Abstract
Background
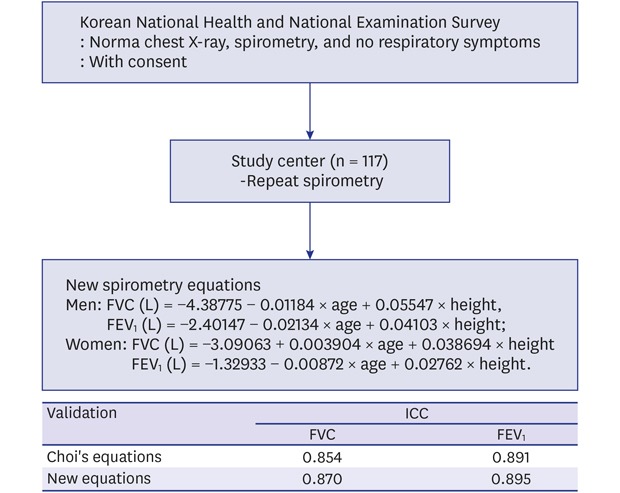
Pulmonary functions are interpreted using predicted values from reference equations that vary with ethnicity, gender, age, height, and weight. The universally used Choi's reference equations are not validated for Korean populations, and the purpose of this study was to validate them and develop new reference equations.
Methods
Subjects with normal spirometry and chest radiographs, no co-morbidities, and non-smokers, from the Korean National Health and National Examination Survey (KNHANES)-VI were enrolled (n = 117). Intraclass correlation coefficient (ICC) was assessed for reliability of reference equations. New reference equations were developed using linear regression analysis. Differences between observed and predicted values were assessed to compare the reference equations from Choi's, Global Lung Function Initiative 2012, KNHANES-IV, and newly developed equations.
Results
The ICC of Choi's reference equations was 0.854 (P < 0.001). The new reference equations for men were: forced vital capacity (FVC) (L) = − 4.38775 − 0.01184 × age + 0.05547 × height, forced expiratory volume – 1 second (FEV1) (L) = − 2.40147 − 0.02134 × age + 0.04103 × height; and for women: FVC (L) = − 3.09063 + 0.003904 × age + 0.038694 × height; FEV1 (L) = − 1.32933 − 0.00872 × age + 0.02762 × height. The differences between the predicted and observed means were largest in Choi's equations, but lowest in the new equations with highest goodness of fit.
Conclusion
Because Choi's reference equations presented larger differences from the observed values, despite reliability, and the new reference equations showed better goodness of fit, we suggest the latter for Korean populations.
Keywords: Spirometry, Reference Equations, Predicted Values
Graphical Abstract
INTRODUCTION
Spirometry is a physiological test measuring how an individual inhales or exhales volumes of air as a function of time.1 It is invaluable as a screening test of general respiratory health.1 The indications for spirometry include evaluating respiratory symptoms, measuring effects of disease on pulmonary function, screening individuals at risk of having pulmonary disease, assessing pre-operative risk, assessing prognosis, and monitoring diseases.1
Interpretation of spirometry is achieved from comparison of data measured in a subject with predicted values derived from healthy subjects. Predicted values should be calculated from reference equations developed from studies of healthy subjects of a general population with the same anthropometrics such as gender, age, and height and ethnic characteristics of the subject.2 Predicted values of spirometry vary according to age, height, gender, and race/ethnic groups.3,4 Thus, reference equations for subjects' nationalities or ethnicities is pivotal in interpreting spirometry results. Even though spirometry is performed with the highest standards of technical skill and quality, spirometry results can only be clinically acceptable if interpreted using appropriate and reliable reference values.4
Reference equations are widely available for a wide range of populations and sub-populations within countries.3,4,5,6,7 Global Lung Function Initiative (GLI) network has produced worldwide standardized lung function reference values for spirometry in 2012.4 GLI reference equations were derived for healthy individuals in the 3–95 year age range for various ethnic groups including Caucasians, African Americans, South East Asians, and North East Asians.4
In Korea, the Morris' equation was commonly used,8 which was originally developed for Caucasians. Reference equations for Korean population developed from the first national chronic obstructive pulmonary disease (COPD) survey in Korea, which was conducted as a part of the Korean National Health and Nutrition Examination Survey (KNHANES)-II in 2001. Thereafter, Korean Academy of Tuberculosis and Respiratory Disease (KATRD) recommended reference equations for the Korean population, called Choi's reference equation.7 However, there is no validation for this reference equation. Choi's reference values for forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FEV1/FVC % were calculated to be much higher than those from other reference equations.7,9,10 Choi's reference was developed 17 years ago. Recently, the other reference equations for Korean populations were developed from KNHANES-IV (2007–2009).10 It represented pulmonary functions of the current Korean healthy adults,10 but were not used in real world clinics and laboratories.
