Abstract
Background:
Cervical cancer is a public health problem that disproportionately affects women in less-developed countries despite the availability of effective screening tools. The objective of this study was to determine the level of knowledge of cervical cancer and uptake of the Papanicolaou (Pap) smear test among teachers in public secondary schools in Akwa Ibom State, Nigeria.
Methodology:
This was a cross-sectional descriptive study among 370 female teachers in public secondary schools in Akwa Ibom State, Nigeria. Data were collected with a self-administered questionnaire and were analyzed using Stata software version 10.
Results:
The mean age of respondents was 37.9 ± 7.9 years. More than two-thirds (71.0%) of the respondents had low knowledge of cervical cancer risk factors, whereas 168 (57.9%) respondents had low knowledge of the symptoms. Among the 226 (77.9%) respondents who knew that cervical cancer was preventable, only 65 (28.8%) had high knowledge of preventive measures. About 42.2% of respondents were aware of the Pap smear test and only 8.4% had ever had a Pap smear test. There were significant associations between knowledge of symptoms, prevention of cervical cancer, and the uptake of the Pap smear test (P < 0.05).
Conclusion:
The levels of knowledge of risk factors, symptoms, and methods of prevention of cervical cancer were low in this study. This may have accounted for the low uptake of the Pap smear test. Regular and comprehensive health education concerning cervical cancer and its prevention is advocated in the media and clinics to encourage higher uptake of the Pap smear test.
Keywords: Cervical cancer, knowledge, teacher, uptake of the Pap smear test
INTRODUCTION
Cervical cancer is the second most common cancer among women and the most common cancer among women in Sub-Saharan Africa (SSA).1 Bruni et al., of the Human Papillomavirus Information Centre, placed it as the fourth most common cancer among women.2 It is estimated that women in middle- and low-income countries account for 80.0% of annual cervical cancer deaths occurring worldwide.3,6 Cervical cancer is a preventable disease, but it is a major public health problem despite the availability of effective screening tools.1,7,8
Cervical cancer disproportionately affects women in less-developed countries with age-standardized incidence rates (ASIRs) ranging from about 25–43 cases/100,000 women.2,7 The ASIR for Nigeria, where it is the most common gynecological cancer, is 29.0/100,000 women.9 The disparity in prevalence between the developing and developed countries has been attributed to lack of awareness of cervical cancer by several studies.7,10,11
Studies in North-Western Nigeria and South-Eastern Nigeria have reported low levels of knowledge of cervical cancer among teachers,12,13 but similar studies have not been conducted in Akwa Ibom State.
A key aspect of cervical cancer prevention is the detection of the premalignant form by cervical screening, and there is a long transition time between the premalignant lesions to a frank cancer of the cervix.14,15
The uptake of the Papanicolaou (Pap) smear test, which is a screening tool for premalignant lesions, has been reported to be low by some studies in North-Western Nigeria and South-Eastern Nigeria.12,13
Teachers were a target population for this study because they are in a position to influence the attitude and behavior of a large number of adolescents with whom they come in contact with.
The objective of this study was to ascertain the level of knowledge of cervical cancer as well as the uptake of the Pap smear test among teachers in public secondary schools in Akwa Ibom State, Nigeria.
METHODOLOGY
The study was conducted in Uyo and Abak local government areas (LGAs) which are in Akwa Ibom State, Nigeria. Akwa Ibom State had an estimated population of 5,165,502 in 2014.16 It comprises 31 LGAs and Uyo is the state capital. The major ethnic groups are Ibibio, Annang, and Oron.17 Christianity is the predominant religion with a mix of traditional religion and Islam. The state government is the major employer of labor and many people are civil servants among whom are 3948 teachers in public secondary schools. Furthermore, a significant proportion of inhabitants of the state engage in various small-scale businesses such as farming, fishing, and trading. The state has 1160 public primary schools, 230 public secondary schools, and 4 public tertiary education institutions. There are also a number of private primary, secondary, and tertiary educational institutions.18,19
The study was a cross-sectional study using a quantitative research method to determine the knowledge of cervical cancer and the Pap smear test among 370 female teachers in public secondary schools in Uyo and Abak local education councils (LECs).
The study population included consenting female teachers enrolled by the Akwa Ibom State Secondary Education Board and teaching in public secondary schools in Uyo and Abak LECs, whereas those who did not give consent or had had total hysterectomies were excluded.
