KEY POINTS
The Kidney Health Strategic Clinical Network (KH SCN) is dedicated to improving the kidney health of all Albertans.
This is achieved through innovation facilitated by frequent, purposeful collaboration with patients and families, health care service providers and researchers.
Priority projects have led to positive change, through extensive consultation following proven change management principles; they require ongoing commitment by all partners.
Investing sufficient time to ensure full endorsement of the KH SCN’s roadmap and projects by the broad kidney community, and providing comprehensive data on the state of the disease and clinical practices across the province, have been keys to success.
Chronic kidney disease (CKD) affects 12% of adults in Alberta,1 encompassing a spectrum of disease from mild and asymptomatic to end-stage kidney disease characterized by a dramatic reduction in quality of life, adverse clinical outcomes and substantial strain on patients and their caregivers. Although most patients with CKD are managed in primary care,2 more advanced disease requires specialized care that may include dialysis, transplantation or conservative symptom management. The annual cost of health care in Alberta is $14 600 per patient with CKD,3 and dialysis costs per patient vary from $55 000 (peritoneal dialysis) to $100 000 (hemodialysis) annually, with lower costs for a kidney transplant ($22 000 annually after the first year).4 The direct and indirect financial burden to patients and their caregivers is also considerable.5 The prevalence of Stage 3 and 4 CKD has increased by 7.1% over the past 2 years,6 making it a priority to prevent and manage CKD, optimize health outcomes and ensure sustainability of the health care system. The Kidney Health Strategic Clinical Network (KH SCN; www.ahs.ca/khscn) was launched in January of 2016 to provide a unique platform where patients, clinicians, health care administrators, front-line staff, health researchers and policy-makers jointly identify, prioritize and launch new initiatives.
The KH SCN structure builds on lessons learned from SCNs that were established earlier and comprises a Leadership Team, a direction-setting 40-member Core Committee and the Scientific Office that ensures activities are evidence-based, coordinated and appropriately evaluated. The KH SCN incorporates and partners with several well-established entities. Provincial delivery of specialized kidney care is through Alberta Kidney Care, which comprises the northern and southern programs, and the regional transplant programs, each with existing organizational structures. These entities are foundational, and partnerships are facilitated by dual participation because the members of the Leadership Team are members of the KH SCN Core Committee and vice versa.
The Alberta kidney research community is internationally recognized, and includes Alberta Kidney Disease Network and key participation with the Can-SOLVE CKD Network (www.cansolveckd.ca). Leveraging these existing research resources has allowed integration of best evidence and research practices for all KH SCN activities. The SCN has strong partnerships with patient and caregiver advisors representing the full spectrum of kidney disease and geography, as well as with the Kidney Foundation of Canada. These partners are actively engaged, participating on our Core Committee and numerous projects to respect and integrate their voices. Through the Patient and Community Engagement Research program, the KH SCN is building capacity for patient-directed research as patients become part of the research team.7
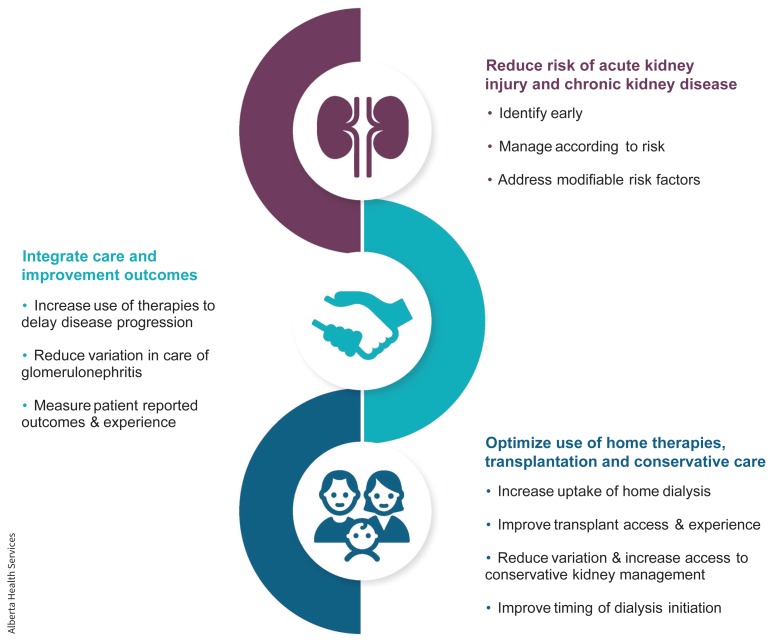
