Summary
Background
Autoimmune hepatitis requires long‐term therapy, and systemic corticosteroids are the backbone of therapeutic management. Prolonged use of corticosteroids may lead to adverse events but data from long‐term studies are mainly derived from studies in rheumatic diseases.
Aim
To assess cataract, diabetes and fractures in relation to corticosteroid doses in the long‐term maintenance treatment of patients with autoimmune hepatitis.
Methods
We retrospectively collected data on 476 patients (77% women) with an established diagnosis of autoimmune hepatitis. Binary logistic regression with a generalised estimating equation was used to analyse the association between current corticosteroid use and the incidence of cataract, diabetes and fractures with onset after autoimmune hepatitis diagnosis. We corrected for sex, age, cirrhosis at diagnosis and predniso(lo)ne use in the prior 3 years to account for possible ongoing effects.
Results
A total of 6634 years, with a median of 13 (range 1‐40) per patient were recorded. The median age at diagnosis was 44 years (range 2‐88). Adverse events were documented in 120 (25%) patients. Low‐dose predniso(lo)ne (0.1‐5.0 mg/d) increased the odds of fractures whereas higher doses (>5.0 mg/d) increased the odds of cataracts and diabetes. Budesonide increased the odds of cataract and fractures; this effect was independent of predniso(lo)ne use in the prior 1, 2 or 3 years.
Conclusions
Even low doses of corticosteroids frequently lead to substantial adverse events refuting the assumption that adverse events are prevented by administering low doses.
1. INTRODUCTION
Autoimmune hepatitis is a severe immune‐mediated inflammation of unknown aetiology that primarily targets hepatocytes. Treatment is aimed to prevent disease relapse, relieve symptoms and achieve full biochemical and histological normalisation in order to prevent progression to fibrosis, cirrhosis and end‐stage liver failure requiring liver transplantation. Since the introduction of prednisone, survival has improved dramatically.1 Unfortunately, most patients require life‐long immunosuppressive therapy, as relapse after cessation of therapy has been shown in up to 90% of patients.2 In early clinical trials, it was found that the addition of azathioprine decreased steroid‐related side effects and that this combination was as effective as prednisone alone. Currently, treatment regimens for autoimmune hepatitis are based on these trials and 44%‐75% of patients require a glucocorticosteroid‐based maintenance therapy, with or without azathioprine.3, 4 Up to 30% of these patients may suffer from corticosteroid‐related side effects, including diabetes, osteoporotic fractures, cataract, hypertension, cushingoid appearance and weight gain.5 Corticosteroid‐specific side effects are thought to arise in autoimmune hepatitis patients on doses exceeding 7.5‐10 mg/d predniso(lo)ne when administered over several months and it is advocated to reduce the dose below this threshold to prevent adverse events.6 However, studies on dose‐related side effects of corticosteroids supporting this assumption have predominantly been performed in rheumatic diseases, and data on the prevalence of side effects in patients with autoimmune hepatitis on long‐term corticosteroids are scarce.7
In this study, we focused on three frequently occurring and documented adverse events. We aimed to assess the incidence of cataract, diabetes and osteoporotic fractures in relation to corticosteroid doses in the long‐term maintenance treatment of patients with autoimmune hepatitis.8
2. MATERIALS AND METHODS
The registry of the Dutch Autoimmune Hepatitis Study Group contains data from autoimmune hepatitis patients, the collection of data started in 2008 and is ongoing. The cohort of this study was described in detail in a previous study.9 All patients fulfilled the revised score of the International Autoimmune Hepatitis Study Group with a probable or definite diagnosis of autoimmune hepatitis.9, 10 The study protocol (number 2008.84) was approved by the institutional review boards of all participating tertiary referral (n = 6) and general hospitals (n = 10) in the Netherlands. Medical records of 506 patients were retrospectively reviewed; 20 did not have available treatment regimen data and were excluded; 10 patients with cirrhosis at diagnosis who were prescribed budesonide during the disease course were excluded.