The minimum sample size was determined using the formula for cross-sectional studies: n = z2 pq/d2,20 where n is the minimum sample size required, z is the standard normal deviate set at 1.96 for a confidence level of 95%, p is the proportion with the knowledge of cervical screening (69.8%) in a previous study in Sokoto,21 and d is the tolerable error margin of 5%. The estimated sample size, including 10% overestimation to accommodate for nonresponse, was 350. A total of 370 respondents, however, participated in the study. Furthermore, Uyo and Abak LECs were selected by simple random sampling from the 31 LECs in Akwa Ibom State using the Free web Quickcalcs of the GraphPad Prism software by Graphpad Software Incorporated, La Jolla Carlifornia, USA.
The number of teachers enrolled from each school was determined using a proportionate sampling process from a sampling frame obtained from the Principals of all the public secondary schools in Uyo LEC (13 schools) and Abak LEC (10 schools). There were 649 female teachers in Uyo LEC and 581 female teachers in Abak LEC. One hundred and eighty-two teachers were selected by simple random sampling using the Free web Quickcalcs of the GraphPad Prism software by Graphpad Software Incorporated, La Jolla Carlifornia, USA.
The study instrument was a self-designed semistructured questionnaire and the Cronbach's alpha (0.98) was used to estimate the internal consistency for the items in the questionnaire. The questionnaire had three sections that included the sociodemographic characteristics of participants, knowledge of cervical cancer and its risk factors, awareness, and uptake of the Pap smear test. It was self-administered and was pretested on a convenience sample of 36 teachers from Ikot Ekpene LEC that was similar in setting to the study sites. Four research assistants, who were medical doctors, were trained for a day to assist in data collection, and the data were collected over 4 weeks.
There were fourteen knowledge questions on risk factors for cervical cancer. Each correct answer was scored one point; each incorrect answer was scored zero and the “don't know” responses were also scored zero. The risk factor knowledge score was got by dividing the total score by the total possible correct answers (14) and multiplying by 100%. Scores <50% were categorized as low knowledge of risk factors, scores between 50% and 74% were categorized as intermediate knowledge, and scores ≥75% were considered high knowledge.
In the assessment of the knowledge of symptoms of cervical cancer, respondents were to list eight symptoms they knew. Each correct symptom listed was awarded one point. Scores of three or less were considered low, scores of four to five were considered intermediate, and scores of six or more were considered high.
In the assessment of the knowledge of preventive measures of cervical cancer, six responses were expected and each correct response was scored one point with a maximum of six points; scores of two or less were considered low, scores of three to four were considered intermediate, and scores of five or more were considered high knowledge.
Three hundred and seventy-seven questionnaires were distributed to participants: 192 questionnaires in Uyo LEC and 185 questionnaires in Abak LEC with a response rate of 100%. Seven questionnaires in Uyo LEC were excluded from the analysis because of incomplete information. Three hundred and seventy respondents were therefore used for the study.
The data were then analyzed using Stata Data Analysis and Statistical software version 10 by StataCorp. LLC, College Station, Texas, USA.
Frequency was used for categorical variables, and the measure of association was determined using Chi-square test. The level of significance was set at 5%.
Ethical approval was obtained from the Institutional Health Research Ethical Committee of the University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, and permission to conduct the study was obtained from the Akwa Ibom State Secondary Education Board and the principals of each school. Written informed consent was obtained from participants and they were assured of their anonymity as well as freedom to withdraw from the study at anytime.
RESULTS
The mean age of respondents was 37.9 ± 7.9 years. A large proportion, 252 (68.1%), were married and majority, 300 (81.0%), had first degree [Table 1].
Table 1.
Sociodemographic characteristics of respondents (n=370)
| Variables | Frequency, n (%) |
|---|---|
| Age group (years) | |
| 20-29 | 68 (18.4) |
| 30-39 | 126 (34.1) |
| 40-49 | 140 (37.8) |
| 50 and above | 36 (9.7) |
| Mean±SD | 37.9±7.9 |
| Marital status | |
| Single | 87 (23.5) |
| Married/cohabiting | 252 (68.1) |
| Divorced/separated | 15 (4.1) |
| Widowed | 16 (4.3) |
| Level of education | |
| NCE/OND | 28 (7.6) |
| B Sc/HND | 300 (81.0) |
| Master and above | 42 (11.4) |
SD – Standard deviation
Two hundred and ninety (78.4%) respondents were aware of cervical cancer, and the most common source of information was the media, 214 (57.8%) [Table 2].
Table 2.
