Abstract
Objective:
There are few quantitative studies on art therapy for the treatment of depression. The objective of this study was to evaluate if art therapy is beneficial as an adjuvant treatment for depression in the elderly.
Methods:
A randomized, controlled, single-blind study was carried out in a sample of elderly women with major depressive disorder (MDD) stable on pharmacotherapy. The experimental group (EG) was assigned to 20 weekly art therapy sessions (90 min/session). The control group (CG) was not subjected to any adjuvant intervention. Patients were evaluated at baseline and after 20 weeks, using the Geriatric Depression Scale (GDS), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and cognitive measures.
Results:
Logistic regression analysis adjusted for age revealed that women in EG (n=31) had significant improvement in GDS (p = 0.007), BDI (p = 0.025), and BAI (p = 0.032) scores as compared with controls (n=25). No difference was found in the cognitive measures.
Conclusion:
Art therapy as an adjunctive treatment for MDD in the elderly can improve depressive and anxiety symptoms.
Clinical trial registration:
RBR-2YXY7Z
Keywords: Art therapy, depression, anxiety, elderly patients, clinical trial
Introduction
Major depressive disorder (MDD) is not part of aging, even though it is a common problem in the elderly. MDD may have physical and mental consequences that worsen general health condition and quality of life in elderly patients.1,2 Less than half of patients with depressive disorders receive proper treatment.3-8 This lack of access to treatment is greater among elderly, low-income, and minority populations.2,9
Pharmacotherapy is frequently indicated in the management of depression, especially in moderate to severe cases. The combination of pharmacotherapy and psychotherapy in elderly patients with MDD is often more efficient than any of these approaches alone,9 and is associated with lower abandonment rates than pharmacotherapy alone; thus, this combination may be indicated for patients with low medication adherence.10
Several types of psychotherapy can be used in the treatment of depression, with large variability in adherence and response, depending, among other factors, on patient characteristics. Although most studies on psychotherapy for depression have involved the adult population, several studies indicate that numerous types of psychotherapy are also effective in elderly patients.9,11-14
Cognitive-behavioral therapy, interpersonal psychotherapy, and problem-solving therapy are considered first-line treatments both for adult and elderly patients.9 Reminiscence therapy, psychodynamic therapy, support therapy, and nondirective counseling,3,5,12,13 as well as self-esteem therapy,14 life review therapy, and depression management therapy,6 can also be beneficial in the treatment of depressive symptoms in the elderly.
Among these many therapies and approaches, evidence suggests that active engagement in creative activities, including art, can bring many benefits, including improved well-being, quality of life, health, and socialization.15,16 Art therapy is a creative approach used as a therapeutic technique. It is intrinsically connected to artistic making, which has been a human practice since time immemorial. The therapeutic function of art is related to the possibility of concretization of thoughts, feelings, desires, and the facts of life using expressive resources. Art therapy uses these resources, which mobilize several aspects of the human mind: cognition, the sensorimotor system, emotions, and intuition. Art therapy does not concern itself only with the final product (visual arts, body expression, and other forms of art per se), but also with the creative process and the connection of artistic making and the person who makes it.16 Art therapy is suited to treating issues or themes that are also managed by other well-known forms of psychotherapy, such as interpersonal therapy, depression management therapy, and life review therapy.17
Art therapy can be used in various populations. For example, it may be particularly beneficial in individuals who do not adapt to psychotherapeutic approaches that are exclusively verbal. Art therapy can help establish communication between patient and therapist and may aid in the emergence of personality aspects or facts of life to be dealt with in the therapeutic process.16,18,19 An art therapy session is often preceded by activities that promote relaxation and introspection, such as mental imagery. It can be used to link sensory perception and emotions,20 and thus relieve the discomfort associated with mood disorders.21,22
Meta-analyses and systematic reviews of art therapy are scarce. In a study of 15 randomized controlled trials (n=777), meta-analysis was not possible because of clinical heterogeneity and insufficiently comparable data on outcome measures across studies. Although the quality of the randomized trials was generally low, art therapy was associated with significant positive changes in nonpsychotic mental health symptoms relative to control groups in 10 out of the 15 studies. Therefore, art therapy can be an acceptable treatment and appears to be cost-effective compared with wait-listing, but further studies are needed.16
Thus, there is evidence that art therapy may contribute to improvement of psychological parameters in different disorders. However, controlled studies with quantitative measures are still needed to establish its potential role in MDD, a highly prevalent disorder. In this context, the present study was designed to evaluate the effects of 20 sessions of adjunctive art therapy on mood, cognition, and functionality in elderly women with MDD stable under pharmacological treatment.
Methods
This randomized, controlled, single-blind study was carried out at the Instituto de Psiquiatria, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (IPq-HCFMUSP), Brazil. All participants signed an informed consent form approved by the local ethics committee before enrolling in this study. The study was approved and authorized by the FMUSP ethics committee (protocol no. 211.133/13), and was registered with the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; UTN U1111-1192-1365) and the Brazilian Registry of Clinical Trials (Registro Brasileiro de Ensaios Clínicos [ReBec]; RBR-2YXY7Z).
