Abstract
Penile prosthetic surgery is an effective treatment for men with erectile dysfunction. Cancellation of surgery is disruptive and costly to patients, physicians, and the healthcare system. This pilot study sought to analyze surgery cancellations and implement a video-based patient education program to decrease surgery noncompletion.
Baseline penile prosthetic surgery completion, rescheduling, and cancellation rates among consecutively scheduled surgeries were determined using a national cohort. Selected prosthetic surgeons then implemented Vidscrip, a video-based patient education program. Prerecorded videos were delivered via text message 14 days, 7 days, and 1 day preoperatively, as well as 1 day postoperatively. Subsequent analysis determined noncompletion rates, reasons for noncompletion, surgeon volume, and video utilization.
Two-hundred twenty-six surgeries were scheduled in the baseline cohort; 141 were completed, and 85 were rescheduled or canceled. Among the intervention cohort, 290 patients completed, 7 rescheduled, and 37 canceled surgery. After program implementation, the surgery noncompletion rate was reduced compared to baseline (13.2% vs. 37.6%, p < .05), corresponding to a number needed to treat of 4.1. When stratified by surgeon volume, there was no difference in noncompletion rate (>20 cases vs. ≤20 cases: 8.20% vs. 32.0%, p = .35). Video utilization was widely variable among practices (median viewing time 58.6 min, IQR 5.09–113).
Penile prosthetic surgery is frequently rescheduled or canceled. Implementing a video-based patient education program reduces surgery noncompletion, improving efficiency and quality of care. Wider implementation is needed to validate these findings, while cost-effectiveness analyses may further support their broad adoption.
Keywords: Penile implantation, quality improvement, physician–patient relations, patient-centered care, information technology
Surgery rescheduling or cancellation represents a significant cost and inefficiency shared by patients, families, surgeons, and the health care system. Among urologic surgeries, non-oncologic elective procedures are subject to the highest rate of cancellation, with some reporting as high as 15% on the day of surgery, with nearly 60% modifiable causes for cancellation (Leslie et al., 2013). The reasons for surgery cancellation are myriad; however, they include patient factors (decision for surgery, scheduling conflict), structural factors (operating room availability, anesthesia/staff availability), and medical factors (comorbid condition, change in condition, and unexpected illness) (Keller et al., 2014). Risk factors for cancellation of elective surgeries have been evaluated and include patient illness, socioeconomic status, and afternoon scheduling (Tan et al., 2019).
Multiple interventions in the broader literature have achieved a reduction in surgery cancellation, including nurse telephone screening, preoperative anesthesia clinic assessment, and streamlined electronic scheduling procedures (Hovlid et al., 2012; Olson & Dhakal, 2015; Singhal et al., 2014). Furthering this work, the concept of the perioperative surgical home offers patients navigation through the complex process of preoperative assessment, perioperative education and aligning of expectations, and postoperative evaluation (Silvay et al., 2016). No prior evaluations have been established to demonstrate reduction in cancellation of penile prosthetic surgeries. Therefore, the authors elected to develop a technology-based educational platform as a low-cost intervention to serve as a perioperative surgical electronic “home.”
A pilot study was designed to evaluate whether this video-based patient education program would reduce the rate of rescheduling and cancellation of elective penile prosthetic surgery. This study sought to understand the baseline rates of surgery noncompletion and to empower surgeons with technology that aims to assist with perioperative surgical education. The authors proposed to evaluate the impact of the intervention upon surgery noncompletion and to understand reasons for surgery noncompletion. Analysis of groups by surgeon volume was performed to evaluate whether this surgical practice characteristic would impact surgery noncompletion rates.
Materials and Methods
This analysis represents a prospective cohort study among men undergoing penile prosthesis surgery, utilizing a deidentified industry-reported database to identify surgical case data regarding surgery completion, rescheduling, and cancellation, as well as data regarding video utilization. Reasons for cancellation were abstracted by surgeon offices and categorized into one of four prespecified factors. The baseline population was comprised of men undergoing penile prosthesis surgery within California and Colorado during a specified time period before the intervention was implemented. The intervention population comprised of men undergoing penile prosthesis surgery performed by selected surgeons, whose offices elected to participate in the intervention. The population was accrued via consecutive cases performed during a prespecified time period. Surgeons included within the study represented academic and nonacademic practices, fellowship, and nonfellowship trained surgeons, and all geographic regions.