Awareness of cervical cancer and sources of information among respondents (n=370)
| Variables | Frequency, n (%) |
|---|---|
| Awareness of cervical cancer | |
| Yes | 290 (78.4) |
| No | 80 (21.6) |
| Sources of information# | |
| Media | 214 (57.8) |
| Clinic | 37 (10.0) |
| Friend | 29 (7.8) |
| Family | 16 (4.3) |
| Others | 16 (4.3) |
#Multiple response
Table 3 displays the knowledge of risk factors for cervical cancer among the respondents. More than half of the respondents did not know the risk factors for cervical cancer.
Table 3.
Knowledge of risk factors for cervical cancer among respondents who were aware of cervical cancer (n=290)
| Variables | Frequency, n (%) |
|---|---|
| HPV infection | |
| Yes | 118 (40.8) |
| No | 19 (6.6) |
| Don’t know | 152 (52.6) |
| Prolonged use of oral contraceptive pill | |
| Yes | 119 (41.0) |
| No | 24 (8.3) |
| Don’t know | 147 (50.7) |
| Early marriage before 18 years of age | |
| Yes | 96 (33.1) |
| No | 37 (12.8) |
| Don’t know | 157 (54.1) |
| Tobacco use | |
| Yes | 70 (24.1) |
| No | 48 (16.6) |
| Don’t know | 172 (59.3) |
| Sex with multiple partners | |
| Yes | 100 (34.5) |
| No | 25 (8.6) |
| Don’t know | 165 (56.9) |
| Heredity | |
| Yes | 73 (25.1) |
| No | 44 (15.2) |
| Don’t know | 173 (59.7) |
HPV – Human papillomavirus
Table 4 displays the levels of knowledge of risk factors for cervical cancer, symptoms of cervical cancer, the knowledge that the illness is preventable, and the methods of prevention. In this study, 206 (71.0%) respondents had low level of risk factor knowledge, whereas 168 (57.9%) had low knowledge of symptoms of the disease. Among the respondents who had heard of cervical cancer, 226 (77.9%) knew that it was preventable, but only 65 (28.8%) of these had high knowledge of preventive measures for cervical cancer.
Table 4.
Overall level of knowledge of cervical cancer risk factors, symptoms, preventability, and prevention methods among respondents (n=290)
| Variables | Frequency, n (%) |
|---|---|
| Level of risk factor knowledge (%) | |
| Low (<50) | 206 (71.0) |
| Intermediate (50-74) | 68 (23.5) |
| High (≥75) | 16 (5.5) |
| Knowledge of symptoms | |
| Low (≤3) | 168 (57.9) |
| Intermediate (4-5) | 97 (33.4) |
| High (≥6) | 25 (8.7) |
| Knowledge that cervical cancer is preventable | |
| Yes | 226 (77.9) |
| No | 7 (2.4) |
| Don’t know | 57 (19.7) |
| Knowledge level of cervical cancer prevention methods (n=226) | |
| Low (≤2) | 81 (35.8) |
| Intermediate (3-4) | 80 (35.4) |
| High (≥5) | 65 (28.8) |
Table 5 displays awareness, sources of information, and frequency of the Pap smear test among respondents. About 42.2% of respondents in this study were aware of the Pap smear test, and among these, about a quarter got their information from the media whereas about 12.7% became aware of the test in clinics. Furthermore, 78.2% of those aware of the Pap smear test knew that it should be done at least once every 3 years. At the time of the study, only 8.4% of participants had ever had a Pap smear test.
Table 5.
Awareness, sources of information, and knowledge of frequency of the Papanicolaou smear test (n=370)
| Variables | Frequency n (%) |
|---|---|
| Awareness of the Pap smear test | |
| Yes | 156 (42.2) |
| No | 214 (57.8) |
| Sources of information# | |
| Media | 93 (25.1) |
| Clinic | 47 (12.7) |
| Family | 10 (2.7) |
| Friend | 21 (5.7) |
| Others | 10 (2.7) |
| Knowledge of frequency of the Pap test (n=156) | |
| Yes | 122 (78.2) |
| No | 6 (3.8) |
| I don’t know | 28 (18.0) |
| Uptake of Pap smear test | |
| Yes | 31 (8.4) |
| No | 339 (91.6) |
#Multiple response. Pap – Papanicolaou
The reasons for the nonuptake of the Pap smear test by participants were a lack of awareness (46.5%), nonrecommendation by health worker (11.5%), lack of time (7.0%), reluctance to do the test (6.5%), and not knowing where to do the test (5.5%) [Figure 1].
