Abstract
Introduction:
Pediatric postoperative opioid prescribing has come under scrutiny as a result of the ongoing opioid epidemic. Previous research has demonstrated that African American adults are less likely to receive analgesics, particularly opioids, after surgery, even after controlling for pain severity. We sought to examine racial disparities in the filling of opioid prescriptions by pediatric surgical patients after cholecystectomy.
Methods:
We studied patients aged 1 to 18 years of age who were enrolled in Ohio Medicaid and underwent cholecystectomy. Procedures performed in January 2013 - July 2016 were included. The percentage of patients who filled a postoperative opioid prescription within 14 days of their procedure was compared between black and white patients using log binomial regression models fit using generalized estimating equations to account for patient clustering within hospitals.
Results:
We identified 1277 patients who underwent a cholecystectomy. In unadjusted analyses, black children were significantly less likely than white children to fill an opioid prescription postoperatively (74.9% vs 85.7%, p<0.001). After adjustment for patient-level clinical and demographic characteristics, we found that black children treated at non-children’s hospitals in large/medium sized urban counties were significantly less likely to fill an opioid prescription after cholecystectomy when compared to white children treated at urban children’s hospitals or to white children treated in non-children’s hospitals in either large/medium urban counties or other counties. However, this association was partly explained by a longer average length of stay among black children.
Conclusions:
Black children who undergo cholecystectomy at urban non-children’s hospitals are less likely to fill a postoperative opioid prescription than white children who undergo cholecystectomy at those same hospitals or other hospitals. Further research is needed to identify whether this disparity is due to a lower rate of opioid prescribing or a lower rate of prescription filling.
Keywords: opioids, racial disparities, cholecystectomy, pediatric
Introduction
Previous studies have demonstrated racial disparities in pain management in adults in a variety of settings (1–5). In children, similar findings of racial disparities have been shown in treatment for acute pain when patients present to the emergency department with long bone fractures and appendicitis (6, 7). However, little is known about whether disparities exist in prescribing patterns for outpatient postoperative opioid use. Laparoscopic cholecystectomy is a common surgical procedure in adults that results in moderate postoperative pain typically treated with opioids (8, 9). In children, there is an increasing incidence of gallbladder disease, and along with it, a rise in the number of cholecystectomies performed (10, 11). Pain levels and pain medication prescribing after pediatric cholecystectomy have not been reported in population-based studies. Based on evidence from adult studies, we hypothesized that opioids are frequently prescribed and that black children are less likely than white children to fill an opioid prescription after cholecystectomy.
Methods
Data Source and Study Population
This study used Ohio Medicaid claims data from January 2013-August 2016. The Institutional Review Board at Nationwide Children’s Hospital approved this study as minimal risk with a waiver of written consent. Health care claims and enrollment data on all Ohio Medicaid/Children’s Health Insurance Program (CHIP) enrollees under 19 years of age were available. During the study period, all children in families with incomes up to 206% of the federal poverty level were eligible for Medicaid/CHIP in Ohio (12). Data from a total of 2,028,130 unique children aged 0 to 18 years were available. We identified children aged 1-18 years who underwent either open or laparoscopic cholecystectomy. These procedures were identified by searching for professional (physician) claims containing Current Procedural Terminology (CPT®) codes 47562, 47563, 47564, 47600, 47605, 47610, 47612, or 47620. In order to include a relatively consistent set of surgeons and other postsurgical opioid prescribers throughout the entire study period, we excluded children who underwent surgery outside of Ohio or who were operated on by a surgeon not based in Ohio. Because the study aimed to examine disparities in the receipt of postsurgical opioids between black and white children, we also excluded children with missing race or a race other than black or white. We also excluded patients who underwent other major abdominal surgical procedures on the same day as cholecystectomy. Such procedures included liver biopsy (CPT 47000, 47001), hepatectomy or liver lobectomy (CPT 47120, 47122, 47125, 47130), liver transplant (CPT 47135, 47140, 47141, 47142), pancreatic transplant (CPT 48550, 48554), bariatric surgery (13), or splenectomy (CPT 38120, 38100). Finally, in order to capture all opioid prescription fills within 14 days of surgery, we excluded children not covered by Ohio Medicaid in the month after their surgery. Due to the nature of the claims database, information is not available on prescriptions written, so our analysis focused on the outcome of opioid prescription filling.