The aim of this study was to validate Choi's reference equation for Korean population, and develop new reference equations for the current healthy Korean population.
METHODS
Data source and subjects
This study was a part of the quality control program of spirometry at the sixth KNHANES (2013–2015).11 Additionally, this study was performed along with a study for the development of reference equations for diffusing capacity of the lungs.12
We recruited non- smokers with normal spirometry results and normal chest X-ray findings from those participating in KNHANES-VI. Non-smoker was defined as < 10 cigarettes/lifetime. The selected subjects had no coughing, sputum, or dyspnea at least in the previous 3 months. We excluded any subjects with history of self-reported co-morbidities; hypertension, stroke, myocardial infarction, angina, hyperlipidemia, osteoarthritis, rheumatic arthritis, osteoporosis, pulmonary tuberculosis, bronchial asthma, sinusitis, bronchiectasis, allergic rhinitis, depression, diabetes mellitus, lung cancer, lung resection operation, or congestive heart failure, which influence the lung function.12
Spirometry
We used dry rolling seal spirometers (Model 2130; SensorMedics, Yorba Linda, CA, USA) for pulmonary function test. We accepted the spirometry results, which showed two or more acceptable curves and satisfied reproducibility criteria of American Thoracic Society/European Respiratory Society.1 The spirometry data were recorded on web-hard to be examined for quality control and quality confidence.
After spirometry in KNHANES-VI, eligible subjects with normal spirometry and chest X-ray findings were asked to take part in this study.
Participants who signed the written consent moved to 16 regional university hospitals located within an hour's distance from their households to repeat the spirometry. Spirometry was re-performed by expert technicians who performed the diffusing capacity test ≥ 200 times/year for 5 years or more at the university hospitals.12 All technicians had undergone quality control training.
Statistical analysis
All statistical analyses were performed using SPSS version 24.0 (IBM Corp., Armonk, NY, USA). Data was presented as mean ± standard deviation or percentage numbers. We used regression analysis to make new prediction equations for spirometry. Prediction equations for FVC, FEV1, and FEV1/FVC were derived separately according to gender. To validate the regression equation, we used the k-fold cross-validation method. For cross-validation, some of the data are used as a training set and the rest is used as a test set. The training set made a regression equation, and the test set made a validation. The cross validation was performed as the method published previously which was researched together with this study.12
To compare the goodness of fit of the reference equations obtained in this study with the previous equations from Choi's,7 GLI 2012,4 and KNHANES IV,10 we calculated the differences between the observed values and the predicted values using each prediction equation. The differences were presented as the mean squared difference, and the means of predicted values and observed values were compared using a paired t-test. Choi's reference equations used age, height, and weight,7 GLI 2012 used age and height to calculate predicted values, while KNHANES-IV used age, height, and weight.10 We used GLI 2012 reference equations for North East Asian populations.4 Reference equations from KNHANES IV used age, height, and weight.10
To validate the Choi's reference equations, we assessed reliability. Reliability of reference equations for spirometry was assessed by examining the relationship between measured pulmonary functions (FVC and FEV1) and reference values (FVC and FEV1), using intraclass correlation coefficiency (ICC).
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of each participating hospital where the spirometry was performed (Hallym University Sacred Heart Hospital, IRB No. 2015-I069).12 We obtained the informed consents from participants who permitted enrollment in this study.
RESULTS
Baseline characteristics
A total of 117 subjects (men 37, women 80) were enrolled in this study. Table 1 shows the baseline characteristics according to the gender. The mean age of participants was 46 years. Table 2 shows the distribution of number, height, and weight according to the age groups. The distributions according to the ages were as follows: 18 in their twenties, 22 in their thirties, 26 in their forties, 28 in their fifties, 15 in their sixties, and 8 in their seventies. The mean values of FVC and FEV1 were 3.65 ± 0.82 L and 2.96 ± 0.67 L, respectively.
