Abstract
Objective:
To analyze the prevalence of common mental disorders (CMD) assessed with the Self Reporting Questionnaire (SRQ-20), using the established cutoff point, and comparing it with the results of a joint correspondence factor analysis (CFA) and cluster analysis and of a latent class analysis (LCA).
Methods:
A cross-sectional study was carried out in an urban sample of 1,095 women aged 19 to 55 years. Joint CFA-cluster analysis and LCA were used.
Results:
We found a high prevalence of CMD, regardless of classification method (37.6% when using the cutoff point; 44.4% and 52% for LCA and joint CFA-cluster, respectively). The alternative analysis strategies describe the cases more efficiently when compared to the traditional cutoff method, especially regarding more severe symptoms. Both alternative strategies also provide a description of the SRQ-20 dimensions in their particularities, which may be useful for the planning and implementation of specific actions in a given population.
Conclusion:
The SRQ-20 cutoff point seems to underestimate the magnitude of CMD among women. The alternative methods of analysis presented herein highlight the different possibilities of using this important instrument of screening for mental health.
Keywords: Screening, mental health, multivariate analysis, latent class analysis, correspondence analysis
Introduction
Epidemiological studies have consistently reported a high prevalence of psychiatric disorders worldwide, especially in developing countries.1 Although disorders including insomnia, anxiety, fatigue, irritability, depressive moods, difficulty concentrating, and somatic complaints are very common among adults, they are quite often overlooked and effective treatment is not provided.1-4
This set of symptoms comprises the group of common mental disorders (CMD).1 CMDs refer to conditions of psychic distress that meets the nosological criteria of the ICD-10 and the DSM for the most prevalent disorders, including the groups of anxiety, depressive, and substance abuse disorders (mainly alcohol), in their mild or even moderate forms. They are well-known causes of major functional incapacity, which is often as significant as that seen in well-established psychiatric conditions. In addition to the individual’s distress, this condition has a considerable socioeconomic impact due to absenteeism and demands for health services, and thus represents a public health concern.1,5 CMDs have particularly significant implications regarding women’s health and prenatal and childhood health.6
Population-based studies conducted in industrialized countries have reported a prevalence of CMD ranging from 7 to 30%, with a mean of 17% (12.5% in men and 20% in women).7 In Latin America, Africa, and India, the reported prevalence exceeded 30% in the community and approximately 50% in the primary care setting.6,8,9 In Brazil, around 50% of patients seeking primary care services were identified as suspected CMD cases.10 An overall prevalence of 23% was reported in the town of Pelotas, and 35% in the city of Recife.6
Considering the socioeconomic impact of CMDs in developing countries and how challenging it can be to diagnose these disorders in primary care practice, the World Health Organization (WHO) developed the Self Reporting Questionnaire (SRQ-20), a screening instrument to identify suspected CMD cases in primary care settings,11,12 which has been used in many countries.13-15 The SRQ-20 has been validated in Brazil, with high sensitivity (83%) and specificity (80%). Despite not being a diagnostic instrument, it has screening ability to detect relevant psychic distress. The traditional method is to define individuals who reach a certain cutoff as CMD cases. This cutoff is set based on gender: six or more positive answers for men (as they are more likely to yield false-negative results) and eight or more positive answers for women.12
Evidence for the latent structure of the SRQ-20 is conflicting; point analyses have been unable to reveal specific symptoms that support specific results, which demonstrates a need for other scoring methods. A more accurate classification of individuals13-15 could be achieved by alternative analytical methods. Such alternative strategies for analysis of multidimensional categorical data include latent class analysis (LCA) and a joint strategy using correspondence factor analysis (CFA) and cluster analysis.16-19 These have been used to measure levels of different psychosocial variables.16 LCA considers the model-based clustering approach, which derives clusters using a probabilistic model that describes data response patterns, whereas joint CFA-cluster analysis finds clusters with some arbitrarily chosen distance measure, defining groups of observations based on similarities between them.
Within this context, the aim of the present study was twofold: to assess the prevalence of CMD using the SRQ-20 in a sample of women living in a Brazilian urban area; and to identify differences between the standard cutoff approach and alternative statistical methods to describe CMD symptoms and prevalence.
Methods
Study design and sample
This a cross-sectional study is part of the SCAALA (Social Changes, Asthma, and Allergy in Latin America) research program carried out in Salvador, Brazil. SCAALA aims to investigate potential risk factors, such as early exposure to infections and nutritional, immunological, and psychosocial aspects, associated with the occurrence of asthma and other allergic diseases.20,21 The study population was 1,445 children selected through random sampling from 24 poor geographical areas used previously to evaluate the impact of a sanitation program in the city of Salvador.21 For the present study, we included 1,095 women, aged 19 to 55, who were the mothers of the children participating in SCAALA and from whom all information necessary for the analyses of interest was available.