Figure 1.
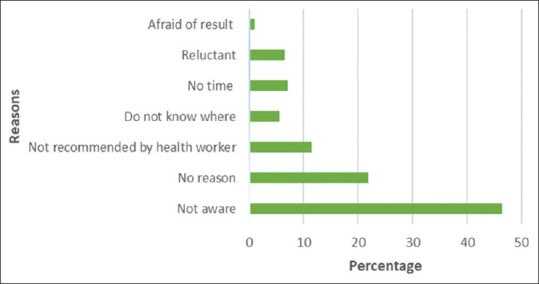
Reasons for the nonuptake of the Papanicolaou smear test by participants
Table 6 demonstrates that the association between the sociodemographic characteristics and the uptake of the Pap smear test among the participants who were aware of the test was not statistically significant, but the uptake was highest among participants in the age group of 40–49 years and lowest among participants in the age group of 20–29 years. Furthermore, uptake increased with higher educational qualification.
Table 6.
Association between sociodemographic characteristics and the uptake of the Papanicolaou smear test among respondents who were aware of the test (n=156)
| Variable | Uptake of Pap smear test |
||
|---|---|---|---|
| Yes (n=31), n (%) | No (n=125), n (%) | Statistic | |
| Age (years) | |||
| 20-29 | 2 (10.0) | 18 (90.0) | Fisher’s exact=0.685 |
| 30-39 | 9 (19.9) | 38 (80.9) | |
| 40-49 | 16 (22.5) | 55 (77.5) | |
| ≥50 | 4 (22.2) | 14 (77.8) | |
| Marital status | |||
| Single | 2 (8.7) | 21 (91.3) | Fisher’s exact=0.2528 |
| Married/cohabiting | 26 (21.1) | 97 (78.9) | |
| Divorced/separated | 1 (50.0) | 1 (50.0) | |
| Widowed | 2 (25.0) | 6 (75.0) | |
| Level of education | |||
| NCE/OND | 1 (12.5) | 7 (87.5) | χ2=5.461P=0.065 |
| B Sc/HND | 20 (16.7) | 100 (83.3) | |
| Master and above | 10 (35.7) | 18 (64.3) | |
Pap – Papanicolaou
Table 7 displays that there was a significant association between the knowledge of symptoms of cervical cancer and the uptake of the Pap smear test (P = 0.028) with the highest uptake among those with intermediate knowledge of symptoms of the disease. In addition, there was a significant association between the knowledge of prevention of cervical cancer and the uptake of the Pap smear test (P = 0.001) with the highest uptake among those with high knowledge of prevention. Although the association between the knowledge of the risk factors for cervical cancer and the uptake of the test was not statistically significant, the uptake of the test increased as the knowledge of risk factors increased.
Table 7.
Association between knowledge about cervical cancer and the uptake of the Papanicolaou smear test among respondents who were aware of the test (n=156)
| Variable | Uptake of Pap smear test |
||
|---|---|---|---|
| Yes (n=31), n (%) | No (n=125), n (%) | Statistic (χ2, P) | |
| Knowledge of risk factors | |||
| Low | 10 (16.7) | 50 (83.3) | 2.102, 0.350 |
| Intermediate | 17 (21.8) | 61 (78.2) | |
| High | 4 (22.2) | 14 (77.8) | |
| Knowledge of symptoms | |||
| Low | 13 (18.1) | 59 (81.9) | 7.160, 0.028* |
| Intermediate | 16 (38.1) | 26 (61.9) | |
| High | 2 (12.5) | 14 (87.5) | |
| Knowledge of prevention | |||
| Low | 11 (15.7) | 59 (84.3) | 13.599, 0.001* |
| Intermediate | 9 (21.4) | 33 (78.6) | |
| High | 11 (25.0) | 33 (75.0) | |
*P<0.05. Pap – Papanicolaou
DISCUSSION
Cervical cancer is the second most common cancer among women and it disproportionately affects women in less-developed countries. It is the most common cancer among women in SSA and a major public health problem despite the availability of effective screening tools. This study set out to assess knowledge of cervical cancer and the Pap smear test as well as the uptake of the test among teachers in public secondary schools in Akwa Ibom State, Nigeria.
