Abstract
Large proportions of patients are edentulous and wear removable dentures leading to reduced functional comfort and less oral health‐related quality of life. Satisfaction with the oral situation after implantation depends on the outcome in eating comfort, speech comfort and aesthetics. Modification in form and location of the teeth may affect speech. The aim of this study is to determine speech, oromyofunctional behaviour, satisfaction with the treatment and the impact on quality of life of the horse‐shoe overdenture retained by mini‐dental implants (MDIs) in the maxilla. This prospective multicentre cohort study included 32 patients for treatment. 5 to 6 implants were placed, traumatically piercing the mucosa. Patients were evaluated three times during treatment (pre‐operatively with conventional prosthesis including full palatal coverage (CD), post‐operatively with provisionally relined CD and with horse‐shoe overdenture on MDI). The assessment included a phonetic evaluation, examination of oromyofunctional behaviour, evaluation of the impact on quality of life (OHIP‐14) and a rating of satisfaction with the treatment and speech on a visual analogue scale. Several speech sounds are found to be disturbed before treatment. In the next two stages of the treatment, the number of speech issues decreases. In the final stage, ten people show minor speech problems, especially with the /s/ sound. In this stage, seven people still present with oromyofunctional problems, especially whistling problems. In this last stage, people are very satisfied with the treatment (83%) and with speech (84%). The impact on quality of life is low (8.23/56).
Keywords: adults, dental implants, edentulism, oromyofunction, prosthodontics, quality of life, speech
1. INTRODUCTION
Speech is a part of a larger system called communication. In this study, we focused on the part of speech called articulation. Articulation involves the movement of the speech production mechanism, the so‐called articulators (eg the jaw, lips, tongue and the soft palate). This mechanism moulds the air stream, coming from the lungs, against the other structures in the mouth (alveolar ridge, hard palate and teeth) or narrows the airstream, resulting in high pitched sounds. Speech sounds are characterised by the way the speech structures are positioned.1 In the study of articulation disorders, different causes of deviant speech are known. There are two main categories in articulation problems. Firstly, functional problems caused by a wrong use of the articulatory muscles. Secondly, organic problems which appear due to changes of the structures responsible for articulation.1 Hence, it is obvious that modifications in the form and location of teeth, as is the case with tooth loss, denture wearing or tooth rehabilitations, may affect speech. Life expectancy is rising and provided that oral hygiene measures are applied properly, patients will keep their natural teeth longer and functional. However, large proportions of patients are edentulous and wear removable dentures leading to reduced functional comfort and less oral health‐related quality of life.2 Lack of stability and retention as well as decreased chewing ability is the most prevalent patient complaint.3 Moreover, long time removable denture wearing induces further bone resorption and decreases functionality of the denture. Dental implants are useful in the improvement of denture retention, and the overdenture on two implants in the lower jaw has been suggested as the minimal standard of care.4 Long‐term implant survival for dentures is in the order of 93% to 97%.5 For the majority of the edentulous patients, a 2‐4 mandibular implant overdenture provides a satisfying treatment solution with 95% implant survival after 10 years.6 Treatment with conventional dental implants of at least 3.5 mm diameter is the most common way to anchor a dental prosthesis.7 However, some patients present with an advanced resorption of their jawbone, whereby regular dental implants cannot be placed due to limitations in bone morphology. In those cases, often invasive reconstructive bone regenerative procedures are required with higher costs, more morbidity and higher barrier for treatment as compared to conventional implant placement.8, 9 Furthermore, ageing edentulous patients are often medically compromised and benefit more from minimally invasive surgery. In the light of this evolution, one piece mini‐dental implants (MDIs) with diameter less than or equal to 2.5 mm should be considered as an alternative treatment solution for improved denture retention.10, 11
Treatment with MDI is introduced early 2000, and in general, its outcome is promising although the clinical outcome defined by implant survival, bone stability or complications is often underreported especially in the upper jaw. Literature on treatment outcome related to implant survival, load resistance and quality of life is scarce. Also, the effect of this treatment on people's speech is lacking.10 The latter has been investigated mainly using regular diameter implant‐supported overdentures in mandible12, 13 and fixed dentures in the mandible12, 13, 14, 15 and maxilla,12, 14, 16, 17 as well as single tooth replacements.18 A frequently heard complaint is the occurrence of distortions of the /s/ sound during speech.7, 12, 13, 14, 15, 16, 17, 18, 19 One of the causes of deviations in the pronunciation of the /s/ sound is the angle of the frontal teeth.20 Changes in thickness of the ridge and the palate of the prosthesis are also found to be an important factor in the occurrence of speech problems in patients treated with fixed rehabilitation.21, 22 Because the production of most consonants involves speech structures in the upper jaw (palate, upper incisors), it is to expect that speech problems are more likely to occur when people are treated with reconstructions in the maxilla compared to reconstructions in the mandible.19 It is also possible that other problems present depending on which jaw is treated. As suggested in the research of Jacobs et al (2001), there are especially problems with the fricatives (s and z) in fixed rehabilitation of the maxilla and fixed reconstruction in the mandibula seems to cause more problems with the plosives (t and d).12 Figure 1 shows the tongue contact position with the palate forming the speech sounds. This palate is covered differently with conventional dentures compared to an overdenture with horse‐shoe design. It is plausible to say that different shapes of dentures (eg with and without palatal coverage) can cause other distortions especially in the maxilla.
Figure 1.
