Abstract
Context:
Health-care workers experience psychosocial stress in their workplace. Available statistics are at variance, and hence, the need to know the overall prevalence of psychosocial stress among Nigerian health-care workers and associated risk factors.
Aims:
The aim of this study was to determine the prevalence of psychosocial stress and its risk factors among health-care workers in Nigeria through meta-analysis.
Materials and Methods:
PubMed, CINAHL, and Google Scholar databases were searched for articles. Search terms include “psychosocial stress,” “occupational health,” and “Nigerian health-care worker.” Articles were included if they used validated psychosocial stress assessment instruments. Of the 17 articles with data on psychosocial stress prevalence, eight met all inclusion criteria. Each article independently reviewed by the authors and relevant data abstracted. Statistical analysis was done using MedCalc version 18.10.
Results:
Overall, the prevalence of psychosocial stress was 61.97% (95% confidence interval [CI]: 41.013–80.823) based on analyzed eight articles with the sample size of 1763. Work overload rate at 67.72% (95% CI: 33.24–93.76) was the most prevalent psychosocial stress risk factor. Other risk factors were poor communication and staff attitude and lack of resources and equipment at 50.37% (95% CI: 13.35–87.16) and 62.4% (95% CI: 7.70–99.9), respectively. Headache, with neck and back pain, was the most prevalent psychosocial stress-related health outcome at 73.26% (95% CI: 66.14–79.82).
Conclusion:
Prevalence of psychosocial stress is high among health-care workers in Nigeria, necessitating preventive measures
Keywords: Health-care workers, meta-analysis, Nigeria, psychosocial stress prevalence
INTRODUCTION
Psychosocial stress causes a significant loss of job productivity within healthcare. More specifically, psychosocial stress can be defined by the response people may have when presented with work demands and work pressures that are not matched to their knowledge and abilities and which challenge their ability to cope.1 Health-care workers are a neglected group, often presumed to be immune to occupational hazards, hence not adequately protected.1
Psychosocial stress is rapidly becoming an occupational health epidemic.2 The need to deliver quality health-care services consistently is putting an unprecedented strain on the well-being of health-care workers and their productivity1,8 is negatively affecting organizational health indices. There is a positive association between work-related illness and exposure to psychosocial stress.4,9 Among the European Union member nations, psychosocial stress, affected 22% of workers from 2000 to 2005, contributing to 60% of all lost working days, with cost amounting to 4% of gross national product lost.4,10,11
Nigeria, with a population of over 180 million, has one of the largest stocks of human resources for health in Africa, with 1.95/1000 population.12 There are 3827 doctors per 10,000 populations, and 14,524 nurses and midwives per 10,000 population.13
Although there have been few studies published on the prevalence of psychosocial stress among health-care workers in Nigeria, the statistics have been far apart with wide margins. Hence, the need to know what the general prevalence of psychosocial stress among health-care workers in Nigeria is to make informed preventive and therapeutic policy decisions. There are currently no pooled data available assessing psychosocial stress prevalence and its risk factors among health-care workers in Nigeria. Hence, this meta-analysis is conducted.
The aim of this systematic review and meta-analysis is, therefore, to determine and to provide health-care organizations the general quantitative estimates of psychosocial stress prevalence and its risk factors among health-care workers in Nigeria, by summarizing available studies that have used validated and standardized assessment instruments.
MATERIALS AND METHODS
A meta-analysis approach was chosen, deemed appropriate for the study aim and objective.
Literature searches were conducted using appropriate keywords: psychosocial stress, risk assessment, health-care workers, and psychosocial stress hazards for articles published in the English from January 2000 to September 2018. Searches were in Google Scholar, PubMed, MEDLINE, International Journal of Public Health, International Journal of Community Medicine and Public Health, Journal of Occupational Health, Journal of Occupational Medicine and Toxicology, and Nigerian Medical Journal. Supplementary information was also used from the WHO, ILO, ICOH Conference proceedings, NIOSH, CDC, and Nigerian Federal Ministry of Health.
A proper protocol of the statement for reporting systemic reviews (four-step PRISMA) was adopted, as shown in Figure 1.14 Psychosocial stress prevalence articles that used validated and standardized psychosocial stress assessment instruments and evaluated psychosocial stress-related health outcomes and risk factors were included in this study analysis.
