Abstract
Background:
The Health Directors of the US Affiliated Pacific Islands (USAPI) declared a State of Emergency due to epidemic proportions of lifestyle diseases: cancer, obesity and other non-communicable diseases (NCDs) in 2010. This paper describes the development, implementation, and evaluation of a USAPI policy, system and environment (PSE) approach to address lifestyle behaviors associated with cancer and other NCDs.
Methods:
Each of USAPI jurisdictions applied the PSE approach to tobacco and nutrition interventions in a local institution, faith based, or community setting. A participatory community engagement process was utilized to: identify relevant deleterious health behaviors in the population, develop PSE interventions to modify the context in which the behavior occurs in a particular setting, implement the PSE intervention through five specified activities, and evaluate the activities and behavior change associated with the intervention.
Results:
PSE interventions have been implemented in all USAPI jurisdictions. Current human and financial resources have been adequate to support the interventions. Process and behavior change evaluations have not been completed and is ongoing. Personnel turnover and maintaining the intervention strategy in response due to shifting community demands has been the biggest challenge in one site.
Conclusion:
From 2014 through 2016 the PSE approach has been used to implement PSE interventions in all USAPI jurisdictions. The intervention evaluations have not been completed. The PSE intervention is novel and has the potential to be a scalable methodology to prevent cancer and modify NCD risk in the USAPI and small states.
Keywords: Policy, system and environment change; Disparity; Pacific; Nutrition; Tobacco; Cancer prevention
1. Introduction
In 2010, the Directors of Health of the United States Affiliated Pacific Islands (USAPI) declared a Regional State of Emergency due to epidemic proportions of lifestyle diseases: cancer, obesity, and other non-communicable diseases (NCDs) [1]. The declaration was put forth to mobilize resources and bring greater focus on prevention, screening, and treatment of cancer and NCDs. Between 2010 and 2016, many of the local cancer and NCD programs were reorganized, additional funding was found, the output and performance of the health programs were heavily scrutinized, and new methods to more effectively address the cancer, obesity, and NCD epidemic were sought.
Lifestyle diseases are associated with prolonged exposure to three modifiable lifestyle behaviors: smoking, unhealthy diets, and physical inactivity. In the USAPI, several public health and population health measures have been employed to decrease exposure to unhealthy lifestyle behaviors and to promote healthy behaviors. These include interventions based on the individual (health counseling, clinical interventions) and health policy interventions (tobacco tax, quality food control, health education in schools). Interventions that address the social determinants of health (poverty, population education achievement, unhealthy environments) have been difficult to implement and were pursued to a much lesser extent.
The USAPI health services in partnership with the University of Hawai’i, and supported by Centers for Disease Control and Prevention (CDC) grants, is developing and evaluating a novel approach to modify lifestyle behaviors and thereby reduce the USAPI population risk for cancer, obesity and NCDs. This paper discusses the USAPI experience with the development and implementation of the policy, systems, and environment (PSE) approach to changing deleterious lifestyle behaviors.
The USAPI are composed of two United States (US) Territories (American Samoa (AS) and Guam), the Commonwealth of the Northern Mariana Islands (CNMI), and three sovereign countries, the Federated States of Micronesia (FSM), Republic of Palau (ROP), and the Republic of the Marshall Islands (RMI). The FSM, ROP, and RMI are freely associated with the US through their respective treaties called Compacts of Free Association (COFA). The COFA describe the political, economic, and military relationship between the US and these three sovereign island nations.
There are over 450,000 people in the USAPI [2]. The USAPI is culturally diverse with at least 12 main languages spoken. The economies and stages of development of the USAPI vary widely. In 2016, the FSM was classified by the World Bank as a low-middle income country; the RMI, ROP, and AS were middle income countries, and the CNMI and Guam are considered high income countries.
Life expectancy at birth in the USAPI are shorter than those living in the US [3]. (Table 1)
Table 1.