Patient and Institutional Characteristics
We evaluated several patient and institution-level characteristics as potential confounders of the association between patient race and the filling of an opioid prescription after pediatric cholecystectomy. Characteristics were selected for evaluation based on their availability in the claims database and their reported associations with postsurgical opioid prescribing in previous studies (2, 14, 15). In addition to patient race, other patient level factors evaluated included age, sex, surgical approach (open or laparoscopic), postoperative length of stay, and a diagnosis of sickle cell disease. The institution-level characteristics examined were children’s hospital status and urban/rural location. Members of the Children’s Hospital Association were considered children’s hospitals. All children’s hospitals in Ohio are either freestanding or, if not freestanding, still bill as a distinct entity from the general acute care hospital in which they are located. Therefore, procedures performed in children’s units within general acute care hospitals were identifiable. The only exception was Cleveland Clinic Children’s, which could not be distinguished from the main campus Cleveland Clinic in the Medicaid claims data. Thus, all pediatric cholecystectomies performed in this hospital were assumed to have been performed in Cleveland Clinic Children’s. Urban/rural location was defined using the National Center for Health Statistics 2013 county-level urban/rural classification scheme (16). In this scheme, counties in metropolitan statistical areas (MSA) with populations of 1 million or more that contain the principal city of the MSA are considered large central metro counties. Counties in MSAs with populations of 1 million or more that do not contain the principal city of the MSA are considered large fringe metro counties. Counties in MSAs with populations of 250,000 to 999,999 are medium metro counties. Counties in MSAs with populations less than 250,000 are small metro counties. Counties in micropolitan statistical areas are micropolitan counties, and all other counties are considered noncore. All children’s hospitals in Ohio are located in large central or medium metro counties as defined by this classification scheme.
Outcome Definition
The outcome of interest in this study was whether a patient filled an opioid prescription within 14 days after cholecystectomy. To identify opioid prescription fills, we searched outpatient pharmacy claims for the national drug codes (NDCs) that represent opioids according to the Centers for Disease Control and Prevention (17).
Statistical Analysis
Frequencies and percentages or medians and interquartile ranges were used to describe patient and institutional characteristics overall as well as by patient race and whether an opioid prescription was filled. Nearly all included black children were treated at hospitals located in large central metropolitan and medium sized metropolitan counties, and black children were also much more likely to receive their care at a children’s hospital. Therefore, we relied on a combined exposure variable that took into account patient race, hospital location, and children’s hospital status in our multivariable regression analyses. This combined exposure variable allowed us to eliminate confounding of racial differences in postsurgical opioid prescription filling by these institutional characteristics, and enabled us to include institutions that performed cholecystectomies in no or few black children. However, the use of this composite variable did require us to exclude from regression analyses twelve black children who were treated outside of large central and medium metropolitan counties. The probability of filling an opioid prescription after surgery was modelled using log binomial regression models fit using generalized estimating equations to account for patient clustering within institutions. In addition to the combined patient race/hospital type exposure variable that was of primary interest, all other preoperative patient characteristics evaluated were included in the multivariable model. Differences in rates of opioid prescription filling by patient race, children’s hospital status, and hospital location were evaluated as relative differences (probability ratios). Lastly, because some opioid prescriptions filled within 14 days of surgery may not have been for postoperative pain, particularly among children with sickle cell disease, we reran all analyses examining only opioid prescriptions filled within 3 days of surgery. All statistical analyses were conducted using SAS Enterprise Guide 7.15 (SAS Institute Inc., Cary, NC). Two sided p values less than 0.05 were considered statistically significant.
Results
We included 1277 children covered by Ohio Medicaid who underwent a cholecystectomy in Ohio during the study period (Figure 1). In unadjusted analyses, there were significant differences in patient and institution level characteristics between patients who did and did not fill an opioid prescription (Table 1). Notably, only 74.9% of black children filled an opioid prescription postoperatively as compared to and 85.7% of white children (p<0.001). In addition, children who filled an opioid prescription were slightly older, had shorter lengths of stay, were less likely to have sickle cell disease, and were more likely to be treated at a hospital in a rural county or at a non-children’s hospital (Table 1). There were also several differences in both patient-level and institution-level characteristics between black and white pediatric cholecystectomy patients: black children were slightly younger, had longer lengths of stay, were more likely to be treated at a hospital in a large or medium-sized metro county, and were more than twice as likely as white children to be treated in a children’s hospital (Table 2).
Figure 1.