Figure 1.
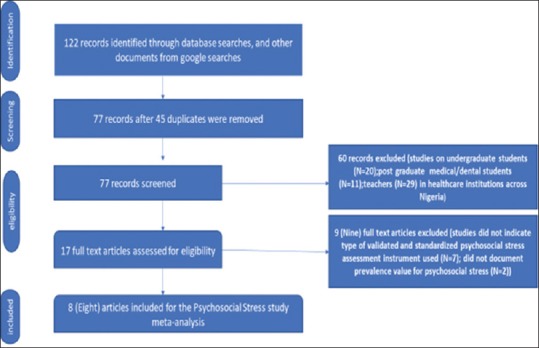
PRISMA literature search flow chart for psychosocial stress prevalence meta-analysis
The corresponding author initially, independently reviewed and screened the articles based on title and abstract for relevance. Subsequently, the full text assessed in detail, for eligibility using the inclusion criteria. Discrepancies were resolved and eligible studies confirmed independently by the corresponding author.
The first search resulted in 122 references, of which 45 duplicates were removed. The remaining 77 searches further reviewed on their titles and abstracts, from which 17 articles were deemed relevant. The remaining 60 articles were studies based on undergraduate medical students (n = 20), postgraduate medical and dental students (n = 11), and teachers in Nigerian medical schools (n = 29). Of the 17 articles, nine full-text records eliminated due to the lack of documentation on the validated and standardized psychosocial stress assessment instruments used (n = 7) and failure to document psychosocial stress prevalence value (n = 2). Only eight studies that met inclusion criteria are used [Figure 1].
Variables extracted from each article include authors' name, year of publication, study location, design and setting, sample size, psychosocial stress risk factors, and psychosocial stress-related health outcomes; confounders measured, validated, and standardized psychosocial stress assessment instruments used. Opinion articles, abstracts, book chapters, and review articles were excluded from the study.
All eight articles were carried out in Nigeria between 2000 and 2018, with a combined total study population of 1763 health-care workers [Table 1]. All the studies were cross sectional, involving all cadres of the health-care industry.
Table 1.
Psychosocial stress prevalence rates, risk factors, sample sizes, settings and study designs of eight articles for meta-analysis
| Author(s), year of publication, country of study | Setting | Study design | Study sample size (n) | Psychosocial stress prevalence rates (%) | Risk factor(s) reported for psychosocial stress |
|---|---|---|---|---|---|
| Adamu & Abdullahi, 2017 Nigeria | Federal Medical Center, Bida | Cross-sectional | 200 | 46 | Work overload, Job ambiguity |
| Mojoyinola JK, 2008 Nigeria | Two hospitals in Ibadan (State Hospital, and University College Hospital-UCH) | Cross-sectional | 153 | 55.5 | Work overload |
| Owolabi et al. 2012 Nigeria | Baptist (Mission) Hospital, Oyo | Cross-sectional | 351 | 26.2 | Low job control (52%), High job demand (49.7%) |
| Etim et al. 2015 Nigeria | One General Hospital, One Private Hospital In Ugep. | Cross-sectional | 198 | 92.9 | Work overload and Emergency situations (24.2%), adhoc duties (3.5%), lack of equipment (30.8%), staff attitude (29.8%) |
| Obasohan et al. 2014 Nigeria | Three General hospitals in Lagos | Cross-sectional | 290 | 86/2 | Work overload and job discrepancies (r2=0.305; F=23.291, P>.05) |
| Adeolu et al. 2016 Nigeria | University College Hospital (UCH) Ibadan | Cross-sectional | 253 | 31.6 | Work overload |
| Ladan et al. 2014 Nigeria | Ahmadu Bello University Teaching Hospital (ABUTH) Zaria | Cross-sectional | 107 | 90.7 | Work overload (87.5%), infrequent rest (64.4%), poor communication (71.2%), lack of support from workers (55.8%) |
| Onowhakpor A, 2018 Nigeria | University of Benin Teaching Hospital, Benin City | Cross-sectional | 107 | 50.8 | Work overload (94.3%), sleep deprivation (89.5%), inadequate resources (89.1%) |
All eight articles used validated psychosocial stress assessment instruments [Table 2] and observed various risk factors for psychosocial stress [Table 1]. Only Etim et al., Owolabi et al., Ladan et al., and Onowhakpor documented the prevalence rates for observed risk factors for psychosocial stress in percentages. All the studies elicited various psychosocial stress-related health outcomes [Table 2] ranging from emotional symptoms (anger and irritability), mental symptoms (forgetfulness and disorganized thinking), personal behavioral symptoms (absenteeism and low motivation), and physical symptoms (high blood pressure, headaches, and muscle cramps). However, only articles by Ladan et al. and Etim et al. expressed psychosocial stress-related health outcomes in percentages.
