Abstract
Objective:
To examine predictors associated with quality of life (QoL) in Brazilian medical students.
Methods:
PubMed, PsycINFO, EMBASE, LILACS, and Google Scholar were searched for research articles in English or Portuguese published through August 2018. Observational studies that measured QoL with standard instruments were selected. Three instruments were used to evaluate QoL: the World Health Organization QoL questionnaires (WHOQOL-Bref and WHOQOL-100) and 36-item Short Form Health Survey (SF-36). Hedges’ g was used to calculate effect sizes. A random-effects model was used in meta-analyses. PRISMA guidelines were followed.
Results:
The initial search retrieved 8,504 articles; 24 met the eligibility criteria for systematic review, and seven for meta-analyses of gender (n=3,402 students). Predictors of QoL such as gender, years of medical school(years of study), economic class, educational environment, academic efficacy, depression, burnout, resilience, empathic concern, sleep difficulties, chronic illness, body mass index, and leisure-time physical activity were identified in the systematic review. The most frequent predictors of QoL detected in Brazilian medical students were associated with gender and years of study.
Conclusions:
Female medical students had lower QoL scores in the physical health and psychological domains of WHOQOL-Bref compared to male students. Specific interventions should be designed for this group as appropriate.
Systematic review registry number:
PROSPERO CRD-42018102259.
Keywords: Quality of life, medical students, meta-analysis, systematic review, Brazilian
Introduction
Medical students face many stress factors compared to the general population. A recent study conducted in the United States noted that medical students, residents/fellows, and early-career physicians were more likely to experience burnout than a control sample.1 New Zealander, Brazilian, and Italian medical students also exhibited lower quality of life (QoL) scores than reference or general population groups.2-4
Although these findings appear to be consistent across different cultures, major differences have also been reported. Depression and stress were more frequently detected among Brazilian medical students than U.S. students.5 Additionally, U.S. medical students reported greater wellness and environmental QoL.5 Medical male students in Jimma (Ethiopia) were more empathetic than their counterparts in Munich (Germany), a finding that was significantly associated with religious activity in the community.6 It is well recognized that the personal beliefs, value systems, environment, socioeconomic background, and prevalence of mental disorders may explain these conflicting results between countries. As a consequence, what is significant in one culture or country may not be in another.
Interestingly, one of the first Brazilian groups to provide support to medical students observed that most students requested help due to depressive disorders, followed by a decrease in leisure time and relationship with old friends, less availability to their significant other, and the end of idealized notions about medical school. Psychosis and drug addiction were occasional.7 Presently, the prevalence of depression among Brazilian medical students is estimated at 30.6%, burnout at 13.1%, problematic alcohol use at 32.9%, and anxiety at 32.9%; academic overload correlated with these disorders.8 These rates are higher if compared to those of adults living in the city of São Paulo (any mood disorder, 11%; alcohol abuse disorders, 2.7%; any anxiety disorder, 19.9%) or among college students worldwide (anxiety disorders, 11.7-14.7%; mood disorders, 6.0-9.9%; substance disorders, 4.5-6.7%; behavioral disorders, 2.8-5.3%).9,10
Brazil has about 300 medical schools. Data from Brazilian medical demographics projected that, by 2020, approximately 32,400 new physicians will have been added the Brazilian health workforce – 11,677 new physicians compared to 2014.11 Furthermore, the growing proportion of women among medical graduates and an increase in the number of physicians per population have been noted.11
Measurement of QoL is a comprehensive evaluation of health in the context of an individual’s perception of well-being. It is a broader evaluation compared to the detection of a specific condition, disease, or disorder in a target population. Global health is evaluated according to specific domains, such as physical and psychological health, social relationships, environment, mental health, financial resources, and bodily pain, depending on the instrument used for evaluation. Additionally, the measurement of QoL provides a wide overview of the nature of diseases to which subjects are exposed. Considering that the quality of medical care is a critical component of the private and public healthcare systems, this systematic review was designed to identify predictors associated with QoL in Brazilian medical students. We believe this information will help manage academic performance and will provide support for affirmative action.12
Material and methods
The present systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13
Eligibility criteria
We included observational studies that measured QoL in Brazilian medical students with standard instruments: the World Health Organization Quality of Life instrument (WHOQOL-100), its abbreviated 26-question version (WHOQOL-Bref), and the 36-item Short-Form Health Survey questionnaire (SF-36). Additionally, studies were required to have evaluated factors associated with QoL in statistical analyses.
Studies with no measure of QoL, those designed to evaluate the frequency of mental disorders, quality of sleep, headache, or cross-cultural differences among medical students, and those with a sample composed of residents were excluded.
Information sources
PubMed, PsycINFO, EMBASE, LILACS, and Google Scholar were searched for research articles in English or Portuguese through August 2018, with no restriction on year of publication. The search terms were “QoL AND medical student OR medical students AND Brazil”. No efforts were made to contact the authors.
Data collection process and items of interest
We extracted the following data: setting, number of participants, frequency of females, age, study design, recruitment period, instruments, QoL scores, and positive and negative predictors associated with QoL (Tables 1 and 2). Table 3 shows the summary of predictors identified in the systematic review. One reviewer conducted the full abstraction of all data (ACS), and two reviewers (ACS and FLN) verified their accuracy. Consensus-based discussion was used to decide about the inclusion of primary studies.
Table 1. Characteristics of studies conducted in a specific Brazilian region.
