Abstract
Objective:
To determine the prevalence of childhood emotional and behavioral problems and examine their associations with cesarean delivery.
Methods:
Our sample consisted of 8,900 preschoolers from 35 kindergartens in four cities in East China. Parents completed the Strengths and Difficulties Questionnaire (SDQ) and provided other information. Children’s emotional and behavioral problems were assessed using five subscales of the SDQ. Mode of delivery was classified as vaginal or cesarean section (CS); in sub-analyses, we divided CS into elective or emergency delivery. Logistic regression was used to examine associations.
Results:
A total of 1,209 (13.6%) children had a total SDQ score within abnormal range; 25.5% had peer problems within abnormal range, 9.0% had abnormal emotional symptoms, 13.9% had abnormal conduct problems, 18.9% had abnormal hyperactivity problems, and 16.2% were rated abnormal in pro-social behavior. Overall, 67.3% of the children who participated were delivered by CS. In fully adjusted analysis, CS was significantly associated with abnormal total SDQ score (OR = 1.27; 95%CI 1.10-1.46; p < 0.05) and pro-social behavior (OR = 1.27; 95%CI 1.12-1.45; p < 0.0001). No significant association was found between CS and risk of having conduct problems (OR 1.13; 95%CI 0.98-1.29), peer problems (OR 1.11; 95%CI 0.99-1.24), hyperactivity (OR 1.02; 95%CI 0.91-1.15), or emotional problems (OR 1.06; 95%CI 0.90-1.24).
Conclusion:
In this sample, CS was associated with risk of behavioral problems, but not with emotional problems. Further research is needed to better understand these associations.
Keywords: Problem behavior, cesarean section, delivery mode, pregnancy, preschool children
Introduction
Emotional and behavioral problems in children are widely prevalent in many countries,1,2 ranging from 4.8 to 25.4% in European, Asian, and American preschool samples.2-4 In China, for example 9.49% children were diagnosed with various psychiatric disorders,5 while in Australia, 5.3% of schoolboys had scores within the abnormal clinical range on the five subscales of the Strengths and Difficulties Questionnaire (SDQ).6 In Germany, Fuchs et al.7 observed abnormal total SDQ scores in 16.0% of preschool children.
A previous study highlighted the impact of gender in the development of childhood behavior at preschool age, with boys presenting a higher rate of abnormal SDQ scores than girls.7 In a sample of Korean children, Park et al. found that boys were more likely to have attention deficit/hyperactivity disorder (ADHD), while girls were more likely to have depressive symptoms.4 Behavioral problems, conduct disorder, emotional problems, and hyperactivity can have a negative impact on child development and on the family’s everyday life.
Globally, cesarean section (CS) rates increased from 12% in 2000 to 15.5% in 2012.8 In China, the nationwide CS rate increased from 3.4% in 1988 to 39% in 2012, being highest in urban areas.9 Recent studies revealed a CS rate ranging from 50 to 60% in most parts of China.10-12 Such high rates demand an understanding of the long-term consequences of cesarean delivery, specifically on development of childhood behavior. Cesarean delivery includes both emergency and elective CS. Elective CS is normally scheduled for a gestational age of 37-39 weeks, most commonly as a result of the presence of a medical condition or complication or at the clinician’s or mother’s discretion. Severe fear of childbirth has been found to increase the risk of elective CS.13 Emergency CS, in turn, is performed when serious complications arise during pregnancy or labor in the mother and/or fetus, such as preeclampsia or fetal distress.14 At present, the national or worldwide prevalence of elective vs. emergency CS is difficult to estimate. However, overall rates of CS delivery are known to be high, as a result of clinical, societal and economic realities.15
Studies on cesarean delivery in relation to development of childhood behavior have yielded inconsistent results. Some studies have linked birth by CS to an increases risk of ADHD16 and autism spectrum disorders (ASD).17 In contrast, Curran et al.18 recently reported no significant association between planned CS and ASD or ADHD. Similarly, Al Khalaf et al.19 reported no significant association between any CS and abnormal total SDQ in 3-year-old children. In China, a previous study found that CS by maternal request was associated with a lower risk of childhood psychopathological problems.20 However, few studies have used SDQ to measure the different aspects of childhood behavior problems in relation to mode of delivery.
Gao et al.21 suggested that the rapid economic development, massive rural-to-urban migration, highly competitive education system, and increased number of children attending preschools in China may have negative effects on the psychological wellbeing of Chinese children. On the other hand, the increased divorce rate,22 shorter breastfeeding,23 former one-child policy, and greater environmental difficulties faced by children who live in cities may also increase the risk of developing behavioral and emotional problems among Chinese children. Studies investigating the prevalence of behavioral and emotional problems and their association with CS among Chinese preschoolers are apparently lacking. Therefore, the aim of this study was to determine the prevalence of childhood emotional and behavior problems, as measured with the SDQ, and examine their association with cesarean delivery in preschoolers aged 3 to 6 years.