The strong foundation of collaborative relationships facilitated the development of the Transformational Roadmap (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.190573/-/DC1) and rapid project execution by the KH SCN. Specific strengths include research on patient priorities (www.cansolveckd.ca/research/theme-1/kidney-check), robust population-based data on the incidence and prevalence of CKD,8,9 uptake of evidence-based treatment, and existing initiatives in research, quality improvement and patient advocacy. The SCN’s Core Committee obtained input from more than 350 people to prioritize strategies by importance to patients, opportunity to improve patient outcomes and potential to improve efficiency in the health care system. This 10-month process included examination of available data and evidence, consultations with leaders and front-line staff, surveys to gather stakeholder feedback on proposed priorities and use of priority-setting tools in face-to-face meetings of the committee. The strategic goals and priorities are shown in the figure. The Transformational Roadmap was recently updated (summary, Appendix 2, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.190573/-/DC1) to reflect achievements as described below and to reflect new priorities in prevention, integrating pediatric care and better transitions.
Strategic priorities of the Kidney Health Strategic Clinical Network (KH SCN).
Image courtesy of Alberta Health Services
The first key achievement was the Starting dialysis on Time, At home, on the Right Therapy (START)10 project, a partnership with Alberta Kidney Care. Its goals were to achieve a 5% absolute increase in the proportion of patients who received peritoneal dialysis within 180 days of starting dialysis province-wide, and a 5% absolute reduction in the proportion of outpatients who started dialysis with an estimated glomerular filtration rate greater than 9.5 mL/min/1.73 m2. The process included a structured review embedded into the patient pathway to ensure patients were appropriately identified, assessed, educated and supported when choosing peritoneal dialysis. A custom data system was implemented provincially that captured reliable and timely data, and a quality improvement process addressed areas of variability. The proportion of patients who received peritoneal dialysis within the first 180 days increased from 25% to 32% (p < 0.001) with 6 of 7 participating sites showing growth. The proportion of outpatients starting dialysis earlier than the guideline decreased from 16% to 13%, with 3 sites exceeding their goals. Continuing efforts include a recent Physician Indicator report that provided customized audit and feedback data to each physician, and an opportunity for further physician discussion is planned. One difficulty encountered throughout this project has been finding and sustaining the resources required for detailed data collection.
A second key achievement has been the Living Donor Kidney Transplant initiative. The KH SCN launched a multifaceted initiative to optimize rates of living donor kidney transplants. Education for patients and providers has been standardized across programs to ensure consistency. The 2 provincial transplant programs in northern and southern Alberta are structured differently, which has presented a challenge to standardization of services. However, there have been successes. Criteria for reimbursement of costs for donors have been revised to be more comprehensive, and a policy for donor wage replacement has been implemented for eligible employees of Alberta Health Services. The donor workup process continues to be optimized. Other KH SCN projects are outlined in Appendix 3 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.190573/-/DC1).
A core supporting activity for all priorities is the development of Key Performance Indicators. In partnership with Alberta Kidney Care, the KH SCN has identified indicators to assess system performance and quality of delivery of clinical care. High-quality data are collected and used to monitor quality of care, determine the impact of new strategies, and identify opportunities for future improvement and intervention. Indicators are reviewed and updated by a Key Performance Indicators Committee to ensure alignment with the new priorities in the Transformational Roadmap.