Data collection
The SRQ-20 was used to investigate suspected CMD cases among the children’s caretakers. This instrument consists of 20 yes/no questions pertaining to the month before the interview. Answers indicate whether symptoms in four scales – anxiety and depression, somatic symptoms, reduced vital energy, and depressive thoughts – were present or absent.12,15 The four SRQ-20 scales were evaluated separately, focusing on the most prevalent symptoms in each scale, as well as globally. Data were collected through home interviews administered by trained psychologists and psychology students between January and November 2006. Sociodemographic data were collected using a standard questionnaire administered jointly with the SRQ-20.
Statistical analysis
The prevalence of CMD was estimated from a cutoff point defined according to the number of positive answers for symptoms. Subjects were classified as suspected CMD cases when they had eight or more positive items. Joint CFA-cluster analysis and LCA were used to identify structures within the data, reducing their dimensionality based on similarity/dissimilarity patterns and visualization techniques. We used both approaches for classifying the individuals as suspected CMD cases.
CFA is a multivariate, descriptive, and exploratory approach for statistical analysis of contingency tables including a large number of variables.22 This method assesses the association between categorical variables that produce contingency tables.23 CFA was used to assess potential associations or similarities between answers in each CMD scale (depression, anxiety, somatoform disorders)12 of the SRQ-20. The chi-square distance metric produced by CFA was used directly to cluster the individuals, resulting in a joint CFA-cluster analysis to classify the women according to the reported symptoms. This enables the elements of a sample to be arranged into groups so that elements that are similar with regard to the measured variables are grouped together. As a result, elements of different groups would be heterogeneous with regard to the same characteristics measured.22 Based on this analytical strategy, cases were classified according to the aforementioned four scales of symptoms. Analyses were performed separately for each scale, and then results were used for a combined description of symptoms. The conditional probabilities generated by this joint analysis were used to describe the corresponding clusters. One of the most attractive features of this method is the graphic display of the results of correspondence analysis. The association between categories of variables is represented graphically by points in a space of reduced dimension (through factor axes). R software version 3.1.1 was used for the joint CFA-cluster analysis.
The other methodology used was the LCA, a well-known approach for analysis of multivariate categorical variables,23,24 usually referred to as the analogous factor analysis of continuous measurements. It postulates the categorical latent variable with c classes such that the observed relationships between the manifest variables (also known as indicators) are assumed to result from the underlying classification of the data produced by the categorical latent variable. An important assumption of LCA is conditional independence, i.e., within any class of the latent variable, the observed categorical variables are assumed to be independent of each other. This assumption refers only to the condition based on the latent variable and does not imply that the manifest variables are independent in the analyzed data. In fact, the relationships between manifest variables can be explained by the latent variable. The interpretation of the LCA results is mainly based on class membership probabilities and item-response probabilities conditional on class membership. The conditional probabilities represent a measure of the degree of association between each manifest variable and each latent class, with higher probability representing the greater association. Goodness-of-fit statistics include entropy, likelihood ratio test, the Akaike information criterion, and the Bayesian information criterion, which can be used to choose the best number of classes to describe the data. Initially, we applied LCA to each dimension separately to uncover the underlying latent classes. Then, we applied LCA using the latent classes described in the initial step and the manifest variables describing CMD. Mplus V.5.2 software25 was used to fit the LCA.
Finally, Cohen’s kappa statistic was used to measure agreement between the two different forms of classification based on the joint CFA-cluster analysis and on LCA. STATA v.10 software was used for data management and descriptive univariate and bivariate analyses.
Ethical considerations
The protocol used in this study was approved in 2004 by the ethics committee of Universidade Federal da Bahia and by the appropriate regulatory authorities of the Brazilian Ministry of Health. All participants signed informed consent forms. Women who were found to have severe symptoms of mental distress or who spontaneously requested psychological support were advised to seek adequate care within the public mental health care service.
Results
The majority of the women in the study population owned their homes (87.7%), which were connected to the sewerage system (83.1%). About 58.0% of the women were aged 30 or older, 19.8% completed high school or college, 25.1% were single, and 2.5% were divorced or widowed (data not shown).