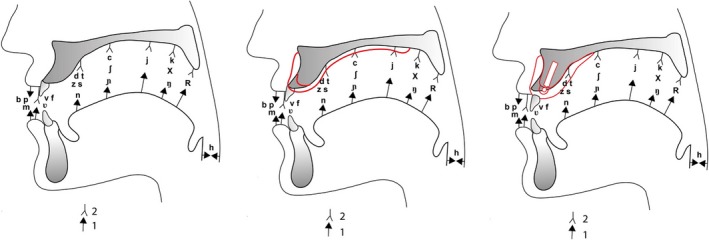
Sagittal view on the oral cavity with contact spots of the tongue (1) to the palate (2) with normal dentition (left), conventional denture (middle) and horse‐shoe overdenture on MDI (right)
Van Lierde et al examined the difference in articulation problems in different kinds of fixed dental rehabilitation in the maxilla and found a significant difference between articulation in people who have different kinds of dental rehabilitation. Most problems were observed in fixed rehabilitation on implants followed by conventional dentures, and the least problems were seen in rehabilitation with single implants. All groups had normal oromyofunctional behaviour and reported mostly problems with the /s/ sound.15 Additionally, clinical experience shows that dental implants placed in a resorbed alveolar processes are often mispositioned due to the resorption of the crest in palatal direction. Because of that, overdentures can have to wide bucco‐lingual volumes, causing obstruction of the tongue during speech or movement. The study of Collaert et al states that it is possible that removing some of the volume of the denture on the palatal side of the premolar region can solve this problem. In their study, ten edentulous patients who received fixed prosthesis in the maxilla were examined for speech problems at four occasions with proper adaptation. They found that in some patients, the /s/ sound seemed distorted, even after adaptation. After reduction of the volume of the premolar region of the denture, all patients returned to baseline speech or improved speech.23 The most common distorted sounds are the /s/, /z/, /ʃ/ (as in show), /ʒ/ (as in garage) and /t/.
Research on oromyofunctional behaviour does not report severe problems in implant treatment of any kind.14, 15, 17, 24 Research of Molly et al showed an increase of tongue thrust in patients receiving fixed dentures in the maxilla. This is the frontal position of the tongue during rest and swallowing. This could be affected by the conversion of a palate covering denture to an implant prosthesis without palatal coverage.
There has been a lot of research about patients satisfaction after dental rehabilitation.25 In general, patients are more satisfied when rehabilitated with single crowns compared to fixed dentures on implants or removable implant retained overdentures.15 Compared to fixed dentures on implants, people are more satisfied with overdentures on implants.26 Satisfaction with the oral situation after implantation depends on the outcome in eating comfort, speech comfort and aesthetics.27
Based on the aforementioned literature, one can assume that maxillary overdentures retained by mini‐implants may affect speech, especially problems with the /s/ sound, and mild problems with articulation and oromyofunction are likely to occur. It is important for dentists to inform the patients before starting the treatment that speech can be affected and a certain adaptation period including further adjustments of the prosthesis may be required.
The main object of this study is to determine speech, oromyofunctional behaviour as well as satisfaction with the treatment and the impact on quality of life in patients treated with a horse‐shoe‐shaped overdenture retained by mini‐implants in the maxilla. Changes in speech from the pre‐operative condition, with the original conventional removable denture, to the provisional denture and fixation of the horse‐shoe overdenture on the mini‐implants are assessed by a professional speech therapist, who worked independently from the clinician.
2. METHODS AND MATERIALS
2.1. Patient selection and clinical procedure
The clinical study was designed as a prospective multicentre cohort study in patients seeking treatment for poor stability and discomfort with their conventional denture. Patients were included if the following criteria were met: patients aged 50 years or older with a fully edentulous maxilla (either with or without a complete removable prosthesis); they had to be partially or fully dentate in the mandible consisting of a natural dentition, a combination of natural teeth and partial prosthesis without tooth‐supported prosthesis or an implant‐supported overdenture or fixed bridges on implants.
The study protocol was set up according to the principles of the Helsinki Declaration on clinical research (1975, revised in 2002). All patients received detailed oral and written information about the study protocol, treatment plan, financial costs, follow‐up period, and potential risks and complications. A written consent was obtained from each patient before being enrolled in the study. The study was approved by the Ethical Committee of the Ghent University Hospital on clinical research involving human beings (EC/2014/1253) and by the Ethical Committee of the General Hospital AZ ZENO Knokke‐Blankenberge.
The mini‐dental implants (MDIs) used in this study were made in one piece of a high strength pure titanium class 4 with a screw part diameter of 2.4 mm and a coronal ball attachment of 1.8 mm width (ILZ, Southern Impl. Inc). Patients were treated under local anaesthesia with free‐handed flapless surgery. This means that the surgeon is piercing the mucosa and preparing the implant bed without reflecting a mucoperiosteal flap. Pre‐operative cone beam computed tomography (CBCT) planning and adaptation of the conventional denture in a surgical guide were performed for proper implant positioning. 5 to 6 implants were inserted with the ball head of the MDI extending 3 mm to 5 mm above the mucosa. No sutures were needed, and ice packs were provided immediately after surgery. Detailed written post‐operative instructions were discussed thoroughly and given to the patient. All patients were advised to abstain from denture wearing one week post‐operatively until the denture was adapted for provisional loading. Additional space underneath the prosthesis was prepared to make room for the transmucosal implant ball head. The conventional prosthesis including the full palatal coverage was relined with Coesoft soft reliner gel (GC America). After 6 months, the final prosthetic connection with a palatal free and reinforced horse‐shoe denture was established. The prosthetic housings in the denture were imbedded by a dental laboratory to allow fixation of the denture with the ball attachments on the implants. Figure 2 shows the shape of the dentures in the different stages of the treatment.
Figure 2.
