Abstract
Patient: Male, 25
Final Diagnosis: Unilateral giant vulvar lipoma with fat necrosis
Symptoms: Mild discomfort
Medication: —
Clinical Procedure: Surgical excision of the mass
Specialty: Obstetrics and Gynecology
Objective:
Rare disease
Background:
A subcutaneous lipoma is a benign tumor comprised of mature adipocytes. Clinically it presents as a soft, freely moveable, doughy mass that is typically painless and slow growing. Lipomas containing fat necrosis and corresponding palpable nodular elements are rare and suggest an alternative diagnosis. Lipomas in the vulvar region are rare and giant vulvar lipomas with palpable fat necrosis are unreported.
Case Report:
A 25-year-old patient presented with a 4-year history of an enlarging right vulvar mass with multiple small (<1 cm) firm nodules within the tumor. A pelvic MRI (magnetic resonance imaging) did not visualize the nodules but histopathologic examination revealed a benign lipoma containing fat necrosis and discrete areas of calcium deposition.
Conclusions:
Fat necrosis can occur in vulvar lipomas and present with intratumor nodularity. MRI imaging, clinical findings and histology may be discordant.
MeSH Keywords: Fat Necrosis, Lipoma, Vulvar Diseases
Background
A lipoma is a slow-growing, benign tumor comprised of mature adipocytes encased in a thin, fibrous, well-circumscribed capsule. It occurs almost anywhere on the body, but is most commonly found in the upper back, neck, shoulder, abdomen, and proximal portions of the extremities. Lipomas are usually painless, soft, freely-moveable, and of a uniform doughy consistency. Typically, the diagnosis can be made clinically [1,2]. Vulvar region lipomas are unusual and giant vulvar lipomas are extremely rare [3]. Fat necrosis is an uncommon benign condition of unknown etiology and, if present in a lipoma, can change the clinical presentation by adding a component of corresponding palpable nodularity. If a lipoma shows nonadipose solid areas, liposarcoma or other benign conditions should be considered and excluded. Very few cases of fat necrosis areas in a lipoma have been reported [4–6], and no cases of fat necrosis in a vulvar lipoma have been described. We present a case of a female patient with an 18 cm right vulvar lipoma that was characterized by palpable nodularity and continued growth over two years of medical observation. Prominent fat necrosis was noted on clinical examination and confirmed on histologic section at the time of surgical removal.
Case Report
A 25-year-old G3P2002 at 37 weeks gestation presented in labor with no prenatal care and 2 previous cesarean deliveries. She complained of a large right labial, freely-moveable, doughy mass that had been present for over 4 years. Twenty-six months earlier she had been examined for the delivery of her second pregnancy and the mass was 10×4 cm in size. The mass was soft, non-tender to palpation, reducible, and contained multiple small firm nodular areas that were all less than 1 cm. At that time, the mass had been present 2 years, was reducible, and was thought to be a hernia. There was no inguinal lymphadenopathy. The recommendation from the general surgical consult was that the mass did not warrant a combined herniorrhaphy at the time of cesarean delivery, and the patient was instructed to follow-up as an outpatient. She failed to keep her outpatient appointments and was next seen in labor with the current pregnancy. Her family history and social history were noncontributory. Her past medical history was only significant for iron deficiency anemia. Her surgical history was significant for 2 cesarean deliveries. An ultrasound revealed a large non-specific, homogenous, mass-like enlargement with lobular structures consistent with fat deposition in the right labia majora measuring 14.2×7.1×4.8 cm (Figure 1). No significant internal vascularity was noted. On physical examination, the right labial mass was approximately 8×16 cm, soft, mildly tender to palpation, with several small areas of intralipoma nodularity measuring less than 1 cm. (Figure 2). A repeat cesarean delivery was performed, and on postpartum day 2 a pelvic magnetic resonance imaging (MRI) with and without contrast revealed a 14.5×8.8×6.8 cm encapsulated fat-containing mass in the right vulva with no intralesional fluid collection or hematoma (Figure 3). When the images were reevaluated after the histology returned, a T2-weighted cross section MRI image demonstrated nonspecific amorphous changes which were felt to be secondary to manipulation (Figure 4). She had an unremarkable postpartum recovery course, and 6 weeks postpartum she underwent surgical excision of the mass. The entire lipoma was separated from its capsule and delivered through the incision intact. Pathology of the mass demonstrated 18×8.5×3 cm well circumscribed pink-yellow segment of fatty tissue (Figure 5). There were rubbery to fibrous areas within the pink-yellow fatty parenchyma corresponding to the nodules. Histopathologic examination confirmed a lipoma with foci of organizing fat necrosis and dystrophic calcification (Figure 6) which was responsible for the nodularity. She was discharged from short-stay surgery and the examination at the 3-month follow-up visit found complete restoration of normal vulvar anatomy.