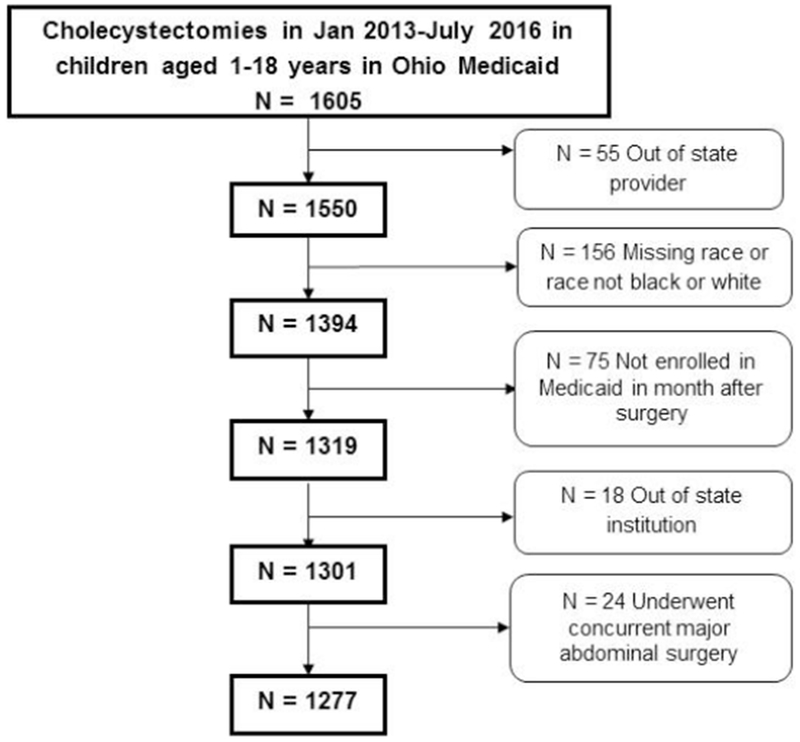
Cohort development
Table 1.
Characteristics of cholecystectomy patients and their treating institutions, by opioid prescription fill status
| Variable | Overall (N=1277) |
No Opioid within 14 days (N=202) |
Opioid fill within 14 days (N=1075) |
P |
|---|---|---|---|---|
| Age in years, median (Q1, Q3) | 16 (14, 17) | 16(13, 17) | 16(15, 17) | 0.02 |
| Race, n (%) | <.001 | |||
| White | 1094 (85.7) | 156(77.2) | 938(87.3) | |
| Black | 183 (14.3) | 46(22.8) | 137(12.7) | |
| Laparoscopic approach, n (%) | 1253 (98.1) | 190(94.1) | 1063(98.9) | <.001 |
| Postoperative length of stay (days) | 0 (0, 1) | 1(0, 2) | 0(0, 1) | <.001 |
| Sick cell disease, n (%) | 38 (3.0) | 12(5.9) | 26(2.4) | 0.007 |
| Urban/Rural Classification of Hospital County, n (%) | 0.07 | |||
| Large central metro | 398 (31.2) | 72(35.6) | 326(30.3) | |
| Large fringe metro | 93 (7.3) | 13(6.4) | 80(7.4) | |
| Medium metro | 372 (29.1) | 69(34.2) | 303(28.2) | |
| Small metro | 82 (6.4) | 12(5.9) | 70(6.5) | |
| Micropolitan | 299 (23.4) | 33(16.3) | 266(24.7) | |
| Noncore | 33 (2.6) | 3(1.5) | 30(2.8) | |
| Teaching Hospital, n (%) | 985 (77.1) | 166(82.2) | 819(76.2) | 0.06 |
| Children’s Hospital, n (%) | 456 (35.7) | 91(45.0) | 365(34.0) | 0.003 |
Table 2.