Methods
Study population
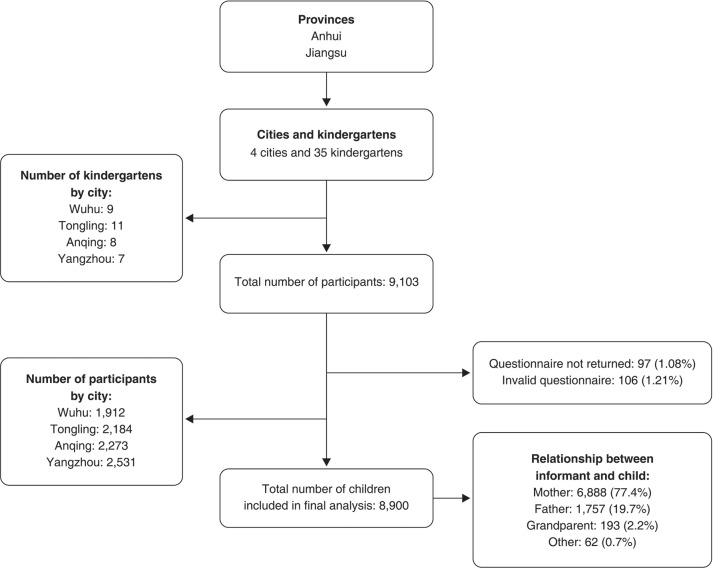
Data collection took place from March to June 2015. A cluster sampling technique was used to select 35 kindergarten schools from three prefecture-level cities in Anhui province (Wuhu, Tongling, Anqing) and one prefecture-level city (Yangzhou) in Jiangsu province. Anhui is a landlocked province of the People’s Republic of China located in the eastern region of the country; it is bordered by Jiangsu province to the northeast. Also located in the east of China, Jiangsu province is bordered by the Yellow Sea to the east, Shanghai to the southeast, and Anhui to the west. In socioeconomic terms, Jiangsu is more developed than Anhui province. However, there are no marked socioeconomic differences across the four small prefecture-level cities in which the study was conducted. Of the 9,103 children enrolled in the study and given the questionnaire to be completed by their parents or other family members, 9,006 returned the questionnaire during the study period; 106 subjects were excluded due to incomplete information. The final sample consisted of 8,900 children aged 3-6 years. Among the informants who completed the survey, 8,645 (97.1%) were parents (Figure 1). This study was approved by the ethics committee of Anhui Medical University and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from the parents of all children who participated in the study.
Figure 1. Flow diagram of study population.
Outcome variables
The SDQ was completed by children’s parents or other guardians. To assess children’s emotional and behavior problems, we used five subscales of the SDQ: emotional symptoms, conduct problems, hyperactivity/inattention, peer problems and pro-social behavior. The SDQ is a validated and reliable instrument to measure emotional and behavior problems among children in the community and clinical settings.24-26 Its total and subscale abnormal scores are considered to be in a clinical range and can be used to identify children with psychiatric disorders.27 We used the parent version of the SDQ for 3-to-17-year-olds, due to its brevity (only 25 items), the fact that the questionnaire also addresses children’s strengths and difficulties, and its generally good acceptance by parents.
The total difficulties score (i.e., the sum of all subscales except pro-social behavior) and scores for each SDQ subscale were dichotomized into healthy (normal category) or at-risk (borderline and abnormal) groups using the following cutoffs: SDQ total difficulties, raw score 0-14 as normal range, raw score 15-16 as borderline range, and raw score 17-40 as abnormal range; emotional symptoms, raw score 0-3 as normal range, raw score 4 as borderline, and raw score 5-10 as abnormal range; conduct problems, raw score 0-2 as normal, raw score 3 as borderline, and raw score 3-10 as abnormal range; hyperactivity, raw score 0-6 as normal, raw score 7 as borderline, and raw score 8-10 as abnormal range; peer problems, raw score 0-4 as normal, raw score 5 as borderline, and raw score 6-10 as abnormal range; and pro-social behavior, raw score 10-6 as normal, raw score 5 as borderline, and raw score 4-0 as abnormal. These cutoff points were previously used in one of our recent studies,28 and their validity and reliability have been confirmed.29
Definition of delivery mode
Delivery modes were determined by asking parents the following question: “Through which mode of delivery did the mother give birth to this child?” The mode of delivery was classified as vaginal or CS. If the answer was CS, the respondent was asked to specify whether it was an elective or emergency procedure.
Potential confounders
Information on maternal factors was collected through a self-report questionnaire taken home by children. Parents were asked to complete questionnaires and return them within 2 weeks. The parameters of interest included maternal age in years, highest achieved maternal education level (primary school, middle school, secondary school, college, or higher), maternal smoking (never, one cigarette per day or less, 1-5 cigarettes per day, 6 cigarettes or more per day), maternal drinking (never, 1-2 drinks per day, ≥ 3 drinks per day), pre-pregnancy weight in kg, maternal weight before delivery in kg, breastfeeding status (never, less than 4 months, 4-5 months, 6 months or more). Child-related factors, including birth weight in g, age, gestational age (preterm/full-term), and gender (male/female), as well as paternal factors including age, education level, smoking, drinking, height, and weight, were also collected.
Maternal pre-pregnancy body mass index (BMI) was calculated based on self-reported maternal height and pre-pregnancy weight. We calculated gestational weight gain as the difference between self-reported weight at the last antenatal care appointment and self-reported pre-pregnancy weight (mothers were reminded to check the weight on their antenatal and postnatal care card). Paternal BMI was calculated from self-reported height and weight. Parental BMI was calculated as weight (kg)/(height [m2]) then categorized as normal for BMI less than 25.0, overweight for BMI between 25.0-29.9, and obese for BMI 30.0 or above.
Statistical analysis
Child and parental characteristics were described in relation to delivery mode; categorical variables were presented as absolute and relative frequencies, while continuous variables were expressed as mean ± standard deviation (SD). Independent-sample t-tests were used to compare SDQ scores by gender. For the main analysis, we first dichotomized delivery mode as CS or vaginal; in additional analyses, we classified delivery mode into three categories: elective CS, emergency CS, or vaginal delivery, and then examined the relationship between elective or emergency CS and abnormal SDQ scores. In all analyses, normal SDQ scores were used as reference.
To assess the association between mode of delivery and childhood emotional and behavioral outcomes, we used logistic regression models to estimate unadjusted and adjusted odds ratios (OR) with 95% confidence intervals (95%CIs), with vaginal delivery as the reference category. In adjusted logistic regression models, we included maternal factors (age, education, smoking, drinking, BMI, gestational weight gain) as Model 1; child factors (gender, age, birth weight, gestational age, only child, duration of breastfeeding) plus the variables used in Model 1 as Model 2; and paternal factors (age, education, smoking, drinking, BMI) plus the variables used in the first two models as Model 3. P-values < 0.05 were considered statistically significant. All analyses were performed using SPSS version 10.