Despite the relatively high level of awareness of cervical cancer, more than two-thirds of the respondents had low knowledge of specific risk factors for cervical cancer, and more than half of the respondents had low knowledge of symptoms of the disease. Studies in Nigeria and Ghana have documented similar findings of low knowledge of risk factors of cervical cancer.12,13,22,23 Furthermore, other studies in North-Central and South-Western Nigeria have also reported poor knowledge of symptoms of cervical cancer.4,5,22 The low knowledge of risk factors and symptoms identified in this study may be due to the fact that the information received from different sources were not detailed enough. Considering the age and marital status of many of the teachers, possible missed opportunities at educating them may have occurred during antenatal and postnatal visits to the hospital, which if harnessed could make the hospital a common source of factual information.
The most common source of information on cervical cancer, for the respondents in this study, was the media and this is consistent with reports from previous studies in Ethiopia, Uganda, Gabon, Tanzania, and Kenya.24,28 The media is an important source of information as demonstrated by Perkins et al., who conducted a community-based cervical cancer education program among a group of women in Honduras and concluded that radio programs can serve as an intervention tool and a channel to improve knowledge in communities.29 The different media messages that had been received over the course of time by the respondents in this study may have raised awareness, but were neither regular nor detailed enough about the risk factors or symptoms of cervical cancer. Akintayo and Bello reported that despite a high level of awareness of cervical cancer, most of the respondents in the study in Ikenne, Nigeria, chose the wrong options as symptoms.30
Cervical cancer is a preventable disease and the Pap smear test is a recognized screening tool for the early detection of the illness.1,8 In this study, just above a quarter of the respondents had high knowledge of the prevention methods for cervical cancer and this was lower than that reported by Tefera et al. in the Bale zone of Ethiopia.28 Hoque et al. in South Africa and Getahun et al. in Ethiopia also reported that significant proportions of the respondents (57% and 63.9%, respectively) knew that cervical cancer could be prevented, but contrary findings have been reported in North-Central Nigeria, South-East Nigeria, and Southern Ghana.23,31,32,33,34 The contrasts in some of these findings may be explained by the fact that some of these studies were among rural and semiurban dwellers.31,34
There is a 90% risk reduction if cervical screening is done once every 3 years.35 It has been reported that the uptake of the Pap smear test is low in Nigeria even among populations with high levels of awareness.36,37 This study identified that the awareness of the Pap smear test was about average, and the uptake was low (8.4%) but higher than the 0.4% reported in Anambra State, Nigeria, and 1.1% reported in North-Western Nigeria.12,13 The low level of knowledge of risk factors and symptoms of cervical cancer identified in the study may have accounted for the low uptake of the test. About three-quarters of the respondents who were aware knew the recommended interval for the Pap smear test, and this was higher than what was reported in Ilorin, Nigeria.38 This may be due to the content of the information received from the media or clinics by the respondents before the study.
Lack of awareness of the Pap smear test was the reason given by almost half of the respondents who had never had the test, and this has been similarly reported in Anambra State, Nigeria, and North-Western Nigeria.12,13
This study found no significant association between sociodemographic variables and the uptake of the Pap smear test, and this was a similar finding in the Lyimo and Beran's study in Tanzania.39 Adanu et al., in Ghana, reported that women with high educational levels were more likely to take the Pap smear test, and the current study demonstrated a similar pattern, though it was not significant.40 Furthermore, Bayu et al. reported that women in the age range of 30–39 years were about 1.789 times more likely to be screened for cervical cancer compared with those 21–29 years old.41 In the present study, a higher proportion of women aged 40–49 years had done the Pap smear test compared to those aged 20–29 years and the reason may be that the test may have been recommended to women in the older age group who may have presented with symptoms as well as considering the ASIR of 29/100,000 women in Nigeria.9
Furthermore, this study did not find an association between knowledge of risk factors for cervical cancer and the uptake of the Pap smear test, which is similar to the Arulogun and Maxwell's study and the Gebreegziabher et al.'s study,42,43 but demonstrated a pattern similar to the Bayu et al.'s study in Ethiopia and the Chidyaonga-Maseko etal.'s study which reported that knowledge of cervical cancer and its risk factors influence the uptake of the Pap smear test.41,44 The present study identified an association between knowledge of symptoms of the diseases and the uptake of the Pap smear test. Participants who were less knowledgeable about the symptoms of cervical cancer had not done the Pap smear test, and this has been similarly reported by Bayu et al. in Ethiopia and Lyimo and Beran in Tanzania.39,41 An association between knowledge of cervical cancer prevention methods and the uptake of the Pap smear test was also identified in this study and has been similarly reported by Lyimo and Beran in Tanzania.39 This may be an indication that educational intervention is likely to increase the uptake of the Pap smear test among women and should further be researched.
