, 1.39) |
| Sexual Orientation | |||||
| Heterosexual | 81.5 (786) | 68.5 | 31.5 | 1.00 | |
| Gay/Lesbian | 11.8 (108) | 58.4 | 41.6 | 1.21 | (0.82, 1.79) |
| Bisexual | 5.7 (101) | 61.2 | 38.8 | 1.39 | (0.74, 2.59) |
| Other Sexuality | 0.9 (34) | 29.5 | 70.5 | 2.43** | (1.68, 3.53) |
Note. The outcome variable indicates the third (33.5%) of individuals estimated to have experienced an adverse effect from a drug in the past year. aPR = adjusted prevalence ratio; CI = confidence interval.
p < .05
p < .001
Table 2 presents percentages for self-reported adverse effects in descending order according to prevalence of use of each drug in the past 12 months. Two-thirds (67.8%) of adverse effects involved use of alcohol and over a third (37.2%) involved use of marijuana (with over a third [37.6%] of those reporting use of marijuana leading to an adverse effect reporting use of edibles). Adverse outcomes also commonly involved use of ecstasy/MDMA/Molly (14.9%), cocaine (11.4%), and/or LSD (10.0%). Relative to use, adverse effects most commonly resulted from use of opioids (e.g., prescription opioid misuse [41.1%]) and alcohol (33.9%). Concomitant use of other drugs before experiencing an adverse outcome was particularly prevalent among users of cocaine (55.7%), LSD (55.7%), ketamine (56.5%), LSD (41.2%), and ecstasy/MDMA/Molly (47.7%).
Table 2.
Self-reported prevalence of past-year drug use and self-report of drug-related adverse effects
| Prevalence of Past-Year Use % (n) | Prevalence of Drug Mentioned Within Adverse Outcomes % (n) | Prevalence of Adverse Outcome Relative to Past-Year Use % | Only One Drug Used Before Adverse Outcome % (n) | Multiple Drugs Used Before Adverse Outcome % (n) | |
|---|---|---|---|---|---|
| Alcohol | 81.1 (834) | 67.8 (283) | 33.9 | 61.5 (174) | 38.5 (109) |
| Marijuana | 71.5 (736) | 37.2 (172) | 23.4 | 57.6 (99) | 42.4 (73) |
| Ecstasy/MDMA/Molly | 41.1 (423) | 14.9 (86) | 20.3 | 52.3 (45) | 47.7 (41) |
| Cocaine | 34.0 (350) | 11.4 (88) | 25.1 | 44.3 (39) | 55.7 (49) |
| LSD | 23.1(238) | 10.0 (46) | 19.3 | 43.5 (20) | 56.5 (26) |
| Shrooms (psilocybin) | 21.4 (220) | 3.8 (24) | 10.9 | 75.0 (18) | 25.0 (6) |
| Ketamine | 16.1(166) | 5.0 (32) | 19.3 | 43.8 (14) | 56.3 (18) |
| Poppers (amyl/butyl nitrates) | 14.5 (149) | 1.8(13) | 8.7 | 92.3 (12) | 7.7 (1) |
| Amphetamine | 14.5 (149) | 7.8 (29) | 19.5 | 62.1 (18) | 37.9 (11) |
| Prescription Opioids | 9.9 (102) | 7.7 (42) | 41.2 | 90.5 (38) | 9.5 (4) |
| Benzodiazepines | 7.8 (78) | 2.8 (18) | 23.1 | 66.7 (12) | 33.3 (6) |
| GHB (gamma-hydroxybutyrate) | 4.6 (47) | 1.3 (5) | 10.6 | 80.0 (4) | 20.0 (1) |
| Synthetic Cathinones (“Bath Salts”) | 3.8 (39) | 0.9 (7) | 17.9 | 85.7 (6) | 14.3 (1) |