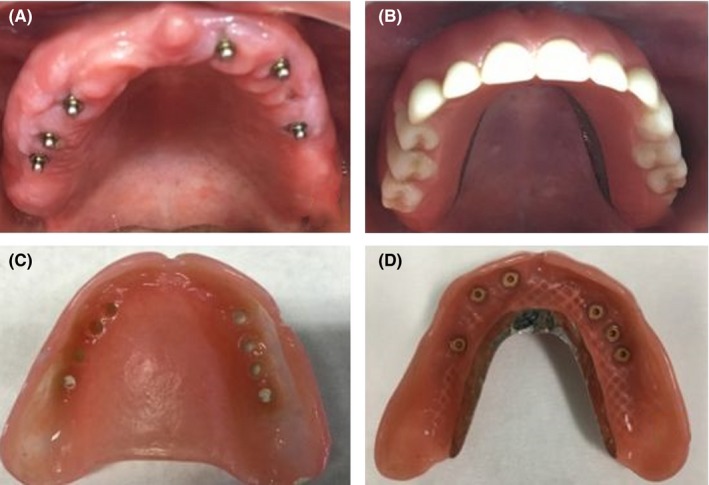
Case PM with view on the maxilla after implant surgery (A) and with horse‐shoe overdenture in the mouth (B). The provisional denture (C) and the horse‐shoe overdenture (D) are displayed
2.2. Methods
The evaluation of the subjects took place in two dental clinics (University Hospital Ghent and Cosmipolis Bruges), in a testing room separated from other practices in the clinic, and adapted for phonetic evaluation. Patients were evaluated three times during their treatment (pre‐operatively, with provisional denture after surgery and with fixed denture on MDI). Positioning of the test (the camera, test items and score form) was each time the same. The subjects were invited by the independent speech therapist. Each time an adaptation period of minimum one month was respected. The subjects were evaluated according to the methods used in the study of Van Lierde et al18 including an assessment of articulation, oromyofunctional behaviour and satisfaction. The whole test took 20 minutes.
2.2.1. Articulation
A perceptive evaluation was used to assess the articulation of the subjects. The evaluation was performed by means of a picture naming test.28 This test requires the subjects to name 135 pictures of common subjects and actions. It elicits all speech samples containing instances of all Dutch single sounds and most consonant clusters in all permissible syllable positions. The samples were recorded digitally with a video camera recorder (Sony Corporation, DCR‐SR75E). The evaluation included a phonetic inventory and phonetic analysis. A sound was considered to be present in the inventory when at least two instances of the production were found. Two speech‐language therapists (E.F and LB) firstly rated independently. In case of disagreement, the samples were replayed and discussed until a consensus was reached. Inter‐rater reliability is displayed in Table 1.
Table 1.
Articulation issues with definitions 1 assessed during the stages of the MDI maxillary overdenture treatment (pre‐operative, provisional loading and final connection). The level of significance according to the paired t test and the McNemar test
| Definition | Interexaminer reliability % | Pre‐operative (n1 + n2/ntot) | Provisional loading (n1 + n2/ntot) | Final connection (n1 + n2/ntot) |
Level of significance between Pre‐operative and provisional P‐value |
Level of significance between provisional and final P‐value |
Level of significance between pre‐operative and final P‐value |
|
|---|---|---|---|---|---|---|---|---|
| /s/ stridens (1) + /s/ simplex (2) | Phonetic disorder of the s sound accompanied with a whistle sound (1) + with insufficient frication (2) | 85 | 10 + 4/30 | 6 + 5/26 | 8 + 1/25 | 1 | 1 | 0.727 |
| Small jaw opening | 81 | 4/30 | 4/26 | 1/25 | 1 | 0.250 | 0.500 | |
| /z/ stridens (1) + /z/ simplex (2) | Phonetic disorder of the z sound accompanied with a whistle sound (1) + with insufficient frication | 96 | 4 + 0/30 | 1 + 1/26 | 3 + 0/25 | 1 | 1 | 1 |
| /t/ interdental (1) + /t/ addental (2) | The t sound with the tongue tip between de central incisors (1) + against the central incisors (2) | 71 | 1 + 2/30 | 1 + 1/26 | 0 + 2/25 | 1 | 1 | 1 |
| /n/ interdental | The n sound with the tongue tip between the central incisors | 100 | 1/30 | 0/26 | 0/25 | 1 | 1 | 1 |
| /l/ interdental | The l sound with the tongue tip between the central incisors | 49 | 1/30 | 0/26 | 0/25 | 1 | 1 | 1 |
| /ʃ/ stridens (1) + /ʃ/ simplex (2) | Phonetic disorder of the ʃ sound (as in show) accompanied with a whistle sound (1) + with insufficient frication (2) | 78 | 3 + 0/30 | 0 + 1/26 | 0 + 0/25 | 0.625 | 1 | 0.500 |
| /ʒ/ stridens (1) + /ʒ/ simplex (2) | Phonetic disorder of the ʒ sound (as in garage) accompanied with a whistle sound (1) + with insufficient frication (2) | 100 | 1 + 1/30 | 0 + 1/26 | 0 + 0/25 | 1 | 1 | 0.500 |
| Number of speech issues per person |
Mean 1 [0‐4] |
Mean 0.78 [0‐4] |
Mean 0.65 [0‐2] |
Mean dif. 0.222 [−0.207;0.652] P = 0.297 |
Mean dif. 0.292 [−0.198;0.782] P = 0.231 |
Mean dif. 0.385 [−0.012;0.782] P = 0.057 |
2.2.2. Oromyofunctional behaviour
The oromyofunctional behaviour was examined by means of the protocol of Lembrechts et al.29 Patients were asked to perform certain tasks with their oral muscles. This protocol contains an evaluation of the tongue function (tongue position at rest, tongue protrusion, tongue retraction, tongue lifting against the upper lip, tongue lifting against the lower lip, lateral movements of the tongue, click one's tongue), jaw movement (lateral movement of the jaw, jaw opening), lip movement (lip position at rest, lip closure, dispersion of the corners of the mouth, lip protrusion, lip strength), facial muscles, spontaneous mime and integrated movements (blowing, sucking, whistling). Swallowing water and saliva were observed to evaluate the tongue position and muscle tension of the lip during swallowing. The oromyofunctional behaviour was measured and video recorded as proposed in the protocol. A three‐point rating scale was used for function (0 = normal, 1 = disturbed and 2 = impossible). At last, the presence of the following oromyofunctional disorders was verified with a questionnaire: presence of sucking habits, mouth breathing, lip incompetence, slavering, nail biting and bruxism.