Sample
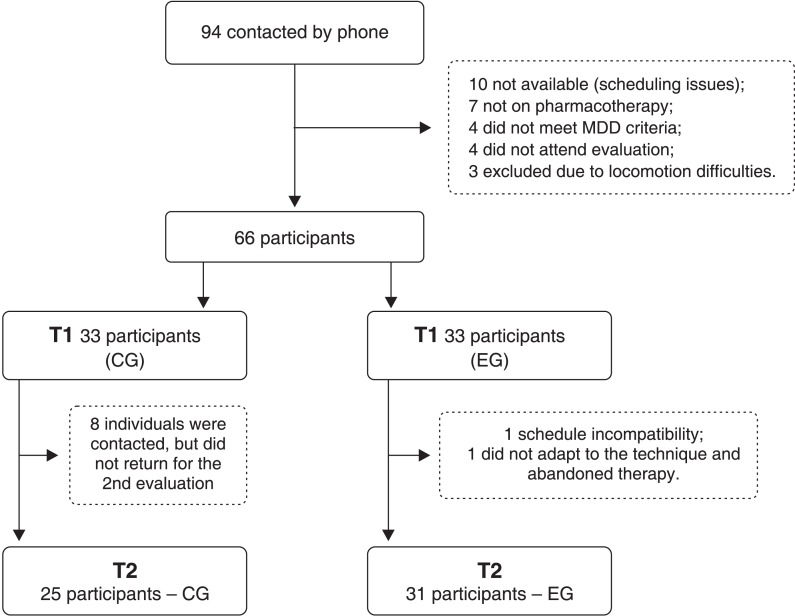
Elderly outpatients attending IPq-FMUSP were invited to take part in the study. Ninety-four patients were initially contacted by telephone and underwent pre-screening (see the flow diagram in Figure 1).
Figure 1. Flow diagram of participant selection. CG = control group. EG = experimental group. MDD = major depressive disorder. T1 = time point 1. T2 = time point 2.
The inclusion criteria were: a lifetime DSM-5 diagnosis of MDD,23 female gender, age 60 years or older, ability to read and write, and agreement to take part in the study. Besides, participants had to be stable on pharmacotherapy for depression, i.e., with no change in medication regimen (agent or dosage) throughout the study period. The decision to keep patients on their current medication regimen was made by each participant’s attending psychiatrist, based on the perception that the best improvement in symptoms was already being achieved with the current dose with the least side effects possible. Patients with depression scale scores above the cutoff were acceptable, and all had to be available to take part in all evaluations and interventions.
The exclusion criteria were cognitive difficulties suggestive of dementia, defined by a Mini-Mental State Examination (MMSE)24,25 score below 25 for people with 1 to 4 years of formal schooling or below 27 for people with 5 years or more of schooling. We also excluded drug users, those with degenerative diseases, and those with any systemic disorders associated with high morbidity and mortality, such as cancers with poor prognosis or progressive renal impairment.
Ninety-four patients were initially screened. Twenty-eight did not meet the inclusion criteria. A psychiatrist interviewed the remaining 66 patients, using the Structured Clinical Interview (SCID) to confirm MDD diagnosis according to the DSM-5 criteria. No patient met the exclusion criteria. To randomize the participants, the order of study entry was obeyed for each group of 22 people per semester. Odd-numbered entrants were allocated to the CG (11 patients), and even-numbered entrants constituted the experimental group (EG) (11 patients).
The CG and EG were thus formed of 33 participants each. At the end of the study, 25 participants were still present in the CG and 31 in the EG.
EG participants received 20 art therapy workshops, while the CG did not receive any type of psychotherapy during the study period. After the study, however, patients in the CG could take part in the art therapy workshops if they so wished.
Evaluation tools
Patients in the CG and in the EG were subjected to the same battery of standardized tests, carried out by the same team of neuropsychologists, at the start of the study (time point 1) and at the end of the 20-week study period (time point 2). The mean duration of the test battery was 45 minutes. For the EG, tests were carried out at the end of the 20 art therapy weekly sessions. For CG, they were carried out the same 20-week interval, in which patients were not subjected to any intervention.
Sociodemographic questionnaires were administered that included information on age, educational attainment, marital status, and income level. Questionnaires about medications used, number of previous depressive episodes, and presence of other diseases besides depression were also applied.
Depression was evaluated with the Geriatric Depression Scale (GDS-15).26,27 This diagnostic instrument is designed to detect depressive symptoms in the elderly and consists of 15 affirmative/negative questions regarding satisfaction and hope in life, fatigue, and memory. The cutoff point for depression is 5. Scores between 1 and 5 are considered subsyndromal depression; scores between 6 and 10 are considered depression; and scores between 11 and 15 are considered severe depression. Depressive symptoms were also evaluated with the Beck Depression Inventory (BDI),28 which consists of 21 questions about how the individual has felt in the preceding week regarding depressive symptoms such as hopelessness, irritability, guilt, or feelings of being punished, as well as physical symptoms such as fatigue, weight loss, and decreased libido. Each question is scored on a scale of 0 to 3; therefore, the maximum BDI score is 63. The cutoff point for depression is 12, and scores between 1 and 11 are considered subsyndromal depression.
