KEY POINTS
The Respiratory Health Strategic Clinical Network (RHSCN) was launched in January 2014 with the mission to facilitate optimal respiratory health through implementation of innovative, patient-centred, evidence-informed and coordinated services.
The RHSCN Core Committee has identified asthma, chronic obstructive pulmonary disease (COPD), sleep-disordered breathing and oxygen therapy as the priorities of the network.
Key initiatives of the RHSCN include the Alberta Childhood Asthma Pathway project and the COPD order set/discharge bundle — challenging projects that require the engagement of clinical communities, opinion leaders and partners to change practice.
The ongoing engagement and investment of the clinical, research, and patient and caregiver communities is a key component to the relevance of the network.
Each year asthma exacerbations lead to 20 000 visits to an emergency department in Alberta.1 Chronic obstructive pulmonary disease (COPD) accounts for $254 million per annum in direct health care costs to the province, with 51% of these costs attributed to admissions to hospital.2 Undiagnosed and untreated obstructive sleep apnea increases the risk of cardiovascular disease, stroke, and traffic incidents.3 The burden of respiratory disease in Alberta continues to impact utilization of health care, contributes to health care costs and affects quality of life. The Respiratory Health Strategic Clinical Network (RHSCN; www.ahs.ca/rhscn) was launched in January 2014 with the mission to “facilitate optimal respiratory health through implementation of innovative, patient-centered, evidence-informed and coordinated services.”4
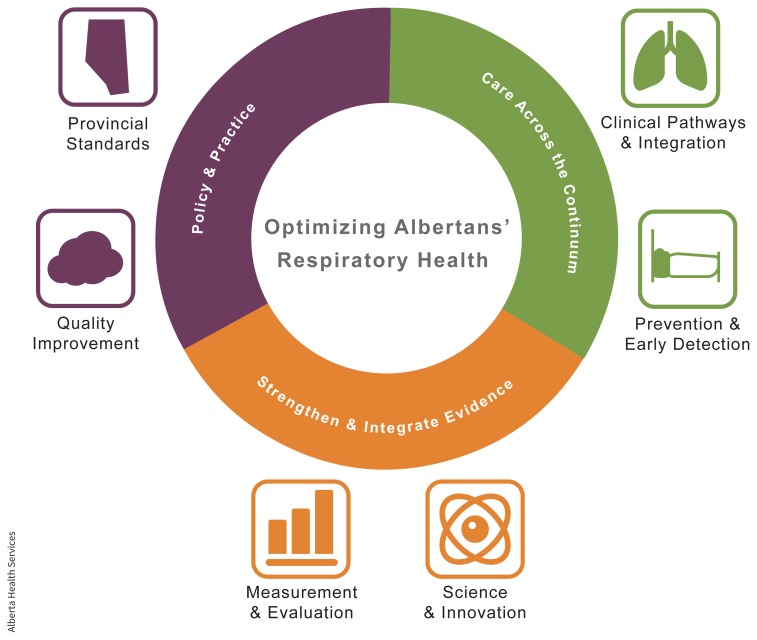
Alberta’s Strategic Clinical Networks (SCNs) support multidisciplinary teams pursuing innovative strategies with the aim of improving outcomes, patient experience and value for the Alberta health care system.5 Members of the RHSCN include a team of researchers, clinicians, policy-makers, patients and caregivers, and community partners that comprise the core committee.4 This committee, in collaboration with the RHSCN leadership team, is responsible for the creation and implementation of the Transformational Roadmap (https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-rh-transformational-roadmap-2018-2021.pdf), which guides the network’s focus and priorities (see figure).
Guided by Working Groups, the SCNs offer an opportunity to trial implementation projects with a strong link to the research community. 6 The RHSCN Core Committee identified asthma, COPD, sleep-disordered breathing and oxygen therapy as the priorities of the network. Network members guide development and implementation of initiatives that address the priorities within areas of focus outlined in the Transformational Roadmap. This bottom–up approach is a hallmark of the networks. Important focus areas include providing care across the disease continuum, integrating policy and practice, and strengthening and integrating evidence.4
The RHSCN is committed to respiratory health care, from disease prevention through diagnosis and acute management to end-of-life care.4 Two signature projects of the RHSCN include The Alberta Childhood Asthma Pathway and COPD order set/discharge bundle. The Alberta Childhood Asthma Pathway began as a regional initiative to reduce variance in the management of pediatric asthma in the emergency department and inpatient settings. The pathway has now been implemented in 105 sites across Alberta and is considered the standard of care. Building this work, a Partnership for Research and Innovation in the Health System grant is currently being used to evaluate a primary care pediatric asthma pathway, using electronic medical records and Web-based learning.7
Recognizing the burden of admissions to hospital owing to COPD, the RHSCN led the development of standardized COPD hospital admission order sets meant to reduce unwarranted variance and optimize best practice for COPD exacerbations. The standardized order sets were successfully piloted at an acute care site and resulted in an average 1-day reduction in length of stay.8 Building on this work, discharge bundles were recognized as an important tool to improve patient transition to the community and reduce risk of hospital readmission.9 In collaboration with clinicians, patients and national leaders from the Canadian Thoracic Society COPD Clinical Assembly, a Canadian discharge care bundle for patients with COPD (funded by the Partnership for Research and Innovation in the Health System) was designed to facilitate the transition from hospital to home.10 The evidence-based COPD discharge bundle includes the following core components for each patient at discharge: ensure the patient has shown adequate inhaler technique, provide a discharge summary and follow-up with primary care, optimize prescription medications, provide a written discharge plan, consider pulmonary rehabilitation referral, screen for frailty and comorbidities, and assess smoking status to assist with a smoking cessation plan.10 Implementation and effectiveness of the discharge bundle is currently being evaluated in 5 sites across Alberta.