| Methamphetamine | 3.8 (39) | 1.4 (8) | 20.5 | 62.5 (5) | 37.5 (3) |
| DMT (N,N-Dimethyltryptamine) | 2.8 (28) | 0.2 (4) | 14.3 | 100.0 (4) | 0.0 (0) |
| Synthetic Cannabinoids | 2.5 (25) | 0.2 (3) | 12.0 | 100.0 (3) | 0.0 (0) |
| 2C Series | 2.5 (25) | 0.1 (3) | 12.0 | 66.7 (2) | 33.3 (1) |
| Other MDx (other than MDMA) | 2.4 (24) | 0.8 (4) | 16.7 | 75.0 (3) | 25.0 (1) |
| PCP (Phencyclidine) | 1.9 (20) | 0.3 (3) | 15.0 | 66.7 (2) | 33.3 (1) |
| Novel Dissociatives | 1.5 (15) | 1.2 (4) | 26.7 | 100.0 (4) | 0.0 (0) |
| Unknown powder | 1.2 (12) | 0.1 (2) | 16.7 | 100.0 (2) | 0.0 (0) |
| NBOMe | 0.9 (9) | 0.1 (2) | 22.2 | 50.0 (1) | 50.0 (1) |
| Fentanyl, its Analogs, & New Opioids | 0.8 (8) | 0.1 (4) | 50.0 | 100.0 (4) | 0.0 (0) |
| Heroin | 0.7 (7) | 0.8 (6) | 85.7 | 66.7 (4) | 33.3 (2) |
Note. Prevalence of use of opioids, amphetamine, and benzodiazepines refers to nonmedical use.
Over a fifth (23.3%) of adverse effects involved co-use of more than one drug. Of those reporting polydrug use before experiencing an adverse effect, 82.4% reported co-using two drugs, 14.5% reported cousing three, and 3.1% reported co-using four or five drugs. Alcohol was most commonly involved (68.5%) in adverse effects related to polydrug use, followed by marijuana (45.1%), cocaine (29.6%), ecstasy/MDMA/Molly (24.7%), LSD (15.4%), and ketamine (11.1%). Table 3 presents some of the most common drugs concomitantly used with other drugs before the experience of an adverse effect. Adverse effects involving use of cocaine (36.4%), marijuana (26.7%), ecstasy/MDMA/Molly (25.6%) and ketamine (25.0%) in particular often involved co-use of alcohol.
Table 3.
Most common drug combinations used before experience of adverse effect
| Alcohol % | Marijuana % | Ecstasy % | Cocaine % | LSD % | Ketamine % | |
|---|---|---|---|---|---|---|
| Alcohol | -- | 16.3 | 7.8 | 11.3 | 2.5 | 2.8 |
| Marijuana | 26.7 | -- | 5.2 | 9.3 | 6.4 | 2.9 |
| Ecstasy/MDMA/Molly | 25.6 | 10.5 | -- | 5.8 | 19.5 | 7.0 |
| Cocaine | 36.4 | 18.2 | 5.7 | -- | 5.7 | 6.8 |
| LSD | 15.2 | 23.9 | 10.5 | 10.9 | -- | 2.2 |
| Ketamine | 25.0 | 15.6 | 18.8 | 18.8 | 3.1 | -- |
As shown in Table 4, over half (57.1%) of individuals reported having asked someone for help when experiencing an adverse outcome after using “bath salts”; 43.8% asked for help after using ketamine, and 41.3% asked someone for help after using LSD. Both users of NBOMe experiencing an adverse effect asked someone for help. Adverse effects resulting from “bath salt” use were most likely to result in a hospital visit (57.1%), followed by opioids (e.g., fentanyl, its analogs, and other new opioids [25.0%], heroin [16.7%], prescription opioids [14.3%]).
Table 4.