Life Expectancy at Birth in the USAPI.
| USAPI Jurisdiction | Life expectancy at birth |
|---|---|
| American Samoa | 72.7 (2012) |
| Commonwealth of the Northern Mariana Islands | 76.9 (2010) |
| Federated States of Micronesia | 70 (2010) |
| Guam | 78.5 (2012) |
| Republic of Palau | 64 (2012) |
| Republic of the Marshall Islands | 71.8 (2011) |
| US | 79 (2012) |
The World Health Organization (WHO) estimates that 75% of deaths in the Pacific are caused by NCDs [4]. Notably, cancer is now the second most common cause of death in nearly all USAPI jurisdictions with 37% of cancer patients dying within 5 years of diagnosis [5]. Currently, the top two cancers in the islands are breast and lung/bronchus [2]. In Guam, the lung cancer mortality rate of Micronesians is more than double the US rate.
Approximately 83% of cancers in the USAPI are associated with tobacco or obesity/overweight. Of the top five cancers in the USAPI, three are linked to tobacco use and second hand smoke (lung/bronchus, colorectal, liver) and four cancers are associated with obesity/overweight (breast, prostate, colorectal, liver) [2]. Whereas, the adult tobacco current smoker rates are 18% in the US, the USAPI smoker rates range from 17% to 57% [6]. Youth smoker rates range from 14% of females in American Samoa to 58% of males in the Republic of Palau [7].
In 2014, as noted by the World Health Organization global health statistics, of the top 12 countries with the highest prevalence of obesity among adult males, nine were in the Pacific Region, of which three were part of the USAPI [8]. The adult composite overweight and obesity prevalence range from 60% in Pohnpei to 94% in American Samoa [9–14]. The overweight and obesity prevalence of high school youth range from 26.5% in the Republic of the Marshall Islands to 60.3% in American Samoa [15–22]. Obesity prevention is a crucial issue for cancer control in the USAPI.
2. Policy, system and environment – methods
2.1. Defining the policy, system and environment approach
A policy, systems and environmental (PSE) approach in the USAPI aims to reduce the risk for cancer and other NCDs. The PSE approach is population based and includes: a) identifying a deleterious health behavior that is associated with an increased risk for cancers and NCDs; b) identifying the setting where the behavior is prevalent; c) identifying PSE interventions which are stakeholder developed, community relevant and sustainable to change the behavior; d) implementing the intervention through five specific activities in a particular setting (assessments, garnering community support, training/education programs, media promotion, signage); e) monitoring the progress of the activities through process evaluation metrics; and f) assessing the change in the targeted health behavior in the respective setting. (Table 2)
Table 2.
USAPI PSE Approach (Intervention Selection, Implementation and Evaluation).
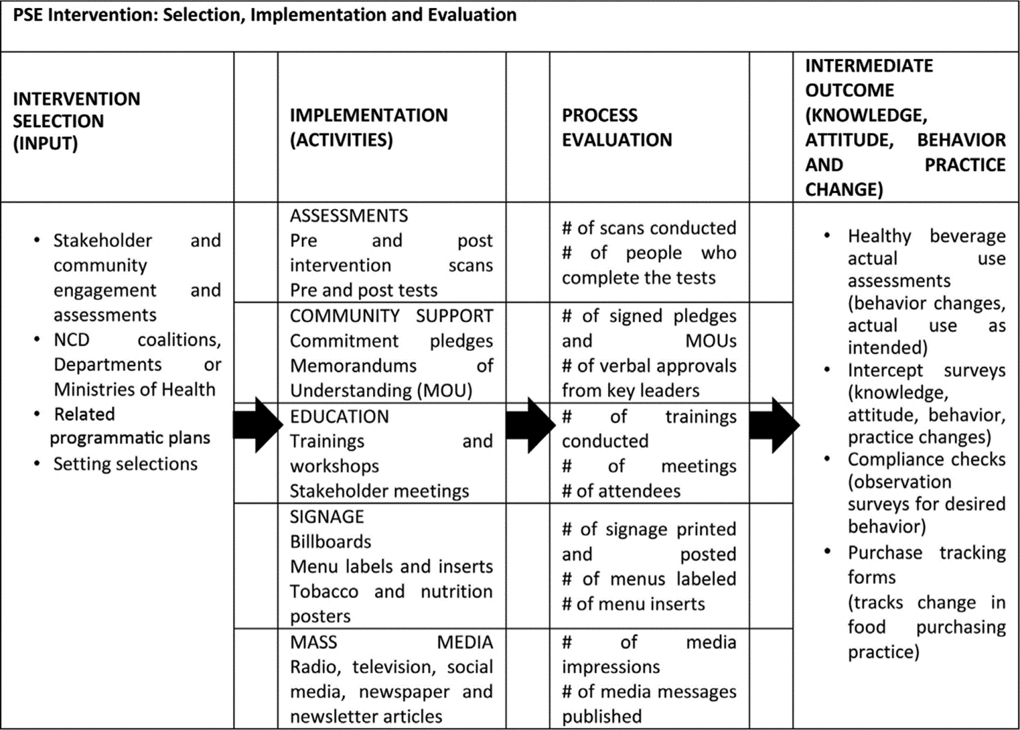
|
The setting for the PSE intervention may be the community (geographic, ethnic, faith based, gender based, business); a system (school, health-care complex, institution); or a natural/built environment. A defined PSE intervention is implemented to modify the context in which health behaviors are made, i.e., to make healthy behaviors the default choice, to make healthy choices possible and desirable, and/or to make an unhealthy behavior difficult within the target setting.