2.2.3. Satisfaction and quality of life
To measure the oral health‐related quality of life, the Dutch version of the shortened Oral Health Impact Profile (OHIP‐14)30 was used. This questionnaire consists of 14 items divided into 7 domains being: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. We used one question of the domain ‘functional limitation’ (Have you had trouble pronouncing any words because of problems with your teeth, mouth, dentures or jaw?) to determine the impact of the prosthesis on speech. The items were rated by a Likert scale ranging from 0 (no discomfort) to 4 (high discomfort). A total OHIP‐14 score is assessed by counting the scores of the 14 individuals questions. A score of 56/56 is indicative for maximal negative appreciation and 0/56 indicates that there are no issues at all. Subjects were also asked to rate overall satisfaction with their oral health and the satisfaction with their speech on a visual analogue scale of 10 cm (VAS) with on the end of the scale reflecting 100% maximal satisfaction and the other end of the scale corresponding 0% to complete dissatisfaction. To minimise bias, the patients were asked to fill in the questionnaires prior to the speech assessment and prior to the clinical assessment of the dental situation.
2.3. Statistical analysis
To compare the changes between the different stages of the treatment, a paired sample t test and a McNemar test were used. We estimated interexaminer reliability using Cohen's Kappa. All levels of significance were set at P = 0.05. For the analysis of the data, SPSS statistics 25 (IBM SPSS Statistics for Windows, Version 25.0; IBM Corp) was used.
3. RESULTS
3.1. Subjects
From 40 consecutively referred patients, 32 signed the informed consent to participate. One patient refused speech assessment by the independent speech therapist and the other patient could not speak due to neurological problems. Finally, 30 patients were enrolled in the treatment protocol: 13 females and 17 males with a mean age of 62.6 (SD 9.0). All participants were native speakers of Dutch. In total, 10% (3/30) reported hearing problems, 13.3% (4/30) reported open mouth breathing, 10% (3/30) reported bruxism, 6.7% (2/30) reported swallowing problems and 10% (3/30) reported drooling. A treatment of the edentulous maxilla with complete horse‐shoe overdentures on MDIs was performed in this group.
30 patients’ records are available pre‐operatively, and records of 26 patients with the provisional fixation of the denture on MDI and 25 patients were examined with their final overdenture. Dropout is related to time issues and logistic issues.
All measurements were performed after an adaptation period of minimum one month and after minimal prosthetic corrections were finalised.
3.2. Articulation profile
Table 1 shows the results of the perceptual evaluation of speech by the speech therapist in the pre‐operative condition, with provisional fixation of the denture on the MDIs and with the final overdenture.
The sounds /s/, /z/, /t/, /n/, /l/, /ʃ/ and /ʒ/ are found to be disturbed before treatment in some participants. The most frequently disturbed sound is the /s/. These speech problems consisted of sigmatismus simplex (production of the /s/ sound with insufficient frication), sigmatismus stridens (production of the /s/ with a whistle), disturbed /ʃ/ (as in the word ‘show’) and the /Ӡ/ (as in the word ‘garage’) and an addental and interdental production of the /t/, /n/ and /l/ (resp. production of the tongue against and between the central incisors). Some people showed a small jaw opening during speech, as if they were mumbling. After insertion of the implants, the provisional denture with palatal coverage was adapted with soft tissue reliner. This temporary adaptation of the denture provides better retention but does not change the external shape. A decrease in speech problems was observed. Still a large percentage of the participants show problems in pronouncing the /s/ sound (either sigmatismus simplex of stridens). There is a decrease in number of problems with the apico‐dental speech sounds (/t/, /n/ and /l/). In this stage, we can conclude that mostly the fricative sounds (/s/, /z/, /ʃ/ and /ʒ/) are difficult to pronounce.
The final horse‐shoe denture is connected to the implants a few months later. At that moment, the palatal coverage was removed. After an average adaptation period 4 months, there is again a decrease in speech problems. In this final stage, still ten people show minor speech problems. Nine of them have problems with the /s/ sound (mostly sigmatismus stridens) in combination with a deviant /z/ sound or in one case small jaw opening during speech. One patient presents with a sigmatismus simplex. One other participant only presents an addental /t/.
3.3. Oromyofunction
Table 2 shows the results of the evaluation of oromyofunctional behaviour before and during the procedure. Overall, there are only 5 functions of the 25 functions evaluated as deviant. In the pre‐operative condition, the participants present with immobility of the jaw (the lateral movement of the mandible is deprived), problems with clicking of the tongue against the palate, problems with whistling and tongue thrust during swallowing. With the provisional denture after insertion of the implants, patients still present with whistling problems, problems with clicking of the tongue against the palate and immobility of the jaw. With the implant connected horse‐shoe denture, seven people still present with whistling problems, one participant still has problems with clicking the tongue against the palate, but two people present with the problem of lifting the tongue to the upper lip. This latter occurred in the last stage after insertion of the final prosthesis.
Table 2.