Description of symptoms
In the anxiety and depression scale, the most reported symptom (75.0%) was feel[ing] nervous, tense, or worried. Only 25.4% reported cry[ing] more than usual. In the somatic symptoms scale, most (49.4%) reported headaches, while only 23.0% reported poor digestion. In the reduced vital energy scale, 14.2% reported daily work suffering, and 26.9% had trouble thinking clearly. In the depressive thoughts scale, the most commonly reported symptom was lost interest in things (23.7%), followed by feeling worthless (12.4%) and thoughts of ending one’s life (7.2%) (Table 1).
Table 1. Prevalence of common mental disorder symptoms in SRQ-20 scales, overall and according to the results of LCA and joint CFA-cluster analysis, Salvador, Brazil.
| Scale/categories | Overall (%) | CFA | LCA | ||
|---|---|---|---|---|---|
| % suspect | % not suspect | % suspect | % not suspect | ||
| Depressive/anxious | (n=785) | (n=262) | (n=530) | (n=517) | |
| Feel nervous, tense or worried | 75.0 | 100.00 | 0.00 | 93.8 | 56.7 |
| Easily frightened | 55.3 | 62.93 | 32.44 | 74.1 | 37.0 |
| Feel unhappy | 52.2 | 62.29 | 22.14 | 92.1 | 13.4 |
| Cry more than usual | 25.4 | 31.08 | 8.40 | 50.3 | 1.10 |
| Somatic symptoms | (n=316) | (n=731) | (n=401) | (n=646) | |
| Often have headaches | 49.4 | 78.80 | 36.36 | 76.7 | 30.1 |
| Sleep badly | 41.7 | 71.84 | 28.73 | 70.6 | 21.3 |
| Uncomfortable feelings in the stomach | 31.3 | 83.86 | 8.62 | 63.2 | 8.80 |
| Poor digestion | 23.0 | 67.09 | 3.97 | 48.5 | 5.10 |
| Poor appetite | 34.7 | 62.97 | 22.44 | 61.4 | 15.8 |
| Hands shake | 24.4 | 50.00 | 13.27 | 44.7 | 10.0 |
| Reduced vital energy | (n=385) | (n=662) | (n=385) | (n=662) | |
| Easily tired | 35.9 | 83.38 | 8.31 | 78.7 | 11.2 |
| Difficult to make decisions | 32.1 | 60.26 | 15.71 | 60.1 | 15.9 |
| Difficult to enjoy your daily activities | 33.1 | 64.16 | 15.11 | 64.7 | 14.9 |
| Daily work suffering | 14.2 | 31.43 | 4.23 | 32.0 | 4.00 |
| Feel tired all the time | 41.1 | 85.19 | 15.41 | 81.6 | 17.6 |
| Trouble thinking clearly | 26.9 | 53.51 | 11.48 | 53.8 | 11.4 |
| Depressive thoughts | (n=351) | (n=696) | (n=150) | (n=897) | |
| Unable to play a useful part | 11.1 | 33.05 | 0.00 | 94.6 | 63.3 |
| Lost interest in things | 23.7 | 70.66 | 0.00 | 88.4 | 21.9 |
| Thought of ending your life | 7.2 | 21.37 | 0.00 | 98.4 | 67.6 |
| Feel that you are a worthless person | 12.4 | 37.04 | 0.00 | 97.4 | 56.5 |
CFA = correspondence factor analysis; LCA = latent class analysis; SRQ-20 = Self Reporting Questionnaire.
Scale-specific analysis
The results both of joint CFA-cluster analysis and of LCA are described for each SRQ-20 dimension separately.
Joint CFA-cluster analysis
One indicator (discriminating women more or less frequently reporting symptom items) was defined for each of the SRQ-20 scales. These indicators depict the groups described in Table 1. The first indicator of reporting items related to anxiety and depression comprises two groups: one in which symptom items are reported more frequently (suspect) and one in which symptoms are reported less frequently (not suspect). The same method was applied to the indicators of somatic symptoms, reduced vital energy, and depressive thoughts. The suspect group shows the highest proportion of subjects reporting CMD symptom items in all four scales. In each scale, the highest proportion of reporting items for this group were in the categories feel nervous, tense or worried (100.0%), uncomfortable feelings in the stomach (83.9%), felt tired all the time (85.2%), and lost interest in things (70.7%). In contrast, 0.0%, 8.6%, 15.4%, and 0.0% of women in the other group (not suspect) reported the corresponding items (Table 1).