The selected PSE intervention is often integrated into an existing infrastructure and is practical, available, and accessible to all community members [23]. Several PSE communities in the US have formed coalitions to advance PSE strategies since 1990 [24]. The PSE concept is drawn from behavior change theory and social ecology models of health [25].
A characteristic of PSE change is that all members of that community or system have equal exposure to the modified environment irrespective of their socio-economic standing, education, or culture. Further, an individual community member would necessarily have to inconvenience themselves to avoid the change created by the intervention.
A PSE intervention may be policy, systems or environmentally focused. Policies may take the form of community or church rules or regulations that define appropriate or inappropriate health behaviors in their respective settings (e.g., no smoking on the church property). Systems level interventions refer to making structural or organizational changes that influence the culture of behavior within a system (e.g., candy machines are banned in the hospital). Environmental interventions are those which change the natural or built environment to make healthy choices possible and practical (e.g., building parks, bikeways, safe walkways). Policy and structural interventions are often linked to affect changes in the desired setting.
2.2. Examples of PSE interventions
Each of the USAPI jurisdictions applied the PSE approach to tobacco and nutrition interventions. The interventions included healthy beverages only (water and coconut only) at faith based gatherings, no salt products on restaurant tables, providing and encouraging exercise time during work hours at government buildings, providing signage and peer monitoring of no smoking zones at public buildings, and developing business policies to increase the amount and location of fresh local produce in local stores.
In Yap State of the Federated States of Micronesia, the government hospital feeding program implemented a healthy food voucher policy. Patients and their caregivers were issued vouchers to purchase fresh local food and produce from the local stores, instead of being provided canned tuna, canned mackerel, and white rice bought from the local stores.
A systems change can be seen in the Republic of Palau when the Ministry of Education provided healthy school lunches for all their public school students.
An environmental change is evident through the poker rooms’ compliance to the smoke-free air law on the island of Saipan in the Commonwealth of the Northern Mariana Islands.
2.3. Process and intermediate outcome evaluation
The evaluation for PSE interventions in these jurisdictions aimed to expand the evidence for the effective interventions, such as increased access to healthy beverages at churches and compliance in smoke-free environments. The horizon for PSE interventions and evaluation was two years (2014–2016).