Problems with oromyofunctional behaviour assessed during the stages of the MDI maxillary overdenture treatment (pre‐operative, provisional loading and final connection). The level of significance according to the paired t test and the McNemar test
| Pre‐operative (n) | Provisional loading (n) | Final connection (n) |
Level of significance between Pre‐operative and provisional P‐value |
Level of significance between provisional and final P‐value |
Level of significance between pre‐operative and final P‐value |
|
|---|---|---|---|---|---|---|
| Immobility of the jaw | 4/30 | 2/26 | 0/25 | 0.500 | 0.500 | 0.250 |
| Problems with clicking of the tongue | 6/30 | 4/26 | 1/25 | 1 | 0.375 | 0.125 |
| Whistling problems | 11/30 | 15/26 | 7/25 | 0.180 | 0.039 | 1 |
| Tongue thrust during swallowing | 1/30 | 0/26 | 0/25 | 1 | 1 | 1 |
| Tongue lift problems | 0/30) | 0/26 | 2/25 | 1 | 0.500 | 1 |
| Number of issues per person |
Mean 1.07 [0‐3] |
Mean 1.15 [0‐3] |
Mean 0.65 [0‐2] |
Mean dif. −0.074 [−0.363;0.215] P = 0.602 |
Mean dif. 0.417 [−0.013;0.847] P = 0.057 |
Mean dif. 0.308 [0.010;0.605] P = 0.043 |
3.4. Satisfaction and quality of life
Table 3 shows the results of the satisfaction scores and the impact on quality of life, given by the participants. Overall satisfaction and impact on the oral health‐related quality of life improved with evolving treatment. Especially, the final connection to the implants showed to be of utmost importance in the treatment.
Table 3.
Total OHIP‐14 (scale 0‐56), VAS overall satisfaction (%), OHIP question 1 (%) (n) and VAS speech‐related satisfaction (%) reported during the stages of the MDI maxillary overdenture treatment (pre‐operative, provisional loading and final connection). The level of significance according to the paired t test
| Pre‐operative | Provisional loading | Final connection |
Level of significance between Pre‐operative and provisional P‐value |
Level of significance between provisional and final P‐value |
Level of significance between pre‐operative and final P‐value |
|
|---|---|---|---|---|---|---|
| Satisfaction total (VAS) (%) |
Mean 67 [41‐100] |
Mean 66 [9‐100] |
Mean 83 [50‐100] |
Mean dif. −0.002 [−0.088;0.085] P = 0.971 |
Mean dif. −0.128 [−0.217;‐0.039] P = 0.007 |
Mean dif. −0.097 [−0.199;0.005] P = 0.061 |
| OHIP‐14 total score (0‐56) |
Mean 21.97 [1‐56] |
Mean 16.93 [0‐48] |
Mean 8.23 [0‐23] |
Mean dif. 5.920 [−0.777;12.617] P = 0.081 |
Mean dif. 7.696 [2.595;12.796] P = 0.005 |
Mean dif. 12.75 [7.285;18.215] P < 0.001 |
| Satisfaction speech (VAS) (%) |
Mean 77 [41‐100] |
Mean 72 [40‐93] |
Mean 84 [58‐100] |
Mean dif. 0.036 [−0.048;0.121] P = 0.382 |
Mean dif. −0.112 [−0.177;0.046] P = 0.002 |
Mean dif. −0.038 [−0.117;0.041] P = 0.326 |
| OHIP Question 1 (n) ‘Have you had trouble pronouncing any words because of problems with your teeth, mouth, dentures, or jaw’ | ||||||
| Never | 5/29 | 9/26 | 9/25 | |||
| Hardly ever | 7/29 | 5/26 | 9/25 | |||
| Occasionally | 14/29 | 8/26 | 5/25 | |||
| Fairly often | 2/29 | 2/26 | 1/25 | |||
| Very often | 1/29) | 2/26 | 1/25 | |||
An average of total treatment satisfaction (measured by the VAS) evolved from 67% pre‐treatment to 66% with the provisional denture and finally 83% with the final loading. The satisfaction with speech (measured by the VAS) evolved from 77% pre‐treatment to 72% with the provisional loading to 84% with the final loading. The OHIP total score is rather high (21.97) pre‐operatively, and this is also reflected in the scores on the first question in the domain ‘functional limitation’. The answers to this question (‘Have you had trouble pronouncing any words because of problems with your teeth, mouth, dentures, or jaw’) reflect the impact of the denture on speech. Pre‐treatment people answered mostly with ‘occasionally’, followed by ‘hardly ever’, ‘never’, ‘fairly often’ and ‘very often’. With the provisional denture, the OHIP total score decreased as well (16.93). The scores on the first OHIP question in ‘functional limitation’ showed better results. Most people reported to ‘never’ notice an impact of their denture to their speech. The second most reported answer was ‘occasionally’ followed by ‘hardly ever’ and both ‘fairly often’ and ‘very often’. In the last stage of the treatment, the average total OHIP score decreases to 8.23. Also, participants report mostly ‘never’ to notice an impact of their denture to their speech, followed by ‘hardly ever’, ‘occasionally’ and both ‘fairly often’ and ‘very often’.