Results
Child and parental characteristics stratified by delivery mode are presented in Table 1. Of 8,900 preschoolers who participated in the study, 58.4% had been delivered by elective CS and 8.9% by emergency CS. Most mothers who gave birth by elective CS (57.5%) were aged 30-35 years, and had a higher education level compared to those who gave birth vaginally or by emergency CS. Mean pre-pregnancy BMI was 21.58 among the mothers who gave birth by elective CS. The mean birth weight of the children born via emergency CS was 3.38 kg, and 95.2% of children born via elective CS were full-term. Among 5,202 children born via elective CS, only 951 (18.3%) had siblings. The fathers of children born via elective CS were more likely to be smokers (with 29.6% smoking more than 6 cigarettes per day), and 34.8% of fathers from this group were overweight.
Table 1. Parental and child characteristics stratified by mode of delivery.
| Characteristics | Vaginal delivery | Elective CS | Emergency CS |
|---|---|---|---|
| Total sample | 2,907 (32.7) | 5,202 (58.4) | 791 (8.9) |
| Maternal characteristics | |||
| Age | |||
| 19-24 | 51 (1.8) | 33 (0.6) | 5 (0.6) |
| 25-29 | 859 (29.5) | 1,249 (24.0) | 252 (31.9) |
| 30-35 | 1,604 (55.2) | 2,990 (57.5) | 443 (56.0) |
| 36 or older | 393 (13.5) | 930 (17.9) | 91 (11.5) |
| Age, mean (SD) | 31.49 (3.8) | 32.23 (3.89) | 31.63 (3.63) |
| Education | |||
| Primary school | 70 (2.4) | 77 (1.5) | 10 (1.3) |
| Middle school | 483 (16.6) | 649 (12.5) | 128 (16.2) |
| Secondary school | 652 (22.4) | 1,293 (24.9) | 195 (24.7) |
| College or higher | 1,702 (58.5) | 3,183 (61.2) | 458 (57.9) |
| Smoking | |||
| Never | 2,896 (99.6) | 5,163 (99.3) | 785 (99.2) |
| 1 cigarette/day or less | 6 (0.2) | 9 (0.2) | 1 (0.1) |
| 1-5 cigarettes/day | 3 (0.1) | 21 (0.4) | 2 (0.3) |
| 6 or more cigarettes/day | 2 (0.1) | 9 (0.2) | 3 (0.4) |
| Drinking | |||
| Never | 2,863 (98.5) | 5,094 (97.9) | 778 (98.4) |
| Occasionally | 40 (1.4) | 100 (1.9) | 12 (1.5) |
| Daily | 4 (0.1) | 8 (0.2) | 1 (0.1) |
| Pre-pregnancy BMI (kg/m2), mean (SD) | 21.09 (2.45) | 21.58 (2.57) | 21.48 (2.53) |
| Gestational weight gain (kg), mean (SD) | 14.10 (7.52) | 15.82 (8.09) | 15.52 (7.92) |
| Child characteristics | |||
| Gender | |||
| Male | 1,529 (52.6) | 2,761 (53.1) | 420 (53.1) |
| Female | 1,378 (47.4) | 2,441 (46.9) | 371 (46.9) |
| Age (years), mean (SD) | 4.34 (1.00) | 4.37 (0.99) | 4.36 (1.01) |
| Birth weight | |||
| Normal | 2,811 (96.7) | 5,046 (97.0) | 768 (97.1) |
| Low birth weight | 96 (3.3) | 156 (3.0) | 23 (2.9) |
| Birth weight (kg), mean (SD) | 3.28 (0.43) | 3.34 (0.46) | 3.38 (0.45) |
| Gestational age | |||
| Preterm | 169 (5.8) | 252 (4.8) | 60 (7.6) |
| Full-term | 2,738 (94.2) | 4,950 (95.2) | 731 (92.4) |
| Sibling | |||
| Yes | 694 (23.9) | 951 (18.3) | 148 (18.7) |
| No | 2,213 (76.1) | 4,251 (81.7) | 643 (81.3) |
| Duration of breastfeeding | |||
| Never | 587 (20.2) | 1,335 (25.7) | 174 (22.0) |
| Less than 4 months | 600 (20.6) | 1,053 (20.2) | 156 (19.7) |
| 4-5 months | 786 (27) | 1,300 (25.0) | 193 (24.4) |
| 6 months or longer | 934 (32.1) | 1,514 (29.1) | 268 (33.9) |
| Paternal characteristics | |||
| Age | |||
| 19-24 | 12 (0.4) | 9 (0.2) | 3 (0.4) |
| 25-29 | 409 (14.1) | 519 (10.0) | 104 (13.1) |
| 30-35 | 1,574 (54.1) | 2,852 (54.3) | 449 (56.8) |
| 36 or older | 912 (31.4) | 1,822 (35.0) | 235 (29.7) |
| Age, mean (SD) | 34.05 (4.65) | 34.67 (4.67) | 33.94 (4.56) |
| Education | |||
| Primary school | 32 (1.1) | 30 (0.6) | 10 (1.3) |
| Middle school | 1,029 (35.4) | 1,674 (32.2) | 283 (35.8) |
| Secondary school | 720 (24.8) | 1,435 (27.6) | 213 (26.9) |
| College or higher | 1,126 (38.7) | 2,063 (39.7) | 285 (36.0) |
| Smoking | |||
| Never | 1,408 (48.4) | 2,312 (44.4) | 350 (44.2) |
| One cigarette/day or less | 159 (5.5) | 285 (5.5) | 46 (5.8) |
| 1-5 cigarettes/day | 528 (18.2) | 1,063 (20.4) | 170 (21.5) |
| 6 or more cigarettes/day | 812 (27.9) | 1,542 (29.6) | 225 (28.4) |
| Drinking | |||
| Never | 1,692 (58.2) | 2,883 (55.4) | 465 (58.8) |
| Occasionally | 948 (32.6) | 1,804 (34.7) | 253 (32.0) |
| Daily | 267 (9.2) | 515 (9.9) | 73 (9.2) |
| BMI | |||
| Normal | 1,871 (65.1) | 3,132 (60.7) | 502 (64.2) |
| Overweight | 898 (31.2) | 1,795 (34.8) | 253 (32.4) |
| Obese | 107 (3.7) | 229 (4.4) | 27 (3.5) |
Data presented as n (%), unless otherwise specified.