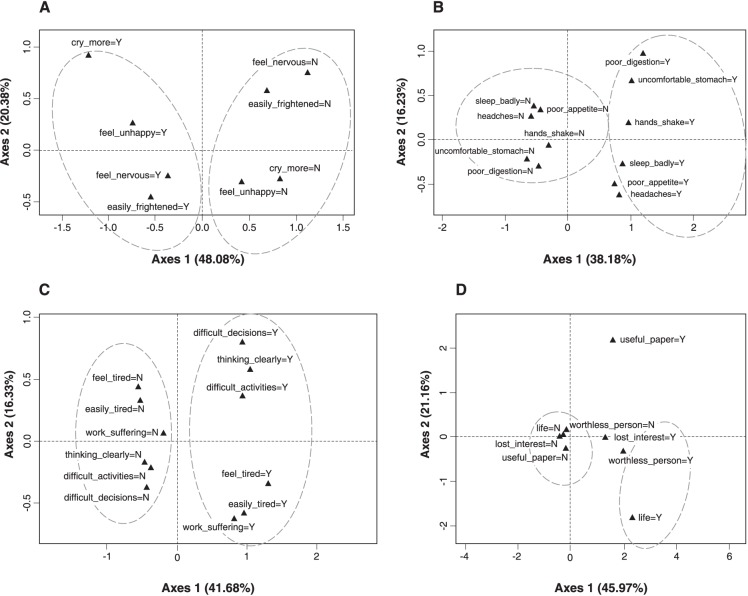
Figure 1 graphically represents CFA results for each of the scales assessed. The goal here is to analyse the relationships between the symptoms in each of the SRQ-20 scales. The graphs show the position of each answer category, and these positions can be interpreted as the associations between response patterns. Points that are close together in the chart imply a stronger association between symptom categories. The variability of the data is broken down and expressed by factor axes. In general, the first two factor axes explain the majority of the variability in the data and were considered in this analysis. For the anxiety and depression scale (Figure 1A), the first two axes explain 68.5% of the total data variability. For the somatic symptoms scale, however, these axes explain 54.4% of the total variability of the analyzed characteristics (Figure 1B). In the assessment of association between symptoms of related scales, two clearly distinct groups of women were identified: one with all symptoms and one with no symptoms. This distinction between groups was illustrated in each scale using oval diagrams (Figure 1). The left-hand side of Figure 1D shows a cluster of negative responses for lacking inability to play a useful part, lost interest in things, thought of ending one’s life, and feeling a worthless person, while on the right-hand side, all these symptoms are reported positively. In the quadrants of Figure 1C, four groups can be distinguished, indicating co-occurrence of the following symptoms: quadrant 1 – difficulty enjoying your daily activities, trouble thinking clearly, and making decisions (difficult_activities=Y, trouble thinking=Y, and difficult_decisions=Y); quadrant 2 – not easily tired all the time (tired=N and easily tired=N) and no daily work suffering (work suffering=N); quadrant 3 – no difficulty enjoying your daily activities, no trouble thinking clearly, no difficulty making decisions (difficult_activities=N, trouble thinking=N, and difficult_decision=N); quadrant 4 – easily tired all the time (tired=Y and easily tired=Y) and daily work suffering (work suffering=Y).
Figure 1. Correspondence factor analysis for each symptom scale: A) anxiety and depression, B) somatic symptoms, C) reduced vital energy, and D) depressive thoughts.
Latent class analysis (LCA)
For the depressive/anxious dimension, we observed that, among the participants classified as suspects, the probability of having symptoms in any of the items ranged from 50.3 to 93.8%. On the other hand, among those who were classified as not suspects, the probability of such symptoms ranged from 1.1 to 56.7% (Table 1). A similar pattern was observed for the somatic symptoms subscale, in which the probability of having CMD symptoms among participants classified as suspects ranged from 44.7 to 76.7%, while those classified as not suspects had a lower probability of such symptoms (from 5.1 to 30.1%). Furthermore, for the items that made up the dimension of reduced vital energy, the probability of reporting this type of symptoms ranged from 32.0 to 81.6% and from 4.0 to 17.6% among women classified as suspect and not suspect, respectively (Table 1). The entropy values for the each dimension analyzed were: depressive/anxious, 0.70; somatic symptoms, 0.65; reduced vital energy, 0.73; and depressive thoughts, 0.75, indicating adequate fit overall (Table 1).
Overall analysis
Here, we will describe and compare the results regarding CMD prevalence and characterization of symptoms in both groups, as detected by the three statistical methodologies used to define CMD.
The prevalence of CMD according to the conventional cutoff point was 37.6%. Joint CFA-cluster analysis used the four aforementioned indicators for each scale of the SRQ-20 to define an overall indicator of CMD based on associations between the scales of the questionnaire. According to this method, 52.0% of participants were classified as having CMD symptoms (denoted as Suspect/CFA). Based on the LCA method, 44.4% of women were classified as suspected CMD (entropy = 0.57) (Table 2).
