Abstract
There is substantial evidence for normal relationships between spine and postural parameters, as measured from radiographs of standing patients. Sagittal balance, cervical lordosis, thoracic kyphosis, lumbar lordosis, pelvic tilt, and the more complex understanding of the interrelations between these essential components of normal stance have evolved to where there are known, established thresholds for normalcy. These spinal parameters are reliably measured from X-ray images and serve as goals of care in the treatment of spine and postural disorders. Initial and follow-up spinal imaging by X-ray is thus crucial for the practice of contemporary and evidence-based structural rehabilitation. Recent studies have demonstrated that improvement in the spine and posture by nonsurgical methods offers superior long-term patient outcomes versus conventional methods that only temporarily treat pain/dysfunction. Low-dose radiation from repeated X-ray imaging in treating subluxated patients is substantially below the known threshold for harm and is within background radiation exposures. Since alternative imaging methods are not clinically practical at this time, plain radiography remains the standard for spinal imaging. It is safe when used in a repeated fashion for quantifying pre–post spine and postural subluxation and deformity patterns in the practice of structural correction methods by chiropractic and other manual medicine practices.
Keywords: repeat radiography, chiropractic, spine rehabilitation, X-ray, spine imaging
Normal Spine Alignment as a Desirable Treatment Outcome
A normal spine alignment and sagittal balance is critical for optimal biomechanical function.1-12 Although some have questioned an ideal spine configuration,13 these views are antiquated and unscientific.12 A plethora of biomechanical literature substantiates that an optimal spine configuration is critical for normal activities of daily living, optimal sport performance, optimal lifting, and injury prevention and is associated with a higher quality of life.14-20
An ideal biomechanical alignment is also apparent from evolutionary considerations (lumbar lordosis essential for bipedal gait21), anatomical considerations (ie, the backward wedging of the discs create the cervical and lumbar lordosis9; the forward wedging of the vertebra create the thoracic and sacral kyphosis9; the orientation of the facet joints9 and sagittal spine alignment determines spinal coupling patterns22,23; the essentiality of sagittal balance4,24,25), the biomechanical considerations of spine load-bearing capabilities,9,26,27 and injury mechanisms.9,26-30 For these reasons, an ideal spine alignment is the outcome goal for those who treat and correct spine deformity (subluxation), including specifically spine surgeons, as well as specialty-trained chiropractors and physiotherapists (Figures 1 and 2).31-36
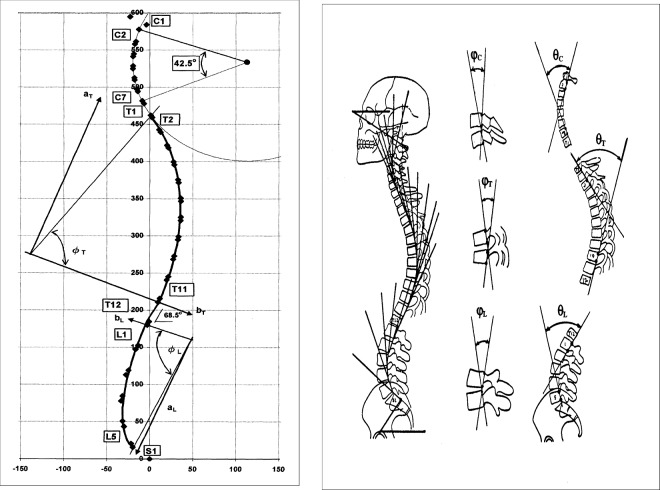
Figure 1.
Left: The Harrison normal spine model as the path of the posterior longitudinal ligament. Right: Harrison posterior tangent method used to quantify subluxation patterns (Courtesy Chiropractic BioPhysics® (CBP®) seminars).35
Figure 2.
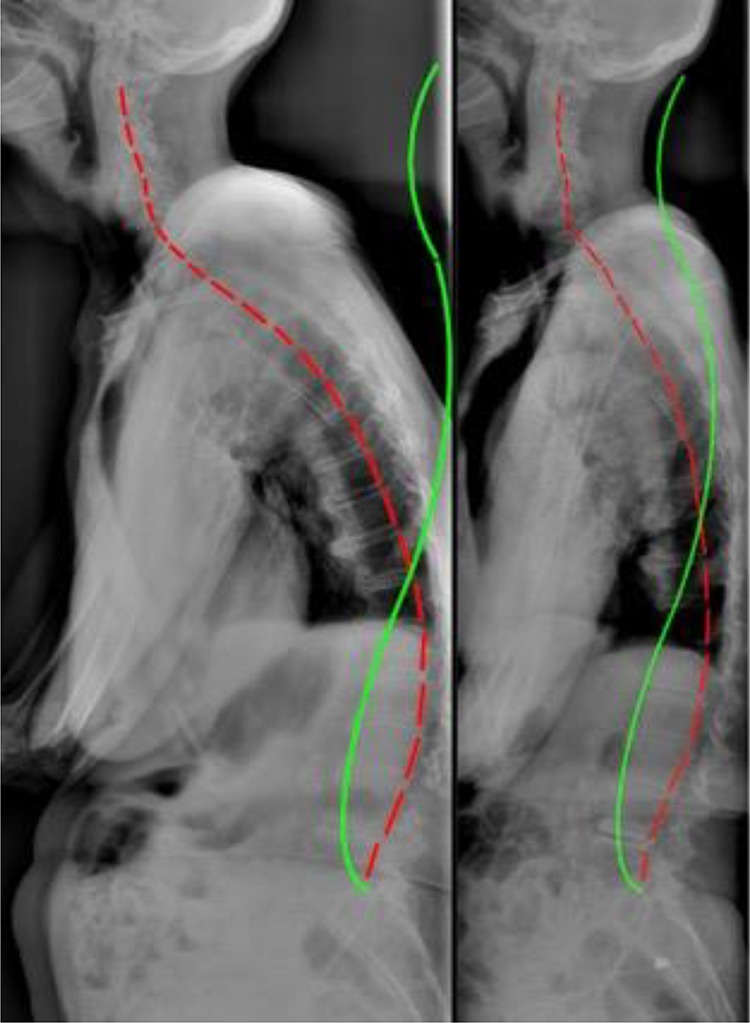
Sagittal full-spine radiographs demonstrating a before and after of a geriatric patient (red line) treated by Chiropractic BioPhysics protocol resulting in dramatic spine and posture improvements toward the ideal spinal configuration that represents the Harrison full-spine normal model (green line) (Image courtesy of Dr J. Haas, Windsor, Colorado).