BMI = body mass index; CS = cesarean section; SD = standard deviation.
Prevalence of emotional and behavior problems
Mean scores (for total difficulties and each SDQ subscale), by age and gender, are shown in Table 2. In both boys and girls, the mean SDQ total difficulty scores decreased with age. The only significant gender difference for SDQ total difficulty score was observed among 6-year-olds. Overall, girls presented significantly more emotional symptoms, while boys had significantly more hyperactivity problems.
Table 2. Mean SDQ subscale scores of 8,900 preschoolers from four cities in China, stratified by age and gender.
| Age (years)/gender | n | Total difficulties | Emotional symptoms | Conduct problems | Hyperactivity/inattention | Peer problems | Pro-social behavior |
|---|---|---|---|---|---|---|---|
| 3 | |||||||
| Male | 1,081 | 11.73 (4.57) | 1.96 (1.63) | 2.24 (1.42) | 4.68 (2.19) | 2.83 (1.55) | 5.80 (2.09) |
| Female | 1,006 | 11.26 (4.60) | 2.12 (1.66) | 2.11 (1.46) | 4.45 (2.09) | 2.56 (1.55) | 6.40 (2.08) |
| 4 | |||||||
| Male | 1,514 | 11.64 (4.68) | 1.94 (1.62) | 2.15 (1.45) | 4.85 (2.23)* | 2.68 (1.61) | 6.08 (2.11) |
| Female | 1,281 | 11.03 (4.67) | 2.15 (1.77)* | 1.97 (1.45) | 4.48 (2.08) | 2.42 (1.61) | 6.68 (2.08) |
| 5 | |||||||
| Male | 1,404 | 11.02 (4.79) | 1.84 (1.69) | 1.93 (1.49) | 4.65 (2.28)* | 2.58 (1.55) | 6.48 (2.13) |
| Female | 1,290 | 10.51 (4.84) | 2.11 (1.84)* | 1.80 (1.43) | 4.19 (2.10) | 2.39 (1.55) | 6.96 (2.05) |
| 6 | |||||||
| Male | 711 | 10.38 (4.55)* | 1.71 (1.59) | 1.83 (1.39) | 4.46 (2.18) | 2.37 (1.45)* | 6.81 (2.08) |
| Female | 613 | 10.30 (5.27) | 2.10 (1.96)* | 1.80 (1.55) | 4.02 (2.25) | 2.36 (1.60) | 7.10 (2.10) |
| All | |||||||
| Male | 4,710 | 11.29 (4.69) | 1.88 (1.64) | 2.06 (1.45) | 4.69 (2.23)† | 2.64 (1.56) | 6.25 (2.13) |
| Female | 4,190 | 10.82 (4.81) | 2.12 (1.80)† | 1.93 (1.47) | 4.32 (2.12) | 2.43 (1.58) | 6.76 (2.09) |
Scale completed by parents or guardians. Data presented as mean (standard deviation).
SDQ = Strengths and Difficulties Questionnaire.
p < 0.05;
p < 0.0001.
A total of 1,279 (14.4%) children had SDQ total difficulty scores in the borderline range (15.5% boys and 13.1% girls). Of the 1,209 (13.6%) children with total difficulty scores in the abnormal range, 14.2% were boys and 12.9% were girls. In all subscales and in the total SDQ scores, there were significant gender differences (p < 0.0001): there were more boys in the abnormal range for total SDQ scores, conduct problems, hyperactivity, peer problems and pro-social behavior, while girls presented more emotional symptoms (Table 3).
Table 3. Prevalence of childhood behavior problems as measured by the SDQ.
| All children (n=8,900) | Male (n=4,710, 52.9%) | Female (n=4,190, 47.1%) | p-value for interaction male vs. female | ||||
|---|---|---|---|---|---|---|---|
| SDQ scores | Borderline | Abnormal | Borderline | Abnormal | Borderline | Abnormal | |
| Total SDQ scores | 1,279 (14.4) | 1,209 (13.6) | 729 (15.5) | 667 (14.2) | 550 (13.1) | 542 (12.9) | 0.001 |
| Emotional symptoms | 766 (8.6) | 804 (9.0) | 385 (8.2) | 365 (7.7) | 381 (9.1) | 439 (10.5) | <0.0001 |
| Conduct problems | 1,361 (15.3) | 1,237 (13.9) | 782 (16.6) | 691 (14.7) | 579 (13.8) | 546 (13.0) | <0.0001 |
| Hyperactivity problems | 1,148 (12.9) | 1,679 (18.9) | 645 (13.7) | 1,022 (21.7) | 503 (12.0) | 657 (15.7) | <0.0001 |
| Peer problems | 1,982 (22.3) | 2,273 (25.5) | 1,084 (23.0) | 1,305 (27.7) | 898 (21.4) | 968 (23.1) | <0.0001 |
| Pro-social behavior | 1,566 (17.6) | 1,440 (16.2) | 910 (19.3) | 895 (19.0) | 656 (15.7) | 545 (13.0) | <0.0001 |
Scale completed by parents or guardians. Data presented as n (%).
SDQ = Strengths and Difficulties Questionnaire.
The prevalence of total abnormal SDQ scores was 14.4% among 3-year-olds and 8.5% among 6-year-olds. Across all ages, peer problems and hyperactivity seems to be the most frequent problems among the assessed children (Table 4).