Responses to Adverse Outcomes
| Asked Someone for Help, % | Felt Needed to Visit ED or Hospital, % | Went to ED or Hospital, % | |
|---|---|---|---|
| Alcohol | 39.2 | 9.9 | 4.6 |
| Marijuana | 29.7 | 9.3 | 1.2 |
| Ecstasy/MDMA/Molly | 37.2 | 14.0 | 7.0 |
| Cocaine | 22.7 | 11.4 | 4.5 |
| LSD | 41.3 | 21.7 | 6.5 |
| Shrooms | 25.0 | 12.5 | 0.0 |
| Ketamine | 43.8 | 3.1 | 0.0 |
| Poppers | 7.7 | 7.7 | 0.0 |
| Amphetamine | 17.2 | 3.4 | 3.4 |
| Prescription Opioids | 31.0 | 23.8 | 14.3 |
| Benzodiazepines | 22.2 | 5.6 | 0.0 |
| GHB | 20.0 | 0.0 | 0.0 |
| Synthetic Cathinones ("Bath Salts") | 57.1 | 71.4 | 57.1 |
| Methamphetamine | 12.5 | 12.5 | 12.5 |
| DMT | 0.0 | 25.0 | 25.0 |
| Synthetic Cannabinoids | 0.0 | 0.0 | 0.0 |
| 2C Series | 0.0 | 33.3 | 33.3 |
| Other MDx | 50.0 | 25.0 | 25.0 |
| PCP | 0.0 | 0.0 | 0.0 |
| Novel Dissociatives | 25.0 | 25.0 | 0.0 |
| Unknown powder | 50.0 | 0.0 | 0.0 |
| NBOMe | 100.0 | 0.0 | 0.0 |
| Fentanyl, its Analogs, & Other New Opioids | 25.0 | 50.0 | 25.0 |
| Heroin | 33.3 | 16.7 | 16.7 |
Note. ED = emergency department.
Discussion
While it has been well-documented that drug use is prevalent among those who attend EDM parties, further research was needed in order to determine the extent to which use among this high-risk group leads to adverse drug outcomes. Although there are national reports of poisonings and mortality related to drug use in the US, it is unknown to what extent these estimates are reflective of the EDM party-attending population. To our knowledge, this was among the first epidemiological studies to query drug-related adverse effects (via survey self-administration) with regard to dozens of individual drugs. Moreover, whereas most studies on this high-risk population have relied on convenience samples of frequent attendees (e.g., via internet survey), we utilized time-space sampling in order to increase generalizability of estimates.
We estimate that a third of EDM attendees in NYC have experienced an adverse drug-related outcome in the past year. This suggests that drug use is not only prevalent among this population, but that there is a substantial amount of drug-related harm experienced by these individuals as well. Although we could not deduce whether adverse effects occurred at or after attending such parties, we determined that the likelihood of experiencing an adverse drug-related effect increases as EDM party attendance increases, possibly suggesting a dose-response association. This may be because more frequent attendance is associated with higher risk (and higher frequency) of use of various drugs (Palamar, Acosta, Sherman, Ompad, & Cleland, 2016; Palamar, Barratt, Ferris, & Winstock, 2016; Palamar, Griffin-Tomas, & Ompad, 2015). Therefore, regardless of where drug use and adverse effects occurred, it appears that increased involvement with the EDM scene indicates higher risk of experiencing adverse drug-related effects.
Alcohol use was associated with the greatest number of adverse outcomes, involved in over two-thirds of all mentions. This may simply be, in part, a function of the ubiquitous nature of alcohol. However, what is of particular concern is polydrug use involving alcohol as our findings demonstrate that over two-thirds of adverse effects involving polydrug use also involved alcohol. More specifically, over a quarter of adverse outcomes involving cocaine, marijuana, ecstasy/MDMA/Molly, and/or ketamine involved co-use of alcohol, suggesting that alcohol may increase risk of an adverse effect. In 2014, alcohol was involved in 12–22% of fatal drug overdoses in the US that were related to use of opioids, benzodiazepines, or cocaine (Warner, Trinidad, Bastian, Minino, & Hedegaard, 2016). Therefore, prevention and harm reduction efforts need more focus on alcohol use in these high-risk scenes.
