Abstract
Purpose of Review:
The purpose of this review is to summarize the current state of knowledge regarding the evaluation and measurement of urinary urgency and bladder sensation.
Recent Findings:
New technologies have been developed to improve our diagnostic capabilities in urinary urgency and bladder sensation. Recent developments include MRI-based neuroimaging and novel tablet-based sensation meters that can be used during urodynamics as well as during oral hydration.
Summary:
Commonly used metrics for urinary urgency and bladder sensation include the use of validated surveys/void diaries and standardized verbal sensory thresholds during urodynamics. However, these metrics are highly subjective and prone to significant bias. There has been an evolution in evaluation metrics ranging from the use of reflex testing to electrical perception testing to the use of neuroimaging and the development of sensation meters. Neuroimaging allows for mapping of specific brain areas involved in the different phases of voiding and provides an anatomic basis for different forms of overactive bladder. The sensation meter allows for generation of real-time sensation-capacity curves which enables easy and objective comparison between patients as well as potential sub-typing of different forms of overactive bladder. In addition, new research supports the concept of differing forms of urgency and the use of novel patient-derived terminologies for urinary urgency and bladder sensation.
Keywords: Urinary Urgency, Bladder Sensation, Overactive Bladder, Urodynamics, Detrusor Overactivity, Afferent Nerves
INTRODUCTION:
The 1997 conference “The Overactive Bladder: From Basic Science to Clinical Management” launched a formally unknown term, “Overactive Bladder” (OAB), that has subsequently become widely adapted in both clinical research and pharmaceutical marketing [1]. Coined by Drs. Paul Abrams and Alan Wein, OAB has since been recognized by the International Continence Society (ICS), which defines the condition as a “syndrome characterized by symptoms of urgency, with or without urgency incontinence, usually with increased daytime frequency and nocturia” [2]. Based on this definition, OAB is at its root, a disorder of bladder sensation and urinary urgency. The condition is prevalent in both men and women and is estimated to affect up to 30 million individuals in the United States alone [3]. While the underlying pathophysiology is still unclear, symptoms of OAB are known to increase in frequency with age and exert tremendous impact on patient-reported quality of life and mental health [4].
Recognizing urgency as the sensory hallmark of OAB has been paramount in the development of clinical assessments to better understand abnormal micturition patterns. As defined by the ICS, urgency is “the complaint of a sudden compelling desire to pass urine which is difficult to defer” [2]. However, in assessing OAB as a disorder of bladder sensation, certain limitations must be recognized as they shape the context and development of urgency metrics. These include but are not restricted to the subjective nature of urgency, difficulty in standardizing descriptive terminology, distinguishing urgency from normal bladder sensation, and challenges of translating clinical observations to still-unclear pathophysiologic mechanisms [5].
However, despite the high prevalence and associated morbidity and mortality of OAB, metrics that objectively quantify bladder sensation and urinary urgency remain limited. Better-developed and more meaningful assessments in this area might allow for enhanced phenotyping of OAB and other disorders of bladder sensation. For example, novel methods utilized to identify OAB subtypes and characterize sensation may allow patients to be stratified more appropriately and effectively for treatments and clinical trials. This discussion of new concepts in urinary urgency and bladder sensation, will review previous metrics used to characterize bladder sensation, discuss methods for improved diagnosis of bladder sensation syndromes and finally, explore novel approaches to redefining urgency. Table 1 presents a list of metrics for bladder sensation and urinary urgency with discussion of advantages and disadvantages.
Table 1.
Metrics for Bladder Sensation and Urinary Urgency
| Type | Advantages | Disadvantages |
|---|---|---|
| Validated Surveys | Allow comparison of patients in different research groups | Subject to recall bias (i.e. over the past four weeks) |
| Void Diaries | Can provide timing and frequency of urgency events in non-clinical settings | Subject to recall bias and don’t fully characterize urgency events |
| Verbal Sensory Thresholds during Urodynamics | Widely used, accepted by the ICS | Episodic, poorly characterized, and mainly used during invasive urodynamics testing |
| Sensation meter | Allows for generation of real-time sensation-capacity curves during oral hydration or urodynamics | Not commercially available and validated with large scale studies and not integrated into available urodynamics systems |
| Ice Water Testing | May identify occult neuropathy during urodynamics | Only gives a yes/no response and its validity has been questioned |
| Electrical Perception Threshold Testing | Provide objective measures of sensory function | Require use of urethral catheters |
| Functional Imaging | MRI during UD studies can highlight CNS pathways involved in voiding function/dysfunction. US can a provide non-invasive method to study bladder function | MRI is expensive and requires special UD equipment. US is operator dependent and requires additional training |
ICS – International Continence Society, MRI – magnetic resonance imaging, US – ultrasound, UD – Urodynamics.
