Abstract
Objectives:
To address increasing rates of stimulant misuse in college students, this study developed an evidence-based, brief clinical practice intervention for primary care providers (PCPs) to reduce stimulant medication diversion among young adults with ADHD.
Methods:
College students (N-114; 18-25 years; 68% attending universities; 24% attending community college) treated for ADHD with a stimulant and their PCPs across six practices participated in this initial, uncontrolled study of pre- to post-intervention change. An educational workshop providing strategies aimed at reducing stimulant diversion was developed and delivered to providers and staff across all practices (50% pediatric; 50% family medicine). Patients and providers completed baseline and post intervention surveys.
Results:
Diversion was relatively infrequent, 16.7% at baseline and 14.9% post-intervention, respectively. Statistically significant decreases from baseline to post-intervention were found for three diversion risk factors: (1) number of times approached to divert, (2) intent to share, sell, or trade stimulants, and (3) disclosure of stimulant use. Providers and staff reported mostly high satisfaction with the training.
Conclusions:
This study provides initial evidence for a PCP-delivered intervention to reduce stimulant diversion. Research is needed on the efficacy of targeting college students directly, working with pharmacies and student health centers, and preventing misuse among teenagers.
Keywords: Attention-Deficit/Hyperactivity Disorder (ADHD), College Students, Prescription Misuse
Introduction
Stimulant medications for Attention-Deficit/Hyperactivity Disorder (ADHD), amphetamines and methylphenidate, are among the most researched and acutely efficacious psychoactive medication treatments in behavioral health.1,2 They are also classified by the U.S. Food and Drug Administration as Schedule II controlled substances due to their potential for abuse. Although few children and adults with ADHD misuse their prescribed stimulants (i.e., take more than prescribed),3,4 non-prescribed use by college students is prevalent. In one of the largest surveys to date, 9.3% of undergraduates used them without a prescription in the prior year, and prevalence increased significantly between 2003 and 2013.5 Between 2005 and 2010, stimulant-related presentations to the emergency department increased by 68%.6 As a result, calls have been made at the national level for the development of preventive methods.6-8
Surveys have revealed that non-prescribed stimulants are largely acquired from peers who share, sell, or trade their own prescribed medication8,9 to other students to enhance academic performance or for recreation.9-11 One-quarter to one-third of college students prescribed stimulants report diverting their medication, and well over half are approached to divert.12-14 A small cross-sectional literature suggests some similarity between diverters and misusers in risk characteristics such as having friends who misuse stimulants, recreational substance use (e.g., marijuana), and other externalizing behaviors.15-18 In addition to the obvious legal risks of distributing a controlled substance, diversion increases risk of untreated ADHD. Reducing diversion is therefore important for individuals with prescriptions, and it has the potential to lower the rate of non-prescribed stimulant misuse among college students.
Intervening at the level of the prescribing provider is a potential route to stimulant diversion reduction. Past studies have demonstrated reduction in risk behaviors, such as alcohol misuse, after brief intervention in primary care.19-21 However, current practice guidelines for treating ADHD do not offer specific strategies for addressing diversion.22 Moreover, most stimulant prescriptions are written in primary care settings and primary care providers (PCPs) are often the sole managers of care for children with ADHD up to at least age 21.23 Thus, there is a need to develop and test evidence-based strategies for reducing diversion risk in primary care. The current study reflects the first systematic attempt to develop a training workshop for PCPs and their staff on brief clinical practice strategies for the prevention of stimulant diversion by their college student patients with ADHD. In a pre-post design, we hypothesized that after provider and staff training, patients would report reduced stimulant diversion and associated risk for the sharing, selling, and trading of prescribed stimulant medications for ADHD.
Methods
Overview
Patients, n=114, from six primary care practices (3 pediatric, 3 family medicine) participated in a study of stimulant diversion risk following provider and practice staff training in stimulant diversion prevention. Surveys were collected from patients twice – pre- (Time 1) and post- (Time 2) training -- and their reports of stimulant diversion risk are the focus of this paper. Satisfaction ratings were collected from providers and practice staff immediately after training.
Participating practices and patients
Primary care practices.
Practices were selected based on geographic proximity (within ~20 miles of the University of Pittsburgh), participation in Pediatric PittNet (a practice-based research network hosted by the university; pediatric practices only), practice size (targeting larger practices), and provider willingness; no practices declined participation. Practices were predominantly suburban (one pediatric practice was within the city of Pittsburgh). (See Supplement 1 for data describing practices.)
Patients.