Figure 1.
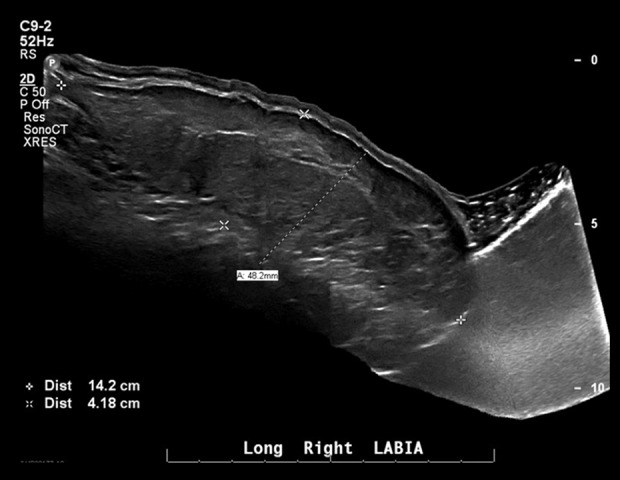
Right vulvar ultrasound shows marked mass-like enlargement. Findings were nonspecific.
Figure 2.

Large protruding right vulvar mass.
Figure 3.
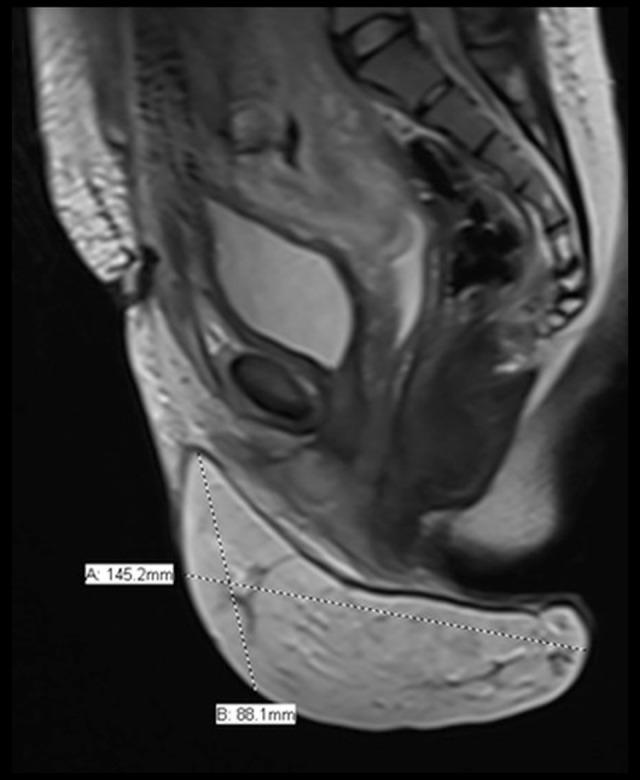
Sagittal slice magnetic resonance imaging after 6.8 cc of gadobutrol contrast shows an encapsulated fat containing mass in the right vulvar area.
