Abstract
Introduction:
Influenza infection is a viral disease with significant morbidity and mortality during the cold months. Clinical presentation typically includes cough, fever, and pain. Influenza disease is hardly diagnosed only on the basis of clinical symptoms due to similar clinical presentation of other diseases such as a typical cold or other flu-like diseases. We evaluated patients with proven influenza who presented at an emergency department of internal medicine in a university hospital according to the clinical presentation and different age groups.
Materials and Methods:
From October 2017 to April 2018, 723 reverse transcription-polymerase chain reaction (RT-PCR) tests for influenza were performed in the emergency department on patients with suspected influenza diagnosed clinically. A total of 240 influenza-positive patients were retrospectively assessed for documented main symptoms, vital parameters, risk factors for an unfavorable course, hospitalization, and death.
Results:
The mean age of influenza patients was 65 years. Overall, 30 patients were aged 18 to 39 years, 48 patients 40 to 59 years, and 162 patients ⩾60 years. Influenza B in 168 (70%) was predominant to 72 influenza A (mostly H1N1). In only 30% of the patients all three typical symptoms (cough, fever, and headache/myalgia) were documented. Headache or myalgia (with 34%) was rather uncommon in influenza B. Sudden onset was cited in only 5.4%; 57% of all influenza patients were in hospital for a mean of 7.1 days, and 5.8% of all influenza patients died. Patients aged above 60 years had more risk factors, showed typical symptoms less frequently, and were hospitalized longer than younger patients (<60 and <40 years).
Conclusions:
At an emergency department of internal medicine, influenza-diseased patients are of higher age, show an increased number of comorbidities, and are more likely to have milder symptoms documented. Elderly patients with influenza have a higher hospitalization rate with a longer hospital stay as compared with younger patients.
Keywords: Influenza, season, cough, fever, myalgia, headache, risk factors
Introduction
Influenza is a common human virus infecting the population during the cold winter months. In particular, the elderly population may suffer from severe and life-threatening disease. Frequently, clinical symptoms are myalgia, headache, fever, and cough, and in the case of influenza B infection, gastrointestinal symptoms.1 The clinical triad of cough, fever, and pain is held to be very indicative for influenza disease during the dedicated season, but they cannot distinguish from those of other viral respiratory tract infections. The absence of that triad cannot exclude influenza infection. Influenza may present as an exacerbation or complication of an underlying illness.2 Data in the literature focus on the elderly population or pediatric patients.3-7 Most of the patients recover from the illness without needing any intensive medical attention. However, increasing age and fragility due to comorbidities increase the risk of a severe course of influenza infection. Moreover, community outbreaks during the cold winter months can overload emergency departments and hospital units of internal medicine. In hospital, influenza patients need isolated rooms and more resources due to contagiosity of neighboring patients. According to the Robert Koch Institute (RKI) report, during the season 2017/2018, influenza disease caused increased health care visits in Germany to as high as 9 million medical visits, and thus increased by about 2 million (+28%) compared with the severe seasons of 2012/2013 and 2014/2015.8 A total of 68% of the influenza patients were aged above 60 years, and the hospitalization rate was much higher with 69% than in the group of <60 years with about 31%, too.
Our retrospective analysis was aimed at characterization of the clinical presentation and features of influenza-positive patients admitted to the emergency department of internal medicine of our university hospital in season 2017/2018 according to different age groups.
Materials and Methods
The retrospective study was performed at our emergency department of internal medicine with about 10 500 adult patients in the year 2017. Patients are admitted by self-motivation, after a visit of a referring outpatient doctor or by ambulance (sometimes with emergency doctor). The local ethics committee approved the retrospective analysis. The study complies with the ethics guidelines of the Helsinki Declaration. Between October 11, 2017, and April 27, 2018, all patients aged above 18 years with a reverse transcription-polymerase chain reaction (RT-PCR)-positive influenza test were included. The reverse transcription-polymerase chain reaction was performed in patients with suspicion of influenza, presenting singular or several symptoms of flu diseases or just for exclusion of influenza disease (question of isolating patients within the care units).