Table 1. Baseline characteristics.
| Characteristics | Total | Men | Women |
|---|---|---|---|
| Total | 117 (100) | 37 (31.6) | 80 (68.4) |
| Age, yr | 46.2 ± 14.9 | 43.2 ± 16.4 | 47.6 ± 16.0 |
| Height, cm | 162.3 ± 8.5 | 170.7 ± 6.7 | 158.3 ± 6.0 |
| Weight, kg | 63.2 ± 11.5 | 71.8 ± 11.3 | 59.3 ± 9.3 |
| BMI, kg/m2 | 24.0 ± 3.77 | 24.6 ± 3.5 | 23.7 ± 3.8 |
| FVC, L | 3.65 ± 0.82 | 4.60 ± 0.64 | 3.22 ± 0.43 |
| FVC, % predicted | 97.2 ± 19.6 | 97.0 ± 9.2 | 97.3 ± 13.1 |
| FEV1, L | 2.96 ± 0.67 | 3.69 ± 0.61 | 2.63 ± 0.35 |
| FEV1, % predicted | 97.2 ± 11.4 | 96.6 ± 9.2 | 97.5 ± 12.3 |
Data are presented as number (%) or mean ± standard deviation.
BMI = body mass index, FVC = forced vital capacity, FEV1 = forced expiratory volume in 1 second.
Table 2. Distribution of number, height, and weight according to age and gender.
| Age group, yr | No. (%) | Height, cm | Weight, kg | |||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| 20–29 | 9 (24.3) | 9 (11.2) | 172.67 ± 6.56 | 161.56 ± 6.35 | 76.00 ± 8.72 | 54.44 ± 7.35 |
| 30–39 | 8 (21.6) | 14 (17.5) | 172.42 ± 5.43 | 161.21 ± 5.65 | 73.63 ± 19.32 | 55.43 ± 10.79 |
| 40–49 | 8 (21.6) | 18 (22.5) | 173.00 ± 5.95 | 159.74 ± 5.90 | 73.00 ± 3.66 | 58.78 ± 8.34 |
| 50–59 | 4 (10.8) | 24 (30.0) | 168.75 ± 2.87 | 156.33 ± 4.89 | 66.75 ± 6.13 | 64.62 ± 9.85 |
| 60–69 | 5 (13.5) | 10 (12.5) | 164.20 ± 8.53 | 154.10 ± 4.82 | 64.00 ± 11.47 | 58.40 ± 6.48 |
| ≥ 70 | 3 (8.1) | 5 (6.2) | 167.67 ± 8.96 | 157.10 ± 7.99 | 70.67 ± 6.03 | 61.20 ± 5.59 |
| Total | 37 (100) | 80 (100) | 170.71 ± 6.73 | 158.33 ± 6.02 | 71.78 ± 11.35 | 59.26 ± 9.25 |
Data are presented as number (%) or mean ± standard deviation.
Development of new prediction equation for spirometry
After considering other prediction equations and clinical significance,2,4,7,8,13 we selected age, height, and body weight as the parameters for the equation of FVC and FEV1. Age and height were significant variables for the predication equation after multiple linear regression analysis (Table 3). The developed new prediction equations for spirometry were described in Table 4.
Table 3. Development of new prediction equations for spirometry.
| Variables | Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t value | P value | r2 | Estimate | SE | t value | P value | r2 | ||
| FEV1 | 0.702 | 0.418 | |||||||||
| Intercept | −2.40147 | 1.56054 | −1.54 | 0.130 | −1.32933 | 0.93219 | −1.43 | 0.1575 | |||
| Age | −0.02134 | 0.00345 | −6.19 | < 0.001 | −0.00872 | 0.00253 | −3.44 | 0.0009 | |||
| Height | 0.04103 | 0.00879 | 4.67 | < 0.001 | 0.02762 | 0.00554 | 4.99 | < 0.001 | |||
| FVC | 0.531 | 0.233 | |||||||||
| Intercept | −4.38775 | 2.05482 | −2.14 | 0.039 | −3.09063 | 1.308857 | −2.361 | 0.0205 | |||
| Age | −0.01184 | 0.00454 | −2.61 | 0.013 | 0.003904 | 0.003558 | 1.097 | 0.2756 | |||
| Height | 0.05547 | 0.01158 | 4.79 | < 0.001 | 0.038694 | 0.007776 | 4.976 | < 0.001 | |||
| FEV1/FVC | 0.500 | 0.500 | |||||||||
| Intercept | 0.889052 | 0.34126 | 2.61 | 0.013 | 0.667268 | 0.229033 | 2.91 | 0.0046 | |||
| Age | 0.004455 | 0.000754 | 5.91 | < 0.001 | 0.005535 | 0.000623 | 8.89 | < 0.001 | |||
| Height | 0.001 | 0.001923 | 0.52 | 0.606 | 0.001891 | 0.001361 | 1.39 | 0.1682 | |||
SE = standard error, FVC = forced vital capacity, FEV1 = forced expiratory volume in 1 second.