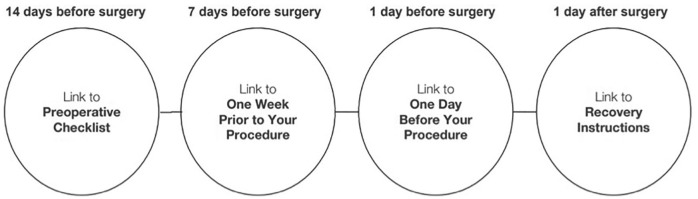
The intervention was a video-based patient educational instruction program developed in conjunction with a patient engagement startup company (Vidscrip) to develop and distribute the videos using their technological platform. The instructional videos were developed by individual surgeons and contained preoperative education, expectations, and recovery instructions. These videos were then distributed via text message 14 days, 7 days, and 1 day preoperatively as well as 1 day postoperatively (Figure 1).
Figure 1.
Schematic of Perioperative Instructional Video Schedule.
The primary outcome was the rate of surgery noncompletion on the initially scheduled day, with surgery rescheduling and cancellation also tabulated. The secondary outcome was the reason for surgery noncompletion, categorized via prespecified reasons based upon prior literature—these encompassed broad categories including patient factors, facility factors, and surgical personnel (Argo et al., 2009). Reasons for procedure cancellation or rescheduling were reported by individual surgeon offices. Patient decision-making was defined as the decision to pursue elective penile prosthetic surgery. The sample size was determined by convenience; a power calculation would not have been possible because the intervention effect magnitude was unable to be determined as no similar intervention has been published in the literature for this population. Similarly, patients were unable to be blinded to the intervention and thus no randomization was performed within this pilot study. Cluster randomization was not performed by surgeon so as not to deprive specific patient groups from experiencing the intervention. Patients within the group not receiving the intervention received standard perioperative care as performed by each individual surgeon’s office. Video data including the total number of views as well as the total viewing time was tabulated for each individual surgeon practice during the study period.
Statistical analysis was performed to assess the impact of the intervention on primary and secondary outcomes. Overall completion, rescheduling, and cancellation rates were tabulated for both groups. Reasons for noncompletion were also tabulated for the intervention and baseline groups separately. Relative risk of noncompletion and number needed to treat were determined. Among surgeons participating in the intervention, a volume analysis was performed to compare noncompletion rates among surgeons completing >20 cases versus ≤20 cases over the study period, with t-test performed. Video viewing data were tested for equality using the Kruskal–Wallis test for equality among high-volume and low-volume surgeons (Quandt, 1960). All statistical analyses were performed using Stata 13.1. The study was exempted from institutional review board oversight as no patient identifying data was abstracted.
Results
Baseline cohort data were established between January and September 2018, during which 226 men were scheduled and reached their surgery date. Subsequently, the intervention was implemented in selected surgeon offices between July 2018 and March 2019. During this period, 334 men were scheduled for surgery and reached their surgery date by study completion; these men comprised the intervention cohort.
Data analysis was performed according to the assigned groups. Among the baseline group, 85 (37.6%) men rescheduled or canceled their surgery, while 141 (62.4%) men completed surgery. Among men receiving the intervention, 44 (13.2%) rescheduled or canceled surgery, while 290 (86.8%) completed surgery. The relative risk of surgery noncompletion was 0.35 among men receiving the intervention (95% CI 0.25–0.48, p < .0001); this corresponds to a number needed to treat of 4.1 (95% CI 3.2–5.7).
Reasons for cancellation differed between the two groups (Table 1). The top three reasons for surgery noncompletion among the baseline population were patient decision-making (32%), scheduling changes (30%), and incomplete medical clearance (25%); in the intervention population, the top three reasons for noncompletion were scheduling changes (46%), unknown/other (22%), and incomplete medical clearance (19%). A reduction of noncompletion rate was observed among men receiving the intervention compared to baseline (13.2% vs. 37.6%, p < .05).
Table 1.
Reasons for Surgery Cancellations Among Men Receiving the Patient Education Intervention.
| Reasons for cancellation (%) | Baseline | Intervention |
|---|---|---|
| Reversed decision for surgery | 32 | 13 |
| Schedule change | 30 | 46 |
| No medical clearance | 25 | 19 |
| Unknown/other | 13 | 22 |
Surgeons who completed the intervention were assessed for difference in noncompletion rate by volume of cases over the study period (Table 2). Among surgeons performing more than 20 cases during the study period, there was a decreased noncompletion rate compared to surgeons performing less than 20 cases, although the difference was not statistically significant (8.20% vs. 30.0%, p = .35).