Posture and Spine Subluxation as the Source of Pathology
While normal spine morphology is essential for normal function, abnormal alignment referred to as spine deformity (surgical literature) or subluxation (chiropractic) results in compensation/adaptation and, over time, dysfunction and named pathology. In the transition from normal alignment to abnormal alignment, critical thresholds of essential spinal parameters get surpassed by either acute traumatic spinal injury events (ie, motor vehicle collision, lifting injury, fall, etc) or chronic repetitive or sustained strain injuries (ie, habitual sitting, habitual bending, habitual slouching, etc). In this process, it is the devolution of the spine from working physiologically to pathologically.
There are 6 main types of spinal subluxation patterns and each type has deleterious effects on the related spinal tissues.37 For example, thoracic hyperkyphosis (posterior translation of thorax over pelvis) is associated with diverse symptoms and early death.38-44 Scoliosis (slow-loading buckling) is also associated with various symptoms including back pains, osteoarthritis, and also early demise.45,46 Lumbar spine spondylolisthesis (ligament instability featuring a single vertebra shifting/sliding beyond normal limits) is a definitive source of back pain and sciatica often warranting surgery.47 Lumbar spine hypolordosis is a definitive source of back pain.48,49 Atlantoaxial rotatory fixation (segmental subluxation) is associated with upper neck and/or neurological symptoms.50,51 Cervical kyphosis (snap-through forward buckling of neck) is associated with craniocervical and neurological symptoms.32-34
It is pointed out that any postural subluxation pattern will change the biomechanical loading onto the spine9,26,27,52,53 such that Wolff’s Law will dictate a remodeling of the architecture of the bone over time.54-56 Thus, the long-term consequences of spinal deformity or subluxation is spinal osteoarthritis and degenerative disc disease.57-65 Further, it is a logical premise that if posture deteriorates over time, then the earliest recognition should warrant consideration for its correction. This would change the otherwise untoward trajectory of postural deterioration coupled with the degenerative spine tissue cascade, which would evolve over several years.
The Correction of Spine and Posture in Chiropractic and Manual Medicine
There have been several chiropractic and manual physiotherapeutic methods that have achieved the status of having positive randomized clinical controlled trials (RCT) evidence showing that definitive spine and posture structural improvements can be made for various subluxation patterns. Randomized clinical controlled trial evidence shows efficacy for nonsurgical methods to reduce scoliosis curves,66-68 reduce thoracic hyperkyphosis,17,69,70 reduce anterior head translation,71-78 increase cervical lordosis,71-78 and increase lumbar lordosis.79-81 Further, these postural improvements have been shown to correlate with improvements in various patient outcomes, including pain, disability, quality of life, range of motion, and specific physiological measures including improved neurological central conduction times, which is a measure of the ability of the brain to communicate with the body.
Several recent RCTs have shown that physiotherapy scoliosis-specific exercise (PSSE) programs lead to larger reductions in spinal curve measures versus generalized (nonspecific) exercise programs in the treatment of adolescent idiopathic scoliosis.66-68 Since scoliosis of the spine may present in several different patterns, radiographic assessment is critical to prescribe curve-specific corrective exercise programs such as the popular “Schroth method” that has proven to reduce spine curvature. Comparison control groups receiving generic physiotherapy exercises, not specific to the patient’s presenting curve pattern, do show patient improvements, albeit significantly less than PSSE groups.
The reduction in thoracic hyperkyphosis has also been documented in several RCTs.17,69,70 Radiographic assessment is critical to determine whether there are thoracic vertebral compression fractures which will limit the correction potential. Although the first 2 RCTs69,70 demonstrate a modest correction (∼3° Cobb angle), a recent trial17 has shown that more intensive corrective procedures (Schroth methods for hyperkyphosis) are superior (∼9° Cobb angle) to antigravity exercises. Either are superior to no correction from conventional physiotherapy methods.
Importantly, there seems to be an emerging trend in the literature. Methods shown to provide structural correction to the spine and posture for various spinal ailments are proving to provide long-term relief versus “cookie-cutter” treatments that help with temporary pain relief only. In several RCTs,71-81 the Moustafa group has demonstrated that only short-term relief is experienced by patients receiving traditional physiotherapy treatments for various craniocervical and lumbosacral disorders, where the trend for regression of symptoms occurs after the cessation of treatment (Figures 3 and 4). Alternatively, in the experimental treatment arms of these trials, patients receiving the same treatment plus spine correcting methods—Chiropractic BioPhysics extension traction to improve the natural lordotic spine alignment for the cervical (Figure 3) or lumbar spinal (Figure 4) areas—show lasting relief of symptoms persisting well beyond the cessation of treatment (3 months to 2 years).71-81 These trials also show similar trends in many of the measured neurophysiologic parameters including pain intensity, disability, quality of life, dizziness, headache index, head repositioning accuracy, central somatosensory conduction time, H-reflex, and flexion–extension kinematics.
