Abstract
There is an unacceptably high mortality in acute pancreatitis, which is due to the lack of specific treatments for the disease. A major reason stated to account for the inability to develop effective treatments is that there are multiple pathobiologic pathways activated in the acinar cell mediating pancreatitis making it difficult to choose molecular targets for therapeutic strategies. However, this reasoning limits opportunities for therapeutic development because it does include another important participant in pancreatitis - the pancreatic duct cells. The most recent advance in pancreatitis research is that depletion of both glycolytic and oxidative ATP synthesis is a common event in both acinar and ductal cells. Although ATP has a very short half-life in the blood and is hydrolysed to ADP, there is clear evidence that encapsulating ATP into liposomes can effectively drive ATP into the cells which can be effective in protecting them from necrosis.
In this review, we will examine the effects of different insults associated with pancreatitis on both the acinar and ductal components of the exocrine pancreas pointing out the role of the ductal epithelial responses in both attenuating and increasing the severity of pancreatitis. In addition, we propose that exogenous ATP administration may restore ductal and acinar function providing therapeutic benefit.
BACKGROUND
Acute pancreatitis is a sudden inflammation of the exocrine pancreas which usually develops either as a result of gallstones impacting in the papilla of Vater, or as a result of moderate to heavy ethanol consumption.1,2 Bile duct stones and alcohol abuse together account for about 80% of the cases of acute pancreatitis.1 Although most episodes are mild and self-limiting, the overall mortality of acute pancreatitis remains 5–10%, and may increase to 30% or higher if complications develop.1 This unacceptably high mortality rate is due to the lack of specific treatments for acute pancreatitis. A major reason stated to account for the inability to develop effective treatments is that there are multiple pathobiological pathways activated in the acinar cell mediating pancreatitis making it difficult to choose molecular targets for therapeutic strategies.3–6 However, this reasoning limits opportunities for therapeutic development because it does include another important participant in pancreatitis—the pancreatic duct.7
The most recent advances in pancreatitis research indicate that depletion of glycolytic and oxidative ATP synthesis are common events in both acinar8 and ductal cells during pancreatic injury.9 Notably, non-physiological and sustained increases in Ca2+ concentration lead to decreased ATP levels in the cell, resulting in cell death. Furthermore, because ATP is necessary for the activity of cellular Ca2+ pumps that remove calcium from the cytoplasm of the cell, reducing intracellular Ca2+ (Ca2+) i concentrations to promote ATP production will : have further benefits of reducing excess and ‘toxic’ calcium in the cell cytoplasm. Thus, strategies to increase cellular ATP or otherwise reduce “toxic” levels of cytoplasmic calcium can be useful potential strategies for the treatment of acute pancreatitis.8–12 Although ATP has a very short half-life in the blood and is hydrolysed to ADP, there is clear evidence that encapsulating ATP into liposomes can effectively transport ATP into the cells which can be effective in protecting them from necrosis.13–16
In this review we will examine the effects of different insults associated with pancreatitis on both the acinar and ductal components of the exocrine pancreas, pointing out the role of the ductal epithelial responses in both attenuating and increasing the severity of pancreatitis. In addition, we propose that exogenous ATP administration may restore ductal and acinar function providing therapeutic benefit.
INTRODUCTION
The physiological importance of both the acinar and ductal cells is well known. The acinar cell is responsible for the synthesis, storage and excretion of pancreatic digestive enzymes into the lumen,5 and the duct cells form the pancreatic ductal, system responsible for secreting a bicarbonate-rich isotonic solution which is necessary for transport of the digestive enzymes into the duodenum and neutralising gastric acid.17,18 The coordinated processes of digestive enzyme synthesis, processing and secretion, and secretion of water and electrolyte, are crucially important in maintaining the integrity of the pancreas. Derangement of the above-mentioned acinar cell functions such as observed in cationic trypsinogen (PRSS1) mutations leads to acute and chronic pancreatitis.19,20 Importantly, compromised ductal fluid secretion as occurs in cystic fibrosis leads to destruction of the whole gland,21 or compromised ductal fluid secretaion in different cystic fibrosis transmembrane conductance regulator (CFTR) mutations22 increases the risk of pancreatitis.23,24
In vivo experiments provide additional evidence that both acinar cells and ductal cells are also involved in the pathogenesis of acute pancreatitis. It is well documented that pancreatic enzyme secretion is reduced in both oedematous and necrotising pancreatitis models, indicating that blockade of digestive enzyme secretion occurs in pancreatitis.25–28 Further, pancreatic fluid secretion is greatly increased (by 4-5 fold) at the initiation of pancreatitis, suggesting a possible wash-out defence mechanism activated to attenuate the severity of the disease.26–29 The beneficial effect of this ductal fluid hypersecretion is also indicated by the fact that secretin, a major mediator of pancreatic duct secretion, has been shown to protect against caerulein-induced experimental pancreatitis,30,31 although the level of protection is controversial. Some studies showed that concomitant infusion of secretin with caeruletide (diethylamine salt of caerulein) does not completely prevent the onset of acute pancreatitis, but substantially reduces its severity.30,31 Other studies indicated that secretin has only a very small beneficial effect on the histological alterations and does not significantly reduce the mortality rate32,33 Finally, some investigators found no effect or slightly harmful effects of secretin administration.34,35
EFFECTS OF PANCREATIC DUCTAL CELLS ON THE ACINAR CELLS
As we indicated in the introduction, insufficient electrolyte and fluid secretion by pancreatic ductal cells in cystic fibrosis leads to destruction of acinar cells.21 Although small quantities of CFTR may exist in acinar cells,36 the majority of CFTR Cl− channels are dominantly expressed in ductal cells.36 Therefore, pancreatic ducts are probably responsible for the acinar cell damage and exocrine pancreatic failure in cystic fibrosis. In addition, it is well documented that diminished pancreatic ductal secretion leads to a primary defect in membrane trafficking at the apical plasma membrane of acinar cells.37 Importantly, correction of the luminal pH in the pancreatic tissue of cftr−/− mice reverses the membrane trafficking defects in pancreatic acinar cells and largely restores the membrane dynamics required for exocytosis of zymogen granules and endocytosis for membrane recycling.37 Furthermore, pancreatic duct obstruction alone can cause altered acinar cell membrane trafficking, which can have an important role in the evolution of pancreatitis.38 The importance of luminal pH is also suggested in a model of post-endoscopic retrograde cholangiopancreatography pancreatitis in rats.39 Contrast solution at pH 6.0 or 6.9 injected into the pancreatic duct causes a significant increase in pancreatic oedema, serum amylase activity, neutrophil infiltration and histological damage with more damage seen at pH 6.0.39 However, solutions of pH 7.3 injected at equal pressure cause little damage.39
It has been recently shown that pancreatic fluid and HCO3− secretion by the duct cells and digestive enzyme secretion by acinar cells are severely compromised in patients with autoimmune pancreatitis.40 Ko et al clearly demonstrated that corticosteroid treatment repairs pancreatic parenchymal damage and improves ductal HCO3− secretion and acinar digestive enzyme secretion.40 The decreased pancreatic ductal function in autoimmune pancreatitis and its reversal by corticosteroids might be due to partial mislocalisation of CFTR to the cytoplasm and correction of its targeting to the apical membrane of duct cells.40 Furthermore, recent studies have shown that lowering extracellular pH, which can occur during the deficit of luminal bicarbonate concentration, enhances secretagogue-induced zymogen activation and injury in acinar cells.41 These data clearly suggest that (i) alterations in pancreatic ductal fluid and bicarbonate secretion can increase patients’ risk of pancreatitis and (ii) restoration of pancreatic ductal bicarbonate and fluid secretion may have therapeutic benefits (box 1).