4. DISCUSSION
Speech sounds are the result of delicate interaction of the speech structures and the air stream. The air stream gets well‐adjusted by the position of the speech structures and produces the sounds we know as speech sounds. It is known that changes to these structures, as is the case in dental rehabilitation, can cause difficulties in speech production. In this study, a horse‐shoe implant overdenture design was used. The bucco‐lingual dimension of this prosthesis is slightly wider than fixed dentures to allow space for the housing of the attachment system. Pre‐treatment, patients who were unsatisfied with their removable denture came for treatment and were included in this study. Patients included in this study were referred with retention problems of their existing removable prosthesis. Hence, it is reasonable to accept that the speech therapist revealed several problems. Bothur and Garsten stated that patients’ subjective experiences of speech may vary and patients who were previously accustomed to a well‐fitted conventional denture are not presenting with many speech problems.31 However, patients with less retention of their denture present with poor speech and poor satisfaction. Their study did not describe in detail the speech problems that occurred. The speech problems reported in our study are similar, yet not completely in agreement to the ones reported in previous studies on conventional removable dentures in the maxilla. In those studies, problems with /s/, /z/, /l/ and /t/ are reported.13, 15 This difference can be due to the fact that in our study, the conventional removable dentures were inadequate and not perfect as compared to participants with well‐fitted and adapted dentures in other studies. Especially because the conventional dentures covered the palate and had unsatisfying retention, the outcome on speech, oromyofunction and satisfaction was rated negatively prior to treatment.7
After surgery, the prosthesis was adjusted and relined which resulted in less speech problems. It is understandable that the relining of the prosthesis over the implants led to this improvement of speech. The nature of those distortions is not fully understood, and it seems to be reasonable to assume that bad retention may have an impact. Especially, the modification in the palatal coverage during the treatment procedure is to be considered as an additional factor affecting speech. The relined dentures covered the palate of the participants. As seen in Figure 1, the palate is an important structure in forming several consonants. This can explain the remaining speech problems. The importance of the palate plate in conventional dentures was described before by several authors.21, 22, 32 They highlight the importance of landmarks on the palate to provide the tongue with sufficient referential information to make proper contact to mould the airstream into speech sounds32 and a strong effect of a palate coverage on speech sounds was found.21, 22 However, studies on speech with fixed dentures without palate coverage are also reporting difficulties with speech. This suggests that not all speech problems in denture wearers can only be related to the coverage of the palate.13 The remaining speech problems are, as mentioned before, similar to the ones reported in literature on conventional dentures.13, 15 Here, it is to stress that the conventional dentures in the post‐operative situation were adjusted especially with improved retention by relining of the denture. Despite that, the patients were aware of the transient period of provisionalisation of the denture a certain disappointment with the outcome can be expected.
After final connection of the denture (horse‐shoe design) to the implants, it is striking that the /s/ sound in nine of the 25 subjects is distorted. All of the nine participants who received a horse‐shoe design presented with a sigmatismus stridens. As described earlier, the difference in shape of the horse‐shoe overdenture in comparison with the conventional denture with palate plate is in many ways important to discuss. The production of speech depends on how the speech structures mould the airstream into a recognisable sound. In dental rehabilitation, these structures are replaced and/or adjusted, which may influence speech. In the transition from a conventional denture with palatal coverage (which comprises the oral space in vertical dimension) to a horse‐shoe overdenture without palatal plate (which comprises the oral space in horizontal dimension), the tongue needs to find back the proper contact places and referential points to be able to mould the airstream in the same way as before. In the majority of the participants, this was no problem, especially because a proper adaptation period was respected. Still some participants suffered from problems producing the /s/ sound. This is in agreement with previous studies on overdentures and fixed dentures in the maxilla.12, 15 It is obvious to state that the /s/ sound is the most vulnerable sound in rehabilitation of the maxilla. This was already reported by other authors.12, 13, 15, 16, 23
The oromyofunctional behaviour of the participants during treatment showed some striking findings. In comparison with primary studies, there are more problems to report.12, 14, 15 It is possible that this disagreement is due to the difference in dental rehabilitation, age of the participants and way of examination. In our study, whistling seems very fragile in all stages of the treatment. Pre‐operatively, participants present with the most deviant behaviours. This can be explained by the bad fit and retention of the denture. It is possible that people put a lot of effort in keeping their denture in place and therefore cannot use their oral muscles properly. After relining of the provisional denture, more retention of the denture is accomplished and some of the pre‐treatment oromyofunctional problems disappeared. But more people present with whistling problems. There is no other report of this kind of problem in previous research mainly because this function was not assessed before. The anatomical changes during whistling are not yet fully understood. We know that the air flow is directed through the pursed lips by the tongue in combination with the hard palate.33 Due to the denture, it is possible that the formation of the right position of the anatomical structures to produce the whistling sound is distorted. In the last phase of the treatment surprisingly, tongue lift problems occur in 2 patients. This phenomenon has never been reported. To lift the tongue to the upper lip, the tongue muscles extend in ventral direction, pushing the tongue base up and forward. It is possible that because of the specific shape of the overdenture, the movement of the tongue base is obstructed and lifting of the tongue to the upper lip is more difficult in some participants. This is a matter for further research.
Besides the opinion of professionals about function, it is equally important to evaluate participants’ opinion about their situation. The results obtained by the VASs showed both low ratings for total satisfaction and satisfaction with speech pre‐treatment. This can be explained by the fact that participants apply for this treatment because they are in some way dissatisfied with their situation. Literature states that eating comfort, speech comfort and aesthetics are the main causes of dissatisfaction in denture wearers.27 Surprisingly after relining of the provisional denture, the rates on the VAS slightly drop. It is possible that people expected more of this phase of the treatment or they still suffer from small complications due to the surgery.34 In the final stage, after loading with the actively retained horse‐shoe overdenture, the satisfaction rises tremendously to a level that is comparable to the ones previously reported.15, 17 In the domain ‘functional limitation’, participants rated the impact of their denture on speech. Over the different stages of the treatment, people reported less impact of their denture on speech. This is also in line with previous studies on speech.15, 17
It is worth mentioning that the strength of this study lies in the large sample size, the detailed and professional speech analysis and the longitudinal design. The limitation of this design is the dropout of the participants during the study due to organisational and logistic issues. It is known that hearing problems can affect speech production. We did not perform a hearing test before treatment but we asked the patients whether they had any hearing conditions. This subjective manner could have been less precise. It was impossible to assess the speech profile of the participants in normal conditions because they presented already with complaints about their dental situation at the start of the study. In an ideal situation, we know about possible speech problems in normal conditions, so we can detect what speech problems are due to the treatment and what problems already existed. A last limitation is the fact that only one speech therapist was blinded for time points measured when examining the videos. It is possible that the expectation of the therapist influenced the rating. Still there was a good inter‐rater reliability.
