KEY POINTS
Strategic Clinical Networks (SCNs) are a key resource for Alberta’s health system, help to get evidence into practice, and improve outcomes and health care sustainability on a provincial scale.
The SCNs provide a structure for patients and families, policymakers, clinicians and researchers to collaborate across geographical and institutional boundaries and co-design solutions that address priority health challenges and support transformational change.
Alberta’s SCNs are embedded within a single, province-wide health care system, which enables wide-scale implementation of strategies proven to reduce unwarranted variation and improve care, clinical appropriateness and health outcomes.
The networks support a learning health system by bringing together people, research and innovation, and are delivering a positive return on investment in terms of cumulative savings in the health system.
In April 2009, Alberta Health Services (AHS) became Canada’s first province-wide health system.1 Today, AHS delivers health services to more than 4.3 million people,2 in every part of the province, and remains committed to providing patient-focused, appropriate and high-quality care that is accessible and sustainable for all Albertans.3,4
The decision to move to a fully integrated health system marked the beginning of a decade of health system transformation in Alberta. However, system innovations of this size have no template, and continuous adaptation and learning have been part of AHS’ journey to date. In evolving to a province-wide health system, Alberta’s provincial health authority has worked closely with the provincial government to align policies, plans and priorities, and to develop strategies that address system-wide pressures and needs and support continuous improvement and evidence-informed decision-making.1,5
In 2012, AHS established Strategic Clinical Networks (SCNs) to support these objectives. These multistakeholder teams comprise clinicians, patients, operational leaders and other stakeholders who work together to advance health system innovation and improvement (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.191232/-/DC1). Each network uses data and evidence to identify gaps in care, prioritize areas for improvement, develop and evaluate strategies, and implement solutions that improve health outcomes, access, patient and family experiences, and delivery of health services.5
Clinical networks have existed system-wide in England, Scotland and parts of Australia for nearly 20 years. Although their role and structure within health organizations varies, clinical networks focus on bringing research, evidence and knowledge into clinical practice and actively supporting improvement, innovation and learning in the health system. Typically, clinical networks concentrate on complex issues and challenges that require integrated solutions (e.g., unwarranted variation in care, excessive wait times and health system sustainability).6,7
Clinical networks provide a unique opportunity for operational leaders and managers, clinicians, researchers and other stakeholders to work across geographical, organizational and institutional boundaries on an ongoing basis, to rigorously test changes in practice and implement proven solutions. Working as integrated teams, networks are able to co-design solutions that incorporate the best available evidence, clinical knowledge, patient and family experiences, and input from diverse stakeholders and communities. This bottom–up approach provides an alternative to health system change being driven solely from the top down, which can have a negative effect on clinician engagement and innovation.8
Alberta’s SCNs use a collaborative partnership model in which members bring different skills, experiences and perspectives, and work together to design strategies and solutions that improve outcomes and address priority needs. The networks work closely with clinicians and operational leaders across the province, but their scope and membership extends beyond AHS and includes community and health partners, industry, research institutes, policy-makers and citizens. In this way, the networks help connect AHS to partners across the health spectrum.3,9 This “network model” encourages broad-scale input, partnerships and 360-degree thinking. It also provides a mechanism to encourage ongoing communication, integration and alignment of priorities, and best use of health resources.
Alberta’s SCNs are embedded within a province-wide health system. This structure is advantageous because it enables stakeholders to collaborate across regions, address system-wide challenges and priorities, test solutions in relevant settings (e.g., remote and rural communities) and then, where appropriate, spread and implement practice changes on a provincial scale. A provincial system, including integrated zones, minimizes barriers to collaboration across the system and facilitates sharing of information and implementation of health innovations and quality improvements on a system level.6 Although not responsible for health policy or decision-making, the SCNs work alongside operational leaders to support these functions, suggest actions based on evidence, evaluate outcomes and encourage appropriate use of health resources.