In these 7 months, 723 RT-PCR tests for influenza were performed in the emergency department, 249 (34.4%) of which were positive. Nine patients needed to be excluded due to missing clinical data—these patients were apparently only tested. Children (aged <18 years) present specifically in the children’s hospital and therefore, they were not part of our baseline cohort. The remaining 240 patients were assessed for epidemiological, clinical, laboratory, and radiological profile, as well as outcome (need for and duration of hospitalization and/or death). Patients were grouped according to the circulating influenza subtype A (H1N1 or H3N2) or B and divided into 3 different age groups (<40 years [ie 18-39 years], 40-60 years, and ⩾60 years).
Influenza testing was performed by taking nasal and pharyngeal swabs that were sent to the virology laboratory for RT-PCR testing by Xpert® Xpress Flu/RSV (Cepheid, Sunnyvale, CA, USA). Subtyping of influenza A-positive samples was performed by type-specific in-house PCR assays for the H1pdm2009 and H3 hemagglutinin gene as described previously.9,10 We chose 6 documented risk factors for a severe course or complications of the influenza disease indicating the use of neuraminidase inhibitors: age ⩾ 60 years, chronic obstructive pulmonary disease (COPD), diabetes mellitus, cardiac insufficiency, immunosuppression, or neurologic disorders (previous stroke or ongoing neurologic disease with motor impairment).11 Immunosuppression included immunosuppressant drugs or patients who have received chemotherapy. Conditions such as home nursing, bed confinement, or pregnancy were also evaluated. Documented symptom onset (sudden or not), duration of symptoms before admittance to the emergency department, and documented clinical symptoms such as cough, sputum, fever (including body temperature >38°C, feverishness [subjective feeling of fever], and shivering) as well as headache or myalgia were surveyed. Additional features such as heart rate (per minute), respiratory rate (per minute), systolic blood pressure (mmHg), and O2 saturation (%) and such as need for and duration of hospitalization, suspicion of consolidation in a chest X-ray, and initial application of a first dose of a neuraminidase inhibitor (oseltamivir) or of antibiotics were analyzed. Analysis of laboratory investigation at the time of presentation in the emergency department included leukocytes (normal: 4-10 × 103/µL), thrombocytes (normal: 160-400 × 103/µL), and C-reactive protein (normal: <5 mg/L). The presence of secondary bacterial infection, sometimes observed within the course of disease, was not checked.
For statistical analysis, clinical and laboratory parameters were expressed as mean ± standard deviation together with the range in square brackets. The t-test was used to compare mean values. Results were considered statistically significant for P < .05 and statistically highly significant for P < .001. All reported P-values are two-sided. Statistical analysis was performed using the Statistical Package for the Social Sciences (Version 24.0.0.2; IBM Corp, Armonk, NY, USA).
Results
Patients’ characteristics
From 723 RT-PCR tests for influenza performed in the emergency department of internal medicine during season 2017/2018, a total of 240 positive tested adult patients (132 females and 108 males, mean age: 65 years) were included in the final analysis. Of which, 168 (70%) patients were diagnosed with influenza B (95 females and 73 males, mean age: 68 years), whereas 72 patients had influenza A (64 [27%] H1N1, 6 (3%) H3N2, and 2 without typing possible) with a mean age of 57 years (Table 1). In some cases, data were insufficient or missing or examination not performed (see tables).
Table 1.
Overall characteristics of the 240 patients with positive influenza RT-PCR testing.