Characteristics of cholecystectomy patients and their treating institutions, by patient race
| Variable | Overall (N=1277) |
White (N=1094) |
Black (N=183) |
P |
|---|---|---|---|---|
| Age in years, median (Q1, Q3) | 16 (14, 17) | 16(15, 17) | 16(13, 17) | <.001 |
| Opioid Fill, n (%) | 1075 (84.2) | 938(85.7) | 137(74.9) | <.001 |
| Laparoscopic approach, n (%) | 1253 (98.1) | 1076(98.4) | 177(96.7) | 0.13 |
| Postoperative length of stay (days) | 0 (0, 1) | 0(0, 1) | 1(1, 2) | <.001 |
| Sick cell disease, n (%) | 38 (3.0) | 0(0.0) | 38(20.8) | <.001 |
| Urban/Rural Classification of Hospital County, n (%) | <.001 | |||
| Large central metro | 398 (31.2) | 290(26.5) | 108(59.0) | |
| Large fringe metro | 93 (7.3) | 90(8.2) | 3(1.6) | |
| Medium metro | 372 (29.1) | 309(28.2) | 63(34.4) | |
| Small metro | 82 (6.4) | 74(6.8) | 8(4.4) | |
| Micropolitan | 299 (23.4) | 298(27.2) | 1(0.5) | |
| Noncore | 33 (2.6) | 33(3.0) | 0(0.0) | |
| Teaching Hospital, n (%) | 985 (77.1) | 813(74.3) | 172(94.0) | <.001 |
| Children’s Hospital, n (%) | 456 (35.7) | 337(30.8) | 119(65.0) | <.001 |
After creating a composite variable defined by patient race, hospital location, and children’s hospital status, we found that black children treated at non-children’s hospitals in large or medium-sized metro counties were the least likely to fill an opioid prescription (Table 3). In multivariable regression analyses, we found that that black children treated at children’s hospitals were not significantly less likely to fill an opioid prescription than white children treated at children’s hospitals (probability ratio=0.97, p=0.41) (Table 4). However, black children treated at non-children’s hospitals were significantly less likely to fill an opioid prescription when compared to white children treated at children’s hospitals or non-children’s hospitals regardless of their location. Other factors independently associated with a higher rate of opioid prescription filling included older age and discharge on the same day or day following surgery (Table 4). A sensitivity analysis examining opioid prescription filling within 3 rather than 14 days of cholecystectomy yielded similar results to our analysis of opioid prescription filling within 14 days of cholecystectomy.
Table 3.
Numbers and percentages of pediatric patients who filled an opioid prescription after cholecystectomy by race, hospital location and children’s hospital status
| Procedure | Percent filling an opioid prescription within 14 days | Pb |
|---|---|---|
| Black children treated at non-children’s hospitals in large central metro and medium metro counties | 38/52 (73.1) | <0.001 |
| Black children treated at children’s hospitals in large central metro and medium metro counties | 90/119 (75.6) | |
| White children treated at non-children’s hospitals in large central metro and medium metro counties | 226/262 (86.3) a | |
| White children treated at children’s hospitals in large central metro and medium metro counties | 275/337 (81.6) a | |
| White children treated at non-children’s hospitals in other Ohio counties | 437/495 (88.3) ab |
P<0.05 vs. black children treated at non-children’s hospitals in large central metro and medium metro counties.
P<0.05 vs. white children treated at children’s hospitals and black children treated at either children’s or non-children’s hospitals.
Table 4.
Multivariable model for the filling of a postoperative opioid prescription after cholecystectomy
| Characteristic | Probability Ratio (95% CI) | P value |
|---|---|---|
| Patient race, hospital location, and children’s hospital status (composite variable) | ||
| Black children treated at non-children’s hospitals in large central metro and medium metro counties | ref | ---- |
| Black children treated at children’s hospitals in large central metro and medium metro counties | 1.13 (1.00-1.28) | 0.06 |
| White children treated at non-children’s hospitals in large central metro and medium metro counties | 1.15 (1.03-1.30) | 0.02 |
| White children treated at children’s hospitals in large central metro and medium metro counties | 1.16 (1.01-1.33) | 0.03 |
| White children treated at non-children’s hospitals in other counties | 1.16 (1.03-1.31) | 0.02 |
| Age group | ||
| <13 | ref | ---- |
| 13-15 | 1.11 (1.01-1.21) | 0.02 |
| 16-18 | 1.09 (0.99-1.20) | 0.06 |
| Postoperative length of stay (days) | ||
| 0 | ref | ---- |
| 1 | 0.96 (0.89-1.03) | 0.23 |
| 2 | 0.82 (0.69-0.96) | 0.02 |
| ≥3 | 0.76 (0.60-0.97) | 0.02 |
| Male | 0.96 (0.90-1.03) | 0.25 |
| Laparoscopic procedure | 1.30 (0.89-1.91) | 0.18 |
| Sickle cell disease | 0.97 (0.78-1.20) | 0.75 |
Discussion
This study demonstrates that a racial disparity exists in opioid prescription filling after pediatric cholecystectomy. Black children who are treated at urban non-children’s hospitals are significantly less likely to fill an opioid prescription than white children treated in the same hospitals or in urban children’s hospitals or non-urban general acute care hospitals. Whether or not opioids are necessary for the majority of pediatric patients after cholecystectomy is unclear, but the existence of a disparity in the receipt of postoperative opioids that is not driven by clinical factors is concerning.