The clinical characteristics including adverse events and treatment regimen of 476 patients were collected for analysis. Maintenance therapy was recorded as the mean dose of medication per milligram per day over each follow‐up year. Cataracts, diabetes and fractures with an onset after the date of autoimmune hepatitis diagnosis were considered as new‐onset and registered for this study. Cataracts were defined as patients being subjected to cataract surgery or as determined by the ophthalmologist or the attending physician. Diabetes was defined as determined by the treating physician and by the requirement of initiation of treatment (diet change, oral anti‐diabetics or insulin). Fractures that occurred after the diagnosis of autoimmune hepatitis were assessed using the emergency room and surgery reports and imaging reports. Normal bone density, osteopenia and osteoporosis were defined as T‐scores above −1.0; −1 to −2.5 and −2.5 or lower respectively. Autoimmune hepatitis variants with concurrent primary biliary cholangitis (AIH‐PBC) and autoimmune hepatitis with features of primary sclerosing cholangitis (AIH‐PSC) were defined according to the current guidelines.11, 12
2.1. Statistical analysis
Normally distributed variables were described as mean with standard deviation (SD), whereas nonnormally distributed variables were described as median with range. Categorical data were described as numbers and percentages of the total. Binary logistic regression with a generalised estimating equation was used to analyse the association between the occurrence of adverse events and predictors. Adverse events which occurred before the diagnosis of autoimmune hepatitis were discarded. In the case of multiple fractures in one patient, only the date of the first fracture was used in the model. Factors that were possibly predictive of adverse events and that were available in the database, were included simultaneous in the multivariate model to provide estimates adjusted for other factors/predictors. The doses of immunosuppressive therapy and the occurrence of adverse events were analysed per patient per follow‐up year. For every year, a patient was at risk of developing an adverse event, the age in that year was used. By these means, ageing was taken into account. In addition, the effect of the predniso(lo)ne dose in the prior years was assessed. Patient‐years without the use of predniso(lo)ne or budesonide were used as reference categories. The outcome is described as an estimation of the odds ratio with its 95% CI. The level of significance (α) was set at 0.05. Statistical analyses were performed with IBM SPSS 22.0.
3. RESULTS
A total of 476 patients with a median follow‐up time of 13 years (range 1‐40) who were treated in 16 hospitals in the Netherlands were included (Table 1). Paediatric onset (<18 years) of the disease was present in 68 (14%) of the patients at a median age of 14 years. The majority (96%; n = 65) of these patients with a paediatric onset had predominantly been followed during adulthood years. Details of immunosuppressive therapy are shown in Table 2. Complete biochemical remission was achieved in 424 (90%) patients, whereas 47 (10%) patients did not. The predominantly prescribed medications were predniso(lo)ne and azathioprine. In total, 428 (90%) patients were prescribed predniso(lo)ne. Of the years that predniso(lo)ne was used in these patients, the mean daily dose was ≤ 5.0 mg (n = 96; 20%), 5.1‐10 mg (n = 272; 56%) or > 10 mg (n = 67; 14%). Budesonide was prescribed to 84 (17%) patients in mean daily doses of 0.1‐3 mg (n = 17; 4%), >3.0 mg (n = 67; 14%). A total of 367 (77%) patients had received combination therapy with both predniso(lo)ne and azathioprine, during a median time of 5 years (range 1‐29). Cirrhosis on histology was present at diagnosis in 64 (17%) of the patients and developed in another 22 (5%) patients during therapy.
Table 1.
Characteristics at diagnosis
| Autoimmune hepatitis | AIH‐PBC | AIH‐PSC | |
|---|---|---|---|
| Patients, n (%) | 406 (87) | 30 (6) | 40 (9) |
| Female, n (%) | 315 (78) | 27 (90) | 24 (60) |
| Age in years, median (range) | 46 (2‐88) | 46 (16‐70) | 31 (12‐77) |
| MELD‐score, median (range) | 10 (0‐32) | 7 (1‐22) | 8 (1‐17) |
| IgG g/L, median (range) | 26 (7‐91) | 22 (8‐59) | 22 (13‐51) |
| ALT U/L, median (range) | 513 (11‐4693) | 268 (18‐2649) | 273 (46‐2500) |
| Cirrhosis, n (%) | 57 (18) | 4 (14) | 3 (9) |
| ANA and or SMA positive, n (%) | 333 (88) | 20 (72) | 32 (91) |
| ANA positive, n (%) | 268 (74) | 13 (43) | 23 (70) |
| SMA positive, n (%) | 217 (63) | 15 (60) | 20 (59) |
Abbreviations: AIH‐PBC, autoimmune hepatitis with concomitant primary biliary cholangitis; AIH‐PSC, autoimmune hepatitis with concomitant primary sclerosing cholangitis; ALT, alanine aminotransferase; ANA, anti‐nuclear antibody; IgG, immunoglobulin G; MELD, model for end‐stage liver disease; SMA, smooth muscle antibody.