Box 1. Effects of pancreatic ductal cells on acinar cells.
Ductal cells→acinar cells
Insufficiency of electrolyte and fluid secretion by pancreatic ductal cells in cystic fibrosis leads to destruction of acinar cells
Diminished pancreatic ductal secretion leads to a primary defect in membrane trafficking at the apical plasma membrane of acinar cells
Correction of the luminal pH in the pancreatic tissue in cystic fibrosis reverses the membrane trafficking defects in pancreatic acinar cells
Lowering extracellular pH, which can occur during the deficit of luminal bicarbonate concentration, enhances secretagogue-induced zymogen activation and injury in acinar cells
EFFECTS OF ACINAR CELLS ON PANCREATIC DUCTAL CELLS
Acinar cells secrete a NaCl-rich fluid containing digestive enzymes. It is well documented that luminal Cl− secreted by acinar cells and Cl− channels of ductal cells are crucially important in bicarbonate secretion.17,42 Of note, the greatest proportion of bicarbonate secretion occurs in proximal ductal cells which are next to the acinar cells.17 The Cl− secreted by acinar cells and proximal ductal cells are exchanged for bicarbonate by the luminal anion exchanger, resulting in bicarbonate secretion. Thus, damage to the Cl− transport of acinar cells will decrease bicarbonate secretion from ductal cells.
Haanes and Novak43 have recently demonstrated that zymogen granules not only contain proenzymes but also ATP, which is very important in coordinating acinar and ductal secretion. Luminal ATP was shown to stimulate pancreatic ductal fluid and bicarbonate secretion via purinergic receptors,44 therefore exocytosis of the zymogens into the ductal lumen will stimulate ductal secretion which will transport the digestive enzymes into the duodenum. In acute pancreatitis, when the trafficking of zymogen granules is damaged and the exocytosis is blocked, the resulting lack of ATP delivered to the ducts may result in less bicarbonate and fluid secretion, causing further inhibition of acinar cell secretion and augmenting injury to the acinar cell.
However, the most important question is whether digestive enzymes have any effects on pancreatic ductal function. Trypsin is secreted as its inactive zymogen precursor, trypsinogen, which is inactive until it is cleaved by enterokinase in the intestinal lumen. There is substantial evidence that trypsinogen in pancreatic juice becomes prematurely converted to trypsin in both acute and chronic pancreatitis.45 Most investigators believe that acute pancreatitis results from the premature intra-acinar cell activation of zymogens, especially trypsinogen.46 Following this intra-acinar activation, a trypsin cascade occurs in the gland which leads to the autodigestion of acinar cells.46 There are different opinions about how trypsin affects bicarbonate secretion in duct cells. Nguyen et al found that activation of basolateral protease activated receptor-2 (PAR-2) led to increased apical Ca2+-activated Cl− conductances, suggesting increased bicarbonate secretion.47 In contrast, Alvarez et al found inhibition of bicarbonate secretion by luminally administered trypsin or PAR-2 activating peptide.48 There is no information available about the effects of other enzymes on pancreatic ductal function. Other studies show that the effects mediated via PAR-2 are complicated in the pancreas and can actually protect or harm the pancreas depending on the model used.49–52 Some studies indicate that the severity of pancreatic injury in caerulein-induced pancreatitis is reduced in rats and mice that have been pretreated with PAR-2-activating peptide.50,51 However, others show that the severity of pancreatic injury during experimental pancreatitis can be either increased or decreased by the activation of PAR-2.49 Further investigation is warranted to determine the roles of PAR-2 in both normal and pathophysiological states the exocrine pancreas (box 2).
Box 2. Effects of the acinar cells on pancreatic ductal cells.
Acinar cells→ductal cells
Acinar cells secrete Cl−, which is important in promoting ductal bicarbonate secretion
Damage of Cl− transport in acinar cells may decrease bicarbonate secretion from ductal cells
ATP is secreted by acinar cells into the ductal lumen
Luminal ATP stimulates pancreatic ductal fluid and bicarbonate secretion via purinergic receptors
EFFECTS OF BILE ACIDS IN THE EXOCRINE PANCREAS
Acinar cells
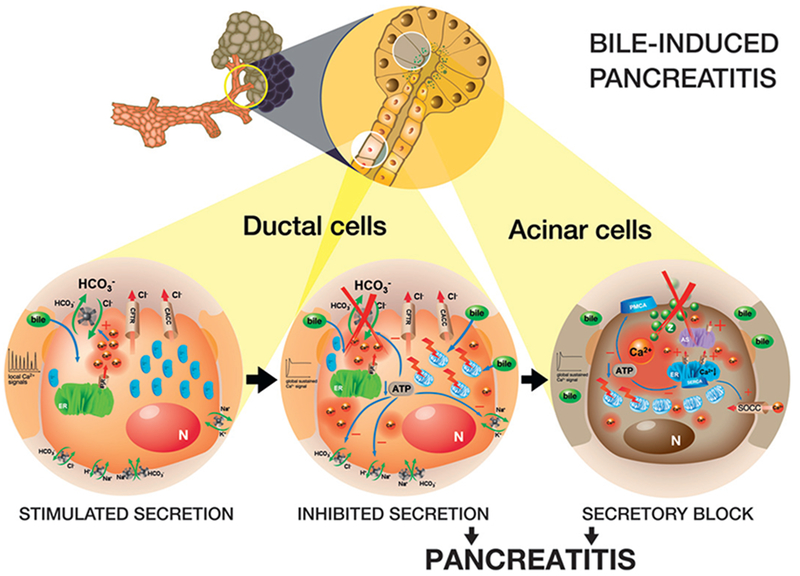
Reflux of bile acids into the pancreatic ductal system is proposed as one mechanism initiating gallstone pancreatitis. Although the bile acids refluxed can reach both ductal and acinar cells through the pancreatic ductal system, much more research has been done on their effects in acinar cells. Taurine-conjugated bile acids have been found to induce Ca2+ signalling in pancreatic acinar cells via inositol 1,4,5-triphosphate receptor and ryanodine receptor-mediating mobilisation of Ca2+i from endoplasmic reticulum53 and acidic Ca2+ stores,54 but not from the mitochondria54 (figure 1). In addition, the bile acids inhibit the sarco/endoplasmic reticulum Ca2+ ATPase (SERCA)-dependent Ca2+ reloading into intracellular pools.55 Of note, the depletion of intracellular calcium stores also activates calcium influx into the cytosol from the extracellular space. The combination of release of calcium from intracellular stores and inhibition of calcium reuptake into the stores along with increased influx of extracellular calcium leads to a marked increase in the concentration of calcium in the cytoplasm of the acinar cell. This increased cytoplasmic calcium is taken up by the mitochondria, leading to excess mitochondrial calcium and mitochondrial failure. The mitochondrial failure, in turn, leads to decreased production of ATP which is necessary for the calcium pumps at both the endoplasmic reticulum (SERCA) and the plasma membrane (ie, plasma membrane calcium ATPase). Thus, abnormal calcium levels in the cytoplasm lead to a vicious cycle of more and more calcium toxicity and necrosis.53,56 If this pathological calcium signal continues for more than 15–20 min, activation of intracellular trypsinogen occurs,12,57,58 which can further augment necrosis11.