MEASUREMENT OF BLADDER SENSATION/URGENCY WITH VOID DIARIES AND VALIDATED QUESTIONNAIRES:
Bladder diaries have provided researchers with a non-invasive tool to understand bladder sensation and urinary urgency in a variety of settings. Assessment of micturition behaviors, as provided by bladder diaries, has allowed clinicians to recognize individual urgency events and track responses to treatment. Whether paper or electronic, diaries have been useful in gathering information such as frequency of micturition events, times at which they took place, fluid intake, voided volumes, incontinence events, as well as the degree of urgency as reported by the patient [2,6]. Since their clinical utility in assessing urgency in OAB was introduced, many groups have sought to customize the method to better cater to their research interests or study populations. However extensive their implementation in both clinical and research settings, several limitations, aside from self-reported data and non-compliance, remain: records are normally completed after micturition and great variation persists with regards to how long individuals should record their urinary habits (typically 1, 3, or 7+ days). Some researchers have argued that a 24-hour diary is sufficient to understanding voiding habits in certain clinical settings such as patients with motor urgency complaints [7,8]. Others maintain that multiple recorded days, either consecutive or non-consecutive, might offer additional information and internal consistency [6,9]. It must be noted that frequency-volume charts, which track micturition events and associated voided volume, are at times equated with bladder diaries, albeit less comprehensive. Like bladder diaries, validated surveys reflect simple, non-invasive methods of assessing sensation. Literature reviews seeking validated questionnaires highlight the tremendous variety available to clinicians, a factor that, while helpful in customizing individualized management, may simultaneously hamper communication across studies [10]. While both bladder diaries and questionnaires provide relatively quick and economically friendly initial evaluations of bladder dysfunction, they do not definitively capture real-time sensation and thus fall short of providing a comprehensive, mechanistic approach to investigating sensation disorders.
Another issue with the use of validated surveys is the extreme variation between different instruments. Because so many different surveys are used in both clinical practice and research, it is difficult to compare results between different centers. This makes the objective assessment of urinary urgency and sensation even more challenging. To address this problem, it is now recommended that researchers use the modular questionnaires from the International Consultation on Incontinence modular questionnaires (ICIq). These questionnaires cover most aspects of voiding dysfunction and have been validated in multiple languages. They are available for free upon request from the ICI and can be found at the website: http://www.iciq.net.
URODYNAMIC STUDIES AND VERBAL SENSORY THRESHOLDS AS METRICS FOR BLADDER URGENCY/SENSATION:
Urodynamic (UD) studies remain the gold standard for assessing urinary incontinence and bladder sensation. While debates persist over when this methodology should be applied in the course of patient management, UD studies have undeniably changed how clinicians understand lower urinary tract function. A powerful diagnostic tool, UD studies began in the 1950s and have since undergone multiple modifications in that the current variety includes uroflowmetry, cystometry, pressure flow studies, electromyography, and video urodynamics [11]. Unlike the limitations associated with void diaries and surveys, invasiveness is the main limitation of UD studies, which often require the placement of urethral and rectal catheters. Even when used appropriately and following strict guidelines, use of invasive catheters may affect our ability to interpret, validate, or generalize patient reported bladder sensations during UDS. For example, in a conventional UD study, the bladder is often filled at a rate significantly faster than physiological diuresis; these supra-physiological filling rates have been demonstrated to increase vesical pressure and decrease bladder compliance [12]. This, in addition to the artificial setting, positioning of the individual, provocation by investigators, and use of catheters, may all affect perceived sensation.
Nevertheless, the influence of UD studies on presently accepted terminology cannot be overstated. Cystometric studies of healthy individuals by Wyndaele and de Wachter represented the catalyst for current ICS-recognized verbal sensory thresholds (VSTs): first sensation, first desire, and strong desire [13,14]. Widely used in practice, including during UD studies, VSTs present one method by which researchers may trace and characterize an individual’s desire to void. Outside the relatively vague definitions provided by the ICS, there are no standardized methods to guide interpretation of VSTs in the clinical setting, making comparison across studies particularly challenging. In fact, two separate studies of lower urinary tract symptom (LUTS) patients by Erdem et al reported that some patients perceived sensation (VSTs) when 1) catheterized and without filling and 2) not catheterized [15,16]. The authors attributed these inappropriate sensations to both afferent signaling pathways and cognitive factors, with their ultimate conclusion highlighting the limitations of applying VSTs to interpret sensation.