Table 2.
Treatment details of patients with autoimmune hepatitis
|
Years of medication use n (%)a |
Patients n (%) |
Years of use, median (range) | Dose mg/d median (range) | |
|---|---|---|---|---|
| Predniso(lo)ne | 3767 (57) | 429 (90) | 7 (1‐39) | 8 (1.67‐33.75) |
| Budesonide | 449 (7) | 85 (18) | 4 (1‐16) | 6 (1‐12) |
| Azathioprine | 4541 (68) | 392 (82) | 12 (1‐34) | 73 (4‐500) |
| Mycophenolate mofetil | 195 (3) | 33 (7) | 6 (1‐15) | 1000 (50‐4000) |
| Ciclosporin | 66 (1) | 11 (2) | 6 (1‐14) | 138 (13‐400) |
| Tacrolimus | 28 (0) | 6 (1) | 5 (1‐8) | 5 (0.7‐12.0) |
| Mercaptopurine | 60 (1) | 15 (3) | 2 (1‐21) | 50 (1‐100) |
| Tioguanine | 35 (1) | 9 (2) | 2 (1‐10) | 18 (3‐50) |
| Allopurinol | 39 (1) | 14 (3) | 3 (1‐6) | 100 (50‐100) |
| Ursodeoxycholic acid | 1661 (25) | 164 (34) | 11 (1‐28) | 825 (50‐1800) |
The total patient‐years was 6634.
3.1. Adverse events
In 120 (25%) patients cataract, diabetes or one or more fractures occurred after the diagnosis of autoimmune hepatitis. The effect of one additional daily milligram predniso(lo)ne or budesonide on the odds of developing any of the studied side effects, corrected for age and sex is shown in Table 3. For example, adding 1 milligram of predniso(lo)ne increased the odds of a first combined primary side effect by 8%; two additional milligrams of predniso(lo)ne would increase the odds by 17%. There was no relation between the response to treatment and the occurrence of any of the adverse events. The effects of predniso(lo)ne and budesonide doses on the odds of cataract and fracture, with and without a correction for predniso(lo)ne use in the year prior to the adverse event are shown in Figure 1.
Table 3.
Increase in odds ratio of adverse events for each additional milligram of corticosteroid dose
| Possible adverse events | Predniso(lo)ne | P value | Budesonide | P value | ||
|---|---|---|---|---|---|---|
| Odds ratio | (95% CI) | Odds ratio | (95% CI) | |||
| Combined primary adverse events | 1.08 | 1.06‐1.11 | <.001 | 1.09 | 1.00‐1.20 | .06 |
| Primary adverse event | ||||||
| Cataract | 1.06 | 1.03‐1.10 | <.001 | 1.17 | 1.02‐1.33 | .02 |
| Diabetes | 1.09 | 1.05‐1.12 | <.001 | 0.96 | 0.70‐1.30 | .78 |
| Bone fracture | 1.05 | 1.01‐1.10 | .01 | 1.14 | 1.03‐1.27 | .02 |
Generalised estimated equations, corrected for sex and age at that year.
Figure 1.
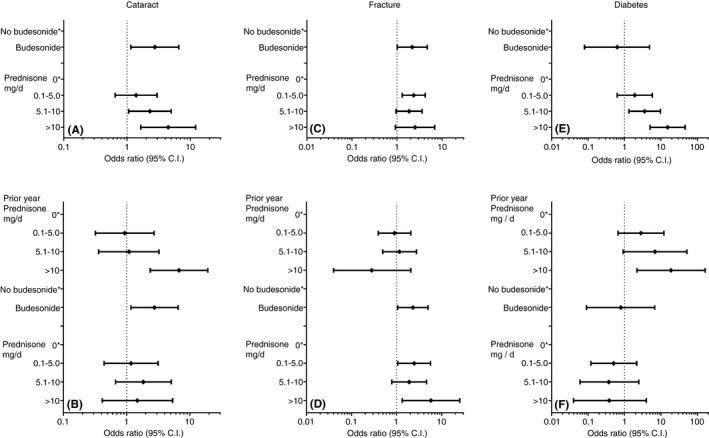
The effect of predniso(lo)ne and budesonide on the odds of cataract (panels A and B) or fracture (panels C and D) or diabetes (panels E and F). The asterisk indicates the reference category of patient‐years that no predniso(lo)ne or budesonide was used. The odds ratios of adverse events are uncorrected (panel A, C and E) or corrected for predniso(lo)ne use in the prior year (panel B, D and F)
Cataracts in either one or both eyes developed in 45 (9%) patients at a median age of 66 years (range 36‐86). In generalised estimating equations, predniso(lo)ne doses exceeding 5 mg/d increased (P = .018) the odds of cataract, corrected for budesonide use, sex and the age at that year (Figure 1, panel A). Cirrhosis did not increase the odds of cataract (OR 0.7; CI 0.6‐2.0 P = .6). The effect of predniso(lo)ne on the odds of cataract persisted for 1 year (P < .001), whereas predniso(lo)ne doses 2 years (P = .8) or 3 years (P = .2) before did not increase the odds of cataract (Figure 1, panel B). Budesonide use increased the odds of cataract (P = .023); this effect was independent (P = .021) of predniso(lo)ne use in the prior 1, 2 or 3 years.