Table 2.
Confounders, validated psychosocial stress assessment instruments and health outcomes from eight articles for psychosocial stress prevalence study
| Author(s), year of publication, country of study | Confounders measured | Psychosocial stress validated assessment instrument | Medical evaluation of Psychosocial stress outcome | Psychosocial stress health outcome(s) |
|---|---|---|---|---|
| Adamu & Abdullahi, 2017 Nigeria | Age, gender, educational level, marital status, years of employment, safety practices | Job Content Questionnaire | Direct interview | Mental, behavioural and physical symptoms |
| Mojoyinola JK, 2008 Nigeria | Age, years of experience | Stress Assessment Questionnaire for Hospital Nurses (SAQFHN) | Direct interview | Headaches, back and neck pains, hypertension, Mental health symptoms |
| Owolabi et al. 2012 Nigeria | Age, gender, marital status, religion, Education, CVD status, physical exercise, BMI, lifestyle. | Job Demand Control Questionnaire | Blood pressure (mmHg) measurements, BMI assessments | Hypertension, Overall job strain was 26.2% |
| Etim et al. 2015 Nigeria | Age, gender, marital status, religion | Stress Assessment Questionnaire | Key Information Interview (KII), Hospital Records, Direct Field Observations | headache (76.3%), poor concentration (11.6%), loss of work interest (10.1%) |
| Obasohan et al. 2014 Nigeria | Age, gender, years of experience | Job Stress and Workers Productivity (JSWP) | Direct interview | Headaches, loss of work interest, poor sleep |
| Adeolu et al. 2016 Nigeria | Age, gender, marital status, ethnicity, religion, department, experience | General Health Questionnaire (GHQ-12)General Practitioners Job Stress Inventory, Job Satisfaction Scale | Direct interview | Loss of work interest, Mental health symptoms (χ2-16.980, P<0.001) |
| Ladan et al. 2014 Nigeria | Age, gender, marital status, literacy, profession, years in service, work hours, environment | Job Demand Control Questionnaire | Key Information Interview (KII), Blood pressure (mmHg) measurements | Headaches (69.2%), muscle cramps (59.6%), hypertension (51%), Mental health symptoms |
| Onowhakpor A, 2018 Nigeria | Age, years of experience | General Health Questionnaire (GJQ-12) | Health status via Key Information Interview (KII) | Headaches and Mental health symptoms |
All the studies controlled for at least one confounder [Table 2] either sociodemographic (gender, age, ethnicity, marital status, children, and religion); biological factors (hypertension and diabetes); work organization factors (work and shift schedule); lifestyle habits (alcohol and smoking consumption, physical activity) and/or socioeconomic (professional cadre and years of work experience).