| Author (city) | n (% of women) | Age | University | Design (recruitment period) | Instruments | WHOQOL/SF-36 (scores) | Positive predictors | Negative predictors |
|---|---|---|---|---|---|---|---|---|
| Paro12
(Uberlândia) |
390 (61.3) | 19.1 (n=38) 22.3 (n=352) |
Universidade Federal de Uberlândia (UFU) (public) |
Cross-sectional (Feb 2006 and Feb 2007) | SF-36 BDI |
SF-36 (the mean score for each SF-36 domain of the entire population was not reported) |
Depressive symptoms (BDI ≥ 9) Female Third year of study |
|
| Alves14
(Recife) |
370 (57.02) | Not reported | Universidade Federal de Pernambuco (UFPE) (public) Universidade de Pernambuco (UPE) (public) Escola Pernambucana de Medicina (EPM) (private) |
Cross-sectional (Aug 2006-Apr 2007) | WHOQOL-Bref | WHOQOL-Bref (the mean score for each domain of the entire population was not reported) |
Sixth year of study | |
| Ramos-Dias15
(Sorocaba) |
100 (51.0) | 20.5 (first year of study) 24.4 (sixth year of study) |
Pontifícia Universidade Católica de Sorocaba (PUC-SP) (private) |
Cross-sectional (not reported) | WHOQOL-Bref CAGE questionnaire |
WHOQOL-Bref (the mean score for each domain of the entire population was not reported) |
First year of study | |
| Meyer16
(state of Santa Catarina) |
302 (55.6) | 25.3 (mean) | Universidade Federal de Santa Catarina (UFSC) (public) and 10 private universities*
(public/private) |
Cross-sectional (Jun 2011-Sep 2011) | WHOQOL-Bref Job Stress Scale |
WHOQOL-Bref Physical = 73.0 Psychological = 73.1 Social relationship = 79.3 Environment = 76.8 |
Undetected | Undetected |
| Olmo17
(Santos) |
94 (62.76) | 17-30 (years) | Universidade Metropolitana de Santos (UNIMES) (private) |
Cross-sectional (May 2011) | WHOQOL-Bref | WHOQOL-Bref (the mean score for each domain of the entire population was not reported) |
Sixth year of study | |
| Paro18
(Campinas) |
309 (not reported) | Not reported | Universidade de Campinas (UNICAMP) (public) |
Cross-sectional (not reported) | SF-36 | SF-36 Physical functioning = 91.1 Role physical = 63.0 Bodily pain = 70.6 General health = 68.0 Vitality = 43.4 Social functioning = 64.7 Role emotional = 50.1 Mental health = 61.1 |
Later years of study | |
| Chazan19
Chazan20 (Rio de Janeiro) |
394 (61.0) | 23 (mean) | Universidade do Estado do Rio de Janeiro (UERJ) (public) |
Cross-sectional (Apr 2010-May 2010) | WHOQOL-Bref Reported chronic morbidity |
WHOQOL-Bref Physical = 66.0 Psychological = 63.5 Social relationship = 68.9 Environment = 58.0 |
Economic class C Quota students† Chronic illness Female gender Third and sixth years of study |
|
| Hickel21
(Pelotas) |
298 (58.1) | 22 (mean) | Universidade Federal de Pelotas (UFPel) (public) |
Cross-sectional (Dec 2012-Mar 2013) | WHOQOL-Bref | WHOQOL-Bref Physical = 67.0 Psychological = 65.0 Social relationship = 71.0 Environment = 67.0 |
Distance from hometown | |
| Pagnin & Queirós2
(Niterói) |
206 (55.8) (students) |
Not reported | Universidade Federal Fluminense (UFF) (public) |
Cross-sectional (not reported) | WHOQOL-Bref | WHOQOL-Bref Physical = 60.26 Psychological = 60.98 Social relationship = 67.48 Environment = 58.78 |
Female gender | |
| Pagnin & Queirós22
(Niterói) |
193 (53.9) (second-year medical students) |
21.42 (mean) | Universidade Federal Fluminense (UFF) (public) |
Cross-sectional (not reported) | WHOQOL-Bref MBI-SSMSQSRRSBDI |
WHOQOL-Bref Physical = 59.55 Psychological = 62.36 Social relationship = 66.97 Environment = 61.97 |
Sense of academic efficacy/accomplishment | Burnout Sleep problems Cynicism Depressive symptoms |
| Lins23
Lins24 (Salvador) |
180 (58.33) | 17-33 (years) | Escola Bahiana de Medicina e Saúde Pública (private) |
Cross-sectional (Oct 2013-Nov 2013) | SF-36 ESS |
SF-36 Physical functioning = 51.5 Role physical = 44.9 Bodily pain = 50.2 General health = 46.2 Vitality = 46.7 Social functioning = 42.7 Role emotional = 41.6 Mental health = 45.9 |
Male students not supported by FIES | Students supported by the loan program (FIES), especially in the sixth year of school Female students supported by FIES Lack of physical activity Headache Sleepiness |
| Legey25
(Rio de Janeiro) |
140 (46.42) | 23.6 (mean) | Universidade Veiga de Almeida (UVA) (private) |
Cross-sectional (not reported) | SF-36 STAI Silhouette Scale POMS |
SF-36 Not reported |
Body image satisfaction | |
| Cunha26
(São Paulo) |
607 (42.6) | 22.9 (mean) | Universidade Federal de São Paulo (UNIFESP) (public) |
Cross-sectional (Aug 2011-Dec 2011) | WHOQOL-100 | WHOQOL-100 Physical health = 64.7 Psychological = 70.1 Level of independence = 79 Social relationship = 77.3 Environment = 70.5 Spirituality = 72.3 |
Sixth year of study Economic class C/D Female gender |
|
| Serinolli & Novaretti27
(São Paulo) |
405 (56.3) | 23.55 (mean) | Universidade Nove de Julho (UNINOVE) (private) |
Cross-sectional (Oct 2014-Nov 2014) | WHOQOL-Bref | WHOQOL-Bref‡
Physical = 63.67 Psychological = 65.11 Social relationship = 70.97 Environment = 59.01 |
Religious beliefs Male gender At least one physician parent |
Body mass index Daily commute time |
| Pereira28
Ribeiro29 (Patos) |
138 (58.7) | 18-24 (years) | Faculdades Integradas de Patos (FIP) (private) |
Cross-sectional (2016-2017) | WHOQOL-Bref MBI-SSISSLBDI |
WHOQOL-Bref Physical = 62.42 Psychological = 65.36 Social relationship = 69.92 Environment = 62.36 |
Satisfaction with course contentment Psychological treatment |
Depression Burnout Stress |
| Santos30
(Jequié) |
115 (46.9) | 24.7 (mean) | Universidade Estadual do Sudoeste da Bahia (UESB) (private) |
Cross-sectional (2016) | WHOQOL-Bref SRQ-20 |
WHOQOL-Bref Physical = 62.42 Psychological = 65.36 Social relationship = 69.92 Environment = 62.36 |
Psychiatric symptoms (SRQ-20 > 6) |
BDI = Beck Depression Inventory; CAGE = cut-annoyed-guilty-eye questionnaire; ESS = Epworth Sleepiness Scale; FIES = Fundo de Financiamento ao Estudante do Ensino Superior; MBI-SS = Maslach Burnout Inventory – Student Survey; MSQ = Mini-Sleep Questionnaire; POMS = Profile of Mood States Scale; RCM = referred chronic morbidity; SF-36 = 36-item Short Form Health Survey questionnaire; SRQ-20 = Self Report Screening Questionnaire-20; SRRS = Social Readjustment Rating Scale; STAI = State-trait anxiety inventory; WHOQOL-100 = World Health Organization Quality of Life instrument; WHOQOL-Bref = World Health Organization Quality of Life instrument-Abbreviated version.