Like alcohol, we found that marijuana use was also associated with a substantial proportion of adverse effects, accounting for over a third (37.2%) of mentions. Furthermore, at least 40% of these situations involved co-use of other drugs, which effectively recapitulates that polydrug use is a potential area of concern in this population. Further still, over a third of the individuals experiencing an adverse effect after marijuana use specified that it occurred after ingesting edibles. This may have resulted from consuming too much due to delayed onset of action and experiencing a more intense and/or prolonged high (Ouellette, Cearley, Judge, Riley, & Jones, 2018). While marijuana is among the most prevalent drugs used, more research is needed to determine whether use increases risk or exacerbates adverse effects of other drugs.
Cocaine is a popular party drug that has been shown to be associated with a higher likelihood of leading to physical harm compared to most other drugs (Nutt, King, Saulsbury, & Blakemore, 2007; Substance Abuse and Mental Health Services Administration [SAMHSA], 2013b). Our findings show that cocaine use was associated with over one-fifth (11.4%) of adverse outcomes, with over half (55.7%) of these events being associated with concomitant use of other drugs as well (primarily alcohol). We also found that use of other stimulants, such as ecstasy/MDMA/Molly, amphetamine, methamphetamine, and “bath salts”, commonly led to adverse effects, with 14–48% of use of these stimulants being associated with co-use of other drugs (primarily alcohol). Indeed, it is also known that stimulants are often used in a polydrug manner; for example, two-thirds of the 22,000 ED visits involving “bath salt” use in 2011 involved co-use of other drugs (SAMHSA, 2013a), while an estimated three-fourths of cocaine use in the US involves concomitant use of alcohol (Liu, Williamson, Setlow, Cottler, & Knackstedt, 2018). It is unknown, however, whether co-use of alcohol may have exacerbated or ameliorated adverse effects associated with stimulant use among these users.
Ketamine is typically regarded as a less risky drug than many others investigated in this study, and is associated with far fewer poisonings and deaths than most other drugs (Gable, 2004; Gummin et al., 2017). Our findings show that 5% of adverse effect mentions included ketamine. However, the findings also suggest that ketamine use becomes riskier when used concomitantly with other drugs. Thus, the safety profile of ketamine appears to be altered when used in a polydrug manner. The same may be true of benzodiazepines, which tend to also be regarded as lower risk relative to other drugs examined in this study (Nutt, King, & Phillips, 2010); while over one-fifth of nonmedical users in this sample reported an adverse effect from use, a third of these individuals reported co-use of other drugs. These findings are in agreement with national trends, where almost two thirds of poisonings involving benzodiazepines in 2016 involved use of one or more other drugs (Gummin et al., 2017). While motives for specific drug combinations were not assessed, self-medication with drugs such as benzodiazepines to ‘come down’ from other drugs appears to be common, and these drugs are commonly used in medical settings to treat agitation related to use of stimulants (Richards et al., 2015).
Although nonmedical use of prescription opioids is less prevalent than use of many other drugs among this sample, it appears to lead to more frequent and consequential outcomes than most other drugs. For example, 41% of past-year nonmedical opioid use resulted in an adverse outcome, with 14% of these events leading to an ED visit as a result. Similarly, a quarter and nearly one-fifth (17%) of those experiencing an adverse outcome after using novel opioids and heroin, respectively, also reported visiting an ED. These findings add to previous research indicating that opioids appear to be among the riskiest drugs, as they have the highest potential for acute severe toxicity (Gable, 2004; Morgan, Muetzelfeldt, Muetzelfeldt, Nutt, & Curran, 2010; Nutt, King, Saulsbury, & Blakemore, 2007).