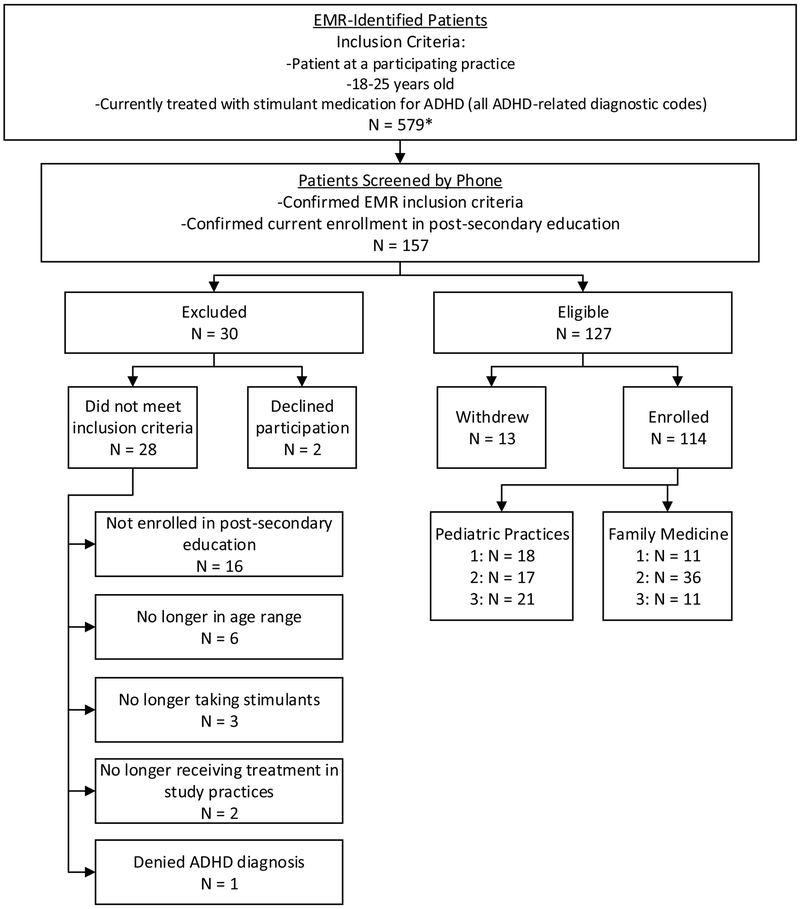
Patients were recruited if they were 18-25 years old and prescribed stimulant medication for ADHD (any diagnostic or billing code related to ADHD) at one of the six participating practices. Patients were required to be in post-secondary education or training. Table 1 provides additional descriptive information on enrolled patients. Figure 1 describes the method and flow of recruitment.
Table 1.
Patient characteristics at Time 1 (n=114)
| N | % | |
|---|---|---|
| Age (Mean, SD) | 20.4 | (1.6) |
| Male | 60 | (52.6%) |
| Single | 105 | (92.1%) |
| Race | ||
| White or Caucasian | 109 | (95.6%) |
| Native Hawaiian or Other Pacific Islander | 1 | (0.9%) |
| More than one race | 4 | (3.5%) |
| Hispanic Ethnicity | 5 | (4.4%) |
| Highest level of Parent Education | ||
| High School Graduate | 8 | (7.0%) |
| Technical or specialized training | 6 | (5.3%) |
| Partial College | 9 | (7.9%) |
| Associate degree | 7 | (6.1%) |
| College graduate | 44 | (38.6%) |
| Graduate Degree | 40 | (35.1%) |
| Educational Type | ||
| On the job training | 4 | (3.5%) |
| Community College or Trade School | 27 | (23.7%) |
| 4-year college/university | 77 | (68.1%) |
| Graduate School | 5 | (4.4%) |
| Year in College | ||
| Freshman | 32 | (28.1%) |
| Sophomore | 28 | (24.6%) |
| Junior | 19 | (16.7%) |
| Senior | 34 | (29.8%) |
| Full Time Student | 93 | (81.6%) |
| Fraternity/Sorority Member | 23 | (20.2%) |
| Housing Type | ||
| With parents | 44 | (38.6%) |
| On Campus | 33 | (28.9%) |
| Off Campus | 23 | (20.2%) |
| Fraternity/Sorority House | 4 | (3.5%) |
| Other | 10 | (8.8%) |
Figure 1. Flow of Study Recruitment.
Note: EMR-identified patients were initially contacted by practice staff during office visits, by letter, and/or by phone. If the patient was successfully contacted and agreeable to participation, he/she was referred to study staff who completed phone screens to determine final eligibility.
*The number of EMR-identified patients by practice include the following: n=74, 85, and 50 for pediatric practices 1, 2, and 3, respectively (practice 3 is an estimate); n=51, 125, 194 for family medicine practices 1, 2, and 3, respectively.
Data Collection
Patients completed electronic surveys, programmed in Qualtrics (Provo, UT), about stimulant diversion and associated risk behaviors at Time 1 and Time 2. Time 2 assessments occurred M(SD)=7.26 (1.70) months after provider and practice staff stimulant diversion prevention training. Patients were assured confidentiality, including from their providers, bolstered by a NIDA-issued Certificate of Confidentiality. Informed consent was collected from all participating providers, staff, and patients; the study was IRB-approved.
Measures.
In addition to basic demographics and stimulant diversion, domains of assessment reflected psychosocial and environmental factors related to diversion and misuse.12,15-18,24,25 Surveys were pilot-tested by research staff and five patients at an ADHD specialty clinic at Western Psychiatric Hospital, Pittsburgh, PA. Electronic medical records (EMRs) were reviewed for patient contact with their study practice between provider training and completion of the Time 2 survey.