Figure 1.
Effects of bile acids on the exocrine pancreas. Ductal cells. Bile acids have dual effects on the ductal fluid and HCO3− secretion. First, when the non-conjugated bile acids reach the ductal cells in low concentration, they induce a dose-dependent elevation of Ca2+i concentration via an inositol 1,4,5-triphosphate receptor (IP3R) and phospholipase C-mediated pathway and stimulate HCO3− secretion through the luminal Cl−/HCO3− exchanger. Theoretically, ductal cells may try to wash out the toxic acids and thus defend the acinar cells. If this defence mechanism is inefficient and bile acids reach the ductal cells in high concentration, they induce a toxic sustained Ca2+i concentration signal and decrease [ATP]i, which will inhibit all of the acidebase transporters including the basolateral Na+/H+ exchanger, Na+/HCO3− cotransporter and the luminal Cl−/HCO3− exchanger. Acinar cells. Most probably when the ductal defence mechanism is damaged, bile acids can reach the acinar cells at high concentrations. The key point in the toxic effects of bile acid on acinar cells is the generation of global sustained Ca2+ waves. Bile acids elevate the Ca2+i concentration by stimulating Ca2+ efflux from the (i) endoplasmic reticulum (ER) via IP3R and ryanodine receptors, from the (ii) acidic Ca2+ stores (AS) and by (iii) stimulating indirectly the opening of store-operated Ca2+ channels (SOCC). In addition, bile acids inhibit Ca2+ restoration to the basal level by blocking both the sarco/endoplasmic reticulum Ca2+ ATPase (SERCA)-dependent Ca2+ reloading into intracellular pools and the plasma membrane Ca2+ ATPase (PMCA)-dependent Ca2+ excretion. Depletion of Ca2+i defends the acinar cells from death. CaCC, Ca2+-activated Cl− channel; CFTR, cystic fibrosis transmembrane conductance regulator Cl− channel; N, nucleus; Z, zymogen granule; +, stimulation; −, inhibition.
The calcium chelator 1,2-bis(2-aminophenoxy) ethane-N,N,N’,N’-tetra-acetic acid (BAPTA) can prevent the processes involved in necrosis of acinar cells as described above.55 The beneficial effects of BAPTA are well documented by other studies as well.46,59,60 Pretreatment of animals with this calcium chelator before pancreatic duct ligation significantly reduces (by more than 50%) the elevations of serum pancreatic enzyme activities as well as pancreatic trypsinogen activation.46 In addition, BAPTA prevents caerulein-induced NF-κB activation in acini.59 Therefore, there is a general consensus that Ca2+ toxicity is the most important factor contributing to bile acid-induced acinar cell damage.
A recent study demonstrated that a G-protein-coupled cell surface bile acid receptor (Gpbar1) mediates the effects of bile acids on the pancreas. Therefore, interfering with Gpbar1 function may have beneficial effects.61
Ductal cells
Basolateral or luminal administration of the non-conjugated bile acid chenodeoxycholate (CDC) dose-dependently and reversibly reduces the intracellular pH (pHi) of pancreatic ductal cells.60 The conjugated glycochenodeoxycholate has a significantly smaller effect than the non-conjugated CDC,60 suggesting that while non-conjugated bile salts (as weak acids) can pass through the cell membranes by passive diffusion, conjugated bile acids are impermeable to cell membranes and require active transport mechanisms for cellular uptake.62 After entering the cell, bile acids induce a dose-dependent increase in Ca2+i concentration by a phospholipase C- and 1,4,5-triphosphate receptor-mediated mechanism60 (figure 1). Notably, the non-conjugated CDC had significantly larger effects on Ca2+i concentration than the conjugated glycochenodeoxycholate.60
Effects of low doses of bile acids
Luminal administration of low doses of CDC significantly stimulates HCO3− efflux through the luminal anion exchanger of the cells.60 Importantly, the stimulatory effect of low doses of luminal CDC on HCO3− secretion is dependent on Ca2+i.60 Therefore, CDC may have additional effects either on Ca2+-dependent channels/transporters in pancreatic ductal cells (such as Ca2+-activated Cl− channel, Ca2+-activated potassium channels, or SLC26 anion transporters). Since the stimulatory effect of CDC is Ca2+ dependent, bile acids may influence the activities of these channels. In addition, these channels may play an important part in the stimulatory effects of bile acids. CFTR expression but not Cl− transport is also important in the stimulatory effect of bile acids on ductal secretion.9,60,63 The conjugated bile acids have no effects on HCO3− secretion.9,60
Theoretically, when small stones impact in the papilla of Vater and obstruct the pancreatic duct, bile acids can diffuse up into the ductal tree in a low concentration. The findings discussed here suggest that in this situation ductal cells may try to wash out the toxic bile acids and thus defend the acinar cells by increasing fluid and bicarbonate secretion, which stops or delays the bile acid diffusion towards the acinar cells. Also, the greater ductal flow may push stones through the papilla to clear the obstruction (figure 1).
The importance of this theory can be argued by the fact that under physiological conditions the pressure in the main pancreatic duct is higher than in the bile ducts64 and thus it is still controversial whether bile acids can enter the pancreatic ductal tree. However, this does not deny the fact that if bile acids enter the pancreatic ducts, the ductal cells act as a guard of acinar cells.