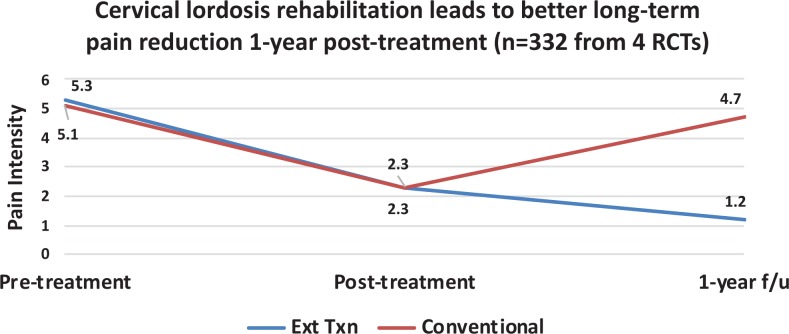
Figure 3.
Spine-specific treatment shows better long-term symptom relief versus non-spine-specific conventional treatments. Data reported for the improvement in cervical lordosis and are weighted average from 4 randomized clinical controlled trials (RCTs).72,74,75,77 Note: Red line = conventional treatments (n = 166); blue line = conventional treatments plus extension traction to improve cervical lordosis (n = 166). Y-axis = pain intensity (0 = no pain; 10 = worst pain ever).
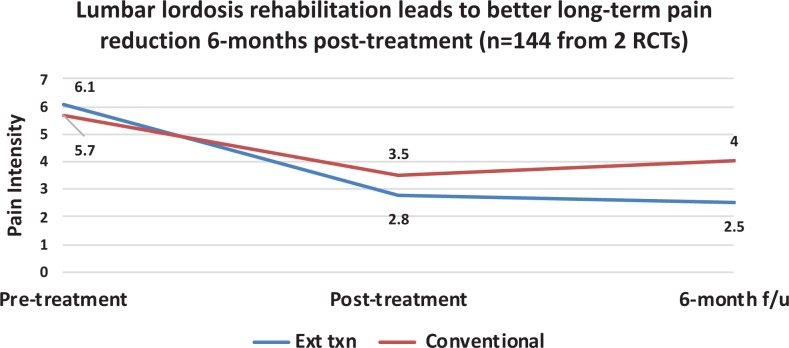
Figure 4.
Spine-specific treatment shows better long-term symptom relief versus non-spine-specific conventional treatments. Data reported for the improvement in lumbar lordosis and are weighted average from 2 randomized clinical controlled trials (RCTs).80,81 Note: Red line = conventional treatments (n = 72); blue line = conventional treatments plus extension traction to improve lumbar lordosis (n = 72). Y-axis = pain intensity (0 = no pain; 10 = worst pain ever).
Due to the recent and expanding evidence base for nonsurgical structural spine and posture correction methods, these protocols are expected to gain traction and become more popular. These contemporary methods should prove to help humanity by reducing the need for risky surgical procedures that are often associated with adverse events including major complications, hospital readmissions, and unplanned reoperations.82
Safety of Low-Dose Radiation From Repeated Radiographs
Despite the traditional notion of the risk of radiogenic cancers associated with medical X-rays, the lack of harm from (low-dose) computed tomography scans and radiography has been thoroughly discussed in several recent articles.83-89 It has been argued that the linear no-threshold (LNT) assumption for assessing radiation risk for low-dose exposures is erroneous as the most recent atomic bomb lifespan study data90 show a better fit to a hormetic dose–response model.91-93
Despite the fact that the main data underpinning the LNT concept have now been shown to better support the hormesis model (nonlinearity), there continues to be an acknowledged discount by those who downplay the concept of hormesis in defense of LNT ideology. Specifically, in discouraging the routine use of X-rays in clinical practice, for example, Kawchuk et al state: “While knowledge in topics such as radiation exposure modeling and radiation hormesis continually evolve, there are no large-scale studies that would justify the application of this principle in clinical practice today. To suggest otherwise at this time is professionally irresponsible.”94 Ironically, the use of radiation hormesis (“radiotherapy”) in the treatment of human ills is not a new concept but has great historical evidence and documentation.
Throughout the early 20th century, many human diseases were treated by X-rays. This includes arthritis,95 bronchial asthma,96 carbuncles,97 cervical adenitis,98 deafness,98 furuncles,97 gas gangrene,99 necrotizing fasciitis,100 otitis media,98 pertussis,101 pneumonia,102 sinus infection,103 and tendonitis/bursitis.104 In a recent summary of radiotherapy treatment by X-rays,105 it was determined that success rates typically ranged from 75% to 90% from exposures that typically ranged from 30 to 100 roentgen (263-877 mSv). It was also noted that often the symptoms would be mitigated after only a single treatment and would occur within 24 hours; the treatment effect would even last for months to years.105 Radiotherapy was a very effective treatment but lost popularity due to the emergence of pharmaceuticals and the fears from radiation following the atomic bombings during WWII. It should be noted that radiotherapy (whether given by X-rays or radon) is quietly making a resurgence in the literature; recent cases have documented successful treatment for those suffering from cancers (prostate, colon, uterine, lung, and liver cell), ulcerative colitis, rheumatoid arthritis, pemphigus, diabetes types I and II, Alzheimer disease, and Parkinson disease.106-110
It should be noted that there were no studies found documenting increased cancers from those treated for various health ailments from radiotherapy treatment. There are studies, however, that demonstrate that doses in the range of what was experienced by radiotherapy patients show less cancer rates. For example, in reanalyzing the Canadian breast fluoroscopy study data,111 Cuttler and Pollycove showed that females treated for tuberculosis to up to 300 mGy had one-third less breast cancer incidence.112 Further, Tubiana et al113 determined the cancer incidence for secondary malignant neoplasms in those who have been treated by high-dose radiation for cancers in childhood. The findings indicated that those who received doses up to 0.5 Gy (500 mGy) had less cancers than expected.113 The question is how can those receiving doses (much higher than X-rays) experience health improvements if LNT modeling tells us that radiation exposures are cumulative and harmful?