Previous studies have demonstrated the existence of racial disparities in in-hospital pain management in children. In a study by Sadhasivam et al. that examined black and white children undergoing tonsillectomy, it was found that black children reported significantly more postoperative pain as evidenced by higher pain scores (18). This study also found that black children received higher doses of opioid medications as compared to white children. This is in contrast to a study by Goyal et al. that examined racial disparities in pain management in children undergoing treatment for acute appendicitis in the emergency department. This study found no differences in severity of illness or pain scores by race, but did find that black children were significantly less likely than white children to receive an opioid in the emergency department (7). In a broader study by Pletcher et al. that examined differences in opioid prescribing for patients of all ages who presented to the emergency department with pain, it was found that white patients were significantly more likely to receive an opioid prescription at discharge (14).
Similar to the study by Pletcher et al., we examined outpatient opioid prescribing in the acute setting. We found that black children treated at non-children’s hospitals were less likely to fill an opioid prescription than white children regardless of their treatment location. We also found that children with a shorter length of stay and older children were more likely to fill an opioid prescription. It is likely that patients who had longer lengths of stay received opioids in the hospital, and their pain may have largely resolved by the time of discharge, thus leading to a lower fill rate. It is unclear why black patients had longer postoperative lengths of stay overall, but this difference may be related to patient disease severity or comorbidities. Racial disparities in access to surgical care lead to greater disease severity at the time of presentation, as has been shown previously in a variety of illnesses (19).
Though racial disparities in the receipt of opioids after surgery are concerning, another concern among all surgical patients is the overprescribing of opioids. Previous studies in adults have shown significant variation and excess prescribing of opioids after routine surgery. One recent study that examined opioid prescribing and patient opioid use after five common outpatient surgical procedures found that only 28% of prescribed pills were taken (20). Another study of patients undergoing urologic surgical procedures found that 67% of patients had excess opioids prescribed (21). Due to a lack of information on clinical details and pain medication in the database used for our study, we are unable to determine whether the rates of opioid prescribing we found represent over-prescribing or under-prescribing. However, based on previous studies, there likely was some overprescribing in our study cohort, and our results indicate this may have disproportionately affected white children. Previous studies have demonstrated that white children are more likely to receive opioids when compared to black or other racial/ethnic minority children (22, 23). However, these studies are also unable to comment on whether over- or under-prescribing occurred due to a lack of clinical details. Goyal et al. looked at overall analgesia and opioid prescribing in the setting of pediatric acute appendicitis and found that after accounting for pain level, black children were less likely to receive opioid analgesia in the emergency department than white children, but there was no difference in overall rates of analgesic use by race (7). Further research is needed to understand the various patient and provider-level characteristics that may drive racial disparities in opioid prescribing and use.
Due to the nature of the data source used, this study had several limitations. We could look only at rates of postoperative opioid prescription filling. Therefore, we could not determine whether the detected disparity was driven by a lower rate of opioid prescribing or a lower rate of filling of received prescriptions among black children. Additionally, clinical details such as pain levels were not available. These types of data are needed for future research examining potential disparities in pain treatment in pediatric surgical patients. Lastly, because we had data only through August 2016, we were unable to examine the impact of Ohio’s August 2017 law limiting the quantity of postoperative opioids that can be prescribed (24). Future research should examine the impact of this policy and other similar policies at the state or health system level on racial disparities in the receipt of postoperative opioids.
Conclusion
Our study identified a racial disparity in opioid prescription filling after pediatric cholecystectomy, with black children treated at urban non-children’s hospitals being significantly less likely to fill an opioid prescription than white children, though this disparity was partly explained by a longer average length of stay among black children. Further research is needed to fully identify the sources of this disparity.