METRICS FOR IMPROVED CHARACTERIZATION OF BLADDER SENSATION/URGENCY:
In his review of urgency assessments, Starkman et al state, “Developing a standardized instrument which measures the experience of urgency across a spectrum, or continuum of severity is one of the more arduous challenges facing researchers currently investigating OAB” [17]. While the task of objectively characterizing a highly contested and subjective aspect of OAB is undoubtedly impressive, many creative, innovative approaches have been developed to address this critical clinical and research need.
The Urgeometer:
Lowenstein et al evaluated sensation in 51 females (42 with urologic diagnoses, 9 controls) during cystometry using a lab-developed “Urgeometer,” a lever operated hand-held device used by participants to rate urgency from “No urge to void” to “Most extreme urge to void that I can imagine” [18]. Data from the device was obtained during UD filling and utilized to generate a continuous presentation of patient-reported urgency. Individuals were also asked to report first desire, strong desire, and maximum cystometric capacity, the latter determined by when the participant reported not being able to “take any more water in [their] bladder” [18]. While urgency levels remained consistent at the beginning and end of filling, the device reported significantly different urgencies when compared to standard patient-reported VSTs. Urgencies at strong desire were found to be significantly different and could be used to distinguish individual patient groups including detrusor overactivity incontinence (DOI), urodynamic stress incontinence (USI), and mixed incontinence (both USI and DOI). In this regard, the continuous generation of sensory data during UD testing provides a practical technique to improve upon the standard VST terminology.
The Ice Water Test:
Unlike the “Urgeometer,” investigations into reflex pathways involved in micturition have long played a role in detrusor overactivity research. The ice water test or bladder-cooling reflex, first presented in 1957 by Drs. Borr and Blinn, can be used to confirm intact detrusor inhibition by central nervous system upper motor neurons [19]. While the logistical and procedural details vary, the ice water test, in general, is conducted by rapidly infusing cold fluid into the bladder, thereby activating cold receptors and afferent C fibers. In healthy individuals without neurological disease, no detrusor contraction occurs thereby resulting in a negative finding. Classically, individuals with spinal cord injuries and disorders, including those with multiple sclerosis, demonstrate involuntary detrusor contractions; this is in contrast to what Drs. Borr and Blinn’s originally considered a positive test, which involved the expulsion of water less than a minute after infusion. The reflex has been shown to persist in children until the age of four or five, after which neuronal maturation permits inhibition of the reflex by upper motor neurons [20]. Clinically, not all researchers agree to implementing the test for the purposes of detecting spinal and cerebral lesions, where a positive result would suggest loss of central inhibition. It is important to note that, for unexplained reasons, damage to lower motor neurons has also been shown to result in a positive test.
Recent studies have attempted to use the ice water test to uncover occult neurological causes of detrusor overactivity in otherwise idiopathic cases. In a study of 13 idiopathic detrusor overactivity patients by Steanu et al, a positive ice water test was found in 10/13 participants; this resulted in a 54% improvement in diagnosis with the use of the ice water test as compared to traditional cystometry testing [19]. While ambiguous about their final decision on the use of ice water test in clinical practice, the team remained resolute on its speed, simplicity, and accuracy in confirming an intact reflex. Other groups, who have demonstrated increased sensitivity of the ice water test with repetition in patients with urologic complaints, maintain reservation about its use as the sole assessor of neurologic dysfunction but remain optimistic about its continued use in uncovering urinary pathology [21].
Electrical Perception Threshold Testing:
Other studies have attempted to understand afferent nerve activity and potential plasticity through electrical perception threshold testing. First described in 1972 by Dr. Frimodt-Møller, electrical perception testing is a clinically feasible technique that, similar to the ice water test, has been implemented to distinguish neuropathically driven bladder dysfunction from other causes [22]. Generally, catheter electrodes are utilized to stimulate the bladder while individuals report perceived sensations, thus providing a relatively quick, accessible tool that, while invasive, has already demonstrated utility in understanding hyposensitivity and even absent sensation [23]. While assessment of afferent nerve fiber function has been well documented in animal models, many limitations persist [24]. Attempts at establishing electrical sensory thresholds in early studies by de Wachter and Wyndaele demonstrated no correlation between electrical stimuli and patient-reported sensation [22]. Similarly studies by Laet et al and Ukimara et al also demonstrated a lack of strong evidence to support the clinical utility of electrical perception threshold testing in examining sensation in clinical practice [25,26]. However, both sets of investigators ultimately reasoned that more research towards the standardization of electrical perception thresholds was a practical and necessary next step.