It is to highlight that despite the speech problems, assessed by the speech therapists, people are in the end very satisfied with their speech and oral situation. Therefore, it is very important to ask patients opinion about their speech and oral situation and the impact of it on their quality of life before pointing out possible problems you notice as a professional. When people give a rating about speech, it is possible that besides the sound they produce they also rate the comfort they experience while speaking. This is something speech therapists cannot assess. Hypothetically, the comfort of speaking is for non‐professional speakers more important than the way they sound. It is important to inform patients before treatment about the possible difficulties they may encounter during treatment. In the future, research should focus on the possibility to deal with patients with remaining speech problems. To avoid speech problems, it is necessary to check whether the retention of de denture is sufficient and whether the coverage of the palate is not obstructing good speech production. The shape of the denture should get as close as possible to the shape of a normal oral cave. The technique of Collaert et al applied on fixed dentures may be useful in overdentures as well. It is possible that the reduction of the volume of the resin in the premolar area can solve remaining problems, especially with the /s/ sound. It is to be examined whether the size of the implants influences the size of the prosthesis and therefore affects speech and oromyofunctional behaviour. It is possible that the reduction of the volume of the resin in overdentures on MDI is easier because the attachment structure is smaller. Besides the adjustment of the denture, it is possible that conventional speech therapy can offer a solution to the remaining speech problems.
5. CONCLUSION
Speech and oromyofunctional problems occur during all stages of the treatment. Especially, the /s/ sound and the whistling function seem very fragile and occur in all stages. The speech problems seen during the two first stages are similar, yet slightly different from the ones seen in previous studies. Especially, the introduction of the horse‐shoe overdenture on MDI seemed to be important. People are very satisfied with their oral and speech situation in this last stage, despite the fact that speech therapists detect some difficulties with the pronunciation of in particular the /s/ sound. Therefore, it is important for dentists to inform their patients that speech and oromyofunctional problems may occur during treatment, but most likely will disappear after an adaptation period.
CONFLICT OF INTEREST
Dr De Bruyn reports, on behalf of Ghent University, a research collaboration agreement with Southern Implants Inc, during the conduct of the study. He also reports on behalf of Radboud Medical Center an educational grant from Southern Implants Inc outside the submitted work.
ACKNOWLEDGMENTS
The authors wish to thank Drs. Simone Knuijt for her critical view and expertise on the part of speech therapy in this study and Ms Ann‐Sophie Deproost for her excellent skills in graphic design. It is important to mention that co‐author Dr Van Doorne Luc has contributed equally for this paper.
Fonteyne E, Van Doorne L, Becue L, Matthys C, Bronckhorst E, De Bruyn H. Speech evaluation during maxillary mini‐dental implant overdenture treatment: A prospective study. J Oral Rehabil. 2019;46:1151–1160. 10.1111/joor.12852
REFERENCES
- 1. Pena‐Brooks A, Hegde MN. Assessment and Treatment of Articulation and Phonological Disorders in Children. Texas, TX: Pro‐Ed; 2007. [Google Scholar]
- 2. Müller F, Naharro M, Carlsson GE. What are the prevalence and incidence of tooth loss in the adult and elderly population. Clin Oral Implant Res. 2007;18(3):2‐14. [DOI] [PubMed] [Google Scholar]
- 3. van Waas MA, Kalk W, van Zetten B, van Os J. Treatment results with immediate overdentures: an evaluation of 4.5 years. J Prosthet Dent. 1996;76:153‐157. [DOI] [PubMed] [Google Scholar]
- 4. Feine JS, Carlsson GE. The McGill consensus statement on overdentures: mandibular two‐implant overdentures as first choice standard of care for edentulous patients. Gerodontology. 2002;19:3‐4. [PubMed] [Google Scholar]
- 5. Hoeksema AR, Visser A, Raghoebar G, Vissinck A, Meijer H. Influence of age on clinical performance of mandibular two‐implant overdentures: a 10‐year prospective comparative study. Clin Implant Dent Relat Res. 2016;18:745‐751. [DOI] [PubMed] [Google Scholar]
- 6. Meijer H, Raghoebar G, Batenburg R, Visser A, Vissink A. Mandibular overdentures supported by two or four endosseous implants: a 10‐year clinical trial. Clin Oral Implants Res. 2009;20:722‐728. [DOI] [PubMed] [Google Scholar]
- 7. Kalk W, Slop D. De volledige gebitsprothese, uitgangspunten bij de diagnostiek en behandeling van de edentate patiënt. Alphen aan den Rijn: Samsom Stafleu; 1989. [Google Scholar]
- 8. Boven G, Meijer H, Vissink A, Raghoebar G. Reconstruction of the extremely atrophied mandible with iliac crest onlay grafts followed by two endosteal implants: a retrospective study with long‐term follow‐up. Int J Oral Maxillofac Surg. 2014;43:626‐632. [DOI] [PubMed] [Google Scholar]
- 9. Stellingsma K, Raghoebar G, Visser A, Vissink A, Meijer H. The extremely resorbed mandible, 10‐years results of a randomized controlled trial on 3 treatment strategies. Clin Oral Implant Res. 2014;25:926‐932. [DOI] [PubMed] [Google Scholar]