Stimulant diversion was assessed with questions about selling, sharing, or trading prescribed stimulant medication (e.g., “How many times in the last year has someone asked you to share your stimulant medication for studying?”, “Did you actually share your stimulant medication for studying?”, 0=no, 1=yes). Items assessed self- and other-initiated diversion (e.g., “How many times in the last year have you offered your medication to a friend—to help them study—without their asking?”). Diversion for recreational purposes (“☆ for partying”) was also assessed. To accommodate skew, diversion was coded “1” (else=0) if any selling, sharing, or trading occurred in the last year. Approached to divert in the last year was a count of the number of times patients were approached to share for studying, for partying, or to buy (3 items, open-ended response). Intent to divert was modeled after similar measures used with adolescents.26 Patients were asked how likely they were to give away, sell, or trade their stimulant medication in each of 9 situations such as “to help a friend or family member who needed it to study.” Response options ranged from 0=not at all likely to 3=very likely. The variable analyzed was a count of situations that the patient indicated any likelihood of diverting (score of 1 or higher). Perceived harm to self was one item indexing “likelihood that you would get in trouble for giving away, selling, or trading your stimulant medication?”; four responses ranged from 1=0-25% chance to 4=76-100% chance. Perceived harm to others, mean score (3 items), was adapted from Johnston and colleagues27 to assess how much people risk harming themselves, physically or in other ways, if they take stimulant medication without a prescription once or twice, occasionally, or regularly, alpha(T1)=0.82. Responses were 0=no risk to 3=great risk. Knowledge of school policies was one item inquiring about awareness (0=no; 1=yes) of their school policies about stimulant medication. Stimulant use disclosure was number of social network types (e.g., roommates, a small circle of friends, coworkers, acquaintances) who know that the patient has a stimulant prescription (family members and romantic partners were excluded). Stimulant storage (access) was one item, “Is your stimulant medication kept in a shared location where other people have access to it?” (0=no, 1=yes). Changed storage was one item at Time 2 only, “In the last year, have you changed how you store your stimulant medication?” (0=no, 1=yes), followed by an open-ended query, “What did you change and why?” Stimulant storage (locked) was one item, “Do you typically lock up your stimulant medication?” (0=no, 1=yes). Patients also reported any psychoactive medication use.
Intervention (Stimulant Diversion Prevention Training)
All providers and practice staff interfacing with patients (e.g., nurses, medical assistants, receptionists) were asked to attend a one-hour workshop on brief clinical practice strategies to reduce the likelihood of stimulant diversion by their patients (a total of 55 providers and 75 additional staff attended). Workshops were conducted at each practice and led by the first author (BSGM) and clinical coordinator (HLK). Continuing medical education credit and meals were provided. A prescribing provider of record for all but six patients participated in training. Two to eight providers at each practice had one to 14 patients in the study, M(SD)=3.60 (3.16) patients/provider.
The workshop content included training in 1) brief patient education and counseling (e.g., negative consequences of diversion), 2) enhancing diversion prevention strategies, and 3) effective medication monitoring. The presentation included three brief video demonstrations of provider:patient interactions. A handout was provided in ample quantity, and with demonstration of its use, to facilitate provider: patient discussion. Workshop content was based on selected findings from the Time 1 surveys, consultations with providers, methods for opioid management,28,29 recent recommendations for provider behavior when prescribing stimulants,7,8 and trials in pediatric care to reduce adolescent health risk behaviors.30 The workshop was refined with consultant feedback and piloting in the ADHD clinic.
Statistical Analysis
Generalized Estimating Equations (GEE) analyses were used to analyze data for all available patients and to account for the correlated nature of the repeated measurements within each patient. Several types of GEE models were used for a priori outcome variables: binomial logistic for binary outcomes, negative binomial with log link for count outcomes, linear models for continuous (interval scale; mean score) outcomes, and multinomial distribution with cumulative logit link for ordinal outcomes. Practice effects were accounted for through a fixed-effects approach (practice was treated as a nominal covariate). Preliminary analyses showed dependence among patients sharing a provider to be negligible (working correlations across outcomes were uniformly small, −.01−.02). Provider effects were therefore not included in the fitted models.
Results
Participation and treatment by Time 2
At Time 2, 93% (106/114) participated (M=14.1 months after Time 1, SD=4.4, mean age=21.5, SD=1.6). Most (82.1%, 87/106) were enrolled in post-secondary education in the past year: 64.4% (56/87) in a 4-year college/university; 19.5% (17/87) in community college or trade school; 9% (8/87) in advanced college education; 3.4% (3/87) in on-the-job training. Nearly all (95.2%, 100/105) were still taking a prescription stimulant. (Medication information was missing for one patient at Time 2.) Most (76.4%; 81/106) were still receiving treatment at their Time 1 practice. Of those for whom identifiable EMR data were available to the study team (n=97) and were still medicated (n=75), 75% (n=56/75) had EMR-recorded contact related to ADHD treatment with their provider’s office after diversion prevention training (e.g., office visit, prescription, phone conversation), M(SD)=3.40(3.66) contacts, range=1-17. Slightly more had contact with their practice for any reason, 83% (62/75).
Diversion and risk factors, Time 1 to Time 2
Table 2 shows the results of the analyses examining change in diversion and diversion risk from Time 1 to Time 2. None of the practice effects were statistically significant at p<05.
Table 2.