Table 2. Proportion of women who reported symptoms on the SRQ-20 among those suspected of having common mental disorders, Salvador, Brazil.
| Scale/categories | % | ||
|---|---|---|---|
| Score ≥ 8 | Suspect/CFA | Suspect/LCA | |
| CMD prevalence | 37.6 | 52.0 | 44.4 |
| Depressive/anxious | |||
| Feel nervous, tense, or worried | 96.2 | 95.6 | 96.2 |
| Easily frightened | 82.0 | 70.6 | 70.2 |
| Feel unhappy | 85.8 | 74.3 | 96.0 |
| Cry more than usual | 51.3 | 38.6 | 49.8 |
| Somatic symptoms | |||
| Often have headaches | 74.4 | 65.3 | 80.3 |
| Sleep badly | 71.3 | 59.9 | 75.3 |
| Uncomfortable feelings in the stomach | 55.8 | 50.4 | 66.1 |
| Poor digestion | 43.4 | 38.1 | 52.9 |
| Poor appetite | 61.7 | 50.9 | 67.1 |
| Hands shake | 48.5 | 37.7 | 48.6 |
| Reduced vital energy | |||
| Easily tired | 69.0 | 60.8 | 83.4 |
| Difficult to make decisions | 56.3 | 50.2 | 60.3 |
| Difficult to enjoy your daily activities | 52.4 | 52.0 | 64.2 |
| Daily work suffering | 31.5 | 24.4 | 31.4 |
| Feel tired all the time | 73.9 | 65.4 | 85.2 |
| Trouble thinking clearly | 52.0 | 42.6 | 53.5 |
| Depressive thoughts | |||
| Unable to play a useful part | 21.6 | 20.0 | 49.3 |
| Lost interest in things | 51.3 | 44.1 | 88.0 |
| Thought of ending your life | 17.8 | 13.8 | 40.7 |
| Feel that you are a worthless person | 28.7 | 23.0 | 67.3 |
CFA = correspondence factor analysis; CMD = common mental disorders; LCA = latent class analysis; SRQ-20 = Self Reporting Questionnaire.
Among the women classified as suspected CMD cases based on all three methods, high rates of anxiety and depression symptoms were found. For instance, 96.2%, 95.6%, and 96.2% of the women reported feeling nervous, tense, and worried, respectively, among suspected CMD cases using the conventional cutoff, CFA, and LCA. The rates of reporting symptom items were systematically higher among women with suspected CMD symptoms based on the LCA method, although they did not differ substantially (Table 2).
The results of analysis of agreement between the subgroups created by LCA and by the joint CFA-cluster analysis are presented in Table 3. For all dimensions, we observed that 78.8 to 100.0% of the participants classified as being a suspected CMD case using LCA were also classified as suspect cases using the joint CFA-cluster method. However, among the subjects classified as not suspects using LCA, 53.2% were classified as suspect cases through joint CFA-cluster analysis for the depressive/anxious dimension. For the other dimensions, the agreement between not-suspect classification with the two techniques was >77.6%.
Table 3. Levels of agreement between suspected common mental disorders subgroups, classified according to LCA and joint CFA-cluster analysis (n=1,013).
| Subgroups created using LCA | Subgroups created using joint CFA-cluster analysis | Overall % agreement | kappa | |
|---|---|---|---|---|
| Suspect n (%) | Not suspect n (%) | |||
| Depressive/anxious | ||||
| Suspect | 510 (96.2) | 20 (3.8) | 71.5 | 0.43* |
| Not Suspect | 275 (53.2) | 242 (46.8) | ||
| Somatic symptoms | ||||
| Suspect | 316 (78.8) | 85 (21.2) | 89.4 | 0.82* |
| Not Suspect | 0 | 646 (100) | ||
| Reduced vital energy | ||||
| Suspect | 385 (100) | 0 | 100 | 1.00* |
| Not Suspect | 0 | 662 (100) | ||
| Depressive thoughts | ||||
| Suspect | 150 (100) | 0 | 88.8 | 0.50* |
| Not Suspect | 201 (22.4) | 696 (77.6) | ||
| Global indicator | ||||
| Suspect | 379 (69.7) | 165 (30.3) | 75.0 | 0.50* |
| Not Suspect | 99 (19.7) | 404 (80.3) | ||
CFA = correspondence factor analysis; CMD = common mental disorders; LCA = latent class analysis.
p < 0.001.
Nevertheless, the overall percentage of agreement was high for all dimensions, ranging from 71.5% for the depressive/anxious dimension to 100.0% for the reduced vital energy dimension. Kappa values were always statistically significant, with strong agreement for the somatic symptoms and reduced vital energy dimensions and moderate agreement for all other dimensions (Table 3).