Figure 4.
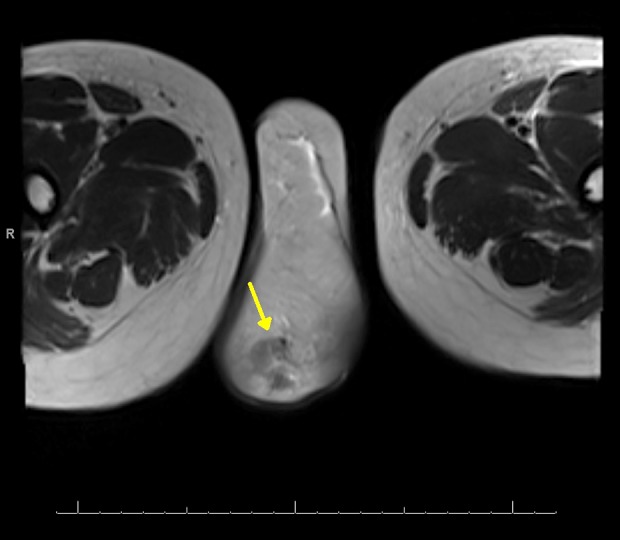
Cross section magnetic resonance image of the vulvar region, T2 weighted. Nonspecific amorphous changes (arrow) which were felt to be secondary to manipulation.
Figure 5.

Entire lipoma removed with capsule intact.
Figure 6.
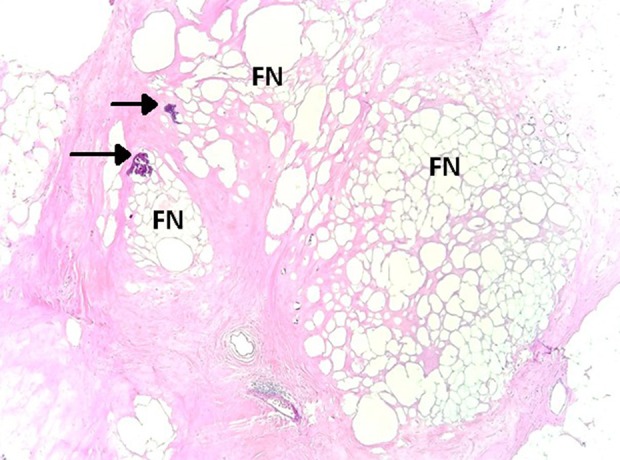
Lipoma. Remote fat necrosis (FN) with fibrosis and dystrophic calcification (arrows). The necrotic adipocytes are devoid of nuclei. Hematoxylin and eosin stain; original magnification 40×.
Discussion
This report is important for 3 reasons. First, this case describes palpable nodularity as a finding in a benign giant vulvar lipoma. Simple uncomplicated lipomas are characteristically uniformly doughy in consistency and well-demarcated. Nodularity within the structure suggests additional pathology which might be benign but is not characteristic. In fact, the first time the mass was examined, the surgical consultant misdiagnosed a right hernia rather than lipoma partly because of the findings at palpation. It appears that not only are vulvar lipomas extremely rare but nodularity from fat necrosis during palpation is unreported. We performed a MEDLINE search of the English language literature via PubMed from January 1, 1946 to present, using the keywords “vulvar”, “vulva”, “lipoma”, and “fat necrosis”. However, we could find no article. This is significant considering the differential diagnosis of mixed density masses of the vulva. Liposarcomas, especially when nodularity is present, inguinal hernia, abscess, Bartholin’s cyst and cystic swellings of Nuck’s canal can present with a similar clinical profile [1–3,7].