The answer is that it has been shown that the collective dose concept that is consistent with the prevailing LNT ideology for risk assessment is not valid for low-dose exposures since the body’s adaptive response mechanisms lead to repair of any damage caused.114 In fact, there are numerous and redundant tissue-inherent protective mechanisms that prevent, repair, or remove damage (Table 1).115-118 Ironically, the most damage induced on a daily basis is metabolically produced reactive oxygen species (ROS) and H2O2 from aerobic respiration, and this damage is many orders of magnitude larger than any induced from low-dose radiation exposures.115-117 Due to this fact, X-rays are rendered negligible.89
Table 1.
Body’s Multiple Adaptive Response Mechanisms That Prevent, Repair, and Remove Damage Caused From Mostly Endogenous Reactive Oxygen Species and H2O2 From Aerobic Metabolism.118
|
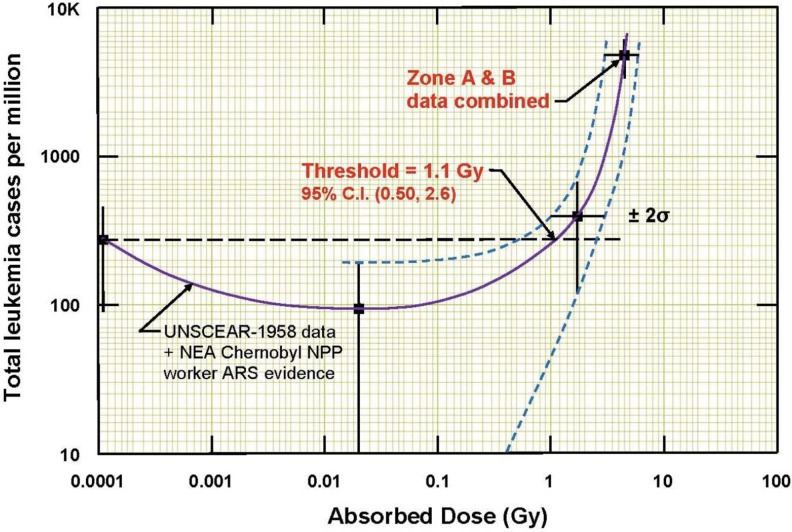
As recently discussed by Oakley et al, the only consideration about repeated radiographs given to spine patients is the radiation dose they receive during each radiograph, not the sum of all the X-ray doses that they received during other radiographic sessions, taken weeks or months apart.119 The radiation exposure a patient would receive could range from 0.25 mGy for a single posterior–anterior image to 3 mGy for a full-spine radiographic examination.88 A 3 mGy dose is several times lower than the 1100 mGy (95% confidence interval, 500-2600 mGy) dose threshold of radiation-induced leukemia,120 the first cancer expected from a high-dose exposure (Figure 5). Therefore, it is very unlikely that X-ray images of the spine taken in a serial fashion over several months or years, as currently performed in the treatment of patients with spinal subluxation, would ever contribute to the induction of future malignancies.
Figure 5.
Leukemia incidence versus absorbed radiation dose for 95 819 Hiroshima atomic bomb survivors, indicating a threshold of about 1100 mGy for radiation-induced leukemia.120
Conclusions
The treatment goal of achieving an improved spine alignment, as has been practiced by spine surgeons for many decades, is also an evidence-based practice by chiropractors, physiotherapists, and other manual medicine providers who specialize in modern methods of spine and posture rehabilitation. This is because the cause of spinal pain, dysfunction, and disability often lies in the failure of the body’s attempt to compensate for a discordance within biomechanical relationships of the specific spinal regions and pelvis. Various advances in nonsurgical methods have evolved showing spine and posture corrections that lead to simultaneous pain, dysfunction, quality of life, and physiological and biomechanical improvements. These methods are also displaying the trend that improving posture and spine alignment lead to better long-term outcomes versus traditional or conventional treatments that do not improve spine alignment. Lastly, the essential reliance on repeat radiographs to monitor treatment effect over time is a safe and evidence-based practice.
Acknowledgments
The authors thank Jerry M. Cuttler for critical review of an earlier version of the manuscript as well as for the image used in Figure 5. The authors also thank Dr Jason Haas for the image used in Figure 2.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: P.A.O. is a paid research consultant for CBP NonProfit, Inc. D.E.H. teaches spine rehabilitation methods and sells products to physicians for patient care that require radiography for biomechanical analysis.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funds from CBP NonProfit, Inc.