Private universities: Universidade do Sul de Santa Catarina (UNISUL) (Pedra Branca – Palhoça and Tubarão campuses), Universidade do Oeste de Santa Catarina (UNOESC), Universidade do Vale do Itajaí (UNIVALI), Universidade da Região de Joinville (UNIVILLE), Universidade do Planalto Catarinense (UNIPLAC), Universidade Comunitária da Região de Chapecó (UNOCHAPECÓ), Universidade do Extremo Sul Catarinense (UNESC).
At the time of the study, 45% of places for incoming students at UERJ were set aside for the admission of socially disadvantaged students. More information on this quota policy is available elsewhere.19
Data extracted from the supplemental material.
Table 2. Results of a multicenter study conducted in 22 Brazilian universities.
| Author | n (%) | Age (mean) | University | Design (recruitment period) | Instruments | WHOQOL/SF-36 (scores) | Positive predictors | Negative predictors |
|---|---|---|---|---|---|---|---|---|
| Paro31 | 1,350 (52.9) | 22.76 | Brazilian medical schools (n=22) (public and private) |
Cross-sectional, multicenter (Aug 2011-Aug 2012) | WHOQOL-Bref MBI-HSSIRI |
WHOQOL-Bref
Physical = 65.2* Psychological = 61.7* Social relationship = 63.6* Environment = 63.8* |
Personal accomplishment Perspective taking Empathic concern (females) |
Emotional exhaustion Depersonalization Personal distress |
| Tempski32 | 1,350 (52.9) | 22.8 | Brazilian medical schools (n=22) (public and private) |
Cross-sectional, multicenter (Aug 2011-Aug 2012) | WHOQOL-Bref QoL self-assessment QoL related to medical school (MSQoL) DREEM RS-14 BDI STAI |
WHOQOL-Bref
Physical = 65.2 Psychological = 61.7 Social relationship = 63.6 Environment = 63.8 |
Resilience | |
| Enns33 | 1,350 (52.9) | 22.8 | Brazilian medical schools (n=22) (public and private) |
Cross-sectional, multicenter (Aug 2011-Aug 2012) | WHOQOL-Bref DREEM QoL self-assessment QoL related to medical school (MSQoL) |
WHOQOL-Bref
Physical = 65.2 Psychological = 61.7 Social relationship = 63.6 Environment = 63.8 |
Positive perception of educational environment | |
| Peleias34 | 1,350 (52.9) | 22.8 | Brazilian medical schools (n=22) (public and private) |
Cross-sectional, multicenter (Aug 2011-Aug 2012) | WHOQOL-Bref QoL self-assessment QoL related to medical school (MSQoL) Leisure time physical activity evaluation VERAS-Q questionnaire |
WHOQOL-Bref
Physical = 65.2* Psychological = 61.7* Social relationship = 63.6* Environment = 63.8* |
Leisure time physical activity |
BDI = Beck Depression Inventory; DREEM = Dundee Ready Education Environment Measure; IRI = Interpersonal Reactivity Index; MBI-HSS = Maslach Burnout Inventory-Human Services Survey; RS-14 = Wagnild and Young’s Resilience Scale; SF-36 = 36-item Short Form Health Survey questionnaire; STAI = State-Trait Anxiety Inventory; VERAS-Q = a questionnaire created to evaluate the QoL of students in the health professions; WHOQOL-Bref = World Health Organization Quality of Life instrument-Abbreviated version.
Data extracted from Enns et al.33
Table 3. Summary of the main positive and negative predictors of quality of life according to demographic, academic, psychological, and physiological factors.
| Category | Positive predictors | Negative predictors |
|---|---|---|
| Demographic | Male gender | Female gender Economic class C/D Quota students* Student loans (FIES) Distance from home town/daily commute time |
| Academic | Positive perception of educational environment Sense of academic efficacy Accomplishment |
Third and sixth years of study |
| Psychological | Resilience Personal accomplishment Perspective taking Empathic concern (females) |
Depressive symptoms Burnout Cynicism Emotional exhaustion Depersonalization Personal distress Psychiatric symptoms |
| Physiological | Leisure-time physical activity Body image satisfaction |
Chronic illness Body mass index Sleep problems Headache |
FIES = Fundo de Financiamento ao Estudante do Ensino Superior.
At the time of the study, 45% of places for incoming students at UERJ were set aside for the admission of socially disadvantaged students. More information on this quota policy is available elsewhere.19
Data analysis, summary measures, and synthesis of results
Data were stored in Microsoft Excel and evaluated using Comprehensive Meta-Analysis version 3 software (Biostat, Englewood, U.S.). Hedges’ g was used to calculate the effect sizes of the four WHOQOL-Bref/WHOQOL-100 domains (physical, psychological, social relationship, and environment). Pooled effect sizes were calculated using the random effects model. The I 2 statistic was used to measure heterogeneity. Visual inspection of the funnel plot was used to estimate the publication bias.
Statistical power calculation
The power calculation was done to detect a summary effect size of g = 0.30 in the psychological domain of WHOQOL-Bref, since mental disorders are frequently studied among Brazilian medical students.08 We estimated a low level of between-study variance based on previous studies,2,26,31 a statistical power of 0.80, and an alpha value of 0.05. The power of the test of the main effect of the random meta-analysis was calculated in R35 according to the following formula36: power = 1 - ϕ (Cα - λ*) + ϕ (-Cα - λ*).
Quality and levels of evidence and risk of bias
The quality of evidence was rated according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach, which encompasses four levels of evidence: very low, low, moderate, and high.37 Observational studies always start as low-quality evidence, and randomized clinical trials always start at the high level of evidence.37 Five factors may decrease the quality of evidence (study limitations, imprecision, inconsistency of results, indirectness of evidence, and publication bias), and three factors may increase it (large effect, dose-response relationship, and one factor related to confounding).