Neuro-imaging Techniques:
Recently, studies of signaling pathways have also utilized neuro-imaging techniques to better understand the central modulation of both storage and elimination aspects of micturition. Gao et al implemented a non-invasive water loading protocol and captured brain scans using resting state functional magnetic resonance imaging in healthy adults [27]. Images were taken with empty bladders and right before elimination when the patient reported a strong desire to void. Like previous studies, researchers confirmed activation of executive centers (prefrontal cortex), anterior cingulate cortex, and the hypothalamus [28]. Notably, the investigators demonstrated significant differences in activation of brain centers between males and females, suggesting future consideration be given to understand these gender-related differences [27]. Central processes were also explored by Shy et al, who combined urodynamics with magnetic resonance imaging to yield an analogous network of brain activity [29]. While invasive, their protocol allows for greater precision with regards to which stage of micturition was captured on imaging. For example, these researchers aimed to distinguish the initiation of micturition from the void itself in order to further explore initiation pathways and possible pathologies. While still in the preliminary stages, this approach may guide future endeavors in network analysis and software development that seek to integrate imaging and UD data in an attempt to unravel the underlying pathological mechanisms.
REDEFINING URINARY URGENCY:
Since the ICS recognized VSTs as a method to track sensation during UD filling, many researchers have sought to better comprehend interpretation of these thresholds in UD and non-invasive water-loading protocols. While officially accepted, few guidelines have been provided for the usage of VSTs in research. In order to understand how individuals might describe their own sensation, Heeringa et al sought to lead focus group sessions during a non-invasive water loading protocol [30,31]. These group sessions were conducted separately in both healthy and OAB volunteers and resulted in a collection of sensory terminology that was found to be highly similar between the two groups. While the researchers fully acknowledged the subjective nature of the focus groups and qualitative data acquired from those sessions, rational steps were taken to limit observer bias and confirm patient reports, including the use of a validation session and strictly regulating moderator input. Participants chose to describe bladder sensation as either a pressure or tingling feeling, with OAB individuals defining urgency as either a sudden or slowly developing need to void. Volunteers noted their ability to define their sensations throughout bladder filling, an observation which researchers suggested aligned with a more continuous, rather than episodic, model of sensation development. Most importantly, both healthy and OAB participants separately characterized bladder sensation using similar terminology. This, the researchers argued, “suggests that urgency might not be a pathological sensation but an intensification of a normal desire to void that patients as well as healthy subjects can experience” [31].
Certainly, whether urgency is an escalated form of a physiological sensation or a pathological, separate feeling has been a source of continued dispute. Blaivas et al conducted a study of 48 individuals with urinary urgency, where participants were asked to complete two separate questionnaires in order to address which definition of urgency aligned most with their perceived sensations [32]. Without a bladder filling protocol, individuals completed the first questionnaire, waited a few days, and then completed the one they had not yet received. Participant interpretation of urgency did not change in all but one case, demonstrating the fidelity of responses. Nearly 69% of patients interpreted urgency as an “intensification of the normal urge to void” whereas 29% thought it was a “different sensation,” and 2% were not sure [32]. Blaivas et al advised using both definitions in future research. Furthermore, in acknowledging the complexity of their findings, the researchers reported that, while the majority of patients understood urgency as an escalation of physiological sensations, nearly 1/3 of their study population did not agree or could not decide, a finding that the researchers attributed to varying individual pathophysiology that is still not understood.