Table 4. Reference equations for spirometry.
| Models | Sex | Indices | Reference equations |
|---|---|---|---|
| Choi's7 | Men | FVC | −4.8434 − 0.00008633 × age2 + 0.05292 × height + 0.01095 × weight |
| FEV1 | −3.4132 − 0.0002484 × age2 + 0.04578 × height | ||
| Women | FVC | −3.0006 − 0.0001273 × age2 + 0.03951 × height + 0.006892 × weight | |
| FEV1 | −2.4114 − 0.0001920 × age2 + 0.03558 × height | ||
| Present | Men | FVC | −4.38775 − 0.01184 × age + 0.05547 × height |
| FEV1 | −2.40147 − 0.02134 × age + 0.04103 × height | ||
| Women | FVC | −3.09063 + 0.003904 × age + 0.038694 × height | |
| FEV1 | −1.32933 − 0.00872 × age + 0.02762 × height |
FVC = forced vital capacity, FEV1 = forced expiratory volume in 1 second.
Validation of Choi's equations
The means of the observed values of FVC and FEV1 for the reference population were statistically different from those of the predicted values from Choi's equations. Significant differences between observed values and predicted values from Choi's equations were presented according to the gender (Table 5). Choi's equations overestimated the FVC and FEV1 as compared to the observed values. ICC for reliability of Choi's equations was scored at 0.854 for FVC, and 0.891 for FEV1. The ICCs of four equations were all > 0.80 (Table 6).
Table 5. Differences for FVC and FEV1 between observed and predicted values according to different equations.
| Variables | Total | Men | Women | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean diff, mean ± SD | Mean squared diff | Mean ± SD | Mean diff, mean ± SD | Mean squared diff | Mean ± SD | Mean diff, mean ± SD | Mean squared diff | |||
| FVC, L | |||||||||||
| Observed | 3.65 ± 0.82 | 4.60 ± 0.64 | 3.22 ± 0.43 | ||||||||
| Predicted | |||||||||||
| Present | 3.65 ± 0.76 | 0.01 ± 0.39 | 0.15 | 4.58 ± 0.48 | 0.03 ± 0.40 | 0.15 | 3.22 ± 0.22 | −0.01 ± 0.39 | 0.14 | ||
| Choi's7 | 3.81 ± 0.78a | −0.15 ± 0.43 | 0.20b | 4.79 ± 0.48 | −0.20 ± 0.45a | 0.23b | 3.35 ± 0.34 | −0.13 ± 0.42a | 0.19 | ||
| GLI4 | 3.57 ± 0.79 | 0.07 ± 0.47 | 0.23b | 4.59 ± 0.63 | 0.15 ± 0.43a | 0.20 | 3.17 ± 0.45 | 0.04 ± 0.50 | 0.24b | ||
| KNHANES-IV10 | 3.56 ± 0.73a | 0.09 ± 0.42 | 0.18 | 4.43 ± 0.55 | 0.10 ± 60.39a | 0.17 | 3.15 ± 0.36 | 0.05 ± 0.43 | 0.18 | ||
| FEV1, L | |||||||||||
| Observed | 2.96 ± 0.67 | 3.69 ± 0.61 | 2.63 ± 0.35 | ||||||||
| Predicted | |||||||||||
| Present | 2.96 ± 0.63 | 0.00 ± 0.29 | 0.08 | 3.68 ± 0.52 | 0.00 ± 0.04 | 0.10 | 2.63 ± 0.24 | 0.00 ± 0.27 | 0.07 | ||
| Choi's7 | 3.10 ± 0.69 | −0.14 ± 0.32a | 0.11b | 3.87 ± 0.57a | −0.19 ± 0.33 | 0.14 | 2.75 ± 0.39a | −0.12 ± 0.31 | 0.11b | ||
| GLI4 | 2.93 ± 0.68 | 0.03 ± 0.34 | 0.11b | 3.62 ± 0.61 | 0.06 ± 0.34 | 0.11 | 2.61 ± 0.43 | 0.01 ± 0.34 | 0.11b | ||
| KNHANES-IV10 | 2.89 ± 0.62 | 0.06 ± 0.29a | 0.09 | 3.57 ± 0.55a | 0.10 ± 0.31 | 0.10 | 2.58 ± 0.34 | 0.04 ± 0.28 | 0.08 | ||
Mean difference = observed value − calculated value, Mean squared difference = (observed values − calculated values)2
FVC = forced vital capacity, FEV1 = forced expiratory volume in 1 second, SD = standard deviations, diff = difference, KNHANES = Korean National Health and National Examination Survey.