As the GDS is validated for the study of depression in the elderly26,27 and the BDI is widely used for adults and it is more comprehensive in several aspects of depression, we also checked for correlation between these scales.
Anxiety was evaluated by the Beck Anxiety Inventory (BAI),29 which consists of 21 questions about how the individual has felt in the preceding week regarding common anxiety symptoms, such as sweating, tremor, fear, and feelings of distress. The cutoff point for anxiety is 12, and scores between 1 and 11 are considered subsyndromal anxiety.
A cognitive assessment battery was also administered, consisting of the MMSE,24,25 the Verbal Fluency Test – animal category,30 the Trail Making Test A,31 and the Rey Complex Figure (Rey CF) task.32 In the Verbal Fluency Test – animal category,30 normal performance was defined as the ability to remembering more than 12 animals (for participants with 1 to 7 years of formal schooling) or more than 13 animals (for participants with 8 years or more of schooling). The Trail Making Test A31 was used to evaluate cognitive functions involving sustained attention, cognitive flexibility, executive functions, sequencing ability, and motor speed. The Rey CF32 is a visuospatial task that requires visual attention and memory. First, the participant copied a complex drawing while observing it. This first step analyzes visuospatial processing and strategy development. After 30 minutes, the patient was asked to draw the figure again, without seeing it. This step of the test is known as the Rey Delayed Recall (Rey DR) task, and was used to assess visual and operational memory. The lower the score, the worse the participant’s visuospatial aptitude.
Study intervention
Art therapy sessions were carried out at the IPq-HCFMUSP workshop facility. EG patients participated in 20 art therapy sessions lasting 90 minutes each, all led by the same art therapist. Although the art therapy intervention involved three groups of 11 participants each, the workshops had an individual focus, that is, each participant was instructed to work on her own artistic output during the session.
The workshops produced a therapeutic context in which nonverbal expression was used to facilitate self-knowledge, self-esteem, and self-acceptance. The techniques used involved themes that led to reflection on adaptation to difficult life circumstances, such as losses, death, finitude, resentment, solitude, and feelings of impotence.
All sessions were divided into four parts:
Welcome: patients entered the room and got ready to start working.
Relaxation and guided imagery: the art therapist asked patients to disconnect from their daily thoughts and breathe gently. With the aid of a specific song selected for each session, relaxation and guided imagery activities were carried out, usually by inducing the participants to imagine a nature setting of their choice. Then, the topic for artistic creation during the session was proposed. The art therapist’s spoken guidance during the guided imagery activity was conceived as an introduction to the artistic work itself, so that the participants would get in touch with images and emotions related to the topic to be addressed during the session.
Artistic output. After the guided imagery activity, the art therapist instructed the participants to work out the topic that had been proposed, using the art supplies available. Techniques such as painting, drawing, clay modeling, weaving, and collage were used. For the workshop devoted to the topic of “self-esteem,” for instance, participants were instructed to fashion a mandala out of grains and seeds glued onto a piece of cardboard, and were told that each grain or seed was to represent a quality they recognized in their personality. The topic “sense of loss” was worked through by having participants stop while their artworks were still unfinished and switching works with another participant. “Difficulty in dealing with difficult situations” was worked through by providing participants with rocks, which they were instructed to “place in a more beautiful context” within their artworks, thus helping them change their outlook on the situation. The topic “controlling tendencies” was worked through by having participants blow paint through a soda straw; the fact it is very difficult to control the direction of the paint was intended to show participants that life is difficult to control.
Once the artworks were completed, each participant was invited to verbally express her reflections and any feelings that surfaced during the activity. This verbalization step was important for participants to elaborate on what emerged during their production, while the group and the art therapist listened; the art therapist then helped each patient understand her artistic output. The participants took their artworks home at the end of each session.
On average, the relaxation and guided imagery step lasted 7 minutes; the artistic output step lasted 60 minutes; and the verbalization step lasted 15 to 20 minutes.
Statistical analysis
Quantitative data were analyzed in SPSS version 20 for Windows. The Kolmogorov-Smirnov method was used to test for normality of data distribution. As the assumption of normality was rejected, nonparametric tests were used to evaluate participant scores. The Mann-Whitney U test was used to compare sociodemographic data, number of depressive episodes, and cognitive and psychiatric variables between the EG and CG. The chi-square test and, as necessary, Fisher’s exact test were used to test for associations between group allocation and the categorical variables. The Wilcoxon test was used to compare differences (baseline vs. follow-up) in scale scores for each of the groups (EG and CG, separately). The Mann-Whitney U test was also used to verify homogeneity between groups at baseline; as a significant difference in age between groups was observed (p = 0.033), all subsequent analyses were designed to control for age. Age-adjusted logistic regression analysis was used to assess differences between groups (EG and CG, as the dependent variable) in change in psychometric instrument scores (delta = time point 2 ‐ time 1, as explanatory variables). Spearman correlation coefficients were calculated to assess potential relationships among changes in the different psychometric instruments, and the correlation between delta GDS and delta BDI was found relevant. The significance level was set at p < 0.05 for all analyses.