A total of 102 fractures occurred in 69 (15%) patients, at a median age at the first fracture of 64 years (range 14‐88). Cirrhosis did not increase the odds of a fracture (OR 0.6; CI 0.3‐1.3 P = .1). Predniso(lo)ne (0.1‐5.0 mg/d) and budesonide were predictive of one or more fractures (Figure 1, panel C), corrected for sex and the age in that year. The predniso(lo)ne and budesonide‐associated increase in odds ratio persisted after correction for predniso(lo)ne use in the prior year before the fracture (Figure 1, panel D). Predniso(lo)ne use in the prior one (P = .6), two (P = .9) or three (P = .8) years did not influence the odds of a fracture. The different types of fractures that were observed include vertebral compression (n = 36; 35%), femur or hip (n = 12; 11%), pelvis (n = 1; 1%), tibia or fibula (n = 9; 9%), humerus or radius or ulna (n = 21; 20%), (meta)carpal (meta)tarsal or phalanx bones (n = 15; 15%), rib (n = 5; 5%), nasal bone (n = 1; 1%), patella (n = 1; 1%) and transverse process fractures (n = 1; 1%). Osteoporotic vertebral fractures can occur asymptomatic and slowly over time, subsequently the date of diagnosis on X‐ray can be different from the onset. Hence, a sub analysis including fractures with a preceding trauma and excluding vertebral fractures was performed. This analysis further characterised the effect of predniso(lo)ne (0.1‐5.0 mg/d), but not of budesonide (Figure S1) on nonvertebral fractures. Predniso(lo)ne use in the prior 1 (P = .5), 2 (P = .9) or 3 (P = .2) years did not influence the odds of a nonvertebral fracture. Data on bone density in patients with one or more fractures were available in 49 of 69 patients and showed a normal bone density (10%; n = 5), osteopenia (53%; n = 26) or osteoporosis (37%; n = 18). Bone density data were available in 261 of 407 patients without a fracture and showed a normal bone density (37%; n = 96), osteopenia (49%; n = 128) or osteoporosis (14%; n = 37). In 13 hospitals (n = 369 patients), data on treatment to prevent bone loss were available. Medication to prevent or treat bone loss was prescribed to 265 (72%) patients and consisted of calcium carbonate (n = 247; 67%), vitamin D (n = 210; 57%), bisphosphonate (n = 165; 45%) and denosumab (n = 3; 1%). In these 13 hospitals, all patients (n = 42) who had been diagnosed with osteoporosis and 97 of 110 patients with osteopenia have received bone protective therapy. Patients who were treated for bone loss, where not at different odds of a fracture (OR 1.3; CI 0.7 2.6 P = .3).
New‐onset diabetes developed in 46 (10%) patients at a median age of 60 years (range 29‐86). Both moderate (5.1‐10.0 mg/d) and higher (>10 mg/d) doses of predniso(lo)ne doses increased the odds of diabetes when corrected for budesonide, cirrhosis at diagnosis, age and sex (Figure 1, panel E). Eighteen of the cases with new‐onset diabetes (39%) occurred in the first year after autoimmune hepatitis diagnosis and start of treatment. In those patients with diabetes onset after more than 1 year (n = 28), previous high‐dose prednisolone exposure (>10mg/day) in the previous year was a significant predictor (P = .05, Figure 1F). The effect of predniso(lo)ne on the odds of diabetes persisted for 1 year (P = .05), whereas predniso(lo)ne doses 2 years (P = .3) or 3 years (P = .1) before did not increase the odds of diabetes (Figure 1 panel F). Only one case of new‐onset diabetes occurred in a patient using both predniso(lo)ne and budesonide in high daily doses of >10 and >3.0 mg respectively. The effect of budesonide on new‐onset diabetes could not be established.