A key lesson throughout has been recognition of the importance of a full and rigorous consultation process to develop a Transformational Roadmap that is fully endorsed by the kidney community and the time required for participants to understand the role of an SCN. Ensuring broad, meaningful physician engagement is critical to overcome potential barriers to deployment of changes to clinical care. Ensuring that priorities and initiatives are co-designed, actionable, acceptable and align with the interests of the operational groups that provide specialized kidney care is fundamental. As in many health care settings, the ongoing dynamic tension between the SCN and clinical operations requires close consultation and collaboration to ensure projects are implementable. Key facilitators include engagement and partnerships with health services researchers, facilitating provision of evidence to inform priority setting, and embedding research principles into evaluation and Key Performance Indicators. Committed, engaged patient advisors and patient advocacy groups were instrumental in identifying priority areas and projects. Finally, leveraging existing regional and provincial organization structures committed to optimizing care and outcomes, including transplant programs and Alberta Kidney Care, provided a foundational element on which to build feasible projects in the KH SCN.
The revised Transformational Roadmap will guide us to further transform kidney care in Alberta, and our first step will be to work with our various partners and committees to operationalize new priorities with updated goals and plans for achievement.
Footnotes
Competing interests: Loreen Gilmour is an employee of Alberta Health Services (AHS). Neesh Pannu and Scott Klarenback are remunerated through a contract with AHS. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Loreen Gilmour contributed substantially to the conception of the work and drafted it. Neesh Pannu and Scott Klarenbach contributed substantially to the design of the work, identified key elements of content, provided specific data related to the key elements and critically revised the work for important intellectual content. All of the authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: Scott Klarenbach and Neesh Pannu are supported by the Division of Nephrology at the University of Alberta. Scott Klarenbach is also supported by the Kidney Health Research Chair.
References
- 1.Arora P, Vasa P, Brenner D. Prevalence estimates of chronic kidney disease in Canada: results of a nationally representative survey. CMAJ 2013;185: E417–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manns B, Tonelli M, Culleton B, et al. ; Alberta Kidney Disease Network. A cluster randomized trial of an enhanced eGFR prompt in chronic kidney disease. Clin J Am Soc Nephrol 2012;7:565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manns B, Hemmelgarn B, Tonelli M, et al. ; Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease. The cost of care for people with chronic kidney disease. Can J Kidney Health Dis 2019;6: 2054358119835521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klarenbach SW, Tonelli M, Chui B, et al. Economic evaluation of dialysis therapies. Nat Rev Nephrol 2014;10:644–52. [DOI] [PubMed] [Google Scholar]
- 5.The burden of out-of-pocket costs for Canadians with kidney failure: 2018 report. Montréal: Kidney Foundation of Canada; updated 2018 Sept. 20. Available: www.kidney.ca/burden (accessed 2019 Apr. 10). [Google Scholar]
- 6.Kidney Health Strategic Clinical Network; Interdisciplinary Chronic Disease Collaboration; Alberta Kidney Disease Network. Prevalence and quality of care in chronic kidney disease: Alberta Kidney Care Report. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-kh-ckd-report-2019.pdf (accessed 2019 Oct. 9). [Google Scholar]
- 7.Shklarov S, Marshall DA, Wasylak T, et al. “Part of the Team”: Mapping the outcomes of training patients for new roles in health research and planning. Health Expect 2017;20:1428–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidney Health Strategic Clinical Network. Prevalence of severe kidney disease and use of dialysis and transplantation across Alberta from 2004 to 2013: Alberta Annual Kidney Care Report. Edmonton: Alberta Health Services; 2015. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-kh-annual-kidney-care-2015.pdf (accessed 2019 Oct. 9). [Google Scholar]
- 9.Kidney Health Strategic Clinical Network. Quality of care in early stage chronic kidney disease 2012–2013: supplementary report to the 2015 Alberta Annual Kidney Care Report. Edmonton: Alberta Health Services; 2015. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-kh-annual-kidney-care-2015-supp.pdf (accessed 2019 Oct 9). [Google Scholar]
- 10.Kidney Health Strategic Clinical Network. The START Project: final report. Edmonton: Alberta Health Services; 2018. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-kh-start-final-report.pdf (accessed 2019 Oct. 9). [Google Scholar]