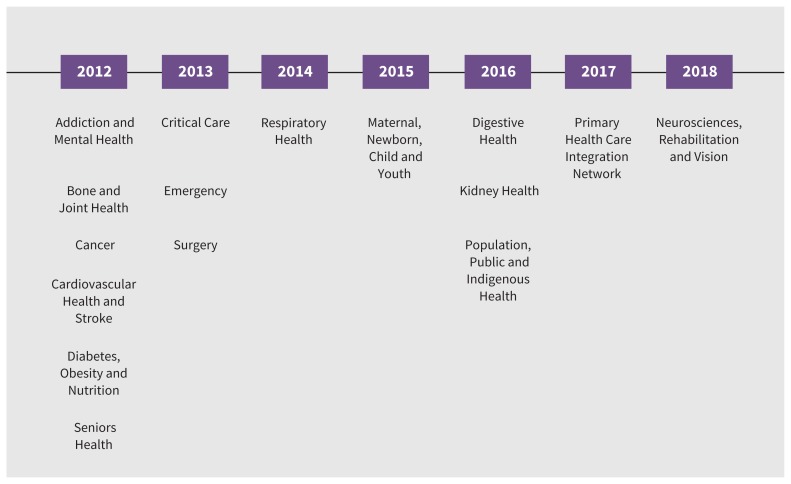
Alberta launched its first SCNs in 2012 with an emphasis on engaging patients, families and the public, and rigorous adherence to implementation science and evidence-based practice.5 Over the past 7 years, the networks have matured and evolved in scope and experience. As they have gained traction, and as provincial capacity allowed, they have expanded to other areas of health (see figure) and have begun tackling increasingly complex challenges that span patient populations and health disciplines such as pain, chronic disease management, transitions in care and access to specialist care.3,6
There are now 16 SCNs in Alberta. Each network is multidisciplinary and operates with a provincial scope and mandate.9 Most networks focus on a specific area of health (e.g., cancer and digestive health); some cross multiple disease areas (e.g., diabetes, obesity and nutrition) or support specific populations (e.g., Indigenous health and maternal, newborn, child and youth health). Others focus on high-cost, high-utilization areas (e.g., surgery and emergency care) or align with provincial programs (e.g., seniors’ health and addiction and mental health).
Each SCN identifies strategic priorities specific to its network and patient population but is guided by a common mission to improve the health of Albertans by bringing together people, research and innovation. Their work aligns with the vision, mission and values of AHS, and supports the operational priorities and business plans of AHS and the Government of Alberta. Alignment with operational goals, the AHS Executive Board and the Government of Alberta helps ensure efficient use of resources and leverages the support, oversight, leadership and executive sponsorship these agencies can provide. All networks operate with a clear understanding that patients and families should be actively involved in setting priorities and co-designing solutions that improve health outcomes and patient and family experiences.
Alberta’s Strategic Clinical Networks (2019).
The SCNs have become an important resource for Alberta’s health system. Their value lies in their ability to work together as integrated teams to address challenges, advance innovation and improve health outcomes on a provincial scale. Appendix 2 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.191232/-/DC1) summarizes the mandate and some of the key structures and processes Alberta’s SCNs use for priority setting, patient engagement and project execution. These processes and structures are helping the SCNs advance innovation within Alberta’s health system and build momentum for future health system improvement.5
The networks and their operational partners have also provided a solid return on investment for all Albertans. The current annual budget for all 16 SCNs is $17 million for core infrastructure and $16 million for projects. An interim analysis of cumulative SCN costs, benefits and value (based on 15 projects that were started between 2012 and Mar. 31, 2018) showed estimated total gross savings of $178.74 million and a cumulative return on investment of $1.54 for every dollar invested.10 This return is based on monetary benefits and reflects direct cost savings ($16.41 million) as well as cost avoidance through improvements in utilization of health services (e.g., reduced length of stay and readmissions to hospital). To date, it is estimated that these improvements have resulted in more than 143 800 hospital bed-days avoided (the equivalent of operating 13 medical inpatient units for 1 year).10 The SCNs have also delivered substantial value through their contributions to patient care, safety and experience; improved health outcomes; and development of clinical pathways. Since 2012, the SCNs have also led or been a major collaborator in clinical research that has brought more than $65 million to Alberta from outside the province. While a clear benefit for Albertans, this also enables the SCNs to align the efforts of academic researchers with network research priorities. Specific outcomes and projects are profiled in a 2019 retrospective report,6 which also highlights critical partnerships that enabled this work.