Table 2.
Cases Completed, Canceled, and Rescheduled: Stratified by Individual Surgeon Practice After Implementation of Patient Education Intervention.
| Surgeon | Total cases | Completed cases | Canceled cases | Rescheduled cases | Cancellation/rescheduling rate (%) |
|---|---|---|---|---|---|
| 1 | 193 | 177 | 13 | 3 | 8.29 |
| 2 | 37 | 34 | 3 | 0 | 8.11 |
| 3 | 19 | 19 | 0 | 0 | 0 |
| 4 | 19 | 13 | 5 | 1 | 31.6 |
| 5 | 15 | 11 | 4 | 0 | 26.7 |
| 6 | 13 | 10 | 3 | 0 | 23.1 |
| 7 | 13 | 8 | 4 | 1 | 38.5 |
| 8 | 6 | 4 | 2 | 0 | 33.3 |
| 9 | 5 | 3 | 2 | 0 | 40 |
| 10 | 4 | 4 | 0 | 0 | 0 |
| 11 | 4 | 4 | 0 | 0 | 0 |
| 12 | 3 | 1 | 0 | 2 | 66.7 |
| 13 | 2 | 2 | 0 | 0 | 0 |
| 14 | 1 | 0 | 1 | 0 | 100 |
| Total | 334 | 290 | 37 | 7 | 13.2 |
Video total views and viewing time data were available for 10 surgeons at study completion. The median number of views per surgeon was 447 (interquartile range (IQR) 50–773), while the median viewing time per surgeon was 58.6 min (IQR 5.09–112.6). Kruskal–Wallis test for equality comparing the median number of views and viewing time stratified by surgeon volume did not demonstrate a significant difference for number of views (p = .12) or viewing time (p = .12).
Discussion
This study has three important findings. This is the first direct evaluation of rates of rescheduling and cancellation of penile prosthetic surgeries. The study findings suggest that the rate of surgery noncompletion for penile prosthetic surgery more than doubles the cancellation rate for elective procedures performed in urology in general; however, the 37.6% noncompletion rate is not directly comparable to studies that focused on day-of-surgery cancellation only, as this study incorporated cancellation anytime after surgery was initially scheduled (Keller et al., 2014; Leslie et al., 2013).
The cancellation rate significantly decreased after the intervention, with the 13.2% noncompletion rate more consistent with the urologic literature for elective surgery cancellations. There was a wide range of video utilization between surgeon practices, with some surgeons reporting markedly higher utilization compared to others. In this sense, this evaluation represents an “intention to treat” analysis; further studies may consider a patient-centered evaluation to determine the impact, reach, and effectiveness of the video-based technology platform, particularly using a qualitative approach.
Second, the most common reason for cancellation after the intervention was patient-related. Forty-six percent of case rescheduling or cancellation occurred because of patient’s desire to cancel or delay surgery, primarily due to logistical factors. This proportion was less marked in the baseline group, likely because the prevalence of incomplete medical clearance and reversed patient decisions for surgery were higher. Future studies will need to evaluate factors for surgery cancellation and rescheduling in more detail, perhaps through qualitative methods. Medical impediments to noncompletion decreased after the intervention, as would be expected with more patient education and opportunities for physician contact prior to surgery. These findings are strengthened by the heterogeneity of the multi-institutional and geographically diverse study cohort, which represents multiple different practice settings.
Finally, although the volume analysis did demonstrate a clinically significant difference, it was not statistically significant. This finding likely results from the small number of surgeons overall, as well as the skewed practice pattern of the top two surgeons, who between them completed nearly 70% of cases within the total intervention cohort. These surgeons likely have the most resources dedicated to filling an operative room schedule. The video utilization by patients of high versus low volume surgeons was not significantly different, suggesting that other factors may underpin the difference in cancellation rates. Future studies should seek to identify outlier practices to develop models that can be broadly adopted. This study did not analyze high performing practices to identify other factors that may be contributing to lower noncompletion rates (the positive deviance method), although future such analyses may be useful (Sternin et al., 2010).