CONCLUSION
There was a relatively high level of awareness of cervical cancer among the respondents in this study, with the media being the most common source of information. Despite the relatively high level of awareness of cervical cancer, there were low levels of knowledge of risk factors and of symptoms for the illness. Furthermore, despite the good knowledge that cervical cancer is preventable, there was low knowledge of the methods of prevention. The uptake of the Pap smear test was low in this study with lack of awareness identified as a major reason for not doing the test. This study also identified that knowledge of symptoms of cervical cancer and methods of prevention of the disease could influence the uptake of the Pap smear test.
Recommendations
Because the media and clinics have been identified as common sources of information in this study, it would be beneficial to use these sources to deliver regular and comprehensive messages concerning cervical cancer and its prevention. This will improve knowledge of cervical cancer and the uptake of the Pap smear test.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Guidance Note: comprehensive Cervical Cancer Prevention and Control: a Healthier Future for Girls and Women. World Health Organization. 2013. [Last accessed on 2016 Feb 2]. pp. 1–16. Available from: http://apps.who.int/iris/bitstream/10665/78128/3/9789241505147_eng.pdf .
- 2.Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, et al. Human Papillomavirus and Related Diseases in the World. Summary Report. ICO Information Centre on HPV and Cancer (HPV Information Centre) 2016. [Last accessed on 2016 Nov 24]. pp. 7–34. Available from: http://www.hpvcentre.net/statistics/reports/XWX.pdf .
- 3.WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Human Papilloma virus and Related Cancers in Nigeria. Summary Report WHO/ICO. Information Centre on HPV and Cervical Cancer (HPV Information Centre. 2010. [Last accessed on 2016 Nov 24]. Available from: http://www.who.int/hpvcentre .
- 4.Abiodun O, Fatungase O, Olu-Abiodun O, Idowu-Ajiboye B, Awosile J. An assessment of women's awareness and knowledge about cervical cancer and screening and the barriers to cervical screening in Ogun State, Nigeria. IORS J Dent Med Sci. 2013;10:52–8. [Google Scholar]
- 5.Amosu A, Degun A, Babalola A, Thomas M. Level of specific knowledge, awareness, perception, and screening behavior regarding carcinoma of the cervix among rural women in Iwo local government area, Osun state Nigeria. Ann Biol Res. 2011;2:206–21. [Google Scholar]
- 6.World Health Organization. Comprehensive Cervical Cancer Control: a Guide to Essential Practice. 2nd ed. Geneva: World Health Organization; 2014. [Last accessed on 2016 Nov 25]. Available from: http://apps.who.int/iris/bitstream/10665/144785/1/9789241548953_eng.pdf?ua=1 . [PubMed] [Google Scholar]
- 7.Balogun MR, Odukoya OO, Oyediran MA, Ujomu PI. Cervical cancer awareness and preventive practices: A challenge for female urban slum dwellers in Lagos, Nigeria. Afr J Reprod Health. 2012;16:75–82. [PubMed] [Google Scholar]
- 8.Abdullah F, O'Rorke M, Murray L, Su TT. Evaluation of a worksite cervical screening initiative to increase Pap smear uptake in Malaysia: A cluster randomized controlled trial. Biomed Res Int. 2013;2013:572126. doi: 10.1155/2013/572126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, et al. Human Papillomavirus and Related Diseases in Nigeria. Summary Report. ICO Information Centre on HPV and Cancer (HPV Information Centre) 2016. [Last accessed on 2016 Nov 24]. pp. 6–21. Available from: http://www.hpvcentre.net/statistics/reports/NGA.pdf .