| Total | A | B | |
|---|---|---|---|
| No. of patients | 240 | 72 | 168 |
| Sex (female/male) | 132/108 | 37/35 | 95/73 |
| Age (years) | 65 ± 18 [18-94] | 57 ± 19 | 68 ± 17** |
| Systolic blood pressure (mmHg) | 140 ± 22 [73-199] | 138 ± 22 | 140 ± 22 |
| Heart rate (per minute) | 89 ± 18 [55-151] | 93 ± 17 | 87 ± 19* |
| Respiratory rate (per minute) | 19 ± 5 [10-40] | 19 ± 5 | 20 ± 5 |
| O2 saturation (%) | 95 ± 4.3 [64-100] | 95.5 ± 3.7 | 94.6 ± 4.5 |
| Leukocyte (× 103/µL) | 7.13 ± 4.7 [0.43-37.09] | 7.32 ± 5.1 | 7.04 ± 4.5 |
| Thrombocyte (× 103/µL) | 191.6 ± 79 [9-720] | 182.6 ± 59 | 195.2 ± 86 |
| CRP (mg/L) | 51 ± 63 [0.6-360.6] | 60 ± 78 | 47.3 ± 55 |
| Sudden onset of symptoms | 13 (5%) | 8 (11%) | 5 (3%) |
| Duration of symptoms (days) | 5.2 ± 5.4 [0.12-42] | 5.0 ± 6.7 | 5.3 ± 4.7 |
| No. of symptoms (out of 3) | 1.9 ± 1.2 | 2.0 ± 1.3 | 1.8 ± 0.9 |
| Cough | 200 (83%) | 62 (86%) | 138 (82%) |
| Headache/myalgia | 90 (38%) | 39 (54%) | 57 (34%) |
| Fever/shivering | 146 (62%) | 45 (63%) | 101 (60%) |
| Sputum | 62 (26%) | 14 (19%) | 48 (29%) |
| No. of risk factors (out of 6) | 1.5 ± 1.2 [0-6] | 1.2 ± 1.2 | 1.7 ± 1.2* |
| Age ⩾ 60 years | 162 (68%) | 36 (50%) | 126 (75%) |
| COPD | 48 (20%) | 11 (15%) | 37 (22%) |
| Diabetes mellitus | 52 (22%) | 12 (17%) | 40 (24%) |
| Cardiac insufficiency | 27 (11%) | 7 (10%) | 20 (12%) |
| Immunosuppression | 42 (18%) | 8 (11%) | 34 (20%) |
| Neurologic disorders | 32 (13%) | 5 (7%) | 27 (16%) |
| Nursing home/bed confinement | 21 (9%) | 3 (4%) | 18 (11%) |
| Pregnancy | 2 (1%) | 2 (3%) | 0 |
| Suspicion of infiltrate in X-ray | 52 (22%) | 19 (26%) | 34 (20%) |
| First antibiotics | 119 (50%) | 32 (44%) | 87 (52%) |
| Oseltamivir | 194 (81%) | 56 (78%) | 138 (82%) |
| Hospitalization | 136 (57%) | 32 (44%) | 104 (62%) |
| Duration of hospitalization (days) | 7.1 ± 4.1 [1-22] | 7.6 ± 4.9 | 6.9 ± 3.8 |
| Mortality | 14 (5.8%) | 5 (7%) | 9 (5.4%) |
Abbreviations: COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; RT-PCR, reverse transcription-polymerase chain reaction.
Missing data: heart rate (n = 1), respiratory rate (n = 12), O2 saturation (n = 1), systolic blood pressure (n = 2), leucocytes/thrombocytes (n = 9), CRP (n = 8), and duration of symptoms (n = 19). Data are represented as mean ± standard deviation [range].
[Range], *P < .05, **P < .001.
Sudden onset of symptoms was documented in only 5.4% of influenza-positive cases and less frequently in influenza B patients. The most frequently documented symptom was cough (83%). Fever (61%), headache/myalgia (31%), and sputum (26%) were observed less frequently. The presence of headache or myalgia was lower in influenza B than in A. Overall, on average, 2 documented symptoms out of the 3 main symptoms were presented with a mean symptom duration of 5.2 days before admission to the emergency department. Analyses of the average number of the documented symptoms (out of 3) presented in the emergency department (Table 2) showed that, on average, 2.7 symptoms were presented in the first group <40 years, as opposed to 1.6 of the patients aged ⩾60 years (P = .0001, Figure 1). Documented duration of symptoms was shorter in the group of <40 years. Younger patients went often self-motivated to the emergency department (65%), elderly rarely (19%, Table 2).
Table 2.