aP values < 0.05 using paired t-test between observed values and predicted values; bP values < 0.05 using paired t-test between mean squared difference of present values and those of predicted values.
Table 6. Reliability of variable reference equations for spirometry.
| Variables | Reliability | |||
|---|---|---|---|---|
| ICC | 95% CI | P value | ||
| FVC | ||||
| Present | 0.870 | 0.818–0.908 | < 0.001 | |
| Choi's7 | 0.854 | 0.796–0.897 | < 0.001 | |
| GLI4 | 0.824 | 0.756–0.875 | < 0.001 | |
| KNHANES-IV10 | 0.854 | 0.796–0.896 | < 0.001 | |
| FEV1 | ||||
| Present | 0.895 | 0.853–0.926 | < 0.001 | |
| Choi's7 | 0.891 | 0.847–0.923 | < 0.001 | |
| GLI4 | 0.872 | 0.821–0.910 | < 0.001 | |
| KNHANES-IV10 | 0.894 | 0.851–0.925 | < 0.001 | |
CI = confidence interval, FVC = forced vital capacity, GLI = Global Lung Function Initiative, KNHANES = Korean National Health and National Examination Survey, FEV1 = forced expiratory volume in 1 second, ICC = Intraclass correlation coefficient.
Differences and comparisons between observed and predicted values
In Table 5, there were no significant differences between the means of the observed values and the means of the predicted values in new equations for FEV1 and FVC. Predicted values calculated from GLI 2012 equations showed no significant differences from the observed spirometric values, except for the predicted FVC in men. The largest mean difference of FVC and FEV1, between observed values and predicted values, was examined in Choi's equations followed by KNHANES-IV, GLI 2012, and present equations. Choi's reference equations predicted higher values than observed, on the other hand three equations predicted lower values than the observed values, except for FVC from present equations in women. The mean squared differences between observed and predicted values were the lowest in this study compared to other equations, which means the highest goodness of fit of the regression models (Table 5).
DISCUSSION
In this study, we validated Choi's reference equations of FVC and FEV1. Choi's reference equations were reliable to predict values, however, it predicted higher lung functions compared to observed lung functions. Furthermore, we developed new reference equations of spirometry for the Korean population. New reference equations showed the lowest differences between observed values and predicted values compared to Choi's equations, GLI 2012, and KHNAES IV equations for Korean populations.
Normal predicted values of spirometry may differ depending on the anthropometry requirements of the subjects and statistical methods.14 Thus, for interpretation of spirometry, reference equations considering subjects' ethnicities or nationalities will be needed.
In Korea, reference equations from Morris et al.8 and from Choi et al.7 were commonly used. Patients with COPD had more severe airflow limitations9 and higher proportion of ventilator dysfunction15 when Choi's reference equations were compared to other equations for different ethnicities. Choi's reference equations predicted higher values than the observed values as compared to other reference equations. Although Choi's reference was developed from KNHANES-II and was universally used in Korea, Choi's equations were not validated for normal populations. In this study, ICC reliability was good in Choi's reference equations. This is the first report to validate Choi's reference equations in healthy populations.