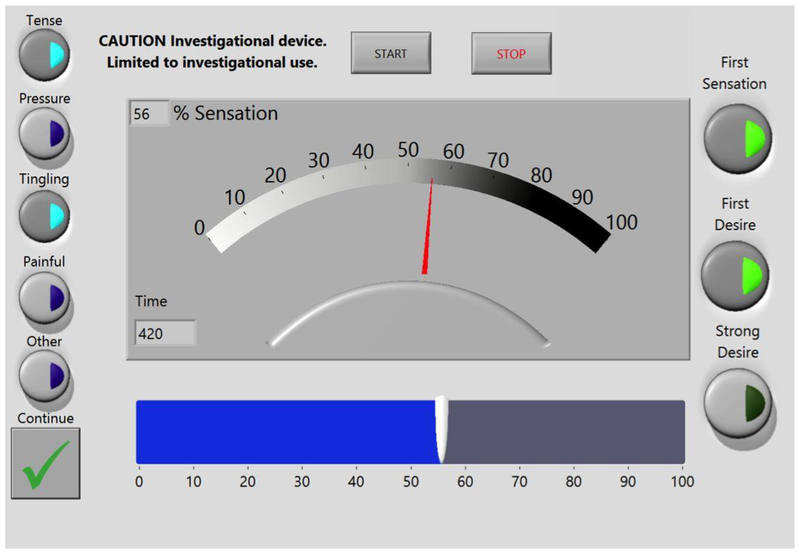
In order to better characterize urgency and development of sensation in healthy and OAB individuals, Nagle et al reported on the use of a new electronic “sensation meter,” a graphical user interface on a handheld touch-screen tablet that permits participants to rate their sensation 0–100% and record VSTs (Figure 1) [33]. Investigators conducted an accelerated hydration protocol where participants drank 2L G2-Gatorade® and underwent two fill-void cycles involving usage of the sensation meter with BladderScan® and intermittent ultrasound imaging to record filling volumes. Results demonstrated the limitations of VSTs in OAB individuals, who showed reduced consistency across the two fills. In healthy participants, sensation-capacity curves shifted left, suggesting increased sensation with faster filling. On the other hand, individuals with OAB had a right shift in their sensation curves, suggesting a paradoxical decrease in sensation with faster filling. Researchers attributed the observed increase in sensation in normal individuals to predicted visco-elastic properties of the detrusor muscle. However, they recognized that further research was needed to understand the apparent loss of sensation associated with faster filling in OAB individuals [33]. Through this initial study, the sensation meter was demonstrated to be an alternative, noninvasive, objective method capable of characterizing real-time bladder sensation in both healthy and OAB individuals.
Figure 1.
Screenshot of sensation meter with associated Start and Stop buttons, slider bar interface (bottom), and verbal sensation threshold (VST) selection (right). Screenshot represents change in sensation from example participant data. At 7 minutes (420 seconds as measured by sensation meter), the participant perceived bladder sensation at 56% (bottom), selected first desire from the VST selection (right), and marked tense and tingling from the descriptors selection (left).
Seeking validation in the device’s ability to adapt to a variable rate protocol, researchers enrolled 24 healthy individuals who underwent a similar aforementioned accelerated hydration protocol involving two fill-void cycles while using the sensation meter [34]. The updated device required individuals to mark one or more newly added sensation descriptors (tense, pressure, tingling, painful, and other) each time they recorded a sensation (0–100%), otherwise defined as a “sensation event” [35]. The study indicated that normal individuals on average marked 8–9 sensation events during both fills, regardless of the variation in fill rate. The non-invasive technique also demonstrated an acceleration of sensation during the course of filling. Tingling and pressure were chosen throughout the entire filling process whereas tense and painful were perceived at higher (>75%) sensations. While not tested on OAB individuals, this study highlighted the limitations of applying VSTs for the purposes of describing complex sensations and ultimately demonstrated the flexibility of the sensation meter, which could be employed at variable fill rates and thus applied in a range of clinical settings.
FUTURE CONSIDERATIONS:
There is no doubt that the measures discussed in this paper do not fully encapsulate the range of devices and metrics used to understand bladder sensation and urinary urgency. Furthermore, we believe that multiple modalities, both old and new, may be required to provide the most robust analysis of sensory information. In fact, many researchers have revitalized previous methods of understanding urgency and created novel techniques to improve current knowledge of underlying physiological mechanisms. Nenadic et al studied compliance of the organ in healthy and dysfunctional bladder volunteers using simultaneous ultrasound bladder vibrometry and urodynamic studies [36]. Bladder vibrometry results correlated with detrusor pressure measurements, suggesting potential for this non-invasive tool in assessing mechanical activity of detrusor muscle and even bladder function [36,37]. Others have utilized ultrasound imaging as a non-invasive means to characterize bladder biomechanics during a new type of “ultrasound urodynamics” in OAB individuals [38,39]. Results demonstrated the feasibility of this method in collecting a range of structural and functional information including tension, stress, strain, and elasticity. Investigations into the motility properties of bladder muscle by Colhoun et al have also highlighted the limitations of using traditional compliance metrics in the study of bladder function [40]. Ultimately, future investigation into overactive bladder physiology, which is necessary in grounding any clinical work, must be accompanied by addressing gaps in assessing urgency.