Results
At baseline (time point 1), EG (n=31) and CG (n=25) were homogeneous for all variables, except age (p = 0.033), as seen in Table 1. There were no differences in educational attainment, marital status, depression onset after age 60 years, or number of previous depressive episodes. Groups were also similar in terms of pharmacological treatment (classified as an antidepressant alone, an antidepressant plus anxiolytics, or an antidepressant plus other psychotropic drugs; p = 0.60).
Table 1. Sociodemographic and clinical features of the control (CG) and experimental (EG) groups at baseline.
| Characteristics | CG (n=25) | EG (n=31) | p-value |
|---|---|---|---|
| Age (years) | 69.8±6.4 | 66.1±5.7 | 0.033 * |
| Schooling | 12.7±4.2 | 11.6±4.3 | 0.40* |
| Marital status, n (%) | |||
| Single | 10 (40.0) | 9 (29.0) | 0.096† |
| Married | 8 (32.0) | 6 (19.4) | |
| Widowed | 6 (24.0) | 7 (22.6) | |
| Divorced | 1 (4.0) | 9 (29.0) | |
| First episode after 60 years, n (%) | 5 (15.2) | 6 (18.2) | 0.741‡ |
| Number of depressive episodes | 3.0±1.2 | 3.6±1.7 | 0.225* |
| Geriatric Depression Scale ≤ 5 | 9±3.4 | 6±5.3 | 0.162‡ |
| Medication, n (%) | |||
| Antidepressant only | 14 (56.0) | 15 (48.4) | |
| Antidepressant and anxiolytic | 2 (8.0) | 2 (6.4) | 0.598† |
| Antidepressant and psychotropic | 9 (36.0) | 14 (45.2) |
Data presented as mean ± standard deviation, unless otherwise specified.
Mann-Whitney U; † Fisher’s exact test; ‡ chi-square test.
Furthermore, there were no between-group differences in psychiatric or cognitive variables of interest at baseline (Table 2).
Table 2. Psychiatric and cognitive variables in the control (CG) and experimental (EC) groups at baseline.
| Cognitive and psychiatric variables | CG (n=25) | EG (n=31) | p-value* |
|---|---|---|---|
| MMSE | 28.2±1.6 | 27.4±2.2 | 0.16 |
| Fluency | 17.0±5.4 | 16.8±3.3 | 0.87 |
| Trail Making A | 35.4±13.7 | 32.5±11.7 | 0.58 |
| Rey CF | 76.0±20.9 | 65.5±29.4 | 0.20 |
| Rey DR | 47.4±26.4 | 48.6±27.1 | 0.87 |
| GDS | 7.5±3.7 | 8.6±3.3 | 0.24 |
| BDI | 15.9±8.4 | 20.9±10.8 | 0.07 |
| BAI | 13.7±15.8 | 18.5±13.6 | 0.08 |
Data presented as mean ± standard deviation.
BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; Fluency = Verbal fluency test; GDS = Geriatric Depression Scale; MMSE = Mini-Mental State Examination; Rey CF = Rey Complex Figure Test; Rey DR = Rey Delayed Recall Task.
Mann-Whitney U.
Table 3 presents a longitudinal analysis of variables in each group. Baseline data (time point 1) were compared with data from the end of the study (time point 2) for each group. EG participants exhibited improvement in MMSE, GDS, BDI, BAI, and Rey DR scores, i.e., a reduction in depression and anxiety scores and an increase in cognition and visuoconstructive performance scores. CG participants only exhibited improvement in BDI scores.
Table 3. Longitudinal analysis of the data of each group separately: time 1 (T1) compared to time 2 (T2).
| T1 and T2 | CG (n=25) | p-value* | EG (n=31) | p-value* |
|---|---|---|---|---|
| MMSE 1 | 28.2±1.6 | 0.80 | 27.4±2.2 | 0.034 |
| MMSE 2 | 28.3±1.6 | 28.0±2.4 | ||
| Fluency 1 | 17.0±5.4 | 1.00 | 16.8±3.3 | 0.950 |
| Fluency 2 | 17.2±4.1 | 16.9±4.4 | ||
| Trail Making A1 | 35.4±13.7 | 0.27 | 32.5±11.7 | 0.150 |
| Trail Making A2 | 37.3±12.8 | 35.8±12.2 | ||
| Rey CF 1 | 76.0±20.9 | 0.29 | 65.6±29.4 | 0.570 |
| Rey CF 2 | 72.0±26.7 | 68.1±23.7 | ||
| Rey DR 1 | 47.4±26.5 | 0.19 | 48.6±27.1 | 0.002 |
| Rey DR 2 | 52.1±25.8 | 60.2±30.0 | ||
| GDS 1 | 7.5±3.65 | 0.12 | 8.6±3.3 | < 0.001 |
| GDS 2 | 6.9±3.53 | 5.5±3.4 | ||
| BAI 1 | 13.7±15.79 | 0.32 | 18.5±13.6 | 0.004 |
| BAI 2 | 10.8±10.26 | 9.6±8.3 | ||
| BDI 1 | 15.9±8.37 | 0.04 | 20.9±10.8 | < 0.001 |
| BDI 2 | 14.4±8.73 | 12.3±10.2 |
Data presented as mean ± standard deviation.
BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; CG = control group; EG = experimental group; Fluency = Verbal fluency test; GDS = Geriatric Depression Scale; MMSE = Mini-Mental State Examination; Rey CF = Rey Complex Figure Test; Rey DR = Rey Delayed Recall.
Wilcoxon test. Bold font indicates statistical significance.
Comparison of improvement/variation (delta) in psychometric scale scores between groups EG and CG was performed by age-adjusted logistic regression analysis (Table 4). EG participants exhibited a greater reduction (delta) in GDS, BDI, and BAI scores than controls. There was no significant difference between EG and CG in terms of the change in cognitive battery scores.
Table 4. Improvement (variation) in variables of interest in the control (CG) and experimental (EC) groups between time points 1 and 2.
| Delta | CG (n=25) | EG (n=31) | p-value* |
|---|---|---|---|
| MMSE | 0.1±0.8 | 0.6±1.7 | 0.090 |
| Fluency | 0.1±3.1 | 0.1±2.6 | 0.930 |
| Trail Making | 1.9±10.1 | 3.3±11.9 | 0.360 |
| Rey CF | 4.0±16.4 | 2.5±18.6 | 0.160 |
| Rey DR | 4.7±17.8 | 11.6±20.1 | 0.380 |
| GDS | -0.6±2.32 | -3.2±3.4 | 0.007 |
| BAI | -2.9±11.36 | -8.9±14.5 | 0.032 |
| BDI | -1.6±4.86 | -8.6±12.8 | 0.025 |
Data presented as mean ± standard deviation.
BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory;
Fluency = Verbal fluency test; GDS = Geriatric Depression Scale; MMSE = Mini-Mental State Examination; Rey CF = Rey Complex Figure Test; Rey DR = Rey Delayed Recall.
Logistic regression adjusted for age. Bold font indicates statistical significance.
In the EG, a ≥ 50% reduction in depression scores was achieved by 32.3% of participants (n=10) in the GDS and 41.9% of the participants (n=13) in BDI. None scored 0 in either scale at the end of the experiment. In the CG, only one participant (4%) had a 50% reduction in scores in both scales, and none remitted.
As an additional analysis, we tested for correlation between GDS and BDI. A significant, moderate to strong correlation was found for both groups, both at baseline and at the end of the study (CG, time point 1: p = 0.001, rho = 0.629; time point 2: p < 0.001, rho = 0.663; GE, time point 1: p < 0.001, rho = 0.731; time point 2: p < 0.001, rho = 0.696). This correlation shows evidences that the two scales corroborate the statistical analysis.
Discussion
The art therapy intervention for elderly women with stable, pharmacologically treated MDD described in this randomized, single-blind study led to improvement in depression and anxiety symptoms. This was demonstrated both on comparison of the EG versus the CG and by the response rates observed in the EG, ranging from 32.2 (GDS) to 41.9% (BDI). The intervention was a preset program of art therapy workshops consisting of a brief relaxation exercise through guided imagery, followed by artistic output and, finally, sharing of feeling and thoughts with the group and therapist. The decrease in depressive and anxiety symptoms observed after this intervention is consistent with that observed following other forms of nonpharmacological treatment, such as other types of psychotherapy with a scope similar to that of art therapy.17
The themes addressed by this art therapy intervention resemble those dealt with in other psychotherapies known to lead to improvement in depressive symptoms in the elderly,17 such as interpersonal therapy (as it stimulated social interaction in the group, as well as interaction with the therapist when patients shared their feelings and thoughts); depression management therapy (as it enabled reflection on depression-related issues, such as losses, physical disability, and solitude, correcting dysfunctional beliefs); and life review therapy (because past situations were revisited, providing the patient with the opportunity to work out these situations using expressive techniques).
Anxiety scores were reduced at the end of this study, which is in accordance with the therapeutic objective of the sessions. This finding was also reported in other studies of guided imagery.20,21 In the present intervention, guided imagery was used with the aim of helping participants relax, move their thoughts away from worries or unpleasant situations, and bring their attention to the topic of the workshop.33 Visualization of positive and pleasant images during guided imagery may also have contributed to decreasing the negative thoughts and feelings of sadness that are characteristic of depression. These results are similar to those reported in previous studies on guided imagery using projected images.22 The most unique part of the model proposed in this study – artistic making through art therapy sessions – stimulated and increased the possibility of observation and revaluation of patients’ feelings, values, and even attitudes. This is possible especially because, during artistic output, emotions and feelings are concretized through art, becoming more active than rational thoughts. This can promote insight, leading to changes in how a given situation or problem is viewed by the patient; this, in turn, may have contributed to a reduction in anxiety and depressive symptoms.
Searching for the meaning of life is a coping strategy during stressful events, which are numerous during old age and are worsened by awareness of the approach and inexorability of death.34 In the art therapy intervention used herein, themes such as the finiteness of existence, fear of death and disease, and solitude were addressed nonverbally. The benefit of this approach is that patients can become aware of these issues without having to tackle them rationally and defensively. Artworks can represent the concretization of emotions, enabling the patient to gain insight into problems that can then be changed, which is the main objective of psychotherapy. Art therapy can allow the individual to enter a plastic, expressive universe that is different from her daily routine, facilitating new perceptions. Patients are encouraged to share this process with the art therapist, who sees, listens, and supports the patient, making transformation of the patient’s reality possible.