Acknowledgments
Declaration of interest: This study was funded by Grant #R21 MD011767 from the National Institute on Minority Health and Health Disparities of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- 1.Egan KL, Gregory E, Sparks M, Wolfson M. From dispensed to disposed: evaluating the effectiveness of disposal programs through a comparison with prescription drug monitoring program data. The American journal of drug and alcohol abuse. 2017;43(1):69–77. [DOI] [PubMed] [Google Scholar]
- 2.Anderson KO, Green CR, Payne R. Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care. The Journal of Pain. 2009;10(12):1187–204. [DOI] [PubMed] [Google Scholar]
- 3.Hewes HA, Dai M, Mann NC, Baca T, Taillac P. Prehospital Pain Management: Disparity By Age and Race. Prehospital Emergency Care. 2018;22(2): 189–97. [DOI] [PubMed] [Google Scholar]
- 4.Mossey JM. Defining Racial and Ethnic Disparities in Pain Management. Clinical Orthopaedics and Related Research®. 2011;469(7): 1859–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernabei R, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R, et al. Management of Pain in Elderly Patients With Cancer. Jama. 1998;279(23): 1877–82. [DOI] [PubMed] [Google Scholar]
- 6.Ortega HW, Vander Velden H, Lin C-W, Reid S. Race, ethnicity, and analgesia provision at discharge among children with long-bone fractures requiring emergency care. Pediatr Emerg Care. 2013;29(4):492–7. [DOI] [PubMed] [Google Scholar]
- 7.Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial Disparities in Pain Management of Children With Appendicitis in Emergency Departments. JAMA pediatrics. 2015; 169(11):996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ure BM, Troidl H, Spangenberger W, Dietrich A, Lefering R, Neugebauer E. Pain after laparoscopic cholecystectomy. Surgical Endoscopy. 1994;8(2):90–6. [DOI] [PubMed] [Google Scholar]
- 9.McMahon AJ, Russell IT, Ramsay G, Sunderland G, Baxter JN, Anderson JR, et al. Laparoscopic and minilaparotomy cholecystectomy: a randomized trial comparing postoperative pain and pulmonary function. Surgery. 1994;115(5):533–9. [PubMed] [Google Scholar]
- 10.Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical Characteristics and Risk Factors for Symptomatic Pediatric Gallbladder Disease. Pediatrics. 2012;129(1):e82–e8. [DOI] [PubMed] [Google Scholar]
- 11.Waldhausen JHT, Benjamin DR. Cholecystectomy is becoming an increasingly common operation in children. The American Journal of Surgery. 1999;177(5):364–7. [DOI] [PubMed] [Google Scholar]
- 12.Ohio Department of Medicaid. Programs for Children, Families, and Pregnant Women [Available from: http://medicaid.ohio.gov/FOR-OHIOANS/Programs/Children-Families-and-Women.
- 13.CPT and ICD-9 Codes for Bariatric Surgery: American Society for Metabolic and Bariatric Surgery; 2013. [Available from: https://asmbs.org/app/uploads/2012/01/1CPTandICD-9-Codes-for-Bariatric-Surgery-updated-Feb-2013d.pdf.
- 14.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. Jama. 2008;299(1):70–8. [DOI] [PubMed] [Google Scholar]
- 15.Green CR, Tait RC, Todd KH, Vallerand AH, Anderson KO, Baker TA, et al. The Unequal Burden of Pain: Confronting Racial and Ethnic Disparities in Pain. Pain medicine. 2003;4(3):277–94. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties [updated 5/6/2014. Available from: https://www.cdc.gov/nchs/data_access/urban_rural.htm.
- 17.Centers for Disease Control and Prevention. Analyzing prescription data and morphine milligram equivalents (MME) [updated 09/29/2017. Available from: https://www.cdc.gov/drugoverdose/resources/data.html.
- 18.Sadhasivam S, Chidambaran V, Ngamprasertwong P, Esslinger HR, Prows C, Zhang X, et al. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics. 2012;129(5):832–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haider AH, Scott VK, Rehman KA, Velopulos C, Bentley JM, Cornwell EE III, et al. Racial Disparities in Surgical Care and Outcomes in the United States: A Comprehensive Review of Patient, Provider, and Systemic Factors. Journal of the American College of Surgeons. 2013;216(3):482–92.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr.. Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Annals of surgery. 2017;265(4):709–14. [DOI] [PubMed] [Google Scholar]
- 21.Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of Postoperative Narcotics: A Look at Postoperative Pain Medication Delivery, Consumption and Disposal in Urological Practice. Journal of Urology. 2011;185(2):551–5. [DOI] [PubMed] [Google Scholar]
- 22.Groenewald CB, Rabbitts JA, Hansen EE, Palermo TM. Racial differences in opioid prescribing for children in the United States. Pain. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rasooly IR, Mullins PM, Mazer-Amirshahi M, van den Anker J, Pines JM. The Impact of Race on Analgesia Use among Pediatric Emergency Department Patients. The Journal of Pediatrics. 2014; 165(3):618–21. [DOI] [PubMed] [Google Scholar]
- 24.Prescribing of opiate analgesics for acute pain. Effective: August/31/2017, 4731-11-13 (2017). [Google Scholar]