CONCLUSIONS:
Urinary urgency is the key symptom reported in the condition of OAB. However, a critical research objective is the identification of methods that can objectively characterize sensory information (including urinary urgency), which is often highly subjective and difficult to quantitate. Various techniques are now being utilized to achieve this objective including the incorporation of validated surveys, void diaries, verbal sensory threshold responses during urodynamics, sensation meters, ice water reflex testing, electrical perception threshold testing, and neuroimaging. Investigators are also reexamining the symptom of “urgency” as two or more different conditions and have made strides exploring new and more specific sensory terminologies. Continued study of urinary urgency and bladder sensation in basic and translational studies that aspire to incorporate multiple disciplines and modalities is the way to improve our understanding of these conditions and advance the development of new and more distinct sub-types of OAB.
FUNDING:
This work was supported by NIH R01-DK101719
Footnotes
Conflict of interest
Hameeda Naimi, John Speich, and Adam Klausner declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
In all studies performed by the authors, Institutional Review Board approval was obtained and all subjects provided informed consent for participation.
REFERENCES:
- 1.Cardona-Grau D, Spettel S (2014) History of the Term Overactive Bladder. 9:48–51. doi: 10.1007/s11884-013-0218-3 [DOI] [Google Scholar]
- 2.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A, Standardisation Sub-committee of the International Continence Society (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 3.Coyne KS, Sexton CC, Vats V, Thompson C, Kopp ZS, Milsom I (2011) National community prevalence of overactive bladder in the United States stratified by sex and age. Urology 77:1081–1087. doi: 10.1016/j.urology.2010.08.039. [DOI] [PubMed] [Google Scholar]
- 4.Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR (2012) Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol 61:88–95. doi: 10.1016/j.eururo.2011.07.049. [DOI] [PubMed] [Google Scholar]
- 5.Abrams P, Chapple CR, Junemann KP, Sharpe S (2012) Urinary urgency: a review of its assessment as the key symptom of the overactive bladder syndrome. World J Urol 30:385–392. doi: 10.1007/s00345-011-0742-8. [DOI] [PubMed] [Google Scholar]
- 6.Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN, International Urogynecological Association, International Continence Society (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20. doi: 10.1002/nau.20798. [DOI] [PubMed] [Google Scholar]
- 7.van Melick HH, Gisolf KW, Eckhardt MD, van Venrooij GE, Boon TA (2001) One 24-hour frequency-volume chart in a woman with objective urinary motor urge incontinence is sufficient. Urology 58:188–192. doi: S0090–4295(01)01136–0. [DOI] [PubMed] [Google Scholar]
- 8.Fitzgerald MP, Ayuste D, Brubaker L (2005) How do urinary diaries of women with an overactive bladder differ from those of asymptomatic controls?. BJU Int 96:365–367. doi: BJU5632. [DOI] [PubMed] [Google Scholar]
- 9.Locher JL, Goode PS, Roth DL, Worrell RL, Burgio KL (2001) Reliability assessment of the bladder diary for urinary incontinence in older women. J Gerontol A Biol Sci Med Sci 56:M32–5. [DOI] [PubMed] [Google Scholar]
- 10.Shy M, Fletcher SG (2013) Objective Evaluation of Overactive Bladder: Which Surveys Should I Use?. Curr Bladder Dysfunct Rep 8:45–50. doi: 10.1007/s11884-012-0167-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosier PF (2013) The evidence for urodynamic investigation of patients with symptoms of urinary incontinence. F1000Prime Rep 5:8–8. 10.12703/P5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klevmark B (2002) Volume threshold for micturition. Influence of filling rate on sensory and motor bladder function. Scand J Urol Nephrol Suppl (210):6–10. [DOI] [PubMed] [Google Scholar]