The results of this study can inform prevention, harm reduction, and perhaps medical response in relation to this high-risk population. We determined that some drugs (e.g., alcohol) are associated with high prevalence of harm, while other drugs (e.g., opioids, NBOMe, “bath salts”), though less prevalent, appear to be associated with more severe effects. Each drug is associated with its own relative level of risk, and this needs to be considered in prevention efforts. Importantly, though, our findings also confirm that polydrug use is common in this population and may increase the risk of experiencing adverse outcomes, depending on the drugs combined. While we could not deduce to what extent adverse effects occurred at EDM parties, these are in fact high-risk venues due to a combination of high prevalence of drug use and environmental factors. Dancing for hours, hot temperature, and dehydration occurring at such events, for example, appears to exacerbate the risk for experience of adverse effects among those who use drugs (Parrott et al., 2006; Parrott, 2004; Ridpath et al., 2014). Public health experts need to consider these circumstances when considering prevention and harm reduction promotion. However, current drug policy in the US (e.g., the “RAVE Act”) discourages harm reduction organizations and party promoters from disseminating drug-related harm reduction messages and this appears to be a major obstacle in preventing adverse effects related to drug use (Laing, Tupper, & Fairbairn, 2018). Policy enabling harm reduction practices (e.g., pill testing, drug education about how to prevent adverse effects) may help address the extent of adverse effects—or severity of adverse effects—experienced by many drug users who attend such events.
Limitations
It may be difficult for participants to recall drug use and drug effects up to a year ago, and inebriation at the time of experiencing an adverse effect can affect perception and recall of the experience. Polydrug use was common and limits the ability of the individual using to decipher if and how effects were related to each drug used. Likewise, the data provided limited our ability to determine whether responses applied to a single drug or a combination of drugs in cases where polydrug use was reported. However, we did conduct sensitivity tests and results were similar when comparing results of the primary drug reported and when assigning effects to all drugs reportedly used before the adverse outcome.
Adverse effect questions were not standardized. We did not assess severity of effects, and adverse effects are subjective and participants could have had differing interpretations regarding what was harmful or unpleasant. A “scary” situation experienced by a user, for example, may constitute an adverse outcome. It is also possible that some individuals reported a hangover from alcohol as an adverse effect. Needing and seeking help could have also been interpreted differently for different participants. Results are also limited by the fact that participants reported drugs they believed they used, but it is possible adulterated drugs were used (Oliver et al., 2018). Finally, while drugs like “bath salts” and NBOMe appeared to be particularly high-risk (e.g., for needing help), we focused less on these drugs because prevalence of use was so low that even a few mentions of “asked someone for help” inflated the prevalence of responses. Finally, estimated age and gender were not recorded of those who refused to take the survey.
Conclusion
Adverse effects from drug use among the EDM attendee population are prevalent. Alcohol-related adverse effects, in particular, are highly prevalent, and opioid-related adverse effects appear to be especially detrimental in this population, so additional attention needs to be paid to individuals who use these drugs. This information can be used to inform prevention and to guide harm reduction efforts among those who insist on using various drugs. Knowing the risks of experiencing adverse effects may allow individuals to use in a safer manner. Finally, although we could not deduce the extent to which adverse effects occurs at such parties, party staff and medical staff may be more equipped to respond to drug-related adverse outcomes if they are aware of the relative prevalence and risk of specific drug-related adverse outcomes.
Acknowledgement
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Numbers K01DA038800, R01DA044207, and P30DA011041. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Interest: The authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Chhabra N, Gimbar RP, Walla LM, & Thompson TM (2018). Emergency department patient burden from an electronic dance music festival. The Journal of Emergency Medicine, 54(4), 435–439. 10.1016/j.jemermed.2017.10.007. [DOI] [PubMed] [Google Scholar]
- Edwards IR, & Aronson JK (2000). Adverse drug reactions: definitions, diagnosis, and management. Lancet, 356(9237), 1255–1259. 10.1016/s0140-6736(00)02799-9. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction (2018). Preventing overdose deaths in Europe. Retrieved from http://www.emcdda.europa.eu/topics/pods/preventing-overdose-deaths_en.