Results
Search strategy
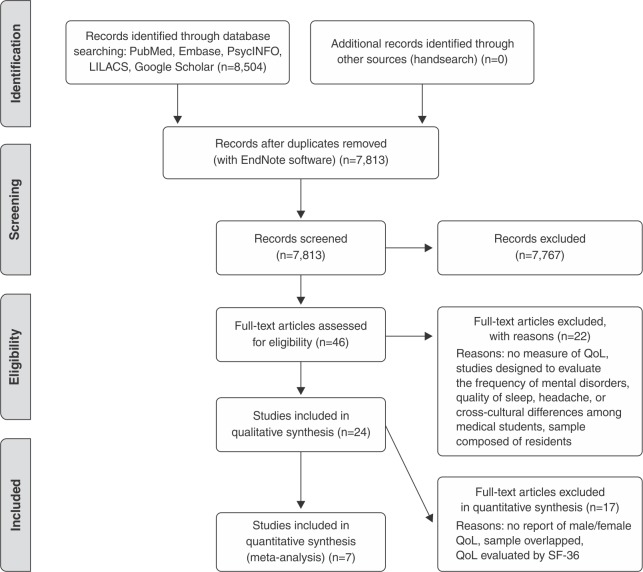
A total of 8,504 studies were initially identified, of which 7,767 were excluded based on their titles and abstracts; 46 full-text articles were retrieved, and 22 were excluded. A total of 24 studies were included in the systematic review; 17 were excluded from meta-analysis due to unreported male/female QoL, overlapping sample, or use of the SF-36 to evaluate QoL. A flow diagram of study selection is depicted in Figure 1.
Figure 1. Flow diagram of study selection. QoL = quality of life; SF-36 = 36-item Short Form Health Survey.
Sample characteristics
Nineteen cross-sectional studies and four multicenter studies derived from a single cross-sectional survey comprised our data (Tables 1 and 2). The majority of respondents were aged 18-24 and female.
A total of 21 medical schools were represented in the 19 cross-sectional studies: Universidade Federal de Uberlândia, Universidade Federal de Pernambuco, Universidade Estadual de Pernambuco, Escola Pernambucana de Medicina, Pontifícia Universidade Católica de Sorocaba, Universidade Estadual do Rio de Janeiro, Universidade Federal de Pelotas, Universidade Federal Fluminense, Escola Bahiana de Medicina e Saúde Pública, Universidade Veiga de Almeida, Universidade Federal de São Paulo, Universidade Nove de Julho, Faculdades Integradas de Patos, Universidade Federal de Santa Catarina, Universidade do Sul de Santa Catarina, Universidade do Oeste de Santa Catarina, Universidade do Vale do Itajaí, Universidade da Região de Joinville, Universidade do Planalto Catarinense, Universidade Comunitária da Região de Chapecó, and Universidade do Extremo Sul Catarinense.
The multicenter survey covered 22 Brazilian medical schools: Escola Bahiana de Medicina e Saúde Pública, Faculdade de Medicina de Marília, Faculdade de Medicina de São José do Rio Preto, Faculdade de Ciências Médicas da Paraíba, Faculdade Evangélica do Paraná, Faculdade de Medicina do ABC, Fundação Universidade Federal de Rondônia, Pontifícia Universidade Católica do Rio Grande do Sul, Pontifícia Universidade Católica de São Paulo, Universidade Estadual do Piauí, Universidade Federal do Ceará, Universidade Federal de Ciências da Saúde de Porto Alegre, Universidade Federal de Goiás, Universidade Federal de Mato Grosso do Sul, Universidade Federal do Rio de Janeiro, Universidade Federal do Tocantins, Universidade Federal de Uberlândia, Universidade Estadual Paulista Julio de Mesquita Filho, Centro Universitário Serra dos Órgãos, Universidade de Fortaleza, and Universidade de Passo Fundo.
QoL instruments
Three instruments were used to evaluate QoL, as described below.
WHOQOL-100 and WHOQOL-Bref
The WHOQOL is a QoL assessment instrument developed by international centers to measure individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns. The WHOQOL-100 encompasses 24 facets important in assessing QoL, and four general questions that address overall QoL and health. The WHOQOL-Bref was derived from the WHOQOL-100 and produces scores on four domains related to QoL: physical health, psychological, social relationships, and environment. It also includes one facet on overall QoL and general health.38,39 In a sample of 300 subjects surveyed in Porto Alegre, Southern Brazil, the instrument exhibited adequate internal consistency, discriminant validity, criterion validity, concurrent validity, and test-retest reliability.40
SF-36
The SF-36 is a self-report questionnaire designed to evaluate QoL in eight main domains: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning, and mental health.41 This instrument presented good performance in a Brazilian sample and is widely considered a reliable and valid measure of QoL for research purposes.42
General instruments
The instruments used to associate the scores of QoL in statistical analysis were: Beck Depression Inventory (BDI),43,44 CAGE (cut-annoyed-guilty-eye),15,45 Job Stress Scale,16,46 presence of reported chronic morbidity,19,20 Maslach Burnout Inventory – Student Survey (MBI-SS),22,47 Mini-Sleep Questionnaire (MSQ),22,48 Social Readjustment Rating Scale (SRRS),22,49 Epworth Sleepiness Scale (ESS),23,50 State-Trait Anxiety Inventory (STAI),25,51 Silhouette Scale,25,52 Profile of Mood States Scale (POMS),25,53 Inventário de Sintomas de Stress para Adultos de Lipp (ISSL),29,54 Self-Report Screening Questionnaire-20 (SRQ-20),30,55 Maslach Burnout Inventory – Human Services Survey (MBI-HSS),31,56 Interpersonal Reactivity Index (IRI),31,57 Dundee Ready Education Environment Measure (DREEM),32,58,59 Wagnild and Young’s Resilience Scale (RS),32,60 Leisure-time physical activity evaluation,34 and VERAS-Q (a questionnaire created to evaluate the QoL of students in the health professions).61
Results of the predictors associated with quality of life (QoL)
Positive predictors associated with QoL were: sense of academic efficacy/accomplishment, being a male student not supported by Fundo de Financiamento ao Estudante do Ensino Superior (FIES), body image satisfaction, religious beliefs, male gender, having at least one parent be a physician, satisfaction with the course, and psychological treatment (Tables 1, 2, and 3).