Symptomatic appearance of influenza illness according to age groups.
| <40 years (n = 30) |
40-59 years (n = 48) |
⩾60 years (n = 162) |
|
|---|---|---|---|
| Duration of symptoms (days) | 3.3 ± 2.9 | 5.4 ± 7.8 | 5.5 ± 4.8* |
| No. of symptoms (out of 3) | 2.7 ± 0.5 [2-3] | 2.0 ± 1.0 [0-3] | 1.6 ± 0.8 [0-3]** |
| 0 | 0 | 5 (10.4%) | 12 (7.4%) |
| 1 | 0 | 8 (16.7%) | 58 (36%) |
| 2 | 9 (30%) | 18 (37.5%) | 68 (42%) |
| 3 | 21 (70%) | 17 (35.4%) | 24 (15%) |
| Cough | 28 (93%) | 38 (79%) | 134 (83%) |
| Fever/shivering | 28 (93%) | 32 (67%) | 86 (53%) |
| Headache/myalgia | 25 (83%) | 25 (52%) | 45 (28%) |
| Emergency admission by | |||
| Self-motivation | 19 (65%) | 25 (58%) | 29 (19%) |
| Referring outpatient doctor | 4 (14%) | 8 (18.5%) | 31 (20%) |
| Ambulance | 6 (21%) | 8 (18.5%) | 75 (49%) |
| Preclinical emergency doctor | 0 | 2 (5%) | 18 (12%) |
Missing data: type of emergency admission (n = 15).
[Range], *P < .05, **P < .001.
Figure 1.
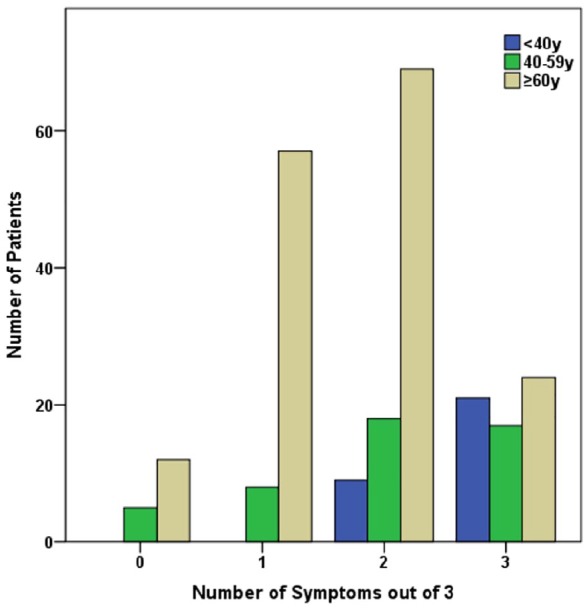
Symptoms (cough, fever, or headache/myalgia) presented by influenza patients (n = 240) according to age groups.
Risk factors, in general, describe the individual condition of a person that makes him or her more affectable for a disease or for a more severe course of it. The analysis of the 6 main risk factors (Table 3) showed age to be the most frequent risk factor, followed by diabetes mellitus, COPD, and immunosuppression. The oldest group (⩾60 years) has highly significantly more documented risk factors and consequently, a higher hospitalization rate with a longer duration than the younger groups. Patients with influenza B had more risk factors than patients with influenza A (P = .0023). Patients aged <40 years had fewer risk factors than the other, older patient groups (Figure 2). About one-fourth of the elderly patients showed no additional dedicated and documented risk factor except advanced age (⩾60 years). Patients with immunosuppression (n = 42) showed significantly fewer documented main symptoms (mean number: 1.8) than patients without immunosuppression (mean number: 2.2, P = .042). The subanalysis of the remaining 198 patients (without immunosuppression) showed fewer documented symptoms with increasing age as it was shown in all patients. Overall, 57% of the influenza patients were cared for in hospital. The average duration of hospitalization overall was 7.1 ± 4.1 days [1-22], without a statistically significant difference between influenza A and B patients (7.6 versus 6.9 days, respectively). Rate and duration of hospitalization were higher in the elderly group (⩾60 years; Figure 3). Patient age, the average number of risk factors, and the respiratory rate among patients hospitalized were significantly higher than those who left the emergency department in an outpatient setting (P < .0001, P = .001, and P < .0001, respectively).
Table 3.