Effects of high doses of bile acids
High concentrations of bile acids can reach the ductal cells either from the basolateral side or if the above-mentioned defence mechanism is insufficient, from the luminal side.7,60 Non-conjugated bile acids induce a toxic sustained Ca2+i signal and inhibit all the acid—base transporters including the basolateral Na+/H+ exchanger, Na+/HCO3− cotransporter and the luminal Cl−/HCO3− exchanger60 (figure 1). Importantly, in contrast to the effects of bile salts on acinar cells, Ca2+i chelators do not prevent the strong inhibitory effect of CDC on the above-mentioned transporters.60 We have recently provided evidence that mitochondrial damage and [ATP]i depletion are the most crucial factors in the toxic inhibitory effect of CDC on pancreatic ductal secretion.9
Contrary to the effects of low concentrations of bile acids, high concentrations of CDC lead to epithelial barrier damage,60,65,66 the secretory mechanisms of pancreatic ductal cells are inhibited and the ducts can no longer act as a defensive wall against the toxic bile. Notably, longer administration of high concentrations of bile acids can cause a detergent-like, uncontrolled increase in plasma membrane H+ permeability60; and if this occurs, cell injury and death cannot be prevented. It has been shown that administration of 1 mM CDC to pancreatic ductal cells for 6–9 min is sufficient to permeabilise the pancreatic ductal membrane to larger molecules.60
The normal concentration of bile salts in human gall bladder bile is approximately 5—10 mM. Therefore, up to 1 mM of bile salts (considered a high concentration) can easily reach the pancreas in pathological circumstances. It has been documented that 100 μM of CDC stimulates, whereas 1 mM inhibits, pancreatic ductal secretion.60 Therefore, it is more than likely that the ductal epithelium will switch from stimulated to inhibited secretion during the onset of bile-induced pancreatitis. Consequently, the inhibited secretion by high concentrations of bile acids will increase the risk of bile salts reaching the acinar cells.
Of note, if the bile is infected with bacteria, hydrolase enzymes can convert conjugated bile salts into their deconjugated counterparts. Since the non-conjugated bile acids are more toxic than the conjugated ones, bacterial infection can increase bile toxicity in the pancreas.
EFFECTS OF ETHANOL ON THE EXOCRINE PANCREAS
Interestingly, ethanol itself does not induce experimental pancreatitis.67,68 Neither liquid ethanol-containing diets nor continuous intragastric ethanol infusion induces pancreatitis in rats.69 In addition, ethanol even at very high concentration has little effect on Ca2+i concentration in pancreatic acinar cells.10,70,71
Ethanol can be metabolised via oxidative and non-oxidative pathways. Alcohol dehydrogenase mediates the oxidative pathway by catalysing ethanol conversion to acetaldehyde. Very little oxidative metabolism of ethanol takes place in the pancreas, in contrast to the liver, where the majority of the body’s oxidative metabolism occurs. Further, it is unlikely that acetaldehyde induces pancreatitis, since this metabolite had no toxic effect on pancreatic acinar cells.3,70 However, the non-oxidative ethanol fatty acid ethyl esters (FAEE) metabolites induce a sustained toxic calcium signal in pancreatic acinar cells, leading to necrosis.3,10,70 In addition, FAEE infusion into rats causes pancreatic acinar cell vacuolisation and trypsinogen activation.72 The pancreas has the highest activity of FAEE synthases of any organ in the body as demonstrated in postmortem measurements showing that the greatest levels of FAEE were in the pancreas of subjects intoxicated with alcohol.73 The fact that FAEE stimulates, whereas ethanol and acetaldehyde inhibit, nuclear factor κB binding activity, a key participant in the inflammatory response of pancreatitis,74 also suggests that the key harmful factors of ethanol are its non-oxidative metabolites. Very importantly, cftr−/− versus wild-type mice demonstrate a quantitative increase in FAEE in the liver after ethanol administration, with an increase in selective FAEE species (ethyl oleate) in the liver and pancreas.75 Since FAEE can be converted to fatty acids in the mitochondria and can induce sustained toxic elevation of cytosolic Ca2+, CFTR deficiency can lead to increased susceptibility to acute pancreatitis via altered ethanol metabolism. However, the alleged role of ethanol on CFTR in pancreatitis is not supported by clinical data.76 CFTR mutations are not more common in patients with alcohol-induced pancreatitis.76
Acinar cells
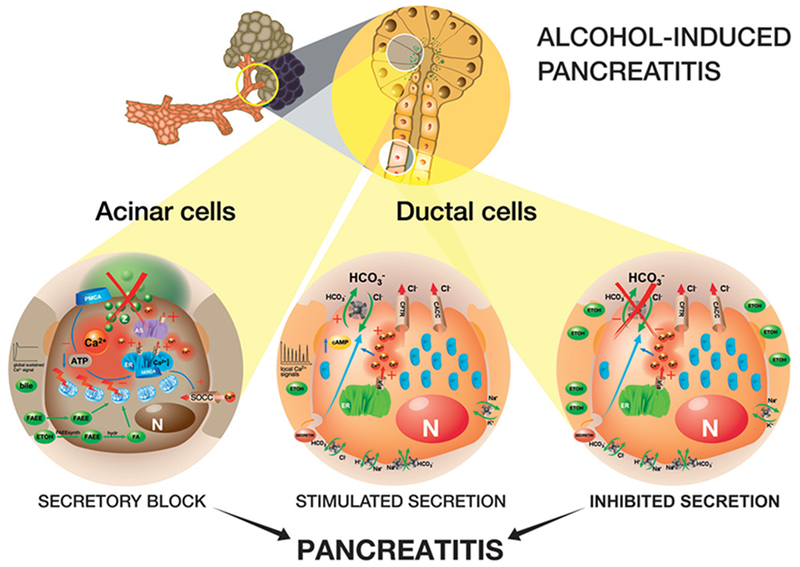
As indicated above, ethanol is metabolised by FAEE synthases in the acinar cell, and the FAEE products cause a sustained increase in calcium in the cell which can have a toxic effect on mitochondrial function leading to necrosis.10,70,71 In addition, FAEEs are converted to free fatty acids by cytosolic hydrolases which also inhibit mitochondrial ATP synthesis causing a marked reduction in the [ATP]i3 (figure 2). Very importantly, [ATP]i supplementation maintains Ca2+-ATPase activity in the presence of non-oxidative ethanol metabolites10 (figure 2). FAEEs were also found to induce caspase-3-mediated apoptosis77 and necrosis74 in pancreatic cell lines, which can further increase the ethanol-induced pancreatic injury.
Figure 2.
Effects of ethanol on pancreatic ductal cells. Acinar cells. Ethanol (ETOH) or fatty acid ethyl esters (FAEE) can enter the cells by diffusion. Ethanol will be metabolised by FAEE synthase (synth.). FAEE and their metabolites fatty acids (FA) strongly elevate the intracellular Ca2+ (Ca2+i) concentration by stimulating Ca2+ efflux from the (i) endoplasmic reticulum (ER) via inositol 1,4,5-triphosphate receptor (IP3R) and ryanodine receptor-dependent pathways, from the (ii) acidic Ca2+ stores (AS) and by (iii) indirectly stimulating the opening of store-operated Ca2+ channels (SOCC). FA strongly damage the mitochondria and decrease [ATP]i. This energetic breakdown will inhibit the Ca2+ restoration to the basal level by blocking both the sarco/endoplasmic reticulum Ca2+ ATPase-dependent Ca2+ reloading into intracellular pools and the plasma membrane Ca2+ ATPase (PMCA)-dependent Ca2+ excretion. Restoration of [ATP]i can defend the acinar cells from death. Ductal cells. Low concentration of ethanol and secretin together cause elevation of Ca2+i concentration and cAMP level. Ethanol augments the secretin-stimulated pancreatic ductal fluid and HCO3− secretion. However, high concentration of ethanol inhibits HCO3− secretion induced by physiological concentration of secretin. CaCC, Ca2+-activated Cl− channel; CFTR, cystic fibrosis transmembrane conductance regulator Cl− channel; N, nucleus; Z, zymogen granule; +, stimulation; −, inhibition.