ORCID iD: Paul A. Oakley  https://orcid.org/0000-0002-3117-7330
https://orcid.org/0000-0002-3117-7330
References
- 1. Shah AA, Lemans JV, Zavatsky J. Spinal balance/alignment—clinical relevance and biomechanics [published online ahead of print] J Biomech Eng. 2019. doi:10.1115/1.4043650. [DOI] [PubMed] [Google Scholar]
- 2. Ling FP, Chevillotte T, Leglise A, Thompson W, Bouthors C, Le Huec JC. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur Spine J. 2018;27(suppl 1):8–15. [DOI] [PubMed] [Google Scholar]
- 3. Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J. 2011;20(suppl 5):564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Le Huec JC, Saddiki R, Franke J, Rigal J, Aunoble S. Equilibrium of the human body and the gravity line: the basics. Eur Spine J. 2011;20(suppl 5):558–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11(1):80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87(2):260–267. [DOI] [PubMed] [Google Scholar]
- 7. Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery. 2015;76(suppl 1):S42–S56. [DOI] [PubMed] [Google Scholar]
- 8. Patwardhan AG, Khayatzadeh S, Havey RM, et al. Cervical sagittal balance: a biomechanical perspective can help clinical practice. Eur Spine J. 2018;27(suppl 1):25–38. [DOI] [PubMed] [Google Scholar]
- 9. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(suppl 5):609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16(9):1459–1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5-s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005;30(6 suppl):S27–S34. [DOI] [PubMed] [Google Scholar]
- 12. Harrison DE, Harrison DD, Troyanovich SJ, Harmon S. A normal spinal position: it’s time to accept the evidence. J Manipulative Physiol Ther. 2000;23(9):623–644. [DOI] [PubMed] [Google Scholar]
- 13. Haas M, Taylor JA, Gillette RG. The routine use of radiographic spinal displacement analysis: a dissent. J Manipulative Physiol Ther. 1999;22(4):254–259. [DOI] [PubMed] [Google Scholar]
- 14. Protopsaltis TS, Lafage R, Smith JS, et al. The lumbar pelvic angle, the lumbar component of the T1 pelvic angle, correlates With HRQOL, PI-LL mismatch, and it predicts global alignment. Spine. 2018;43(10):681–687. [DOI] [PubMed] [Google Scholar]
- 15. Banno T, Togawa D, Arima H, et al. The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur Spine J. 2016;25(11):3687–3693. [DOI] [PubMed] [Google Scholar]
- 16. Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Watanabe K. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J. 2016;25(11):3675–3686. [DOI] [PubMed] [Google Scholar]
- 17. Bezalel T, Carmeli E, Levi D, Kalichman L. The effect of Schroth therapy on thoracic kyphotic curve and quality of life in Scheuermann’s patients: a randomized controlled trial. Asian Spine J. 2019;13(3):490–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lafage R, Challier V, Liabaud B, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and Mcgregor’s slope with health-related quality of life. Neurosurgery. 2016;79(1):108–115. [DOI] [PubMed] [Google Scholar]
- 19. Araújo F, Lucas R, Alegrete N, Azevedo A, Barros H. Sagittal standing posture, back pain, and quality of life among adults from the general population: a sex-specific association. Spine. 2014;39(13):E782–E794. [DOI] [PubMed] [Google Scholar]
- 20. Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96(19):1631–1640. [DOI] [PubMed] [Google Scholar]
- 21. White AA, III, Panjabi MM. Clinical Biomechanics of the Spine. Philadelphia, PA: Lippincott Williams & Wilkins; 1990. [Google Scholar]
- 22. Panjabi MM, Oda T, Crisco JJ, III, Dvorak J, Grob D. Posture affects motion coupling patterns of the upper cervical spine. J Orthop Res. 1993;11(4):525–536. [DOI] [PubMed] [Google Scholar]
- 23. Panjabi M, Yamamoto I, Oxland T, Crisco J. How does posture affect coupling in the lumbar spine? Spine. 1989;14(9):1002–1011. [DOI] [PubMed] [Google Scholar]
- 24. Kuntz C, IV, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine. 2007;6(2):104–112. [DOI] [PubMed] [Google Scholar]
- 25. Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011;20(suppl 5):626–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine. 1988;13(5):447–449. [DOI] [PubMed] [Google Scholar]
- 27. McGill SM. Low Back Disorders Evidence-Based Prevention and Rehabilitation. Windsor, ON: Human Kinetics; 2002. [Google Scholar]
- 28. Kaneoka K, Ono K, Inami S, Hayashi K. Motion analysis of cervical vertebrae during whiplash loading. Spine. 1999;24(8):763–769. [DOI] [PubMed] [Google Scholar]
- 29. Grauer JN, Panjabi MM, Cholewicki J, Nibu K, Dvorak J. Whiplash produces an S-shaped curvature of the neck with hyperextension at lower levels. Spine. 1997;22(21):2489–2494. [DOI] [PubMed] [Google Scholar]
- 30. Nightingale RW, Sganga J, Cutcliffe H, Bass CR. Impact responses of the cervical spine: a computational study of the effects of muscle activity, torso constraint, and pre-flexion. J Biomech. 2016;49(4):558–564. [DOI] [PubMed] [Google Scholar]
- 31. La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am. 1988;19(2):383–393. [PubMed] [Google Scholar]
- 32. Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19(2):141–159. [DOI] [PubMed] [Google Scholar]
- 33. Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine. 2013;38(22 suppl 1):S149–S160. [DOI] [PubMed] [Google Scholar]
- 34. Bess S, Protopsaltis TS, Lafage V, et al. Clinical and radiographic evaluation of adult spinal deformity. Clin Spine Surg. 2016;29(1):6–16. [DOI] [PubMed] [Google Scholar]
- 35. Oakley PA, Harrison DD, Harrison DE, Haas JW. Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc. 2005;49(4):270–296. [PMC free article] [PubMed] [Google Scholar]
- 36. Bettany-Saltikov J, Parent E, Romano M, Villagrasa M, Negrini S. Physiotherapeutic scoliosis-specific exercises for adolescents with idiopathic scoliosis. Eur J Phys Rehabil Med. 2014;50(1):111–121. [PubMed] [Google Scholar]