- 13.Wyndaele JJ (1998) The normal pattern of perception of bladder filling during cystometry studied in 38 young healthy volunteers. J Urol 160:479–481. doi: S0022–5347(01)62929-X. [PubMed] [Google Scholar]
- 14.Wyndaele JJ, De Wachter S (2002) Cystometrical sensory data from a normal population: comparison of two groups of young healthy volunteers examined with 5 years interval. Eur Urol 42:34–38. doi: S030228380200221X. [DOI] [PubMed] [Google Scholar]
- 15.Erdem E, Tunckiran A, Acar D, Kanik EA, Akbay E, Ulusoy E (2005) Is catheter cause of subjectivity in sensations perceived during filling cystometry?. Urology 66:1000–3; discussion 1003–4. doi: S0090–4295(05)01125–8. [DOI] [PubMed] [Google Scholar]
- 16.Erdem E, Akbay E, Doruk E, Cayan S, Acar D, Ulusoy E (2004) How reliable are bladder perceptions during cystometry?. Neurourol Urodyn 23:306–9; 10.1002/nau.20045. [DOI] [PubMed] [Google Scholar]
- 17.Starkman JS, Dmochowski RR (2008) Urgency assessment in the evaluation of overactive bladder (OAB). Neurourol Urodyn 27:13–21. doi: 10.1002/nau.20472. [DOI] [PubMed] [Google Scholar]
- 18.Lowenstein L, FitzGerald MP, Kenton K, Brubaker L, Gruenwald I, Papier I, Durazo-Arvizu RA, Elliot C, Mueller ER, Vardi Y (2008) Validation of a real-time urodynamic measure of urinary sensation. Am J Obstet Gynecol 198:661.e1–4; 10.1016/j.ajog.2008.02.023. [DOI] [PubMed] [Google Scholar]
- 19.Steanu ID, Albu SE, Persu C (2012) The Place of the Ice Water Test (IWT) in the Evaluation of the Patients with Traumatic Spinal Cord Injury. Maedica (Buchar) 7:125–130. [PMC free article] [PubMed] [Google Scholar]
- 20.Geirsson G, Lindstrom S, Fall M, Gladh G, Hermansson G, Hjalmas K (1994) Positive bladder cooling test in neurologically normal young children. J Urol 151:446–448. doi: S0022–5347(17)34984–4. [DOI] [PubMed] [Google Scholar]
- 21.van Meel TD, de Wachter S, Wyndaele JJ (2007) Repeated ice water tests and electrical perception threshold determination to detect a neurologic cause of detrusor overactivity. Urology 70:772–776. doi: S0090–4295(07)00605-X. [DOI] [PubMed] [Google Scholar]
- 22.De Wachter S, Wyndaele JJ (2001) Can the sensory threshold toward electrical stimulation be used to quantify the subjective perception of bladder filling? A study in young healthy volunteers. Urology 57:655–8; discussion 658–9. doi: S0090–4295(01)00914–1. [DOI] [PubMed] [Google Scholar]
- 23.De Wachter S, Smith PP, Tannenbaum C, Van Koeveringe G, Drake M, Wyndaele JJ, Chapple C (2012) How should bladder sensation be measured? ICI-RS 2011. Neurourol Urodyn 31:370–374. doi: 10.1002/nau.22214. [DOI] [PubMed] [Google Scholar]
- 24.Yamada Y, Ukimura O, Liu G, Miki T, Daneshgari F (2012) Efficacy of neuroselective and site-specific nociceptive stimuli of rat bladder. Urology 79:483.e7–483.12. doi: 10.1016/j.urology.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Laet K, De Wachter S, Wyndaele JJ (2005) Current perception thresholds in the lower urinary tract: Sine- and square-wave currents studied in young healthy volunteers. Neurourol Urodyn 24:261–266. doi: 10.1002/nau.20095. [DOI] [PubMed] [Google Scholar]
- 26.Ukimura O, Ushijima S, Honjo H, Iwata T, Suzuki K, Hirahara N, Okihara K, Mizutani Y, Kawauchi A, Miki T (2004) Neuroselective current perception threshold evaluation of bladder mucosal sensory function. Eur Urol 45:70–76. doi: S0302283803004275. [DOI] [PubMed] [Google Scholar]
- 27.Gao Y, Liao L, Blok BF (2015) Erratum to: A resting-state functional MRI study on central control of storage: brain response provoked by strong desire to void. Int Urol Nephrol 47: 10.1007/s11255-015-1057-2.[**Noninvasive hydration protocol with concurrent MRI imaging techniques which confirmed earlier studies of brain activity during micturition and suggested differences between male and female healthy individuals].