We have performed additional analyses after excluding paediatric onset patients and found that this did not change the results for cataract and diabetes. The effect of current year predniso(lo)ne in high‐dose (>10 mg) on the odds of a fracture was slightly more pronounced in the analysis with adult onset only (OR 2.9; 1.0‐7.8).
3.2. Patients with autoimmune hepatitis variant syndromes
The odds of cataract, diabetes and fractures was similar when patients with an autoimmune hepatitis variant with primary biliary cholangitis or primary sclerosing cholangitis were excluded from analysis (data not shown). Patients with autoimmune hepatitis variants were prescribed mycophenolate mofetil more often compared with patients with autoimmune hepatitis (data not shown). No significant differences were observed in predniso(lo)ne, budesonide, azathioprine, mercaptopurine, tioguanine (thioguanine), tacrolimus and cyclosporine prescriptions, between autoimmune hepatitis and autoimmune hepatitis variant patients.
4. DISCUSSION
The results of this study re‐establish the fracture risk in patients taking corticosteroids. Here we show that in patients with autoimmune hepatitis, this fracture risk is already increased at low‐doses corticosteroid use. In addition, we show that the odds of all studied adverse events increase with corticosteroid use.
Oral predniso(lo)ne use increased the odds of all studied side effects in our cohort; cataract, diabetes and fractures. The mechanism of action of glucocorticoids via the cytosolic or membrane‐bound glucocorticoid receptor is dose‐dependent.13 Likewise, the occurrence of adverse events increases with increasing doses in our and other studies.14, 15, 16 In our cohort, the odds of new‐onset fractures increased even when low average doses of ≤5 mg predniso(lo)ne was prescribed, whereas the odds of diabetes and cataract increased at a threshold of >5 mg predniso(lo)ne daily. We observed that the effect of predniso(lo)ne dose on the occurrence of cataract and diabetes persisted for 1 year and did not observe this effect for predniso(lo)ne in the prior 2 or 3 years, implicating that discontinuing glucocorticoids decreased the odds of adverse events. Vertebral compression fractures are the most common type of low‐trauma osteoporotic fractures and were the most frequent observed fractures in our cohort. This is in line with a large study from the United Kingdom that found an increased risk of vertebral compression fractures even with low‐dose predniso(lo)ne (2.5 mg/d).17 Accurate ‘dating’ of these often nontraumatic fractures can be challenging due to an asymptomatic course. However, predniso(lo)ne was significantly associated with nonvertebral fractures, suggesting that this is indeed a risk factor for osteoporosis related fractures.
In our cohort, we observed that budesonide use increased the odds of fractures and cataract. This effect persisted after correction for predniso(lo)ne use in the years prior to these events, suggesting that the ‘topically’ acting budesonide does not completely prevent an increase in the odds of fractures or cataract and may be an independent risk factor for these adverse events. However, it should be noted that despite efforts to control for prior exposure of predniso(lo)ne, this may have influenced the outcome of the odds of budesonide. As only one patient developed de novo diabetes while treated with budesonide, we could not establish a possible effect on the odds of this event. Overall, budesonide seems to have a favourable adverse event profile which is consistent with Danielsson et al18 who found a low frequency of adverse events in patients with autoimmune hepatitis treated with budesonide after prior occurrence of prominent side effects on prednisone. In addition, Manns et al19 found significantly less short‐term corticosteroid‐specific side effects in autoimmune hepatitis patients treated with budesonide compared to predniso(lo)ne. This is supported by evidence in the long‐term treatment of patients with inflammatory bowel disease with budesonide.20
A separate analysis provided a detailed assessment of the effect of each additional milligram of daily corticosteroid doses, with sex and age being equal; one additional milligram of daily predniso(lo)ne increased the odds of a first side effect in that year by 8%. Correspondingly, a patient with two additional milligrams of predniso(lo)ne per day would face a 17% increase of the odds of any of the studied adverse effects compared with patients without these additional two milligrams.