- 37. Harrison DE, Harrison DD, Janik TJ, Cailliet R, Haas JW. Do alterations in vertebral and disc dimensions affect an elliptical model of the thoracic kyphosis? Spine. 2003;28(5):463–469. [DOI] [PubMed] [Google Scholar]
- 38. Oakley PA, Harrison DE. Reducing thoracic hyperkyphosis subluxation deformity: a systematic review of Chiropractic Biophysics® methods employed in its structural improvement. J Contemporary Chiropr. 2018;1:59–66. [Google Scholar]
- 39. Kado DM, Browner WS, Palermo L, et al. Study of osteoporotic fractures research group: vertebral fractures and mortality in older women: a prospective study. Arch Intern Med. 1999;159(3):1215–1220. [DOI] [PubMed] [Google Scholar]
- 40. Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14(7):589–594. [DOI] [PubMed] [Google Scholar]
- 41. Kado DM, Huang MH, Karlamangla AS, et al. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52(10):1662–1667. [DOI] [PubMed] [Google Scholar]
- 42. Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12(3):225–233. [DOI] [PubMed] [Google Scholar]
- 43. Anderson F, Cowan NR. Survival of healthy older people. Br J Prev Soc Med. 1976;30(4):231–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cutler WB, Friedmann E, Genovese-Stone E. Prevalence of kyphosis in a healthy sample of pre- and postmenopausal women. Am J Phys Med Rehabil. 1993;72(1):219–225. [DOI] [PubMed] [Google Scholar]
- 45. Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality after diagnostic radiography: findings from the U.S. scoliosis cohort study. Spine. 2000;25(16):2052–2063. [DOI] [PubMed] [Google Scholar]
- 46. Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174(1):83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Raastad J, Reiman M, Coeytaux R, Ledbetter L, Goode AP. The association between lumbar spine radiographic features and low back pain: a systematic review and meta-analysis. Semin Arthritis Rheum. 2015;44(5):571–585. [DOI] [PubMed] [Google Scholar]
- 48. Chun SW, Lim CY, Kim K, Hwang J, Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J. 2017;17(8):1180–1191. [DOI] [PubMed] [Google Scholar]
- 49. Sadler SG, Spink MJ, Ho A, DeJonge XJ, Chuter VH. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: a systematic review of prospective cohort studies. BMC Musculoskeletal Disord. 2017;18(1):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Roche CJ, O’Malley M, Dorgan JC, Carty HM. A pictorial review of atlanto-axial rotatory fixation: key points for the radiologist. Clin Radiol. 2001;56(12):947–958. [DOI] [PubMed] [Google Scholar]
- 51. Biedermann H. Kinematic imbalances due to suboccipital strain in newborns. J Manual Med. 1992;6:151–156. [Google Scholar]
- 52. Keller TS, Colloca CJ, Harrison DE, Harrison DD, Janik TJ. Influence of spine morphology on intervertebral disc loads and stresses in asymptomatic adults: implications for the ideal spine. Spine J. 2005;5(3):297–309. [DOI] [PubMed] [Google Scholar]
- 53. Harrison DE, Colloca CJ, Harrison DD, Janik TJ, Haas JW, Keller TS. Anterior thoracic posture increases thoracolumbar disc loading. Eur Spine J. 2005;14(3):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chen JH, Liu C, You L, Simmons CA. Boning up on Wolff’s Law: mechanical regulation of the cells that make and maintain bone. J Biomech. 2010;43(1):108–118. [DOI] [PubMed] [Google Scholar]
- 55. Frost HM. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004;74(2):3–15. [DOI] [PubMed] [Google Scholar]
- 56. Frost HM. Wolff’s Law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175–188. [DOI] [PubMed] [Google Scholar]
- 57. Murray KJ, Le Grande MR, Ortega de Mues A, Azari MF. Characterisation of the correlation between standing lordosis and degenerative joint disease in the lower lumbar spine in women and men: a radiographic study. BMC Musculoskelet Disord. 2017;18(1):330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Harrison DE, Harrison DD, Janik TJ, Jones EW, Cailliet R, Normand M. Comparison of axial and flexural stresses in lordosis and three buckled modes in the cervical spine. Clin Biomech. 2001;16(4):276–284. [DOI] [PubMed] [Google Scholar]
- 59. Harrison DD, Jones EW, Janik TJ, Harrison DE. Evaluation of flexural stresses in the vertebral body cortex and trabecular bone in three cervical configurations with an elliptical shell model. J Manipulative Physiol Ther. 2002;25(6):391–401. [DOI] [PubMed] [Google Scholar]
- 60. Lv X, Liu Y, Zhou S, et al. Correlations between the feature of sagittal spinopelvic alignment and facet joint degeneration: a retrospective study. BMC Musculoskelet Disord. 2016;17(1):341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10(4):320–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S. Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res. 2011;469(3):674–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014;14(7):1228–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hohl M. Soft-tissue injuries of the neck in automobile accidents. Factors influencing prognosis. J Bone Joint Surg Am. 1974;56(8):1675–1682. [PubMed] [Google Scholar]
- 65. Norris SH, Watt I. The prognosis of neck injuries resulting from rear-end vehicle collisions. J Bone Joint Surg Br. 1983;65(5):608–611. [DOI] [PubMed] [Google Scholar]
- 66. Noh DK, You JS, Koh JH, et al. Effects of novel corrective spinal technique on adolescent idiopathic scoliosis as assessed by radiographic imaging. J Back Musculoskelet Rehabil. 2014;27(3):331–338. [DOI] [PubMed] [Google Scholar]
- 67. Monticone M, Ambrosini E, Cazzaniga D, et al. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J. 2014;23(2):1204–1214. [DOI] [PubMed] [Google Scholar]