Table 4. Prevalence of abnormal total and subscale SDQ scores by age.
| 3-year-olds (n=2,087) | 4-year-olds (n=2,795) | 5-year-olds (n=2,694) | 6-year-olds (n=1,324) | |
|---|---|---|---|---|
| Total | 307 (14.4) | 397 (14.2) | 343 (12.7) | 162 (8.5) |
| Emotional symptoms | 180 (8.6) | 245 (8.8) | 266 (9.9) | 113 (8.5) |
| Conduct problems | 324 (15.5) | 412 (14.7) | 336 (12.5) | 165 (12.5) |
| Hyperactivity problems | 401 (19.2) | 564 (20.2) | 494 (18.3) | 220 (16.6) |
| Peer problems | 583 (27.9) | 723 (25.9) | 675 (25.1) | 292 (22.1) |
| Pro-social behavior | 429 (20.6) | 492 (17.6) | 366 (13.6) | 153 (11.6) |
Data presented as n (%).
SDQ = Strengths and Difficulties Questionnaire.
Association between cesarean delivery and abnormal SDQ scores
The ORs for total difficulties and each SDQ subscale in 3-to-6-year-olds in relation to mode of delivery were estimated using logistic regression (Table 5). In the unadjusted analysis, CS was significantly associated with total abnormal SDQ scores (OR = 1.21; 95%CI 1.05-1.38; p < 0.0001). Both elective (OR = 1.17; 95%CI 1.02-1.34); p < 0.0001) and emergency (OR = 1.46; 95%CI 1.17-1.82; p < 0.0001) CS were significantly associated with total abnormal SDQ scores. These associations persisted in the fully adjusted model (model 3) for overall CS (OR = 1.27; 95%CI 1.10-1.46; p < 0.0001), as well as separately for elective (OR = 1.24; 95%CI 1.07-1.43; p < 0.0001) and emergency (OR = 1.46; 95%CI 1.16-1.83; p < 0.0001) CS.
Table 5. Association between mode of delivery and abnormal SDQ scores.
| Abnormal SDQ (n) | Unadjusted model | Model 1: Maternal factors | Model 2: Model 1 + child factors | Model 3: Model 1 + 2 + paternal factors | |
|---|---|---|---|---|---|
| Total score | |||||
| Vaginal delivery | 353 | Ref | Ref | Ref | Ref |
| CS | 856 | 1.21 (1.05-1.38)* | 1.27 (1.10-1.46)* | 1.27 (1.10-1.45)* | 1.27 (1.10-1.46)* |
| Elective | 726 | 1.17 (1.02-1.34)* | 1.24 (1.07-1.43)* | 1.23 (1.07-1.42)* | 1.24 (1.07-1.43)* |
| Emergency | 130 | 1.46 (1.17-1.82)* | 1.46 (1.16-1.83)* | 1.46 (1.16-1.83)* | 1.46 (1.16-1.83)* |
| Emotional | |||||
| Vaginal delivery | 260 | Ref | Ref | Ref | Ref |
| CS | 544 | 1.01 (0.87-1.18) | 1.04 (0.89-1.22) | 1.05 (0.89-1.23) | 1.06 (0.90-1.24) |
| Elective | 461 | 0.99 (0.84-1.16) | 1.02 (0.87-1.20) | 1.02 (0.87-1.21) | 1.03 (0.88-1.22) |
| Emergency | 83 | 1.19 (0.91-1.54) | 1.19 (0.91-1.55) | 1.18 (0.91-1.54) | 1.19 (0.91-1.55) |
| Conduct problems | |||||
| Vaginal delivery | 390 | Ref | Ref | Ref | Ref |
| CS | 847 | 1.07 (0.94-1.22) | 1.12 (0.98-1.28) | 1.12 (0.98-1.29) | 1.13 (0.98-1.29) |
| Elective | 731 | 1.06 (0.93-1.21) | 1.11 (0.97-1.28) | 1.12 (0.97-1.28) | 1.12 (0.97-1.29) |
| Emergency | 116 | 1.15 (0.92-1.45) | 1.15 (0.91-1.45) | 1.16 (0.92-1.47) | 1.16 (0.92-1.46) |
| Hyperactivity | |||||
| Vaginal delivery | 545 | Ref | Ref | Ref | Ref |
| CS | 1,134 | 1.01 (0.90-1.13) | 1.04 (0.92-1.17) | 1.03 (0.92-1.16) | 1.02 (0.91-1.15) |
| Elective | 973 | 0.99 (0.88-1.12) | 1.04 (0.92-1.17) | 1.03 (0.91-1.16) | 1.02 (0.90-1.15) |
| Emergency | 161 | 1.10 (0.90-1.35) | 1.07 (0.87-1.31) | 1.06 (0.86-1.20) | 1.05 (0.85-1.29) |
| Peer problems | |||||
| Vaginal delivery | 718 | Ref | Ref | Ref | Ref |
| CS | 1,555 | 1.07 (0.96-1.19) | 1.11 (1.00-1.24)* | 1.10 (0.99-1.23) | 1.11 (0.99-1.24) |
| Elective | 1,332 | 1.04 (0.93-1.17) | 1.09 (0.98-1.22) | 1.08 (0.97-1.21) | 1.09 (0.97-1.22) |
| Emergency | 223 | 1.23 (1.02-1.48)* | 1.24 (1.03-1.50)* | 1.24 (1.02-1.50)* | 1.25 (1.03-1.51)* |
| Pro-social behavior | |||||
| Vaginal delivery | 422 | Ref | Ref | Ref | Ref |
| CS | 1,018 | 1.21 (1.06-1.37)* | 1.26 (1.11-1.44)† | 1.27 (1.11-1.44)† | 1.27 (1.12-1.45)† |
| Elective | 889 | 1.21 (1.07-1.38)* | 1.28 (1.12-1.46)† | 1.28 (1.12-1.46)† | 1.29 (1.13-1.47)† |
| Emergency | 129 | 1.15 (0.92-1.43) | 1.17 (0.93-1.46) | 1.17 (0.93-1.46) | 1.17 (0.94-1.47) |
Data presented as odds ratio (95% confidence interval).
CS = cesarean section; Ref = reference category; SDQ = Strengths and Difficulties Questionnaire.
Model 1 (maternal factors): maternal age, education, smoking, drinking, body mass index (BMI), and gestational weight gain; Model 2 (Model 1 + child factors): child gender, age, birth weight, gestational age, having sibling, duration of breastfeeding; Model 3 (Model 1 + Model 2 + paternal factors): paternal age, education, smoking, drinking, and BMI.
p < 0.05;
p < 0.0001.