Discussion
This study investigated the occurrence of CMD among women living in a poor urban area in Salvador, Brazil. We found a high prevalence of CMD using the SRQ-20, regardless of the classification method (37.6% when using the conventional cutoff; 52% using joint CFA-cluster analysis; 44.4% using LCA).
The first analysis of each scale separately and of their related symptoms showed a predominance of the anxiety and depression scale. Three of its categories – feel nervous, tense, or worried; easily frightened; and feel unhappy – were positive at high rates: 75.0%, 55.3%, and 52.2%, respectively. The predominance of symptoms of this scale has also been reported in previous studies with women.6
In the depressive thoughts scale, the lowest prevalence values were found for unable to play a useful part and thought of ending one’s life (11.1% and 7.2%, respectively). The most prevalent symptom was lost interest in things (23.7%). According to Gonçalves,26 the symptom feeling unable to play a useful role in life had the lowest sensitivity among those included in the instrument, which can be attributed to difficulties related to understanding and interpretation, as the question includes a negative. Additionally, the most prevalent symptom of this dimension was loss of interest in things (technically called anhedonia), which is one of the core symptoms of depressive disorder,27 confirming the importance of this dimension in the characterization of suspected cases. Regarding the symptom thought of ending one’s life, indicative of more serious suffering and/or mental disorder, some special considerations are warranted, as the greatest chance of false negatives occurs here, especially when questionnaires are not self-applied (as in the case of this study).
In the somatic symptoms scale, the most prevalent symptom was often have headaches (49.4%). Higher prevalence values were seen for feel tired all the time and easily tired (41.1% and 35.9%, respectively) in the reduced vital energy scale. The prevalence values found for each scale and for each of their symptoms were consistent with previous studies.13,15,28
The distinction of two groups in the joint CFA-cluster analysis shows that, in the group with higher rates of symptoms (suspects), all women (100.0%) reported feeling nervous, tense, or worried; 62.9% reported being easily frightened; and 62.3% reported feeling unhappy. Again, the contribution of the depression/anxiety dimension to defining the groups is clear.
According to Coutinho et al.,4 a higher CMD prevalence in population groups with common characteristics may suggest potential methodological biases and contributions of biological factors and social determinants. Selection and diagnostic biases can result in higher CMD prevalence among women, as they use health services more often than men due to social and cultural factors. This is based on the assumption that women tend to perceive and report symptoms more often than men do. Regarding biological factors, intrinsic hormonal characteristics may have contributed to a higher prevalence of depressive symptoms among women. The assumption of social determination is based on the theory of life events/social support29 and social roles,30 in which common daily events, known as stress-producing events, become generic stressors that cause abnormalities in body systems, such as the endocrine system, increasing the risk of disease development (including of mental disorders).2,28
Other aspects should be taken into consideration when interpreting the data presented herein. Information bias may have influenced the responses to the questionnaire, particularly regarding depressive symptoms, due to the low socioeconomic status of our population.21 It has been previously reported that individuals with lower educational attainment tend to over-report health complaints in mental health evaluations, even when no mental condition is identified in standard psychiatric interviews.10
Clearly, the choice of analysis strategy should depend on the substantive questions posed by the researchers. However, when there is interest in describing patterns and/or data structure, different methods are available. The similarity between LCA and joint CFA-cluster analysis is that both can be expressed in a log-linear form to describe the number of observations due to each data pattern. CFA can be a rich source of valuable insights into data, particularly when the primary interest is to extract patterns in the data to visualize geometric relationships which can be summarily displayed in graphic form. The advantages of LCA over CFA include assessment of goodness of fit, modeling of the latent structure of the data, the fact it is a confirmatory analysis, the possibility of including covariates to predict the latent class membership of individuals, and the ability to model changes in the structure of the data over time. Joint CFA-cluster analysis is a dimension reduction method for data analysis which describes associations between categorical variables, and in a subsequent step defines the clusters. The main advantage of CFA is that it is not based on inferential methods, which may have questionable assumptions. It is important to highlight that LCA might not always provide a good fit to the data. Therefore, its assumptions should be evaluated carefully.31
Different techniques yield information about different aspects of data. However, there is no reason why one cannot use more than one approach when trying to uncover interesting data patterns or structures. In this paper, we used two strategies separately to explore their strengths. Other possible strategies for data analysis using these methodologies include: 1) first use LCA to test concepts, interpret, and find the meaning of latent classes, and then use CFA to illustrate the associations between the manifest variables graphically; or 2) use CFA as an exploratory technique to generate concepts and then use LCA to test the model.16,17 The first strategy is particularly helpful when the number of manifest variables is large.