Number of risk factors (age, COPD, cardiac insufficiency, diabetes mellitus, neurologic disorders, or immunosuppression) and hospitalization according to age groups.
| <40 years (n = 30) |
40-59 years (n = 48) |
⩾60 years (n = 162) |
|
|---|---|---|---|
| Risk factors | 0.3 ± 0.7 [0-3] | 0.4 ± 0.7 | 2.1 ± 1 [1-6]** |
| 0 | 21 (72%) | 31 (65%) | 0 |
| 1-2 | 8 (25%) | 16 (33%) | 114 (70%) |
| 3-4 | 1 (3%) | 1 (2%) | 43 (27%) |
| 5-6 | 0 | 0 | 5 (3%) |
| Suspicion of infiltrate in X-ray | 2 (7%) | 6 (13%) | 45 (28%) |
| Antibiotics | 4 (13%) | 16 (34%) | 99 (61%) |
| Outpatient | 23 (77%) | 31 (65%) | 50 (31%) |
| Hospitalization | 7 (23%) | 17 (35%) | 112 (69%) |
| Mean duration | 7.4 ± 7.6 [1-22] | 5.1 ± 2.5 [1-10] | 7.2 ± 4 [1-19]** |
| Duration of hospitalization (days) | |||
| 1-3 | 3 (43%) | 4 (24%) | 21 (19%) |
| 4-7 | 1 (14%) | 9 (52%) | 44 (39%) |
| 8-10 | 1 (14%) | 4 (24%) | 30 (27%) |
| >10 | 2 (29%) | 0 | 17 (15%) |
Abbreviation: COPD, chronic obstructive pulmonary disease.
[Range], **P < .001.
Figure 2.
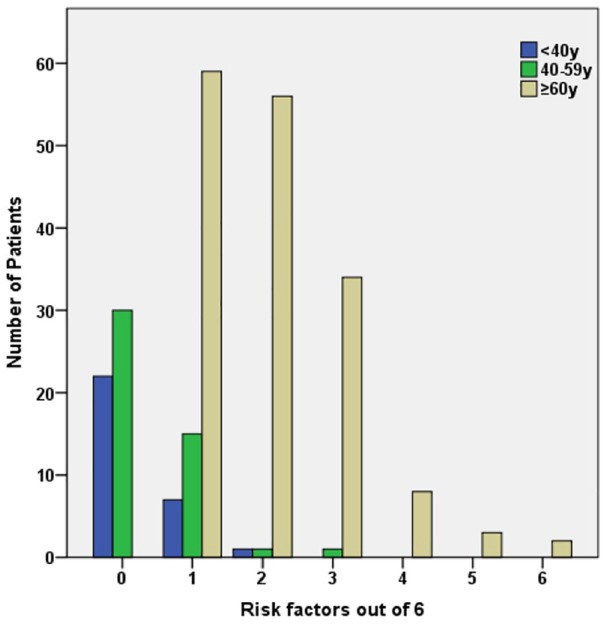
Risk factors (age, COPD, cardiac insufficiency, diabetes mellitus, neurologic disorders, or immunosuppression) presented by influenza patients (n = 240) according to age groups. COPD indicates chronic obstructive pulmonary disease.
Figure 3.
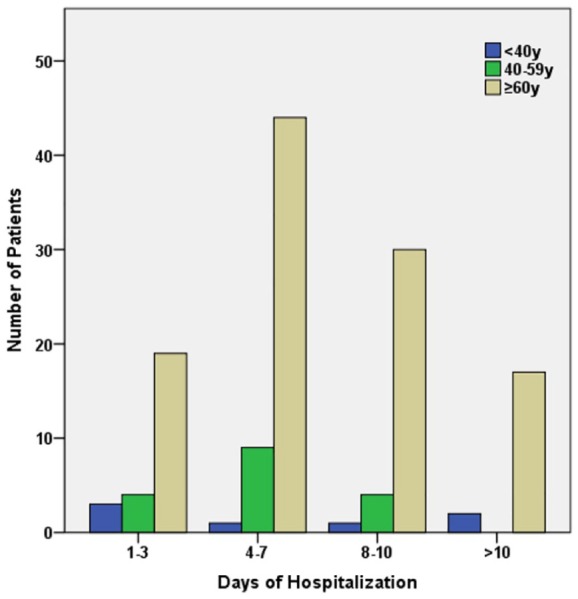
Duration of hospitalization of n = 134 (57%) of all influenza patients according to age groups.