- 10.Wright KO, Aiyedehin O, Akinyinka MR, Ilozumba O. Cervical cancer: Community perception and preventive practices in an urban neighborhood of Lagos (Nigeria) ISRN Prev Med. 2014;2014:950534. doi: 10.1155/2014/950534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Isa IA, Gani OO, McFubara K. Cervical cancer screening among female undergraduates and staff in the Niger Delta region of Nigeria. [Last accessed on 2015 Jul 12];Open J Obstet Gynaecol. 2013 3:61–6. Available from: http://dx.doi.org/10.4236/ojog. 2013.31014 . [Google Scholar]
- 12.Adamu AN, Abiola AO, Ibrahim M. The effect of health education on the knowledge, attitude, and uptake of free Pap smear among female teachers in Birnin-Kebbi, North-Western Nigeria. Niger J Clin Pract. 2012;15:326–32. doi: 10.4103/1119-3077.100632. [DOI] [PubMed] [Google Scholar]
- 13.Njelita IA, Egenti NB, Adogu PO, Ubajaka CF, Ibeh CC. How effective is health education on the knowledge of cervical cancer risk and practice of its preventive measures among female primary school teachers in urban Anambra state, Nigeria. [Last accessed on 2016 Jun 04];Int J Multidiscip Res Inf. 2016 2:275–83. Available from: http://www.journalijmri.com/sites/default/files/issue-files/0134.pdf . [Google Scholar]
- 14.Kumar V, Abbas AK, Aster JC. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Philadelphia: Elsevier/Saunders; 2015. pp. 1002–6. Ch. 22. [Google Scholar]
- 15.Shrestha J, Saha R, Tripathi N. Knowledge, attitude and practice regarding cervical cancer screening amongst women visiting tertiary centre in Kathmandu, Nepal. Nepal J Med Sci. 2013;2:85–90. [Google Scholar]
- 16.Akwa Ibom State Government. AKSG Online 2014. Population of Akwa Ibom State. [Last accessed on 2016 Aug 24]. Available from: http://www.aksgonline.com/about_people_population.aspx .
- 17.United Nations Population Fund Nigeria. UNFPA in Akwa Ibom State. 2010. [Last accessed on 2016 Aug 24]. Available from: http://nigeria.unfpa.org/akwaibon.html .
- 18.Akwa Ibom State Government. 2016. [Last accessed on 2016 Aug 22]. Available from: https://AkwaIbomstate.gov.ng/page-page-ministry-of-education.html .
- 19.AKSG Online. Education. 2019. [Last accessed on 2016 Aug 22]. Available from: http://www.aksgonline.com.ws033.alentus.com/educ/default.aspx .
- 20.Ibrahim T. Research Methodology and Dissertation Writing for Health and Allied Health Professionals. 1st ed. Abuja: Cress Global Link; 2009. [Google Scholar]
- 21.Oche M, Kaoje A, Gana G, Ango J. Cancer of the cervix and cervical screening: Current knowledge, attitude and practices of female health workers in Sokoto, Nigeria. Int J Med Med Sci. 2013;5:184–90. [Google Scholar]
- 22.Durowade K, Osagbemi G, Salaudeen A, Musa OI, Bolarinwa OA, Babatunde OA, et al. Knowledge of cervical cancer and its socio-demographic determinants among women in an urban community of North-central Nigeria. [Last accessed on 2016 Jun 07];Savannah J Med Res Pract. 2013 2:46–54. Available from: http://unilorin.edu.ng/publications/bolarinwaoa/Knowledgement%20of%20Cervical%20Cancer%20and%20its%20Socio.demographic.pdf . [Google Scholar]
- 23.Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. Int J Womens Health. 2015;7:31–9. doi: 10.2147/IJWH.S71797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mwaka AD, Orach CG, Were EM, Lyratzopoulos G, Wabinga H, Roland M. Awareness of cervical cancer risk factors and symptoms: Cross-sectional community survey in post-conflict Northern Uganda. Health Expect. 2016;19:854–67. doi: 10.1111/hex.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assoumou SZ, Mabika BM, Mbiguino AN, Mouallif M, Khattabi A, Ennaji MM. Awareness and knowledge regarding of cervical cancer, Pap smear screening and human papillomavirus infection in Gabonese women. BMC Womens Health. 2015;15:37. doi: 10.1186/s12905-015-0193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cunningham MS, Skrastins E, Fitzpatrick R, Jindal P, Oneko O, Yeates K, et al. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro region, Tanzania. BMJ Open. 2015;5:e005828. doi: 10.1136/bmjopen-2014-005828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris RM. Factors associated with the uptake of cervical cancer screening among women of reproductive age in Homabay County, Kenya: a case of Kanyadhiang Sub Location. [Last accessed on 2016 Jun 07];Clin Mother Child Health. 2016 13:1. Available from: http://dx.doi.org/10.4172/2090-7214.1000232 . [Google Scholar]