Negative predictors associated with QoL included depressive symptoms, female gender, being a third- or sixth-year student, economic class C/D, quota students, reported chronic illness, distance from hometown, burnout, sleep difficulties, cynicism, being supported by the FIES loan program, body mass index ≥ 30, daily commute time, stress, and psychiatric symptoms (Tables 1, 2 and 3).
Synthesis of results and risk of bias (results of meta-analysis)
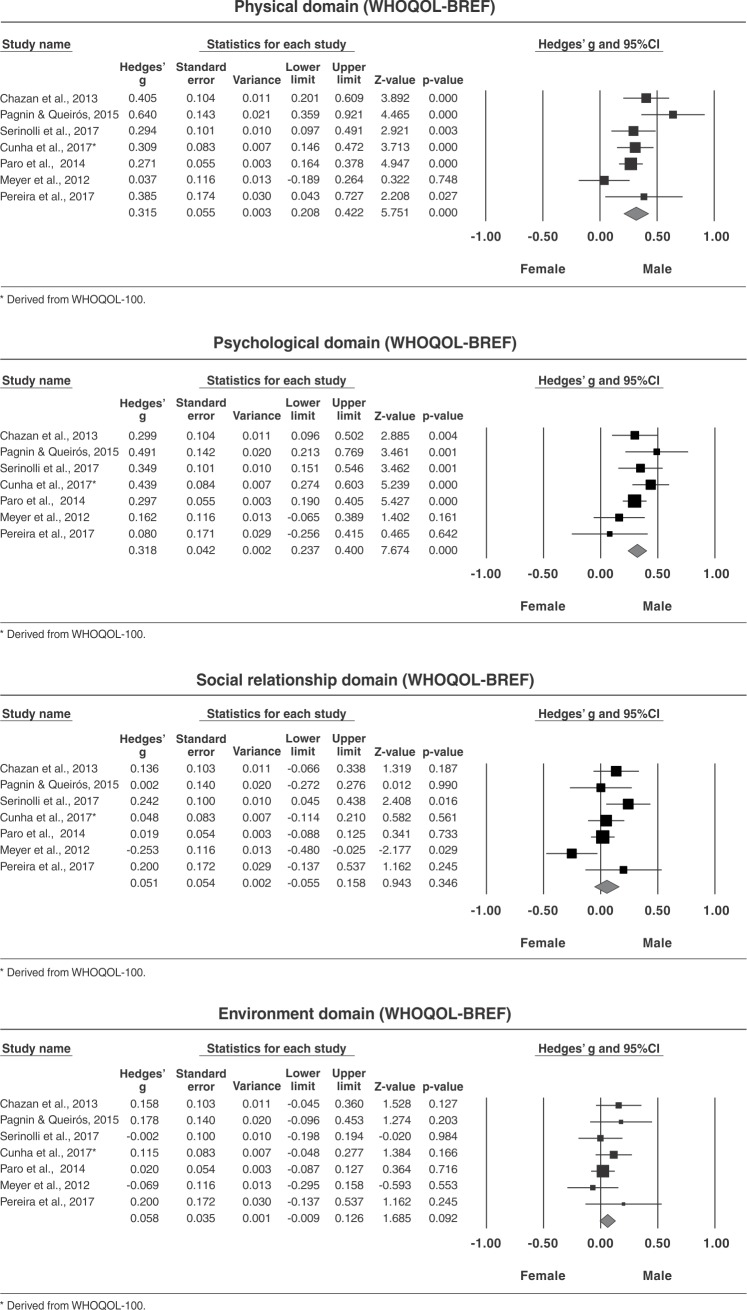
Seven studies were included in the meta-analysis.2,16,19,20,26-28,31 A significant between-groups effect size was observed for physical domain QoL (g = 0.315, 95% confidence interval [95%CI] = 0.20 to 0.42, p < 0.001), and a moderate heterogeneity (I2 = 51.42) was calculated (Figure 2). Trim-and-fill adjustment estimated a mean effect size of g = 0.258 (95%CI = 0.14-0.37). The failsafe N was 125, which means we would need 17.9 missing studies for every included study for the effect to be nullified, or 125 “null” studies with a two-tailed p-value to exceed 0.050.
Figure 2. Forest plot of between-group analyses – WHOQOL-Bref domains. 95%CI = 95% confidence interval; WHOQOL-100 = World Health Organization Quality of Life instrument; WHOQOL-Bref = World Health Organization Quality of Life instrument-Abbreviated version.
We also observed a significant between-groups effect size for the psychological domain (g = 0.318, 95%CI = 0.23 to 0.40, p < 0.001), and low heterogeneity (I2 = 20.83) (Figure 2). After adjustment, the estimate for Hedges’ g remained the same. The failsafe N was 123, i.e., we would need 123 “null” studies with a two-tailed p-value to exceed 0.05 or 17.6 missing studies for every included study for the effect to be nullified.
No difference in between-groups effect size was observed the for social relationship domain (g = 0.051, 95%CI = -0.05 to 0.15, p = 0.346) with moderate heterogeneity (I2 = 51.38) (Figure 2). The trim-and-fill values were g = 0.018 (95%CI = -0.09 to 0.12). The failsafe N was not relevant.
The mean effect size for the environment domain was g = 0.058 (95% CI = -0.009 to 0.126, p = 0.092); after adjustment, Hedges’ g was 0.043 (95% CI = -0.020 to 0.108) (Figure 2). No heterogeneity (I2 = 0.0) was detected. The failsafe N was not relevant. The quality of evidence was rated only for the studies included in the meta-analysis (Table 4).