Change from Time 1 to Time 2 in diversion and diversion risk
| Time 1a | Time 2b | Results of GEE Models | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n or | % or SD | n or | % or SD | Wald χ2 | p | β | SE | Exp(β) | |
| Diversion | |||||||||
| Diverted in the last year, n (%) | 19 | (16.67) | 17 | (14.91) | 0.003 | (0.959) | −0.01 | (0.28) | 0.99 |
| Approached to Divert | |||||||||
| Number of times approached in the last year, mean (SD) | 10.51 | (20.79) | 4.47 | (12.72) | 17.548 | (0.000) | −0.94 | (0.22) | 0.39 |
| Intent to Divert | |||||||||
| Intent to divert, mean (SD) | 1.20 | (1.84) | 0.89 | (1.79) | 4.666 | (0.031) | −0.03 | (0.01) | 0.97 |
| Perceived Harm of Diversion | |||||||||
| To self (likelihood of getting in trouble), n (%) | 0.119 | (0.730) | −0.07 | (0.20) | 0.93 | ||||
| 0-25% | 68 | (59.65) | 59 | (51.75) | |||||
| 26-50% | 8 | (7.02) | 16 | (14.04) | |||||
| 51-75% | 10 | (8.77) | 10 | (8.77) | |||||
| 76-100% | 26 | (22.81) | 20 | (17.54) | |||||
| To others, mean (SD) | 1.57 | (0.73) | 1.55 | (0.86) | 0.157 | (0.692) | −0.04 | (0.09) | - |
| Knowledge | |||||||||
| Knowledge of school policies (for stimulant medication), n (% with reported awareness) | 26 | (22.81) | 27 | (23.68) | 0.833 | (0.361) | 0.22 | (0.24) | 1.25 |
| Stimulant Use Disclosure | |||||||||
| Number of social network types who know about your stimulant medication, mean (SD) | 2.77 | (2.17) | 1.99 | (1.96) | 15.922 | (0.000) | −0.44 | (0.11) | 0.64 |
| How many roommates know | 0.89 | (0.87) | 0.66 | (0.86) | 7.038 | (0.008) | −0.55 | (0.21) | 0.58 |
| How many friends know | 1.04 | (0.76) | 0.74 | (0.75) | 15.411 | (0.000) | −0.79 | (0.20) | 0.45 |
| How many fraternity brothers/sorority sisters know | 15 | (13.16) | 15 | (13.16) | 0.919 | (0.338) | −0.53 | (0.56) | 0.59 |
| How many coworkers or acquaintances know | 0.20 | (0.50) | 0.10 | (0.39) | 3.861 | (0.049) | −0.85 | (0.43) | 0.43 |
| Stimulant Storage | |||||||||
| Access (shared location), n (%) | 31 | (27.19) | 26 | (22.81) | 0.282 | (0.595) | −0.13 | (0.25) | 0.88 |
| Locked storage, n (%) | 14 | (12.28) | 14 | (12.28) | 0.048 | (0.827) | 0.08 | (0.36) | 1.08 |
Note:
Time 1: n = 114,
Time 2: n = 105.
Diversion was infrequent, with 16.7% and 14.9% diverting at Times 1 and 2, respectively. This reduction was not statistically significant. For descriptive purposes, we provide the breakdown of diversion behaviors at Time 1: 75.0% (12/16) diverted for cognitive performance (studying), and 18.8% (3/16) diverted for recreational purposes (partying). One person diverted for studying and for partying. For n=3, reasons for diverting were not available. The mean number of times diverting was 1.79(SD=1.27), range=1-6, n=19.
Statistically significant reduction was found for three of eight diversion risk factors (approached to divert, intent to divert, and stimulant use disclosure). The average number of times approached to divert was reduced by half, from 10.5 to 4.5 times in the last year. At Time 1, 52.6% (60/114) were approached to divert (range=1 to 106 times). Of those, 36.7% (22/60) were approached for studying, 5.0% (3/60) were approached for partying, and 50.0% (30/60) were approached for both reasons (8.3% or 5/60 were approached to sell without associated reason). At Time 2, 33.9% (36/106) were approached to divert (range=1 to 112 times). Of those, 41.7% (15/36) were approached for studying, 11.1% (4/36) were approached for partying, and 47.2% (17/36) were approached for both reasons.
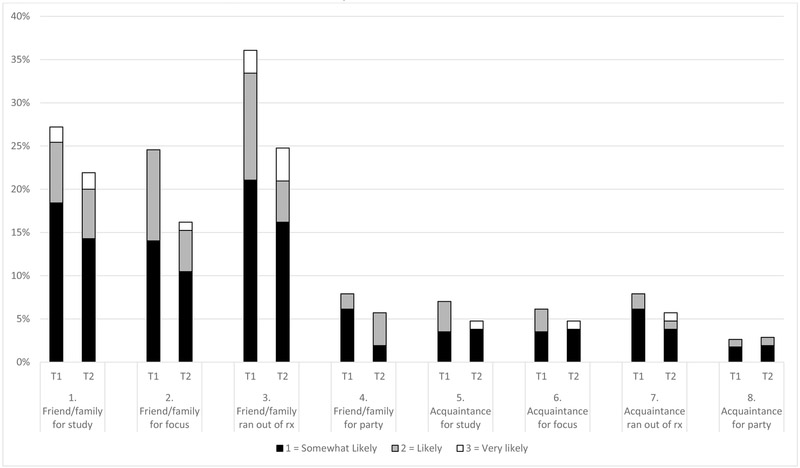
Intent to divert decreased significantly over time. The mean number of situations in which a patient would divert dropped to 0.89 from 1.20. Although most endorsed being “not at all likely” to divert across all situations, intent was more likely in situations involving a friend or family member needing the medication for reasons other than recreational use. Figure 2 displays these results by situation at Times 1 and 2. At Time 2, the circumstances that produced the greatest reported likelihood of diversion were to friends or family for studying (22%, down from 27% at Time 1) or to replenish an existing prescription (25%, down from 33% at Time 1). Very few patients (1%-6%) reported any likelihood, pre- or post-training, of diverting their medication to acquaintances or strangers for any reason.