- 28.Tefera B, Kerbo AA, Gonfa DB, Haile MT. Knowledge of cervical cancer and its associated factors among reproductive age women at Robe and Goba towns, Bale Zone, Southeast Ethiopia. [Last accessed on 2016 May 09];Global J Med Res. 2016 16:27–8. Available from: http://www.medicalresearchjournal.org/index.php/GJMR/article/view/1056 . [Google Scholar]
- 29.Perkins RB, Langrish S, Stern LJ, Simon CJ. A community-based education program about cervical cancer improves knowledge and screening behavior in Honduran women. Rev Panam Salud Publica. 2007;22:187–93. doi: 10.1590/s1020-49892007000800005. [DOI] [PubMed] [Google Scholar]
- 30.Akintayo JB, Bello AA. Creating awareness on cervical cancer via radio broadcasting in Ikenne local government. [Last accessed on 2016 May 04];New Med Mass Commun. 2015 41:1–14. Available from: http://www.iiste.org/Journals/index.php/NMMC/article/view/25769 . [Google Scholar]
- 31.Hoque M, Hoque E, Kader SB. Evaluation of cervical cancer screening program at a rural community of South Africa. East Afr J Public Health. 2008;5:111–6. [PubMed] [Google Scholar]
- 32.Getahun F, Mazengia F, Abuhay M, Birhanu Z. Comprehensive knowledge about cervical cancer is low among women in North West Ethiopia. BMC Cancer. 2013;13:2. doi: 10.1186/1471-2407-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hyacinth HI, Adekeye OA, Ibeh JN, Osoba T. Cervical cancer and pap smear awareness and utilization of Pap smear test among federal civil servants in North central Nigeria. PLoS One. 2012;7:e46583. doi: 10.1371/journal.pone.0046583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eze JN, Umeora OU, Obuna JA, Egwuatu VE, Ejikeme BN. Cervical cancer awareness and cervical screening uptake at the mater Misericordiae hospital, Afikpo, Southeast Nigeria. Ann Afr Med. 2012;11:238–43. doi: 10.4103/1596-3519.102856. [DOI] [PubMed] [Google Scholar]
- 35.Parhizkar S, Latiff LA, Afshari M. Disseminating cervical cancer knowledge: Impact of a public seminar. Int J Learn Dev. 2013;3:203–11. [Google Scholar]
- 36.Dim CC, Ekwe E, Madubuko T, Dim NR, Ezegwui HU. Improved awareness of Pap smear may not affect its use in Nigeria: A case study of female medical practitioners in Enugu, southeastern Nigeria. Trans R Soc Trop Med Hyg. 2009;103:852–4. doi: 10.1016/j.trstmh.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 37.Hoque ME. Awareness of cervical cancer, Papanicolau's smear and its utilization among female, final year undergraduates in Durban, South Africa. J Cancer Res Ther. 2013;9:25–8. doi: 10.4103/0973-1482.110350. [DOI] [PubMed] [Google Scholar]
- 38.Aboyeji PA, Ijaiya M, Jimoh A. Knowledge, attitude and practice of cervical smear as a screening procedure for cervical cancer in Ilorin, Nigeria. Trop J Obstet Gynaecol. 2004;21:114–7. [Google Scholar]
- 39.Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health. 2012;12:22. doi: 10.1186/1471-2458-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adanu RM, Seffah JD, Duda R, Darko R, Hill A, Anarfi J. Clinic visits and cervical cancer screening in Accra. Ghana Med J. 2010;44:59–63. doi: 10.4314/gmj.v44i2.68885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bayu H, Berhe Y, Mulat A, Alemu A. Cervical cancer screening service uptake and associated factors among age eligible women in Mekelle zone, Northern Ethiopia, 2015: A community based study using health belief model. PLoS One. 2016;11:e0149908. doi: 10.1371/journal.pone.0149908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arulogun OS, Maxwell OO. Perception and utilization of cervical cancer screening services among female nurses in university college hospital, Ibadan, Nigeria. Pan Afr Med J. 2012;11:69. [PMC free article] [PubMed] [Google Scholar]
- 43.Gebreegziabher M, Asefa NG, Berhe S. Factors affecting the practices of cervical cancer screening among female nurses at public health institutions in Mekelle town, Northern Ethiopia, 2014: a cross-sectional study. [Last accessed on 2016 April 05];J Cancer Res 2016. 2016 7 Available from: http://dx.doi.org/10.1155/2016/4743075 . [Google Scholar]
- 44.Chidyaonga-Maseko F, Chirwa M, Muula AS. Underutilization of cervical cancer prevention services in low and middle income countries: a review of contributing factors. [Last accessed on 2016 April 25];Pan Afr Med J. 2015 21:23. doi: 10.11604/pamj.2015.21.231.6350. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4607967/pdf/PAMJ-21-231.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]