- 28.Krhut J, Tintera J, Holy P, Zachoval R, Zvara P (2012) A preliminary report on the use of functional magnetic resonance imaging with simultaneous urodynamics to record brain activity during micturition. J Urol 188:474–479. doi: 10.1016/j.juro.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Shy M, Fung S, Boone TB, Karmonik C, Fletcher SG, Khavari R (2014) Functional magnetic resonance imaging during urodynamic testing identifies brain structures initiating micturition. J Urol 192:1149–1154. doi: 10.1016/j.juro.2014.04.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heeringa R, de Wachter SG, van Kerrebroeck PE, van Koeveringe GA (2011) Normal bladder sensations in healthy volunteers: a focus group investigation. Neurourol Urodyn 30:1350–1355. doi: 10.1002/nau.21052. [DOI] [PubMed] [Google Scholar]
- 31.Heeringa R, van Koeveringe GA, Winkens B, van Kerrebroeck PE, de Wachter SG (2012) Do patients with OAB experience bladder sensations in the same way as healthy volunteers? A focus group investigation. Neurourol Urodyn 31:521–525. doi: 10.1002/nau.21232. [DOI] [PubMed] [Google Scholar]
- 32.Blaivas JG, Panagopoulos G, Weiss JP, Somaroo C (2009) Two types of urgency. Neurourol Urodyn 28:188–190. doi: 10.1002/nau.20525. [DOI] [PubMed] [Google Scholar]
- 33.Nagle AS, Speich JE, De Wachter SG, Ghamarian PP, Le DM, Colhoun AF, Ratz PH, Barbee RW, Klausner AP (2017) Non-invasive characterization of real-time bladder sensation using accelerated hydration and a novel sensation meter: An initial experience. Neurourol Urodyn 36:1417–1426. doi: 10.1002/nau.23137.[***Description of a novel sensation meter interface, which was developed to advance characterization of urgency in healthy and OAB individuals].
- 34.Naimi H, Nagle A, Vinod N, Kolli H, Sheen D (2018) Characterization of bladder sensation event descriptions during non-invasive oral hydration in healthy adults. Neurourol Urodyn 2018;37:S518–S669 (Abstract #S654). [Google Scholar]
- 35.Speich JE, Nagle AS, De Wachter SG, Klausner AP (2017) The Sensation Meter: An Unprompted Method to Characterize Patient-Reported Bladder Sensation in Real-Time:V001T04A001-V001T04A001.
- 36.Nenadic I, Mynderse L, Husmann D, Mehrmohammadi M, Bayat M, Singh A, Denis M, Urban M, Alizad A, Fatemi M (2016) Noninvasive Evaluation of Bladder Wall Mechanical Properties as a Function of Filling Volume: Potential Application in Bladder Compliance Assessment. PLoS One 11:e0157818. doi: 10.1371/journal.pone.0157818.[*Study employs noninvasive, focused ultrasound radiation in order to enhance current understanding of detrusor muscle physiology].
- 37.Bayat M, Kumar V, Denis M, Webb J, Gregory A, Mehrmohammadi M, Cheong M, Husmann D, Mynderse L, Alizad A, Fatemi M (2017) Correlation of ultrasound bladder vibrometry assessment of bladder compliance with urodynamic study results. PLoS One 12:e0179598. doi: 10.1371/journal.pone.0179598.[*Study demonstrated the utility of bladder vibrometry in evaluating changes in detrusor muscle physiology].
- 38.Nagle AS, Bernardo RJ, Varghese J, Carucci LR, Klausner AP, Speich JE (2018) Comparison of 2D and 3D ultrasound methods to measure serial bladder volumes during filling: Steps toward development of non-invasive ultrasound urodynamics. Bladder (San Franc) 5 doi: e32.[*Argues for the use of ultrasound imaging alongside UDS suggesting potential for subtyping OAB].
- 39.Nagle AS, Klausner AP, Varghese J, Bernardo RJ, Colhoun AF, Barbee RW, Carucci LR, Speich JE (2017) Quantification of bladder wall biomechanics during urodynamics: A methodologic investigation using ultrasound. J Biomech 61:232–241. doi: S0021–9290(17)30399–8.[*Argues for the use of ultrasound imaging alongside UDS suggesting potential for subtyping OAB.]
- 40.Colhoun AF, Klausner AP, Nagle AS, Carroll AW, Barbee RW, Ratz PH, Speich JE (2017) A pilot study to measure dynamic elasticity of the bladder during urodynamics. Neurourol Urodyn 36:1086–1090. doi: 10.1002/nau.23043. [DOI] [PMC free article] [PubMed] [Google Scholar]