Table 4. GRADE evidence profile according to WHOQOL-Bref domains of the studies included in meta-analysis.
| Factors which would downgrade the quality of evidence | Factors which would upgrade the quality of evidence | Summary of results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| WHOQOL-Bref outcomes (n) | Limitations | Inconsistency | Indirectness | Imprecision | Publication bias | Large effect | Dose-response | Confounders | Other | Quality of evidence/response | Comments |
| Physical domain 7 studies (3,402) |
Undetected (0) | Detected I2 = 51.42 (-1) |
Undetected (0) | Undetected Power of meta-analysis ≥ 80% (0) |
Undetected (0) | N/A (0) | N/A (0) | Confounder increased confidence in estimated effects in all studies (+1) | Detected representative samples (+1) | Moderate | +1 due to sample characteristics |
| Psychological domain 7 studies (3,402) |
Undetected (0) | Detected I2 = 20.83 (0) |
Undetected (0) | Undetected Power of meta-analysis ≥ 80% (0) |
Undetected (0) | N/A (0) | N/A (0) | Confounder increased confidence in estimated effects in all studies (+1) | Detected representative samples (+1) | High | +1 due to sample characteristics |
| Social relationship domain 7 studies (3,402) |
Undetected (0) | Detected I2 = 51.38 (-1) |
Undetected (0) | Detected Power of meta-analysis = 15.36% (-2) |
Undetected (0) | N/A (0) | N/A (0) | Confounder increased confidence in estimated effects in all studies (+1) | Detected representative samples (+1) | Low | +1 due to sample characteristics |
| Environment domain 7 studies (3,402) |
Undetected (0) | Undetected I2 = 0.0 (0) |
Undetected (0) | Detected Power of meta-analysis = 45% (-2) |
Undetected (0) | N/A (0) | N/A (0) | Confounder increased confidence in estimated effects in all studies (+1) | Detected representative samples (+1) | Low | +1 due to sample characteristics |
N/A = not applicable or not rated.
Discussion
The present systematic review aimed to identify studies that evaluated predictors associated with QoL in Brazilian medical students. We observed that female students exhibited lower QoL scores compared to male students. To facilitate understanding of the framework of our systematic review, predictors were clustered into four major types: demographic, academic, psychological, and physiological (Table 3).
Two main predictors related to demographic factors were associated with a decrease in QoL: gender (female) and economic class. Seven cross-sectional studies2,12,19,23,26-28 and one multicenter study31 observed that female students presented lower QoL scores in the physical and psychological domains compared to male students. This finding is probably related to a higher frequency of mood disorder in female patients and, as observed in the WHO World Mental Health (WMH) Survey Initiative, with pre-matriculation onset.10 Two studies applied the SF-36 to evaluate QoL,12,23 five studies used the WHOQOL-Bref,2,19,27,28,31 and one used the WHOQOL-100.26 Two studies were excluded from meta-analysis because of weak correlation (r ≤ 0.6) between WHOQOL-Bref and SF-36 domains.12,23 The power of meta-analysis was ≥ 80% for the physical and psychological domains, 15.36% for the social relationship domain, and 45% for the environment domain (Figure 2). Although the social relationship and environment domains have previously been identified as significant predictors of QoL in Brazilian medical students,19,20,27 the pooled effect sizes of these two domains were underpowered to reach a definitive conclusion (g = 0.051, 95%CI = -0.05 to 0.15, p = 0.346; and g = 0.058, 95% CI = -0.009 to 0.122, p = 0.126, respectively). This means that a significant effect size would probably be identified if more studies were included in the meta-analyses.
Three cross-sectional studies observed that economic factors were associated with lower QoL scores,25,19,20,23 and one found no correlation of QoL with income factors.12 These studies were conducted in private and public universities. Interestingly, two of them examined students supported by Brazilian government funding.19,20,23 While this incentive allows admission low-income students into the medical school, the financial value should be reappraised, at least to balance the scores of QoL between students. The daily strains associated with socioeconomic status may affect mental health, and further surveys should investigate this factor in a nationwide sample to encourage action by the government.
The most frequent academic predictor investigated was related to the year of medical school (years of study). Some cross-sectional studies2,12,14,15,19,20,23,26 and a large multicenter survey31 evaluated this parameter. Studies that applied the SF-36 generally observed a deterioration of physical and mental health in the sixth year of study compared to the first.12,23 On the other hand, conflicting results were reported in studies which used WHOQOL instruments. Two studies detected significant differences between the first and sixth year of study19,20,26 in all domains of QoL, and two studies reported no differences.2,27 The other studies observed a significant difference in a specific domain of WHOQOL-Bref – specifically, the psychological14 and social relationship15,31 domains. Academic overload, the nature of the medical school curriculum, hospital training, and sleep disturbances may explain some of the QoL impairment experienced in the last years of medical training.12 Meta-analyses were done to compare the first and second versus the fifth and sixth years of study, but the pooled effect sizes were underpowered to detect significant differences between the groups in all domains of WHOQOL-Bref (data not shown). Additional studies are needed to ensure an adequately powered meta-analysis.
Depressive symptoms were the main psychological predictor associated with low QoL scores.12,22 This result is in agreement with a recent meta-analysis which focused on the prevalence of mental disorders among Brazilian medical students.08 Interestingly, these authors also noted that the high frequency of mental disorders in this population is not related to the learning environment. Furthermore, as observed in the U.S., depression and suicidal symptoms among medical students may influence the quality of care provided to patients in academic medical centers, and affect adversely students’ long-term health.62
Several physiological factors identified as relevant elsewhere, such as presence of chronic illness,19,20 body mass index,27 body image satisfaction,25 sleep difficulties,22 and other factors, such as daily commute time,27 distance from one’s hometown,21 having at least one parent be a physician,27 religious beliefs,27 cynicism,22 satisfaction with medical school,28 and sense of academic efficacy/accomplishment,22 were not yet well-replicated in our country, and should be further investigated in other studies.
This study has major limitations that should be addressed. First, not all medical schools were included. This means that potentially significant regional predictors were not detected/replicated in the systematic review or meta-analysis to measure their impact on QoL. Second, there is a high probability that lower QoL scores observed in female students are related to mental disorders and with pre-matriculation onset. Unfortunately, this study does not provide data to support this statement. Therefore, we believe that medical students should be screened for mental disorders when entering medical school. This information will help institutional leaders provide support when necessary.
Finally, we conclude that the main predictors that can change the scores of QoL of Brazilian medical students are related to the emotional and physical domains of female students. Medical school curricula might warrant revision considering this overall finding, and specific interventions should be designed for this group as appropriate.
Implications for research
Future studies should focus on determining whether scores on the social relationships and environment domains of QoL are associated with gender.
There is evidence to speculate that specific years of medical school are associated with a decline in students’ QoL. Additional studies should address this question.
Household income was considered a significant predictor of QoL in some Brazilian regions. This predictor should be further investigated in all Brazilian states.
Disclosure
The authors report no conflicts of interest.