The primary outcomes of interest were: a) whether the respective PSE interventions influenced the desired health behavior change; b) actual use, which is defined by the CDC as the number of people who use an enhanced environment or system to support improved health as intended. [26] Actual use was determined by the number of individuals who were reached/impacted as a result of the intervention, such as there was a change in their knowledge, attitude or behavior. Evaluation of the USAPI PSE approach included process evaluation of the five activities (noted in Table 2).
With the support of an evaluator, an evaluation plan and tools were created with the staff from these jurisdictions. This allowed for the incorporation of technical evaluation criteria and critical information from the local level that informed the feasibility and appropriateness of the evaluation efforts. Purchasing of produce and healthy menu items were identified to be tracked. Actual use assessments were planned for the healthy beverages at the churches. The lunch menus for the schools were tracked. Knowledge, attitude, behavior and practice (KABP) or intercept surveys were administered for the nutrition interventions. Compliance checks and employee and intercept surveys were administered for the tobacco intervention. The intent of these evaluations was to build evidence on interventions implemented at new settings.
3. Results
The evaluation results are not complete as of date. Examples of process evaluation metrics and intermediate outcomes evaluation, which have been completed are noted in Table 3. The evaluation process is ongoing.
Table 3.
PSE Intervention and Evaluation in American Samoa and Guam, August 2017.
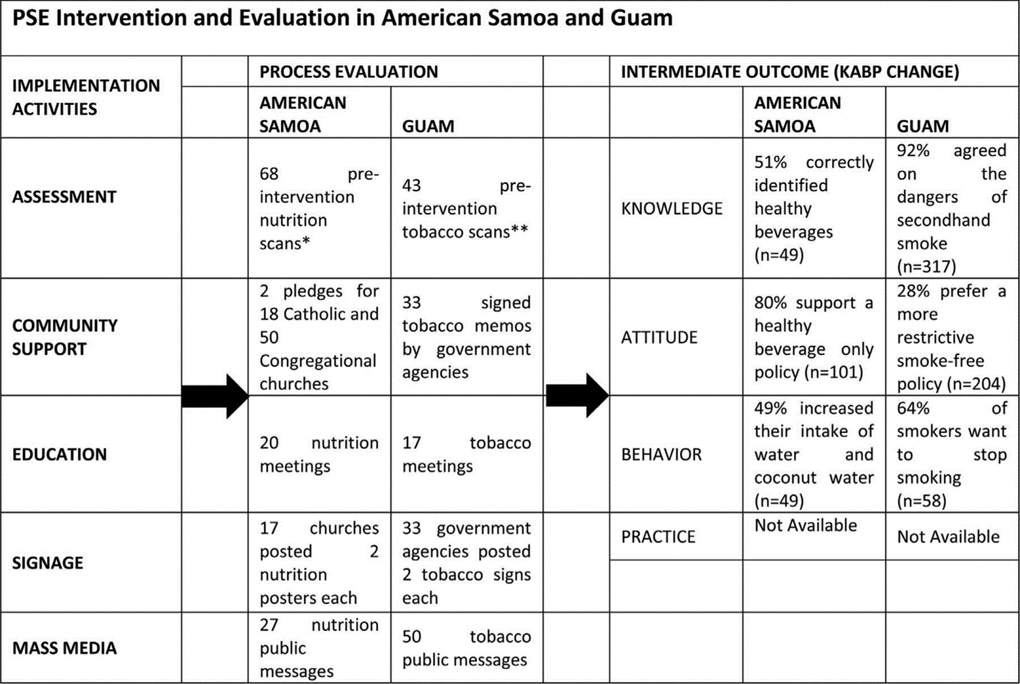
|
Pre-intervention scans are PSE assessments done prior to implementing the PSE intervention. Nutrition observations may include beverages being served at the target setting, visible sugar-sweetened beverages, and knowledge of existing policies. **Tobacco observations may include tobacco signage at the target setting, visible smokers and cigarette butts as well as knowledge of existing tobacco policies.