With large-scale provincial research projects such as the Alberta Childhood Asthma Pathway and the COPD order set/discharge bundle work, there are challenges. Both projects were affected by the engagement of stakeholders and by ensuring buy-in from the clinical community. Specifically, both projects needed substantially more time to engage sites, build relationships and create a willingness to change than first anticipated. These projects required a dedicated team member to work closely with the sites, identify site-specific barriers to implementation and work with site leaders to ensure that the implementation plan was feasible. Implementation of both projects faced site-specific limitations such as competing projects, staffing changes and technology challenges, which delayed local implementation and affected uptake.
Based upon our learning from these 2 large-scale projects we have several suggestions to offer teams working outside of Alberta who are engaged in similar work. First, establish site-based teams early and identify site champions to lead the implementation and facilitate communication with the provincial team. Second, bring together site champions to discuss their strengths and challenges, offer opportunities to learn from each other and develop a network to facilitate collaboration. Third, facilitate early access to data and feedback at individual sites. As an example, within the COPD order set/discharge bundle work, the senior analyst provided site-specific data regularly to ensure each site could view their data relative to the larger provincial data and identify where improvements could be made.
Recently, the RHSCN has begun working to promote disease prevention and early detection of respiratory illness. The Tobacco Use Task Force was created to work with clinical practitioners to target prevention and cessation of tobacco use. The task force recently began a pilot project to evaluate the effect of an early smoking cessation intervention with cigarette smokers who are identified in community pharmacies.
Strategic priorities of the Respiratory Health Strategic Clinical Network (RHSCN).
Image courtesy of Alberta Health Services
The RHSCN Scientific Office focuses on science and innovation through building research capacity, facilitating uptake of evidence and guiding the RHSCN’s research priorities. Given this role, the Scientific Office recently completed a research prioritization process led by a steering committee of patient and caregiver advisors and clinicians to identify what both communities feel should be the focus of the research agenda. The research questions generated through this process will guide the work of the RHSCN Scientific Office and set direction for funding opportunities such as seed grants and studentships. As a network, the RHSCN continues to evolve to meet the needs of the clinical, research, and patient and caregiver communities more effectively. The Transformational Roadmap was refreshed in 2019 to allow for an exploration of upcoming priorities and initiatives, and to ensure the network remains aligned with stakeholders and continues to forge strong partnerships. Future work should include a stronger focus in prevention and early detection of respiratory disease. The ongoing engagement and investment of all communities is a key component to the success and relevance of the network.
The RHSCN will continue to be driven by engaged stakeholders, holding itself accountable to quality improvements that benefit patients with respiratory conditions. Going forward, the RHSCN will build on lessons learned with the aim to strengthen the relationships between clinical operations and the research community to reduce the time to implement evidence into practice, build new partnerships to further liberate and integrate respiratory data to enhance the respiratory health community’s utilization of real-world evidence, and increasingly leverage the expertise of the community to improve respiratory health for all Albertans.
Acknowledgements
The authors thank Shelley Valaire, Dr. Dale Lien, Jim Graham and Eileen Young (members of the Respiratory Health Strategic Clinical Network leadership team) for their assistance with the development of this manuscript.
Footnotes
Competing interests: Heather Sharpe is an employee of Alberta Health Services (AHS), and Michael Stickland is remunerated through a contract with AHS. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Heather Sharpe drafted the manuscript. Michael Stickland identified key elements of content, provided specific data information related to the key elements and critically revised the work for intellectual content. Both authors contributed substantially to the the design of the work, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
References
- 1.Rosychuk RJ, Youngson E, Rowe BH. Presentations to Alberta emergency departments for asthma: a time series analysis. Acad Emerg Med 2015;22:942–9. [DOI] [PubMed] [Google Scholar]
- 2.Waye AE, Jacobs P, Ospina MB, et al. Economic surveillance for chronic obstructive pulmonary disease (COPD) in Alberta [economic report]. Edmonton: Institute of Health Economics; 2016. April 12. [Google Scholar]
- 3.Knauert M, Naik S, Gillespie MB, et al. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg 2015;1:17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Respiratory Health Strategic Clinical Network Transformational Roadmap 2018–2021. Edmonton: Alberta Health Services; 2019. January 22. [Google Scholar]
- 5.Noseworthy T, Wasylak T, O’Neill B. Strategic clinical networks in Alberta: structures, processes, and early outcomes. Healthc Manage Forum 2015;28:262–4. [DOI] [PubMed] [Google Scholar]
- 6.Manns B, Braun T, Edwards A, et al. Alberta Innovates; Health Solutions Interdisciplinary Chronic Disease Collaboration. Identifying strategies to improve diabetes care in Alberta, Canada, using the knowledge-to-action cycle. CMAJ Open 2013;1:E142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cave AJ, Sharpe H, Anselmo M, et al. Primary care pathway for childhood asthma: protocol for a randomized cluster-controlled trial. JMIR Res Protoc 2016;5:e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pendharkar SR, Ospina MB, Southern DA, et al. Effectiveness of a standardized electronic admission order set for acute exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med 2018;18:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ospina MB, Mrklas K, Deuchar L, et al. A systematic review of the effectiveness of discharge care bundles for patients with COPD. Thorax 2017;72:31–9. [DOI] [PubMed] [Google Scholar]
- 10.Ospina MB, Michas M, Deuchar L, et al. Development of a patient-centred, evidence-based and consensus-based discharge care bundle for patients with acute exacerbation of chronic obstructive pulmonary disease. BMJ Open Respir Res 2018; 5:e000265. [DOI] [PMC free article] [PubMed] [Google Scholar]