GLI 2012 presented standardized spirometry prediction equations for ethnic and geographic groups from 26 countries, including Korea, for the age group of 3–39 years.4 GLI 2012 spirometry reference equations used age, height, gender, and ethnic groups to predict FVC, FEV1, and FEV1/FVC. Predicted values, including FEV1 and FVC, differed proportionally between ethnic groups from that of Caucasians.4 The GLI 2012 reference equations currently provide the most reliable spirometric prediction equations for appropriate age-dependent lower limits of normal. Many national respiratory societies endorsed and adopted the GLI equations for the recommended equation.4
In this study, we compared the reference values between Choi's, KHANES-IV, and GLI equations. Mean squared difference of FVC was larger in GLI equations than Choi's equations; however, mean difference of FVC between observed values and predicted values from Choi's was larger than that from GLI equations. Choi's equations predicted higher FVC than observed values. Other equations predicted lower FVC than observed values. In FEV1, mean squared difference from GLI equation was the same as that from Choi's equations, but mean difference was larger in Choi's equations. Although GLI provided standardized and reliable worldwide reference equations for different ethnic groups, specific reference equations for Korean population might need to be used.
We developed new reference equations for more reliable predicted values. Limitations of Choi's equations in this study were higher predicted values than observed values, and larger mean differences than GLI despite good reliability. The new reference equations predicted closer values to observed values as compared to Choi's and GLI equations. Mean squared differences of FVC and FEV1 from new equations were almost close to “0,” which indicated that goodness of fit of the new equations was the best among the three equations. This was consistent in men and women; especially in women, where fitness was the best in FEV1 as the mean squared difference was 0.07. These findings imply that our newly developed reference equations have a high goodness of fit for Korean populations. Reference equations from KNHANES IV predicted values closer to observed values than Choi's equations. On the other hand, mean differences and mean squared differences from the present study were lesser than KNHANES IV. Present reference equations showed highest goodness of fit among four reference equations.
Reference equations from the present study, Choi's, KNHANES IV, and GLI 2012 were reliable to predict lung functions despite the mean differences being larger in Choi's equations and GLI 2012 equations. Until recently, the KATRD recommended Choi's reference equations for Korean populations and GLI provided global reference equations for North East Asian populations. They were reliable in this study to predict spirometry; however, differences between observed values and predicted values were higher than the present newly developed equations. Thus, we can suggest that the new reference equations are more suitable and more reliable to predict lung functions for Korean populations.
There were a few limitations in this study. First, the number of subjects assessed to validate Choi's reference equations and to develop new reference equations was 117. The number in this study is too small to represent the entire Korean population. Previous equations from KNHANES IV10 included over 4,000 subjects, but the spirometry were performed on the survey vehicle. In our study, we enrolled subjects who had first undergone KNHANES spirometry in the vehicle. Then, the spirometry tests were repeated in hospital by professional spirometry technicians who worked over 5 years in a university hospital. The technicians also cross checked the repeated spirometry results. Therefore, the spirometry results of our study were more qualified. The survey of the KNHANES IV was performed during 2007–2009. This study was performed during 2013–2015. This may explain why our study revealed more precise equations compared to equations from KNHANES IV despite the small number of subjects. Second, the number of men (31.6%) is too small to compare to women. In the equations from KNHANES IV,10 the men were 14.8%. Spirometry are used to assess pulmonary function, diagnose pulmonary disease, and follow up. Prevalence of COPD16 is higher in men than women and asthma17 is higher in women than men. The higher number of men than women is not a prerequisite for development of equations. Third, the number of subjects age ≥ 70 years old is too small (6.8%). The population of people age ≥ 70 years old was 8.2% in Korea.18 Although the number of old subjects is too small, the proportion of age population is acceptable. Fourth, respiratory symptoms and co-morbidities for inclusion or exclusion criteria were collected from a self-reported survey. This is the major limitation of a national survey. This is a pivotal study because it is the first report that validates the commonly used Choi's reference equations. Validation for new reference equations will be needed in future studies.
To summarize, the usually used Choi's reference equations for spirometry was reliable, but there were large differences between observed values and predicted values as compared to GLI 2012 and KNHANES IV equations. Thus, we developed new reference equations for Korean populations. New reference equations in the present study showed the least differences between observed values and predicted values for spirometry, and showed highest goodness of fit to predict lung functions. It is necessary to use reference equations developed for Korean populations, and newly developed reference equations could be the answer. Further study to validate of new spirometry with a large number of subjects will be needed.