When SDQ scores were broken down by subgroup, CS was significantly associated with peer problems in Model 1 (OR = 1.11; 95%CI 1.00-1.24; p < 0.05). In the unadjusted analysis, CS was significantly associated with pro-social behavior (OR = 1.21; 95%CI 1.06-1.37; p < 0.0001). In the fully adjusted model, CS only remained significantly associated with pro-social behavior (OR = 1.27; 95%CI 1.12-1.45; p < 0.0001). Additionally, elective CS was significantly associated with pro-social behavior in both the unadjusted (OR = 1.21; 95%CI 1.07-1.38; p < 0.0001) and fully adjusted models (OR = 1.29; 95%CI 1.13-1.47; p < 0.0001). Emotional symptoms, conduct problems, and hyperactivity were not associated with any CS in unadjusted or adjusted models.
Discussion
The results of this study suggest that the prevalence of emotional and behavior problems reported by parents through the SDQ for this sample of preschoolers (aged 3 to 6 years) is consistent with previous studies conducted in other Asian and Western countries. Overall, 13.6% of children had SDQ total difficulty scores in the abnormal range. This prevalence is partially in line with that of a German sample reported by Fuchs et al.,7 who found 7.8% of preschool children in abnormal range. A higher prevalence of total SDQ difficulties in abnormal range (27.6%) was reported by Theunissen et al.29 in a sample of Dutch preschoolers. In Iranian and Malaysian child samples, the prevalence of total SDQ ranged from 5 to 16.7%.30,31
The prevalence of peer problems in our sample was 25.5%. We also found a significant association between emotional/behavior problems and gender, with emotional symptoms being more prevalent in girls. Abnormal total difficulties, conduct problem, hyperactivity, and pro-social behavior scores were more prevalent among boys. These results are consistent with several previous studies.6,30 Emotional or behavior problems among preschoolers may arise due to the fact that, when children enter kindergarten, external factors may become very important in influencing what children do and the choices they make. Parenting factors or the home environment might also have a greater effect. A previous report suggested that children’s self-concepts of ability were primarily influenced by parents’ beliefs, expectations, attitudes, and behavior.32 The present study revealed that the prevalence of abnormal total SDQ, conduct problems, peer problems, and pro-social behavior scores in Chinese preschoolers decreased with age.
The CS rate among all mothers participating in the study was 67.3% (58.4% for elective CS, at the mother’s request or suggested by a healthcare provider, and 8.9% for emergency CS performed after failure of spontaneous delivery). Parental education level, parental age, firstborn status, high pre-pregnancy BMI, and more gestational weight gain were the main determinants of high CS rate in this sample. Several studies conducted in China have reported various reasons that contribute to an increased rate of CS by maternal request, including choice of specific birth date, fear of pain, wish to keep fit, socioeconomic factors, and belief that CS is safer for the mother and newborn.10,33 It has been suggested that healthcare providers in China may opt for CS without medical reasons due to profits gained from successfully performed CS; some healthcare providers also suggest CS to expectant mothers as a defensive medicine practice for fear of malpractice claims which may arise from events occurring during spontaneous delivery.11,34,35 Despite the proven risks of CS for newborns during early or later childhood, as well as its socioeconomic burden on individuals and on the healthcare system, the unnecessary CS rate continues to rise in China.
In the present study, we found evidence suggesting that CS was significantly associated with total SDQ scores, which is consistent with previous studies reporting associations of CS with ASD36 and ADHD.16 In contrast, two recent studies reported no such associations. Curran et al.18 found no association between CS and abnormal SDQ scores in children at age 7, while Al Khalaf et al.19 reported no significant association between CS and total SDQ scores in 3-year-olds. Regarding SDQ subscales, our results suggest that CS is associated with childhood behavior problems but not with emotional problems, conduct problems, or hyperactivity. The significant association observed between CS and total SDQ scores, but not with most of the SDQ subscales, may be explained by the lower confidence intervals (close to one) in all four subscales. Our large sample size might also have increased the chance of detecting a significant association between CS and total SDQ scores.
Our findings are difficult to compare with those of previous studies: first, because few studies used the parent-rated version of the SDQ to examine the association between CS and development of childhood behavior; second, because of the age bracket in which outcomes were assessed. These factors may explain our inconsistent findings. For example, in China, Li et al.20 used the Child Behavior Checklist (CBCL) and reported a lower risk of childhood psychopathological problems in preschool children born via maternally requested CS. In sub-analyses, we divided CS into elective or emergency CS, and the significant association observed remained in both unadjusted and adjusted models. In SDQ subscales, no association of elective or emergency CS with emotional problems, conduct problems, or hyperactivity was found. However, emergency CS was significantly associated with peer problem scores, while elective CS was associated with pro-social behavior scores. Contradicting these findings, a recent British cohort study found no association of elective or emergency CS with any SDQ subscales.18 These conflicting results could be attributable to age at outcome (peer and behavior problems) assessment. The British cohort study assessed childhood behavior at age 7 years, while our study included preschoolers aged 3-6 years. The risk of abnormal total scores or abnormal SDQ subgroups might decrease as children grow, and may thus be lower at school age than at preschool age.
One putative biological mechanism for the association between CS and development of behavior problems is early-life exposure to microbiota. In an animal model study, the microbiome was found to play a crucial role in the presentation of distinct social behaviors.37 This is relevant, considering that behavioral problems may also be influenced by CS delivery. Children born via elective CS lack first exposure to the maternal vaginal flora, resulting in delayed and altered colonization of the infant gut microbiota.38
It has been suggested that CS mothers are more likely to have postpartum complications, which may have an impact on child development and increase the risk of adverse behavior in their children. As a psychological impact factor, development of negative behaviors and attitudes toward CS by the mother may have effects on peer and behavior problems in the child; this might explain the increased rate of neurobehavioral problems among children born via CS. These unanswered questions notwithstanding, the findings of our study are important for setting aims for future studies that can potentially identify causal pathways for childhood emotional and behavioral problems.