- 10. Lemos CA, Verri FR, Batista VE, Santiago Júnior JF, Mello CC, Pellizzer EP. Complete overdentures retained by mini implants: a systematic review. J Dent. 2017;57:4‐13. [DOI] [PubMed] [Google Scholar]
- 11. Jung RE, Al‐Nawas B, Araujo M, et al. Group 1 ITI Consensus Report: the influence of implant length and design and medications on clinical and patient‐ reported outcomes. Clin Oral Impl Res. 2018;29:69‐77. [DOI] [PubMed] [Google Scholar]
- 12. Jacobs R, Manders E, Van Looy C, Lembrechts D, Naert I, Van Steenberghe D. Evaluation of speech in patients rehabilitated with various oral implant‐supported protheses. Clin Oral Implant Res. 2001;12:167‐173. [DOI] [PubMed] [Google Scholar]
- 13. Manders E, Jacobs R, Nackaerts O, Van Looy C, Lembrechts D. The influence of oral implant‐supported prostheses on articulation and myofunction. Acta Otorhinolaryngol Belg. 2003;57:73‐77. [PubMed] [Google Scholar]
- 14. Molly L, Nackaerts O, Vandewiele K, Manders E, Van Steenberghe D, Jacobs R. Speech adaptation after treatment of full edentulism through immediate‐loaded implant protocols. Clin Oral Implant Res. 2008;19(1):86‐90. [DOI] [PubMed] [Google Scholar]
- 15. Van Lierde KM, Corthals P, Browaeys H, Mussche P, Van Kerckhove E, De Bruyn H. Comparison of speech intelligibility, articulation and oromyofunctional behaviour in subjects with single‐tooth implants, fixed implants prosthetics or conventional removable prostheses. J Oral Rehabil. 2012;39(3):285‐293. [DOI] [PubMed] [Google Scholar]
- 16. Lundqvist S, Haraldson T, Lindblad P. Speech in connection with maxillary fixed prosthesis on osseointegrated implants: a three‐year follow‐up study. Clin Oral Implant Res. 1992;3:176‐180. [DOI] [PubMed] [Google Scholar]
- 17. Van Lierde KM, Browaeys H, Corthals P, et al. Impact of fixed implant prosthetics using the ‘all‐on‐four’ treatment concept on speech intelligibility, articulation and oromyofunctional behaviour. Int J Oral Maxillofac Surg. 2012;41(12):1550‐1557. [DOI] [PubMed] [Google Scholar]
- 18. Van Lierde KM, Corthals P, Browaeys H, Mussche P, Van Kerckhove E, De Bruyn H. Impact of anterior single‐tooth implants on quality of life, articulation and oromyofunctional behaviour: a pilot study. J Oral Rehabil. 2011;38(3):170‐175. [DOI] [PubMed] [Google Scholar]
- 19. Heydecke G, McFarland DH, Feine JS, Lund JP. Speech with maxillary implant prostheses: ratings of articulation. J Dent Res. 2004;83(3):236‐240. [DOI] [PubMed] [Google Scholar]
- 20. Runte C, Lawerino M, Dirksen D, Bollmann F, Lambrecht‐Dinnesen A, Seifert E. The influence of maxillary central incisor position in complete dentures on [s] sound production. J Prosthet Dent. 2001;85(5):485‐495. [DOI] [PubMed] [Google Scholar]
- 21. Ichikawa T, Komoda J, Horiuchi M, Matsumoto N. Influence of alterations in the oral environment on speech production. J Oral Rehabil. 1995;22(4):295‐299. [DOI] [PubMed] [Google Scholar]
- 22. Petrovic A. Speech and sound distortions caused by changes in complete denture morphology. J Oral Rehabil. 1985;12(1):69‐79. [DOI] [PubMed] [Google Scholar]
- 23. Colleart B, Van Dessel J, Konings M, et al. On speech problems with fixed restorations on implants in the edentulous maxilla: introduction of a novel management concept. Clin Implant Dent Relat Res. 2015;17(2):745‐750. [DOI] [PubMed] [Google Scholar]
- 24. Sansone KM, Filho HN, Berretin‐Felix G, Braslotto AG. Oral myofunctional and vocal characteristics in subjects subjected to oral rehabilitation with osseointegrated implants. Clin Oral Implant Res. 2006;17:328‐330. [DOI] [PubMed] [Google Scholar]
- 25. De Bruyn H, Raes S, Matthys C, Cosyn J. The current use of patient‐centered/reported outcomes in implant dentistry: a systematic review. Clin Oral Implant Res. 2015;26(11):45‐56. [DOI] [PubMed] [Google Scholar]
- 26. Heydecke G, Boudrias P, Awad MA, de Albuquerque RF, Lund JP, Feine JS. Within‐subjects comparisons of maxillary fixed and removable implant prostheses: patient satisfaction and choice of prosthesis. Clin Oral Implant Res. 2003;14(1):125‐130. [DOI] [PubMed] [Google Scholar]
- 27. Dierens M, Collaert B, Deschepper E, Browaeys H, Klinge B, De Bruyn H. Patient‐centered outcome of immediately loaded implants in the rehabilitation of fully edentulous jaws. Clin Oral Implant Res. 2009;20(10):1070‐1077. [DOI] [PubMed] [Google Scholar]
- 28. Van Borsel J. Articulation in Down's syndrome adolescents and adults. Eur J Disord Commun. 1996;31:415‐444. [DOI] [PubMed] [Google Scholar]
- 29. Lembrechts D, Verschueren D, Heulens H, Valkenburg H, Feenstra L. Effect of a logopedic instruction program after adenoidectomy on open mouth posture: a single‐blind study. Folia Phoniatrica et Logopaedica. 1999;51(3):117‐123. [DOI] [PubMed] [Google Scholar]
- 30. Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11(1):3‐11. [PubMed] [Google Scholar]
- 31. Bothur S, Garsten M. Initial speech problems in patients treated with multiple zygomatic implants. Int J Oral Maxillofac Implants. 2010;25:379‐384. [PubMed] [Google Scholar]
- 32. Palmer J. Structural changes for speech improvement in complete upper denture fabrication. J Prosthet Dent. 1979;41:507‐510. [DOI] [PubMed] [Google Scholar]
- 33. Azola A, Palmer J, Mulheren R, Hofer R, Fischmeister F, Tecumseh FW. The physiology of oral whistling: a combined radiographic and MRI analysis. J Appl Physiol. 2018;124:34‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yao J, Tang H, Gao X, McGath C, Mattheos N. Patients’ expectations to dental implant: a systematic review of the literature. Health Qual Life Outcomes. 2014;12:153. [DOI] [PMC free article] [PubMed] [Google Scholar]