- Gable RS (2004). Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction, 99(6), 686–696. 10.1111/j.1360-0443.2004.00744.x. [DOI] [PubMed] [Google Scholar]
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, & Banner W (2017). 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clinical Toxicology (Philadelphia, Pa.), 55(10), 1072–1252. 10.1080/15563650.2017.1388087. [DOI] [PubMed] [Google Scholar]
- Hughes CE, Moxham-Hall V, Ritter A, Weatherburn D, & MacCoun R (2017). The deterrent effects of Australian street-level drug law enforcement on illicit drug offending at outdoor music festivals. International Journal of Drug Policy, 41, 91–100. 10.1016/j.drugpo.2016.12.018. [DOI] [PubMed] [Google Scholar]
- Jenness SM, Neaigus A, Murrill CS, Gelpi-Acosta C, Wendel T, & Hagan H (2011). Recruitmentadjusted estimates of HIV prevalence and risk among men who have sex with men: effects of weighting venue-based sampling data. Public Health Reports, 126(5), 635–642. 10.1177/003335491112600505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laing MK, Tupper KW, Fairbairn N (2018). Drug checking as a potential strategic overdose response in the fentanyl era. The International Journal on Drug Policy, 62, 59–66. 10.1016/j.drugpo.2018.10.001. [DOI] [PubMed] [Google Scholar]
- Liu Y, Williamson V, Setlow B, Cottler LB, & Knackstedt LA (2018). The importance of considering polysubstance use: lessons from cocaine research. Drug and Alcohol Dependence, 192, 16–28. 10.1016/j.drugalcdep.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, & Sullivan PS (2007). Surveillance of HIV Risk and prevention behaviors of men who have sex with men--a national application of venuebased, time-space sampling. Public Health Reports, 122 Suppl 1, 39–47. 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CJ, Muetzelfeldt L, Muetzelfeldt M, Nutt DJ, & Curran HV (2010). Harms associated with psychoactive substances: findings of the UK National Drug Survey. Journal of Psychopharmacology, 24(2), 147–153. 10.1177/0269881109106915. [DOI] [PubMed] [Google Scholar]
- Nutt D, King LA, Saulsbury W, & Blakemore C (2007). Development of a rational scale to assess the harm of drugs of potential misuse. Lancet, 369(9566), 1047–1053. 10.1016/s0140-6736(07)60464-4. [DOI] [PubMed] [Google Scholar]
- Nutt DJ, King LA, & Phillips LD (2010). Drug harms in the UK: a multicriteria decision analysis. Lancet, 376(9752), 1558–1565. 10.1016/s0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Oliver CF, Palamar J, Salomone A, Simmons SJ, Philogene-Khalid H, Stokes-McCloskey N, & Rawls S (2018). Synthetic cathinone adulteration of illegal drugs. Psychopharmacology, in press. 10.1007/s00213-018-5066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellette L, Cearley M, Judge B, Riley B, & Jones J (2018). Cooking with cannabis: The rapid spread of (mis)information on YouTube. American Journal of Emergency Medicine, 36(7), 1300–1301. 10.1016/j.ajem.2017.10.060. [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Acosta P, Ompad DC, & Cleland CM (2017). Self-reported Ecstasy/MDMA/”Molly” use in a sample of nightclub and dance festival attendees in New York City. Substance Use and Misuse, 52(1), 82–91. 10.1080/10826084.2016.1219373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Acosta P, Sherman S, Ompad DC, & Cleland CM (2016). Self-reported use of novel psychoactive substances among attendees of electronic dance music venues. The American Journal of Drug and Alcohol Abuse, 42(6), 624–632. 10.1080/00952990.2016.1181179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Barratt MJ, Ferris JA, & Winstock AR (2016). Correlates of new psychoactive substance use among a self-selected sample of nightclub attendees in the United States. American Journal on Addictions, 25(5), 400–407. 10.1111/ajad.