- 68. Schreiber S, Parent EC, Khodayari Moez E, et al. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis—an assessor and statistician blinded randomized controlled trial. PLoS One. 2016;29;11(12):e0168746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69(11):1054–1059. [DOI] [PubMed] [Google Scholar]
- 70. Katzman WB, Vittinghoff E, Lin F, et al. Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos Int. 2017;28(10):2831–2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Moustafa IM, Diab AM, Ahmed A, Harrison DE. The efficacy of cervical lordosis rehabilitation for nerve root function, pain, and segmental motion in cervical spondylotic radiculopathy. Phys Ther. 2011;97(suppl):846–847. [Google Scholar]
- 72. Moustafa IM. Does improvement towards a normal cervical configuration aid in the management of fibromyalgia. A randomized controlled trial. Bull Fac Phys Ther Cairo Univ. 2013;18(2):29–41. [Google Scholar]
- 73. Moustafa IM, Diab AA, Harrison DE. Does improvement towards a normal cervical sagittal configuration aid in the management of lumbosacral radiculopathy: a randomized controlled trial. Proceedings of the 13th World Federation of Chiropractic Biennial Congress/ECU Convention, Athens, Greece, May 13-16, 2015. Paper #184 Mediterranean Region Award Winning Paper. [Google Scholar]
- 74. Moustafa IM, Diab AA, Taha S, Harrison DE. Addition of a sagittal cervical posture corrective orthotic device to a multimodal rehabilitation program improves short- and long-term outcomes in patients with discogenic cervical radiculopathy. Arch Phys Med Rehabil. 2016;97(12):2034–2044. [DOI] [PubMed] [Google Scholar]
- 75. Moustafa IM, Diab AA, Harrison DE. The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. Eur J Phys Rehabil Med. 2017;53(1):57–71. [DOI] [PubMed] [Google Scholar]
- 76. Moustafa IM, Diab AAM, Hegazy FA, Harrison DE. Does rehabilitation of cervical lordosis influence sagittal cervical spine flexion extension kinematics in cervical spondylotic radiculopathy subjects? J Back Musculoskelet Rehabil. 2017;30(2):937–941. [DOI] [PubMed] [Google Scholar]
- 77. Moustafa IM, Diab AA, Hegazy F, Harrison DE. Does improvement towards a normal cervical sagittal configuration aid in the management of cervical myofascial pain syndrome: a 1-year randomized controlled trial. BMC Musculoskelet Disord. 2018;19(1):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Moustafa IM, Diab AA, Harrison DE. The effect of normalizing the sagittal cervical configuration for the management of cervicogenic headaches: a 2-year pilot randomized controlled trial. Proceedings of the 15th World Federation of Chiropractic Biennial Congress/78th European Chiropractor’s Union Convention, Berlin, Germany, March 20-23, 2019:142. [Google Scholar]
- 79. Diab AA, Moustafa IM. Rehabilitation for pain and lumbar segmental motion in chronic mechanical low back pain: a randomized trial. J Manipulative Physiol Ther. 2012;35(4):246–253. [DOI] [PubMed] [Google Scholar]
- 80. Moustafa IM, Diab AA. Extension traction treatment for patients with discogenic lumbosacral radiculopathy: a randomized controlled trial. Clin Rehabil. 2012;27(1):51–62. [DOI] [PubMed] [Google Scholar]
- 81. Diab AA, Moustafa IM. The efficacy of lumbar extension traction for sagittal alignment in mechanical low back pain. A randomized trial. J Back Musculoskelet Rehabil. 2013;26(2):213–222. [DOI] [PubMed] [Google Scholar]
- 82. Pellisé F, Serra-Burriel M, Smith JS, et al. Development and validation of risk stratification models for adult spinal deformity surgery [published online ahead of print June 28, 2018]. J Neurosurg Spine. 2019:1–13. doi:10.3171/2019.3.SPINE181452. [DOI] [PubMed] [Google Scholar]
- 83. Siegel JA, Sacks B. Eliminating use of the linear no-threshold assumption in medical imaging. J Nucl Med. 2017;58(6):1014–1015. [DOI] [PubMed] [Google Scholar]
- 84. Siegel JA, Pennington CW, Sacks B. Subjecting radiologic imaging to the linear no-threshold hypothesis: a non sequitur of non-trivial proportion. J Nucl Med. 2017;58(1):1–6. [DOI] [PubMed] [Google Scholar]
- 85. Sacks B, Meyerson G, Siegel JA. Epidemiology without biology: false paradigms, unfounded assumptions, and specious statistics in radiation science. Biol Theory. 2016;11(3):69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Siegel JA, McCollough CH, Orton CG. Advocating for use of the ALARA principle in the context of medical imaging fails to recognize that the risk is hypothetical and so serves to reinforce patients’ fears of radiation. Med Phys. 2017;44(1):3–6. [DOI] [PubMed] [Google Scholar]
- 87. Siegel JA, Sacks B, Pennington CW, et al. Dose optimization to minimize radiation risk for children undergoing CT and nuclear medicine imaging is misguided and detrimental. J Nucl Med. 2017;58(6):865–868. [DOI] [PubMed] [Google Scholar]
- 88. Oakley PA, Cuttler JM, Harrison DE. X-ray imaging is essential for contemporary chiropractic and manual therapy spinal rehabilitation: radiography increases benefits and reduces risks. Dose Response. 2018;16(2):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Oakley PA, Harrison DE. Radiophobia: 7 reasons why radiography used in spine and posture rehabilitation should not be feared or avoided. Dose Response. 2018;16(2):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Ozasa K, Shimizu Y, Suyama A, et al. Studies of the mortality of atomic bomb survivors, report 14, 1950-2003: an overview of cancer and noncancer diseases. Radiat Res. 2012;177(3):229–243. [DOI] [PubMed] [Google Scholar]
- 91. Andronikou S. Letting go of what we believe about radiation and the risk of cancer in children. Pediatr Radiol. 2017;47(1):113–115. [DOI] [PubMed] [Google Scholar]
- 92. Doss M. Should the ALARA Concept and the Image Gently campaign be terminated? Paper Presented at: the International Pediatric Radiology, Chicago, IL: May 17, 2016. https://www.slideshare.net/MohanDoss6/should-the-alara-concept-and-the-image-gently-campaign-be-terminated. Accessed June 21, 2019. [Google Scholar]