Improvement in depressive and anxiety symptoms was also reported in a meta-analysis of art therapy for patients with breast cancer.35 Even though depression and anxiety were probably effects of the disease itself and not the primary issue in this meta-analysis, it may be inferred that both patients with cancer and those with MDD may benefit from art therapy, given the fact that the two disorders have common precipitating or perpetuating factors.
The results of the GDS corroborate the results of the BDI scale, with a significant, moderate to strong correlation for both groups. The GDS has been validated for the study of depression in the elderly,26,27 and the BDI28 is widely used for adults. The advantages of the BDI are its more comprehensive coverage of several aspects of depression and the wider range of scores (up to 63 points instead of 15 in the GDS), which may make the BDI more appropriate to measure slight changes. The fact that it is widely used worldwide also makes comparison between studies easier. Therefore, both scales seem adequate to evaluate depression and its treatment in older adults.
To create a more homogenous group, recruitment was restricted to female participants. The literature shows that depression is more prevalent and often more chronic and recurrent in women than in men.1,2 Besides, women are generally more likely to seek healthcare; among the elderly, women are more socially active than men,6,36 and may therefore adhere better to treatment. The age group chosen in the study (60 years or older) also has particular characteristics, such as greater social difficulties, increased risk of several diseases, faster loss of function, and greater risk of depression.3-5,7,8
The use of group sessions made it possible to increase the number of people seen by the therapist, enabled the exchange of experiences among the participants, and allowed mediation of interpersonal relationships by the therapist, which decreased social isolation (a possible consequence of depression). This important benefit of group psychotherapy has also been reported in other studies.5,9
The duration of psychotherapy is an important issue, and has been considered in many studies. As the objective of the present study was to test art therapy as an adjunct to pharmacotherapy for treatment of MDD, a duration of 20 sessions was chosen, as it enables a better grasp of the concepts and establishment of well-being. In previous studies of art therapy, at least 12 sessions were recommended for treatment of depression and anxiety symptoms.35 A systematic review and meta-analysis of psychosocial interventions for depression in elderly patients found more positive results with at least 3 months of therapy.37
Although the main characteristic of art therapy is its use of expressive resources, verbal communication was also favored in this study. An artwork that mirrors the individual, and about which she may talk, is an important communication facilitator between the patient, the therapist and, in this case, the group. Nevertheless, a systematic review and meta-analysis suggested that, as art therapy interventions are powerful techniques for psychic mobilization, some painful or distressing contents may surface to the conscious mind. Thus, art therapy sessions should be conducted carefully by the therapist, who must pay close attention to the emotional status of the patients.35
EG participants experienced improvement in GDS, BDI, and BAI scores, which were the focus of the intervention. The EG also showed significant improvement in cognition, as assessed by the MMSE and Rey DR. One factor that might have contributed to this improvement in cognition is stimulation through artistic making, as well as the therapeutic process of art therapy itself and the improvement in mood. However, on comparison with the CG, the improvement in cognition disappears. Several explanations for this are possible. One factor is the relatively small sample size; moreover, a nonsignificant improvement was also found in the CG, perhaps because of a learning effect regarding the test tasks. CG participants showed only a slight improvement in BDI without receiving any intervention. The reason for this improvement cannot be stated; perhaps the fact that these participants received some care (through the application of tests) influenced this reduction in symptoms. Therefore, no cognitive improvement was observed in the present study. These findings contradict those of a pilot study that investigated the efficacy of 12 art therapy sessions in improving cognitive performance.38 One possible explanation is that, in this pilot study, cognitive aspects were better explored during the sessions, whereas the main focus of the art therapy intervention described herein was emotional improvement rather than cognitive aspects, such as memory and executive functions. Future studies could better explore this important issue.
The present intervention included high-income, highly educated elderly patients and low-income women with few years of schooling in the same group. This heterogeneity did not seem to have any negative impact on understanding, participation, or involvement in the study intervention. It should be emphasized that artistic ability is not a requirement for participation in art therapy sessions. Therefore, the applicability of art therapy in different situations, contexts, and populations, as well as its cost-effectiveness, are also relevant aspects to be explored in future studies.39 Research on art therapy is still incipient, especially in the field of medicine, where quantitative validation is in high demand. Furthermore, the term “art therapy” is somewhat imprecise, as “art” refers to visual art and “art as therapy” is related to a broader category that includes music, dance, and drama therapy as well.40 It bears stressing that, given the heterogeneity of approaches, expressive techniques, and ways in which workshops are conducted by art therapists, leading to a wide range of strategies, concepts, and modalities, it is difficult to compare studies and assess the overall effects of art therapy.35
This study has several limitations. The integration of a brief relaxation and guided imagery step during the art therapy sessions, in addition to artistic production per se, means we cannot know which component was responsible for the effects observed. Another limitation was the duration of the intervention, as patients abandoned treatment in both groups. Only two patients dropped out of the EG, but in the no-intervention CG, eight patients abandoned the study. It is also important to consider the size and quality of the sample. Recruitment was limited to elderly women living in the city of São Paulo, and, although the group showed heterogeneous socioeconomic and cultural characteristics, it was not representative of the Brazilian elderly female population. The fact that only women participated in this study means that entirely different results may be observed in a study of male participants alone or of both genders. A sham therapy would also be of great value. However, the number of patients recruited was relatively small; the addition of a sham group would have diluted the sample even further. The absence of a multiple-baseline design is also a limitation, because it precludes assessment of whether the positive effects of art therapy were long-lasting.