Footnotes
Funding: This research was supported by the Korea Centers for Disease Control and Prevention (grant No. 2015-P35006-00).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yoo KH, Shim JJ, Hwang YI.
- Formal analysis: Choi HS, Kim TE, Hwang YI.
- Investigation: Park YB, Yoon HK, Lim SY, Kim TH, Park JH, Lee WY, Park SJ, Lee SW, Kim WJ, Kim KU, Shin KC, Kim DJ, Yoo KH, Shim JJ, Hwang YI.
- Methodology: Park YB, Yoon HK, Lim SY, Kim TH, Park JH, Lee WY, Park SJ.
- Supervision: Lee SW, Kim WJ, Kim KU, Shin KC, Kim DJ.
- Visualization: Choi HS, Kim TE, Hwang YI.
- Writing - original draft: Choi HS.
- Writing - review & editing: Park YB, Yoo KH, Lim SY, Kim TH, Park JH, Lee WY, Park SJ, Lee SW, Kim WJ, Kim KU, Shin KC, Kim DJ, Yoo KH, Shim JJ, Hwang YI.
References
- 1.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 2.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 3.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 4.Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123(6):659–664. doi: 10.1164/arrd.1981.123.6.659. [DOI] [PubMed] [Google Scholar]
- 6.Roca J, Sanchis J, Agusti-Vidal A, Segarra F, Navajas D, Rodriguez-Roisin R, et al. Spirometric reference values from a Mediterranean population. Bull Eur Physiopathol Respir. 1986;22(3):217–224. [PubMed] [Google Scholar]
- 7.Choi JK, Paek D, Lee JO. Normal Predictive values of spirometry in Korean Population. Tuberc Respir Dis (Seoul) 2005;58(3):230–242. [Google Scholar]
- 8.Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- 9.Hwang YI, Kim EJ, Lee CY, Park S, Choi JH, Park YB, et al. Application of a new spirometric reference equation and its impact on the staging of Korean chronic obstructive pulmonary disease patients. Yonsei Med J. 2012;53(2):363–368. doi: 10.3349/ymj.2012.53.2.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eom SY, Kim H. Reference values for the pulmonary function of Korean adults using the data of Korea National Health and Nutrition Examination Survey IV (2007–2009) J Korean Med Sci. 2013;28(3):424–430. doi: 10.3346/jkms.2013.28.3.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korean Center for Disease Control and Prevention. Korean National Health & Nutrition Examination Survey. [Updated 2017]. [Accessed August 2, 2018]. https://knhanes.cdc.go.kr/knhanes/sub02/sub02_02.do.
- 12.Hwang YI, Park YB, Yoon HK, Lim SY, Kim TH, Park JH, et al. Development of prediction equation of diffusing capacity of lung for Koreans. Tuberc Respir Dis (Seoul) 2018;81(1):42–48. doi: 10.4046/trd.2017.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123(6):659–664. doi: 10.1164/arrd.1981.123.6.659. [DOI] [PubMed] [Google Scholar]
- 14.Sim YS, Lee JH, Lee WY, Suh DI, Oh YM, Yoon JS, et al. Spirometry and bronchodilator test. Tuberc Respir Dis (Seoul) 2017;80(2):105–112. doi: 10.4046/trd.2017.80.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oh YM, Hong SB, Shim TS, Lim CM, Koh Y, Kim WS, et al. Effect of a new spirometric reference equation on the interpretation of spirometric patterns and disease severity. Tuberc Respir Dis (Seoul) 2006;60(2):215–220. [Google Scholar]
- 16.Hwang YI, Park YB, Yoo KH. Recent trends in the prevalence of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis (Seoul) 2017;80(3):226–229. doi: 10.4046/trd.2017.80.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park SY, Kim JH, Kim HJ, Seo B, Kwon OY, Chang HS, et al. High prevalence of asthma in elderly women: findings from a Korean national health database and adult asthma cohort. Allergy Asthma Immunol Res. 2018;10(4):387–396. doi: 10.4168/aair.2018.10.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ministry of the Interior and Safety. Resident registration demographics. [Updated 2013]. [Accessed September 12, 2019]. http://27.101.213.4/index.jsp.