Adamu and Abdullahi, while examining occupational hazards among health-care workers in a tertiary hospital in Bida, Niger State, found the overall prevalence of psychosocial stress at 46% (95% confidence interval [CI]: 38.948–53.172) using the Job Content Questionnaire Instrument. The study was carried out in 2014 among 200 health-care workers using a cross-sectional study design. Non–availability of equipment was the most common risk factor for psychosocial stress in this study [Table 1]. Responder bias was a major limitation identified by the authors of this study.15
In a study aimed at assessing the effect of psychosocial stress on the physical, mental, personal health, and work behaviors of 153 nurses in two tertiary hospitals in Ibadan, Mojoyinola confirmed the prevalence of psychosocial stress at 55.5% (95% CI: 47.313–63.579). Stress Assessment Questionnaire for Hospital Nurses instrument (modified from Stress Less, Inc.(2005) and job assessment scale) used in this study that confirmed the significant negative effect of psychosocial stress on physical and mental health among health-care workers (F = 2.376; df = 10/153; P >.05). Mojoyinola also confirmed that work overload, poor staffing, frustration, and lack of promotion were among the risk factors for psychosocial stress among health-care workers.16
Owolabi et al. in a cross-sectional study on 324 mission hospital health-care workers in Oyo State explored the association between psychosocial stress and hypertension health outcome. The job demand – Control Questionnaire Instrument was used to assess psychosocial stress, with BMI and blood pressure measurements to evaluate health outcomes. The combined prevalence rate of psychosocial stress was 26.2% (95% CI: 21.685–31.143). Psychosocial stress was found to be statistically significantly associated with a rise in hypertension prevalence.17
Using the Stress Assessment Questionnaire Instrument, Etim et al. in a study carried out among 198 health-care workers in two hospitals in Ugep, Cross River State, observed the prevalence of psychosocial stress at 92.9% (95% CI: 88.421–96.081). In this cross-sectional study, the risk factors for psychosocial stress were work overload (3.9%), poor managerial support, poor staff attitude (29.8%), poor work environment, and lack of equipment (30.8%). Headache/migraine ranked highest among psychosocial stress-related health outcomes in the study at 76.3%. Other psychosocial stress-related health outcomes included loss of work interest (10.1%) and poor concentration (11.6%).18
Obasohan and Ayodele, while assessing psychosocial stress-related symptoms, among 290 doctors in three hospitals in Lagos established the prevalence of psychosocial stress at 86.2% (95% CI: 81.695–89.960). Using the Job Stress and Workers productivity instrument, Obasohan and Ayodele confirmed a high psychosocial stress prevalence, with job discrimination as a major psychosocial stress risk factor at 30.5% (R2 = 0.305; F = 23.291; P >.05).19
In a cross-sectional study to assess the prevalence of psychosocial stress among 253 doctors at the University College Hospital, Ibadan, Adeolu et al. using the General Health Questionnaire (GHQ-12) instrument, established the psychosocial stress prevalence at 31.6% (95% CI: 25.939–37.739). The General practitioners' job stress inventory and job satisfaction scale were used to evaluate risk factors and health outcomes for psychosocial stress. Adeolu et al. established job dissatisfaction (odds ratio [OR] = 2.33; CI = 1.08–4.04) and poor mental health (OR = 3.82; CI = 1.42–9.95) among the health-care workers were the risk factors for psychosocial stress.20
In another cross-sectional study to assess the prevalence of psychosocial stress among 107 health-care workers at the Ahmadu Bello University Teaching Hospital, Zaria, Ladan et al. observed the prevalence of psychosocial stress at 90.65% (95% CI: 83.484–95.427). The job demand – Control Questionnaire Instrument was used in this study, with work overload and long work hours (75%) were the most important predictor/risk factors for psychosocial stress among health-care workers. Psychosocial stress-related health outcomes recorded were hypertension (51%), muscle cramps (59.6%), discouraging thinking (65.4%), frustration (67.5%), headache (69.2%), forgetfulness (70.2%), and anger (76.9%).21
Onowhakpor, in a study to assess the prevalence, sources, and coping mechanisms of psychosocial stress among 238 doctors in a hospital in Benin City, Edo State, confirmed the prevalence of psychosocial stress at 50.84% (95% CI: 44.303–57.356). The GHQ-12 instrument applied in this study, confirmed inadequate resources (85.1%), sleep deprivation (89.5%), and work overload (94.3%) were the risk factors for psychosocial stress.22
Statistical analysis
MedCalc online statistical software 18.1 (MedCalc Software bvba, Acacialaan, Ostend, Belgium) was used to analyze data, and a pooled prevalence rate for psychosocial stress was calculated. Inverse variance method was used to allocate weight to each article, with the pooled estimates and CI assessed assuming a random-effects model. L2 index was used to measure the statistical heterogeneity of the data. A similar analysis performed for psychosocial stress risk factors and psychosocial stress-related health outcomes documented in percentages.