3.1. Observations
A dedicated, paid, half-time staff member who has the vocational and/or positional influence with the community is essential. Financial and logistic resources are required for travel to the various communities, hosting meetings, utilizing radio and communication, and creating signage. These costs, paid through a US Federal grant, were on average about $US 27,000 annually. The community and health systems in several of the low resource settings noted that these costs could be managed by the community over time.
The PSE changes were identified and developed by the stakeholder communities, which promoted community support. In the USAPI, the indigenous cultural norms for community decision making and organizing community action were congruent with the community engaged processes of the PSE approach. Training of staff members was not found to be a complex or long process, although local staff turnover was high in some jurisdictions. Expensive technologies are not required and success of the intervention is not dependent on higher education attainment of the community or significant financial support by the community.
The community and health systems provide the human resources to implement and sustain the intervention. Support from the government and local health services, in the form of in-kind and political encouragement, are necessary to reinforce the credibility of the PSE efforts and to provide medical and evaluation expertise.
4. Discussion
4.1. Opportunities
Implementation and evaluation of PSE change in the USAPI will hopefully result in the development of evidence based PSE strategies that lead to healthy lifestyles choices and behaviors. The PSE interventions may then be scaled to different communities and tested in other settings and small countries or nations.
The health impact for tailored PSE interventions has great potential. As an example, on small island nations, the imported western non-nutritious foods and carcinogens (tobacco) may greatly influence lifestyle behavior and healthy choices. At the community and village level, PSE interventions could change the context (supply and demand) for businesses as they purchase and sell food, beverages and tobacco.
Other practical applications for the PSE approach include development of interventions to affect health care seeking behavior, instead of modifiable lifestyle behaviors, for cancer screenings and vaccinations. The environment for cancer screenings (clinical exams and mammography) and vaccinations could be promoted at local churches and villages through structuring a scheduled cancer prevention day at the local churches once every three months. During this fixed interval, which is an environmental change, the church community and health services support a cancer screening week (colon, breast, cervical, skin) on site for all its members.
4.2. Challenges
The population impact of PSE change strategies is dependent on several factors: the effect size of the intervention on a particular health outcome, the intensity and frequency of exposure to the intervention’s health benefits, and the number of people who are exposed to the intervention [24,27]. In small populations with multi-variables that may be associated with cancer and NCD risk, it may be very difficult to isolate the effect size of a particular PSE intervention.
The two year experience with the PSE approaches is relatively new in the USAPI. The PSE approaches and personnel are in part supported with US grant funds. Should the particular grant funding cease, it is unclear which of the PSE interventions will be sustainable in the small island environments.
5. Conclusions
The process and intermediate outcome measures for the USAPI PSE interventions have not been completed. Thereby, it is premature to draw any major conclusions.
We observed that USAPI PSE approach utilizes a community based participatory approach which incorporated knowledge and wisdom of the indigenous and/or local culture, and utilizes expertise and funding from external stakeholders. PSE changes that evolved from community engagement and assessments appear to be resource, and culturally appropriate for the respective small island states. The researchers are working towards PSE interventions which require minimal external stakeholder support.
The USAPI PSE approach to community health may be a primary strategy to curb the epidemic of cancer and other NCDs at the population level in the USAPI. The PSE approach would complement current public health programs. Evidence for PSE interventions that are effective and sustainable are underway.
Acknowledgements
This publication is supported by the Centers for Disease Control and Prevention (CDC) Racial and Ethnic Approaches to Community Health Cooperative Agreement (U58 DP005810).
We thank all of our partners. This project would not be possible without their hard work and effort of Evonne Sablan, the departments/ministries of health, and their coalitions and partners in American Samoa, Commonwealth of the Northern Mariana Islands, Federated States of Micronesia (National, Chuuk, Kosrae, Pohnpei and Yap), Guam, Republic of the Marshall Islands, and Republic of Palau, as well as the Cancer Council of the Pacific Islands.