Figure 2. Likelihood of Diversion in Specific Situations by Time.
Note: T1 = Time 1 survey, n = 114; T2 = Time 2 survey, n = 105. Responses were rated on a 4-point scale ranging from 0 = Not at all likely to 3 = Very likely; 0 = Not at all likely not shown in figure for clarity. Although analyzed as a count of situations that the participant indicated any likelihood of diverting (score of 1 or higher), the full range of responses in the affirmative is displayed here for descriptive purposes.
The number of non-family, non-romantic partner social network types who knew about the patients’ stimulant medication decreased significantly, from mean of 2.77 to 1.99. Table 2 shows that the number of roommates, friends, and coworkers or acquaintances who knew were significantly lower at Time 2, and the odds of these social network types knowing about the patient’s stimulant medication usage were halved by Time 2.
No other diversion risk factors changed significantly. Most patients reported 0-25% chance of getting in trouble for diverting their stimulant medication (perceived harm to self). Perceived harm to others was very stable and perceived as greatest for regular use of stimulants without a prescription. For example, at Time 1, 79.8% (91/114) of patients perceived “moderate risk” (response=3) or “great risk” (response=4) for individuals taking stimulants without a prescription “regularly” versus 21.9% (25/114) perceiving moderate or great risk associated with taking stimulants without a prescription “once or twice.” Knowledge of school policies pertaining to stimulant misuse was low. For stimulant storage, a substantial minority reported keeping their medications in locations accessible to others (under 30% at both times), and few (12% at both times) reported locked storage of their stimulant medication.
At Time 2, 21% (22/105) reported having changed how they store their medication. Post-hoc exploration of reported storage locations revealed an increase from Time 1 to Time 2 in purse/backpack storage (see Supplement 2).
Satisfaction and feasibility
Table 3 shows that provider and staff ratings of satisfaction collected immediately following training were generally high. Providers and staff indicated a “moderate” perceived need for additional training to feel comfortable using the diversion risk skills and strategies.
Table 3.
Provider and staff satisfaction at the conclusion of the workshop
| 1 = Very Low | 2 = Low | 3 = Moderate | 4 = High | 5 = Very High | Mean | SD | |
|---|---|---|---|---|---|---|---|
| Prescribers (n = 55) | |||||||
| 1. Satisfied with overall quality of educational activity | 0% | 0% | 5.5% | 36.4% | 58.2% | 4.53 | 0.60 |
| 2. Content of program was relevant to practice | 0% | 0% | 22.0% | 30.9% | 47.3% | 4.25 | 0.80 |
| 3. Program enhanced your knowledge | 0% | 3.6% | 9.1% | 45.5% | 41.8% | 4.25 | 0.78 |
| 4. As a result of participation, feel equipped to implement the strategies | 0% | 0% | 16.4% | 43.6% | 40.0% | 4.24 | 0.72 |
| 5. Time allotted for training was sufficient | 0% | 0% | 21.8% | 43.6% | 34.6% | 4.13 | 0.75 |
| 6. Feel that you need additional training to feel comfortable using the strategies | 9.1% | 36.4% | 23.6% | 20.0% | 10.9% | 2.87 | 1.17 |
| 7. Content of training was useful to you | 0% | 3.6% | 12.7% | 36.4% | 47.3% | 4.27 | 0.83 |
| All others (n = 75) | |||||||
| 1. Satisfied with overall quality of educational activity | 0% | 0% | 10.7% | 44.0% | 45.3% | 4.35 | 0.67 |
| 2. Content of program was relevant to practice | 0% | 0% | 14.7% | 44.0% | 42.7% | 4.27 | 0.70 |
| 3. Program enhanced your knowledge | 0% | 0% | 16.0% | 46.7% | 37.3% | 4.21 | 0.70 |
| 4. As a result of participation, feel equipped to implement the strategies | 0% | 0% | 28.0% | 45.3% | 26.7% | 3.97 | 0.74 |
| 5. Time allotted for training was sufficient | 0% | 0% | 20.0% | 53.3% | 26.7% | 4.07 | 0.68 |
| 6. Feel that you need additional training to feel comfortable using the strategies | 16.0% | 30.7% | 17.3% | 24.0% | 12.0% | 2.85 | 1.29 |
| 7. Content of training was useful to you | 0% | 6.7% | 10.7% | 48.0% | 34.7% | 4.11 | 0.85 |
Note: Ratings provided by 130 workshop attendees (124 in-person and 6 prescribers online due to schedule incompatibility); 43/55 prescribers (78%) held M.D. or D.O. degrees; the remaining were nurse practitioners (10) or physician assistants (2); 50/75 staff (66%) held MSN, BSN, CMA, LPN, RN, or MA degrees; the remaining were other office staff.
Discussion
This study provides new data pertinent to the prevention of stimulant misuse by college students being treated for ADHD. Brief clinical practice strategies for use in primary care, to aide in the prevention of stimulant medication diversion by college student patients, were developed and delivered in educational workshops to primary care providers and their practice staff in an open, uncontrolled clinical trial. Patients treated across primary care practices reported low rates of stimulant diversion, but patient diversion risk decreased after training. An absence of practice effects suggests that results generalize to pediatric and family medicine settings. These findings provide preliminary evidence for the ability of pediatric and family medicine PCPs to lower stimulant diversion risk and thereby decrease the supply of medicine that supports non-prescribed stimulant use by college students.