Ethical consideration
Based on the use of already published secondary data and the meta-analysis nature, ethical approval was not required.
RESULTS
A total of eight articles published between 2000 and 2018 were assessed using the four-step protocol of PRISMA statement, with a total sample size of reviewed articles at 1763 health-care workers, averaging 220 people/study.
Ladan et al. and Etim et al. recorded the highest prevalence for psychosocial stress in their studies with 90.65% (95% CI: 83.484–95.427) and 92.93% (95% CI: 88.42–96.081), respectively, whereas reviews by Owolabi et al. at 26.21% (95% CI: 21.685–31.143) and Adeolu et al. at 31.62% (95% CI: 25.939–37.739) recorded the lowest prevalence rates. Details of all individual article prevalence rates for psychosocial stress are presented in Table 3.
Table 3.
Psychosocial stress prevalence meta-analysis of all articles
| S/N | Study | Sample size | Proportion (%) | 95% CI | Weight (%) |
|
|---|---|---|---|---|---|---|
| Fixed | Random | |||||
| 1 | Adamu and Abdullahi 2017 | 200 | 46.000 | 38.948 to 53.172 | 11.18 | 12.50 |
| 2 | Mojoyinola JK, 2008 | 153 | 55.556 | 47.313 to 63.579 | 8.57 | 12.45 |
| 3 | Owolabi et al. 2012 | 351 | 26.211 | 21.685 to 31.143 | 19.58 | 12.57 |
| 4 | Etim et al. 2015 | 198 | 92.929 | 88.421 to 96.081 | 11.07 | 12.50 |
| 5 | Obasohan et al. 2014 | 290 | 86.207 | 81.695 to 89.960 | 16.18 | 12.55 |
| 6 | Adeolu et al. 2016 | 253 | 31.621 | 25.939 to 37.739 | 14.13 | 12.54 |
| 7 | Ladan et al. 2014 | 107 | 90.654 | 83.484 to 95.427 | 6,01 | 12.36 |
| 8 | Onowhakpor A, 2018 | 238 | 50.840 | 44.303 to 57.356 | 13.29 | 12.53 |
| Total (fixed effects) | 1790 | 57.629 | 55.306 to 59.926 | 100.00 | 100.00 | |
| Total (random effects) | 1790 | 61.971 | 41.013 to 80.823 | 100.00 | 100.00 | |
In this meta-analysis, the pooled prevalence rate of psychosocial stress among health-care workers in Nigeria with a sample size of 1763 was 61.97% (95% CI: 41.01–80.82) [Table 3] using the random-effects model, and heterogeneity of the effect measures was observed (Cochran's Q = 575.42; DF = 7; P < 0.0001; l2 98.8%) [Table 4]. Findings indicate a statistically significant heterogeneity. Differences observed in the various studies presumed due to differences in study sample sizes and prevalence rates for psychosocial stress of the individual studies, as shown in Figures 2 and 3.
Table 4.
Cochran’s Q test for heterogeneity for all psychosocial stress articles
| Test for heterogeneity | |
|---|---|
| Q | 575.4200 |
| DF | 7 |
| Significance level | P<0.0001 |
| l2 (inconsistency) | 98.78% |
| 95% Cl for l2 | 98.38 to 99.09 |
Figure 2.
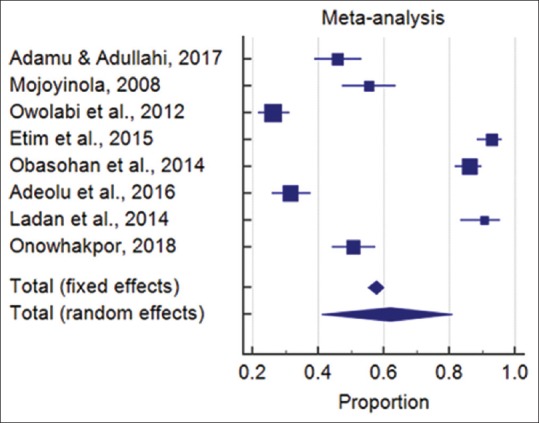
Psychosocial stress prevalence (rectangles), 95% confidence interval (horizontal lines), and pooled prevalence rate (diamonds) for all articles
Figure 3.