A possible infiltrate in a chest X-ray was suspected in 22%. Initial treatment included antibiotics in 50% and a neuraminidase inhibitor (oseltamivir) in 81%. Out of our 240 analyzed patients, a total of n = 14 (5.8%) died during hospitalization. Of them, 2 patients were <60 years (mortality: 2.6%) and 12 patients were ⩾60 years (mortality: 7.4%, Table 4); 5 had influenza A (mortality: 7%) and 9 suffered from influenza B (mortality: 5.4%). These patients died mostly (83%) within 7 days after admission and showed in average only 1 out of 3 typical symptoms. Moreover, the number of risk factors documented was in average 3 including the age and thus was higher than that of the survivors (Table 4).
Table 4.
Characteristics of influenza patients with mortality aged ⩾60 years (n = 12).
| Elderly with mortality | Elderly hospitalized survivors | |
|---|---|---|
| Age ⩾60 years | 12 (100%) | 100 (100%) |
| Mean age (years) | 76.6 ± 6 | 77 ± 8 |
| Respiratory rate (per minute) | 22 ± 6 [15-36] | 21 ± 6 [13-40] |
| Heart rate (per minute) | 89 ± 22 [59-126] | 89 ± 19 [55-140] |
| Systolic blood pressure (mmHg) | 134.8 ± 24 [95-176] | 142 ± 24 [73-199] |
| Duration of symptoms (days) | 4.8 ± 3.3 | 6 ± 5.4 |
| No. of symptoms (out of 3) | 1.0 ± 1 | 1.54 ± 0.8* |
| Cough | 7 (58%) | 83 (83%) |
| Fever/feverishness | 3 (25%) | 52 (52%) |
| Headache/myalgia | 2 (17%) | 18 (18%) |
| No. of risk factors (out of 6) | 3.1 ± 1 [1-5] | 2.1 ± 1** |
| Duration of hospitalization (days) | ||
| 1-3 | 3 (25%) | 18 (18%) |
| 4-7 | 7 (58%) | 37 (37%) |
| 8-10 | 0 | 30 (30%) |
| >10 | 2 (17%) | 15 (15%) |
[Range], *P < .05, **P < .001.
Discussion
Pronounced incidence of influenza disease during winter months is generally due to influenza A in up to 85% of cases.8,12 In winter 2017/2018, RT-PCR-positive tested adult patients (⩾18 years) in our emergency department had mainly influenza B (70%) compared with influenza A (30%). In our retrospective analysis of all influenza cases at our emergency department, sudden onset of symptoms was rarely documented (5.4%). Symptoms had been present for 5 days on average before presentation at the emergency department. In other studies, influenza patients with complaints longer than 3 or 7 days were excluded.1,13,14 Neuraminidase inhibitors may alleviate the course of the disease, particularly if administered within 48 hours of onset. We started treatment directly in our emergency department in 81% of patients. In similar settings, oseltamivir is administered in up to 88.7%, also after a delayed admission.2,12,13 The effectiveness of oseltamivir may be questioned. We started the first dose of oseltamivir immediately in case of suspicion of influenza disease and risk of severe course in the emergency department. Considering a positive rate of influenza testing of about 1/3, a relevant proportion of patients were treated without having an influenza illness. We justify this procedure given the low side effects of oseltamivir after one first dose, the relevant mortality of influenza, and being at an emergency department with high incidence of influenza. Moreover, this retrospective study was limited to RT-PCR-positive influenza cases, and some patients admitted to the emergency department may have had health complications exacerbated by a waning influenza infection which could not be detected by RT-PCR.