Footnotes
How to cite this article: Solis AC, Lotufo-Neto F. Predictors of quality of life in Brazilian medical students: a systematic review and meta-analysis. Braz J Psychiatry. 2019;41:556-567. http://dx.doi.org/10.1590/1516-4446-2018-0116
References
- 1.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 2.Pagnin D, de Queiroz V. Comparison of quality of life between medical students and young general populations. Educ Health (Abingdon). 2015;28:209–12. doi: 10.4103/1357-6283.178599. [DOI] [PubMed] [Google Scholar]
- 3.Messina G, Quercioli C, Troiano G, Russo C, Barbini E, Nisticò F, et al. Italian medical students quality of life: years 2005-2015. Ann Ig. 2016;28:245–51. doi: 10.7416/ai.2016.2103. [DOI] [PubMed] [Google Scholar]
- 4.Henning MA, Krägeloh CU, Hawken SJ, Zhao Y, Doherty I. The quality of life of medical students studying in New Zealand: a comparison with nonmedical students and a general population reference group. Teach Learn Med. 2012;24:334–40. doi: 10.1080/10401334.2012.715261. [DOI] [PubMed] [Google Scholar]
- 5.Lucchetti G, Damiano RF, DiLalla LF, Lucchetti AL, Moutinho IL, da Silva Ezequiel O, et al. Cross-cultural differences in mental health, quality of life, empathy, and burnout between US and Brazilian medical students. Acad Psychiatry. 2018;42:62–7. doi: 10.1007/s40596-017-0777-2. [DOI] [PubMed] [Google Scholar]
- 6.Dehning S, Gasperi S, Tesfaye M, Girma E, Meyer S, Krahl W, et al. Empathy without borders? Cross-cultural heart and mind-reading in first-year medical students. Ethiop J Health Sci. 2013;23:113–22. [PMC free article] [PubMed] [Google Scholar]
- 7.Millan LR, Arruda PC. [Psychological assistance to medical students: 21 years of experience]. Rev Assoc Med Bras (1992). 2008;54:90–4. doi: 10.1590/s0104-42302008000100027. [DOI] [PubMed] [Google Scholar]
- 8.Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry. 2017;39:369–78. doi: 10.1590/1516-4446-2017-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrade LH, Wang YP, Andreoni S, Silveira CM, Alexandrino-Silva C, Siu ER, et al. Mental disorders in megacities: findings from the São Paulo megacity mental health survey, Brazil. PLoS One. 2012;7:e31879. doi: 10.1371/journal.pone.0031879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016;46:2955–70. doi: 10.1017/S0033291716001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheffer M, Biancarelli A, Cassenote A. Departamento de Medicina Preventiva da Faculdade de Medicina da USP, Conselho Regional de Medicina do Estado de São Paulo, Conselho Federal de Medicina. São Paulo: 2015. Demografia médica no Brasil 2015. [cited 2018 Oct 22]. http:/www.usp.br/agen/wp-content/uploads/DemografiaMedica30nov2015.pdf. [Google Scholar]
- 12.Paro HB, Morales NM, Silva CH, Rezende CH, Pinto RM, Morales RR, et al. Health-related quality of life of medical students. Med Educ. 2010;44:227–35. doi: 10.1111/j.1365-2923.2009.03587.x. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Alves JGB, Tenório M, Anjos AG, Figueroa JN. Qualidade de vida em estudantes de medicina no início e final do curso: avaliação pelo Whoqol-bref. Rev Bras Educ Med. 2010;34:91–6. [Google Scholar]
- 15.Ramos-Dias JC, Libardi MC, Zillo CM, Igarashi MH, Senger MH. Qualidade de vida em cem alunos do curso de medicina de Sorocaba - PUC/SP. Rev Bras Educ Med. 2010;34:116–23. [Google Scholar]
- 16.Meyer C, Guimarães ACA, Machado Z, Parcias SR. Qualidade de vida e estresse ocupacional em estudantes de medicina. Rev Bras Educ Med. 2012;36:489–98. [Google Scholar]
- 17.Olmo NRS, Ferreira LF, Prado AD, Martins LC, Dedivitis RA. Percepção dos estudantes de medicina do primeiro e sexto anos quanto à qualidade de vida. Diagn Tratamento. 2012;17:157–61. [Google Scholar]
- 18.Paro CA, Bittencourt ZZLC. [Quality of life of the undergraduate health students]. Rev Bras Educ Med. 2013;37:365–75. [Google Scholar]
- 19.Chazan AC, Campos MR, Portugal FB. Quality of life of medical students at the State University of Rio de Janeiro (UERJ), measured using Whoqol-bref: a multivariate analysis. Cien Saude Colet. 2015;20:547–56. doi: 10.1590/1413-81232015202.05182014. [DOI] [PubMed] [Google Scholar]
- 20.Chazan ACS, Campos MR. Qualidade de vida de estudantes de medicina medida pelo WHOQOL-bref - UERJ, 2010. Rev Bras Educ Med. 2013;37:376–84. [Google Scholar]
- 21.Hickel F, Fabro BR, Bertoldi EG. Fatores de risco cardiovascular e qualidade de vida de acadêmicos de medicina da Universidade Federal de Pelotas. Rev AMRIGS. 2015;59:186–91. [Google Scholar]
- 22.Pagnin D, de Queiroz V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus. 2015;4:676. doi: 10.1186/s40064-015-1477-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lins L, Carvalho FM, Menezes MS, Porto-Silva L, Damasceno H. Health-related quality of life of medical students in a Brazilian student loan programme. Perspect Med Educ. 2016;5:197–204. doi: 10.1007/s40037-016-0283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lins L, Carvalho FM, Menezes MS, Silva LP, Damasceno H. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ. 2015;6:149–54. doi: 10.5116/ijme.563a.5dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Legey S, Lamego MK, Lattari E, Campos C, Paes F, Sancassiani F, et al. Relationship among body image, anthropometric parameters and mental health in physical education students. Clin Pract Epidemiol Ment Health. 2016;12:177–87. doi: 10.2174/1745017901612010177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cunha DHFda, Moraes MAde, Benjamin MR, Santos AMNdos. Percepção da qualidade de vida e fatores associados aos escores de qualidade de vida de alunos de uma escola de medicina. J Bras Psiquiatr. 2017;66:189–96. [Google Scholar]
- 27.Serinolli MI, Novaretti MC. A cross-sectional study of sociodemographic factors and their influence on quality of life in medical students at Sao Paulo, Brazil. PLoS One. 2017;12:e0180009. doi: 10.1371/journal.pone.0180009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pereira FEL, Ribeiro RdC, Oliveira LMS, Araujo JL, Filho, Tabosa MNR, Gouveia PS, Filho, et al. Correlatos da qualidade de vida com características de saúde e demográficas de estudantes de medicina. Rev Bras Qual Vida. 2017;9:247–60. [Google Scholar]