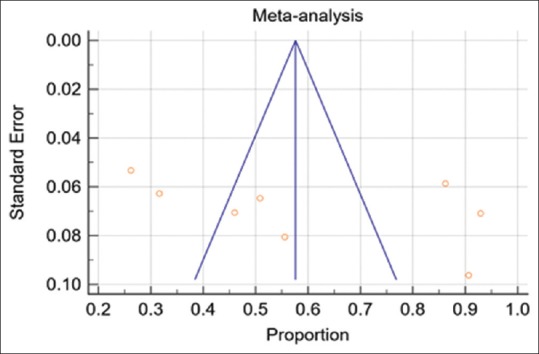
Psychosocial stress prevalence funnel plot of effect estimates against standard error. Central vertical line is pooled effect estimate
As shown in Table 5, the most prevalent psychosocial stress risk factors were poor communication and attitude with a pooled prevalence rate at 50.37% (95% CI: 13.35–87.16), lack of resources and equipment with pooled prevalence rate of 62.4% (95% CI: 7.70–99.91), and work overload with a pooled prevalence rate of 67.72% (95% CI: 33.25–93.76). Health outcome due to psychosocial stress analyzed was headaches, neck and back pain, with a pooled prevalence rate of 73.25% (95% CI: 66.14–79.82) [Table 5].
Table 5.
Psychosocial stress risk factors and related health outcomes prevalence, 95% confidence interval, and heterogeneity test
| Category | Random effects model |
Heterogeneity |
||||
|---|---|---|---|---|---|---|
| Sample size | Pooled prevalence rate (%) | 95% CI | l2 (%) | 95% CI | Cochran’s Q | |
| Psychosocial stress risk factors | ||||||
| Work overload | 867 | 67.40 | 33.25-93.76 | 99.07 | 98.62-99.37 | 322.20 |
| Lack of resources and equipment | 436 | 62.37 | 7.70-99.91 | 99.44 | 99.02-99.68 | 179.22 |
| Poor communication and attitude | 305 | 50.37 | 13.35-87.16 | 98.01 | 95.34-99.15 | 50.25 |
| Psychosocial stress-related health outcome | ||||||
| Headaches, neck and back pain | 305 | 93.26 | 66,14-79,82 | 44.55 | 0.00-0.00 | 1.80 |
CI – Confidence interval
DISCUSSION
In this meta-analysis, the general prevalence rate of psychosocial stress among health-care workers in Nigeria was estimated at 61.97% (CI 95%: 41.013–80.823) using the random-effects model [Table 3]. Hence, the result indicates a high prevalence rate for psychosocial stress among health-care workers in Nigeria, which is very alarming. These values compared to studies carried out in other developing countries using varying validated and standardized assessment instrument were higher. Nwankwo et al.23 observed a prevalence rate of psychosocial stress among Rwandan health-care workers at 15.3%, whereas Alhassan and Poku found that Ghanaian health-care workers had a psychosocial stress prevalence rate of 17%.24 Ndejjo et al. established the psychosocial stress prevalence rate for Ugandan health-care workers at 21.5%,25 and Haq et al. for Pakistan health-care workers found the psychosocial stress prevalence rate at 26%,26 which are not consistent with our findings. However, Fernandes and Marziale, while examining the occupational risks and illnesses among health-care workers in Brazil, estimated the psychosocial stress prevalence rate at 71.1%,27 which is in keeping with our findings. The differences in psychosocial stress levels could be due to health-care management systems and organizational structures of hospitals obtained in the different countries highlighted. Even though there are different levels of psychosocial stress prevalence rates among health-care workers from various studies, the overall prevalence rate of psychosocial stress among Nigerian health-care workers is severely high and a cause for concern.
Although not all the articles stated percentage prevalence rates for most of the psychosocial stress risk factors and health outcomes identified for direct calculation, this analysis elicited valuable information. Regarding psychosocial stress risk factors compiled for this analysis, work overload was the most prevalent, with an overall prevalence rate at 67.72% (95% CI: 33.25–93.64), which is consistent with findings from other studies by Haq et al.,26 Okeafor and Alamina,28 and Alhassan and Poku.24 Other risk factors for psychosocial stress estimated were poor communication and staff attitude (50.37%) and lack of resource and equipment (62.4%).