The type of intervention itself is also a limitation. The workshops and the technique of relaxation with guided imagery, although described in detail, may be carried out differently by another art therapist, with different results. Another limitation of the study was the fact that different antidepressants were used by the participants, even though allocation was random and all participants’ medication regimens remained unchanged during the experiment. In our sample, medication was well tolerated, as no major cognitive side effect was seen according to the cognitive tests. Future studies could better explore if, for instance, antidepressants with superior neurotropic or cognitive-enhancing effects could lead to better responses to therapy.
Additional studies of art therapy may be carried out to discuss impact on quality of life, well-being, and decreasing obsessive reminiscences, as has been done with other psychotherapeutic interventions.6 Finally, it is important that other well-designed, quantitative studies be conducted before art therapy can be indicated as an adjunctive healthcare service.
In conclusion, despite some limitations, the present study contributes to the recognition of art therapy as an adjunct to pharmacotherapy in improving depressive symptoms in patients with MDD. The intervention model used art therapy and relaxation through guided imagery – three approaches have great potential to modify mental states – to enhance the possibility of transforming the patient’s world view and to enable resignification of past events. Furthermore, while most research on art therapy has been qualitative, this study provides quantitative information on the effects of this modality.
Disclosure
The authors report no conflicts of interest.
References
- 1.Taylor WD. Clinical practice. Depression in the elderly. N Engl J Med. 2014;371:1228–36. doi: 10.1056/NEJMcp1402180. [DOI] [PubMed] [Google Scholar]
- 2.Park M, Unützer J. Geriatric depression in primary care. Psychiatr Clin North Am. 2011;34:469–87. doi: 10.1016/j.psc.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andreescu C, Reynolds CF., 3rd Late-life depression: evidence-based treatment and promising new directions for research and clinical practice. Psychiatr Clin North Am. 2001;34:335–55. doi: 10.1016/j.psc.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper C, Katona C, Lyketsos K, Blazer D, Brodaty H, Rabins P, et al. A systematic review of treatments for refractory depression in older people. Am J Psychiatry. 2011;168:681–8. doi: 10.1176/appi.ajp.2011.10081165. [DOI] [PubMed] [Google Scholar]
- 5.Kiosses DN, Leon AC, Aréan PA. Psychosocial interventions for late-life major depression: evidence-based treatments, predictors of treatment outcomes, and moderators of treatment effects. Psychiatr Clin North Am. 2011;34:377–401. doi: 10.1016/j.psc.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gameiro GR, Minguini IP, Alves TCTF. The role of stress and life events in the onset of depression in the elderly. Rev Med (São Paulo). 2014;93:31–40. [Google Scholar]
- 7.Diniz BS, Nunes PV, Machado-Vieira R, Forlenza OV. Current pharmacological approaches and perspectives in the treatment of geriatric mood disorders. Curr Opin Psychiatry. 2011;24:473–7. doi: 10.1097/YCO.0b013e32834bb9bd. [DOI] [PubMed] [Google Scholar]
- 8.Samad Z, Brealey S, Gilbody S. The effectiveness of behavioural therapy for the treatment of depression in older adults: a meta-analysis. Int J Geriatr Psychiatry. 2011;26:1211–20. doi: 10.1002/gps.2680. [DOI] [PubMed] [Google Scholar]
- 9.Cuijipers P. Psychotherapies for adult depression: recent developments. Curr Opin Psychiatry. 2015;28:24–9. doi: 10.1097/YCO.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 10.Guidi J, Tomba E, Fava GA. The sequential integration of pharmacotherapy and psychotherapy in the treatment of major depressive disorder: a meta-analysis of the sequential model and a critical review of the literature. Am J Psychiatry. 2016;173:128–37. doi: 10.1176/appi.ajp.2015.15040476. [DOI] [PubMed] [Google Scholar]
- 11.Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009;66:1332–40. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 12.Aréan PA, Raue P, Mackin RS, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. Am J Psychiatry. 2010;167:1391–8. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinquart M, Forstmeier S. Effects of reminiscence interventions on psychosocial outcomes: a meta-analysis. Aging Ment Health. 2012;16:541–58. doi: 10.1080/13607863.2011.651434. [DOI] [PubMed] [Google Scholar]
- 14.Yassuda MS, Nunes PV. Innovative psychosocial approaches in old age psychiatry. Curr Opin Psychiatry. 2009;22:527–31. doi: 10.1097/YCO.0b013e3283304128. [DOI] [PubMed] [Google Scholar]
- 15.Bungay H, Clift S. Arts on prescription: a review of practice in the U.K. Perspect Public Health. 2010;130:277–81. doi: 10.1177/1757913910384050. [DOI] [PubMed] [Google Scholar]