Ductal cells
Ethanol can stimulate gastric acid secretion.78–81 The increased acid load delivered to the duodenum will result in increased secretin release80 which will, in turn, augment ductal secretion of a bicarbonate-rich fluid.80 Therefore, drinking alcoholic beverages will result in an increase in the concentration of both secretin and ethanol. Interestingly, ethanol has a dual effect on bicarbonate secretion similarly to the non-conjugated bile acids as we describe below.82
Effects of low concentration of ethanol
Neither ethanol nor secretin alone has any effects on Ca2+i signalling in pancreatic duct cells.82 However, when the cells were pretreated with physiological concentrations of secretin, ethanol showed marked increases in Ca2+i concentration. A low concentration of ethanol stimulates pancreatic ductal fluid and bicarbonate secretion; however, to achieve this effect, activation of the cAMP pathway and Ca2+i mobilisation are required82 (figure 2). Since secretin and ethanol elevate the intracellular cAMP level and ethanol induces Ca2+i mobilisation in the presence of secretin, we can assume that during social drinking (when ethanol concentration is <20 mM), bicarbonate and fluid secretion are stimulated.80,82
Effects of high concentration of ethanol
Intravenous administration of a high concentration of ethanol inhibits pancreatic secretion.83–86 In vitro data also showed that ethanol at 100 mM concentration inhibited the secretory response to a physiological concentration of secretin82 (figure 2). Unfortunately, far behind the studies on acinar cells, no further data are available concerning the effects their metabolites or ethanol on pancreatic ductal bicarbonate secretion.
ATP IS A CENTRAL MOLECULE IN ACINAR AND DUCTAL CELLS IN ACUTE PANCREATITIS
Aerobic metabolism in mitochondria generates most of the ATP required for cell function in normal pancreatic cellular physiology. A small fraction of ATP is produced by glycolysis. In anaerobic conditions that occur in the tissue of pancreatitis owing to microvascular dysfunction, ATP generated by mitochondria is decreased and not sufficiently replaced by ATP from anaerobic glycolysis. Needless to say, ATP is necessary for physiological enzyme secretion by acinar cells43,87 and bicarbonate efflux by ductal cells.9 Acinar mitochondrial damage in bile-induced experimental pancreatitis was observed 30 years ago88; however, the central role of ATP was highlighted only recently.1,3,6,10,68,70,71,89
Most recently, Voronina et al8 showed that bile and fatty acids inhibit ATP production obtained by both mitochondrial oxidative phosphorylation and glycolysis in acinar cells. Maléth et al9 suggested that bile acids induce the same metabolic damage in ductal cells. Criddle et al10 showed earlier that intracellular administration of ATP by a patch pipette totally abolished the toxic effect of fatty acids in acinar cells. These data strongly suggest that restoration of intracellular ATP concentration can be beneficial in acute pancreatitis. Since ATP is highly sensitive to enzymatic hydrolysis, the key question is how to deliver this bioenergetic substrate into the cells in vivo. Encapsulating ATP into liposomes was found to protect the myocardium in acute experimental myocardial infarction.14,15,90 In addition, it was shown to protect the liver from injury during shock.13 It would be crucially important to establish a delivery system for pancreatic energy supply that can protect ATP from degradation and can cross the cell membrane.
CONCLUSIONS
The summary we provide here leads to a justification for a hypothesis that pancreatic duct cell secretion of sodium bicarbonate and water has a protective effect for the entire exocrine pancreas during stresses such as passage of biliary stones and ethanol abuse (box 3). These stresses can activate secretory pathways that can defend the pancreas by (i) washing out the toxic agents and (ii) digestive enzymes from the exocrine pancreas; (iii) increasing the intraluminal pH and (iv) maintaining and/or restoring the membrane trafficking in pancreatic acinar cells. If this preliminary ductal defence mechanism is overwhelmed by the stressors, the ductal secretion fails, leading to pancreatitis. However, more studies are needed to demonstrate the protective role of ductal secretions; the mechanisms underlying this protective response; and methods to augment the response for therapeutic benefit.
Box 3. Role of pancreatic ducts in the pathogenesis of acute pancreatitis.
Statements
Damage of electrolyte and fluid secretion by pancreatic ductal cells leads to acinar cell injury
Cystic fibrosis transmembrane conductance regulator mutations increase patients’ risk of pancreatitis
Lowering extracellular pH enhances secretagogue-induced zymogen activation and injury in acinar cells
Low concentrations of toxic agents stimulate pancreatic ductal secretion
High concentrations of toxic agents inhibit pancreatic ductal secretion
Hypothesis
In the early stage of acute pancreatitis, the increased ductal fluid and bicarbonate secretion can defend the pancreas by washing out the toxic agents and digestive enzymes
If this preliminary ductal defence mechanism is overwhelmed by the stressors, ductal secretion can fail, leading to pancreatitis
Importantly, it seems more than likely that energy transfer into the acinar and ductal cells would restore, at least in part, their physiological function and therefore could be beneficial in the early phase of acute pancreatitis (box 4).
Box 4. Role of ATP in the pathogenesis of acute pancreatitis.
Statements
ATP is necessary for physiological enzyme secretion by acinar cells and bicarbonate efflux by ductal cells
Bile acids inhibit glycolysis and oxidative phosphorylation in both acinar and ductal cells
Toxic agents such as bile and fatty acids reduce cytosolic and mitochondrial ATP levels of acinar cells
Bile acids reduce cytosolic ATP in ductal cells
Intracellular administration of ATP totally abolishes the toxic effect of fatty acids in acinar cells
Hypothesis
Restoration of intracellular ATP concentration can be beneficial in acute pancreatitis
Encapsulating ATP into liposomes can be a good delivery method to drive ATP into the cells in acute pancreatitis
Footnotes
Competing interests None.
Provenance and peer review Commissioned; externally peer reviewed.