Strengths of this study include its large sample size compared to those of earlier studies and the multicenter design, which included of preschoolers from four cities in two provinces of the People’s Republic of China. Potential confounders, including maternal BMI, gestational weight gain, duration of breastfeeding, birth weight, and paternal BMI, were controlled, and several adjusted models were constructed to detect any change in the odds of abnormal SDQ in relation to CS. Information on mode of delivery, self-reported pre-pregnancy weight, and weight before delivery in our cross-sectional sample are expected to be accurate. Like other retrospective investigations, this study has some limitations, which may include recall bias for variables adjusted for in multiple regression models. Recall bias for confounders may have an effect on risk estimates. The use of parental informants gives rise to additional concerns: even if parents know their children better, they might be biased by their subjective needs. In addition, parental educational level has implications for parent ratings of children’s behavior, as demonstrated in a previous study.7
Lack of information on other potential confounders, including maternal attachment, depression, and parental mental health, which are known risk factors for psychological problems in children, may have led to overestimation of the risk observed in our study. It has been reported that parental neuropsychiatric disorders may increase the risk of ASD in children.39 Furthermore, the high prevalence of CS reported in our study may have increased our odds of detecting significant association between CS and development of peer or behavior problems in children. Thus, it is important to understand any long-term impact that delivery by CS may have on a child’s development of behavioral problems.
In conclusion, we observed a high prevalence of emotional/behavior problems in preschoolers. Abnormal SDQ scores for total difficulties, conduct problems, hyperactivity, and pro-social behavior were more prevalent in boys than in girls. CS delivery was associated with total SDQ score and especially with the peer problems and pro-social behavior subscales, but was not associated with emotional, conduct, or hyperactivity problems. Specifically, children delivered by elective CS had a higher risk of pro-social behavior problems compared to vaginally delivered children. Further longitudinal studies are warranted to support these findings. Methodological recommendations that could be considered for future research include using teachers as second informants and using clinical observation to identify childhood emotional/behavior problems.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
The authors express their gratitude to the children who participated in this study and their parents. This study was supported by the National Natural Science Foundation of China (grant 81373012).
References
- 1.Tick NT, van der Ende J, Verhulst FC. Twenty-year trends in emotional and behavioral problems in Dutch children in a changing society. Acta Psychiatr Scand. 2007;116:473–82. doi: 10.1111/j.1600-0447.2007.01068.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown CM, Copeland KA, Sucharew H, Kahn RS. Social-emotional problems in preschool-aged children: opportunities for prevention and early intervention. Arch Pediatr Adolesc Med. 2012;166:926–32. doi: 10.1001/archpediatrics.2012.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: homotypic continuity and course over 24 months. Arch Gen Psychiatry. 2009;66:897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park JH, Bang YR, Kim CK. Sex and age differences in psychiatric disorders among children and adolescents: high-risk students study. Psychiatry Investig. 2014;11:251–7. doi: 10.4306/pi.2014.11.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiaoli Y, Chao J, Wen P, Wenming X, Fang L, Ning L, et al. Prevalence of psychiatric disorders among children and adolescents in northeast China. PLoS One. 2014;9:e111223. doi: 10.1371/journal.pone.0111223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayes L. Problem behaviours in early primary school children: Australian normative data using the strengths and difficulties questionnaire. Aust N Z J Psychiatry. 2007;41:231–8. doi: 10.1080/00048670601172715. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs S, Klein AM, Otto Y, von Klitzing K. Prevalence of emotional and behavioral symptoms and their impact on daily life activities in a community sample of 3 to 5-year-old children. Child Psychiatry Hum Dev. 2013;44:493–503. doi: 10.1007/s10578-012-0343-9. [DOI] [PubMed] [Google Scholar]
- 8.Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gulmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2016;123:745–53. doi: 10.1111/1471-0528.13592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng XL, Xu L, Guo Y, Ronsmans C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ. 2012;90:30–9. doi: 10.2471/BLT.11.090399. 39A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu Y, Tao H, Cheng Z. Caesarean sections in Beijing, China - Results from a descriptive study. Gesundheitswesen. 2016;78:e1–5. doi: 10.1055/s-0035-1549937. [DOI] [PubMed] [Google Scholar]
- 11.Shi Y, Jiang Y, Zeng Q, Yuan Y, Yin H, Chang C, et al. Influencing factors associated with the mode of birth among childbearing women in Hunan Province: a cross-sectional study in China. BMC Pregnancy Childbirth. 2016;16:108. doi: 10.1186/s12884-016-0897-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deng W, Klemetti R, Long Q, Wu Z, Duan C, Zhang WH, et al. Cesarean section in Shanghai: women's or healthcare provider's preferences? BMC Pregnancy Childbirth. 2014;14:285. doi: 10.1186/1471-2393-14-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryding EL, Lukasse M, Parys AS, Wangel AM, Karro H, Kristjansdottir H, et al. Fear of childbirth and risk of cesarean delivery: a cohort study in six European countries. Birth. 2015;42:48–55. doi: 10.1111/birt.12147. [DOI] [PubMed] [Google Scholar]