Patients aged above 60 years showed more documented risk factors, presented with milder or missing typical symptoms, had been suffering from symptoms a longer time before admission, and were hospitalized more often and longer than younger patients (<60 and <40 years). Patients with influenza (<60 years) presented mainly (61%) self-motivated without contacting an outpatient doctor, whereas 49% of patients aged ⩾60 years were admitted by ambulance. In addition, our data show cough and fever to be the most important documented symptoms of influenza disease,15 although the complete triad of cough, fever, and myalgia was only present in 26%. In the literature, the cluster of fever, cough, and sore throat occurs in only 31% of influenza cases.4
A clinical diagnosis algorithm—based on the presence of all 3 traditional symptoms—for the detection of influenza in the elderly in the cold months should be used restrictively, since 68% of our influenza cases were elderly people (⩾60 years) showing fewer or milder documented symptoms in comparison with younger patients <60 or <40 years.
Choi et al13 conducted a retrospective, multicenter study of 1405 influenza-positive patients who were predominantly young with 42.9 years. The hospitalization rate was 21% and mortality 3.1% and were therefore lower than in our cohort. Fever and cough were the most frequent signs of influenza. Mean age of patients, rate of influenza B, and hospitalization rate (28.9%) were higher in case of a late diagnosis of influenza disease (diagnosis 4-7 days after symptom onset). According to our data, influenza B was predominant with high patient ages and also with a late diagnosis. N = 53 (22%) of all influenza patients presented no risk factors allowing for outpatient care (n = 38, 72%) or a short duration hospitalization (⩽3 days). Influenza disease might deteriorate concomitant diseases, and anticipating course of disease is difficult, leading to a high hospitalization rate of the elderly. Besides age, diabetes, COPD, and immunosuppression were the most common risk factors in our cohort. In literature, the incidence of comorbidities in influenza disease is reported to be for up to 76%, with mainly arterial hypertension or diabetes.2,4,12,15
In our cohort, duration of hospitalization was about 7 days and mortality 5.8%. Data of 65 influenza A patients showed a mortality of 15.4% during a mean of 6.3 days of hospitalization15; 61.5% had a suspicion of pneumonic infiltrates upon chest X-ray in contrast to 22% in our study. In another study, 1726 hospitalized patients (mean age: 64 years) stayed in hospital for on average 14.8 days and had a mortality of 13%.12 Age and immune deficiency (mainly in type B influenza) were associated with mortality. Our patients with immunosuppression (n = 42) had also predominantly influenza B and showed significantly fewer documented symptoms. Our analysis of the lethal courses of influenza infection indicates that the sum of documented risk factors seems to predict mortality as in contrast, the presenting complex of symptoms cannot. Due to the plurality of patients, establishing a precise prognosis tends to be difficult.16 Figures from these different studies may be difficult to interpret because there are differences in geographic location (Asia1,15 versus North America)4, circumstances (outpatient2 versus hospital)12, patient age (rather young13 versus old),4,12 and type of influenza (A or B).
The power of our findings is limited by certain weaknesses, for example, the retrospective nature of the study. Details of the medical history may be lost in contrast to a standardized, prospective approach. Another drawback might be the fact that the sample size was quite small. Nevertheless, tendencies and statistically significant findings could be shown. Information concerning preceding visits or outpatient contacts before admission to the emergency department was not available. We have no details on influenza vaccination of our patients. Observed characteristics of influenza infection may vary depending on the setting. We showed an evaluation in an emergency department of internal medicine dealing with selected outpatient and pre-hospitalized patients. In an outpatient setting or a common general emergency center, the question of influenza relies more easily on clinical symptoms or may be less frequent. Nevertheless, our observations empower emergency physicians to think of influenza disease more often in their decision-making process for testing and administering antivirals.17,18
In conclusion, at an emergency department, influenza-diseased patients are of higher age and show an increased number of comorbidities and quite rarely the typical symptoms. Elderly patients with influenza are more likely to have milder symptoms and have a high hospitalization rate with a longer hospital stay as compared with younger patients. The observed delay of diagnosis should lead to an earlier contact to health care and proof of influenza by RT-PCR testing, particularly in elderly patients with risk factors, even without having all typical symptoms.
Acknowledgments
The present work was performed in fulfillment of the requirements for obtaining the degree “Dr. med. dent.” for Sonia Mohammad.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interest:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SM wrote the manuscript. SM, KK and RSG collected and analyszed the data. MFN and RSG projected the study. All authors critically reviewed and approved the final manuscript.