Less than 20% of patients reported diverting their stimulants. This low base rate made postintervention change difficult to detect and interesting relative to higher rates reported elsewhere 8-10,12,13,31 Population sampling differences may be contributing. Wilens and colleagues found that only 11% of their still stimulant-medicated participants followed from childhood were selling their medication.32 Individuals with long histories of treatment and strong relationships with providers may be less likely to divert. In contrast to existing surveys of college students, about a quarter of our patients were in community college which may lower diversion risk (e.g., little time spent on campus outside of classes33). Diversion of stimulant medication did not increase over time, suggesting that patient/provider discussions about the problem of stimulant misuse and diversion did not have iatrogenic effects.
The diversion prevention training presented our Time 1 finding that many patients were approached to divert. Other studies have reported this9,13,34,35 which makes the possibility of this social vulnerability especially important as a diversion risk factor. After PCP training, the number of times that patients were approached was cut in half, from an average of 10.57 to 4.47 times. The variability of this important outcome was also reduced; fewer patients were approached 4 or more times (38.6% pre, and 23.8% post). Being approached to divert has been a key factor in the literature on stimulant misuse because most college students who misuse stimulants obtain them from a peer with a prescription.8,9 Our PCP training emphasized vulnerability to approach based on their patients’ baseline data (aggregated across sites), making the data directly applicable. We also shared the well-documented tendency for individuals with ADHD to have interpersonal difficulties which may increase diversion vulnerability.36-38 If our rates of actual diversion are under-estimates, which is possible when measuring any socially undesirable behavior, then the reduction in approaches to divert is especially promising as a prevention target.
We found a reduction in the number of social network types who knew about the patients’ stimulant prescriptions. The findings are encouraging, although we can only infer that this change is in response to reduced patient disclosure. In the PCP training, providers were coached to encourage their patients to disclose information about their treatment selectively. Our findings suggest that a fairly simple conversation, delivered briefly yet effectively (we encouraged and demonstrated motivational enhancement-style interactions39,40), may have important effects on patient behavior.
Behavioral intentions have repeatedly been shown to be the strongest proximal predictor of adolescent health risk behavior.41,42 We found a statistically significant reduction in intentions to divert stimulant medication which signified, despite low rates of diversion, room for improvement in a salient risk factor. When we examined the individual items assessing intentions, decreased likelihood of diverting to friends or family members was primarily responsible for the change.
Although modest, these pre-post changes in diversion risk are promising. Future tests of mediating variables, such as patient-reported change in provider behavior, may be illuminating and increase confidence in our training as a method of diversion prevention. We are unable to know with certainty the extent to which providers and additional practice staff adopted the strategies, because direct observations were impractical (strategy implementation was expected across providers and practice staff, across different kinds of interactions). Our finding that 75% of the patients had ADHD-related contact with their practice between workshop delivery and Time 2 hints at the possibility that diversion risk might have improved more with greater contact. Importantly, the uncontrolled nature of our pre-post study design leaves open the possibility that other, unmeasured, factors may account for the reduction in diversion risk. For example, increased media reports of the dangers of stimulant misuse, although not changing perceived harm per se, may have been responsible for changing intentions. Cognitive maturation typical of this age43,44 that may occur for some with ADHD alongside decreasing symptoms of ADHD45 may also underlie our pre-post changes. A randomized controlled trial is necessary to more definitely conclude that the training was responsible for the reduction in diversion risk.
The remaining diversion risk variables did not change. At Time 2, about one-quarter (26.3%) reported a greater than 50% chance of getting in trouble if they were caught diverting. Our intervention did not specifically address this perception but rather emphasized the range of negative consequences that might follow from diversion (including those associated with being caught). It is somewhat surprising that perceived harm did not increase given the changes we observed in approaches and intent to divert. This may be due to patients already having reasonable expectations of risk. For example, knowledge of school policies stayed low, but our own online research of local colleges and universities suggested lack of policies specifically related to stimulants. Patients may also perceive little reason to investigate this information in the absence of diversion. Regarding secure storage of medication, most patients stored their medication in non-shared locations but not under lock and key. We speculate that preference for easy access to medication often taken at times of greatest need (e.g., while attending class or completing homework) may take precedence; the post-hoc finding that purse/backpack storage increased by Time 2 aligns with this notion.
Our provider and staff training session was very brief yet ratings of satisfaction, relevance, and feasibility were generally high. About one-third of providers and staff indicated a need for additional training; planned analyses of provider-reported strategy implementation and associated factors such as skill self-efficacy and perceived knowledge about ADHD medication prescribing should pinpoint areas for additional training in the future. Other ratings were high, and characteristics of our training preparation and delivery may have contributed (e.g., incorporating feedback from consultants including PCPs, using study data to increase relevance, on-site training with continuing education and meals). The generally high ratings should aide dissemination in the future.46
Conclusions
The findings of this study are encouraging and suggest that a brief PCP training package is feasible, well-received by providers and staff, and may lead to reduced stimulant diversion risk among college students. Importantly, our findings also suggest the absence of iatrogenic effects (e.g., increased diversion). Finally, our results revealed no practice effects which suggests that these strategies may be effective in pediatric and family medicine settings. The pre-post design of this study without a comparison group makes it difficult to know whether the findings reflect natural trends over time for college students versus the effects of our training program. A randomized controlled trial is needed to address this question. It is also helpful to recognize the developmental nature of the assessment battery and limited racial and ethnicity diversity of the sample. The training to reduce diversion risk described herein reflects only one facet of a multipronged approach needed to reduce stimulant misuse. In addition to equipping providers and their staff with knowledge and skills, research is needed on the efficacy of targeting college students directly, working with dispensing pharmacies and student health centers, and targeting misuse at even younger ages.