In most cases, imaging with ultrasound, MRI or computed tomography (CT) will be performed but in cases of uncertainty, expectant management is not an option like it might be for an uncomplicated subcutaneous lipoma. Nonetheless, this case suggests that even when the tumor consistency is non-homogeneous and nodularity is present, the mass might still represent a lipoma rather than a more serious or complicated condition. If there is any doubt, however, a surgical approach is both diagnostic and therapeutic. Our case reflects a simple clinical misdiagnosis on the first examination. Even though subcutaneous liposarcomas are typically well-differentiated, a delay of 2 years could have been disastrous if a cancer were present. The second important element to this case was that this was one of the largest lipomas of the vulva reported and it was followed by a medical team from 10 cm to 18 cm over an approximately 2-year time period. A 1999 report [8] documented a 17 cm right vulvar lipoma in a 52-year-old and noted that at the time fewer than 70 cases of vulvar lipomas had been published. In 2014 [9], a report of a 16 cm vulvar lipoma that was present for 4 years was published. The authors concluded that vulvar lipomas that arise late in life might be due to chronic intermittent mechanical irritation while those seen early on might be congenital and are usually on the right side. They likewise emphasized that vulvar lipomas should be differentiated from the much less common liposarcomas. In 2018, Reda and Gomaa [10] described a vulvar lipoma that was present for over 4 years and was causing discomfort when walking. They noted that surgical removal with complete excision of the capsule was the treatment of choice for lipomas to prevent recurrence. Both previously reported cases had long-standing, large vulvar lipomas. Consequently, if fat necrosis is related to the tumor size or duration in a vulvar region then either one of the previous cases could have demonstrated clinical, imaging, or histologic findings consistent with the necrosis. In all likelihood, the fat necrosis seen in our case was related to a combination of variables, including speed of lipoma growth, which could encourage infarction, and trauma which could result in scarring [11,12]. Nonetheless, even though the incidence of fat necrosis in lipomas is low [4–6] this case illustrates that a nodular consistency within a soft doughy vulvar mass might be a lipoma but should be considered an unexpected finding. A literature of review of fat necrosis [13] in 2000 suggested that the lower extremity is the most commonly affected site for fat necrosis, and none were seen in the vulvar region. Approximately 25% were preceded by trauma. The third important element of our case was the apparent discordance between imaging, clinical, and histologic findings. The nodules were palpable and easily seen on microscopic section as fat necrosis and dystrophic tissue calcification. However, the MRI and ultrasound were of no help in providing positive information. Ultrasound clearly is not an ideal method to differentiate small, dense, solid, uniform subcutaneous lesions unless acoustic shadows or tissue density differences can be detected. MRI on the other hand should be a reliable method depending on the characteristics of the mass. Recently, however, the reliability of MRI to detect and differentiate fat necrosis has been challenged and the MRI appearance of fat necrosis is more varied than previously thought [14]. Generally, T2-weighted image signal intensity higher than that of fat indicates myxoid degeneration, necrosis, or malignancy [15], but our series only showed manipulation artifact which could have represented movement. Our lack of positive reproducible findings was notable, but the MRI provided helpful information, nonetheless. There was no evidence of extension outside the capsule and the tumor was clearly an isolated, encapsulated lesion. Thus, appearance fat necrosis on imaging in lipomas seems to be wide and difficult to distinguish from malignant changes [16], further emphasizing the importance of surgical removal. In summary, a large vulvar lipoma with palpable nodularity for 2 years was managed expectantly for over 4 years. In the process, the patient had 2 term cesarean deliveries without difficulties in conception or gestation. Neither ultrasound nor MRI defined the true nature of the palpable intralipoma nodules. Complete surgical removal of the mass and histopathologic evaluation confirmed the nodules were related to fat necrosis and calcification.
Conclusions
The purpose of this case was to show that when nonfatty components within a subcutaneous vulvar lipomatous tumor are discovered, they do not necessarily indicate a malignancy or hernia. In addition, the measured growth rate of large vulvar lipomas can be rapid. Follow-up imaging can be misinterpreted, and the final diagnosis requires a surgical specimen.
Acknowledgments
Michael Gurian, MD, Radiologist.