Among psychosocial stress-related health outcomes compiled, the only headache, with neck and back pain had percentage rate available for statistical analysis, with an overall prevalence rate estimated at 73.26%, consistent with previous studies.18,21 All the studies used various forms of psychosocial stress assessment instruments.
Strengths and limitations
Considering the lack of current meta-analysis study in any database for comparison, estimating the overall prevalence rate of psychosocial stress among health-care workers in Nigeria is the unique feature and benefit of this present study. In addition, adhering to a rigorous methodology and PRISMA protocol, with inclusion/exclusion criteria, this study's pooled prevalence estimates offer the most current picture of psychosocial stress prevalence, and hence, useful as a baseline estimate in any evidence-based research. Validity and quality enhanced by doing a meta-analysis of peer-reviewed articles, overcoming small sample size and statistical power constraints, thereby increasing statistical significance.
Limitations emanated from the inability to critically review methodological quality and cross-sectional design used in the compiled articles. This study was unable to assess the full text of some articles for more statistical power and establish a statistical association between psychosocial stress prevalence and age, gender, and cadres of the health-care workforce. Despite adjustments for pooled estimates and CIs for between article variances, heterogeneity itself can pose a limitation. Many articles did not include prevalence percentage values for most psychosocial stress risk factors and health outcomes, hence could not be included in direct statistical calculations.
Interpretation and implication
The results of this meta-analysis suggest that psychosocial stress is a common feature with alarming rates among health-care workers in Nigeria. The psychosocial stress environment influences the overall well-being of health-care workers and organizational health indices such as reduced productivity and sickness absence. The actual use of high methodological validated and standardized assessment instruments is required to assess psychosocial stress prevalence and its risk factors to yield more consistent results.
Future research directions
The study findings necessitate advocacy from all stakeholders to identify and implement effective measures to reduce psychosocial stress among Nigerian health-care workers. More prevalence meta-analysis is at this moment necessary to further provide health-care organizations and occupational health practitioners with evidence-based baseline prevalence estimates.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Occupational Health: Health Workers. World Health Organization. 2018. [Last assessed on 2019 Mar 10]. Available from: http://www.who.int/occupational_health/topics/hcworkers/en/
- 2.World Health Organization. Protecting Workers’ Health Series, No. 3. Geneva: World Health Organization; 2003. Work Organization and Stress. [Google Scholar]
- 3.Fingerhut M, Nelson DI, Driscoll T, Concha-Barrientos M, Steenland K, Punnett L, et al. The contribution of occupational risks to the global burden of disease: Summary and next steps. Med Lav. 2006;97:313–21. [PubMed] [Google Scholar]
- 4.EU-OSHA. OSH in Figures: Stress at Work – Facts and Figures. Luxembourg: Office for Official Publications of the European Communities. European Commission. Interpretative Document of the Implementation of Council Directive 89/391/EEC in Relation to Mental Health in the Workplace. Employment, Social Affairs and Inclusion. EU-OSHA. 2009 [Google Scholar]
- 5.Psychosocial Factors at Work: Recognition and Control. Vol. 56. Geneva: International Labour Office; 1986. International Labour Office. [Google Scholar]
- 6.Karasek RA, Theorell T. Healthy Work, Stress, Productivity and the Reconstruction of Working Life. New York: Basic Books; 1990. [Google Scholar]
- 7.Siegrist J. Job control and reward: Effects on well being. In: Cartwright S, Cooper CL, editors. The Oxford Handbook of Organizational Well-Being. Oxford: Oxford University Press; 2009. [Google Scholar]