REFERENCES
- 1.Pandol SJ, Saluja AK, Imrie CW, et al. Acute pancreatitis: bench to the bedside. Gastroenterology 2007;132:1127–51. [DOI] [PubMed] [Google Scholar]
- 2.Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol 2006;101:2379–400. [DOI] [PubMed] [Google Scholar]
- 3.Criddle DN, McLaughlin E, Murphy JA, et al. The pancreas misled: signals to pancreatitis. Pancreatology 2007;7:436–46. [DOI] [PubMed] [Google Scholar]
- 4.Halangk W, Lerch MM. A unique pancreatic mitochondrial response to calcium and its role in apoptosis. Gut 2009;58:328–30. [DOI] [PubMed] [Google Scholar]
- 5.Gaisano HY, Gorelick FS. New insights into the mechanisms of pancreatitis. Gastroenterology 2009;136:2040–4. [DOI] [PubMed] [Google Scholar]
- 6.Pandol SJ. Acute pancreatitis. Curr Opin Gastroenterol 2006;22:481–6. [DOI] [PubMed] [Google Scholar]
- 7.Lerch MM, Aghdassi AA. The role of bile acids in gallstone-induced pancreatitis. Gastroenterology 2010;138:429–33. [DOI] [PubMed] [Google Scholar]
- 8.Voronina SG, Barrow SL, Simpson AW, et al. Dynamic Changes in Cytosolic and Mitochondrial ATP Levels in pancreatic acinar cells. Gastroenterology 2010;138:1976–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maleth J, Venglovecz V, Rázga ZS, Tiszlavicz L, et al. Non-conjugated chenodeoxycholate induces severe mitochondrial damage and inhibits bicarbonate transport in pancreatic duct cells. Gut 2011;60:136–8. [DOI] [PubMed] [Google Scholar]
- 10.Criddle DN, Murphy J, Fistetto G, et al. Fatty acid ethyl esters cause pancreatic calcium toxicity via inositol trisphosphate receptors and loss of ATP synthesis. Gastroenterology 2006;130:781–93. [DOI] [PubMed] [Google Scholar]
- 11.Petersen OH. Ca2+-induced pancreatic cell death: roles of the endoplasmic reticulum, zymogen granules, lysosomes and endosomes. J Gastroenterol Hepatol 2008;23(Suppl 1):S31–6. [DOI] [PubMed] [Google Scholar]
- 12.Petersen OH . Ca2+ signaling in pancreatic acinar cells: physiology and pathophysiology. Braz J Med Biol Res 2009;42:9–16. [DOI] [PubMed] [Google Scholar]
- 13.Konno H, Matin AF, Maruo Y, et al. Liposomal ATP protects the liver from injury during shock. Eur Surg Res 1996;28:140–5. [DOI] [PubMed] [Google Scholar]
- 14.Hartner WC, Verma DD, Levchenko TS, et al. ATP-loaded liposomes for treatment of myocardial ischemia. Wiley Interdiscip Rev Nanomed Nanobiotechnol 2009;1:530–9. [DOI] [PubMed] [Google Scholar]
- 15.Levchenko TS, Hartner WC, Verma DD, et al. ATP-loaded liposomes for targeted treatment in models of myocardial ischemia. Methods Mol Biol 2010;605:361–75. [DOI] [PubMed] [Google Scholar]
- 16.Han YY, Huang L, Jackson EK, et al. Liposomal atp or NAD+ protects human endothelial cells from energy failure in a cell culture model of sepsis. Res Commun Mol Pathol Pharmacol 2001;110:107–16. [PubMed] [Google Scholar]
- 17.Argent BE . Cell physiology of pancreatic ducts In: Johnson LR, ed. Physiology of the gastrointestinal tract. Volume 2 4th edn. San Diego: Elsevier, 2006:1376–96. [Google Scholar]
- 18.Lee MG, Muallem S. Physiology of duct cell secretion In: H B, ed. The pancreas. 2nd edn. Massachusetts: Blackwell Publishing, 2008:78–91. [Google Scholar]
- 19.Kereszturi E, Sahin-Toth M. Intracellular autoactivation of human cationic trypsinogen mutants causes reduced trypsinogen secretion and acinar cell death. J Biol Chem 2009;284:33392–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teich N, Rosendahl J, Toth M, et al. Mutations of human cationic trypsinogen (PRSS1) and chronic pancreatitis. Hum Mutat 2006;27:721–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nousia-Arvanitakis S Cystic fibrosis and the pancreas: recent scientific advances. J Clin Gastroenterol 1999;29:138–42. [DOI] [PubMed] [Google Scholar]
- 22.Weiss FU, Simon P, Bogdanova N, et al. Functional characterisation of the CFTR mutations M348V and A1087P from patients with pancreatitis suggests functional interaction between CFTR monomers. Gut 2009;58:733–4. [DOI] [PubMed] [Google Scholar]
- 23.Hegyi P, Rakonczay Z. Insufficiency of electrolyte and fluid secretion by pancreatic ductal cells lead to increase patients risk to pancreatitis. Am J Gastroenterol 2010;105(9):2119–20. [DOI] [PubMed] [Google Scholar]
- 24.Cavestro GM, Zuppardo RA, Bertolini S, et al. Connections between genetics and clinical data: Role of MCP-1, CFTR, and SPINK-1 in the setting of acute, acute recurrent, and chronic pancreatitis. Am J Gastroenterol 2010;105:199–206. [DOI] [PubMed] [Google Scholar]
- 25.Niederau C, Niederau M, Luthen R, et al. Pancreatic exocrine secretion in acute experimental pancreatitis. Gastroenterology 1990;99:1120–7. [DOI] [PubMed] [Google Scholar]
- 26.Czako L, Yamamoto M, Otsuki M. Exocrine pancreatic function in rats after acute pancreatitis. Pancreas 1997;15:83–90. [DOI] [PubMed] [Google Scholar]
- 27.Czako L, Yamamoto M, Otsuki M. Pancreatic fluid hypersecretion in rats after acute pancreatitis. Dig Dis Sci 1997;42:265–72. [DOI] [PubMed] [Google Scholar]
- 28.Hegyi P, Czako L, Takacs T, et al. Pancreatic secretory responses in L-arginine-induced pancreatitis: comparison of diabetic and nondiabetic rats. Pancreas 1999;19:167–74. [DOI] [PubMed] [Google Scholar]
- 29.Manso MA, San Roman JI, de Dios I, et al. Cerulein-induced acute pancreatitis in the rat. Study of pancreatic secretion and plasma VIP and secretin levels. Dig Dis Sci 1992;37:364–8. [DOI] [PubMed] [Google Scholar]
- 30.Renner IG, Wisner JR Jr, Rinderknecht H. Protective effects of exogenous secretin on ceruletide-induced acute pancreatitis in the rat. J Clin Invest 1983;72:1081–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Renner IG, Wisner JR Jr. Ceruletide-induced acute pancreatitis in the dog and its amelioration by exogenous secretin. Int J Pancreatol 1986;1:39–49. [DOI] [PubMed] [Google Scholar]
- 32.Niederau C, Ferrell LD, Grendell JH. Caerulein-induced acute necrotizing pancreatitis in mice: protective effects of proglumide, benzotript, and secretin. Gastroenterology 1985;88:1192–204. [DOI] [PubMed] [Google Scholar]