The articles in this supplement describe this work and reflect on the SCNs’ experiences to date, their strategic priorities, challenges, lessons learned, and some of the processes and partnerships that have enabled progress in specific areas of health. They show the growth and development of SCNs from launch and initial start-up phases to priority setting and project execution and implementation. They describe the importance of aligning priorities with operational leaders, rigorously testing and evaluating outcomes and innovations, and using evidence to spread and scale solutions provincially. The articles also highlight the partnerships that have enabled this work, the importance of involving patients and families, and the benefits of this approach. In addition, they provide examples that show how strong linkages with clinical operations, academic researchers and community partners have enabled the successful spread and scale of quality improvements and health innovations.
Alberta Health Services is working to embed evidence into clinical practice and accelerate its progress as a learning, sustainable and high-performing health system. Informed, active involvement of all stakeholders is essential to this process, and SCNs provide a critical resource to achieve these goals.
Acknowledgements
The authors thank Allison Strilchuk (scientific writer with the Pan-SCN team), Tracy Wasylak (chief program officer, Strategic Clinical Networks) and Braden Manns (associate chief medical officer, Strategic Clinical Networks) for contributing content and thoughtful revisions to this manuscript.
Footnotes
Listen to a CMAJ podcast about the Strategic Clinical Networks at https://soundcloud.com/cmajpodcasts/ahs
Competing interests: All of the authors are employees of Alberta Health Services. No other competing interests were declared.
This article has not been peer reviewed.
Contributors: All of the authors contributed substantially to the concept and design of the work, revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
References
- 1.Veitch D. One province, one healthcare system: a decade of healthcare transformation in Alberta. Healthc Manage Forum 2018;31:167–71. [DOI] [PubMed] [Google Scholar]
- 2.Alberta Health Services: Get to know us. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/assets/about/org/ahs-org-about-ahs-infographic.pdf (accessed 2019 July 16). [Google Scholar]
- 3.Alberta’s Strategic Clinical Networks: past, present, future. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-reports-past-future-present.pdf (accessed 2019 Aug. 19). [Google Scholar]
- 4.Vision, mission, values & strategies. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/Page12360.aspx (accessed 2019 July 16). [Google Scholar]
- 5.Your AHS. One health system: the AHS story. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/about/Page13648.aspx (accessed 2019 July 16). [Google Scholar]
- 6.Improving health outcomes: SCN retrospective 2012–2018. Edmonton: Alberta Health Services; 2019. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-reports-retrospective-2012-2018.pdf (accessed 2019 Aug. 19). [Google Scholar]
- 7.Manns BJ, Wasylak T. Clinical networks: enablers of health system change. CMAJ 2019;191:E1299–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown BB, Patel C, McInnes E, et al. The effectiveness of clinical networks in improving quality of care and patient outcomes: a systematic review of quantitative and qualitative studies. BMC Health Serv Res 2016;16:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alberta Health Services: Strategic Clinical Networks a primer & working document (August 7, 2012– V5). Edmonton: Alberta Health Services; 2012. Available: www.albertahealthservices.ca/assets/about/scn/ahs-scn-primer.pdf (accessed 2019 July 16). [Google Scholar]
- 10.An interim analysis of SCN return on investment, value and impact, 2012–2019 [internal report]. Calgary: Alberta Health Services; September 2019. [Google Scholar]