Side effects of corticosteroids are well assessed in diseases such as rheumatoid arthritis,16 systemic lupus erythematosus,21 inflammatory bowel disease,22 chronic idiopathic urticaria23 or asthma24 where oral predniso(lo)ne is frequently used. Yet, the relationship between corticosteroid dose and adverse events is not well quantified. The standard immunosuppression that was applied in the classic early clinical trials in autoimmune hepatitis led to a high prevalence of corticosteroid‐related side effects.1 With the introduction of azathioprine in the treatment of autoimmune hepatitis, both doses and corticosteroid‐related adverse events decreased.25, 26, 27 However, recently the International Autoimmune Hepatitis Study Group emphasised that concerns regarding corticosteroid‐related adverse events are ongoing.28 The current study shows that even low‐dose strategies frequently lead to substantial side effects are at odds with the assumption that adverse events are prevented by low‐dose strategies. Yet, the finding that this effect mitigates after discontinuing predniso(lo)ne is reassuring. A recent survey amongst expert hepatologists showed that azathioprine is a widely used corticosteroid‐sparing agent, yet unfortunately often not optimised.29 Thiopurine therapy in autoimmune hepatitis patients with intolerance or insufficient response to azathioprine can be optimised by the addition of allopurinol,30 switching to tioguanine31 or mercaptopurine.32 Alternatively, mycophenolate mofetil has been successfully applied in the treatment of autoimmune hepatitis.33 By these means, the steroid sparing effect can be improved and the risk of being started on other medications can be prevented. The strengths of this study are defined by the long follow‐up period of a large group of clinically characterised patients, the detailed analysis of daily doses of maintenance medication and the representation of patients treated in both transplant, nontransplant and general referral hospitals. Yet, the results of our study may be affected by referral bias, lifestyle or socio‐economic factors and under‐reporting as we could not assess adverse events with a nationwide method. On the contrary, with cross‐checking multiple data sources of each hospital, we have put effort into the complete capture of adverse events.
The focus of this study was limited to three adverse events. We choose to assess these adverse events because they occur frequently, have a major economic and quality of life impact and are usually well documented. Metabolic, neuropsychiatric, cardiovascular and infectious complications of corticosteroids were not within the scope of this study. In addition, alternative analysis such as a propensity score or case‐control study could have strengthened our results, yet confounders for matching and data on incidence ratios of the general Dutch population in the studied time frame were not available. Finally, the types of cataracts were not distinguished in our cohort and we lumped the total number of cataracts that occurred and could not assess the proportion of corticosteroid‐related posterior subcapsular cataracts. Yet, the clear relation between new‐onset cataracts and corticosteroid use in our cohort suggests that posterior subcapsular cataracts were captured. The results of this study show that patients with autoimmune hepatitis on any dose of corticosteroids should be informed about the risk of cataract and, if indicated (ie due to an impaired vision), referred to an ophthalmologist for eye examination.
5. CONCLUSION
In conclusion, treatment with predniso(lo)ne increased the odds of cataract, diabetes and bone fractures in patients with autoimmune hepatitis. This increased odds of adverse events was dose‐dependent and appears to be reversible. An effect of budesonide on adverse events could not confidently be observed, but it appears not to prevent the development of fractures or cataracts.
AUTHORSHIP
Guarantor of the article: Gerd Bouma.
Author contributions: GB had the original idea and supervised the study. KV, BH, JV, JD, RV, YB and CN collected the data. BL and FB analysed the data. FB wrote the manuscript. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Supporting information
ACKNOWLEDGEMENTS
Declaration of personal interests: None.
APPENDIX 1.
N. M. van Gerven, Rode Kruis Hospital, Beverwijk; J. Ph. Kuijvenhoven, Spaarne Hospital, Haarlem; T. C. M. A. Schreuder, University Medical Center Groningen; E. J. van der Wouden, Isala Hospital, Zwolle; J. J. M. van Meyel and L. C. Baak, OLVG, Amsterdam; P. H. G. M. Stadhouders, St. Antonius Hospital, Nieuwegein; M. Klemt‐Kropp, Noordwest Ziekenhuisgroep, Alkmaar; M. A. M. T. Verhagen, Diakonessenhuis, Utrecht; A. Bhalla and J. W. den Ouden, Haga Hospital, The Hague; U. Beuers, Amsterdam UMC, location AMC; K. J. van Erpecum, University Medical Center, Utrecht; H. R. van Buuren, Erasmus University Medical Center, Rotterdam; J. T. Brouwer, Reinier de Graaf Groep, Delft.
van den Brand FF, van der Veen KS, Lissenberg‐Witte BI, et al; on behalf of the Dutch Autoimmune Hepatitis Study Group . Adverse events related to low dose corticosteroids in autoimmune hepatitis. Aliment Pharmacol Ther. 2019;50:1120–1126. 10.1111/apt.15528
The Handling Editor for this article was Professor Gideon Hirschfield, and it was accepted for publication after full peer‐review.