- 8.Siegrist J, Rödel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32:473–81. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- 9.Fischer FM, Oliveira DC, Nagai R, Teixeira LR, Lombardi Júnior M, Latorre Mdo R, et al. Job control, job demands, social support at work and health among adolescent workers. Rev Saude Publica. 2005;39:245–53. doi: 10.1590/s0034-89102005000200016. [DOI] [PubMed] [Google Scholar]
- 10.EU-OSHA. How to Tackle Psychosocial Issues and Reduce Work-Related Stress. Luxembourg: Office for Official Publications of the European Communities; 2002. [Google Scholar]
- 11.Levi L. Working on Stress, Magazine of the European Agency of Safety and Health at Work No. 5. Luxembourg: Office for Official Publications of the European Communities; 2002. Spice of life or kiss of death. [Google Scholar]
- 12.Federal Ministry of Health. National Human Resources for Health Strategic Plan 2008 to 2012. Federal Ministry of Health. 2007 [Google Scholar]
- 13.World Health Organization. The 2018 Update, Global Health Workforce Statistics. Geneva: World Health Organization; 2018. [Last assessed on 2019 Feb 23]. Available from: http://www.who.int/hrh/statistics/hwfstats/ [Google Scholar]
- 14.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adamu GU, Abdullahi A. Common occupational health hazard amongst healthcare workers in a tertiary health institution in Bida, North-central Nigeria. Int J Bio Res. 2016;8:3656. [DOI: 10.7439/ijbr] [Google Scholar]
- 16.Mojoyinola J K. Effects of Job stress on health, personal and work behaviour of nurses in public hospitals in Ibadan Metropolis, Nigeria. Ethno Med. 2008;2:143–8. [Google Scholar]
- 17.Owolabi AO, Owolabi MO, OlaOlorun AD, Olofin A. Work-related stress perception and hypertension amongst health workers of a mission hospital in Oyo State, South-Western Nigeria. Afr J Prim Health Care Fam Med. 2012;14:307. [Google Scholar]
- 18.Etim JJ, Bassey PF, Ndep AO. Work – Related stress among healthcare workers in Ugep, Yakurr local government area, cross river state, Nigeria: A study of sources, effects, and coping strategies. Int J Pub Health Pharm Pharmacol. 2015;1:23–34. [Google Scholar]
- 19.Obasohan MO, Ayodele KO. Assessment of job stress among clinical health workers in three selected health-care industries in Lagos State, Nigeria. IFE Psycholog IA. 2014;22:2. [Google Scholar]
- 20.Adeolu JO, Yussuf OB, Popoola OA. Prevalence and correlates of job stress among junior doctors in the university college hospital, Ibadan. Ann Ib Postgrad Med. 2016;14:92–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Ladan MA, Ani DK, Usa HA, Ugbeh M, Muhammad LF. Occupational stress among health professionals in ahmadu bello university teaching hospital (A.B.U.T.H), Shika, Zaria, Nigeria. West African J Nursing. 2014;25:24–37. [Google Scholar]
- 22.Onowhakpor A. Occupational stress: Prevalence, sources and coping mechanisms among medical doctors in a tertiary institution. TNHJ. 2018;18:34–44. [Google Scholar]
- 23.Nwankwo CM, Karanja S, Vasanthakaalam H. The occurrence of occupational health hazards in districts health facilities in Kigali. [Last assessed on 2019 Feb 17];Int J Community Med Public Health. 2017 5:21–9. Available from: http://www.ijcmph.com . [Google Scholar]
- 24.Alhassan RK, Poku KA. Experiences of frontline nursing staff on workplace safety and occupational health hazards in two psychiatric hospitals in Ghana. BMC Public Health. 2018;18:701. doi: 10.1186/s12889-018-5620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ndejjo R, Musinguzi G, Yu X, Buregyeya E, Musoke D, Wang JS, et al. Occupational health hazards among healthcare workers in Kampala, Uganda. J Environ Public Health. 2015;2015:1–9. doi: 10.1155/2015/913741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haq Z, Iqbal Z, Rahman A. Job stress among community health workers: A multi-method study from Pakistan. Int J Ment Health Syst. 2008;2:15. doi: 10.1186/1752-4458-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandes MA, Marziale MH. Occupational risks and illness among mental health workers. Acta Paul Enferm. 2014;27:539–47. [doi: 10.1590/1982.0194201400088] [Google Scholar]
- 28.Okeafor CU, Alamina FE. A Qualitative study on psychosocial hazards among health care workers in a tertiary health facility in South-South Nigeria. Ann Ib Postgrad Med. 2018;16:23–9. [PMC free article] [PubMed] [Google Scholar]