- 14.Kolas T, Hofoss D, Daltveit AK, Nilsen ST, Henriksen T, Häger R, et al. Indications for cesarean deliveries in Norway. Am J Obstet Gynecol. 2003;188:864–70. doi: 10.1067/mob.2003.217. [DOI] [PubMed] [Google Scholar]
- 15.Tully KP, Ball HL. Misrecognition of need: women's experiences of and explanations for undergoing cesarean delivery. Soc Sci Med. 2013;85:103–11. doi: 10.1016/j.socscimed.2013.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva D, Colvin L, Hagemann E, Bower C. Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133:e14–22. doi: 10.1542/peds.2013-1434. [DOI] [PubMed] [Google Scholar]
- 17.Polo-Kantola P, Lampi KM, Hinkka-Yli-Salomaki S, Gissler M, Brown AS, Sourander A. Obstetric risk factors and autism spectrum disorders in Finland. J Pediatr. 2014;164:358–65. doi: 10.1016/j.jpeds.2013.09.044. [DOI] [PubMed] [Google Scholar]
- 18.Curran EA, Cryan JF, Kenny LC, Dinan TG, Kearney PM, Khashan AS. Obstetrical mode of delivery and childhood behavior and psychological development in a British cohort. J Autism Dev Disord. 2016;46:603–14. doi: 10.1007/s10803-015-2616-1. [DOI] [PubMed] [Google Scholar]
- 19.Al Khalaf SY, O'Neill SM, O'Keeffe LM, Henriksen TB, Kenny LC, Cryan JF, et al. The impact of obstetric mode of delivery on childhood behavior. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1557–67. doi: 10.1007/s00127-015-1055-9. [DOI] [PubMed] [Google Scholar]
- 20.Li HT, Ye R, Achenbach TM, Ren A, Pei L, Zheng X, et al. Caesarean delivery on maternal request and childhood psychopathology: a retrospective cohort study in China. BJOG. 2011;118:42–8. doi: 10.1111/j.1471-0528.2010.02762.x. [DOI] [PubMed] [Google Scholar]
- 21.Gao X, Shi W, Zhai Y, He L, Shi X. Results of the parent-rated strengths and difficulties questionnaire in 22,108 primary school students from 8 provinces of China. Shanghai Arch Psychiatry. 2013;25:364–74. doi: 10.3969/j.issn.1002-0829.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry, Chinese Civil Affair . Civil affair development statistical report 2009 [Internet]. Beijing, China: [cited 2016]. www.mca.gov.cn/article/zwgk/mzyw/201006/20100600080798.shtml?2. [Google Scholar]
- 23.Zhu B, Zhang J, Qiu L, Binns C, Shao J, Zhao Y, et al. Breastfeeding rates and growth charts--the Zhejiang infant feeding trial. Int J Environ Res Pub Health. 2015;12:7337–47. doi: 10.3390/ijerph120707337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the strengths and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534–9. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 25.Vostanis P. Strengths and difficulties questionnaire: research and clinical applications. Curr Opin Psychiatry. 2006;19:367–72. doi: 10.1097/01.yco.0000228755.72366.05. [DOI] [PubMed] [Google Scholar]
- 26.Du Y, Kou J, Coghill D. The validity, reliability and normative scores of the parent, teacher and self report versions of the strengths and difficulties questionnaire in China. Child Adolesc Psychiatry Ment Health. 2008;2:8. doi: 10.1186/1753-2000-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–45. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Wu X, Tao S, Rutayisire E, Chen Y, Huang K, Tao F. The relationship between screen time, nighttime sleep duration, and behavioural problems in preschool children in China. Eur Child Adolesc Psychiatry. 2017;26:541–8. doi: 10.1007/s00787-016-0912-8. [DOI] [PubMed] [Google Scholar]
- 29.Theunissen MH, Vogels AG, de Wolff MS, Reijneveld SA. Characteristics of the strengths and difficulties questionnaire in preschool children. Pediatrics. 2013;131:e446–54. doi: 10.1542/peds.2012-0089. [DOI] [PubMed] [Google Scholar]
- 30.Mohammadi MR, Salmanian M, Ghanizadeh A, Alavi A, Malek A, Fathzadeh H, et al. Psychological problems of Iranian children and adolescents: parent report form of strengths and difficulties questionnaire. J Ment Health. 2014;23:287–91. doi: 10.3109/09638237.2014.924049. [DOI] [PubMed] [Google Scholar]
- 31.Gomez R, Suhaimi AF. Incidence rates of emotional and behavioural problems in Malaysian children as measured by parent ratings of the strengths and difficulties questionnaire. Asian J Psychiatr. 2013;6:528–31. doi: 10.1016/j.ajp.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Wigfield A, Eccles JS. Expectancy-value theory of achievement motivation. Contemp Educ Psychol. 2000;25:68–81. doi: 10.1006/ceps.1999.1015. [DOI] [PubMed] [Google Scholar]
- 33.Lee LY, Holroyd E, Ng CY. Exploring factors influencing Chinese women's decision to have elective caesarean surgery. Midwifery. 2001;17:314–22. doi: 10.1054/midw.2001.0274. [DOI] [PubMed] [Google Scholar]
- 34.Bogg L, Huang K, Long Q, Shen Y, Hemminki E. Dramatic increase of Cesarean deliveries in the midst of health reforms in rural China. Soc Sci Med. 2010;70:1544–9. doi: 10.1016/j.socscimed.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 35.Ji H, Jiang H, Yang L, Qian X, Tang S. Factors contributing to the rapid rise of caesarean section: a prospective study of primiparous Chinese women in Shanghai. BMJ Open. 2015;5:e008994. doi: 10.1136/bmjopen-2015-008994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Curran EA, O'Neill SM, Cryan JF, Kenny LC, Dinan TG, Khashan AS, et al. Research review: birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. J Child Psychol Psychiatry. 2015;56:500–8. doi: 10.1111/jcpp.12351. [DOI] [PubMed] [Google Scholar]
- 37.Desbonnet L, Clarke G, Shanahan F, Dinan TG, Cryan JF. Microbiota is essential for social development in the mouse. Mol Psychiatry. 2014;19:146–8. doi: 10.1038/mp.2013.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Biasucci G, Rubini M, Riboni S, Morelli L, Bessi E, Retetangos C. Mode of delivery affects the bacterial community in the newborn gut. Early Hum Dev. 2010;86:13–5. doi: 10.1016/j.earlhumdev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Khaiman C, Onnuam K, Photchanakaew S, Chonchaiya W, Suphapeetiporn K. Risk factors for autism spectrum disorder in the Thai population. Eur J Pediatr. 2015;174:1365–72. doi: 10.1007/s00431-015-2544-2. [DOI] [PubMed] [Google Scholar]