Data Accessability: An XLS and SPSS archive does not show dedicated patient ID numbers.
ORCID iD: Ruediger S Goertz  https://orcid.org/0000-0002-6998-6635
https://orcid.org/0000-0002-6998-6635
References
- 1. Kaji M, Watanabe A, Aizawa H. Differences in clinical features between influenza A H1N1, A H3N2, and B in adult patients. Respirology. 2003;8:231-233. [DOI] [PubMed] [Google Scholar]
- 2. Irving SA, Patel DC, Kieke BA, et al. Comparison of clinical features and outcomes of medically attended influenza A and influenza B in a defined population over four seasons: 2004-2005 through 2007-2008. Influenza Other Respir Viruses. 2012;6:37-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Falsey AR, McElhaney JE, Beran J, et al. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis. 2014;209:1873-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lam PP, Coleman BL, Green K, et al. Predictors of influenza among older adults in the emergency department. BMC Infect Dis. 2016;16:615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Al Subaie SS, Al Saadi MA. Features associated with severe disease in hospitalized children with 2009 influenza A (H1N1) infection at a university hospital in Riyadh, Saudi Arabia. Ann Saudi Med. 2012;32:53-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hong KW, Cheong HJ, Song JY, Noh JY, Yang TU, Kim WJ. Clinical manifestations of influenza A and B in children and adults at a tertiary hospital in Korea during the 2011-2012 season. Jpn J Infect Dis. 2015;68:20-26. [DOI] [PubMed] [Google Scholar]
- 7. Zhang T, Zhu Q, Zhang X, et al. The clinical characteristics and direct medical cost of influenza in hospitalized children: a five-year retrospective study in Suzhou, China. PLoS ONE. 2012;7:e44391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buda S, Prahm K, Dürrwald R, et al. Report of the epidemiology of influenza in Germany for the 2017/18 season. Berlin: Robert Koch Institute (RKI); 2018. [Google Scholar]
- 9. Panning M, Eickmann M, Landt O, et al. Detection of influenza A(H1N1)v virus by real-time RT-PCR. Euro Surveill. 2009;14:19329. [PubMed] [Google Scholar]
- 10. Schulze M, Nitsche A, Schweiger B, Biere B. Diagnostic approach for the differentiation of the pandemic influenza A(H1N1)v virus from recent human influenza viruses by real-time PCR. PLoS ONE. 2010;5:e9966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization. WHO guidelines for pharmacological management of pandemic influenza A(H1N1) 2009 and other influenza viruses. Geneva: WHO; 2010. [PubMed] [Google Scholar]
- 12. Martinez A, Soldevila N, Romero-Tamarit A, et al. Risk factors associated with severe outcomes in adult hospitalized patients according to influenza type and subtype. PLoS ONE. 2019;14:e0210353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Choi SH, Chung JW, Kim T, Park KH, Lee MS, Kwak YG. Late diagnosis of influenza in adult patients during a seasonal outbreak. Korean J Intern Med. 2018;33:391-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pedersen CJ, Quinn JV, Rogan DT, Yang S. Factors associated with influenza in an emergency department setting. J Emerg Med. 2019;56:478-843. [DOI] [PubMed] [Google Scholar]
- 15. Kshatriya RM, Khara NV, Ganjiwale J, Lote SD, Patel SN, Paliwal RP. Lessons learnt from the Indian H1N1 (swine flu) epidemic: predictors of outcome based on epidemiological and clinical profile. J Family Med Prim Care. 2018;7:1506-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rath B, Penttinen P. Incidence, severity and impact of influenza: a joint meeting organised by the ISIRV epidemiology group and ECDC, Stockholm, 2019. Euro Surveill. 2019;24(23):1900348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bassetti M, Castaldo N, Carnelutti A. Neuraminidase inhibitors as a strategy for influenza treatment: pros, cons and future perspectives. Expert Opin Pharmacother. 2019;20:1711-1718. [DOI] [PubMed] [Google Scholar]
- 18. Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the infectious diseases society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68:895-902. [DOI] [PMC free article] [PubMed] [Google Scholar]