- 29.Ribeiro RC, Reinaldo ARG, de Oliveira DPA, Rezende ACC, Estrela YdCA, Rodrigues VR, et al. Relação da qualidade de vida com problemas de saúde mental em universitários de medicina. Rev Bras Qual Vida. 2018;10:e7646. [Google Scholar]
- 30.Santos LSd, Ribeiro ĺJS, Boery EN, Boery RNSdO. Qualidade de vida e transtornos mentais comuns em estudantes de medicina. Cogitare Enferm. 2017;22:1–7. [Google Scholar]
- 31.Paro HB, Silveira PS, Perotta B, Gannam S, Enns SC, Giaxa RR, et al. Empathy among medical students: is there a relation with quality of life and burnout? PLoS One. 2014;9:e94133. doi: 10.1371/journal.pone.0094133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tempski P, Santos IS, Mayer FB, Enns SC, Perotta B, Paro HB, et al. Relationship among medical student resilience, educational environment and quality of life. PLoS One. 2015;10:e0131535. doi: 10.1371/journal.pone.0131535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Enns SC, Perotta B, Paro HB, Gannam S, Peleias M, Mayer FB, et al. Medical students' perception of their educational environment and quality of life: is there a positive association? Acad Med. 2016;91:409–17. doi: 10.1097/ACM.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 34.Peleias M, Tempski P, Paro HB, Perotta B, Mayer FB, Enns SC, et al. Leisure time physical activity and quality of life in medical students: results from a multicentre study. BMJ Open Sport Exerc Med. 2017;3:e000213. doi: 10.1136/bmjsem-2016-000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.R Core Team . R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2014. http://www.R-project.org/ [Google Scholar]
- 36.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to meta-analysis. Chichester: John Wiley & Sons, Ltd. 2009 [Google Scholar]
- 37.Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 38.Development of the World Health Organization WHOQOL-BREF quality of life assessment The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 39.Fleck MPdA. O instrumento de avaliação de qualidade de vida da Organização Mundial da Saúde (WHOQOL-100): características e perspectivas. Cien Saude Colet. 2000;5:33–8. [Google Scholar]
- 40.Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. [Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref]. Rev Saude Publica. 2000;34:178–83. doi: 10.1590/s0034-89102000000200012. [DOI] [PubMed] [Google Scholar]
- 41.Ware JE jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 42.Laguardia J, Campos MR, Travassos CM, Najar AL, Anjos LA, Vasconcellos MM. Psychometric evaluation of the SF-36 (v.2) questionnaire in a probability sample of Brazilian households: results of the survey Pesquisa Dimensões Sociais das Desigualdades (PDSD), Brazil, 2008. Health Qual Life Outcomes. 2011;9:61. doi: 10.1186/1477-7525-9-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 44.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–7. [PubMed] [Google Scholar]
- 45.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 46.Alves MG, Chor D, Faerstein E, Lopes Cde S, Werneck GL. [Short version of the “job stress scale”: a Portuguese-language adaptation]. Rev Saude Publica. 2004;38:164–71. doi: 10.1590/s0034-89102004000200003. [DOI] [PubMed] [Google Scholar]
- 47.Galán F, Sanmartín A, Polo J, Giner L. Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. Int Arch Occup Environ Health. 2011;84:453–9. doi: 10.1007/s00420-011-0623-x. [DOI] [PubMed] [Google Scholar]
- 48.Falavigna A, de Souza Bezerra ML, Teles AR, Kleber FD, Velho MC, da Silva RC, et al. Consistency and reliability of the Brazilian Portuguese version of the Mini-Sleep Questionnaire in undergraduate students. Sleep Breath. 2011;15:351–5. doi: 10.1007/s11325-010-0392-x. [DOI] [PubMed] [Google Scholar]
- 49.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11:213–8. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 50.Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW. Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol. 2009;35:877–83. doi: 10.1590/s1806-37132009000900009. [DOI] [PubMed] [Google Scholar]
- 51.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the strait-trait anxiety inventory. Paolo Alto: Consulting Psychologists; 1970. [Google Scholar]
- 52.Stunkard AJ, Sørensen T, Schulsinger F. Use of the Danish adoption register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–20. [PubMed] [Google Scholar]
- 53.Viana MF, Almeida PL, Santos RC. Adaptação portuguesa da versão reduzida do perfil de estados de humor - POMS. Ana Psicologica. 2001;19:77–92. [Google Scholar]
- 54.Lipp MEN. Manual do inventário de sintomas de stress para adultos de Lipp (ISSL). Vol. 76 São Paulo: Casa do Psicólogo; 2000. [Google Scholar]
- 55.Mari JJ, Williams P. A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Br J Psychiatry. 1986;148:23–6. doi: 10.1192/bjp.148.1.23. [DOI] [PubMed] [Google Scholar]
- 56.Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach burnout inventory. Palo Alto: Consulting Psychologists; 1986 [Google Scholar]
- 57.Koller SH, Camino C, Ribeiro J. Adaptação e validação interna de duas escalas de empatia para uso no Brasil. Estud Psicol. 2001;18:43–53. [Google Scholar]
- 58.Roff S, McAleer S, Harden RM, Al-Qahtani M, Ahmed AU, Deza H, et al. Development and validation of the Dundee ready education environment measure (DREEM). Med Teach. 1997;19:295–9. [Google Scholar]
- 59.de Oliveira GR, Filho, Vieira JE, Schonhorst L. Psychometric properties of the Dundee ready educational environment measure (DREEM) applied to medical residents. Med Teach. 2005;27:343–7. doi: 10.1080/01421590500046387. [DOI] [PubMed] [Google Scholar]
- 60.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1:165–78. [PubMed] [Google Scholar]
- 61.Tempski P, Perotta B, Pose RA, Vieira JE. A questionnaire on the quality of life of medical students. Med Educ. 2009;43:1107–8. doi: 10.1111/j.1365-2923.2009.03476.x. [DOI] [PubMed] [Google Scholar]
- 62.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–36. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]