- 33.Niederau C, Liddle RA, Ferrell LD, et al. Beneficial effects of cholecystokinin-receptor blockade and inhibition of proteolytic enzyme activity in experimental acute hemorrhagic pancreatitis in mice. Evidence for cholecystokinin as a major factor in the development of acute pancreatitis. J Clin Invest 1986;78:1056–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lankisch PG, Goke B, Folsch UR, et al. Influence of secretin on the course of acute experimental pancreatitis in rats. Digestion 1983;26:187–91. [DOI] [PubMed] [Google Scholar]
- 35.Evander A, Lundquist I, Ihse I. Influence of gastrointestinal hormones on the course of acute experimental pancreatitis. Hepatogastroenterology 1982;29:161–6. [PubMed] [Google Scholar]
- 36.Marino CR, Matovcik LM, Gorelick FS, et al. Localization of the cystic fibrosis transmembrane conductance regulator in pancreas. J Clin Invest 1991;88:712–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freedman SD, Kern HF, Scheele GA. Pancreatic acinar cell dysfunction in CFTR(−/−) mice is associated with impairments in luminal pH and endocytosis. Gastroenterology 2001;121:950–7. [DOI] [PubMed] [Google Scholar]
- 38.Lerch MM, Saluja AK, Runzi M, et al. Luminal endocytosis and intracellular targeting by acinar cells during early biliary pancreatitis in the opossum. J Clin Invest 1995;95:2222–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noble MD, Romac J, Vigna SR, et al. A pH-sensitive, neurogenic pathway mediates disease severity in a model of post-ERCP pancreatitis. Gut 2008;57:1566–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ko SB, Mizuno N, Yatabe Y, et al. Corticosteroids correct aberrant CFTR localization in the duct and regenerate acinar cells in autoimmune pancreatitis. Gastroenterology 2010;138:1988–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhoomagoud M, Jung T, Atladottir J, et al. Reducing extracellular pH sensitizes the acinar cell to secretagogue-induced pancreatitis responses in rats. Gastroenterology 2009;137:1083–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ishiguro H, Naruse S, Kitagawa M, et al. Chloride transport in microperfused interlobular ducts isolated from guinea-pig pancreas. J Physiol 2002;539:175–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haanes KA, Novak I. ATP storage and uptake by isolated pancreatic zymogen granules. Biochem J 2010;429:303–11. [DOI] [PubMed] [Google Scholar]
- 44.Ishiguro H, Naruse S, Kitagawa M, et al. Luminal ATP stimulates fluid and HCO3- secretion in guinea-pig pancreatic duct. J Physiol 1999;519(Pt 2):551–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dery O, Corvera CU, Steinhoff M, et al. Proteinase-activated receptors: novel mechanisms of signaling by serine proteases. Am J Physiol 1998;274:C1429–52. [DOI] [PubMed] [Google Scholar]
- 46.Mooren F, Hlouschek V, Finkes T, et al. Early changes in pancreatic acinar cell calcium signaling after pancreatic duct obstruction. J Biol Chem 2003;278:9361–9. [DOI] [PubMed] [Google Scholar]
- 47.Nguyen TD, Moody MW, Steinhoff M, et al. Trypsin activates pancreatic duct epithelial cell ion channels through proteinase-activated receptor-2. J Clin Invest 1999;103:261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alvarez C, Regan JP, Merianos D, et al. Protease-activated receptor-2 regulates bicarbonate secretion by pancreatic duct cells in vitro. Surgery 2004;136:669–76. [DOI] [PubMed] [Google Scholar]
- 49.Laukkarinen JM, Weiss ER, van Acker GJ, et al. Protease-activated receptor-2 exerts contrasting model-specific effects on acute experimental pancreatitis. J Biol Chem 2008;283:20703–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Namkung W, Han W, Luo X, et al. Protease-activated receptor 2 exerts local protection and mediates some systemic complications in acute pancreatitis. Gastroenterology 2004;126:1844–59. [DOI] [PubMed] [Google Scholar]
- 51.Sharma A, Tao X, Gopal A, et al. Protection against acute pancreatitis by activation of protease-activated receptor-2. Am J Physiol Gastrointest Liver Physiol 2005;288:G388–95. [DOI] [PubMed] [Google Scholar]
- 52.Singh VP, Bhagat L, Navina S, et al. Protease-activated receptor-2 protects against pancreatitis by stimulating exocrine secretion. Gut 2007;56:958–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Voronina S, Longbottom R, Sutton R, et al. Bile acids induce calcium signals in mouse pancreatic acinar cells: implications for bile-induced pancreatic pathology. J Physiol 2002;540:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gerasimenko JV, Flowerdew SE, Voronina SG, et al. Bile acids induce Ca2+ release from both the endoplasmic reticulum and acidic intracellular calcium stores through activation of inositol trisphosphate receptors and ryanodine receptors. J Biol Chem 2006;281:40154–63. [DOI] [PubMed] [Google Scholar]
- 55.Kim JY, Kim KH, Lee JA, et al. Transporter-mediated bile acid uptake causes Ca2+-dependent cell death in rat pancreatic acinar cells. Gastroenterology 2002;122:1941–53. [DOI] [PubMed] [Google Scholar]
- 56.Fischer L, Gukovskaya AS, Penninger JM, et al. Phosphatidylinositol 3-kinase facilitates bile acid-induced Ca(2+) responses in pancreatic acinar cells. Am J Physiol Gastrointest Liver Physiol 2007;292:G875–86. [DOI] [PubMed] [Google Scholar]
- 57.Raraty M, Ward J, Erdemli G, et al. Calcium-dependent enzyme activation and vacuole formation in the apical granular region of pancreatic acinar cells. Proc Natl Acad Sci U S A 2000;97:13126–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kruger B, Albrecht E, Lerch MM. The role of intracellular calcium signaling in premature protease activation and the onset of pancreatitis. Am J Pathol 2000;157:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hietaranta AJ, Singh VP, Bhagat L, et al. Water immersion stress prevents caerulein-induced pancreatic acinar cell nf-kappa b activation by attenuating caerulein-induced intracellular Ca2+ changes. J Biol Chem 2001;276:18742–7. [DOI] [PubMed] [Google Scholar]
- 60.Venglovecz V, Rakonczay Z Jr, Ozsvari B, et al. Effects of bile acids on pancreatic ductal bicarbonate secretion in guinea pig. Gut 2008;57:1102–12. [DOI] [PubMed] [Google Scholar]