One advantage of this study was that we carried out further analyses to establish suspect cases detected by the conventional cutoff point as it is defined from the total of positive responses. Despite being very useful for tracking suspected cases in the population, the cutoff method does not provide detailed knowledge of the contribution of each dimension of the instrument to suspected cases. It is important to emphasize that the SRQ-20 is not a diagnostic tool and that analysis based on the cutoff score provides generic information, which is nevertheless enough to establish the mental health profile of a given population at a given time and plan potential interventions.
Apart from corroborating the results obtained through the identification of suspected cases using the cutoff point, the information presented in this study provides a breakdown of the dimensions assessed by the SRQ-20. This may be useful for the planning and implementation of specific actions in a given population. The LCA and joint CFA-cluster analysis strategies were able describe the cases more efficiently when compared to the traditional cutoff method, which is only valid for the instrument as a whole, considering the four dimensions together. The cutoff point provides a global percentage of suspicion (suspect cases) considering all dimensions of the instrument, but it is not able to disaggregate them or describe their separate contributions to a suspected case. Particularly, the ability to describe the particularities of each dimensions means alternative analyses can describe the population of interest more efficiently, highlighting which dimensions contribute the symptoms of greater severity and their contribution to the indication of suspected cases.
Our primary goals were to assess the prevalence of CMD in a sample of poor urban mothers and to compare different methodologies to define CMD when using the SRQ-20. Even though our sample is not representative of urban Brazilian women, it was adequate to explore the difficulties in measuring CMD and present alternative statistical methodologies that can enhance use of the SRQ-20. While the estimated prevalence should not be generalized to other populations, it is important to highlight that this sample can represent women in urban areas that live in similar conditions under similar societal disparities of wealth and development. Furthermore, similar considerations regarding the methodologies used herein to identify CMD are valid for other populations, and should be used in future research when assessing the prevalence of CMDs in distinct population groups, such as men or childless women.
Additionally, the study results show that, regardless of the data analysis strategy, there is a high prevalence of CMD among poor women living in urban areas in Salvador. These findings provide valuable, detailed input to understand the profile of people considered at risk for CMD. This knowledge could be used to develop mental health prevention and promotion programs targeted at this population.
Brazil is a country characterized by poverty and social inequality, both of which are strongly associated with the prevalence of CMD. The findings of the present study point to a need for counseling services focusing on mental health prevention and promotion to meet the demands of a group of women who are more vulnerable to CMD. Primary care providers must be more aware of these women’s vulnerability to CMD so that this population can be properly identified and treated. Finally, the alternative methods of analysis presented herein highlight different possibilities for using the SRQ-20, an important instrument in mental health screening, and can be useful for the planning and implementation of specific actions targeted at a certain population.
Disclosure
The authors report no conflicts of interest.
References
- 1.World Health Organization (WHO). The World Health Report 2001. Mental health: new understanding [Internet]. 2002. [cited 2017 May 04]. http://who.int/whr/2001/en/whr01_en.pdf. [Google Scholar]
- 2.Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- 3.Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:858–66. [PMC free article] [PubMed] [Google Scholar]
- 4.Coutinho ESF, Almeida N, Filho, Mari JJ. Fatores de risco para morbidade psiquiatrica menor: resultados de um estudo transversal em tres areas urbanas no Brasil. Rev Psiquiatr Clin (São Paulo). 1999;26:246–56. [Google Scholar]
- 5.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 6.Patel V, Araya R, de Lima M, Todd C. Women, poverty and common mental disorders in four restructuring societies. Soc Sci Med. 1999;49:1461–71. doi: 10.1016/s0277-9536(99)00208-7. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg D, Huxley P. Common mental disorders: a biosocial model. London: Tavistock; 1992. [Google Scholar]