Supplementary Material
What’s New? This study provides initial evidence of reduction in stimulant diversion risk by college student patients with ADHD after their primary care providers participated in a new one hour educational workshop on prevention of diversion.
Acknowledgements:
Appreciation is extended to the following consultants who provided their expertise during the conduct of this study: Scott Tyson, MD, FAAP, CEO Pediatrics South; John Lagnese, MD, President, Renaissance Family Practice; Oscar Bukstein, MD, MPH, Boston Children’s Hospital, Associate Psychiatrist-in-Chief, Vice Chair of Psychiatry; Director (Interim), Child & Adolescent Psychiatry Fellowship; Professor of Psychiatry, Harvard Medical School; Bryan Weiner, PhD, Professor of Global Health and Health Services, University of Washington; Evelyn Reis, MD, Director of Pediatric PittNet and Professor of Pediatrics, University of Pittsburgh School of Medicine, and the staff of the ADHD Across the Lifespan Clinic at Western Psychiatric Institute and Clinic of UPMC.
Funding Sources: Funding was provided by DA035464. Additional support was provided by DA040213, MH018951, HRSA NRSA for Primary Medical Care T32HP22240. Pediatric PittNet is funded by the Clinical and Translational Science Institute at the University of Pittsburgh which is supported by UL1 TR001857.
Abbreviations.
- PCPs
primary care providers
- ADHD
Attention-Deficit/Hyperactivity Disorder
- EMR
Electronic Medical Records
- GEE
Generalized Estimating Equations
Footnotes
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fredriksen M, Halmøy A, Faraone SV, Haavik J. Long-term efficacy and safety of treatment with stimulants and atomoxetine in adult ADHD: a review of controlled and naturalistic studies. Eur Neuropsychopharmacol. 2013;23(6):508–527. [DOI] [PubMed] [Google Scholar]
- 2.Faraone SV, Buitelaar J. Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur Child Adolesc Psychiatry. 2010;19(4):353–364. [DOI] [PubMed] [Google Scholar]
- 3.Molina BSG, Howard AL, Swanson JM, et al. Substance use through adolescence into early adulthood after childhood-diagnosed ADHD: findings from the MTA longitudinal study. Journal of child psychology and psychiatry, and allied disciplines. 2018;59(6):692–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. [DOI] [PubMed] [Google Scholar]
- 5.McCabe SE, West BT, Teter CJ, Boyd CJ. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict Behav. 2014;39(7):1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. In: HHS Publication No. (SMA) 13-4760, ed. Rockville, MD: 2013. [PubMed] [Google Scholar]
- 7.Arria AM, DuPont RL. Nonmedical prescription stimulant use among college students: why we need to do something and what we need to do. J Addict Dis. 2010;29(4):417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeSantis AD, Anthony KE, Cohen EL. Illegal college ADHD stimulant distributors: Characteristics and potential areas of intervention. Subst Use Misuse. 2013;48(6):446–456. [DOI] [PubMed] [Google Scholar]
- 9.Gallucci AR, Martin RJ, Usdan SL. The diversion of stimulant medications among a convenience sample of college students with current prescriptions. Psychol Addict Behav. 2015;29(1):154. [DOI] [PubMed] [Google Scholar]
- 10.Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375. [DOI] [PubMed] [Google Scholar]
- 11.Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgraduate medicine. 2014;126(5):64–81. [DOI] [PubMed] [Google Scholar]
- 12.Sepulveda DR, Thomas LM, McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. Journal of pharmacy practice. 2011;24(6):551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144–153. [DOI] [PubMed] [Google Scholar]
- 14.Gallucci AR, Martin RJ, Usdan SL. The diversion of stimulant medications among a convenience sample of college students with current prescriptions. Psychology of Addictive Behaviors. 2015;29(1):154–161. [DOI] [PubMed] [Google Scholar]
- 15.DeSantis AD, Anthony KE, Cohen EL. Illegal college ADHD stimulant distributors: characteristics and potential areas of intervention. Subst Use Misuse. 2013;48(6):446–456. [DOI] [PubMed] [Google Scholar]
- 16.Wilens MDT, Gignac M, Swezey A, Monuteaux M, Biederman J. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(4):408–414. [DOI] [PubMed] [Google Scholar]
- 17.Lasopa SO, Striley CW, Cottler LB. Diversion of prescription stimulant drugs among 10-18-year-olds. Current opinion in psychiatry. 2015;28(4):292–298. [DOI] [PubMed] [Google Scholar]
- 18.McCabe SE, West BT, Teter CJ, Ross-Durow P, Young A, Boyd CJ. Characteristics associated with the diversion of controlled medications among adolescents. Drug Alcohol Depend. 2011;118(2-3):452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaner EF, Beyer FR, Muirhead C, et al. Effectiveness of brief alcohol interventions in primary care populations. The Cochrane database of systematic reviews. 2018;2:Cd004148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozer EM, Adams SH, Orrell-Valente JK, et al. Does delivering preventive services in primary care reduce adolescent risky behavior? The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2011;49(5):476–482. [DOI] [PubMed] [Google Scholar]