- 61.Rerides G, Laukkarinen JM, Vassileva G, et al. Biliary acute pancreatitis in mice is mediated by the G-protein-coupled cell surface bile acid receptor Gpbar1. Gastroenterology 2010;138:715–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meier PJ . Molecular mechanisms of hepatic bile salt transport from sinusoidal blood into bile. Am J Physiol 1995;269: G801–12. [DOI] [PubMed] [Google Scholar]
- 63.Ignath I, Hegyi P, Venglovecz V, et al. CFTR expression but not Cl-transport is involved in the stimulatory effect of bile acids on apical Cl-/HCO3- exchange activity in human pancreatic duct cells. Pancreas 2009;38:921–9. [DOI] [PubMed] [Google Scholar]
- 64.Lerch MM, Weidenbach H, Hernandez CA, et al. Pancreatic outflow obstruction as the critical event for human gall stone induced pancreatitis. Gut 1994;35:1501–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alvarez C, Fasano A, Bass BL. Acute effects of bile acids on the pancreatic duct epithelium in vitro. J Surg Res 1998;74:43–6. [DOI] [PubMed] [Google Scholar]
- 66.Alvarez C, Nelms C, D’Addio V, et al. The pancreatic duct epithelium in vitro: bile acid injury and the effect of epidermal growth factor. Surgery 1997;122:476–83; discussion 483–4. [DOI] [PubMed] [Google Scholar]
- 67.Apte MV, Pirola RC, Wilson JS. Fatty acid ethyl esters-alcohol’s henchmen in the pancreas? Gastroenterology 2006;130:992–5. [DOI] [PubMed] [Google Scholar]
- 68.Petersen OH, Sutton R. Ca2+ signalling and pancreatitis: effects of alcohol, bile and coffee. Trends Pharmacol Sci 2006;27:113–20. [DOI] [PubMed] [Google Scholar]
- 69.Deng X, Wang L, Elm MS, et al. Chronic alcohol consumption accelerates fibrosis in response to cerulein-induced pancreatitis in rats. Am J Pathol 2005;166:93–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Criddle DN, Raraty MG, Neoptolemos JP, et al. Ethanol toxicity in pancreatic acinar cells: mediation by nonoxidative fatty acid metabolites. Proc Natl Acad Sci U S A 2004;101:10738–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Criddle DN, Sutton R, Petersen OH. Role of Ca2+ in pancreatic cell death induced by alcohol metabolites. J Gastroenterol Hepatol 2006;21 (Suppl 3):S14–17. [DOI] [PubMed] [Google Scholar]
- 72.Werner J, Laposata M, Fernandez-del Castillo C, et al. Pancreatic injury in rats induced by fatty acid ethyl ester, a nonoxidative metabolite of alcohol. Gastroenterology 1997;113:286–94. [DOI] [PubMed] [Google Scholar]
- 73.Laposata EA, Lange LG. Presence of nonoxidative ethanol metabolism in human organs commonly damaged by ethanol abuse. Science 1986;231:497–9. [DOI] [PubMed] [Google Scholar]
- 74.Gukovskaya AS, Mouria M, Gukovsky I, et al. Ethanol metabolism and transcription factor activation in pancreatic acinar cells in rats. Gastroenterology 2002; 122:106–18. [DOI] [PubMed] [Google Scholar]
- 75.Blanco PG, Salem RO, Ollero M, et al. Ethanol administration to cystic fibrosis knockout mice results in increased fatty acid ethyl ester production. Alcohol Clin Exp Res 2005;29:2039–45. [DOI] [PubMed] [Google Scholar]
- 76.Sharer N, Schwarz M, Malone G, et al. Mutations of the cystic fibrosis gene in patients with chronic pancreatitis. N Engl J Med 1998;339:645–52. [DOI] [PubMed] [Google Scholar]
- 77.Wu H, Bhopale KK, Ansari GA, et al. Ethanol-induced cytotoxicity in rat pancreatic acinar AR42J cells: role of fatty acid ethyl esters. Alcohol Alcohol 2008;43:1–8. [DOI] [PubMed] [Google Scholar]
- 78.Bunce KT, Parsons ME. Ethanol-stimulated acid secretion in the isolated whole stomach of the rat. J Pharm Pharmacol 1980;32:45–8. [DOI] [PubMed] [Google Scholar]
- 79.Irvine WT, Watkin DB, Williams EJ. The mechanism by which alcohol stimulates acid secretion. Gastroenterology 1960;39:41–7. [PubMed] [Google Scholar]
- 80.Llanos OL, Swierczek JS, Teichmann RK, et al. Effect of alcohol on the release of secretin and pancreatic secretion. Surgery 1977;81:661–7. [PubMed] [Google Scholar]
- 81.Treffot MJ, Tiscornia OM, Palasciano G, et al. Chronic alcoholism and endogenous gastrin. Am J Gastroenterol 1975;63:29–32. [PubMed] [Google Scholar]
- 82.Yamamoto A, Ishiguro H, Ko SB, et al. Ethanol induces fluid hypersecretion from guinea-pig pancreatic duct cells. J Physiol 2003;551:917–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kolbel CB, Singer MV, Mohle T, et al. Action of intravenous ethanol and atropine on the secretion of gastric acid, pancreatic enzymes, and bile acids and the motility of the upper gastrointestinal tract in nonalcoholic humans. Pancreas 1986;1:211–18. [DOI] [PubMed] [Google Scholar]
- 84.Tiscornia OM, Palasciano G, Dzieniszewski J. Simultaneous changes in pancreatic and gastric secretion induced by acute intravenous ethanol infusion. Effect of atropine and reserpine. Am J Gastroenterol 1975;63:389–95. [PubMed] [Google Scholar]
- 85.Kubota K, Magee DF, Sarles H. Biphasic action of intravenous ethanol on dog exocrine pancreatic secretion. Dig Dis Sci 1983;28:1116–20. [DOI] [PubMed] [Google Scholar]
- 86.Staub JL, Sarles H, Chayvialle JA, et al. Relationship between intravenous ethanol, alcohol-induced inhibition of pancreatic secretion and plasma concentration of immunoreactive pancreatic polypeptide, vasoactive intestinal peptide, and somatostatin in man. Regul Pept 1981;2:61–8. [DOI] [PubMed] [Google Scholar]
- 87.Burgoyne RD, Morgan A. Secretory granule exocytosis. Physiol Rev 2003;83:581–632. [DOI] [PubMed] [Google Scholar]
- 88.Aho HJ, Nevalainen TJ. Experimental pancreatitis in the rat. Ultrastructure of sodium taurocholate-induced pancreatic lesions. Scand J Gastroenterol 1980;15:417–24. [DOI] [PubMed] [Google Scholar]
- 89.Petersen OH, Tepikin AV, Gerasimenko JV, et al. Fatty acids, alcohol and fatty acid ethyl esters: toxic Ca2+ signal generation and pancreatitis. Cell Calcium 2009;45:634–42. [DOI] [PubMed] [Google Scholar]
- 90.Verma DD, Levchenko TS, Bernstein EA, et al. ATP-loaded immunoliposomes specific for cardiac myosin provide improved protection of the mechanical functions of myocardium from global ischemia in an isolated rat heart model. J Drug Target 2006;14:273–80. [DOI] [PubMed] [Google Scholar]