INTRODUCTION
While experiential education has been an essential component of pharmacy education for many years, access to experiential education for students with disabilities continues to be a challenge and an evolving topic. Learning disabilities (eg, attention deficit hyperactivity disorder (ADHD), dyslexia, dysgraphia, and dyscalculia) affect one in five of all children in the United States.1 In 2008, 15.9% of first-professional degree graduate students reported a specific learning disability.2 Learning disabilities (LD) are typically accommodated in the classroom using various techniques such as longer examination time and private rooms for examinations. However, accommodations in clinical practice environments are not as straightforward. Currently, proctors for licensing examinations and employers provide accommodations for disabilities, but few recommendations exist for the experiential curriculum on best practices for meeting the needs of students with LD.
The Americans with Disabilities Act (ADA) of 1990 afforded protections to people with “physical or mental impairment that substantially limits [sic] one or more major life areas.” Major life activities include “caring for oneself, performing manual tasks, walking, seeing, speaking, breathing, learning, and working.”3 The ADA Amendments Act (ADAAA) in 2008 expanded those protections to include “thinking” and “concentrating,” thereby opening opportunities for students with disabilities related to learning disorders.4 Furthermore, the Accreditation Council for Pharmacy Education (ACPE) states colleges must provide reasonable accommodations to students with disabilities documented by the university disability office.5
Learning disability (LD) refers to disorders that affect the acquisition, organization, retention, comprehension or use of verbal or nonverbal information resulting from impairment of processes related to perceiving, thinking, remembering, or learning. For example, students with LD may have difficulty processing language, phonetics, visual-spatial processing, as well as memory, attention, and executive functions (eg, planning and decision-making).4 ADHD causes an ongoing pattern of inattention and/or hyperactivity that interferes with functioning and/or development. Parent-reported data estimated that 9.4% of children in the US have received an ADHD diagnosis.6 An estimated 60% of patients with ADHD will have symptoms in adulthood.6,7 In graduate or professional programs, it has been estimated that only 0.7% to 3% of students disclose an LD despite the fact that 15.9% of the population report having it.2,8-11 In other words, despite the high numbers of students with LD, few students disclose such disability. Furthermore, a paucity of literature exists describing accommodations for LD during experiential education for health profession programs.
Preceptors and faculty in experiential education administration are positioned to allow for reasonable accommodations for students with LD given adequate time, resources, and knowledge. The goal of this commentary is to provide a background and collective experience on the topic of reasonable accommodations in experiential education specifically focusing on learning disabilities.
What is a Reasonable Accommodation?
The central core of an accommodation is to allow the student to gain access to the content being taught so he/she can achieve the learning outcome(s) for the experience. For example, a student with a hearing impairment might have a sign language interpreter to provide the information. An accommodation in educational settings can be thought of as an adaptation or removal of a barrier to allow full participation in learning. Accommodations should not detract from competencies, but focus on helping students reach learning outcomes.
From a review of the literature, five basic principles emerged to help colleges ensure that reasonable accommodations are provided. First, the accommodation should be based on a reliable diagnosis. Second, accommodations must mitigate factors of the disability that would otherwise cloud the assessment of the student’s technical ability required to meet affected competencies. Third, it should be tailored for each practice-based experience. Fourth, collaboration and communication must occur among preceptors, students, administration, and disability services staff. Lastly, and most critically, privacy must be upheld.8,12 An accommodation would not be considered reasonable if it decreased quality or posed safety issues to patients, substantially changed curricular elements or altered course objectives, or imposed undue financial or administrative burden on the institution.12,13
Common language surrounding technical standards in pharmacy describe skills necessary to commence, progress, and complete the pharmacy curriculum (eg, observation, communication, motor ability, intellectual ability, and behavioral attributes) and are required by accreditation standards.5,14 Skills required for admissions should be connected to skills taught in the curriculum and required for graduation. Doctor of Pharmacy graduates are expected to meet the college’s educational outcomes and minimum required competencies of a practicing pharmacist. Assessment of technical standards and terminal outcomes in individuals with LD should be done under accommodated conditions, if requested, specific to each student and disability. Furthermore, colleges should review their technical standards considering the broadened definition of disability to ensure students have the necessary range of physical and mental skills and abilities to function competently in the experiential setting and the profession.
Accommodating a student with LD in experiential education can be facilitated by minor adjustments to the environments, policies, and procedures. Being proactive by having policies and procedures in place, preparing preceptors for what to expect, and monitoring student learning outcomes are paramount to the success of the student pharmacist with an LD. Designing a curriculum with clearly defined objectives can help the student plan for necessary adjustments.13 In experiential education, reasonable accommodations should be initiated at the student’s request and follow the guiding principles (ie, based on reliable diagnosis, mitigate factors of the disability but not lower the expectation or outcome, tailored for each practice-based experience while ensuring patient safety, communicated with stakeholders with privacy upheld).
Examples of accommodation in medical education highlight institutional procedures to guide accommodation, such as notification of the disability by the learner, discussion between the learner and teacher or director about limitations and modifications, an accommodation request to preceptors and teachers, and implementation of reasonable accommodations. Learners were required to self-assess and document how their disability affected each general competency and how accommodations could mitigate each concern. It also stressed the importance of self-management, confidentiality, and echoed that these modifications should not alter program standards.8,12 Preceptors and experiential education office faculty and staff should be prepared to accommodate for learning disabilities. Preceptor development in this area is warranted and could include information in a preceptor handbook, newsletter, or orientation program specific to the college’s policies and procedures for accommodations for disabilities.