Contributor Information
Floris F. van den Brand, Email: florisvdbrand@gmail.com.
the Dutch Autoimmune Hepatitis Study Group:
N. M. van Gerven, J. Ph. Kuijvenhoven, T. C. M. A. Schreuder, E. J. van der Wouden, J. J. M. van Meyel, L. C. Baak, P. H. G. M. Stadhouders, M. Klemt‐Kropp, M. A. M. T. Verhagen, A. Bhalla, J. W. den Ouden, U. Beuers, K. J. van Erpecum, H. R. van Buuren, and J. T. Brouwer
REFERENCES
- 1. Cook GC, Mulligan R, Sherlock S. Controlled prospective trial of corticosteroid therapy in active chronic hepatitis. Q J Med. 1971;40:159‐185. [DOI] [PubMed] [Google Scholar]
- 2. van Gerven NM, Verwer BJ, Witte BI, et al. Relapse is almost universal after withdrawal of immunosuppressive medication in patients with autoimmune hepatitis in remission. J Hepatol. 2013;58:141‐147. [DOI] [PubMed] [Google Scholar]
- 3. Lamers MM, van Oijen MG, Pronk M, Drenth JP. Treatment options for autoimmune hepatitis: a systematic review of randomized controlled trials. J Hepatol. 2010;53:191‐198. [DOI] [PubMed] [Google Scholar]
- 4. van Gerven N, Verwer BJ, Witte BI, et al. Epidemiology and clinical characteristics of autoimmune hepatitis in the Netherlands. Scand J Gastroenterol. 2014;49:1245‐1254. [DOI] [PubMed] [Google Scholar]
- 5. Bouma G, van Nieuwkerk CM. Treatment withdrawal in autoimmune hepatitis. Dig Dis. 2015;33(Suppl 2):88‐93. [DOI] [PubMed] [Google Scholar]
- 6. Lohse AW, Mieli‐Vergani G. Autoimmune hepatitis. J Hepatol. 2011;55:171‐182. [DOI] [PubMed] [Google Scholar]
- 7. Dhaliwal H, Peel N, Gleeson D, Karajeh M. PTU‐033 evaluation of bone health in corticosteroid‐treated autoimmune hepatitis. Gut. 2012;61(Suppl 2):A197.192‐A197. [Google Scholar]
- 8. van Gerven NM, de Boer YS, Mulder CJ, van Nieuwkerk CM, Bouma G. Auto immune hepatitis. World J Gastroenterol. 2016;22:4651‐4661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van den Brand FF, van der Veen KS, de Boer YS, et al. Increased mortality among patients with vs without cirrhosis and autoimmune hepatitis. Clin Gastroenterol Hepatol. 2018;17:940‐947. [DOI] [PubMed] [Google Scholar]
- 10. Alvarez F, Berg PA, Bianchi FB, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929‐938. [DOI] [PubMed] [Google Scholar]
- 11. Boberg KM, Chapman RW, Hirschfield GM, Lohse AW, Manns MP, Schrumpf E. Overlap syndromes: the International Autoimmune Hepatitis Group (IAIHG) position statement on a controversial issue. J Hepatol. 2011;54:374‐385. [DOI] [PubMed] [Google Scholar]
- 12. European Association for the Study of the L . EASL Clinical Practice Guidelines: autoimmune hepatitis. J Hepatol. 2015;63:971‐1004. [DOI] [PubMed] [Google Scholar]
- 13. Buttgereit F, Straub RH, Wehling M, Burmester GR. Glucocorticoids in the treatment of rheumatic diseases: an update on the mechanisms of action. Arthritis Rheum. 2004;50:3408‐3417. [DOI] [PubMed] [Google Scholar]
- 14. Sarnes E, Crofford L, Watson M, Dennis G, Kan H, Bass D. Incidence and US costs of corticosteroid‐associated adverse events: a systematic literature review. Clin Ther. 2011;33:1413‐1432. [DOI] [PubMed] [Google Scholar]
- 15. Huscher D, Thiele K, Gromnica‐Ihle E, et al. Dose‐related patterns of glucocorticoid‐induced side effects. Ann Rheum Dis. 2009;68:1119‐1124. [DOI] [PubMed] [Google Scholar]
- 16. Saag KG, Koehnke R, Caldwell JR, et al. Low dose long‐term corticosteroid therapy in rheumatoid arthritis: an analysis of serious adverse events. Am J Med. 1994;96:115‐123. [DOI] [PubMed] [Google Scholar]
- 17. Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2000;15:993‐1000. [DOI] [PubMed] [Google Scholar]