- 16.Uttley L, Scope A, Stevenson M, Rawdin A, Taylor Buck E, Sutton A, et al. Systematic review and economic modelling of the clinical effectiveness and cost-effectiveness of art therapy among people with non-psychotic mental health disorders. Health Technol Assess. 2015;19:1–120. doi: 10.3310/hta19180. v-vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reynolds CF., 3rd Prevention of depressive disorders: a brave new world. Depress Anxiety. 2009;26:1062–5. doi: 10.1002/da.20644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Öster I, Svensk AC, Magnusson E, Thyme KE, Sjõdin M, Aström S, et al. Art therapy improves coping resources: a randomized, controlled study among women with breast cancer. Palliat Support Care. 2006;4:57–64. doi: 10.1017/s147895150606007x. [DOI] [PubMed] [Google Scholar]
- 19.Puig A, Lee SM, Goodwin L, Sherrard PAD. The efficacy of creative arts therapies to enhance emotional expression, spirituality, and psychological well-being of newly diagnosed stage I and stage II breast cancer patients: a preliminary study. Arts Psychother. 2006;33:218–28. [Google Scholar]
- 20.Leão ER, Silva MJP. Música e dor crônica musculoesquelética: o potencial evocativo de imagens mentais. Rev Latinoam Enferm. 2004;12:235–41. doi: 10.1590/s0104-11692004000200013. [DOI] [PubMed] [Google Scholar]
- 21.Apóstolo JLA, Kolkaba K. The effects of guided imagery on comfort, depression, anxiety, and stress of psychiatric inpatients with depressive disorders. Arch Psychiatr Nurs. 2009;23:403–11. doi: 10.1016/j.apnu.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Skeie TM, Skeie S, Stiles TC. The effectiveness of pleasant imagery and a distraction task as coping strategies in alleviating experimentally induced dysphoric mood. Cogn Behav Ther. 2010;18:31–42. [Google Scholar]
- 23.Associação Americana de Psiquiatria . Manual Diagnóstico e Estatístico de Transtornos Mentais, 5a edição (DSM-5). Porto Alegre: Artmed; 2014. [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Brucki SM, Nitrini R, Caramelli P, Bertolucci PH, Okamoto IH. [Suggestions for utilization of the mini-mental state examination in Brazil]. Arq Neuropsiquiatr. 2003;61:777–81. doi: 10.1590/s0004-282x2003000500014. [DOI] [PubMed] [Google Scholar]
- 26.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 27.Almeida OP, Almeida SA. [Reliability of the Brazilian version of the ++abbreviated form of Geriatric Depression Scale (GDS) short form]. Arq Neuropsiquiatr. 1998;57:421–6. doi: 10.1590/s0004-282x1999000300013. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA. Manual for the revised Beck depression inventory. San Antonio: Psychological Corporation; 1987. [Google Scholar]
- 29.Beck AT, Steer RA. Manual for the Beck anxiety inventory. San Antonio: Psychological Corporation; 1990. [Google Scholar]
- 30.Newcombe F. Missile wounds of the brain: a study of psychological deficits. Oxford: Oxford University; 1969. [Google Scholar]
- 31.Army Individual Test Battery . Manual of directions and scoring. Washington: War Department, Adjutant General's Office; 1944. [Google Scholar]
- 32.Rey A. L’examen clinique en psychologie. Paris: Universitaire de France; 1958. [Google Scholar]
- 33.Holmes EA, Mathews A. Mental imagery in emotion and emotional disorders. Clin Psychol Rev. 2010;30:349–62. doi: 10.1016/j.cpr.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 34.Pompili M, Innamorati M, Di Vittorio C, Sher L, Girardi P, Amore M. Sociodemographic and clinical differences between suicide ideators and attempters: a study of mood disordered patients 50 years and older. Suicide Life Threat Behav. 2014;44:34–45. doi: 10.1111/sltb.12051. [DOI] [PubMed] [Google Scholar]
- 35.Boehm K, Cramer H, Staroszynski T, Ostermann T. Arts therapies for anxiety, depression, and quality of life in breast cancer patients: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2014;2014:103297. doi: 10.1155/2014/103297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pledger MJ, Cumming JN, Burnette M. Health service use amongst users of complementary and alternative medicine. N Z Med J. 2010;123:26–35. [PubMed] [Google Scholar]
- 37.Forsman AK, Nordmyr J, Wahlebecck K. Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promot Int. 2011;26:i85–107. doi: 10.1093/heapro/dar074. [DOI] [PubMed] [Google Scholar]
- 38.Alders A, Levine-Madori L. The effect of art therapy on cognitive performance of Hispanic/Latino older adults. Art Ther (Alex). 2010;27:127–35. [Google Scholar]
- 39.Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376:2086–95. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wood MJ, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the management of symptoms in adults with cancer? A systematic review. Psychooncology. 2011;20:135–45. doi: 10.1002/pon.1722. [DOI] [PubMed] [Google Scholar]