This study has several limitations. First, as discussed previously, there was no patient-level data, which would have allowed for risk adjustment to factor into noncompletion rates, given that markedly different patient populations between individual offices may have falsely skewed the results. Additionally, the time from case cancellation to planned surgery date was missing; given that providers could likely fill their operative room schedules with some anticipation, this information would have added to the analysis. Future evaluations should seek to identify the meaning behind the patient factors for noncompletion (e.g., age, income, race, socioeconomic status, and language), possibly through qualitative methods. Second, although the multi-institutional study design allowed for broad incorporation of many groups within the study, other factors leading to reduced noncompletion rates in the intervention group may have skewed these results. Cluster randomization would have allowed for this, yet the technology-based nature of the intervention was such that physicians and their offices were minimally involved; as a result, that the Hawthorne effect is likely limited. Finally, the skewed volume to the top two surgeons weighted the data to their practices; incorporating a larger number of medium-volume practices to balance out these high-volume implanters would render these results more generalizable.
Despite these limitations, the study findings represent a new understanding of surgery noncompletion in urologic prosthetic practice and point toward novel utilization of technology as a solution for operating room and surgeon inefficiency. Further studies should attempt to elucidate specific factors leading to patient cancellation or rescheduling of their surgery and a qualitative analysis of the intervention materials based upon patient feedback may lead to more efficacious outcomes.
Conclusions
Penile prosthetic surgery is frequently rescheduled or canceled. Implementing a video-based patient education program reduces surgery noncompletion, improving efficiency and quality of care. Wider implementation is needed to validate these findings, while cost-effectiveness analyses may further support their broad adoption.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Coloplast.
ORCID iD: Eric Ballon-Landa  https://orcid.org/0000-0002-7291-2485
https://orcid.org/0000-0002-7291-2485
References
- Argo J. L., Vick C. C., Graham L. A., Itani K. M., Bishop M. J., Hawn M. T. (2009). Elective surgical case cancellation in the veterans health administration system: Identifying areas for improvement. The American Journal of Surgery, 198(5), 600–606. [DOI] [PubMed] [Google Scholar]
- Hovlid E., Bukve O., Haug K., Aslaksen A. B., von Plessen C. (2012). A new pathway for elective surgery to reduce cancellation rates. BMC Health Services Research, 11(12), 154. doi: 10.1186/1472-6963-12-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller A., Ashrafi A., Ali A. (2014). Causes of elective surgery cancellation and theatre throughput efficiency in an Australian urology unit. F1000Research, 19(3), 197. doi: 10.12688/f1000research.4824.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie R. J., Beiko D., van Vlymen J., Siemens D. R. (2013). Day of surgery cancellation rates in urology: Identification of modifiable factors. Canadian Urological Association Journal, 7(5–6), 167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson R. P., Dhakal I. B. (2015). Day of surgery cancellation rate after preoperative telephone nurse screening or comprehensive optimization visit. Periopererative Medicine (London), 10(4), 12. doi: 10.1186/s13741-015-0022-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quandt R. E. (1960). Tests of the hypothesis that a linear regression system obeys two separate regimes. Journal of the American Statistical Association, 55(290), 324–330. [Google Scholar]
- Silvay G., Goldberg A., Gutsche J. T., & T, Augoustides J. G. (2016). Same-day admission for elective cardiac surgery: How to improve outcome with satisfaction and decrease expenses. Journal of Anesthesia, 30(3), 444–448. [DOI] [PubMed] [Google Scholar]
- Singhal R., Warburton T., Charalambous C. P. (2014). Reducing same day cancellations due to patient related factors in elective orthopaedic surgery: Experience of a centre in the UK. Journal of Perioperative Practice, 24(4), 70–74. [DOI] [PubMed] [Google Scholar]
- Sternin J., Sternin M., Pascale R. (2010). The power of positive deviance: How unlikely innovators solve the world’s toughest problems. Boston, MA: Harvard Business Press. [Google Scholar]
- Tan A. L., Chiew C. J., Wang S., Abdullah H. R., Lam S. S., Ong M. E., Tan H. K., Wong T. H. (2019). Risk factors and reasons for cancellation within 24 h of scheduled elective surgery in an academic medical centre: A cohort study. International Journal of Surgery, 4(66), 72–78. doi: 10.1016/j.ijsu.2019.04.009 [DOI] [PubMed] [Google Scholar]