- 93. Doss M. Future of radiation protection regulations. Health Phys. 2016;110(3):274–275. [DOI] [PubMed] [Google Scholar]
- 94. Kawchuk G, Goertz C, Axén I, et al. X-ray imaging is essential for contemporary chiropractic and manual therapy spinal rehabilitation: radiography increases benefits and reduces risks. Dose Response. 2018;16(2):1559325818811521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kuhns JG, Morrison SL. Twelve years’ experience in roentgenotherapy for chronic arthritis. N Engl J Med. 1946;235:399–405. [DOI] [PubMed] [Google Scholar]
- 96. Calabrese EJ, Dhawan G, Kapoor R. The use of X rays in the treatment of bronchial asthma: a historical assessment. Radiat Res. 2015;184(2):180–192. [DOI] [PubMed] [Google Scholar]
- 97. Calabrese EJ. X-ray treatment of carbuncles and furuncles (boils): a historical assessment. Hum Exp Toxicol. 2013;32(8):817–827. [DOI] [PubMed] [Google Scholar]
- 98. Calabrese EJ, Dhawan G. Historical use of x-rays: treatment of inner ear infections and prevention of deafness. Hum Exp Toxicol. 2014;33(5):542–553. [DOI] [PubMed] [Google Scholar]
- 99. Calabrese EJ, Dhawan G. The role of x-rays in the treatment of gas gangrene: a historical assessment. Dose Response. 2012;10(4):626–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Dhawan G, Kapoor R, Dhamija A, Singh R, Monga B, Calabrese EJ. Necrotizing fasciitis: low-dose radiotherapy as a potential adjunct treatment. Dose Response. 2019;17(3):1559325819871757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Calabrese EJ, Dhawan G, Kapoor R. Radiotherapy for pertussis: an historical assessment. Dose Response. 2017;15(2):1559325817704760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Calabrese EJ, Dhawan G. How radiotherapy was historically used to treat pneumonia: could it be useful today? Yale J Biol Med. 2013;86(4):555–570. [PMC free article] [PubMed] [Google Scholar]
- 103. Calabrese EJ, Dhawan G. The historical use of radiotherapy in the treatment of sinus infections. Dose Response. 2013;11:469–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Calabrese EJ, Dhawan G, Kapoor R. Use of X-rays to treat shoulder tendonitis/bursitis: a historical assessment. Arch Toxicol. 2014;88(8):1503–1517. [DOI] [PubMed] [Google Scholar]
- 105. Calabrese EJ, Dhawan G, Kapoor R, Kozumbo WJ. Radiotherapy treatment of human inflammatory diseases and conditions: optimal dose. Hum Exp Toxicol. 2019;38(8):888–898. [DOI] [PubMed] [Google Scholar]
- 106. Kojima S, Tsukimoto M, Shimura N, Koga H, Murata A, Takara T. Treatment of cancer and inflammation with low-dose ionizing radiation: three case reports. Dose Response. 2017;15(1):1559325817697531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Kojima S, Thukimoto M, Cuttler JM, et al. Recovery from rheumatoid arthritis following 15 months of therapy with low doses of ionizing radiation: a case report. Dose Response. 2018;16(3):1559325818784719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Kojima S, Cuttler JM, Shimura N, Koga H, Murata A, Kawashima A. Radon therapy for autoimmune diseases pemphigus and diabetes: 2 case reports. Dose Response. 2019;17(2):1559325819850984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Kojima S, Cuttler JM, Inoguchi K, et al. Radon therapy is very promising as a primary or an adjuvant treatment for different types of cancers: 4 case reports. Dose Response. 2019;17(2):1559325819853163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Cuttler JM, Moore ER, Hosfeld VD, Nadolski DL. Second update on a patient with Alzheimer disease treated by CT scans. Dose Response. 2018;16(1):1559325818756461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Miller AB, Howe GR, Sherman GJ, et al. Mortality from breast cancer after irradiation during fluoroscopic examinations in patients being treated for tuberculosis. N Engl J Med. 1989;321(19):1285–1289. [DOI] [PubMed] [Google Scholar]
- 112. Cuttler JM, Pollycove M. Can cancer be treated with low doses of radiation? J Physicians Surg. 2003;8(4):108–111. [Google Scholar]
- 113. Tubiana M, Diallo I, Chavaudra J, et al. A new method of assessing the dose-carcinogenic effect relationship in patients exposed to ionizing radiation. A concise presentation of preliminary data. Health Phys. 2011;100(3):296–299. [DOI] [PubMed] [Google Scholar]
- 114. Mitchel REJ. Cancer and low dose responses in vivo: implications for radiation protection. Dose Response. 2007;5(4):284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Pollycove M, Feinendegen LE. Radiation-induced versus endogenous DNA damage: possible effect of inducible protective responses in mitigating endogenous damage. Human Exp Toxicol. 2003;22(6):290–306. [DOI] [PubMed] [Google Scholar]
- 116. Feinendegen LE, Pollycove M, Neumann RD. Hormesis by low dose radiation effects: low-dose cancer risk modeling must recognize up-regulation of protection In: Baum RP, ed. Therapeutic Nuclear Medicine. Berlin, Heidelberg: Springer; 2012:789–805. [Google Scholar]
- 117. Feinendegen LE, Cuttler JM. Biological effects from low doses and low dose rates of ionizing radiation: science in the service of protecting humans, a Synopsis. Health Phys. 2018;114(6):623–626. [DOI] [PubMed] [Google Scholar]
- 118. Hoffmann GR. A perspective on the scientific, philosophical, and policy dimensions of hormesis. Dose Response. 2009;7:1–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Oakley PA, Navid Ehsani N, Harrison DE. The scoliosis quandary: are radiation exposures from repeated x-rays harmful? Dose Response. 2019;17:1559325819852810.31217755 [Google Scholar]
- 120. Cuttler JM. Evidence of dose threshold for radiation-induced leukemia: absorbed dose and uncertainty. Dose Response. 2019;17:1559325818820973. [DOI] [PMC free article] [PubMed] [Google Scholar]