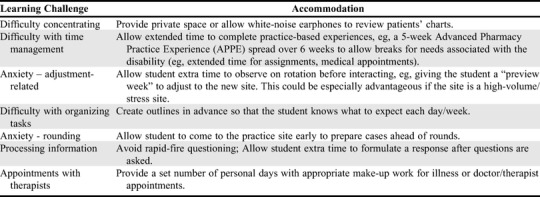
Colleges can use a student’s self-assessment and periodic evaluations by preceptors to determine if the student is meeting competencies and learning objectives. Intermittent monitoring by the preceptor and other health care providers can provide insight into the success or failure of accommodations while maintaining confidentiality. Solutions from experienced faculty may serve to address this issue (Table 1). Employers are required to accommodate workplace environments; therefore, with appropriate accommodations in experiential education, new graduates with learning disabilities will be better prepared to recognize their needs, skills, aptitudes, and energy patterns for their future workplace to better care for the patients they serve.
Table 1.
Examples of Reasonable Accommodations for Specific Learning Disorders
Barriers to Providing Accommodations
Barriers exist to providing reasonable accommodations for students with LD during experiential education. Whether or not students understand the impact of their disability, they may not wish to address it because of perceived detriment to rapport with preceptors or judgment by others. They may also fear stigma, bias, and lack of confidentiality. Alternatively, preceptors may not know how to provide accommodations to students. Preceptors may be able to assist in identifying cognitive or behavioral problems yet may be unwilling to address concerns with students. Similarly, preceptors may wish to circumvent uncomfortable situations and a perceived risk of negative evaluations by avoiding the conversation. This may prevent identification of issues and resolution before subsequent experiential settings and perpetuate the problem.15 These barriers can be compounded by the complex nature of accommodating students with learning disabilities during experiences with team-teaching and patient care.
Preceptor-related challenges described in the literature regard identification and assessment of disabilities as chief limitations to providing accommodations to students in need. Ideally, preceptors should not be the first educator to recognize an LD in a student. Preceptor training often encompasses assessment of knowledge gaps but training likely does not include identification of LD. As a result, preceptors may spend a disproportionate amount of time compensating for issues created by the disability rather than providing accommodations, which allow the student to adapt. As a preventive measure, students should be encouraged to proactively identify and address their disabilities. If unaccommodated, these disabilities can affect the learner, preceptor, institution, and profession.
Given these barriers, the benefits of accommodating likely outweigh the risks. Benefits during experiential education include, but are not limited to, the development of soft skills, assessment of the actual barriers caused by the disability in a controlled environment and knowledge of how to mitigate the challenges associated with their disability in future employment.16
CONCLUSION
There is a compelling legal and moral precedence for providing reasonable accommodations to students with learning disabilities in experiential education. Accommodations during experiential education, although challenging, can be successful through proactive measures such as identification, management, and monitoring. It is critical to consider accommodations to help students with disabilities reach the bar without lowering it while ensuring patient safety. Further study, documentation, and analysis of strategies for accommodating learning disabilities during experiential education in pharmacy curriculum should be conducted. Guidelines for preceptors could be useful in creating novel strategies to accommodate students in a reasonable manner, ensuring all students have access to pharmacy experiential education. Additional training for preceptors is needed to provide knowledge and strategies to facilitate these accommodations.
REFERENCES
- 1.National Center for Learning Disabilities. The State of LD; Executive Summary. https://www.ncld.org/executive-summary. Accessed April 20, 2019.
- 2.US Department of Education. Profile of Students in Graduate and First-professional Education: 2007-2008. https://nces.ed.gov/pubs2011/2011219.pdf. Accessed April 20, 2019.
- 3.U.S. Equal. Employment Opportunity Commission. Titles I and V of the Americans with Disabilities Act of 1990 (ADA). https://www.eeoc.gov/laws/statutes/ada.cfm. Accessed January 8, 2018.
- 4.U.S. Equal Employment Opportunity Commission. ADA Amendments Act of 2008. https://www.eeoc.gov/laws/statutes/adaaa.cfm. Accessed April 2, 2018.
- 5.Accreditation Council for Pharmacy Education. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. (Standards 2016). https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed April 2, 2018.
- 6.Danielson ML, Bitsko RH, Ghandour RM, et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents. J Clin Child Adolesc Psychol. 2016;47(2):199-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC; 2013. [Google Scholar]
- 8.Elliott HW, Arnold EM, Brenes GA, et al. Attention deficit hyperactivity disorder accommodations for psychiatry residents. Acad Psychiatry. 2007;31(4):290-296. [DOI] [PubMed] [Google Scholar]
- 9.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316(21):2214-2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vogel S A, Leonard F, Scales W, Hayeslip P, Hermansen J, Donnels L. The national learning disabilities postsecondary data bank: an overview. J Learn Disabil. 1998;31:234-247. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Education Statistics. An institutional perspective on students with disabilities in postsecondary education. https://nces.ed.gov/surveys/peqis/publications/1999046/. Accessed April 4, 2018.
- 12.Shrewsbury D. Dyslexia in general practice education considerations for recognition and support. Educ Prim Care. 2016;27(4):267-270. [DOI] [PubMed] [Google Scholar]
- 13.Smith WT, Allen WL. Implications of the 2008 Amendments to the Americans With Disabilities Act for Medical Education. Acad Med. 2011;86(6):768-772. [DOI] [PubMed] [Google Scholar]
- 14.Berry TM, Chichester CO, Lundquist LM, et al. Professional technical standards in colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(3):Article 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hicks PJ, Cox SM, Espey EL, et al. To the point: medical education reviews–dealing with student difficulties in the clinical setting. Am J Obstet Gynecol. 2005;193(6):1915-1922. [DOI] [PubMed] [Google Scholar]
- 16.Institute for Community Inclusion. Institute Brief: Making Experiential Education Accessible for Students with Disabilities. https://www.communityinclusion.org/article.php?article_id=130. Accessed January 18, 2018.