- 21.Kalu N, Cain G, McLaurin-Jones T, et al. Impact of a multicomponent screening, brief intervention, and referral to treatment (SBIRT) training curriculum on a medical residency program. Subst Abus. 2016;37(1):242–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921. [DOI] [PubMed] [Google Scholar]
- 23.Anderson LE, Chen ML, Perrin JM, Van Cleave J. Outpatient visits and medication prescribing for US children with mental health conditions. Pediatrics. 2015;136(5):e1178–e1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benson K, Flory K, Humphreys KL, Lee SS. Misuse of Stimulant Medication Among College Students: A Comprehensive Review and Meta-analysis. Clinical Child and Family Psychology Review. 2015;18(1):50–76. [DOI] [PubMed] [Google Scholar]
- 25.Jardin B, Looby A, Earleywine M. Characteristics of college students with attention-deficit hyperactivity disorder symptoms who misuse their medications. Journal of American college health : J of ACH. 2011;59(5):373–377. [DOI] [PubMed] [Google Scholar]
- 26.Choukas-Bradley S, Giletta M, Cohen GL, Prinstein MJ. Peer influence, peer status, and prosocial behavior: An experimental investigation of peer socialization of adolescents' intentions to volunteer. Journal of Youth & Adolescence. 2015;44:2197–2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnston LD, OMP, Bachman JG, Schulenberg JE,. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2012. Ann Arbor: Institute for Social Research, University of Michigan; 2013. [Google Scholar]
- 28.Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain medicine. 2007;8(7):573–584. [DOI] [PubMed] [Google Scholar]
- 29.Chou R, Fanciullo GJ, Fine PG, et al. Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic Noncancer Pain. The Journal of Pain. 2009;10(2):113–130.e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ozer EM, Adams SH, Lustig JL, et al. Increasing the screening and counseling of adolescents for risky health behaviors: a primary care intervention. Pediatrics. 2005;115(4):960–968. [DOI] [PubMed] [Google Scholar]
- 31.Garnier LM, Arria AM, Caldeira KM, Vincent KB, O'Grady KE, Wish ED. Sharing and selling of prescription medications in a college student sample. Journal of Clinical Psychiatry. 2010;71(3):262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilens TE, Gignac M, Swezey A, Monutaux MC, Biederman J. Characteristics of Adolescents and Young Adults With ADHD Who Divert or Misuse Their Prescribed Medications. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(4):408–414. [DOI] [PubMed] [Google Scholar]
- 33.Ryan BE. Alcohol and Other Drugs: Prevention Challenges at Community Colleges. In. Newton, MA: The Higher Education Center for Alcohol and Other Drug Prevention; 1998. [Google Scholar]
- 34.Schultz NR, Silvestri MM, Correia CJ. Diversion of prescription stimulants among college students: An initial investigation of injunctive norms. Addict Behav. 2017;65:264–268. [DOI] [PubMed] [Google Scholar]
- 35.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. J Am Coll Health. 2006;54(5):269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaw-Zirt B, Popali-Lehane L, Chaplin W, Bergman A. Adjustment, social skills, and self-esteem in college students with symptoms of ADHD. Journal of Attention Disorders. 2005;8(3):109–120. [DOI] [PubMed] [Google Scholar]
- 37.Weyandt LL, DuPaul G. ADHD in college students. Journal of Attention Disorders. 2006;10(1):9–19. [DOI] [PubMed] [Google Scholar]
- 38.Bagwell CL, Molina BS, Pelham WE, Hoza B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1285–1292. [DOI] [PubMed] [Google Scholar]
- 39.Arkowitz H, Miller WR, Rollnick S. Motivational interviewing in the treatment of psychological problems. Guilford Publications; 2015. [Google Scholar]
- 40.Rollnick S, Miller WR, Butler CC, Aloia MS. Motivational interviewing in health care: helping patients change behavior. In: Taylor & Francis; 2008. [Google Scholar]
- 41.Malmberg M, Kleinjan M, Vermulst AA, et al. Do substance use risk personality dimensions predict the onset of substance use in early adolescence? A variable-and person-centered approach. J Youth Adolesc. 2012;41(11):1512–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stephens PC, Sloboda Z, Stephens RC, et al. Universal school-based substance abuse prevention programs: Modeling targeted mediators and outcomes for adolescent cigarette, alcohol and marijuana use. Drug Alcohol Depend. 2009;102(1):19–29. [DOI] [PubMed] [Google Scholar]
- 43.Jernigan TL, Brown TT, Bartsch H, Dale AM. Toward an integrative science of the developing human mind and brain: Focus on the developing cortex. Developmental cognitive neuroscience. 2016;18:2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blakemore S-J, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. Journal of Child Psychology and Psychiatry. 2006;47(3-4):296–312. [DOI] [PubMed] [Google Scholar]
- 45.Sudre G, Szekely E, Sharp W, Kasparek S, Shaw P. Multimodal mapping of the brain's functional connectivity and the adult outcome of attention deficit hyperactivity disorder. Proceedings of the National Academy of Sciences of the United States of America. 2017;114(44):11787–11792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: The interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3-4):171–181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.