Note: The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
References
- [1].PIHOA, Declaring a Regional State of Health Emergency Due to the Epidemic of Non-Communicable Diseases in the United States-Affiliated Pacific Islands, in Board Resolution #48–01, P.I.H.O. Association, Editor. 2010.
- [2].Buenconsejo-Lum LE, Navasca D, Jeong Y, Wong E, Torris P, Palafox NA, Cancer in the US Affiliated Pacific Islands 2007–2012, (2014).
- [3].World Health Organization. Country Profiles. World Health Organization. [Google Scholar]
- [4].Pacific Islands Non-Communicable Disease Roadmap. July 12, 2014. 01/27/2017]; Available from: http://www.worldbank.org/en/news/feature/2014/07/11/pacific-islands-non-communicable-disease-roadmap.
- [5].USAPI Pacific Regional Comprehensive Cancer Control Plan 2012–2017, Department of Family Medicine and Community Health, John A. Burns School of Medicine, University of Hawaii, Manoa, 2015. (p. 45.). [Google Scholar]
- [6].WHO, Noncommunicable Diseases in the Western Pacific Region: A Profile, (2012).
- [7].Kessaram T, et al. , Tobacco smoking in islands of the pacific region, 2001–2013, Prev. Chronic Dis 12 (2015) E212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].World Health Organization Global Health Observatory Data – Overweight and Obesity, (2014).
- [9].Aitaoto N, Ichiho HM, Assessing the health care system of services for non-communicable diseases in the US-affiliated Pacific Islands: a Pacific regional perspective, Hawaii J. Med. Public Health 72 (5 Suppl 1) (2013) 106–114. [PMC free article] [PubMed] [Google Scholar]
- [10].Guam Department of Public Health and Social Services and the Non-Communicable Disease Consortium, Guam Non-Communicable Disease Strategic Plan 2014–2018, Mangilao, Guam, 2013. [Google Scholar]
- [11].WHO, Federated States of Micronesia (Chuuk) NCD Risk Factors STEPS Report 2006, (2006).
- [12].W.H. Organization, Federated States of Micronesia (Pohnpei) NCD Risk Factors STEPS Report, WHO Western Pacific Region, Suva, Fiji, 2008. [Google Scholar]
- [13].World Health Organization, Federated States of Micronesia (Yap) NCD Risk Factors STEPS Report, WHO Western Pacific Region, Suva, Fiji, 2009. [Google Scholar]
- [14].Appanaitis I, Republic of Palau, Ministry of Health: National Health Profile 2013, Office of Health Policy Research and Development, 2014.
- [15].American Samoa Youth Risk Behavior Surveillance, (2011).
- [16].Commonwealth of the Northern Mariana Islands Youth Risk Behavior Surveillance, (2015).
- [17].Kosrae Rapid High School Survey, (2015).
- [18].Pohnpei Regional Health Surveillance Survey, (2015).
- [19].Yap 2012 Community Health Assessment, (2012).
- [20].Guam Youth Risk Behavior Surveillance, (2015).
- [21].Palau Youth Risk Behavior Surveillance, (2015).
- [22].Republic of the Marshall Islands Global Youth Tobacco Survey (plus), (2016).
- [23].Frieden TR, A framework for public health action: the health impact pyramid, Am. J. Public Health 100 (4) (2010) 590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bunnell R, et al. , Fifty communities putting prevention to work: accelerating chronic disease prevention through policy, systems and environmental change, J. Commun. Health 37 (5) (2012) 1081–1090. [DOI] [PubMed] [Google Scholar]
- [25].Egger G, Swinburn B, An ecological approach to the obesity pandemic, BMJ 315 (7106) (1997) 477–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Soler R, Actual Use Assessments [PowerPoint Slides], Centers for Disease Control and Prevention – Division of Community Health, 2015.
- [27].Robert C, It’s effect size, stupid: what effect size is and why it is important, Annual Conference of the British Educational Research Association, University of Exeter, England, 2002. [Google Scholar]