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Griffin-Tomas M, & Ompad DC (2015). Illicit drug use among rave attendees in a nationally representative sample of US high school seniors. Drug and Alcohol Dependence, 152, 24–31. 10.1016/j.drugalcdep.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Salomone A, Gerace E, Di Corcia D, Vincenti M, & Cleland CM (2017). Hair testing to assess both known and unknown use of drugs amongst ecstasy users in the electronic dance music scene. International Journal on Drug Policy, 48, 91–98. 10.1016/j.drugpo.2017.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott AC (2004). MDMA (3,4-Methylenedioxymethamphetamine) or ecstasy: the neuropsychobiological implications of taking it at dances and raves. Neuropsychobiology, 50(4), 329–335. 10.1159/000080961. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Rodgers J, Buchanan T, Ling J, Heffernan T, & Scholey AB (2006). Dancing hot on Ecstasy: physical activity and thermal comfort ratings are associated with the memory and other psychobiological problems reported by recreational MDMA users. Human Psychopharmacology, 21(5), 285–298. 10.1002/hup.773. [DOI] [PubMed] [Google Scholar]
- Richards JR, Albertson TE, Derlet RW, Lange RA, Olson KR, & Horowitz BZ (2015). Treatment of toxicity from amphetamines, related derivatives, and analogues: a systematic clinical review. Drug and Alcohol Dependence, 150, 1–13. 10.1016/j.drugalcdep.2015.01.040. [DOI] [PubMed] [Google Scholar]
- Ridpath A, Driver CR, Nolan ML, Karpati A, Kass D, Paone D, … Kunins HV (2014). Illnesses and Deaths Among Persons Attending an Electronic Dance-Music Festival - New York City, 2013. Morbidity and Mortality Weekly Report, 63(50), 1195–1198. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6350a3.htm. [PMC free article] [PubMed] [Google Scholar]
- Seth P, Scholl L, Rudd RA, & Bacon S (2018). Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015–2016. Morbidity and Mortality Weekly Report, 67(12), 349–358. 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2013a). “Bath Salts” Were Involved in Over 20,000 Drug-Related Emergency Department Visits in 2011. Retrieved from http://www.samhsa.gov/data/sites/default/files/spot117-bath-salts-2013/spot117-bath-salts2013.pdf.
- Substance Abuse and Mental Health Services Administration (2013b). The DAWN Report: Highlights of the 2011 Drug Abuse Warning Network (DAWN) Findings on Drug-Related Emergency Department Visits. Retrieved from Rockville, MD: http://www.samhsa.gov/data/sites/default/files/DAWN127/DAWN127/sr127-DAWN-highlights.htm. [PubMed] [Google Scholar]
- Turris SA, Jones T, & Lund A (2018). Mortality at Music Festivals: An Update for 2016–2017 - Academic and Grey Literature for Case Finding. Prehospital and Disaster Medicine, 33(5), 553–557. . [DOI] [PubMed] [Google Scholar]
- Turris SA, & Lund A (2017). Mortality at music festivals: academic and grey literature for case finding. Prehospital and Disaster Medicine, 32(1), 58–63. . [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (2018). Drug-related deaths and mortality rates in Europe. Retrieved from https://dataunodc.un.org/drugs/mortality/europe.
- United States Drug Enforcement Administration (2016). Counterfeit Prescription Pills Containing Fentanyls: A Global Threat (DEA Intelligence Brief No. DEA-DCT-DIB-021–16). US Drug Enforcement Agency; Retrieved from http://www.dea.gov/docs/Counterfeit%20Prescription%20Pills.pdf. [Google Scholar]
- Warner M, Trinidad JP, Bastian BA, Minino AM, & Hedegaard H (2016). Drugs most frequently involved in drug overdose deaths: United States, 2010–2014. National Vital Statistics Reports, 65(10), 115. [PubMed] [Google Scholar]
- Watson K (2018). IMS Business Report 2018–An Annual Study of the Electronic Music Industry. Retrieved from https://www.internationalmusicsummit.com/.../IMS-Business-Report-2018-vFinal2.pdf.