Footnotes
Conflict of interest
None.
References:
- 1.Odoi AT, Owusu-Bempah A, Dassah ET, et al. Vulvar lipoma: Is it so rare? Ghana Med J. 2011;45:125–27. [PMC free article] [PubMed] [Google Scholar]
- 2.Jung HL, Seung MC. Large vulvar lipoma in an adolescent: A case report. J Korean Med Sci. 2008;23:744–46. doi: 10.3346/jkms.2008.23.4.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jayi S, Laadioui M, El Fatemi H, et al. Vulvar lipoma: A case report. J Med Case Rep. 2014;8:203. doi: 10.1186/1752-1947-8-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kransdorf MJ, Bancroft LW, Peterson JJ, et al. Imaging of fatty tumors: Distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224:99–104. doi: 10.1148/radiol.2241011113. [DOI] [PubMed] [Google Scholar]
- 5.Chan LP, Gee R, Keogh C, Munk PL. Imaging features of fat necrosis. Am J Roentgenol. 2003;181:955–59. doi: 10.2214/ajr.181.4.1810955. [DOI] [PubMed] [Google Scholar]
- 6.Gaskin CM, Helms CA. Lipomas, lipoma variants and well-differentiated liposarcomas (atypical lipomas): Results of MRI evaluations of 126 consecutive fatty masses. Am J Roentgenol. 2004;182:733–39. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 7.Jourjon R, Dohan A, Brouland JP, et al. Angiolipoma of the labia majora: MR imaging findings with histopathological correlation. Clin Imaging. 2013;37:965–68. doi: 10.1016/j.clinimag.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Kehagias DT, Smyrniotis VE, Karvounis EE, et al. Large lipoma of the vulva. Eur J Obstet Gynecol Reprod Biol. 1999;84:5–6. doi: 10.1016/s0301-2115(98)00247-4. [DOI] [PubMed] [Google Scholar]
- 9.Jóźwik M, Kołodziejczak M, Klonowska-Dziatkiewicz E, Jóźwik M. Giant vulvar lipoma in an adolescent girl: A case study and literature review. J Pediatr Adolesc Gynecol. 2014;27(5):e117–19. doi: 10.1016/j.jpag.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Reda A, Gomaa I. Vulvar lipoma: A case report. Rev Bras Ginecol Obstet. 2018;40:647–49. doi: 10.1055/s-0038-1670642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sahl WJ., Jr Mobile encapsulated lipomas. Formerly called encapsulated angiolipomas. Arch Dermatol. 1978;114:1684–86. [PubMed] [Google Scholar]
- 12.Hurt MA, Santa Cruz DJ. Nodular-cystic fat necrosis. A reevaluation of the so-called mobile encapsulated lipoma. J Am Acad Dermatol. 1989;21:493–98. [PubMed] [Google Scholar]
- 13.Kiryu H, Rikihisa W, Furue M. Encapsulated fat necrosis – a clinicopathological study of 8 cases and a literature review. J Cutan Pathol. 2000;27:19–23. doi: 10.1034/j.1600-0560.2000.027001019.x. [DOI] [PubMed] [Google Scholar]
- 14.Chan LP, Gee R, Keogh C, Munk PL. Imaging features of fat necrosis. Am J Roentgenol. 2003;181:955–59. doi: 10.2214/ajr.181.4.1810955. [DOI] [PubMed] [Google Scholar]
- 15.Gelineck J, Keller J, Myhre-Jensen O, et al. Evaluation of lipomatous soft tissue tumors by MR imaging. Acta Radiol. 1994;35:367–70. [PubMed] [Google Scholar]
- 16.Soriano AL, Tomasello A, Luburich P, Noel A. Fat necrosis in a chest wall lipoma. Am J Roentgenol. 2004;183:866–66. doi: 10.2214/ajr.183.3.1830866. [DOI] [PubMed] [Google Scholar]