- 8.Araya R, Wynn R, Leonard R, Lewis G. Psychiatric morbidity in primary health care in Santiago, Chile. Preliminary findings. Br J Psychiatry. 1994;165:530–3. doi: 10.1192/bjp.165.4.530. [DOI] [PubMed] [Google Scholar]
- 9.Hollifield M, Katon W, Spain D, Pule L. Anxiety and depression in a village in Lesotho, Africa: a comparison with the United States. Br J Psychiatry. 1990;156:343–50. doi: 10.1192/bjp.156.3.343. [DOI] [PubMed] [Google Scholar]
- 10.Marl JJ. Psychiatric morbidity in three primary medical care clinics in the city of Sao Paulo. Soc Psychiatry. 1987;22:129–38. doi: 10.1007/BF00583847. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO). A user’s guide to the self-reporting questionnaire (SRQ) [Internet]. 1994. [cited 2017 May 04]. http://apps.who.int/iris/bitstream/10665/61113/1/WHO_MNH_PSF_94.8.pdf. [Google Scholar]
- 12.Mari JJ, Williams P. A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Br J Psychiatry. 1986;148:23–8. doi: 10.1192/bjp.148.1.23. [DOI] [PubMed] [Google Scholar]
- 13.Scholte WF, Verduin F, van Lammeren A, Rutayisire T, Kamperman AM. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Med Res Methodol. 2011;11:116. doi: 10.1186/1471-2288-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164–74. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- 15.Paraventi F, Cogo-moreira H, Paula CS, de Jesus Mari J. Psychometric properties of the self-reporting questionnaire (SRQ-20): measurement invariance across women from Brazilian community settings. Compr Psychiatry. 2015;58:213–20. doi: 10.1016/j.comppsych.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 16.Everitt BS, Dunn G. Log-linear modeling, latent class analysis, or correspondence analysis which method should be used for the analysis of categorical data? in: latent trait and latent class models. In: Langeheine R, Rost J, editors. Latent trait and latent class analysis. New York: Plenum; 1988. pp. 109–27. [Google Scholar]
- 17.van der Heijden PGM, Gilula Z, van der Ark LA. An extended study into the relationship between correspondence analysis and latent class analysis. Soc Methodol. 1999;29:147–86. [Google Scholar]
- 18.Lautsch E, Plichta MM. Configural Frequency Analysis (CFA), Multiple Correspondence Analysis (MCA) and Latent Class Analysis (LCA): an empirical comparison. Psychol Sci. 2003;45:298–323. [Google Scholar]
- 19.Jelihovschi EG, Santana CR. University students performance: an interaction between latent class analysis and correspondence analysis. Rev Bras Biom. 2013;31:310–26. [Google Scholar]
- 20.Santos LM, Amorim LD, Neves DN, Barreto ML. Measuring the level of social support using latent class analysis. Soc Sci Res. 2015;50:139–46. doi: 10.1016/j.ssresearch.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Barreto ML, Cunha SS, Alcântara-Neves N, Carvalho LP, Cruz AA, Stein RT, et al. Risk factors and immunological pathways for asthma and other allergic diseases in children: background and methodology of a longitudinal study in a large urban center in Northeastern Brazil (Salvador-SCAALA study). BMC Pulm Med. 2006;6:15. doi: 10.1186/1471-2466-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Everitt BS, Dunn G. Applied multivariate data analysis. 2nd ed. New York: Wiley; 2010. [Google Scholar]
- 23.Clausen SE. Applied correspondence analysis: an introduction. Thousand Oaks: SAGE; 1998. [Google Scholar]
- 24.Collins LM, Lanza ST. Latent class and latent transition analysis with applications in the social, behavioral, and health sciences. Hoboken: Wiley; 2010. [Google Scholar]
- 25.Muthén LK, Muthén BO. Mplus user's guide. 6th edition. Los Angeles: Muthén; 1998-2010. [Google Scholar]
- 26.Gonçalves DM, Stein AT, Kapczinski F. [Performance of the Self-Reporting Questionnaire as a psychiatric screening questionnaire: a comparative study with Structured Clinical Interview for DSM-IV-TR]. Cad Saude Publica. 2008;24:380–90. doi: 10.1590/s0102-311x2008000200017. [DOI] [PubMed] [Google Scholar]
- 27.Ferster CB. A functional analysis of depression. Am Psychol. 1973;28:857–70. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- 28.Lopes CS, Faerstein E, Chor D. [Stressful life events and common mental disorders: results of the Pro-Saude Study]. Cad Saude Publica. 2003;19:1713–20. doi: 10.1590/s0102-311x2003000600015. [DOI] [PubMed] [Google Scholar]
- 29.Cassell EJ. The nature of suffering and the goals of medicine. N Engl J Med. 1982;306:639–45. doi: 10.1056/NEJM198203183061104. [DOI] [PubMed] [Google Scholar]
- 30.Kaplan BH, Cassel JC, Gore S. Social support and health. Med Care. 1977;15:47–58. doi: 10.1097/00005650-197705001-00006. [DOI] [PubMed] [Google Scholar]
- 31.McCutcheon AL. Correspondence analysis used complementary to latent class analysis in comparative social research. In: Blasius J, Greenacre M, editors. Visualization of categorical data. San Diego: Academic; 1998. pp. 477–88. [Google Scholar]