- 18. Danielsson Å, Prytz H. Oral budesonide for treatment of autoimmune chronic active hepatitis. Aliment Pharmacol Ther. 1994;8:585‐590. [DOI] [PubMed] [Google Scholar]
- 19. Manns MP, Woynarowski M, Kreisel W, et al. Budesonide induces remission more effectively than prednisone in a controlled trial of patients with autoimmune hepatitis. Gastroenterology. 2010;139:1198‐1206. [DOI] [PubMed] [Google Scholar]
- 20. Edsbacker S, Andersson T. Pharmacokinetics of budesonide (Entocort EC) capsules for Crohn's disease. Clin Pharmacokinet. 2004;43:803‐821. [DOI] [PubMed] [Google Scholar]
- 21. Shah M, Chaudhari S, McLaughlin TP, et al. Cumulative burden of oral corticosteroid adverse effects and the economic implications of corticosteroid use in patients with systemic lupus erythematosus. Clin Ther. 2013;35:486‐497. [DOI] [PubMed] [Google Scholar]
- 22. Curkovic I, Egbring M, Kullak‐Ublick GA. Risks of inflammatory bowel disease treatment with glucocorticosteroids and aminosalicylates. Dig Dis. 2013;31:368‐373. [DOI] [PubMed] [Google Scholar]
- 23. Ledford D, Broder MS, Antonova E, Omachi TA, Chang E, Luskin A. Corticosteroid‐related toxicity in patients with chronic idiopathic urticariachronic spontaneous urticaria. Allergy Asthma Proc. 2016;37:458‐465. [DOI] [PubMed] [Google Scholar]
- 24. Bloechliger M, Reinau D, Spoendlin J, et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case‐control analysis. Respir Res. 2018;19:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Soloway RD, Summerskill W, Baggenstoss AH, et al. Clinical, biochemical, and histological remission of severe chronic active liver disease: a controlled study of treatments and early prognosis. Gastroenterology. 1972;63:820‐833. [PubMed] [Google Scholar]
- 26. Stern RB, Murray‐Lyon IM, Williams R. Controlled trial of corticosteroids and azathioprine in active chronic hepatitis. Gut. 1973;14:419. [PubMed] [Google Scholar]
- 27. Summerskill WH, Korman MG, Ammon HV, Baggenstoss AH. Prednisone for chronic active liver disease: dose titration, standard dose, and combination with azathioprine compared. Gut. 1975;16:876‐883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dyson JK, De Martin E, Dalekos GN, et al. Review article: unanswered clinical and research questions in autoimmune hepatitis‐conclusions of the International Autoimmune Hepatitis Group Research Workshop. Aliment Pharmacol Ther. 2019;49:528‐536. [DOI] [PubMed] [Google Scholar]
- 29. Liberal R, de Boer YS, Andrade RJ, et al. Expert clinical management of autoimmune hepatitis in the real world. Aliment Pharmacol Ther. 2017;45:723‐732. [DOI] [PubMed] [Google Scholar]
- 30. de Boer YS, van Gerven NM, de Boer NK, Mulder CJ, Bouma G, van Nieuwkerk CM. Allopurinol safely and effectively optimises thiopurine metabolites in patients with autoimmune hepatitis. Aliment Pharmacol Ther. 2013;37:640‐646. [DOI] [PubMed] [Google Scholar]
- 31. van den Brand FF, van Nieuwkerk C, Verwer BJ, et al. Biochemical efficacy of tioguanine in autoimmune hepatitis: a retrospective review of practice in The Netherlands. Aliment Pharmacol Ther. 2018;48:761‐767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hubener S, Oo YH, Than NN, et al. Efficacy of 6‐mercaptopurine as second‐line treatment for patients with autoimmune hepatitis and azathioprine intolerance. Clin Gastroenterol Hepatol. 2016;14:445‐453. [DOI] [PubMed] [Google Scholar]
- 33. Zachou K, Gatselis N, Papadamou G, Rigopoulou EI, Dalekos GN. Mycophenolate for the treatment of autoimmune hepatitis: prospective assessment of its efficacy and safety for induction and maintenance of remission in a large cohort of treatment‐naive patients. J Hepatol. 2011;55:636‐646. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


